True arterial aneurysms are defined as a 50% increase in the normal diameter of the vessel. Clinical symptoms usually arise from the common complications that affect arterial aneurysms—namely, rupture, thrombosis, or distal embolisation. Although the aneurysmal process may affect any large or medium sized artery, the most commonly affected vessels are the aorta and iliac arteries, followed by the popliteal, femoral, and carotid vessels.
Abdominal aortic aneurysms
Aneurysms of the infrarenal abdominal aorta and iliac arteries coexist to such a degree that they may be considered a single clinical entity. Abdominal aneurysms usually affect elderly men (>65 years), with a prevalence of 5%. In England, abdominal aneurysm is responsible for over 11 000 hospital admissions and 10 000 deaths a year. Interestingly, unlike other atherosclerotic vascular disorders, the prevalence of abdominal aortic aneurysms is increasing rapidly, and aneurysmal rupture is now the 13th commonest cause of death in the Western world.
Clinical presentation
Although abdominal aneurysms may cause symptoms because of pressure on surrounding structures, about three quarters remain asymptomatic at initial diagnosis. With the exception of vague abdominal pain, clinical symptoms usually result from embolisation or rupture of the aneurysm.
The appearance of microembolic lower limb infarcts in a patient with easily palpable pedal pulses may suggest the presence of either popliteal or abdominal aneurysms. Additionally, patients with embolisation of mural thrombus from an abdominal aneurysm may present with acute limb ischaemia due to femoral or popliteal occlusion.
The diagnostic triad of hypovolaemic shock, pulsatile abdominal mass, and abdominal or back pain is encountered in only a minority of patients with ruptured abdominal aneurysms. In general, ruptured abdominal aortic aneurysm should be considered in any patient with hypotension and atypical abdominal symptoms. Similarly, the presence of abdominal pain in a patient with a known aneurysm or pulsatile mass must be considered to represent a rapidly expanding or ruptured aneurysm and be treated accordingly. In the community setting, the death rate from ruptured abdominal aortic aneurysms is almost 90%, as 80% of patients will die before reaching hospital and about 50% die during surgery to repair the rupture.
Methods of diagnosis
The sensitivity of abdominal palpation to detect aortic aneurysms increases with the diameter of the aneurysm, but palpation is not sufficiently reliable for routine diagnosis. Similarly, plain abdominal radiography shows a calcified aneurysmal aortic wall in only half of cases.
The simplest diagnostic test is B mode ultrasonography, which gives an accurate assessment of both the diameter and the site of the aneurysm. If more accurate morphological data are required to determine the exact relation of the aneurysm to the visceral or renal arteries, detailed cross sectional imaging may be obtained by computed tomography or magnetic resonance angiography.
The diagnosis of ruptured abdominal aortic aneurysms relies on clinical symptoms. Ultrasonography is used to confirm an aneurysm if it is difficult to palpate. Computed tomography has a low specificity (about 75%) for determining the presence of a rupture and adds little information to routine clinical assessment.
Indications for surgery
Elective surgery
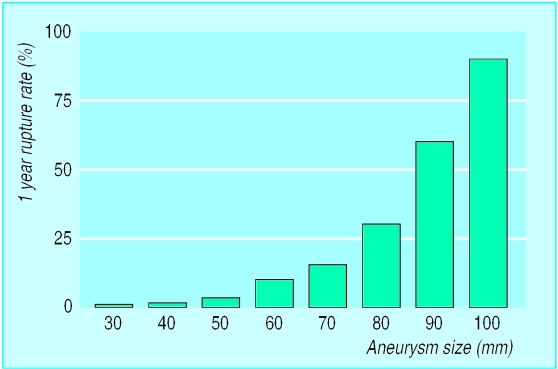
The decision to operate on a patient with an asymptomatic abdominal aneurysm is based on an analysis of the risk of aneurysmal rupture compared with the mortality of elective surgical repair. The risk of rupture is related to many factors, but the diameter of the aortic aneurysm has historically been used as the principal determinant.
Unfortunately, little information is available on the rupture rates of large abdominal aneurysms, but pooled analysis of existing data suggests that the risk of rupture increases exponentially in aneurysms above 55-60 mm. This has led to a broad surgical consensus that aneurysms exceeding 55 mm in diameter should be surgically repaired if there are no confounding factors that would substantially increase the risk of elective surgery.
The treatment for smaller aneurysms has recently been clarified by the UK small aneurysm trial, which studied 1090 patients with aneurysms of 40-55 mm. The study found a 30 day operative mortality of 5.8%, mean risk of rupture for small aneurysms of 1% a year, and no difference in survival between treatment groups at two, four, or six years. The cost for early surgery was higher than for surveillance, but early surgery was associated with improvement in some measures of quality of life.
Emergency treatment
Patients with suspected ruptured aneurysms should be considered for emergency surgical repair. Several studies have looked at preoperative risk factors and survival after emergency repair of an aneurysm. Although there is no precise scoring system that will allow accurate prediction of survival, the presence of several predictive factors (age>80 years, unconsciousness, low haemoglobin concentration, cardiac arrest, severe cardiorespiratory disease) can be used to determine patients in whom the risk of dying during surgery approaches 100%.
Factors predisposing to rupture of abdominal aortic aneurysms
Diameter of aneurysm
Diastolic blood pressure
Chronic obstructive pulmonary disease
Smoking
Family history of ruptured aneurysm
Expansion rate
Intrinsic biology—inflammation within the aortic wall
Thrombus-free surface area of aneurysm sac
Patients with symptomatic aneurysms should be treated as urgent cases and have the aneurysm repaired. The aetiology of pain from abdominal aneurysms is not well understood, although it has been attributed to stretching of the aneurysm sac or severe inflammation within the aneurysm wall (inflammatory aneurysms, see below).
Conventional surgical repair
Traditional surgical repair for asymptomatic abdominal aortic aneurysms involves exposure of the abdominal aorta, aortic and iliac clamping, and replacement of the aneurysmal segment with a prosthetic graft. Graft replacement is an effective, durable procedure, and most centres report 30 day mortality of about 5%, although this varies with the volume of work and type of hospital.
The mortality associated with surgical repair of aneurysms is closely related to the “fitness” of the patient for surgery; patients with severe cardiorespiratory disease have a perioperative mortality approaching 40%, with most deaths caused by cardiac events.
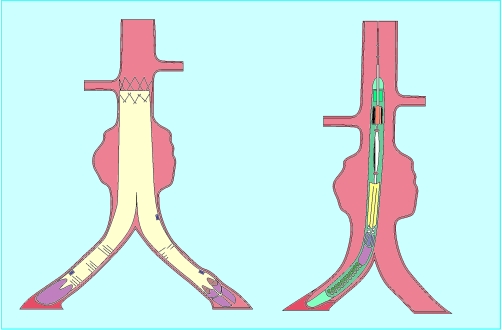
Endovascular repair
One of the major developments in vascular surgery over the past five years has been the introduction of endovascular repair of aneurysms. This technique uses an endoprosthesis, which is delivered through the femoral arteries, to exclude an aneurysm from the circulation. The endograft is secured to the normal calibre aorta and iliac arteries using metallic expandable stents and relies on subsequent thrombosis of the aneurysm to abolish the risk of rupture.
Endovascular repair has several theoretical advantages over conventional surgery, and early evidence suggests that endovascular surgery is better for patients with coexistent disease, who would be high risk for conventional surgery. However, the long term durability of endovascular techniques is unknown, although experience so far shows that up to a quarter of patients undergoing endovascular aneurysm repair will require subsequent endovascular interventions to ensure regression of the aneurysm sac. A multicentre trial of endovascular repair and conventional surgery has started in the United Kingdom.
Potential advantages of endovascular repair over conventional surgery
• No need for abdominal incision
• Avoidance of aortic cross clamping
• No retroperitoneal dissection
• Improved perioperative cardiorespiratory function
• Reduction in metabolic stress response to aortic aneurysm repair
• Improved renal and gastrointestinal function
• Reduced hospital stay
Screening and medical treatment
Ultrasonography-based screening programmes to detect and treat asymptomatic aneurysms have been proposed as a mechanism to reduce the mortality from ruptured abdominal aortic aneurysms. Screening studies report a 2.5% prevalence of abdominal aortic aneurysms larger than 40 mm in men aged over 60 years.
Advocates of community screening have suggested that a single abdominal scan in men aged 65 would exclude 90% of the population from future aneurysm rupture, and long term follow up of screened and control populations in Chichester showed an 85% reduction in rupture in the screened group. A multicentre randomised trial is currently investigating the cost-effectiveness of community based aneurysm screening.
One of the problems with screening programmes is that it identifies many people with small aneurysms. These patients are not offered any form of treatment other than ultrasonographic surveillance, which may have implications for quality of life. However, recent studies have begun to elucidate the molecular and biochemical mechanisms of aneurysm formation, and clinical trials of the effectiveness of several groups of drugs to reduce expansion of small aneurysms are likely. The most promising of these drugs in experimental studies have been inhibitors of matrix metalloproteinases.
Variants of abdominal aneurysms
Inflammatory aneurysms
Inflammatory aneurysms are characterised by a dense inflammatory infiltrate within the aneurysm wall. They are typically white in appearance and may be densely adherent to surrounding structures, which could account for the increased operative mortality in affected patients Patients typically present with fever, malaise, and abdominal pain.
Thoracoabdominal aneurysms
Thoracoabdominal aneurysms extend to a variable degree from the thoracic aorta into the abdominal aorta. They typically affect the origins of the visceral and renal arteries, which must be reimplanted into the graft during repair of the aneurysm. Mortality from repair of thoracoabdominal aneurysms is significantly higher than that for infrarenal surgery.
Peripheral aneurysms
Popliteal aneurysms comprise 80% of all peripheral aneurysms and usually exceed 20 mm in diameter. They are associated with aortic aneurysms (40% of cases), and are frequently bilateral (50%). In contrast to abdominal aortic aneurysms, patients with popliteal aneurysms usually present with acute limb ischaemia secondary to aneurysm thrombosis or distal embolisation. A diagnosis of popliteal aneurysms is suggested by easily palpable popliteal pulses and confirmed by duplex ultrasonography.
Patients who develop acute limb ischaemia due to popliteal thrombosis or embolism have a relatively poor prognosis (15% amputation rate) because of occlusion of the run off vessels. In these cases patients should have saphenous vein bypass and ligation of the popliteal aneurysm with clearance of the crural vessels by balloon thrombectomy or thrombolysis. The indications for elective surgery for asymptomatic popliteal aneurysms are based on suggestive evidence only, with most clinicians opting for surgical treatment when the aneurysm exceeds 25 mm in diameter. Results of bypass of asymptomatic popliteal aneurysms are excellent, with five year graft patency of 80% and limb salvage of 98%.
Femoral artery aneurysms are the second commonest peripheral aneurysm. Patients present with local pressure symptoms, thrombosis, or distal embolisation. Surgical treatment of true femoral aneurysms relies on the principles of excluding the aneurysm and restoration of blood flow in the limb.
Key references
Thompson MM, Sayers RD. Arterial aneurysms. In: Beard JD, Gaines P, eds. Companion to specialist surgical practice. Vol VII. Arterial surgery. London: W B Saunders, 1998.
UK Small Aneurysm Trial Participants. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet 1998;352:1649-55.
Scott RAP, Wilson NM, Ashton HA, Kay DM. Influence of screening on the incidence of ruptured abdominal aortic aneurysm: 5-year results of a randomised controlled study. Br J Surg 1995;82:1066-70.
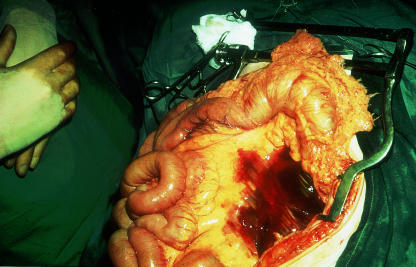
Figure.
Large infrarenal abdominal aortic aneurysm before surgical repair
Figure.
Clinical picture of “trash foot.” The appearance is caused by multiple microscopic atheromatous emboli from a large infrarenal aortic aneurysm. The presence of digital infarcts in a patient with easily palpable pulses may point to an aneurysmal source of emboli
Figure.
Ruptured abdominal aneurysm. Rupture usually occurs posteriorly into the retroperitoneum, which produces a contained leak and allows the possibility of surgical repair. Free anterior intraperitoneal rupture usually results in exsanguination
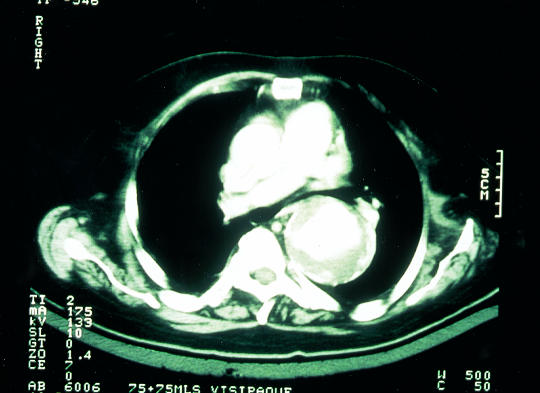
Figure.
Computed tomogram showing large infrarenal abdominal aortic aneurysm
Figure.
Annual rupture rates of abdominal aortic aneurysms according to size (based on pooled available data)
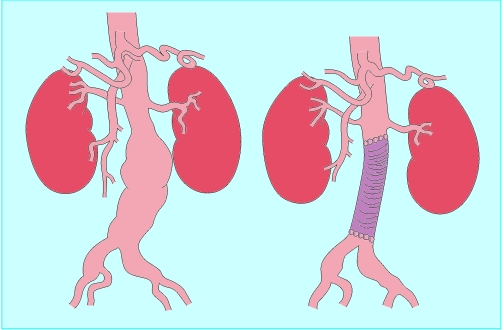
Figure.
Conventional repair of abdominal aortic aneurysm. The aneurysmal segment of the aortoiliac segment is replaced with a prosthetic vascular graft (usually Dacron or ePTFE), which is sutured to the normal arterial “cuffs” above and below the aneurysm
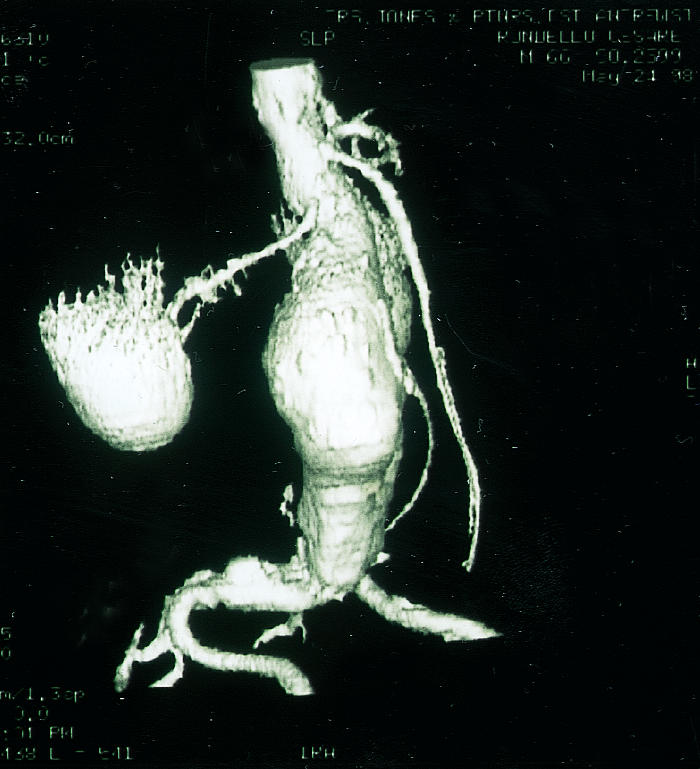
Figure.
Endovascular aneurysm repair. The aneurysm sac is excluded by an endograft, which is introduced through a remote arteriotomy and anchored above and below the aneurysm sac
Figure.
Aortoiliac aneurysm before and after exclusion by a bifurcated endovascular graft
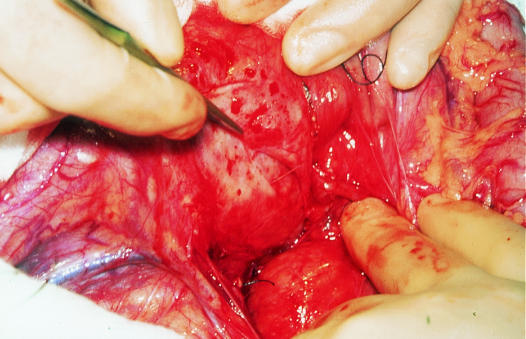
Figure.
Inflammatory abdominal aneurysm. The aneurysm is typically white in appearance and densely adherent to surrounding structures. The duodenum is being mobilised from the aneurysm sac by sharp dissection
Figure.
Computed tomogram of thoracoabdominal aneurysm
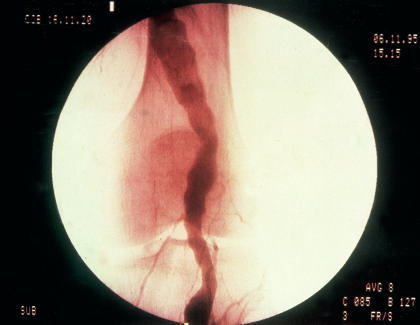
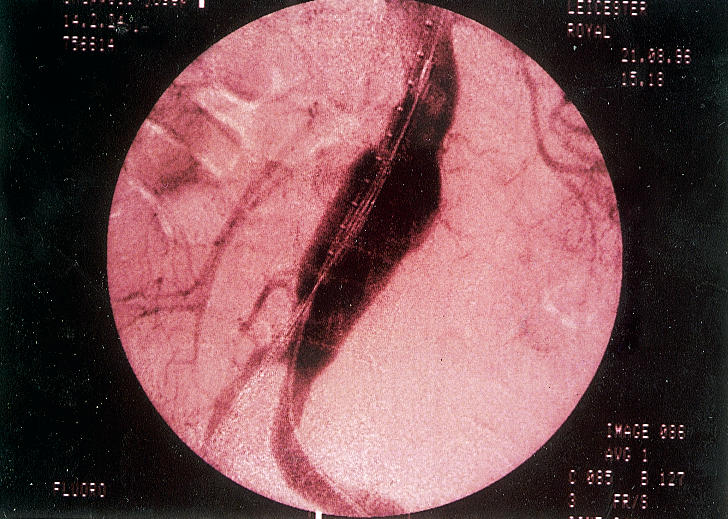
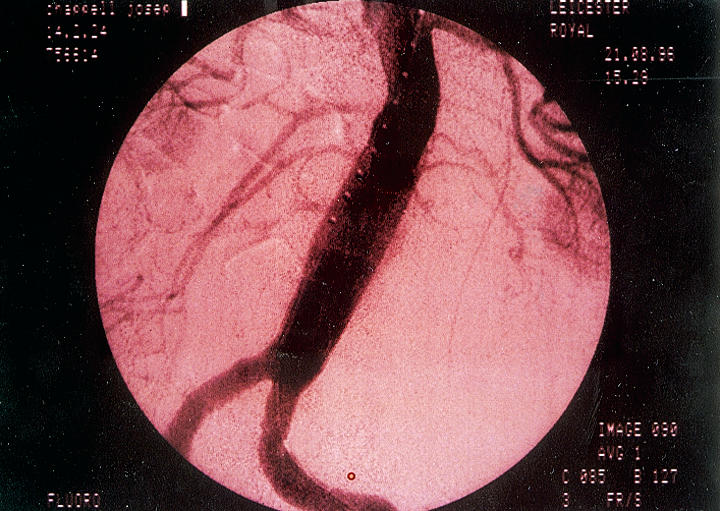
Figure.
Arteriogram of patient with popliteal artery aneurysm showing typical spiralling appearance of the superficial femoral and popliteal arteries
Footnotes
M M Thompson is consultant vascular and endovascular surgeon, Leicester Royal Infirmary (MattT11@aol.com), and P R F Bell is professor of surgery, University of Leicester.
The ABC of arterial and venous disease is edited by Richard Donnelly, professor of vascular medicine, University of Nottingham and Southern Derbyshire Acute Hospitals NHS Trust (richard.donnelly@nottingham.ac.uk) and Nick J M London, professor of surgery, University of Leicester, Leicester (sms16@leicester.ac.uk). It will be published as a book later this year.