Studies on the health effects of income inequality have generated great interest. The evidence on this association between countries is mixed,1–4 but income inequality and health have been linked within the United States,5–11 Britain,12 and Brazil.13 Questions remain over how to interpret these findings and the mechanisms involved. We discuss three interpretations of the association between income inequality and health: the individual income interpretation, the psychosocial environment interpretation, and the neo-material interpretation.
Summary points
Income inequality has generally been associated with differences in health
A psychosocial interpretation of health inequalities, in terms of perceptions of relative disadvantage and the psychological consequences of inequality, raises several conceptual and empirical problems
Income inequality is accompanied by many differences in conditions of life at the individual and population levels, which may adversely influence health
Interpretation of links between income inequality and health must begin with the structural causes of inequalities, and not just focus on perceptions of that inequality
Reducing health inequalities and improving public health in the 21st century requires strategic investment in neo-material conditions via more equitable distribution of public and private resources
Methods
We reviewed the literature through traditional and electronic means and supplemented this with correlational analyses of gross domestic product and life expectancy and of income inequality and mortality trends based on data from the World Bank,14 the World Health Organization,15 and two British sources.16,17
The individual income interpretation
According to the individual income interpretation, aggregate level associations between income inequality and health reflect only the individual level association between income and health. The curvilinear relation between income and health at the individual level18,19 is a sufficient condition to produce health differences between populations with the same average income but different distributions of income.3,20 This interpretation assumes that determinants of population health are completely specified as attributes of independent individuals and that health effects at the population level are merely sums of individual effects.21,22 In contrast, research on income inequality recognises that there may also be important contextual determinants of health. To understand these potential multilevel effects, analyses are needed that use measures of income distribution and individual income to examine health differences across individuals and aggregated units.
In examinations of health differences among individuals, contextual health effects of income distribution have remained after adjustment for individual income in most studies8–11—but not all.23 Not surprisingly, these studies found that individual income was more strongly related to individual differences in health than to income distribution. Only one study has examined the role of individual income and income distribution on health differences among aggregated units: Wolfson and colleagues used a simulation technique to explore the contribution of individual income to aggregate health differences.24 They showed that the individual mechanism explained only a modest proportion of the observed aggregate variation in mortality at the level of US states.
Though empirical tests of this hypothesis indicate that the association between income and health at the individual level is important in understanding differences in health between individuals, they also indicate that individual income may be less important in understanding variation in health across aggregated units. Policies on wages, investments, and taxes help determine the extent of unequal income distribution across the population, and this distribution then influences individual incomes. The statistical adjustment for individual income reveals an important pathway linking aggregate income inequality and individual health—but it may also encourage underestimation of the overall population effects of unequal income distribution.
The psychosocial environment interpretation
The psychosocial environment interpretation proposes that psychosocial factors are paramount in understanding the health effects of income inequality. Wilkinson has argued that income inequality affects health through perceptions of place in the social hierarchy based on relative position according to income.25 Such perceptions produce negative emotions such as shame and distrust that are translated “inside” the body into poorer health via psycho-neuro-endocrine mechanisms and stress induced behaviours such as smoking. Simultaneously, perceptions of relative position and the negative emotions they foster are translated “outside” the individual into antisocial behaviour, reduced civic participation, and less social capital and cohesion within the community. In this way, perceptions of social rank—indexed by relative income—have negative biological consequences for individuals and negative social consequences for how individuals interact. Perceptions of relative income thus link individual and social pathology.
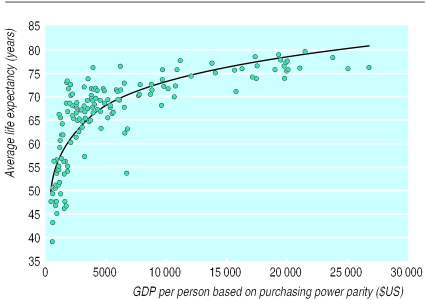
Wilkinson's demonstration that absolute income was unrelated (r=0.08) to health among developed countries has been important in staking a claim for this psychosocial theory of health inequalities.26 Figures 1 and 2 show the association between gross domestic product per person and life expectancy for 155 countries and for the 33 countries where gross domestic product was greater than $10 000—the cut-off used by Wilkinson.26 Our results, however, include data for all the countries above $10 000, not a selection of some countries in the Organisation for Economic Cooperation and Development as used by Wilkinson. The correlation between life expectancy and gross domestic product per person in the complete sample is r=0.51 (P=0.003). Thus the association between absolute income and life expectancy among wealthier countries depends on which countries are included.
Figure 1.
Gross domestic product per person in US dollars (adjusted for purchasing power parity) and life expectancy in 155 countries, circa 1993
Figure 2.
Gross domestic product per person in all 33 countries with GDP/person greater than $10 000
For 15 developed countries with comparable income inequality data, Lynch and colleagues showed that indicators of social capital, such as trust and belonging to and volunteering for community organisations, were all much more strongly related to gross domestic product per person than to income inequality.27 Diener and colleagues showed that absolute income was a better predictor of subjective wellbeing than relative income, and concluded that “exposure in natural settings to others who are better off will not automatically influence one's moods in a negative way.”28 In other analyses, social capital measured as trust and organisational membership mediated the cross sectional association between income inequality and mortality in US states.29 However, this association is difficult to interpret given that time series analyses of data from the same source show little decline in levels of trust, fairness, and helpfulness from the mid-1960s to 1994.30 The psychosocial hypothesis would lead to the expectation that these indicators of social capital should have deteriorated during this period of unprecedented increases in income inequality. In sum then, a broader consideration of relevant research raises questions about the evidence used to exclude absolute income and material conditions, and about the evidence in favour of a mainly psychosocial interpretation of health inequalities.
Areas of concern
We do not deny negative psychosocial consequences of income inequality, but we argue that interpretation of links between income inequality and health must begin with the structural causes of inequalities, and not just focus on perceptions of that inequality.27,31–35 In this regard, the psychosocial interpretation raises several areas of concern.
Firstly, it conflates the structural sources with the subjective consequences of inequality and reinforces the impression that the impact of psychosocial factors on health can be understood without reference to the material conditions that structure day to day experience.36 The structural, political-economic processes that generate inequality exist before their effects are experienced at the individual level.
Secondly, it underplays the ambiguous health consequences of tightknit social networks and greater social cohesion. Strong social networks can be coercive and can be sources of strain as well as support in relationships. In some contexts, network ties function to enhance health; in others they can be detrimental (S Kunitz, unpublished data).
Thirdly, a shallow definition of social cohesion or capital as informal social relations limits its potential relevance for public health.27 In health research, social cohesion and capital have been discussed as horizontal social relations, ignoring the crucial role that vertical, institutional social relations (political, economic, legal) play in structuring the environments in which informal relations play out.27,37,38
Finally, the psychosocial interpretation encourages understanding of psychosocial health effects in a vacuum. Although clearly not intended by its proponents, a decontextualised psychosocial approach can be appropriated for regressive political agendas, leading to claims that we lack the social cohesion of the past; that problems of poor and minority communities are really a result of deficits of strong social networks; and that local communities must solve their own problems. There has been little discussion of the possibility that focusing on what materially and politically disenfranchised communities can do for themselves may be akin to victim blaming at the community level that reinforces low expectations for structural change.39
The neo-material interpretation
The neo-material interpretation says that health inequalities result from the differential accumulation of exposures and experiences that have their sources in the material world. Under a neo-material interpretation, the effect of income inequality on health reflects a combination of negative exposures and lack of resources held by individuals, along with systematic underinvestment across a wide range of human, physical, health, and social infrastructure.3,5,7,32 An unequal income distribution is one result of historical, cultural, and political-economic processes. These processes influence the private resources available to individuals and shape the nature of public infrastructure—education, health services, transportation, environmental controls, availability of food, quality of housing, occupational health regulations—that form the “neo-material” matrix of contemporary life. In the US, higher income inequality is significantly associated with many aspects of infrastructure—unemployment, health insurance, social welfare, work disability, educational and medical expenditure, and even library books per capita.5
Thus income inequality per se is but one manifestation of a cluster of neo-material conditions that affect population health. This implies that an aggregate relation between income inequality and health is not necessary—associations are contingent on the level and distribution of other aspects of social resources. If income inequality is less linked to investments in health related public infrastructure, the aggregate level association between income inequality and health may break down. In fact, recent evidence from Canada supports this view.40 This is in contrast to the psychosocial hypothesis, which implies a universal association. Perceptions of relative position will always be present, regardless of the actual living conditions for those at the bottom of the social hierarchy. Evidence from animal studies on the role of social hierarchy itself in generating health differences has been used to support this aspect of the psychosocial hypothesis.25 Health effects of social hierarchy in animals are, however, contingent on relations between social position and material living conditions such as availability of food, water, and space.Sapolsky, an eminent primate researcher, has recently proclaimed that “it seems virtually meaningless to think about the physiological correlates of rank outside the context of a number of other modifiers—the sort of society in which the rank occurs.”41
A metaphor
To appreciate how neo-material conditions can influence health, it may be useful to consider the metaphor of airline travel. Differences in neo-material conditions between first and economy class may produce health inequalities after a long flight. First class passengers get, among other advantages such as better food and service, more space and a wider, more comfortable seat that reclines into a bed. First class passengers arrive refreshed and rested, while many in economy arrive feeling a bit rough. Under a psychosocial interpretation, these health inequalities are due to negative emotions engendered by perceptions of relative disadvantage. Under a neo-material interpretation, people in economy have worse health because they sat in a cramped space and an uncomfortable seat, and they were not able to sleep. The fact that they can see the bigger seats as they walk off the plane is not the cause of their poorer health. Under a psychosocial interpretation, these health inequalities would be reduced by abolishing first class, or perhaps by mass psychotherapy to alter perceptions of relative disadvantage. From the neo-material viewpoint, health inequalities can be reduced by upgrading conditions in economy class. Of course, this simplistic metaphor assumes that conditions in first class and economy class are independent—in the real world, improvements in economy are often resisted by those able to travel first class.
Examples from India and Britain
Cross nationally, higher levels of social expenditures—markers of neo-material conditions—are associated with greater life expectancy, lower maternal mortality, and a smaller proportion of low birthweight babies.42 Thus, strategic social investment may be important in determining health differences between countries. Interpretation of health differences between and within countries should be based on a historical view of social conditions and policies. Consider, for example, the widely discussed favourable health situation in Kerala state, India.43 Despite low individual income the infant mortality, maternal mortality, childhood mortality, and overall mortality in Kerala are better than in other Indian states and approach levels in richer, industrialised countries. Greater redistributive actions of the Kerala government over recent decades have been viewed as the phenomenon underlying this. It is also the case, however, that the social and cultural basis for these favourable health outcomes can be traced to over a century of social activities that have promoted greater gender equality, education, and general public investment in human resources.44
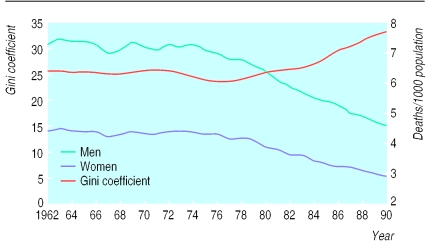
In Britain, income inequality increased greatly from the mid-1970s to the 1990s, but mortality in middle age and at older ages declined dramatically. Correlations between income inequality and mortality range from r=−0.76 for men aged 55-64 to r=−0.86 for women aged 45-54 (fig 3). Understanding the rapid decline in mortality in middle age against a background of escalating income inequality in Britain may require consideration of earlier social investments. Expansion of the welfare state, educational opportunities, and introduction of the NHS had positive influences in early life for those cohorts in which mortality is currently declining, and social circumstances in early life can have important long term effects on later risk of death.45,46 Such findings encourage a view that health in adulthood is the outcome of socially patterned processes acting across the entire life course.47 This perspective would lead to attention being paid to how income inequality—and the broader social processes which income inequality indexes—influences health across the life course of successive cohorts. In several countries, the burden of increased income inequality has fallen disproportionately on poor households containing young children, and this may lead to poor health outcomes in the future.45–48
Figure 3.
Income inequality (Gini coefficient) and mortality in men and women aged 45-54 in Britain, 1962 to 1990
Conclusions
A combination of the individual income and neo-material interpretations is a better fit to the available evidence on income inequality and health, is more comprehensive, and has greater potential to inform interventions that advance public health and reduce inequalities. The psychosocial environment interpretation focuses attention on aspects of personal psychological functioning such as trust, respect, and support. It is hard to understand how this emphasis on psychological functioning and informal interpersonal relations would serve as a basis for a public policy agenda to reduce health inequalities. The neo-material interpretation is an explicit recognition that the political and economic processes that generate income inequality influence individual resources and also have an impact on public resources such as schooling, health care, social welfare, and working conditions. It is strategic investments in neo-material conditions via more equitable distribution of public and private resources that are likely to have the most impact on reducing health inequalities and improving public health in both rich and poor countries in the 21st century.
Acknowledgments
The idea for this paper arose from a meeting of invited participants who discussed the effects of income inequality on health in June 1998 at the University of Michigan School of Public Health. The meeting was sponsored by the University of Michigan Initiative on Inequalities in Health; the Survey Research Center at the University of Michigan; the Health Institute at the New England Medical Center; the Canadian Institute for Advanced Research Population Health Program, and the Population Health Program at the University of Texas at Houston, Health Sciences Center.
Footnotes
Funding: JSH was supported by a health investigator award from the Robert Wood Johnson Foundation. The other authors received no funding for this research.
Competing interests: None declared.
References
- 1.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304:165–168. doi: 10.1136/bmj.304.6820.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Judge K. Income distribution and life expectancy: a critical appraisal. BMJ. 1995;311:1282–1285. doi: 10.1136/bmj.311.7015.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch JW, Kaplan GA. Understanding how inequality in the distribution of income affects health. J Health Psychol. 1997;2:297–314. doi: 10.1177/135910539700200303. [DOI] [PubMed] [Google Scholar]
- 4.Judge K, Mulligan J, Benzeval M. Income inequality and population health. Soc Sci Med. 1998;46:567–579. doi: 10.1016/s0277-9536(97)00204-9. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. doi: 10.1136/bmj.312.7037.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–1007. doi: 10.1136/bmj.312.7037.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch JW, Kaplan GA, Pamuk E, Cohen RD, Heck K, Balfour JL, et al. Income inequality and mortality in metropolitan areas of the United States. Am J Public Health. 1998;88:1074–1080. doi: 10.2105/ajph.88.7.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daly M, Duncan G, Kaplan GA, Lynch JW. Macro-to-micro linkages in the inequality-mortality relationship. Milbank Mem Fund Q. 1998;76:315–339. doi: 10.1111/1468-0009.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waitzman NJ, Smith KR. Separate but lethal: the effects of economic segregation on mortality in metropolitan America. Milbank Mem Fund Q. 1998;76:341–373. doi: 10.1111/1468-0009.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ. 1998;317:917–921. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soobader M-J, LeClere FB. Aggregation and the measurement of income inequality: effects on morbidity. Soc Sci Med. 1999;48:733–744. doi: 10.1016/s0277-9536(98)00401-8. [DOI] [PubMed] [Google Scholar]
- 12.Stainstreet D, Scott-Samuel A, Bellis MA. Income inequality and mortality in England. J Public Health Med. 1999;21:205–207. doi: 10.1093/pubmed/21.2.205. [DOI] [PubMed] [Google Scholar]
- 13.Szwarcwald CL, Bastos FI, Viacava F, de Andrade CL. Income inequality and homicide rates in Rio de Janeiro, Brazil. Am J Public Health. 1999;89:845–880. doi: 10.2105/ajph.89.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Bank Development Indicators CD-ROM. Washington DC: World Bank; 1997. [Google Scholar]
- 15.WHO Statistical Database. www.who.int/whosis/hfa/countries/index.html (accessed June 1999).
- 16.Goodman A, Webb S. For richer, for poorer. The changing distribution of income in the UK. London: Institute for Fiscal Studies; 1994. [Google Scholar]
- 17.Charlton J, Murphy M. The health of adult Britain 1841-1994. London: HMSO; 1994. [Google Scholar]
- 18.Backlund E, Sorlie PD, Johnson NJ. The shape of the relationship between income and mortality in the United States: evidence from the national longitudinal mortality study, Ann Epidemiol 1996;6:1-9. [DOI] [PubMed]
- 19.Ecob R, Davey Smith G. Income and health: what is the nature of the relationship? Soc Sci Med. 1999;48:693–705. doi: 10.1016/s0277-9536(98)00385-2. [DOI] [PubMed] [Google Scholar]
- 20.Gravelle H. How much of the relation between population mortality and unequal distribution of income is a statistical artefact? BMJ. 1998;316:382–385. doi: 10.1136/bmj.316.7128.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koopman JS, Lynch JW. Individual causal models and population systems models in epidemiology. Am J Public Health. 1999;89:1170–1175. doi: 10.2105/ajph.89.8.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88:216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fiscella K, Franks P. Poverty or income inequality as predictor of mortality: longitudinal cohort study. BMJ. 1997;314:1724–1727. doi: 10.1136/bmj.314.7096.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolfson M, Kaplan GA, Lynch JW, Ross N, Backlund E. The relation between income inequality and mortality is not a statistical artefact. BMJ. 1999;319:953–957. doi: 10.1136/bmj.319.7215.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilkinson RG. Unhealthy societies: the afflictions of inequality. London: Routledge; 1996. [Google Scholar]
- 26.Wilkinson RG. Health inequalities: relative or absolute material standards. BMJ. 1997;314:591–595. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynch JW, Due P, Muntaner C, Davey Smith G. Social capital—is it a good investment strategy for public health? J Epidemiol Community Health (in press). [DOI] [PMC free article] [PubMed]
- 28.Diener E, Diener M, Diener C. Factors predicting the subjective well-being of nations. J Pers Soc Psychol. 1995;69:851–864. doi: 10.1037//0022-3514.69.5.851. [DOI] [PubMed] [Google Scholar]
- 29.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87:1491–1499. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith T. Factors relating to misanthropy in contemporary American society. Soc Sci Res. 1997;26:170–196. [Google Scholar]
- 31.Davey Smith G, Egger M. Commentary: understanding it all—health, meta-theories, and mortality trends. BMJ. 1996;313:1584–1585. doi: 10.1136/bmj.313.7072.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davey Smith G. Income inequality and mortality: why are they related? Income inequality goes hand in hand with underinvestment in human resources. BMJ. 1996;312:987–988. doi: 10.1136/bmj.312.7037.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muntaner C, Lynch JW. Income inequality and social cohesion versus class relations: a critique of Wilkinson's neo-Durkheimian research program. Int J Health Serv. 1999;29:59–81. doi: 10.2190/G8QW-TT09-67PL-QTNC. [DOI] [PubMed] [Google Scholar]
- 34.Muntaner C, Lynch JW, Oates G. The social class determinants of income inequality and social cohesion. Int J Health Serv. 1999;29:699–732. doi: 10.2190/HNC9-BEFF-7UWL-92Y2. [DOI] [PubMed] [Google Scholar]
- 35.Newman KS. No shame in my game: the working poor in the inner city. New York: Knopf; 1999. [Google Scholar]
- 36.Lynch JW. Income inequality and health: expanding the debate. Soc Sci Med (in press). [DOI] [PubMed]
- 37.Woolcock M. Social capital and economic development: toward a theoretical synthesis and policy framework. Theory and Society. 1998;27:151–208. [Google Scholar]
- 38.Szreter S. A new political economy for New Labour—the importance of social capital. Renewal. 1999;7:30–44. [Google Scholar]
- 39.Wainwright D. The political transformation of the health inequalities debate. Crit Soc Policy. 1996;49:67–82. [Google Scholar]
- 40.Ross NA, Wolfson MC, Dunn JR, Berthelot J-M, Kaplan GA, Lynch JW. Relation between income inequality and mortality in Canada and in the United States: cross sectional assessment using census data and vital statistics. BMJ. 2000;320:898–902. doi: 10.1136/bmj.320.7239.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sapolsky RM. Hormonal correlates of personality and social contexts: from non-human to human primates. In: Panter-Brick C, Worthman CM, editors. Hormones, health and behavior. New York: Cambridge University Press; 1999. pp. 18–46. [Google Scholar]
- 42.Gough I, Thomas T. Why do levels of human welfare vary among nations? Int J Health Serv. 1994;24:715–748. doi: 10.2190/KHAM-M986-W67T-56B7. [DOI] [PubMed] [Google Scholar]
- 43.World Bank. Improving women's health in India. Washington, DC: World Bank; 1996. [Google Scholar]
- 44.Kabir M, Krishnan TN. Social intermediation and health change: lessons from Kerala. In: Das Gupta M, Chen LC, Krishnan TN, editors. Health, poverty and development in India. Delhi: Oxford University Press; 1996. [Google Scholar]
- 45.Davey Smith G, Hart C, Blane D, Gillis C, Hawthorne V. Lifetime socioeconomic position and mortality: prospective observational study. BMJ. 1997;314:547–552. doi: 10.1136/bmj.314.7080.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davey Smith G, Hart C, Blane D, Hole D. Adverse socioeconomic circumstances in childhood and mortality: prospective observational study. BMJ. 1998;316:1631–1635. doi: 10.1136/bmj.316.7145.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variations in adult health behaviour and psychosocial characteristics, by stage of the socioeconomic lifecourse. Soc Sci Med. 1997;44:809–820. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 48.Lynch JW, Kaplan GA. Socioeconomic position. In: Berkman LF, Kawachi I, eds. Social epidemiology. New York: Oxford University Press (in press).