Most periodontal disease arises from, or is aggravated by, accumulation of plaque, and periodontitis is associated particularly with anaerobes such as Porphyromonas gingivalis, Bacteroides forsythus, and Actinobacillus actinomycetemcomitans. Calculus (tartar) may form from calcification of plaque above or below the gum line, and the plaque that collects on calculus exacerbates the inflammation. The inflammatory reaction is associated with progressive loss of periodontal ligament and alveolar bone and, eventually, with mobility and loss of teeth.
Periodontal diseases are ecogenetic in the sense that, in subjects rendered susceptible by genetic or environmental factors (such as polymorphisms in the gene for interleukin 1, cigarette smoking, immune depression, and diabetes), the infection leads to more rapidly progressive disease. Osteoporosis also seems to have some effect on periodontal bone loss.
The possible effects of periodontal disease on systemic health, via pro-inflammatory cytokines, have been the focus of much attention. Studies to test the strength of associations with atherosclerosis, hypertension, coronary heart disease, cerebrovascular disease, and low birth weight, and any effects on diabetic control, are ongoing.
Gingivitis
Chronic gingivitis to some degree affects over 90% of the population. If treated, the prognosis is good, but otherwise it may progress to periodontitis and tooth mobility and loss. Marginal gingivitis is painless but may manifest with bleeding from the gingival crevice, particularly when brushing the teeth. The gingival margins are slightly red and swollen, eventually with mild gingival hyperplasia.
• Good oral hygiene is essential both in preventing and treating periodontal disease• Antimicrobial drugs have no place in treating chronic gingivitis
Management—Unless plaque is assiduously removed and kept under control by tooth brushing and flossing and, where necessary, by removal of calculus by scaling and polishing by dental staff, the condition will recur. Although gingivitis has a bacterial component, systemic antimicrobials have only transient benefit and therefore no place in treatment. Surgical reduction of hyperplastic tissue by a periodontist (gingivectomy and gingivoplasty) may occasionally be required.
Periodontitis
Chronic periodontitis
Chronic periodontitis (inflammation of the gingiva and periodontal membrane) may be a sequel of chronic gingivitis, usually because of accumulation of plaque and calculus. The gingiva detaches from the tooth, the periodontal membrane and alveolar bone are damaged, and an abnormal gap (pocket) develops between the tooth and gum. The tooth may slowly loosen and eventually be lost.
Diagnosis—Chronic periodontitis (pyorrhoea) is typically seen in adults. It is painless but may be associated with bleeding, halitosis, and a foul taste. Debris and pus may be expressed from the pockets, and there may be increasing tooth mobility. Periodontitis cannot be diagnosed by inspection alone, however, and requires specific diagnostic tests (periodontal probing and, sometimes, radiographs).
Management—Improvement in oral hygiene is necessary, but tooth brushing and mouthwashes have effect only above and slightly below the gum level. They are therefore ineffective in treating periodontitis, as plaque continues to accumulate below the gum line within periodontal pockets. Scaling and polishing and sometimes curettage are also required. Surgical removal of the pocket wall and diseased tissue may be needed to facilitate future cleansing, or attempts to regenerate lost periodontal tissue (such as guided tissue regeneration) may be indicated. Professional attention is therefore required. Although periodontal disease has a bacterial component, systemic antimicrobial drugs have no place in routine treatment, but topical treatment with antimicrobials within the periodontal pockets may be useful.
• Good oral hygiene is essential in treating periodonitis• Peridonitis requires professional care, usually scaling and polishing and possibly periodontal surgery• Periodontitis that is unresponsive to such care, advances rapidly, or appears at an early age may have a systemic background
Causes of gingival bleeding
| Local | Systemic |
| • Gingivitis | • Thrombocytopenia |
| Chronic | Leukaemia |
| Acute necrotising | HIV infection |
| • Periodontitis | • Clotting defects |
| • Rarely, telangiectasia or angioma | Drugs such as anticoagulants |
Periodontitis in young patients or which is rapidly advancing
If periodontitis is seen in children or young adults or is rapidly advancing, systemic factors should be excluded.
Gingival bleeding
Bleeding from the gingival margins is common and usually a consequence of gingivitis. It may be more obvious in women taking oral contraceptives and during the second and third trimesters of pregnancy. However, it may be a sign of platelet or vascular disorders and is common in leukaemia and HIV infection.
Gingival ulcers
Gingival ulcers are often of infectious aetiology.
Herpes simplex virus stomatitis is common in childhood but is increasingly seen in adults. There is a diffuse, purple, “boggy” gingivitis, especially anteriorly, with multiple vesicles scattered across the oral mucosa and gingiva. This is followed by ulcers. Diagnosis is usually clinical. The infection resolves spontaneously in 7-14 days, during which antipyretic analgesics such as paracetamol and adequate hydration are helpful. Antiviral drugs should be used in severe stomatitis and with immunocompromised patients, who may otherwise suffer severe infection. For those who can safely use it, an aqueous chlorhexidine mouthwash helps to maintain oral hygiene.
Acute necrotising ulcerative gingivitis—Also known as Vincent's disease and trenchmouth, this affects mainly adults and causes painful ulceration of the gums between the teeth (interdental papillae), a pronounced tendency to gingival bleeding, and halitosis. Anaerobic fusiform bacteria and spirochaetes are implicated, and predisposing factors include poor oral hygiene, smoking, malnutrition, and immune defects including HIV and other viral infections and leukaemias. Management includes oral debridement and instruction on oral hygiene, peroxide or perborate mouthwashes, and metronidazole 200 mg three times daily for three days.
• Gingival ulceration in herpetic stomatitis is common and is associated with mouth ulcers elsewhere and fever• Gingival ulcers with bleeding and halitosis suggest a diagnosis of necrotising gingivitis
Other causes—Gingival ulcers may also be due to aphthae, self injury in psychologically disturbed or mentally challenged patients, malignant neoplasms, drugs, dermatoses, or systemic disease (haematological, mucocutaneous, gastrointestinal, or chronic infections such as tuberculosis, syphilis, mycoses, herpesviruses, and HIV).
Gingival swelling
Widespread gingival swelling can be a feature of chronic gingivitis and may be caused by drugs, pregnancy, and systemic diseases.
Causes of gingival swelling
| Local causes | Systemic causes |
| • Chronic gingivitis causing | • Hereditary gingival fibromatosis and related disorders |
| Gingival abscesses | • Drugs (phenytoin, cyclosporin, calcium channel blockers) |
| Fibrous epulis | • Pregnancy |
| • Hyperplastic gingivitis due to mouth breathing causing | • Sarcoidosis |
| Exostoses | • Crohn's disease |
| Cysts | • Leukaemia |
| Pyogenic granuloma | • Wegener's granulomatosis |
| Neoplasms | • Rarely, amyloidosis, scurvy, midline lethal granuloma, mucopolysaccharidoses, mucolipidoses |
Drug induced gingival swelling—Drugs implicated include phenytoin, cyclosporin, and calcium channel blockers. Gingival swelling is usually worse if there is accumulation of plaque and calculus and the patient is receiving high drug doses. Improved oral hygiene and excision of enlarged tissue may be indicated.
Pregnancy gingivitis—This usually develops around the second month and reaches a peak in the eighth month. An exaggerated inflammatory reaction to plaque in pregnancy predisposes to gingivitis. Oral hygiene should be improved, particularly in view of the current concern that gingivitis may affect fetal birth weight. Pregnancy gingivitis tends to resolve on parturition.
Hereditary gingival fibromatosis—This rare autosomal dominant condition may be associated with hirsutism, but most patients are otherwise perfectly healthy, although there are rare associations with systemic syndromes. Surgical reduction of the gingiva may be indicated.
• Gingival swelling may occur in pregnancy and typically resolves at parturition• Gingival swelling may be drug induced—by phenytoin, cyclosporin, or calcium channel blockers
Gingival lumps
Erupting teeth, particularly mandibular third molars, may be associated with swelling and tenderness of the overlying soft tissue flap (operculum), especially if this is traumatised by a tooth in the opposing dental arch. This condition, termed pericoronitis, is best treated by cleaning the area and having a dentist grind or remove the opposing tooth if it is causing trauma. If the patient is in severe pain or is feverish antimicrobials such as metronidazole 200 mg thrice daily for up to five days may be indicated.
Pregnancy epulis—Pregnancy may cause a localised swelling (epulis) of the gingival papillae, which may bleed or ulcerate. Occasionally, a large epulis requires surgical removal.
Fibroepithelial polyp—Also called a fibrous lump and fibrous epulis, this is benign in nature. It may need to be removed.
Malignant causes of gingival lumps include carcinoma, Kaposi's sarcoma, and lymphoma.
Red gingival lesions
The most common cause of redness is gingivitis, in which the erythema is usually restricted to the gingival margins and interdental papillae (see above). Red lesions may also be due to desquamative gingivitis, erythroplasia, haemangiomas, orofacial granulomatosis, Crohn's disease, sarcoidosis, Wegener's granulomatosis, and neoplasms such as carcinoma and Kaposi's sarcoma.
Desquamative gingivitis
Widespread erythema, particularly if associated with soreness, is usually caused by desquamative gingivitis. This is fairly common, is seen almost exclusively in women over middle age, and is usually a manifestation of lichen planus or mucous membrane pemphigoid. Its main features include persistent gingival soreness that is worse on eating and red gingivae. Diagnosis is usually obvious from the history and clinical features, but biopsy and immunostaining may be needed to establish the precise cause.
• Desquamative gingivitis is not uncommon in women over middle age• Most desquamative gingivitis is caused by lichen planus or pemphigoid
Management is based on treating the underlying condition and, if there are extraoral lesions, systemic treatment, usually with corticosteroids. Desquamative gingivitis can also often be improved with better oral hygiene and topical corticosteroids such as fluocinonide cream used by a dentist in a plastic splint over the teeth and gums.
Gingival pigmentation
This is usually a normal condition mainly seen in certain races (such as black people). Other causes include particles of dental amalgam embedded in the soft tissues, Addison's disease, Kaposi's sarcoma, drugs such as minocycline, melanotic macules and naevi, and melanoma.
Halitosis
Oral malodour (foetor oris) predominantly originates from the tongue coating, gingival crevice, and periodontal pockets. Plaque organisms—especially Porphyromonas gingivalis, fusobacteria, and other anaerobes—cause putrefaction, resulting in release of volatile chemicals, particularly sulphide compounds (including hydrogen sulphide, methylmercaptan, dimethyl sulphide, and dimethyl disulphide).
Mouthwashes with antimicrobial activity
Chlorhexidine gluconate
0.1-0.2% aqueous mouthwash, rinse for 1 minute twice daily
Has measurable antiplaque activity
May stain teeth superficially if patient drinks tea, coffee, or red wine
Povidone iodide
1% mouthwash used 2-4 times daily for up to 14 days
Contraindicated in iodine sensitivity, pregnancy, thyroid disorders, or those taking lithium
Cetypyridinium chloride
0.05% mouthwash used twice daily
Hexetidine
0.1% mouthwash used twice daily
Some oral malodour is common in healthy individuals, particularly after sleep (morning breath). People who refrain from oral hygiene soon develop malodour, but this is worse with any form of sepsis of the aerodigestive tract such as gingivitis, periodontitis, dental abscess, dry socket, sinusitis, tonsillitis, nasal foreign bodies, and tumours.
Many foods and drinks can cause malodour, especially garlic, onions, curries, the fruit durian, etc. Smoking and drugs— including alcohol, isosorbide dinitrate, and disulphiram—may also be implicated. Rare causes include diabetic ketoacidosis, renal or hepatic dysfunction, and psychiatric disease, as in delusional halitosis or as a feature in schizophrenia.
Management
Management requires establishing the presence of true halitosis and assessing its severity with a portable sulphide monitor (halitometer). Dietary, infective, and systemic causes must be excluded. A full assessment of oral health is always indicated.
Further reading
Beck JD, Pankow J, Tyroler HA, Offenbacher S. Dental infections and atherosclerosis. Am Heart J 1999;138:528-33
Birkenfeld L, Yemini M, Kase NG, Birkenfeld A. Menopause-related oral alveolar bone resorption: a review of relatively unexplored consequences of estrogen deficiency. Menopause 1999;6:129-33
Moore PA, Weyant RJ, Mongelluzzo MB, Myers DE, Rossie K, Guggenheimer J, et al. Type 1 diabetes mellitus and oral health: assessment of periodontal disease. J Periodontol 1999;70:409-17
Morrison HI, Ellison LF, Taylor GW. Periodontal disease and risk of fatal coronary heart and cerebrovascular diseases. J Cardiovasc Risk 1999;6:7-11
Offenbacher S, Beck JD, Lieff S, Slade G. Role of periodontitis in systemic health: spontaneous preterm birth. J Dent Educ 1998;62:852-8
Schenkein H, Committee on Research, Science and Therapy of the American Academy of Periodontology. The pathogenesis of periodontal diseases. J Periodontol 1999;70:457-70
Scully C, Flint S, Porter SR. Oral diseases. London: Martin Dunitz, 1996
Scully C. Oral medicine and periodontology. Periodontol 2000 1998;18:7-110
The most reliably effective management is
• Improving oral hygiene
• Eating regularly
• Avoiding odiferous foods, drugs, and other substances
• Chewing sugar-free gum regularly
• Using one of the many oral deodorants available over the counter
• Using an antibacterial mouthwash or one such as Retardex or Dentyl
• In severe or recalcitrant cases, using metronidazole 200 mg thrice daily for seven days.
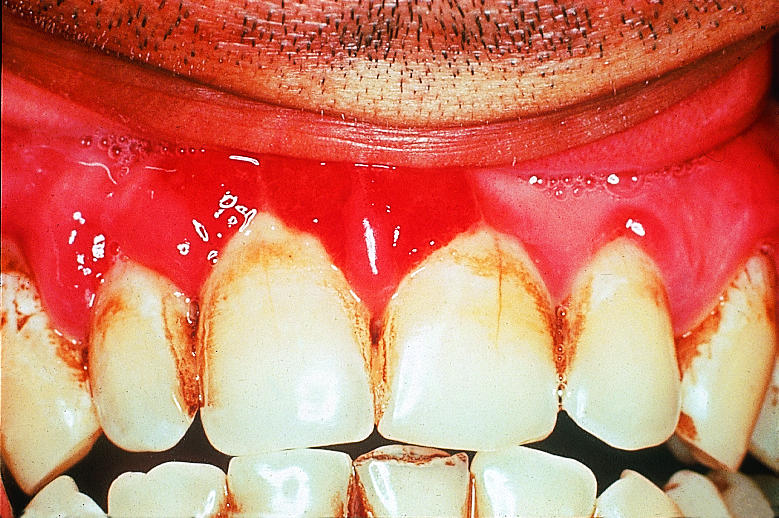
Figure.
Chronic marginal gingivitis showing erythematous oedematous appearance
Figure.
Gingivitis with hyperplasia
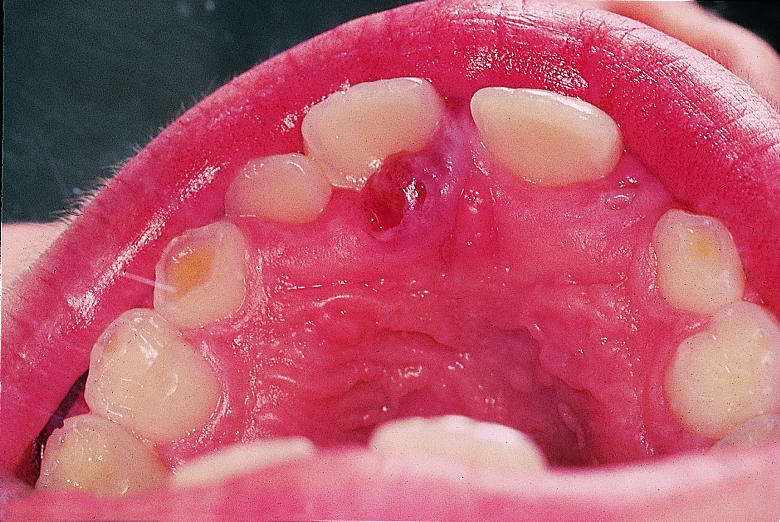
Figure.

Periodonitis with damage to supporting tissues including bone
Figure.
Herpetic stomatitis, with ulcerations on gingivae (top) and elsewhere in the mouth (bottom)
Figure.

Necrotising (ulcerative) gingivitis
Figure.
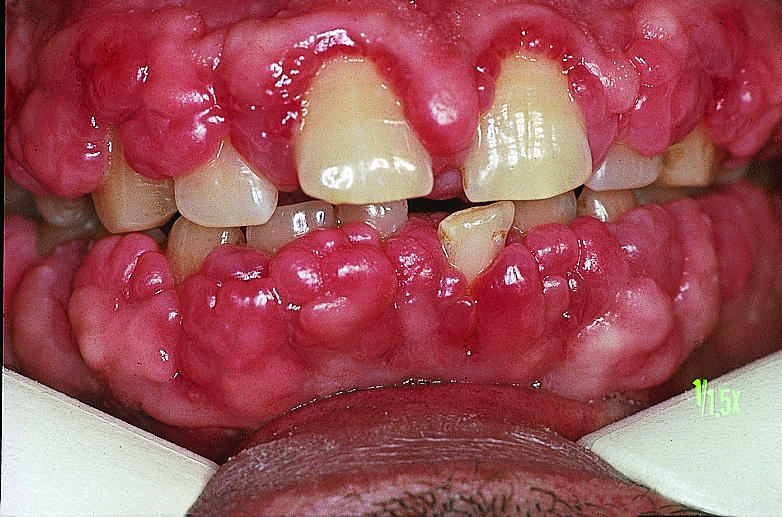
Cyclosporin induced gingival swelling
Figure.

Pregnancy gingivitis
Figure.
Pregnancy epulis (pyogenic granuloma)
Figure.

Desquamative gingivitis; usually a sign of pemphigoid (as here) or lichen planus
Figure.

Gingival pigmentation is common in black people
Acknowledgments
Crispian Scully is grateful for the advice of Rosemary Toy, general practitioner, Rickmansworth, Hertfordshire.
Footnotes
John Coventry is senior lecturer in periodontology, Gareth Griffiths is senior lecturer in periodontology, Crispian Scully is dean, and Maurizio Tonetti is professor of periodontology at the Eastman Dental Institute for Oral Health Care Sciences, University College London, University of London (www.eastman.ucl.ac.uk).
The ABC of Oral Health is edited by Crispian Scully and will be published as a book in autumn 2000.





