Abstract
Most patients diagnosed with and dying from cancer in Canada are older adults, with aging contributing to the large projected growth in cancer incidence. Older adults with cancer have unique needs, and on a global scale increasing efforts have been made to address recognized gaps in their cancer care. However, in Canada, geriatric oncology remains a new and developing field. There is increasing recognition of the value of geriatric oncology and there is a growing number of healthcare providers interested in developing the field. While there is an increasing number of dedicated programs in geriatric oncology, they remain limited overall. Developing novel methods to delivery geriatric care in the oncology setting and improving visibility is important. Formal incorporation of a geriatric oncology curriculum into training is critical to both improve knowledge and demonstrate its value to healthcare providers. Although a robust group of dedicated researchers exist, increased collaboration is needed to capitalize on existing expertise. Dedicated funding is critical to promoting clinical programs, research, and training new clinicians and leaders in the field. By addressing challenges and capitalizing on opportunities for improvement, Canada can better meet the unique needs of its aging population with cancer and ultimately improve their outcomes.
Keywords: geriatric oncology, geriatric assessment, older adults, cancer, systemic therapy, toxicity
1. Introduction
The aging population accounts for a large, predicted increase in cancer incidence in Canada [1]. However, advancements in the care of this group have lagged due to slow progress in clinical care, research, and education of providers. Older adults, aged 65 and over, account for most patients diagnosed with, and dying from, cancer [2]. Older adults face inequities in all aspects of their cancer journey from screening to diagnosis, and treatment to survivorship and end of life (EoL) care. The current system, however, is ill equipped to provide optimal care to this population, which can have increased vulnerability to stressors. Research advances suggest that geriatric assessment (GA) and management can help identify vulnerabilities, which when addressed can improve patient-related outcomes [3,4,5,6]. Despite this, development of services to help operationalize these findings is lagging. Current healthcare providers receive little training in caring for older adults. In addition, older patients are woefully under-represented in the clinical studies that form the basis of treatment recommendations. Combined, these challenges hinder improvements in care for older adults with cancer in Canada. Here, we present a synthesis of the state of geriatric oncology in Canada. This is compiled using the authors’ knowledge of published and unpublished initiatives as leaders in the field within Canada. The intent of this paper is to identify gaps and challenges in the Canadian landscape and propose a dedicated strategy to accelerate developments in clinical care, research, and education about older adults with cancer, which is imperative to improve care for this large segment of the cancer population.
2. Healthcare Inequities and Barriers to Care in Older Adults with Cancer
The aging of the Canadian population is the main driver for the rising cancer incidence. This is unsurprising, as the hallmarks of aging and cancer overlap, reflecting the same critical underlying process, i.e., accumulating cellular damage [7]. The Canadian Cancer Society (CCS) projects that two-thirds of all cancers diagnosed will be in older adults aged 65 years. Older adults therefore comprise most Canadians living with and dying from cancer [2]. This has stark implications for all healthcare workers, as older adults present unique challenges across the cancer care spectrum.
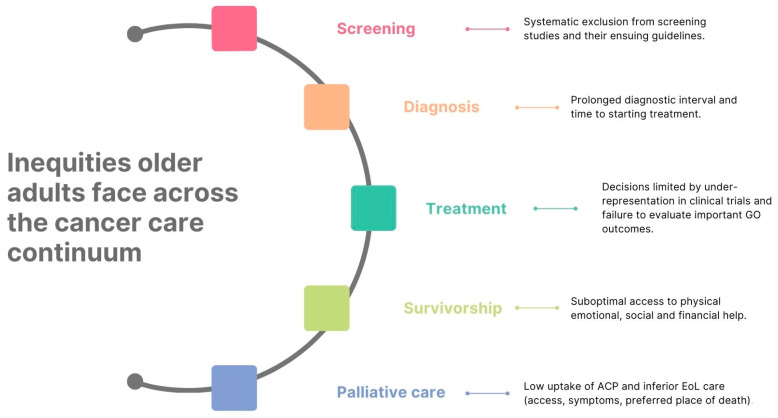
While significant survival gains from cancer have been made over the past few decades, these improvements have not been equally distributed, with large gaps seen between younger and older adults ≥65 [8]. Over three-quarters of cancer deaths are in Canadians ≥65 years of age and for most adult cancers, survival rates fall with advancing age [2]. Although this may reflect limitations in life expectancy as patients age, inequities older adults face from screening to diagnosis and treatment to survivorship and/or palliative care may also contribute, as summarized in Figure 1 [9,10].
Figure 1.
Summary of the inequities in cancer care of older adults in Canada. ACP = advanced care planning, EoL = end of life, and GO = geriatric oncology.
Older adults are less likely to be screened for cancer, a disparity that increases with age, potentially contributing to worse survival outcomes [11]. Older adults are less likely to be included in screening studies and without supporting evidence for screening, it is unsurprising that they are often systematically excluded from resulting guidelines. This particularly impacts adults ≥75 years of age [12,13,14]. Screening patients based on age, as is largely the case in Canada, requires careful consideration, as aging is heterogenous, and chronologic age does not always reflect biologic age. Health and life expectancy can vary drastically among older adults.
Older adults in Canada are at risk of experiencing longer delays until diagnosis and are less likely to be biopsied [15,16]. Diagnostic delays result in a series of negative sequalae including higher stage at presentation, more intensive treatment needs resulting in greater toxicity, and ultimately worse survival [17,18,19,20,21,22,23,24]. Older Canadians can experience further delays in treatment initiation, contributing again to cancer care inequities [25]. Evidence suggests these age-related inequalities may have widened during the COVID-19 pandemic [26,27].
From a treatment perspective, older adults remain under-represented in research studies despite representing most patients diagnosed [28]. Furthermore, those older adults who are included in studies are often highly selected, very fit patients with fewer comorbidities, and thus may not represent the average older adult seen in clinic. This may lead clinicians to be concerned about applicability of data to older, more vulnerable patients seen in clinic, where little information about the rates of toxicity in this population is available. Undertreatment may therefore result. Patient care and decision making may also be hindered by the fact that outcomes important to patients, such as the effects of treatment on function and cognition, are often not collected [29,30]. Treatment decisions may also be impacted by physician biases, relating to ageism and presumptions about patients’ desires for treatment and/or its utility [9,10]. Treatment decisions can also be influenced by patient concerns regarding transportation, financial costs, and “inconveniencing” family and friends with treatment visits, worries not always shared with their healthcare team [30].
Survivorship relates to the long-term physical, mental, emotional, social, and financial sequalae of a cancer diagnosis and treatment. In older adults, survivorship may be further complicated by chronic physical impairment that can threaten functional independence, cognitive decline with impacts on maintaining autonomy, and psychosocial concerns relating to depression and difficulties reintegrating into their community, which is essential for social well-being [31]. Although many older Canadian cancer survivors may report physical, emotional, and practical needs, over half may be unable to obtain the required help [32]. Areas highlighted as requiring improvements in survivorship care provided to older adults here in Canada relate to service delivery (particularly pertaining to side effect management), relationships (including increased support for self and caregivers), and practical assistance (notably with activities of daily living and finances) [33].
Palliative care, as recommended by the ASCO, should be received by all advanced cancer patients, early in their disease course, but delivery in older adults is complex [34]. Many of the validated tools used for symptom assessment are not adapted for older adults, with a heavy reliance on self-reporting and a strong focus on physical symptoms rather than physical functioning [35]. Where symptoms are identified, palliation is complicated by geriatric syndromes, comorbidities, and polypharmacy, with mindful prescribing and non-pharmacologic strategies needed [36]. Uptake of advanced care planning in older cancer patients is low, with provider, caregiver, and patient barriers contributing [37,38,39,40]. Being older is also a risk factor for suboptimal EoL care as it pertains to access, managing terminal symptoms (pain, breathlessness, delirium), discussions around death and dying, preferred place of death, and hospice utilization [36,41,42].
Given older adults represent most cancer patients seen in Canadian clinical practice, addressing these existing inequities, and optimizing their care, is crucial.
3. Improving Outcomes in Older Adults with Cancer—The Role of Geriatric Assessment
Older adults are a diverse population whose cancer care is often more challenging due to concomitant comorbidities, geriatric syndromes, polypharmacy, heterogenous life expectancy, and differing treatment preference, much of which is not commonly captured in routine oncologic assessment [43]. These vulnerabilities complicate oncology-directed treatment decisions, particularly systemic therapy. This can lead to both “over”- or “under”-treatment, with less fit patients receiving cancer treatment with a low likelihood of benefit and fit patients not receiving cancer treatments with a high likelihood of benefit. Both treatment decisions compromise outcomes [8,44,45].
Much attention has therefore been paid to GA. GA is a multidimensional process that seeks to evaluate a patient’s health in multiple domains, including medical, psychosocial, and functional, to identify vulnerabilities not otherwise captured through traditional oncologic assessment. While assessment is important, it is often the intervention and management that is important to capitalize on outcomes. This process of addressing identified impairments is often referred to as GA and management (GAM) or comprehensive geriatric assessment (CGA).
GA can predict several important outcomes including chemotherapy toxicity, early discontinuation of chemotherapy, functional decline, and early mortality [46,47,48,49]. It can also change oncologic treatment decisions for one in four patients [50]. Several phase III randomized controlled trial (RCT) data comparing GAM to usual oncology care have now been completed (Table 1). We present an overview of the most commonly cited and pivotal studies, with an assessment of quality (Table 2), to provider readers with an understanding of major findings supporting the use of GAM in oncology in order to provide context for the paper and recommendations. It is not meant to be a comprehensive systematic review. The authors refer interested readers to the following reviews which include additional studies conducted in this area [50,51,52]. Important proven outcomes include a reduction in moderate to severe (grade 3+) toxicity in patients receiving systemic therapy (predominantly chemotherapy) and improved rates of chemotherapy completion [3,4,5]. One study suggested GAM improved QOL in patients receiving systemic therapy [6]. However, another did not [53]. The effect of GAM on healthcare utilization was also mixed [6,53]. Importantly, no survival differences were seen in any study.
Considering this data, several international organizations, including the International Society of Geriatric Oncology (SIOG) and the American Society of Clinical Oncology (ASCO) recommend GAM in patients aged ≥65 contemplating systemic therapy [54,55]. While GA is very adaptable and can be administered in a variety of ways (e.g., self-administered, electronically, in clinic) and within different healthcare contexts (e.g., through a geriatrician, multidisciplinary team, or within the oncology clinic), uptake of GA has been poor [56]. Cited barriers include lack of knowledge on how to perform a GA, resource limitations, and lack of time [56]. The ASCO therefore updated their guidelines in 2023 to try and address these barriers, unveiling the Practical Geriatric Assessment (PGA) tool, a structured GA which prioritizes evaluation of key geriatric domains associated with cancer care outcomes, namely physical/cognitive/emotional health, comorbidities, polypharmacy, nutrition, and social support. The PGA additionally estimates chemotherapy toxicity, recognizing that validated toxicity tools for targeted treatments and immunotherapy remain lacking. For each domain in the PGA, the ASCO advise assessment measures that can be efficiently completed in clinic and provide suggestions about how to utilize findings and address vulnerabilities identified (management), an important part of improving patient outcomes and actualizing the benefits of GAM reported in randomized studies [51]. The use of PGA was a consensus recommendation by the ASCO panel (Type: Informal consensus; Evidence quality: Moderate; Strength of recommendation: Weak).
Table 1.
Summary of pivotal RCTs evaluating the impact of GA and GA-driven interventions.
| Study | Population | Intervention | Comparison | Outcome Measures | Significant Results |
|---|---|---|---|---|---|
| GAIN [3] N = 605 |
- Age ≥65 - Planned for chemotherapy ± targeted tx. 1 US center |
GA, SPICES, and CARG-TT. GA assessed domains of functional status, comorbidity, cognitive/psychological state, social activity/support, and nutritional status. SPICES evaluated common geriatric syndromes: sleep disorders, problems with eating/feeding, incontinence, confusion, evidence of falls, and skin breakdown. Results reviewed and interventions directed by geriatric trained MDT. |
Results reviewed by oncologist. | 1°: Gr ≥ 3 tx toxicity. 2°: - Chemo dose modifications and/or d/c. - ACP completion. - Healthcare utilization. - OS. |
↓ Gr ≥ 3 tx toxicity in intervention arm (50.5% vs. 60.6%, p = 0.02). ↑ in ACP completion in intervention arm (28.4% vs. 13.3%, p < 0.001). |
| GAP70+ [4] N = 718 |
- Age ≥70 - Stage III/IV - Planned for tx with high risk of toxicity - ≥1 GA domain impairment. Multiple US centers |
GA assessing domains of physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. GA summary and recommended interventions developed by study team for oncologist review. |
No GA summary or recommendations provided to oncologist. | 1°: Gr 3–5 tx toxicity. 2°: - Tx intensity. - OS. |
↓ Gr 3–5 tx toxicity in intervention arm (51% vs. 71%, aRR 0.74, p = 0.0001). ↑ likelihood of reduced tx intensity (aRR 1.38, p = 0.015). |
| GERICO [5] N = 142 |
- Age ≥70 - Stage II-IV colorectal cancer - Planned for adjuvant or 1st line palliative chemo - Life expectancy ≥3 mo - ECOG 0–2 - Vulnerability identified using G8 screening tool. 2 Danish centers |
GA assessing domains of co-morbidity, psycho-cognition, nutrition, and functional and physical status. Results reviewed and interventions directed by study team. |
SOC by oncology team. | 1°: Chemo completion with no additional dose reductions or delays (although oxaliplatin excluded). 2°: - Chemo dose reductions and/or delays. - AEs. - DFS. - PFS. - OS. - Colorectal cancer mortality. |
↑ chemo completion without additional dose reductions or delays in intervention arm (45% vs. 28%, p = 0.04). Difference most prominent with adjuvant chemo (p = 0.01) versus palliative (p = 0.75). ↓ subsequent dose reductions in intervention arm (28% vs. 45%, p = 0.04). |
| INTEGERATE [6] N = 154 |
-Age ≥70 - Planned for systemic tx. 3 Australian centers |
GA assessing domains of co-morbidities, medications, physical/cognitive/psychological social functioning, frailty, falls, nutrition, sensory impairment, immunization status, ACP, and chemo toxicity risk. Results reviewed and interventions directed by dual trained GO during serial visits. |
SOC by oncology team. | 1°: Change in hrQoL. 2°: - Functional status. - Mood. - Nutrition. - Anticancer tx modification. - Healthcare utilization. - Institutionalization. - OS. |
↓ decline in hrQoL with intervention (overall main effect p = 0.039, effect size = 0.38). ↑ ED presentations (multivariable-adjusted incidence RR 0.59, p = 0.005), unplanned hospitalizations (multivariable-adjusted incidence RR 0.60, p = 0.007), and unplanned hospital days (multivariable-adjusted incidence RR 0.77, p < 0.0001). |
| 5C [53] N = 350 |
- Age ≥70 - Referred for 1st or 2nd line adjuvant or palliative systemic tx. -Life expectancy >6 mo - ECOG 0–2. 8 Canadian centers. |
GA assessing domains of functional status, cognition, nutrition, medications, co-morbidities, mobility, and falls. Results shared with oncologist. Results reviewed and interventions directed by team of GO fellows, a geriatrician, and a nurse. |
SOC by oncology team. | 1°: QoL. 2°: - Functional limitations. - Gr 3–5 tx toxicity and/or d/c - Tx modification. - OS. |
No significant difference in any 1° or 2°. outcome. |
| Dumontier et al. [57]. N = 160 |
- Age ≥75 -Hematologic malignancy -not eligible for transplantation -initial consultation with hematologist-oncologist -Frail and pre-frail patients 1 US center |
Consultation by a geriatrician. GA included assessment of function, falls, comorbidity, polypharmacy, cognition, mood, and nutrition. |
Standard of care | 1°: OS at 1 year. 2°: -unplanned healthcare utilization within 6 months (ED visits, unplanned hospitalization admissions, days in hospital). -documented end-of-life goals of care discussions. |
No difference in survival at 1 year (18.3% vs. 21%, p = 0.65). Increased odds of EOL goals-of-care discussions (OR 3.12). No difference in ED visits, hospital admissions or duration of hospital stay. |
Abbreviations: AE = adverse event; aRR = adjusted risk ratio; CARG-TT = Cancer and Aging Research Group chemotherapy toxicity tool; chemo = chemotherapy; d/c = discontinuation; DFS = disease-free survival; ECOG = Eastern Cooperative Oncology Group; ED = Emergency Department; GA = geriatric assessment; GO = geriatric oncologist; Gr = grade; hrQoL = health-related quality of life; MDT = multidisciplinary team; mo = months; OR = odds ratio; OS = overall survival; PFS = progression-free survival; QoL = quality of life; RR = rate ratio; SOC = standard of care; tx = treatment; US = United States; 1° = primary; 2° = secondary; ↓ = decreased; and ↑ = increased.
Table 2.
Study quality assessment of pivotal RCTs evaluating the impact of GA and GA-driven interventions.
| Trial | Adequate Randomization | Concealed Allocation | Sufficient Sample Size | Similar Groups | Double Blinded | Validated and Reliable Measures | Adequate Follow Up | ITT Analysis | Overall Potential Risk of Bias ✩ |
|---|---|---|---|---|---|---|---|---|---|
| GAIN [3] | √ | √ | √ | √ | × | √ | √ | √ | Low |
| GAP70+ [4] | √ | √ | √ | × | × | √ | √ | ? | Low–moderate |
| GERICO [5] | √ | ? | √ | √ | × | √ | √ | √ | Low–moderate |
| INTEGERATE [6] | √ | √ | √ | √ | × | √ | √ | √ | Low |
| 5C [53] | √ | √ | √ | √ | × | √ | √ | √ | Low |
| Dumontier et al. [57] | √ | ? | √ | √ | × | √ | √ | √ | Low–moderate |
Note: √ indicates criteria were met; × indicates criteria were not met; ? indicates insufficient detail, not reported, and/or uncertain if criteria were met. ✩ Ratings are based on the estimation of whether the criterion was met and extent of potential bias, not simply on reporting. Abbreviations: ITT, intention to treat.
4. Current State of Geriatric Oncology in Canada
Geriatric oncology (GO) is a new and developing field. In some countries, such as the United States and France, GO is more firmly established with formal training programs, focused GO clinical programs, and a robust GO presence in clinical trials. In Canada, however, the field of GO is less well established. Below, we outline the current state of GO in Canada.
4.1. Clinical Care
Currently, there are only five specialized GO clinical programs, all concentrated within Eastern Canada. Three are in Quebec (Montreal, Sherbrooke, and Levis) and two in Ontario (both in Toronto) [58]. A previously identified clinic in British Columbia has closed. A recent initiative funded by a pharmaceutical company to connect clinicians who care for older adults with breast cancer has also resulted in discussions to establish more formalized connections between oncologists and geriatricians in Alberta and in Sault Ste. Marie.
Montreal has the most established program, which has been operational for more than 15 years [58]. Patient volume varies, with two of the GO programs reporting that they see 100–300 new consults annually, compared to fewer than 50 new consults annually at the other three centres. Fitness for treatment, multimorbidity, and cognition are the most common reasons for consultation. Between one and four physicians are involved in each clinic. Access to allied health professionals is highly variable. Some programs are well supported but most have limited or no multidisciplinary support. Beyond these specialized clinics, it is difficult to capture if and how GO is being delivered during routine oncology visits. A survey of Canadian healthcare professionals working in medical, radiation, and surgical oncology found one in four respondents screen for frailty in their daily practice, but the use of a formal screening tool was uncommon, as was the use of the Cancer and Aging Research Group chemotherapy toxicity risk calculator. Commonly cited reasons for not doing so included lack of knowledge about the tools, inadequate resources to follow-up on screening results, and time constraints. Collaboration between oncology and geriatrics was also uncommon, predominantly due to poor access to or availability of geriatricians, and to a lesser extent lack of time and knowledge [59].
4.2. Research
Several Canadian clinicians/researchers have dedicated programs of research studying issues pertaining to older adults with cancer. This research ranges from prospective studies in GA to systematic reviews/scoping reviews on GO topics to economic analyses to qualitative work assessing how older adults make decisions [60,61,62,63,64,65]. A highlight of Canadian contributions to the field includes the 5C RCT (described in Table 1) comparing GA and management with usual oncologic care. This study represented one of the first research collaborations resulting from the Canadian Network on Aging and Cancer (CNAC), a network of healthcare professionals interested in improving care for older adults with cancer through clinical, research, and educational initiatives [53].
In addition to this, an increasing number of clinicians and researchers have sought to answer questions related to the clinical care of older adults with cancer, such as why they are undertreated [66,67]. As older adults are often excluded from clinical studies, particularly therapeutic studies, new strategies to target older adults with cancer such as pragmatic, simplified study designs are being used to try to address this. An example is the REaCT-70 study (currently actively recruiting), evaluating the harms and benefits of endocrine therapy in patients 70 years and older, with lower risk breast cancer [68].
4.3. Education
Despite the growing proportion of patients seen who are older, there is no established curriculum in GO within oncology training in Canada. A recently conducted study suggests that more than three quarters of medical oncology trainees receive some exposure to GO, though the majority receive between 1 and 5 h of formal training over the course of two years of training [69]. Most of this training (59.6%) is in the form of clinical teaching. Data also suggest more than half of Canadian radiation oncology trainees lack confidence in managing geriatric issues such as comorbidities, polypharmacy, and functional and cognitive impairments, with 73% reporting that additional training in these areas would be helpful [70].
Unlike in the United States, there is no established pathway to dual geriatrics and oncology certification in Canada. A growing number of clinicians, however, have pursued additional training in GO, many of whom now lead the development of the field in Canada. In Canada, there is a GO fellowship at McGill University which has trained six clinicians (geriatricians and a radiation oncologist) but the lack of established funding for interested candidates remains an important barrier. There is also now a fellowship program at the Princess Margaret Cancer Centre, supported by philanthropy, which has trained eight medical oncologists and geriatricians, with an additional two currently enrolled. Additional trainees have completed Informal (ad hoc) fellowship programs in other parts of Canada, such as at the Ottawa Regional Cancer Centre and the Sunnybrook Cancer Centre.
Gaps in GO knowledge and skills also exist in practicing Canadian healthcare professionals. A CNAC-led survey of predominantly physicians and nurses found respondents lacked confidence in issues relating to mental health, polypharmacy, GO models of care, and helping patients recover function post-treatment [59]. Educational workshops and meetings for Canadian healthcare professionals are emerging, including an annual Canadian GO conference, organized by the CNAC, with the fourth held in 2023 in Ottawa. The Canadian Association of Nurses in Oncology (CANO) has an established special interest group in GO which has held several workshops and webinars. In addition, several specialty organizations, including the Canadian Association of Medical Oncologists (CAMO), Canadian Association of General Practitioners in Oncology (CAGPO), and Canadian Association of Pharmacy in Oncology (CAPhO) have also included GO topics at their annual conferences.
5. Challenges, Opportunities and a Call to Action to Improve Care for Older Adults
Older adults with cancer in Canada continue to face challenges in accessing equitable healthcare as it relates to screening, diagnosis, treatment, survivorship, and palliative care. Despite phase III data supporting the benefits of GA, implementation within routine oncology practice remains challenging, and access to specialized GO clinical services remains limited in Canada. Advancing the field of GO has been further hindered by the research and educational challenges previously described.
There are, however, opportunities to improve GO within the Canadian healthcare system. There is a growing number of newly trained oncologists and geriatricians interested in this field. Many have pursued additional GO training and within their faculty positions, and are helping to advance the care of older adults with cancer in Canada. As Canada’s population continues to age, bringing with it a rise in cancer incidence, now more than ever, attention must be paid to GO. The authors make a call to action to improve the care we provide to this vulnerable patient population (Table 3).
Table 3.
Summary of challenges and opportunities to accelerate development of GO in Canada.
| Challenges |
| Lack of recognition by clinicians of benefits of GO beyond current oncologic care |
| Clinician biases and nihilism resulting in inequities in management of older adults with cancer |
| Paucity of data to guide ideal management of older adults with cancer due to under-representation in studies |
| Lack of training in caring for older adults with cancer |
| Lack of dedicated funding supporting initiatives in GO (clinical, research, and educational) |
| Opportunities |
| Growing interested in GO with more clinicians pursuing additional training in GO |
| Growing cadre of clinicians trained in GO to lead development of GO programs, research, and training |
| Call to Action |
| Improve access to GO and integrate it into oncology culture |
| Change attitudes of clinicians towards older patients and towards value of GO |
| Educate clinicians about the added value of GA and GO |
| Increase the availability and visibility of GO in oncology -Train nurses to screen older adults with cancer with geriatric screening tools -Encourage and support the development of GO services through policy and dedicated funding |
| Consider novel methods of delivering and integrating GA into clinical care |
| Engage with cancer care organizations and politicians to develop a coordinated strategy to advance care of older adults with cancer in Canada |
| Education |
| Incorporate GO training into training programs for oncology trainees and allied healthcare professionals working with cancer patients. Lobby for GO curricula to be formally recognized and included in oncology training (including exams) |
| Establish dedicated funding supporting training for trainees interested in pursuing additional training in GO |
| Research |
| Stimulate research and the development of research programs in GO through funding specifically earmarked for research in this population |
| Foster collaborations between GO researchers and established national networks to increase study opportunities for older adults with cancer |
| Encourage research into implementation sciences to help develop novel methods to integrate GA into clinical care |
Improving outcomes for older adults with cancer will require a shift in oncology culture and attitude. Although many clinicians recognize that this population has unique needs, some clinicians believe they “already take care of older adults” and do not recognize the value of geriatric-oncology-specific care. To many, GO remains a “niche” specialty, inhibiting its uptake and integration into oncology culture [71]. Some clinicians may also harbor negative biases with respect to perceived benefits of treating older adults. The “very old” (≥80 years) are particularly vulnerable as they are less likely to be investigated, referred, and treated [11]. These attitudes must change.
To accelerate progress, more formal recognition and acceptance of the value of geriatric care within the field of oncology is needed. This comes from education of healthcare providers about the benefits of GA and/or geriatric input within the context of cancer care, as well as better and more timely access to specialists with expertise in geriatrics and/or GO. Training nurses to screen older patients to identify those who may benefit from a formal GA can also help to sensitize clinicians on an ongoing basis to considering geriatric-related concepts in patient care, as well as give patients access to some sort of GA. Establishment of GO services is also important. Developing such services would encourage collaboration, giving oncologists the opportunity to interact with geriatricians and directly experience the benefits of co-managing older cancer patients, including bidirectional learning and establishing a common understanding and language about caring for this patient population. In some cases, beginning with a collaborative model allows motivated oncologists to learn to address GO issues without direct ongoing support from geriatricians.
Education of the workforce is important to help accelerate improvements in the care of older adults with cancer. While clinicians with a dedicated interest in GO is important, the reality is that the growth of this patient population will outstrip their capacity to provide care and the care of older adults with cancer will remain under the purview of cancer specialists and their teams. To touch most older adults affected by cancer, and to improve their care, training of the greater oncology workforce is essential. Formal recognition and incorporation of GO training into Canadian oncology residency training by governing bodies, such as the Royal College of Physicians and Surgeons of Canada, is thus essential to ensure delivery of curricula to trainees in various programs, as well as demonstrating to trainees the importance of this topic within their profession.
Expanding research programs in GO in Canada is important to stimulate advances in the field and ultimately improve care of older adults with cancer. Development of a critical mass of researchers in the field is important to cultivate a variety of research skillsets and expertise upon which effective collaboration can occur. This can also provide mentorship and inspire young researchers to become interested in the field. Development of a network to connect researchers who work in different centers can help promote collaboration, reduce duplication of work, and accelerate advancements in the field. Formal collaborations with established research entities such as the Canadian Cancer Trials Group and the Cancer and Aging Research Group would be advantageous. While work remains to be done in multiple facets of GO, research in implementation sciences to look at alternate methods to implement GA (including nursing-led GA, patient self-reported GA, and systematic screening) would be timely and impactful, particularly due to increased demands on oncologists due to more effective and tolerable cancer treatment options available.
Funding is critical to accelerating progress in all the aforementioned areas. Clinicians are increasingly interested in providing GO services but establishing programs has been limited by financial constraints. Recognition by the government of the value of such programs through the allocation of funding would help accelerate the development of GO services, allowing older adults in a variety of locales greater access to the benefits of GA. The result of a recent economic analysis suggests that GO clinics can save the government healthcare dollars (more than CAD 7000 per patient assessed) [62]. Dedicated calls for research related to older adults with cancer, by organizations such as the Canadian Cancer Society and the Canadian Institutes of Health Research, would convey value to researchers and encourage them to engage in this field. Lastly, dedicated and consistent funding for fellowships in GO would help train clinicians who can develop and implement GO services and help to lead the development of the field in Canada.
In addition to increased funding, the authors call for a purposeful and coordinated plan to engage cancer care organizations and politicians involved in healthcare administration. This is important in advancing the care of older adults with cancer in Canada. As an initial step, a study of the current state of affairs in geriatric oncology in Canada would be helpful, including formal characterization of available clinical programs and current outcomes in older adults with cancer. Subsequently sharing evidence of improvements from interventions on outcomes that positively impact patients but also society at large would be beneficial. This plan must involve collaboration with older adults and their caregivers who can advocate for perceived priorities but also provide real stories and faces to the unique problems facing this patient population.
6. Conclusions
In summary, although older adults with cancer comprise an increasing proportion of patients diagnosed with and who die of cancer, advances in their care have been slow and there remain barriers to them receiving optimal caring. Data support that GA and management improves outcomes for patients. Given the already aging population, there is an urgency to implement measures that improve clinical care and outcomes for these patients, educate providers about their needs, and accelerate research, including how best to operationalize the benefits of GA into clinical care. While there is already increasing recognition of this populations’ needs, recognition and establishment of more clinical GO programs, dedicated funding, and encouragement of research in the field is needed to help accelerate current efforts to address the needs of this aging population and ultimately to improve their outcomes.
Author Contributions
Conceptualization, all authors; methodology, S.C., S.A., R.M., M.-F.S., C.M., D.L., D.D., R.P., X.Z., K.A.G. and T.H.; data curation, S.C. and T.H.; writing—original draft preparation, S.C. and T.H.; writing—review and editing, all authors; supervision, T.H.; funding acquisition, K.A.G. and T.H. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
None of the authors have any relationship, financial or otherwise, which influenced the content of this review article. Some authors have advisory relationships with private companies which are described below. These did not impact or contribute in any way to the manuscript. Sarah Cook: None; Shabbir Alibhai: none; Rajin Mehta: none; Marie-France Savard: advisory roles for AstraZeneca, Lilly, Seagen, Roche, Gilead, Novartis, Knight, and Merck; Caroline Mariano: none; Dominique LeBlanc: consultation/advisory roles for AstraZeneca and Novartis and consultation/advisory/speaker roles for Pfizer; Danielle Desautels: consultation/advisory roles for Astrazeneca, Merck, Gilead, Pfizer, and Novartis and speaker fees for Amgen; Xiaofu Zhu: advisory roles for Pfizer, Novartis, Lilly, AstraZeneca, Genomic Health, Apobiologix, Merck, Leo Pharma, Amgen, Taiho Pharma, and Roche and educational support from Taiho Pharma and Novartis; Rossanna Pezo: advisory roles for Pfizer, Novartis, and Lilly; Karen A Gelmon: consultation/advisory roles for AstraZeneca, Pfizer, Novartis, Seagen, Merck, Lilly, Gilead, Celcuity, and City of Hope; Tina Hsu: advisory roles for Pfizer, Knight Therapeutics, Eisai, Ipsen, Mylan, and Apobiologix.
Funding Statement
No funding was obtained for the open access and article processing charge for this publication.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Canadian Cancer Society . Canadian Cancer Statistics, 2015. Canadian Cancer Society; Toronto, ON, Canada: 2015. [Google Scholar]
- 2.2. Canadian Cancer Statistics Advisory Committee in Collaboration with the Canadian Cancer Society, S.C. 2021. Canadian Cancer Statistics 2021. [(accessed on 13 April 2023)]. Available online: https://www.cancer.ca/Canadian-Cancer-Statistics-2021-EN.
- 3.Li D., Sun C.L., Kim H., Soto-Perez-de-Celis E., Chung V., Koczywas M., Fakih M., Chao J., Chien L.C., Charles K., et al. Geriatric Assessment–Driven Intervention (GAIN) on Chemotherapy-Related Toxic Effects in Older Adults With Cancer. JAMA Oncol. 2021;7:e214158. doi: 10.1001/jamaoncol.2021.4158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohile S.G., Mohamed M.R., Xu H., Culakova E., Loh K.P., Magnuson A., A Flannery M., Obrecht S., Gilmore N., Ramsdale E., et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): A cluster-randomised study. Lancet. 2021;398:1894–1904. doi: 10.1016/S0140-6736(21)01789-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lund C.M., Vistisen K.K., Olsen A.P., Bardal P., Schultz M., Dolin T.G., Rønholt F., Johansen J.S., Nielsen D.L. The effect of geriatric intervention in frail older patients receiving chemotherapy for colorectal cancer: A randomised trial (GERICO) Br. J. Cancer. 2021;124:1949–1958. doi: 10.1038/s41416-021-01367-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soo W.K., King M.T., Pope A., Parente P., Dārziņš P., Davis I.D. Integrated Geriatric Assessment and Treatment Effectiveness (INTEGERATE) in older people with cancer starting systemic anticancer treatment in Australia: A multicentre, open-label, randomised controlled trial. Lancet Healthy Longev. 2022;3:e617–e627. doi: 10.1016/S2666-7568(22)00169-6. [DOI] [PubMed] [Google Scholar]
- 7.López-Otín C., Blasco M.A., Partridge L., Serrano M., Kroemer G. The Hallmarks of Aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeng C., Wen W., Morgans A.K., Pao W., Shu X.O., Zheng W. Disparities by Race, Age, and Sex in the Improvement of Survival for Major Cancers: Results From the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program in the United States, 1990 to 2010. JAMA Oncol. 2015;1:88–96. doi: 10.1001/jamaoncol.2014.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dharmarajan K.V., Presley C.J., Wyld L. Care Disparities Across the Health Care Continuum for Older Adults: Lessons From Multidisciplinary Perspectives. Am. Soc. Clin. Oncol. Educ. Book. 2021;41:e215–e224. doi: 10.1200/EDBK_319841. [DOI] [PubMed] [Google Scholar]
- 10.Tucker-Seeley R.D., Wallington S.F., Canin B., Tang W., McKoy J.M. Health Equity for Older Adults With Cancer. J. Clin. Oncol. 2021;39:2205–2216. doi: 10.1200/JCO.21.00207. [DOI] [PubMed] [Google Scholar]
- 11.DeSantis C.E., Miller K.D., Dale W., Mohile S.G., Cohen H.J., Leach C.R., Sauer A.G., Jemal A., Siegel R.L. Cancer statistics for adults aged 85 years and older, 2019. CA Cancer J. Clin. 2019;69:452–467. doi: 10.3322/caac.21577. [DOI] [PubMed] [Google Scholar]
- 12.Canadian Task Force on Preventive Health Care Recommendations on screening for colorectal cancer in primary care. Can. Med. Assoc. J. 2016;188:340–348. doi: 10.1503/cmaj.151125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canadian Task Force on Preventive Health Care Recommendations on screening for lung cancer. Can. Med. Assoc. J. 2016;188:425–432. doi: 10.1503/cmaj.151421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klarenbach S., Sims-Jones N., Lewin G., Singh H., Thériault G., Tonelli M., Doull M., Courage S., Garcia A.J., Thombs B.D. Recommendations on screening for breast cancer in women aged 40–74 years who are not at increased risk for breast cancer. Can. Med. Assoc. J. 2018;190:E1441–E1451. doi: 10.1503/cmaj.180463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sikdar K.C., Dickinson J., Winget M. Factors associated with mode of colorectal cancer detection and time to diagnosis: A population level study. BMC Health Serv. Res. 2017;17:7. doi: 10.1186/s12913-016-1944-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castelo M., Paszat L., Hansen B.E., Scheer A.S., Faught N., Nguyen L., Baxter N.N. Comparing Time to Diagnosis and Treatment Between Younger and Older Adults With Colorectal Cancer: A Population-Based Study. Gastroenterology. 2023;164:1152–1164. doi: 10.1053/j.gastro.2023.02.024. [DOI] [PubMed] [Google Scholar]
- 17.Tørring M.L., Frydenberg M., Hansen R.P., Olesen F., Hamilton W., Vedsted P. Time to diagnosis and mortality in colorectal cancer: A cohort study in primary care. Br. J. Cancer. 2011;104:934–940. doi: 10.1038/bjc.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomson C.S., Forman D. Cancer survival in England and the influence of early diagnosis: What can we learn from recent EUROCARE results? Br. J. Cancer. 2009;101:S102–S109. doi: 10.1038/sj.bjc.6605399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richards M.A. The size of the prize for earlier diagnosis of cancer in England. Br. J. Cancer. 2009;101:S125–S129. doi: 10.1038/sj.bjc.6605402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coates A.S. Breast cancer: Delays, dilemmas, and delusions. Lancet. 1999;353:1112–1113. doi: 10.1016/S0140-6736(99)00082-3. [DOI] [PubMed] [Google Scholar]
- 21.O’Rourke N., Edwards R. Lung Cancer Treatment Waiting Times and Tumour Growth. Clin. Oncol. 2000;12:141–144. doi: 10.1053/clon.2000.9139. [DOI] [PubMed] [Google Scholar]
- 22.Richards M., Westcombe A., Love S., Littlejohns P., Ramirez A. Influence of delay on survival in patients with breast cancer: A systematic review. Lancet. 1999;353:1119–1126. doi: 10.1016/S0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- 23.Neal R.D. Do diagnostic delays in cancer matter? Br. J. Cancer. 2009;101:S9–S12. doi: 10.1038/sj.bjc.6605384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neal R.D., Tharmanathan P., France B., Din N.U., Cotton S., Fallon-Ferguson J., Hamilton W., Hendry A., Hendry M., Lewis R., et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br. J. Cancer. 2015;112:S92–S107. doi: 10.1038/bjc.2015.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim J.O.A., Davis F., Butts C., Winget M. Waiting Time Intervals for Non-small Cell Lung Cancer Diagnosis and Treatment in Alberta: Quantification of Intervals and Identification of Risk Factors Associated with Delays. Clin. Oncol. 2016;28:750–759. doi: 10.1016/j.clon.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Ramanakumar A.V., Annie B., Frederic L., Christine B., Cathy R., Jean L. Evaluating the impact of COVID-19 on cancer declarations in Quebec, Canada. Cancer Med. 2023;12:6260–6269. doi: 10.1002/cam4.5389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker M.J., Meggetto O., Gao J., Espino-Hernández G., Jembere N., Bravo C.A., Rey M., Aslam U., Sheppard A.J., Lofters A.K., et al. Measuring the impact of the COVID-19 pandemic on organized cancer screening and diagnostic follow-up care in Ontario, Canada: A provincial, population-based study. Prev. Med. 2021;151:106586. doi: 10.1016/j.ypmed.2021.106586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernandez-Torres C., Cheung W.Y., Kong S., O’Callaghan C.J., Hsu T. Accrual of older adults to cancer clinical trials led by the Canadian cancer trials group—Is trial design a barrier? J. Geriatr. Oncol. 2020;11:455–462. doi: 10.1016/j.jgo.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Hurria A., Dale W., Mooney M., Rowland J.H., Ballman K.V., Cohen H.J., Muss H.B., Schilsky R.L., Ferrell B., Extermann M., et al. Designing Therapeutic Clinical Trials for Older and Frail Adults With Cancer: U13 Conference Recommendations. J. Clin. Oncol. 2014;32:2587–2594. doi: 10.1200/JCO.2013.55.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bumanlag I.M., Jaoude J.A., Rooney M.K., Taniguchi C.M., Ludmir E.B. Exclusion of Older Adults from Cancer Clinical Trials: Review of the Literature and Future Recommendations. Semin. Radiat. Oncol. 2022;32:125–134. doi: 10.1016/j.semradonc.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitch M.I., Nicoll I., Newton L., Strohschein F.J. Challenges of Survivorship for Older Adults Diagnosed with Cancer. Curr. Oncol. Rep. 2022;24:763–773. doi: 10.1007/s11912-022-01255-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitch M.I., Nicoll I., Lockwood G., Strohschein F.J., Newton L. Cancer survivors 75 years and older: Physical, emotional and practical needs. BMJ Support. Palliat. Care. 2021;13:e352–e360. doi: 10.1136/bmjspcare-2020-002855. [DOI] [PubMed] [Google Scholar]
- 33.Fitch M.I., Nicoll I., Lockwood G., Newton L., Strohschein F.J. Improving survivorship care: Perspectives of cancer survivors 75 years and older. J. Geriatr. Oncol. 2021;12:453–460. doi: 10.1016/j.jgo.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 34.Ferrell B.R., Temel J.S., Temin S., Alesi E.R., Balboni T.A., Basch E.M., Firn J.I., Paice J.A., Peppercorn J.M., Phillips T., et al. Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017;35:96–112. doi: 10.1200/JCO.2016.70.1474. [DOI] [PubMed] [Google Scholar]
- 35.Hui D., Bruera E. The Edmonton Symptom Assessment System 25 Years Later: Past, Present, and Future Developments. J. Pain. Symptom Manag. 2017;53:630–643. doi: 10.1016/j.jpainsymman.2016.10.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huynh L., Moore J. Palliative and end-of-life care for the older adult with cancer. Curr. Opin. Support. Palliat. Care. 2021;15:23–28. doi: 10.1097/SPC.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 37.Smith A.K., Williams B.A., Lo B. Discussing overall prognosis with the very elderly. N. Engl. J. Med. 2011;365:2149–2151. doi: 10.1056/NEJMp1109990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lum H.D., Sudore R.L., Bekelman D.B. Advance care planning in the elderly. Med. Clin. North. Am. 2015;99:391–403. doi: 10.1016/j.mcna.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 39.Volicer L., Cantor M.D., Derse A.R., Edwards D.M., Prudhomme A.M., Gregory D.C.R., Reagan J.E., Tulsky J.A., Fox E. Advance care planning by proxy for residents of long-term care facilities who lack decision-making capacity. J. Am. Geriatr. Soc. 2002;50:761–767. doi: 10.1046/j.1532-5415.2002.50175.x. [DOI] [PubMed] [Google Scholar]
- 40.Brighi N., Balducci L., Biasco G. Cancer in the elderly: Is it time for palliative care in geriatric oncology? J. Geriatr. Oncol. 2014;5:197–203. doi: 10.1016/j.jgo.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 41.Parajuli J., Tark A., Jao Y.L., Hupcey J. Barriers to palliative and hospice care utilization in older adults with cancer: A systematic review. J. Geriatr. Oncol. 2020;11:8–16. doi: 10.1016/j.jgo.2019.09.017. [DOI] [PubMed] [Google Scholar]
- 42.Lindskog M., Tavelin B., Lundström S. Old age as risk indicator for poor end-of-life care quality—A population-based study of cancer deaths from the Swedish Register of Palliative Care. Eur. J. Cancer. 2015;51:1331–1339. doi: 10.1016/j.ejca.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Hurria A., Mohile S., Gajra A., Klepin H., Muss H., Chapman A., Feng T., Smith D., Sun C.-L., De Glas N., et al. Validation of a Prediction Tool for Chemotherapy Toxicity in Older Adults With Cancer. J. Clin. Oncol. 2016;34:2366–2371. doi: 10.1200/JCO.2015.65.4327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mohile S., Dale W., Hurria A. Geriatric oncology research to improve clinical care. Nat. Rev. Clin. Oncol. 2012;9:571–578. doi: 10.1038/nrclinonc.2012.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dale W., Mohile S.G., Eldadah B.A., Trimble E.L., Schilsky R.L., Cohen H.J., Muss H.B., Schmader K.E., Ferrell B., Extermann M., et al. Biological, Clinical, and Psychosocial Correlates at the Interface of Cancer and Aging Research. JNCI J. Natl. Cancer Inst. 2012;104:581–589. doi: 10.1093/jnci/djs145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hurria A., Togawa K., Mohile S.G., Owusu C., Klepin H.D., Gross C.P., Lichtman S.M., Gajra A., Bhatia S., Katheria V., et al. Predicting Chemotherapy Toxicity in Older Adults With Cancer: A Prospective Multicenter Study. J. Clin. Oncol. 2011;29:3457–3465. doi: 10.1200/JCO.2011.34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Extermann M., Boler I., Reich R.R., Lyman G.H., Brown R.H., DeFelice J., Levine R.M., Lubiner E.T., Reyes P., Schreiber F.J., et al. Predicting the risk of chemotherapy toxicity in older patients: The Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer. 2012;118:3377–3386. doi: 10.1002/cncr.26646. [DOI] [PubMed] [Google Scholar]
- 48.Soubeyran P., Fonck M., Blanc-Bisson C., Blanc J.-F., Ceccaldi J., Mertens C., Imbert Y., Cany L., Vogt L., Dauba J., et al. Predictors of Early Death Risk in Older Patients Treated With First-Line Chemotherapy for Cancer. J. Clin. Oncol. 2012;30:1829–1834. doi: 10.1200/JCO.2011.35.7442. [DOI] [PubMed] [Google Scholar]
- 49.Hoppe S., Rainfray M., Fonck M., Hoppenreys L., Blanc J.-F., Ceccaldi J., Mertens C., Blanc-Bisson C., Imbert Y., Cany L., et al. Functional Decline in Older Patients With Cancer Receiving First-Line Chemotherapy. J. Clin. Oncol. 2013;31:3877–3882. doi: 10.1200/JCO.2012.47.7430. [DOI] [PubMed] [Google Scholar]
- 50.Hamaker M.E., te Molder M., Thielen N., van Munster B.C., Schiphorst A.H., van Huis L.H. The effect of a geriatric evaluation on treatment decisions and outcome for older cancer patients—A systematic review. J. Geriatr. Oncol. 2018;9:430–440. doi: 10.1016/j.jgo.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 51.Dale W., Klepin H.D., Williams G.R., Alibhai S.M.H., Bergerot C., Brintzenhofeszoc K., Hopkins J.O., Jhawer M.P., Katheria V., Loh K.P., et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Systemic Cancer Therapy: ASCO Guideline Update. J. Clin. Oncol. 2023;41:4293–4312. doi: 10.1200/JCO.23.00933. [DOI] [PubMed] [Google Scholar]
- 52.Anwar M.R., Yeretzian S.T., Ayala A.P., Matosyan E., Breunis H., Bote K., Puts M., Habib M.H., Li Q., Sahakyan Y., et al. Effectiveness of geriatric assessment and management in older cancer patients: A systematic review and meta-analysis. JNCI J. Natl. Cancer Inst. 2023;115:1483–1496. doi: 10.1093/jnci/djad200. [DOI] [PubMed] [Google Scholar]
- 53.Puts M., Alqurini N., Strohschein F., Koneru R., Szumacher E., Mariano C., Monette J., Hsu T., Brennenstuhl S., McLean B., et al. Impact of Geriatric Assessment and Management on Quality of Life, Unplanned Hospitalizations, Toxicity, and Survival for Older Adults With Cancer: The Randomized 5C Trial. J. Clin. Oncol. 2023;41:847–858. doi: 10.1200/JCO.22.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wildiers H., Heeren P., Puts M., Topinkova E., Janssen-Heijnen M.L.G., Extermann M., Falandry C., Artz A., Brain E., Colloca G., et al. International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients With Cancer. J. Clin. Oncol. 2014;32:2595–2603. doi: 10.1200/JCO.2013.54.8347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mohile S.G., Dale W., Somerfield M.R., Schonberg M.A., Boyd C.M., Burhenn P.S., Canin B., Cohen H.J., Holmes H.M., Hopkins J.O., et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J. Clin. Oncol. 2018;36:2326–2347. doi: 10.1200/JCO.2018.78.8687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dale W., Williams G.R., MacKenzie A.R., Soto-Perez-De-Celis E., Maggiore R.J., Merrill J.K., Katta S., Smith K.T., Klepin H.D. How Is Geriatric Assessment Used in Clinical Practice for Older Adults With Cancer? A Survey of Cancer Providers by the American Society of Clinical Oncology. JCO Oncol. Pract. 2021;17:336–344. doi: 10.1200/OP.20.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.DuMontier C., Uno H., Hshieh T., Zhou G., Chen R., Magnavita E.S., Mozessohn L., Javedan H., Stone R.M., Soiffer R.J., et al. Randomized controlled trial of geriatric consultation versus standard care in older adults with hematologic malignancies. Haematologica. 2021;107:1172–1180. doi: 10.3324/haematol.2021.278802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hernandez-Torres C., Korc-Grodzicki B., Hsu T. Models of clinical care delivery for geriatric oncology in Canada and the United States: A survey of geriatric oncology care providers. J. Geriatr. Oncol. 2022;13:447–453. doi: 10.1016/j.jgo.2022.01.004. [DOI] [PubMed] [Google Scholar]
- 59.Puts M., Szumacher E., Dawe D., Fitch M., Jones J., Fülöp T., Alibhai S.M., Hsu T., Strohschein F. Never too old to learn new tricks: Surveying Canadian healthcare professionals about learning needs in caring for older adults with cancer. J. Geriatr. Oncol. 2021;12:262–273. doi: 10.1016/j.jgo.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 60.Mian H., McCurdy A., Giri S., Grant S., Rochwerg B., Winks E., Rosko A.E., Engelhardt M., Pawlyn C., Cook G., et al. The prevalence and outcomes of frail older adults in clinical trials in multiple myeloma: A systematic review. Blood Cancer J. 2023;13:6. doi: 10.1038/s41408-022-00779-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Donison V., Chesney T.R., Wills A., Santos B., McLean B., Alqurini N., Hossain N., Durbano S., Lemonde M., Alibhai S.M.H., et al. Self-management interventions for issues identified in a geriatric assessment: A systematic review. J. Am. Geriatr. Soc. 2022;70:1268–1279. doi: 10.1111/jgs.17601. [DOI] [PubMed] [Google Scholar]
- 62.Alibhai S.M.H., Alam Z., Saluja R., Malik U., Warde P., Jin R., Berger A., Romanovsky L., Chan K.K.W. Economic Evaluation of a Geriatric Oncology Clinic. Cancers. 2022;14:789. doi: 10.3390/cancers14030789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Szumacher E., Sattar S., Neve M., Do K., Ayala A., Gray M., Lee J., Alibhai S., Puts M. Use of Comprehensive Geriatric Assessment and Geriatric Screening for Older Adults in the Radiation Oncology Setting: A Systematic Review. Clin. Oncol. 2018;30:578–588. doi: 10.1016/j.clon.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 64.Strohschein F.J. Submitting to the Momentum of Care: Processes of Treatment Decision Making Among Older People with Colorectal Cancer. McGill University (Canada) ProQuest Dissertations Publishing; Ann Arbor, MI, USA: 2019. [Google Scholar]
- 65.Sahakyan Y., Li Q., Abrahamyan L., Puts M., Brennenstuhl S., Anwar M.R., Yeretzian S., Matosyan E., Mclean B., Strohschein F., et al. Cost-utility of geriatric assessment in older adults with cancer: Results from the 5C trial. J. Clin. Oncol. 2023;41((Suppl. S16)):12012. doi: 10.1200/JCO.2023.41.16_suppl.12012. [DOI] [Google Scholar]
- 66.Ko J.J., Kennecke H.F., Lim H.J., Renouf D.J., Gill S., Woods R., Speers C., Cheung W.Y. Reasons for Underuse of Adjuvant Chemotherapy in Elderly Patients With Stage III Colon Cancer. Clin. Color. Cancer. 2016;15:179–185. doi: 10.1016/j.clcc.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 67.Chan M., Hugh-Yeun K., Gresham G., Speers C.H., Kennecke H.F., Cheung W.Y. Population-Based Patterns and Factors Associated With Underuse of Palliative Systemic Therapy in Elderly Patients With Metastatic Colon Cancer. Clin. Color. Cancer. 2017;16:147–153. doi: 10.1016/j.clcc.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 68.ClinicalTrials.gov Evaluating Harms and Benefits of Endocrine Therapy in Patients ≥70 years of Age With Lower Risk Breast Cancer. [(accessed on 18 March 2024)]; Available online: https://clinicaltrials.gov/study/NCT04921137.
- 69.Hsu T., LaDonna K., Touchie C. Use of oncology electronic learning resources to learn about geriatric oncology. J. Clin. Oncol. 2020;38((Suppl. S15)):11033. doi: 10.1200/JCO.2020.38.15_suppl.11033. [DOI] [Google Scholar]
- 70.Leifer R., Bristow B., Puts M., Alibhai S., Cao X., Millar B.-A., Giuliani M., Hsu T., Trudeau M., Mehta R., et al. National Survey Among Radiation Oncology Residents Related to Their Needs in Geriatric Oncology. J. Cancer Educ. 2019;34:9–13. doi: 10.1007/s13187-017-1244-1. [DOI] [PubMed] [Google Scholar]
- 71.Buss M.K., Lessen D.S., Sullivan A.M., Von Roenn J., Arnold R.M., Block S.D. Hematology/oncology fellows’ training in palliative care. Cancer. 2011;117:4304–4311. doi: 10.1002/cncr.25952. [DOI] [PubMed] [Google Scholar]