To the editor,
A 44-year-old man with severe sarcoidosis with multiorgan involvement was referred to a tertiary care Interstitial Lung Diseases (ILD) clinic due to clinical and functional respiratory deterioration despite optimized immunosuppressive treatment. Retrospectively, the patient had been diagnosed with surgical lung biopsy 7 years prior. Since then, he had been identified to have lung involvement, with a diffuse nodular pattern on high-resolution chest CT (HRCT) and a very severe impact on lung function, ocular sarcoid disease (flame-shaped retinal hemorrhages and central serous chorioretinopathy), sarcoid liver involvement and cardiac involvement (previous PET-CT with focal hyper-enhancement pattern in the left ventricular free wall). He had been previously treated with systemic corticosteroids and successive immunosuppressors – methotrexate (15mg/week), azathioprine (2.5mg/Kg od) and leflunomide (20mg od) –, with total refractoriness. A decision was made to start anti-tumor necrosis factor (TNF) and, for the last 24 months, he had been on infliximab 5mg/kg/month, prednisolone 7.5mg od, leflunomide 15mg od and hydroxychloroquine 400mg od. The IL2 soluble-receptor (IL2-sR) reduced – 4943 pg/mL to 1992 pg/mL –, without any improvements on HRCT, lung function and symptoms. The patient had active complaints of moderate fatigue (Fatigue Assessment Scale [FAS]: 25), dyspnea on exertion (mMRC 3) and dry cough. Physical examination revealed basilar crackles on lung auscultation. Lung function tests showed a mixed pattern with a very severe airflow obstruction component – post-bronchodilator values of FEV1/FVC 0.49; FEV1 26% pred, FVC 41% pred; TLC 65% pred – and a severe decrease in DLCO-SB – 52% pred. The last HRCT revealed a diffuse nodular pattern affecting all lung lobes, with multiple nodules of variable size randomly distributed, accompanied by mediastinal and hilar lymphadenopathies. A recent PET scan showed features of increased uptake of fluorodeoxyglucose F18 (FDG-F18) throughout the lung parenchyma – maximum standardized uptake value (SUVmax) 6.6, with normalization of cardiac uptake pattern. The transthoracic echocardiogram presented normal biventricular function.
After an ILD multidisciplinary discussion, a decision was made to gradually stop infliximab and start tofacitinib 5mg bid as a fourth-line salvage treatment. After one month, the patient experienced resolution of fatigue (FAS: 13) and improvement of dyspnea on exertion (mMRC 2). Resolution of cough was observed at the three-month mark. After 11 months on tofacitinib (later increased to 15mg od), with good tolerability, there was a positive impact on lung function: post-bronchodilator values of FEV1/FVC 0.47; FEV1 31% pred (+5% absolute change), FVC 51% pred (+10% absolute change); TLC 72% (+7% absolute change) pred and DLCO-SB 63% pred (+11% absolute change). IL2-sR level reduced to 930pg/mL. A reevaluation HRCT showed a clear improvement (Figure 1), with a striking reduction in the number and size of the nodules in all lung zones, along with a reduction of mediastinal and hilar lymph nodes.
Figure 1.
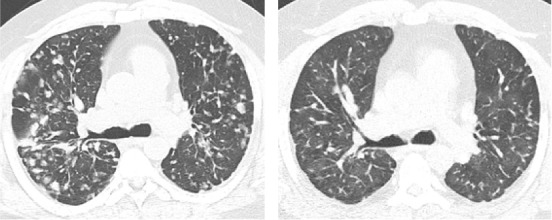
High-resolution chest tomography before (left panel) and eleven months after (right panel) tofacitinib therapy.
Tofacitinib is a type of Janus kinase (JAK) blocker which acts as an inhibitor of inflammatory immune responses. Its use is approved for several refractory immune-mediated inflammatory diseases, such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and ulcerative colitis (1). Sarcoidosis is a systemic inflammatory disorder with an unclear pathophysiology (2, 3). The use of tofacitinib in sarcoidosis is recent and favorable clinical responses have been described in a small number of patients with refractory cutaneous and/or pulmonary disease (3-8). The mechanism of action remains unknown, but has been attributed to the inhibition of type 1 immunity (9). As far as the authors know, this is the first report of a successful use of tofacitinib as a fourth-line therapy in severe refractory sarcoidosis with multiorgan involvement in Portugal. Only ten cases are reported worldwide on the use of tofacitinib in refractory disease with at least pulmonary involvement. This case illustrates the need for further prospective studies on the role of JAK-inhibitors in the context of refractory sarcoid disease.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Goll GL, Kvien TK. Generic Tofacitinib-A More Affordable JAK Inhibitor. Mayo Clin Proc. 2024;99(1):4–6. doi: 10.1016/j.mayocp.2023.11.014. [DOI] [PubMed] [Google Scholar]
- Bilgin B, Bilgin MK, Erol S, Celik G, Ozdemir Kumbasar O. Prognosis of sarcoidosis and factors affecting prognosis. Sarcoidosis Vasc Diffuse Lung Dis. 2023;40(4):e2023054. doi: 10.36141/svdld.v40i4.13244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MA, Le B, Stevens J, et al. Tofacitinib as a Steroid-Sparing Therapy in Pulmonary Sarcoidosis, an Open-Label Prospective Proof-of-Concept Study. Lung. 2021;199(2):147–53. doi: 10.1007/s00408-021-00436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damsky W, Young BD, Sloan B, Miller EJ, Obando JA, King B. Treatment of Multiorgan Sarcoidosis With Tofacitinib. ACR Open Rheumatol. 2020;2(2):106–9. doi: 10.1002/acr2.11112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerkemeyer KL, Meah N, Sinclair RD. Tofacitinib for cutaneous and pulmonary sarcoidosis: A case series. J Am Acad Dermatol. 2021;84(2):581–3. doi: 10.1016/j.jaad.2020.10.016. [DOI] [PubMed] [Google Scholar]
- Liu B, Yin H, Yang S, Lu L. Janus kinase inhibitor treatment improved both subcutaneous and pulmonary sarcoidosis in a patient with glaucoma. Clin Exp Dermatol. 2022;47(10):1868–70. doi: 10.1111/ced.15290. [DOI] [PubMed] [Google Scholar]
- Toriola SL, Satnarine T, Zohara Z, et al. Recent Clinical Studies on the Effects of Tumor Necrosis Factor-Alpha (TNF-α) and Janus Kinase/Signal Transducers and Activators of Transcription (JAK/STAT) Antibody Therapies in Refractory Cutaneous Sarcoidosis: A Systematic Review. Cureus. 2023;15(9):e44901. doi: 10.7759/cureus.44901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Huang ZS, Liu QP, Wei JC. Tofacitinib for sarcoidosis, a new potential treatment. Int J Rheum Dis. 2022;25(11):1217–9. doi: 10.1111/1756-185X.14441. [DOI] [PubMed] [Google Scholar]
- Damsky W, Wang A, Kim DJ, et al. Inhibition of type 1 immunity with tofacitinib is associated with marked improvement in longstanding sarcoidosis. Nat Commun. 2022;13(1):3140. doi: 10.1038/s41467-022-30615-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


