There have been tremendous advances in restorative dentistry, particularly with the development of adhesive materials to replace lost tooth structure and jaw implants on which to place prostheses securely.
Repair of teeth
Individuals vary in tooth shade and shape, and teeth yellow with age. Teeth are damaged by caries, wear, failed restorations, trauma, and congenital and developmental defects. Patients usually demand treatment for pain, when appearance is compromised, or when there are occlusal problems (see previous article).
Restorative dental care is indicated to treat pain, poor aesthetic appearance, and poor occlusal function
Restorations
Most older adults have had restorations (fillings), but, with the benefits of health education and fluoride, many younger people have unrestored teeth.
Most restorations are placed to treat caries. The decay is removed mechanically, the cavity shaped to retain the filling, and material is packed into the cavity and then sets hard. Even high quality restorations have a finite life span. If the pulp is diseased, root canal treatment is necessary, which involves removing the pulp and cleansing and filling the chamber.
Amalgam
Amalgam contains silver, copper, tin, and zinc mixed with mercury, and sets within a few minutes. Exposure to mercury vapour is hazardous. Mercury is neurotoxic, and even in people with low level chronic exposure, subtle preclinical effects on symptoms, mood, motor function, and cognition have been identified. Pregnant dental staff have special concerns related to any daily occupational exposure to mercury (or nitrous oxide).
However, any risk to patients from dental amalgams is less clear. Twenty two million amalgams are placed annually in the United Kingdom, with no reliable evidence of associations with systemic disease, although a few patients have allergies or lichenoid oral reactions. Austria, Germany, and Sweden have restricted amalgam use, but removal of amalgam on health grounds diagnosed by a dentist is unethical. There is no reliable evidence for implicating amalgam in Alzheimer's disease, autoimmune diseases, birth defects, digestive disturbances, multiple sclerosis, or Parkinson's disease.
Amalgam has physical properties superior to tooth coloured materials, the only reasonable alternatives. It is the most cost effective restorative material, with an average life span of about five years, although some fillings last 20 years or more. Amalgam has been used for over 170 years. Nevertheless, because of the health concerns the UK Department of Health has recently advised that amalgams should not be placed in pregnant women. After assessment of the potential risks of undergoing dental treatment during pregnancy, it can be stated that necessary treatment should not be withheld. Dental treatments are best performed in the second trimester for the benefit of the fetus and optimal comfort of the pregnant woman.
• Dental amalgam has been used for more than a century• Amalgam is stronger and longer lasting than toothcoloured restorations but is less aesthetically pleasing• There is no reliable evidence of systemic health risk to those with amalgam restorations, but it is recommended that they are not placed or removed in pregnant women
Tooth coloured materials
Tooth coloured materials or “white fillings” are usually either composite resins that adhere to the tooth or glass ionomer cements. They can contain chemicals such as acrylate, peroxides, bisphenol, formaldehyde, hexane, hydroquinone, phenol, polyurethane, silane, toluene, and xylene, some of which have been suspected of toxicity. However, apart from occasional allergic reactions, there is little evidence of adverse effects arising from the placement of tooth coloured fillings. Concerns about an oestrogenic effect, for example, have not been substantiated. These restorations have aesthetic appeal. The disadvantage is they cannot withstand heavy biting forces.
Bleaching
Extrinsic tooth stains can be reduced by scaling and polishing. Intrinsic staining is difficult to remove. The enamel surface can be removed by rotary instruments, microabrasion sandblasting with aluminum oxide, or polishing with pumice in acid. Bleaching with carbamide peroxide gel in a gum shield is effective for mild discolourations.
Tetracycline staining is now much reduced after the avoidance of its use in pregnant and lactating women and children under 12 years old.
Veneers
Porcelain or composite veneers stuck on the tooth surface can improve their shape and shade for up to 10 years. Minimal preparation is required.
Crowns
Crowns are indicated when little tooth material remains. Crowns generally cover all or much of the tooth crown and are the same size and shape as the original tooth, unless that was malformed or misaligned. Crowns are cemented on the teeth, are not removable by the patient, and can withstand chewing. Full gold or non-precious metal alloy crowns are often prescribed for posterior teeth.
Aesthetic appearance can be improved mainly by• Tooth cleaning• Bleaching• Tooth coloured restorations• Veneers• Crowns
Gold crowns, made from gold alloyed with platinum, palladium, copper, silver, and zinc, last from 10 to 20 years. Lichenoid reactions to them occasionally occur.
Non-precious metal crowns (mainly nickel) are stronger and cheaper. Beryllium is often present, giving rise to concern about toxicity to dental laboratory technicians.
All-porcelain crowns give a better aesthetic appearance, but more tooth preparation is required.
Most crowns have porcelain fused to a metal substructure to combine aesthetics with strength.
Inlays and onlays
These are laboratory made and expensive. They fit a tooth to replace lost tooth material.
Replacement of teeth
In 1988, 52% of people aged 65-74 years in Britain lacked natural teeth, reflecting the high levels of dental disease in the past. By the year 2008, this percentage is expected to have dropped to about 25%. People lose teeth or have tooth spaces for various reasons, including caries, periodontitis, failed dentistry, trauma, and hypodontia. In general, most people desire replacement of anterior teeth so that they have a reasonable smile. Posterior teeth may need to be replaced to restore occlusion.
All teeth can be replaced with removable partial or complete dentures. Bridgework or fixed tooth replacement is possible when sufficient teeth of good quality remain that can be used as supports for false teeth. Dental implants can replace teeth independently of remaining natural teeth and can replace single teeth as well as complete dental arches.
In general, young patients with relatively unrestored teeth have all options for tooth replacement open to them. Tooth replacement is much more difficult if many teeth are missing or they have been heavily restored.
Missing teeth can be replaced with• Removable dentures (placed on mucosa, teeth, roots, or implants)• Non-removable bridges fixed to teeth• Implants in jaw, carrying a denture, crown, or bridge
Dentures
Dentures are removable by the patient and are the most cost effective way of replacing teeth. Dentures are often constructed from plastic (acrylic resin) but may also have cobalt, chromium, or gold components. The cost depends on the complexity of design and materials used. The incidence of allergic responses is extremely low. Maintenance of oral hygiene is fundamental to the success of the treatment.
Complete dentures are retained by adhesion via saliva to the mucosa and the adaptive response of the oral musculature. Most patients have few problems wearing complete upper dentures. The most common complaints are looseness and pain related to a lower denture. Denture problems may increase as the alveolar bone naturally resorbs after tooth extraction or when there is xerostomia or impaired neuromuscular control.
Partial dentures replace teeth in patients who are partially dentate. Metal alloy clasps and rests aid retention and support.
Onlays (overlays, overdentures)—When the dentition is severely worn or only a few teeth remain, dentures may be constructed over the remnants. The advantages in retaining such teeth or roots are that the alveolar bone and proprioception of the roots are maintained and the stability and retention of the denture are improved.
Obturators—Palatal defects may be congenital, as in cleft palate, or acquired after tumour excision. Oral function (speech, drinking, and eating) may be severely compromised since air, food, and fluids pass between the mouth and the nose. Dentures incorporating a bung or obturator component provide a seal between the oral and nasal cavities and thus improve function.
Bridgework
Bridgework involves the preparation of supporting teeth known as abutments. The false tooth or pontic is attached to a crown known as a retainer, and the prosthesis is cemented on to the abutment. The average lifespan for such bridgework is 10 years.
Resin bonded bridgework is secured to the teeth with adhesive composite resin materials. It is indicated when the teeth are relatively unrestored. The main advantage is that little or no tooth preparation is required, and it is particularly suitable for young patients with missing teeth. However, not all teeth can be replaced in this way. The average lifespan is between 5 and 10 years.
Dental implants
Implants provide replacement of missing natural teeth with artificial analogues. Probably the most important development in dentistry, implants can be used singly, to support a crown, or in groups to stabilise dentures or bridges.
A titanium precision screw is surgically inserted into the alveolus where it anchors (a process called osseointegration). After three to six months, an intraoral component or abutment is added to support a prosthesis. These implants have success rates for individual implants of >95% in the lower jaw and >90% in the upper jaw over 10 years. Treatment, however, requires considerable skills and appropriate case selection, planning, clinical procedures, and maintenance.
There are few absolute systemic contraindications to implants. Failure rates increase with diabetes, chemotherapy, tobacco smoking, ectodermal dysplasia, and erosive lichen planus. Implant treatment is expensive, in time and materials, and any contraindication to surgery precludes implants.
Dental implants• Are placed surgically in the alveolus• Carry a denture, crown, or bridge• Result in a very stable retentive prosthesis• Have a high success rate (> 90% last at least 10 years)
Further reading
Albrektsson T, Sennerby L. State of the art in oral implants. J Clin Periodontol 1991;18:474-81
Barclay CW, Walmsley AD. Fixed and removable prosthodontics. Edinburgh: Churchill Livingstone, 1998
Echeverria D, Aposhian HV, Woods JS, Heyer NJ, Aposhian MM, Bittner AC Jr, et al. Neurobehavioral effects from exposure to dental amalgam Hg(o): new distinctions between recent exposure and Hg body burden. FASEB J 1998;12:971-80
Eley BM. The future of dental amalgam: a review of the literature. Part 6: Possible harmful effects of mercury from dental amalgam. Br Dent J 1997;182:455-9
Mount GJ, Hume WR. Preservation and restoration of tooth structure. London: Mosby, 1998
Schmalz G. The biocompatibility of non-amalgam dental filling materials. Eur J Oral Sci 1998;106:696-706
Sheldon T, Treasure E. Dental restoration: what type of filling? Effective Health Care 1999;5(2):1-12
Wasylko L, Matsui D, Dykxhoorn SM, Rieder MJ, Weinberg S. A review of common dental treatments during pregnancy: implications for patients and dental personnel. J Can Dent Assoc 1998;64:434-9
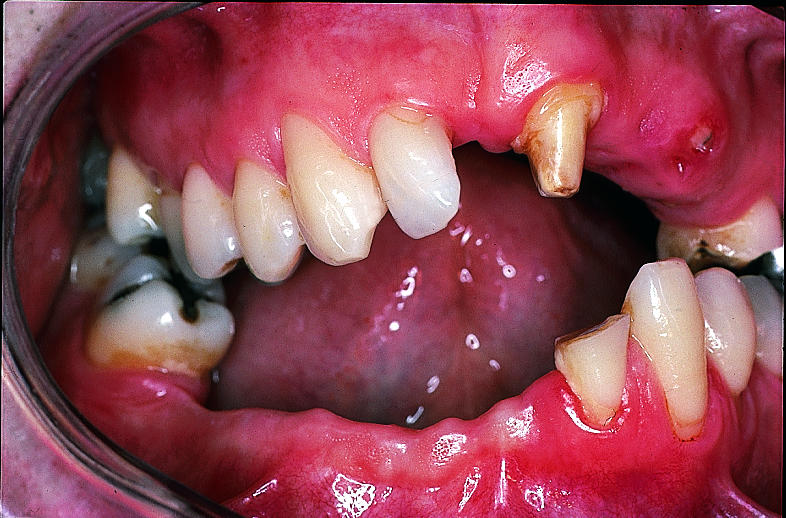
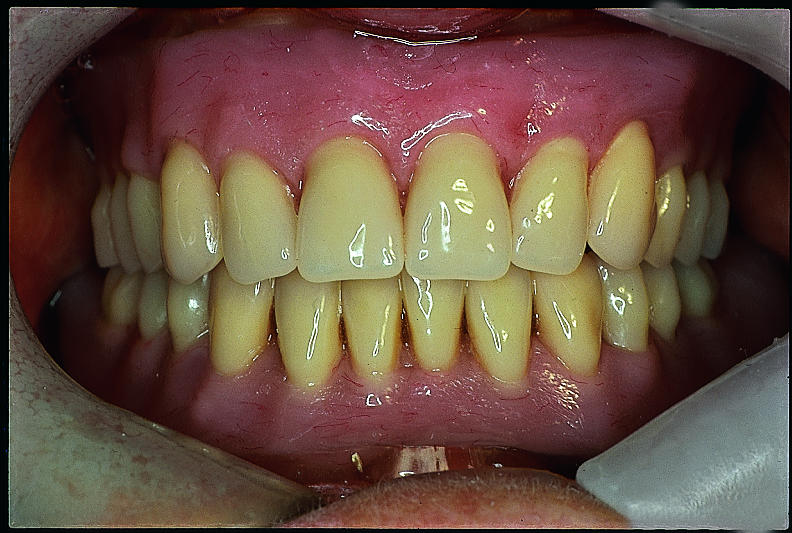
Figure.


Patient with badly worn and spaced teeth (top) and appearance after restoration (bottom)
Figure.

Tooth damage by trauma (top) and appearance after restoration (bottom)
Figure.

Dental amalgams and a composite restoration in molars to treat caries
Figure.

Porcelain veneers to treat tetracycline staining of upper teeth (appearance of lower teeth was deemed acceptable)
Figure.

Conventional crown on maxillary left central incisor
Figure.
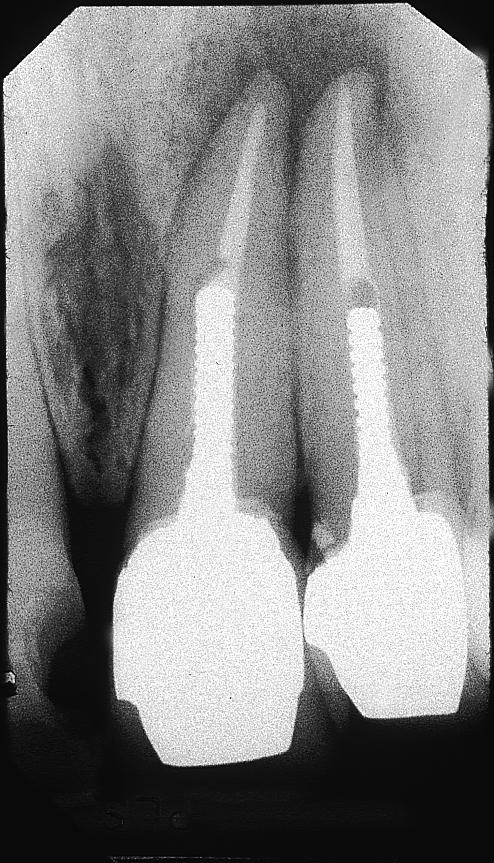
Radiograph of post crowns showing endodontic filling and retaining post
Figure.
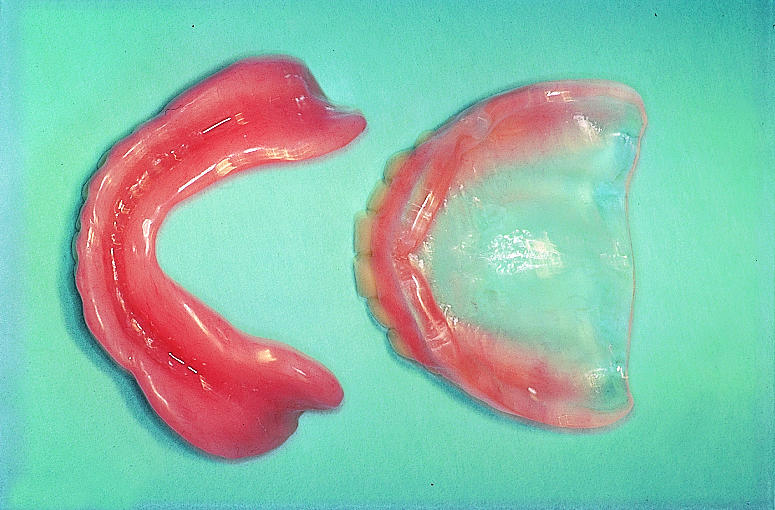
Complete lower and upper dentures (top) and their appearance in situ (bottom)
Figure.
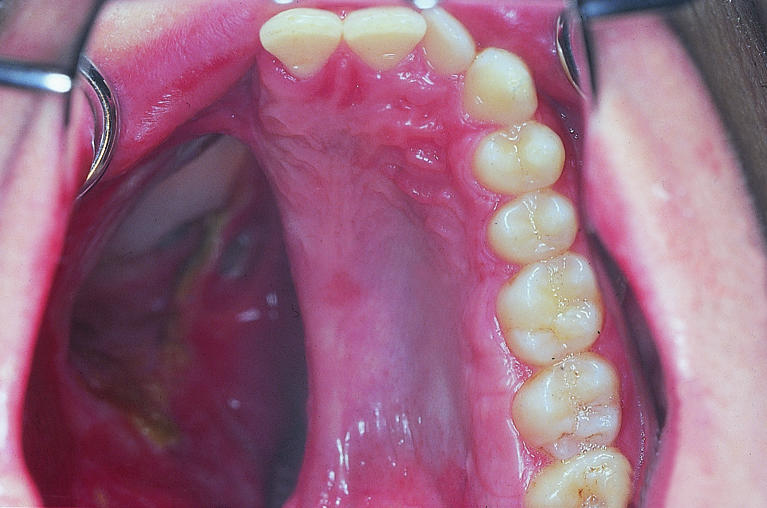
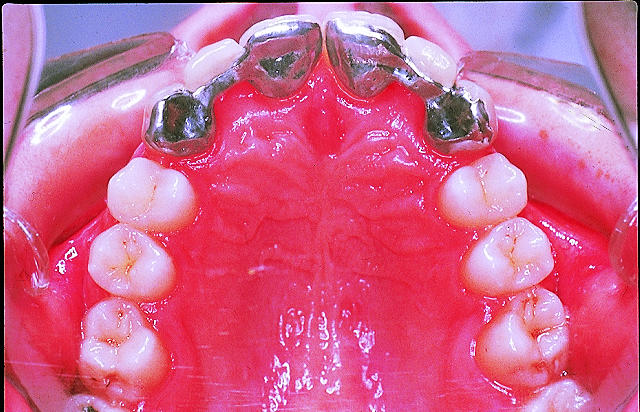
Partial dentures
Figure.
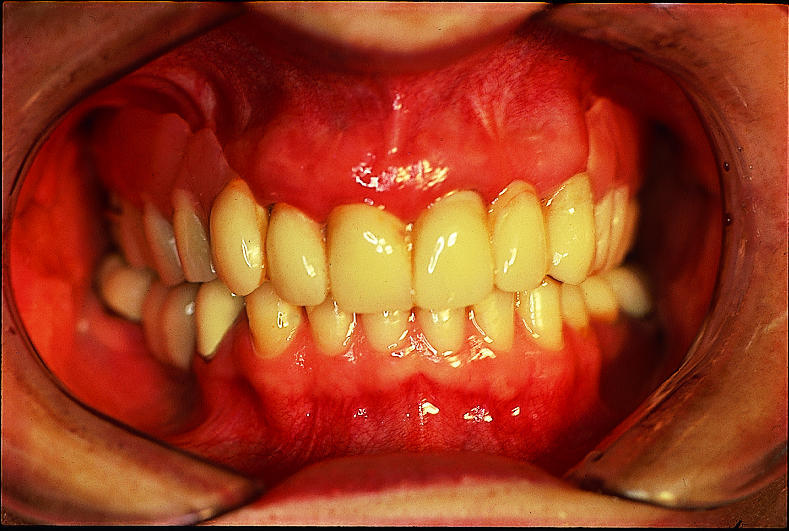
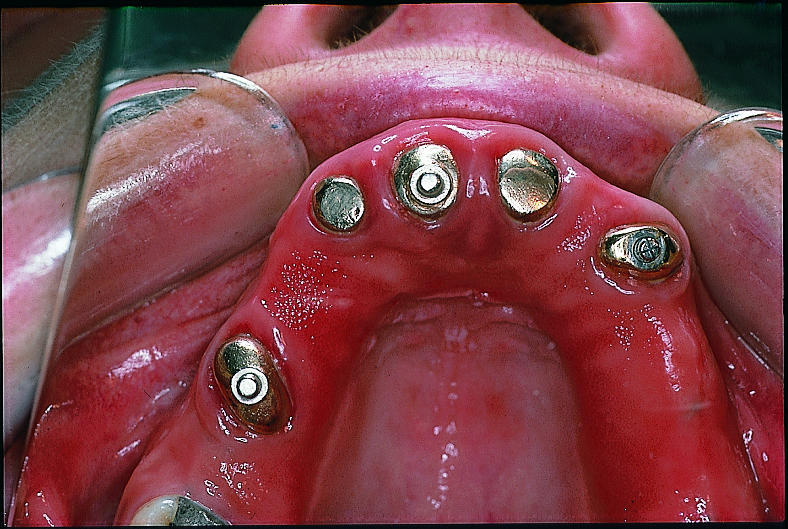
Overdenture (top) supported by metal studs inserted into natural tooth roots (bottom)
Figure.

Patient with palatal defect (left) and obturator made to separate oral and nasal cavities (right)
Figure.


Conventional bridgework in patient with missing incisor: neighbouring teeth are ground down to take artificial crowns (top) and final result (bottom)
Figure.


Resin bonded bridgework in patient with hypodontia (top left): with minimal tooth preparation, the metal substructure is glued to the intact teeth (top right) and final result (left)
Figure.
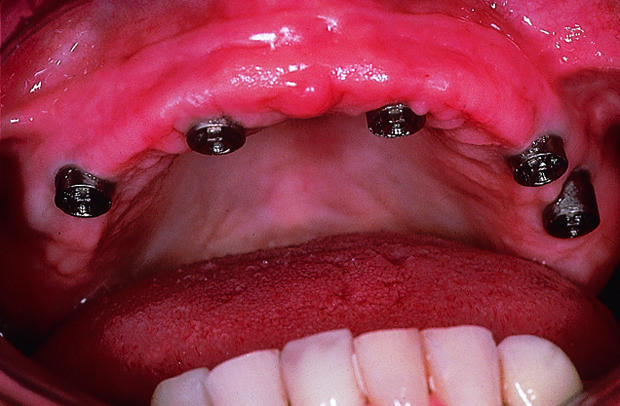

Patient with implants inserted surgically into alveolar bone of edentulous maxilla (left) to stabilise fixed bridge (right)
Figure.


Patient with missing teeth and jaw bone after road traffic accident: temporary appliance on dental implants (left) and definitive prosthesis in place (right)
Acknowledgments
Crispian Scully is grateful for the advice of Rosemary Toy, general practitioner, Rickmansworth, Hertfordshire.
Footnotes
Ken Hemmings is consultant in the department of conservative dentistry, Eastman Dental Institute for Oral Health Care Sciences, University College London, University of London; Brigitte Griffiths is consultant and John Hobkirk is professor in the department of prosthetic dentistry, Eastman Dental Institute for Oral Health Care Sciences; and Crispian Scully is dean at the Eastman Dental Institute for Oral Health Care Sciences (www.eastman.ucl.ac.uk).
The ABC of oral health is edited by Crispian Scully and will be published as a book in autumn 2000.



