Abstract
Molecular determinants of neuropathogenesis have been shown to be present in the hemagglutinin (H) protein of measles virus (MV). An H gene insertion vector has been generated from the Edmonston B vaccine full-length infectious clone of MV. Using this vector, it is possible to insert complete H open reading frames into the parental (Edtag) background. The H gene from a rodent brain-adapted MV strain (CAM/RB) was inserted into this vector, and a recombinant virus (EdtagCAMH) was rescued by using a modified vaccinia virus which expresses T7 RNA polymerase (MVA-T7). The recombinant virus grew at an equivalent rate and to similar titers as the CAM/RB and Edtag parental viruses. Neurovirulence was assayed in a mouse model for MV encephalitis. Viruses were injected intracerebrally into the right cortex of C57/BL/6 suckling mice. After infection mice inoculated with the CAM/RB strain developed hind limb paralysis and ataxia. Clinical symptoms were never observed with an equivalent dose of Edtag virus or in sham infections. Immunohistochemistry (IHC) was used to detect viral antigen in formalin-fixed brain sections. Measles antigen was observed in neurons and neuronal processes of the hippocampus, frontal, temporal, and olfactory cortices and neostriatum on both sides of symmetrical structures. Viral antigen was not detected in mice infected with Edtag virus. Mice infected with the recombinant virus, EdtagCAMH, became clinically ill, and virus was detected by IHC in regions of the brain similar to those in which it was detected in animals infected with CAM/RB. The EdtagCAMH infection had, however, progressed much less than the CAM/RB virus at 4 days postinfection. It therefore appears that additional determinants are encoded in other regions of the MV genome which are required for full neurovirulence equivalent to CAM/RB. Nevertheless, replacement of the H gene alone is sufficient to cause neuropathology.
Measles virus (MV) is a negative-stranded RNA paramyxovirus which causes an acute human infection leading to the death of over 1 million people in developing countries per annum. As a member of the Mononegavirales, MV has a nonsegmented genome which encodes six structural proteins, nucleocapsid (N), phosphoprotein (P), matrix (M), fusion (F), hemagglutinin (H), and polymerase (L); at least two nonstructural proteins, C and V, are produced in infected cells. The F0 protein arises as an inactive precursor. Two disulfide-linked subunits, F1 and F2, are generated by proteolysis, and these associate with the H protein (50). Binding of the F1 cytoplasmic tail to the M protein, which in turn associates with the NC proteins encapsidating the genome, completes the interactions necessary for the assembly of an infectious virus particle (28).
Entry of tissue culture adapted strains of MV is mediated by binding of the H glycoprotein, which is tightly associated with the F glycoprotein, to a cellular receptor, CD46 (9, 24). Cell-to-cell fusion is also mediated by these two glycoproteins (6, 50). As CD46 is not present on all cells which can be infected by MV, it is assumed the virus can utilize other receptors (47).
Two severe infections of the central nervous system (CNS) may follow MV exposure: subacute sclerosing panencephalitis (41) and measles inclusion body encephalitis (1). In the former, a persistent virus infection ensues in the presence of high titers of antiviral antibodies; mutations accumulate in the virus genome, especially in the F and M genes, and transcription of envelope genes is reduced by an altered transcription gradient (2, 36, 40, 41). In attempts to generate a small animal model for CNS infection neurovirulent, rodent-adapted strains of MV have been generated by repeated passage in the brain (4, 7, 15, 19, 21, 26, 47). Sequencing studies have shown that the majority of alterations, in such rodent brain-adapted strains, reside in the H gene, and it is possible that these changes allow MV to infect rodent neural cells by using a different receptor. Escape mutants, isolated in vitro from a neuroadapted CAM/RB strain by using anti-H neutralizing monoclonal antibodies, have altered neurotropism. The mutations are located in what is described as a major antigenic determinant (residues 368 to 396) of the H gene, and it is assumed that residues in this region may be functionally important for neurovirulence (20).
The availability of the MV rescue system (29) allows more defined investigations into virulence determinants in MV strains. A number of recombinant MVs have been generated by using this system and used to elucidate mechanisms of cell-to-cell spread (5) and virulence (42, 50). To determine whether the CAM/RB H gene in isolation is sufficient to confer neurovirulence to the non-brain-adapted Edmonston B, we have inserted this gene into the Edtag background and rescued a recombinant MV. The transfer of neurovirulence determinants was successful. The ability to examine the effects of the CAM H gene in isolation in a constant genetic background will be of value in elucidating the molecular basis of MV neurotropism in this model.
MATERIALS AND METHODS
Viruses and cells.
Edtag virus was rescued from the full-length infectious antigenomic clone p(+)MV (29) as described by Schneider et al. (35). Vero cells (American Type Culture Collection) were grown in Dulbecco’s modified Eagle’s medium supplemented with 8% newborn calf serum and used for the production and titration of measles virus stocks. HeLa cells, grown in RPMI medium (Gibco) supplemented with 5% fetal calf serum, were used for the rescue of recombinant viruses. The rodent brain-adapted measles virus CAM/RB was obtained from U. G. Liebert, Würzburg, Germany. The virus was passaged on Vero cells, and retention of the neurovirulent phenotype was verified routinely by inoculation of 200 50% tissue culture infective doses (TCID50) into the brains of suckling C57/BL/6 mice. Modified vaccinia virus Ankara expressing T7 RNA polymerase (MVA-T7) was obtained from Gerd Sutter, GSF-Forschungszentrum, Neuherberg, Germany. This host-range-adapted virus was passaged and titered in primary chicken embryo fibroblast cells supplied by Mildred Wylie, Veterinary Sciences Division, Belfast, Northern Ireland, as previously described (39).
Single-step growth analysis.
Vero cells were cultured, to 80% confluency, in 35-mm-diameter petri dishes. Cells were infected at a multiplicity of infection (MOI) of 5 with the parental and recombinant viruses for 1 h at 37°C, after which time the inoculum was removed. Infected cells were incubated for 86 h. Every 4 or 5 h, monolayers were scraped from the petri dishes. Cell-associated virus was recovered by freeze-thawing the cell samples twice, and aliquots were stored at −70°C. Titers were obtained by the 50% endpoint dilution assay (30) and are expressed in TCID50.
Construction of H insertion vector.
A ClaI subclone was generated from plasmid p(+)MV, which encodes the complete antigenome of the Edmonston strain of MV (29). The 10,624-bp ClaI fragment was subcloned into pGEM7ZF(+) (Promega). The resulting subclone pscMV(ClaI) was digested with PacI and SpeI to remove the majority of the H gene. Two complementary oligonucleotides, containing the restriction site AatII (underlined), were synthesized. These were designated priHins+ (5′-TAATACAATAGACGTCAGGCATACCCA) and priHins− (5′-CTAGTGGGTATGCCTGACGTCTATTGTATTAAT). Oligonucleotides priHins+ and priHins− were diluted to 10 ng/μl and mixed in an equimolar ratio in annealing buffer (20 mM Tris, 10 mM MgCl2, 50 mM NaCl [pH 7.5]). They were heated to 100°C for 3 min and cooled to 40°C over a period of 30 min. After annealing, the double-stranded product contained ends which were compatible with the PacI/AatII-cut vector pscMV(ClaI). Ligation of the vector and annealed oligonucleotides resulted in the production of the vector pscMVins-H2(ClaI). Excision and reintroduction of this mutagenized ClaI fragment into pscMV(ClaI) resulted in the generation of the insertion vector pMVins-H2. The plasmid was sequenced by dideoxynucleotide chain termination (ABI Prism) using an MV-specific primer (MF3) which binds in the 3′ untranslated region of F (5′-GGTTTATCGAGCACTAGCAT) to verify that the oligonucleotide had been inserted and replaced the H gene as expected.
RNA preparation and RT-PCR.
Total RNA was prepared by a guanidinium isothiocyanate method (34, 46). Briefly, RNA was prepared either from infected monolayers or from frozen brain tissue. Monolayers were solubilized in guanidinium isothiocyanate solution, and brain tissue was homogenized in the same solution. Total RNA was prepared by cesium chloride gradient centrifugation. RNA was precipitated with ethanol, and salts were removed by using cold 70% ethanol. The Superscript one-step reverse transcription (RT)-PCR system (Gibco) was used to produce DNA fragments which were used for cloning strategies, restriction analysis, and DNA sequencing. One microgram of total RNA was used as the template for one-step RT-PCR. Reverse transcriptase was omitted to control for plasmid DNA contamination, and β-actin primers (5′-TCATGAAGTGTGACGTTGACATCCGTAAAG and 5′-CCTAGAAGCATTTGCGGTGCACGATGGAGG) were used as positive controls. PCR products were analyzed on 1.5% DNA agarose gels containing ethidium bromide, and PstI-digested λ DNA was used as size markers. Digitized bitmap images were collected with an Imagestore 5000 analysis system (UVP).
Construction of p(+)MVCAMH.
Vero cells were infected, at an MOI of 1, with the MV CAM/RB strain for 36 h, and total RNA was prepared. Oligonucleotides uniH+ (5′-CGGTAGTTAATTAAAACTTAGGGTGCAAGATCATCCAC) and uniH2− (5′-(ATGCCTGACGTCTGGGTGACATCATG), specific for MV H genes and compatible with the H insertion vector, were designed to include the restriction sites PacI and AatII (underlined). The H gene of the CAM/RB strain was amplified by one-step RT-PCR using these primers. The PCR product was digested with PacI and AatII and ligated into similarly treated pMVins-H2. The resultant construct, designated p(+)MVCAMH, was completely sequenced by using MV H-specific oligonucleotides to verify that the PCR had not introduced nonspecific mutations into the gene upon amplification.
Rescue of infectious viruses, Edtag, and EdtagCAMH.
HeLa cells, grown to 50% confluency in 35-mm-diameter wells, were infected with MVA-T7 at an MOI of 1. Transfections were carried out essentially as outlined by Schneider et al. (35). Plasmids pEMC-Na (1.5 μg), pEMC-Pa (1.5 μg), and pEMC-La (0.5 μg) and the plasmids containing copies of the full-length antigenomes (5 μg) were transfected into the cells over 18 h. After this time, the medium was replaced and transfections were further incubated for 5 days at 37°C. If syncytia were not visible by this time, the cells were scraped from the wells. After two rounds of freeze-thawing, the precleared supernatants were seeded onto HeLa or Vero cell monolayers. Recovery of virus was verified by the appearance of syncytia 10 days posttransfection, and the recombinant viruses were plaque purified twice on Vero cells. Vero cells were infected with the recombinant viruses, and total RNA was prepared as described above.
Neurovirulence in mice.
Four-day-old suckling C57/BL/6 mice were obtained from in-house breeding colonies in the Laboratory Service Unit, The Queen’s University of Belfast. Animals were kept in a barrier system with light negative pressure and a 12-h day (artificial light). Mice were infected into the right cerebral hemisphere, under mild halothane anaesthesia, with 200 TCID50 of the recombinant viruses (20 μl). At least three animals were inoculated for each virus pool. Negative control mice were injected with an equivalent volume of tissue culture medium. Mice were checked for clinical symptoms daily. At 4 days postinfection, mice were sacrificed under ether narcosis. The whole brain was removed immediately and immersed in 10% buffered formalin for 24 h. Brains were blocked into right and left hemispheres, routinely processed, and embedded in paraffin wax. Two EdtagCAMH-infected brains were frozen at −70°C and used for RNA isolation.
Immunopathology.
A monoclonal antibody that recognizes the N protein of MV (Harlan Seralabs) was used for immunohistochemistry at a dilution of 1:1,000. Sections (8 μm) were cut from three levels of the paraffin-embedded brain tissue, using a microtome. The levels were cut to an approximate depth of 100 μm and were separated by 50 μm. Sections were dewaxed, and MV N protein was detected as described previously (22). A semiquantitative scoring system was used to determine the extent of viral infection in both the right and left hemispheres of each animal; when possible, overall number of foci were counted.
RESULTS
Generation of MV H insertion vector.
The ability to modify full-length genomic DNA constructs of MV in a single step is of great benefit. This is not often possible in large cDNA clones due to the paucity of unique restriction sites. To this end, we have generated an insertion vector which enables the rapid exchange of MV H genes in a full-length infectious clone (Fig. 1). The preferred approach aimed to minimize both the number of additional nucleotides, which due to the rule of six (14) must be added in hexamers, and specific sequence alterations, within the genome of the virus. In the production of pMVins-H2, only one nucleotide exchange has been incorporated into the 3′ untranslated region (UTR) of the H gene at position 9162 (A→G). The two unique restriction sites PacI, already present in the 3′ UTR of the F gene, and AatII, introduced using synthetic oligonucleotides, permit the insertion of H genes from other MV strains. Almost the entire H gene (97.4%) was deleted, leaving only 50 nucleotides from the 3′ UTR in the insertion vector backbone. Additionally, the presence of the AatII restriction site within this construct acts as a genetic tag for all recombinant viruses produced via this cloning strategy.
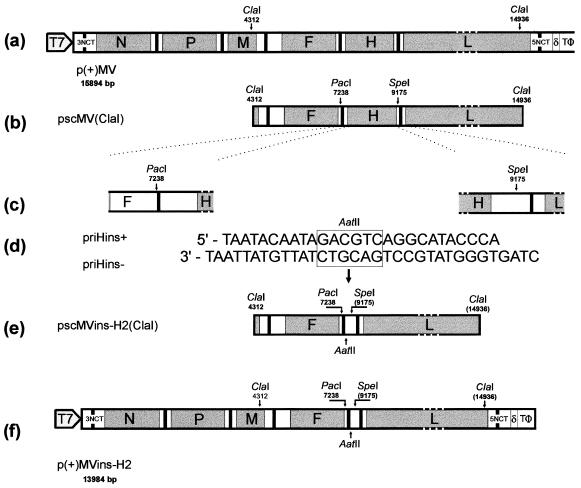
FIG. 1.
Construction of the MV insertion vector p(+)MVins-H2. The full-length infectious clone of MV, p(+)MV (a), was used to generate a ClaI subclone in pGEM7Zf(+) (b). The subclone was restricted with PacI and SpeI to remove the H gene (c). Complementary oligonucleotides were annealed (d) to generate compatible ends with the pscMV(ClaI) cut vector and inserted (e) to introduce a unique AatII restriction site. The ClaI fragment was religated into p(+)MV to generate the insertion vector (f). Nucleotide sequence numbers are given as in EMBL accession no. Z66517; numbers below the plasmid names indicate MV genome lengths before and after modification.
Production and rescue of recombinant MV.
With reference to MV sequence alignments (32), universal H primers were designed to facilitate the amplification of H genes from any strain of the virus. The 5′ primer, uniH+ (nucleotides 7238 to 7272) as numbered in the complete antigenome sequence, includes a PacI restriction site located in the polyadenylation site of the F gene along with the intragenic spacer (CTT) found between the F and H genes. The 3′ primer, uniH2− (9164 to 9145), includes the novel AatII restriction site and thereby generates the single nucleotide exchange at antigenome position 9162 (A→G). Six random nucleotides precede or follow the unique restriction sites in these primers to prevent partial cleavage by the restriction enzyme due to the proximity of the recognition site to the end of the primer. These primers were used to amplify the H gene from the rat brain-adapted CAM/RB strain of MV which, following PacI and AatII restriction, was ligated into similarly treated p(+)MVins-H2.
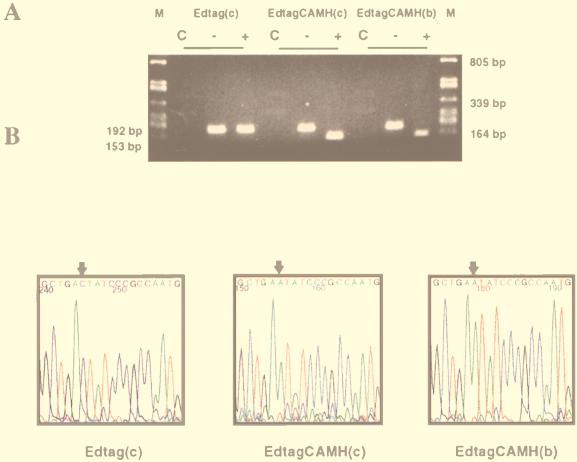
Recombinant virus was rescued in HeLa cells by using the host-range-adapted helper virus MVA-T7 to provide T7 RNA polymerase in the cytoplasm of infected cells. Plasmids expressing the MV proteins N, P, and L were transfected along with the recombinant full-length construct. Virus was rescued 6 to 10 days posttransfection and was plaque purified on Vero cells. The parental virus (Edtag) was rescued as a positive control. This virus contains three nucleotide alterations in the noncoding region between the N and P genes to allow it to be discriminated from the standard vaccine strain of MV (29). Due to the increase in recombination frequency associated with the introduction of MVA-T7, rescued viruses were extensively characterized. Total RNA was prepared from both Edtag- and EdtagCAMH-infected cell monolayers. For molecular characterization, two sections of the virus genome were amplified by RT-PCR using MV-specific primers: (i) nucleotides 9010 to 9202, which contain the AatII genetic tag at position 9163, and (ii) nucleotides 8420 to 8752, which include two CAM/RB-specific mutations at positions 8634 and 8707. Figure 2 shows the restriction digestion and electrochromatograms from this analysis, which confirms the presence of the AatII restriction site and the C→A exchange at position 8634. This indicated that the engineered mutations were stably retained during cell passage. Additionally, the complete H gene from the rescued virus was sequenced to confirm that all CAM/RB mutations were present.
FIG. 2.
Molecular characterization of rescued viruses after passage in Vero cells [Edtag(c) and EdtagCAMH(c)] or intracerebral injection into in C57/BL/6 mouse brain [EdtagCAMH(b)]. (A) Total RNA was prepared from either infected cell sheets or infected brain tissue, and viral RNA was amplified by RT-PCR. Reverse transcriptase was omitted as a negative control (C). Products were restricted with AatII (+), which as a genetic tag for recombinant virus produced by using insertion vector p(+)MVins-H2; undigested samples (−) were included for comparison. Samples were analyzed on 1.5% DNA agarose gels. (B) PR-PCR products from cells infected with Edtag(c) and EdtagCAMH(c) and brain tissue from mice infected with EdtagCAMH(b) were sequenced to verify that CAM/RB sequences were retained upon replication. Sequences which represent nucleotides 8629 to 8647 of the viral genome are shown in the three panels. The C-to-A mutation at nucleotide 8634, which is CAM/RB specific, is indicated by an arrow.
Characterization of recombinant virus.
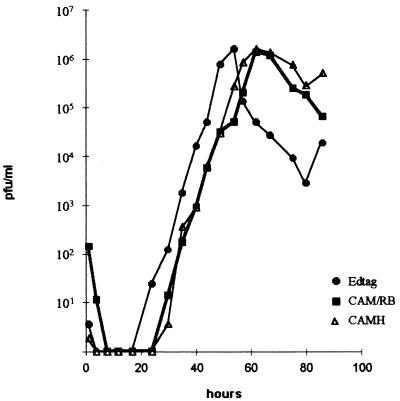
The H gene of measles virus CAM/RB differs from that of Edmonston B strain by 12 nucleotides (20). To gain an understanding of the growth characteristics of the recombinant virus, we carried out a single-step growth analysis. Virus was harvested at four or five hourly time points over 86 h. Titers of cell-associated virus, parental (Edtag and CAM/RB) and recombinant (EdtagCAMH), were obtained in triplicate by determining TCID50. Figure 3 shows the growth curves for the three viruses. Similar titers, approximately 2 × 106, were attained with all three viruses by 60 h postinfection. By this stage, many areas of the cell sheet had detached from the flask. Edtag virus titers were higher than either the CAM/RB or the EdtagCAMH virus at equivalent time points up to 60 h postinfection, indicating that this virus grows slightly faster. Replacement of the Edtag H gene with that of the CAM/RB strain seems to result in a virus which exhibits a growth rate more akin to that of the CAM/RB virus. After this time, the cell-associated titers of all the viruses began to decrease as virus was released from the cells into the supernatant and cells detached from the flask. It appears, therefore, that replacement of the H glycoprotein between the brain-adapted and Edmonston vaccine strains had no apparent effect on the growth of the virus in tissue-cultured Vero cells.
FIG. 3.
Growth curves of cell-associated virus in Vero cells. Monolayers were infected at an MOI of 5 with the three viruses. Lines join an average titer which was obtained from three separate tissue culture infectious dose experiments.
Assessment of neurovirulence and immunopathology.
We wished to determine if the neurovirulent phenotype was transferred to the Edtag virus following replacement of the H glycoprotein with its CAM/RB analogue. A single litter of six to seven C57/BL/6 suckling mice was infected intracerebrally with each virus (200 TCID50) into the right cortex. The infection was allowed to proceed for 4 days, during which time the mice were monitored daily for clinical symptoms of infection. Three days postinfection, mice infected with the CAM/RB strain were showing an awkward gait and ataxia. Mice infected with the EdtagCAMH virus showed similar clinical symptoms. Clinical signs of infection were not observed in either the sham- or Edtag-infected animals. Brains were dissected out from the infected mice and either frozen directly or fixed in formalin. Total RNA was isolated from the frozen brains. RT-PCR followed by restriction digestion was used to confirm that the recombinant virus retained the AatII tag sequence in the untranslated region of the H gene (Fig. 2A). DNA sequencing confirmed that the CAM/RB-specific mutations were retained in the H open reading frame following replication in the mouse brain (Fig. 2B).
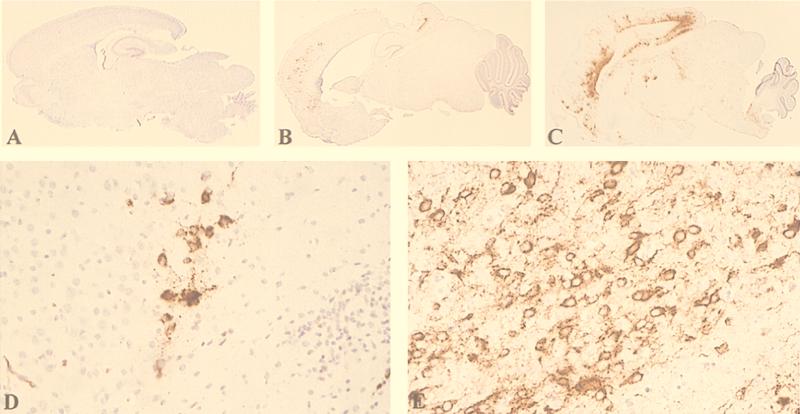
Brain sections were examined for the presence or absence of virus antigen by immunohistochemistry. Representative sections from each virus infection are shown in Fig. 4. Sham-infected mice, inoculated with tissue culture medium, showed no positive staining for MV antigen, as was expected. A pronounced infection can be seen in the CAM/RB-infected C57/BL/6 suckling animals (Fig. 4C and E). Virus was observed in cells with the morphological characteristics of neurons. Anatomically such cells were found in the hippocampus, frontal, temporal, and olfactory cortices and neostriatum on both sides of symmetrical structures. Viral antigen was not found in the ependymal cells of the ventricular layer, the cerebellum, meninges, or choroid plexus. Antigen was detected in the neuronal cytoplasm and along the entire length of processes up to the synaptic terminals. Astrocytes, oligodendrocytes, and microglial cells were all consistently negative for viral antigen. The recombinant EdtagCAMH virus gives rise to a less pronounced but clearly positive infection in the mouse brain (Fig. 4B and D). The same cell type is infected as with the CAM/RB virus, and the MV-infected cells are located in the same anatomical areas of the brain. However, the foci are smaller at the same time point (4 days postinfection), as is obvious in the higher magnification.
FIG. 4.
Immunohistochemistry of brain sections 4 days after infection with rodent brain-adapted CAM/RB, rescued parental Edtag, and recombinant EdtagCAMH (200 TCID50). Sections were formalin fixed, and MV antigen was detected with an anti-(N) monoclonal antibody; positive viral staining appears brown. (A) Edtag; (B) EdtagCAMH; (C) CAM/RB (magnification, ×5.) Sections were digitized with a Kodak RFS 2035 Plus Film scanner directly from the slide. (D) EdtagCAMH; (E) CAM/RB (magnification, ×80.) Sections were photographed on slide film and digitized with a Kodak RFS 2035 Plus Film scanner. The final resolution of all scanned images was 300 dots per in.
To further characterize the virus infections, we used a semiquantitative scoring system that reflects both the degree to which each infection had progressed and the number of MV-positive foci in the three levels of brain tissue (Table 1). Due to the progression of the CAM/RB infection (Fig. 4C), it was impossible to accurately count the foci in the brain sections because they were merged to a large degree. Generally, viral antigen was more abundant in the right cortex, which was the side of infection. Variation was observed between the three animals examined, and this is reflected in the scoring system. It was possible to determine accurate foci numbers in the EdtagCAMH-infected brain sections due to the lower level of infection. Once again, we observed variation between animals and greater abundance of viral antigen in sections from the right cortex. Infected cells were not observed in sections from animals infected with the Edtag virus. Clearly, at the time point observed, the recombinant virus EdtagCAMH replicates in the brains of the C57/BL/6 animals, though to a lesser extent than the CAM/RB virus.
TABLE 1.
Detection of MV N protein by immunohistochemistry in right and left cortices of C57/BL16 mice 4 days after intracerebral infection of the right cortex with 200 TCID50 of brain-adapted (CAM/RB), parental (Edtag), or recombinant virus (EdtagCAMH).
| Virus | Animal | Extent of focus formationa (no. of foci)
|
|||||
|---|---|---|---|---|---|---|---|
| Level 1c
|
Level 2
|
Level 3
|
|||||
| RC | LC | RC | LC | RC | LC | ||
| CAM/RB | a | ++++ | ++++ | +++ | +++ | ++++ | +++ |
| b | ++++ | +++ | ++++ | +++ | ++++ | ++++ | |
| c | +++++ | ++++ | +++++ | +++ | ++++ | +++ | |
| Edtag | a | − | − | − | − | − | − |
| b | − | − | − | − | − | − | |
| c | − | − | − | − | − | − | |
| EdtagCAMH | a | ++ (29) | ++ (24) | ++ (24) | ++ (21) | ++ (20) | ++ (25) |
| b | + (9) | + (3) | ++ (14) | + (8) | ++ (10) | ++ (10) | |
| c | + (5) | + (6) | + (6) | + (7) | ++ (11) | + (2) | |
Three levels of tissue, separated by 50 μm, were examined. Level 1 represents sections cut from the outermost portion of the tissue; levels 2 and 3 are approximately 50 and 100 μm, respectively within the tissue. RC, right cortex; LC, left cortex. +++++, majority of foci of infection (>30) fused together; ++++, many foci of infection (>30), equivalent numbers of separate and fusing foci; +++, many foci (>30), a minority fused together; ++, 10 to 30 foci; +, 1 to 9 foci; −, no foci.
DISCUSSION
Prior to the development of the MV rescue system, it was impossible to modify specific regions of the virus genome. This made the study of the molecular determinants of neuropathogenesis difficult. Nevertheless, when neutralizing monoclonal antibodies were used to modulate the disease process and isolate escape mutants in vitro, a major site was identified in the H gene, residues 368 to 396, which appeared to be functionally important for neurovirulence (20). These observations prompted the present study to investigate whether the H gene alone was sufficient to transfer the neurovirulent phenotype to the parental, attenuated Edmonston strain-derived Edtag virus. To this end, we have generated an insertion vector which permits the addition of variant H genes into a plasmid, thereby generating full-length antigenomic constructs in a single step. In this study, we used the vector to insert the H gene from the brain-adapted CAM/RB and generated an infectious, recombinant virus, EdtagCAMH. This vector has also been used to generate other recombinant viruses with a number of single amino acid changes in the H protein and to accept mutagenized H genes from other MV strains (10a). The recombinant virus grows to similar titers as Edtag and CAM/RB, indicating that the interaction of the newly incorporated H gene with the Edmonston F gene is not impaired and that these proteins can complement each other and give rise to a productive infection. We have shown that the CAM/RB strain and EdtagCAMH recombinant exclusively infect neurons, viral antigen being clearly present in the processes, and have demonstrated the association of neurovirulence with amino acids in the H protein.
Small changes in envelope glycoproteins have profound effects on the neurovirulent phenotype of many viruses, such as lymphocytic choriomeningitis virus mumps virus, rabies virus, and Japanese encephalitis virus (8, 16, 23, 25, 31, 37). Dengue virus provides one of the best models for neurovirulence in rodents. Major determinants of mouse neurovirulence have been identified in the E glycoprotein of the virus. One of these, in common with MV, is in a known antigenic site, residues 383 to 393 (13, 43). Another is comprised of only one amino acid change, E126Q-K (11). The usefulness of this model for mouse neurovirulence is augmented by the availability of the three-dimensional structure, at atomic resolution, of the E glycoprotein of another flavivirus, tick-borne encephalitis virus (31, 38). The three-dimensional structure for the MV H glycoprotein is not, unfortunately, available. However, a putative structure for the protein has been proposed based on the homology modeling with active-site residues in the influenza virus neuraminidase glycoprotein and the paramyxovirus hemagglutinin-neuraminidase glycoprotein. The major determinants of neurovirulence (20) are predicted to be external in this structure (17).
An increase in neurovirulence needs not be due only to the ability to bind a mouse receptor. Neurovirulent Sindbis virus with an alteration in the E2 glycoprotein binds to and enters cells no more efficiently than nonneurovirulent virus. Rather, RNA synthesis is initiated more rapidly and attained fivefold higher levels for the neurovirulent strain (10, 44, 45). For MV, alterations in the H protein have profound effects on CD46 receptor downregulation; the exchange of two amino acids also alters the ability of the virus to use CD46 as a receptor (3, 18).
Rodent models have been generated to investigate the pathogenesis of many viruses, including mumps virus. Alterations in the neuroanatomy and pronounced hydrocephalus were observed upon infection. Cerebellar abnormalities caused by defects in granule cell migration which distinguished neurovirulent and nonneurovirulent mumps strains were also identified (33). We have not observed cerebellar abnormalities in any MV-infected animal. A persistent in vivo infection has been demonstrated in newborn hamsters infected with MV from persistently infected cell cultures. In some cases this infection was accompanied by hydrocephalus which was most likely due to an infection of ependymal cells (12, 27). We have no evidence from the present study for the infection of ependymal cells. It will be interesting to use the EdtagCAMH recombinant virus, in which the progression of the virus is slower, to examine cerebella at later time points to see if later sequelae can be observed in this recombinant MV infection. The relevance of these mouse brain models to human CNS infection by MV is not clear. However, the present study shows that the H gene is very important in MV neuropathogenesis in the model. The H gene has been examined in isolation from the remainder of the brain-adapted CAM/RB genome, and it is clear that its presence allows virus to both enter and replicate in mouse neurons. In particular, it appears that the interactions between the CAM/RB H protein and its F protein counterpart are not perturbed in the recombinant virus. There are six amino acid differences between the Edmonston and CAM/RB F proteins, three of which are nonconservative changes (31a). Clearly, in spite of these differences, the protein interactions necessary for the virus to initiate an infection and grow to equivalent titers in cell culture can occur. Additionally, it is apparent that other regions of the virus genome are involved in neurovirulence. We have demonstrated that for MV, no single gene is exclusively linked to a neurovirulent phenotype, and this correlates well with observations for many other RNA viruses. Future studies will (i) investigate the molecular determinants in the H protein in greater detail and (ii) begin to introduce other genes, M, F, and L, from CAM/RB strain into the Edmonston B strain. We believe that these studies will give important insights into MV neuropathogenesis in the mouse model of encephalitis.
ACKNOWLEDGMENTS
We thank Gudrun Christiansen for helpful discussions and invaluable advice on the establishment of the MV rescue system, Mildred Wylie for providing the chicken embryo fibroblast cells, and Gerd Sutter for the original MVA-T7 virus. Additionally, we thank Roy Creighton for photographic work and Paula Haddock for excellent technical assistance. We acknowledge the help of Uta Gassen in critical reading of the manuscript.
This work was supported by the Wellcome Trust (grant 047245), the European Social Fund, the Deutsche Forschungsgemeinschaft, and the Swiss National Science Foundation (grant 31-43475.95).
REFERENCES
- 1.Agamanolis D P, Tan J S, Parker D L. Immunosuppressive measles encephalitis in a patient with a renal transplant. Arch Neurol. 1979;36:686–690. doi: 10.1001/archneur.1979.00500470056011. [DOI] [PubMed] [Google Scholar]
- 2.Baczko K, Lampe J, Liebert U G, Brinckmann U G, ter Meulen V, Pardowitz I, Budka H, Cosby S L, Isserte S, Rima B K. Clonal expansion of hypermutated measles virus in a SSPE brain. Virology. 1993;197:188–195. doi: 10.1006/viro.1993.1579. [DOI] [PubMed] [Google Scholar]
- 3.Bartz R, Firsching R, Rima B K, ter Meulen V, Schneider-Schaulies J. Differential receptor usage by measles virus strains. J Gen Virol. 1998;79:1015–1025. doi: 10.1099/0022-1317-79-5-1015. [DOI] [PubMed] [Google Scholar]
- 4.Bellini W, Englund G, Rammohan K, McFarlin D E. Evaluation of the structural proteins of the hamster neurotropic strain of measles virus with monoclonal antibodies. J Neuroimmunol. 1986;11:149–163. doi: 10.1016/0165-5728(86)90116-5. [DOI] [PubMed] [Google Scholar]
- 5.Cathomen T, Naim H Y, Cattaneo R. Measles virus with altered envelope protein cytoplasmic tails gain cell fusion competence. J Virol. 1998;72:1224–1234. doi: 10.1128/jvi.72.2.1224-1234.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cattaneo R, Rose J K. Cell fusion by the envelope glycoproteins of persistent measles viruses which cause lethal human brain disease. J Virol. 1993;67:1493–1502. doi: 10.1128/jvi.67.3.1493-1502.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan S P. Induction of chronic measles encephalitis in C57BL/6 mice. J Gen Virol. 1985;66:2071–2076. doi: 10.1099/0022-1317-66-9-2071. [DOI] [PubMed] [Google Scholar]
- 8.Dietzschold B, Wiktor T J, Trojanowski J Q, Macfarlan R I, Wunner W H, Torres-Anjel M J, Koprowski H. Differences in cell-to-cell spread of pathogenic and apathogenic rabies virus in vivo and in vitro. J Virol. 1985;56:12–18. doi: 10.1128/jvi.56.1.12-18.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dörig R E, Marcil A, Chopra A, Richardson C D. The human CD46 is a receptor for measles virus (Edmonston strain) Cell. 1993;75:295–305. doi: 10.1016/0092-8674(93)80071-l. [DOI] [PubMed] [Google Scholar]
- 10.Dropulic L K, Hardwick J M, Griffin D E. A single amino acid in the E2 glycoprotein of sindbis virus confers neurovirulence by altering an early step of virus replication. J Virol. 1997;71:6100–6105. doi: 10.1128/jvi.71.8.6100-6105.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10a.Duprex, W. P. Unpublished results.
- 11.Gualano R C, Pryor M J, Cauchi M R, Wright P J, Davidson A D. Characterisation of dengue 2 virus mutants that induce fusion at elevated pH. Virology. 1998;194:219–223. doi: 10.1006/viro.1993.1252. [DOI] [PubMed] [Google Scholar]
- 12.Haspel M V, Rapp F. Measles virus: an unwanted variant causing hydrocephalus. Science. 1975;187:450–451. doi: 10.1126/science.1111114. [DOI] [PubMed] [Google Scholar]
- 13.Hiramatsu K, Tadano M, Men R, Lai C-J. Mutational analysis of a neutralisation epitope on the dengue type 2 virus (DEN-2) envelope protein: monoclonal antibody resistant DEN-2/DEN-4 chimeras exhibit reduced mouse neurovirulence. Virology. 1996;224:437–445. doi: 10.1006/viro.1996.0550. [DOI] [PubMed] [Google Scholar]
- 14.Kaelin K. Ph.D. thesis. Zurich, Switzerland: University of Zurich; 1995. [Google Scholar]
- 15.Kobune K, Kobune F, Yamanouchi K, Nagashima K, Yoshikawa Y, Hayami M. Neurovirulence of rat brain-adapted measles virus. Jpn J Exp Med. 1993;53:177–180. [PubMed] [Google Scholar]
- 16.Kovamees J, Rydbeck R, Orvell C, Norrby E. Haemagglutinin-neuraminidase (HN) amino acid alterations in neutralisation escape mutants of Kilham mumps virus. Virus Res. 1983;17:117–129. doi: 10.1016/0168-1702(90)90073-k. [DOI] [PubMed] [Google Scholar]
- 17.Langedijk J P, Daus F J, van Oirschot J T. Sequence and structure alignment of Paramyxoviridae attachment proteins and discovery of enzymatic activity for a morbillivirus hemagglutinin. J Virol. 1997;71:6155–6167. doi: 10.1128/jvi.71.8.6155-6167.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lecouturier V, Fayolle J, Caballero M, Carabana J, Celma M L, Fernandez-Munoz R, Wild T F, Buckland R. Identification of two amino acids in the hemagglutinin glycoprotein of measles virus (MV) that govern hemadsorption, HeLa cell fusion, and CD46 downregulation: phenotypic markers that differentiate vaccine and wild-type MV strains. J Virol. 1996;70:4200–4204. doi: 10.1128/jvi.70.7.4200-4204.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liebert U G, ter Meulen V. Virological aspects of measles virus-induced encephalomyelitis in Lewis and BN rats. J Gen Virol. 1987;68:1715–1722. doi: 10.1099/0022-1317-68-6-1715. [DOI] [PubMed] [Google Scholar]
- 20.Liebert U G, Flanagan S G, Loffler S, Baczko K, ter Meulen V, Rima B K. Antigenic determinants of measles virus hemagglutinin associated with neurovirulence. J Virol. 1994;86:1486–1493. doi: 10.1128/jvi.68.3.1486-1493.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liebert U G, Finke D. Measles virus infections in rodents. In: ter Meulen V, Billeter M A, editors. Measles virus. Berlin, Germany: Springer-Verlag; 1995. pp. 149–166. [DOI] [PubMed] [Google Scholar]
- 22.McQuaid S, Cosby S L, Kirk J, Koffi K, Hond M, Lucas S. Distribution of measles virus in the CNS of HIV seropositive children. Acta Neuropathol. 1998;96:637–642. doi: 10.1007/s004010050945. [DOI] [PubMed] [Google Scholar]
- 23.Matloubian M, Somasundaram T, Kolhekar S R, Selvakumar R, Ahmed R. Genetic basis of viral persistence: single amino acid change in the viral glycoprotein affects ability of lymphocytic choriomeningitis virus to persist in adult mice. J Exp Med. 1990;172:1043–1048. doi: 10.1084/jem.172.4.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naniche D, Varior-Krishnan G, Cervoni F, Wild T F, Rossi B, Rabourdin-Combe C, Gerlier D. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J Virol. 1993;67:6025–6032. doi: 10.1128/jvi.67.10.6025-6032.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ni H, Barrett A D. Attenuation of Japanese encephalitis virus by selection of its mouse brain membrane receptor preparation escape variants. Virology. 1998;241:30–36. doi: 10.1006/viro.1997.8956. [DOI] [PubMed] [Google Scholar]
- 26.Niewiesk S, Brinckmann U, Bankamp B, Sirak S, Liebert U G, ter Meulen V. Susceptibility to measles virus-induced encephalitis in mice correlates with impaired antigen presentation to cytotoxic T lymphocytes. J Virol. 1993;67:75–81. doi: 10.1128/jvi.67.1.75-81.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Norrby E, Swoveland P, Kristensson K, Johnson K P. Further studies on subacute encephalitis and hydrocephalus in hamsters caused by measles virus from persistently infected cell cultures. J Med Virol. 1980;5:109–116. doi: 10.1002/jmv.1890050203. [DOI] [PubMed] [Google Scholar]
- 28.Peebles M E. Paramyxovirus M proteins. Pulling it all together and taking it on the road. In: Kingsbury D W, editor. The paramyxoviruses. New York, N.Y: Plenum Press; 1991. pp. 247–256. [Google Scholar]
- 29.Radecke F, Spielhofer P, Schneider H, Kaelin K, Huber M, Dotsch C, Christiansen G, Billeter M A. Rescue of measles virus from cloned DNA. EMBO J. 1995;14:5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reed L J, Muench H. A simple method for estimating fifty percent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 31.Rey F A, Heinz F X, Mandl C, Kunz C, Harrison S C. The envelope glycoprotein from tick-borne encephalitis at 2Å resolution. Nature. 1995;375:291–298. doi: 10.1038/375291a0. [DOI] [PubMed] [Google Scholar]
- 31a.Rima, B. K. Unpublished results.
- 32.Rima B K, Earle J A P, Baczko K, ter Meulen V, Liebert U G, Carstens C, Carabana J, Caballero M, Celma M L, Fernandez-Munoz R. Sequence divergence of measles virus haemagglutinin during natural evolution and adaptation to cell culture. J Gen Virol. 1997;78:97–106. doi: 10.1099/0022-1317-78-1-97. [DOI] [PubMed] [Google Scholar]
- 33.Rubin S A, Pletnikov M, Carbone K M. Comparison of the neurovirulence of a vaccine and wild-type mumps virus strain in the developing rat brain. J Virol. 1998;72:8037–8042. doi: 10.1128/jvi.72.10.8037-8042.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 35.Schneider H, Spielhofer P, Kaelin K, Dotsch C, Radecke F, Sutter G, Billeter M A. Rescue of measles virus using a replication-deficient vaccinia-T7 vector. J Virol Methods. 1997;64:57–64. doi: 10.1016/s0166-0934(96)02137-4. [DOI] [PubMed] [Google Scholar]
- 36.Schneider-Schaulies S, Liebert U G. Pathogenic aspects of persistent measles virus infections of brain tissue. Semin Neurosci. 1991;3:139–147. [Google Scholar]
- 37.Seif I, Coulon P, Rollin P E, Flamand A. Rabies virulence: effect on pathogenicity and sequence characterization of rabies virus mutations affecting antigenic site III of the glycoprotein. J Virol. 1985;53:926–934. doi: 10.1128/jvi.53.3.926-934.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stiasny K, Allison S L, Marchler-Bauer A, Kunz C, Heinz F X. Structural requirements for low-pH-induced rearrangements in the envelope protein of tick-borne encephalitis virus. J Virol. 1996;70:207–212. doi: 10.1128/jvi.70.11.8142-8147.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sutter G, Ohlmann M, Erfle V. Non-replicating vaccinia vector efficiently expresses bacteriophage T7 RNA polymerase. FEBS Lett. 1995;371:9–12. doi: 10.1016/0014-5793(95)00843-x. [DOI] [PubMed] [Google Scholar]
- 40.Taylor M J, Godfrey E, Baczko K, ter Meulen V, Wild T F, Rima B K. Identification of several different lineages of measles virus. J Gen Virol. 1991;57:357–364. doi: 10.1099/0022-1317-72-1-83. [DOI] [PubMed] [Google Scholar]
- 41.ter Meulen V, Stephenson J R, Kreth H W. Subacute sclerosing panencephalitis. In: Fraenkel-Conrat H, Wagner R R, editors. Comprehensive virology. Vol. 18. New York, N.Y: Plenum; 1983. pp. 105–159. [Google Scholar]
- 42.Tober C, Seufert M, Schneider H, Billeter M A, Johnston I C, Niewiesk S, ter Meulen V, Schneider-Schaulies S. Expression of measles virus V protein is associated with pathogenicity and control of viral RNA synthesis. J Virol. 1998;72:8124–8132. doi: 10.1128/jvi.72.10.8124-8132.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trirawatanapong T, Chandran B, Putnak R, Padmanabhan R. Mapping of a region of dengue virus type-2 glycoprotein required for binding by a neutralising monoclonal antibody. Gene. 1992;116:139–150. doi: 10.1016/0378-1119(92)90509-N. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tucker P C, Strauss E G, Kuhn R J, Strauss J H, Griffin D E. Viral determinants of age-dependent virulence of Sindbis virus for mice. J Virol. 1993;67:4605–4610. doi: 10.1128/jvi.67.8.4605-4610.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tucker P C, Lee S H, Bui N, Martinie D, Griffin D E. Amino acid changes in the Sindbis virus E2 glycoprotein that increase neurovirulence improve entry into neuroblastoma cells. J Virol. 1997;71:6106–6112. doi: 10.1128/jvi.71.8.6106-6112.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ullrich A, Shine J, Chirgwin J, Pictet R, Tischer E, Rutter W J, Goodman H M. Rat insulin genes: construction of plasmids containing the coding sequences. Science. 1977;196:1313–1319. doi: 10.1126/science.325648. [DOI] [PubMed] [Google Scholar]
- 47.Urbanska E M, Chambers B J, Ljunggren H-G, Norrby E, Kristensson K. Spread of measles virus through axonal pathways into limbic structures in the brain of TAP1−/− mice. J Med Virol. 1997;52:362–369. doi: 10.1002/(sici)1096-9071(199708)52:4<362::aid-jmv3>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 48.Valsamakis A, Schneider H, Auwaerter P G, Kaneshima H, Billeter M A, Griffin D E. Recombinant measles viruses with mutations in the C, V, or F gene have altered growth phenotypes in vivo. J Virol. 1998;72:7754–7761. doi: 10.1128/jvi.72.10.7754-7761.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wild T F, Malvoisin E, Buckland R. Measles virus. Both the hemagglutinin and fusion glycoproteins are required for fusion. J Gen Virol. 1991;72:439–442. doi: 10.1099/0022-1317-72-2-439. [DOI] [PubMed] [Google Scholar]
- 50.Wild T F, Buckland R. Functional aspects of envelope-associated measles virus proteins. In: ter Meulen V, Billeter M A, editors. Measles virus. Berlin, Germany: Springer-Verlag; 1995. pp. 51–64. [DOI] [PubMed] [Google Scholar]