Abstract
We aimed to examine the drug retention rate (DRR) of the interleukin-17 inhibitor ixekizumab in a real-world monocentric cohort of psoriatic arthritis (PsA) patients and to assess the predictors of drug discontinuation. Consecutive PsA patients who underwent treatment with ixekizumab from October 2019 to February 2023 were enrolled in this observational, retrospective, monocentric study. Clinical records were assessed at baseline and throughout the follow-up period. We collected sociodemographic data, smoking habits, body mass index, the presence of Human Leukocyte Antigen B27, comorbidities, disease involvement and duration, previous therapy, discontinuation of ixekizumab, reasons for discontinuation, and adverse events (AEs). DRR was evaluated as time to drug discontinuation and assessed through Kaplan–Meier curves. Baseline factors predicting drug discontinuation were investigated through logistic regression models. Eighty PsA patients were included in this study. Ixekizumab was administered at a dose of 160 mg by subcutaneous injection at baseline, followed by 80 mg every four weeks thereafter. Ixekizumab had a 38-month-cumulative DRR of 43.8%, accounting for both inefficacy and AEs. When considering only inefficacy, the DRR was 62.6%. Comorbidities (p = 0.665), obesity (p = 0.665), smoking (p = 0.884), disease duration ≤ 2 years (p = 0.071), axial (p = 0.131) and skin involvement (p = 0.460), and previous therapies, including conventional synthetic (p = 0.504) and biological (p = 0.474) Disease-Modifying Antirheumatic Drugs (bDMARDs), as well as the number of previous bDMARDs or targeted synthetic Disease-Modifying Antirheumatic Drugs (tsDMARDs), did not significantly affect the DRR (p = 0.349). Multivariate analysis found no independent predictors of drug discontinuation. The most frequent AEs leading to discontinuation were skin reactions; no severe infections were observed. In our real-world study, comorbidities, disease duration, and previous therapies did not affect the DRR of ixekizumab. Ixekizumab had a favorable safety profile, with no severe AEs observed.
Keywords: drug retention rate, ixekizumab, psoriatic arthritis
1. Introduction
Psoriatic arthritis (PsA) is complex disease characterized by a combination of musculoskeletal manifestations, such as peripheral and axial involvement, dactylitis, and enthesitis, along with various extra-articular abnormalities [1]. PsA affects 24% of individuals with psoriasis (PsO) [1], yet it can go undiagnosed in up to 30% of these cases [2]. Subclinical enthesitis is detectable in up to 36% of PsO patients [3], while synovitis is detected in 50.7–85.0% of these patients across various studies [4,5,6]. Although PsO typically precedes the onset of arthritis, 15% of patients exhibit both PsO and joint symptoms simultaneously, and 20% develop PsA before skin involvement [1]. The diverse clinical manifestations of PsA make its diagnosis particularly challenging. Early diagnosis and treatment, however, are fundamental to prevent joint damage, as they are linked to improved long-term outcomes [1] and better patient-reported outcomes [7]. Early treatment in a prodromal phase in patients with PsO experiencing arthralgia could also help prevent the onset of PsA [8].
PsA patients, moreover, often present with several comorbidities that need careful consideration during the management of the disease, such as cardiovascular disease and metabolic disorders [9].
Interleukin 17 (IL-17) plays a key role in the pathogenesis of PsA, contributing to inflammation, especially in the skin and entheses. Specifically, IL-17A, through its interaction with its receptor, triggers proinflammatory effects in neutrophils and macrophages. These proinflammatory effects also involve keratinocytes and endothelial cells. At the level of endothelial cells, IL-17A may increase procoagulant activity, thus contributing to endothelial dysfunction and increasing the risk of cardiovascular comorbidities [10,11]. Ixekizumab, a monoclonal antibody directed against IL-17A, prevents its binding to the IL-17 receptor [12], and it is approved by the European Medicines Agency for the treatment of PsA, plaque PsO, and axial spondyloarthritis [13].
The early use of IL-17 inhibitors in PsO patients at high risk for PsA has been shown to reduce joint pain and subclinical inflammation, suggesting potential for PsA interception strategies [8].
In patients diagnosed with PsA, however, the phase 3 randomized controlled SPIRIT-P1 and SPIRIT-P3 trials showed that ixekizumab effectively reduces disease activity and radiographic progression, as well as in improving patients’ function and quality of life in biologic-naïve individuals [14]. In the SPIRIT-H2H, Ixekizumab demonstrated greater efficacy than adalimumab in achieving concurrent improvements of joint and skin involvement among biologic-naïve PsA patients [15,16]. Additionally, in the SPIRIT-P2 study, ixekizumab improved signs, symptoms, and patient-reported outcomes, even in patients previously treated with tumor necrosis factor inhibitors (TNF-i) [17,18,19], maintaining a favorable safety profile [14,17,20,21].
There are increasing amounts of data regarding the real-world efficacy and safety of patients with PsO who are treated with ixekizumab [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], and currently, interest in real-world data regarding its efficacy and safety profile in PsA is increasing [31,40,41,42,43,44,45,46,47,48,49,50,51,52]. Indeed, real-world studies offer additional clinical insights into the disease in a heterogenous context such as the clinical setting, when patients comorbidities and contextual factors can impact the management of the disease and its outcome as well as the drug retention rate (DRR) [53,54].
The objective of this study is to examine the DRR of ixekizumab in a real-world monocentric cohort of PsA patients and to assess the predictors of drug discontinuation.
2. Materials and Methods
This is an observational, retrospective, non-profit study, involving consecutive adult patients (≥18 years) affected by PsA, and follow-ups were performed at the Academic Rheumatology Centre of Clinical and Biological Sciences Department of Turin University—Turin, Mauriziano Hospital, Italy, in patients who underwent treatment with ixekizumab from October 2019 to February 2023.
Inclusion criteria encompassed (i) adult age; (ii) fulfilment of CASPAR classification criteria for PsA [55]; and (iii) availability of complete data records. Exclusion criteria were: (i) less than two follow-up visits and (ii) inability to provide informed consent.
Clinical and laboratory data were extracted from patients’ medical records. Specifically, we collected the following information: sociodemographic data, smoking habits, body mass index, the presence of Human Leukocyte Antigen B27 (HLA-B27), comorbidities, phenotypes of PsA, disease duration, previous and concomitant therapies, occurrence of adverse events (AEs) and infections, any withdrawal of ixekizumab, and the cause for discontinuation.
Considering the retrospective study design, no specific sample size was estimated for this study.
The local Institutional Ethics Boards approved the study (Interagency Territorial Ethics Committee A.O.U. Città della Salute e della Scienza, No. 139/2023), and informed consent was obtained from all participating patients.
Statistics
Firstly, descriptive statistics were provided. Dichotomic variables were expressed as percentage whereas continuous variables as mean ± standard deviation (SD) or median and range interquartile range (IQR) according to their distribution. Kaplan–Meier curves were built to evaluate the cumulative DRR of ixekizumab with the event being drug discontinuation due to inefficacy and/or AEs. Furthermore, Kaplan–Meier curves were performed to evaluate the influence of patient clinical characteristics on the DRR of ixekizumab. Survival curves were thus compared by using the log-rank test. To exploratively assess possible baseline predictors of drug discontinuation, age- and male sex-adjusted multivariate regression logistic models were exploited. The purposeful selection process of covariates started by a univariate analysis of each variable and their clinical relevance. At the end of this multistep process of deleting and refitting, age- and sex-adjusted multivariate models were built, providing odds ratio (OR) estimations of significant associations between clinical features and drug discontinuation. Disease duration ≤ 2 years (lacking specific definition of early PsA [56]), HLA-B27, the presence of comorbidities and obesity, axial involvement and concomitant active skin disease, previous therapies with either conventional synthetic Disease-Modifying Antirheumatic Drugs (csDMARDs) or biological Disease-Modifying Antirheumatic Drugs (bDMARDs), were selected as possible characteristics impacting the drug discontinuation considering univariate analyses but also their clinical relevance according to available literature [57]. Different age- and male sex-adjusted multivariate regression logistic models were also built, taking into account the number of patients discontinuing the drug in this cohort.
Correlation analyses were also estimated among the cumulative number of previous bDMARDs/targeted synthetic Disease-Modifying Antirheumatic Drugs (tsDMARDs) and clinical features.
The statistical significance was set at p < 0.05 and all p-values were two-sided. The Statistics Package for Social Sciences (SPSS for Windows, version 22.0, SPSS Inc., Chicago, IL, USA) was used to exploit both regression and correlation analyses, and GraphPad for Windows (version 8.0, San Diego, CA, USA) was used for the assessment of DRR.
3. Results
Eighty patients with PsA were included in the study and followed up on for a median of 12 (IQR 23.2) months. The baseline clinical features of the whole patient cohort are summarized in Table 1.
Table 1.
Demographic, clinical features, and discontinuation of therapy.
| PsA Patients’ Characteristics and Treatment | 80 Patients |
|---|---|
| Demographic characteristics | |
| Age, years, mean ± SD, years | 50.1 ± 11.8 |
| Male sex, n. (%) | 24 (30.0) |
| BMI, mean ± SD, kg/m2 | 28.1 ± 5.4 |
| Obesity (BMI ≥ 30 kg/m2), n. (%) | 27 (33.8) |
| Smoking habit, n. (%) | 22 (27.5) |
| Clinical characteristics | |
| Disease duration median (IQR), years | 4 (9) |
| Disease duration ≤ 2 years, n. (%) | 30 (37.5) |
| Disease duration ≥ 5 years, n. (%) | 38 (47.5) |
| Disease duration ≥ 10 years, n. (%) | 21 (26.3) |
| HLA-B27, n. (%) | 5 (6.3) |
| Peripheral involvement, n. (%) | 80 (100.0) |
| Skin involvement, n. (%) | 68 (85.0) |
| Axial involvement, n. (%) | 25 (31.3) |
| Enthesis involvement, n. (%) | 35 (43.8) |
| Psoriatic onychopathy, n. (%) | 19 (23.8) |
| Comorbidities | |
| Comorbidity, n. (%) | 46 (57.5) |
| High blood pressure, n. (%) | 36 (45.0) |
| Type 2 diabetes, n. (%) | 17 (21.3) |
| Fatty liver disease, n. (%) | 17 (21.3) |
| Cardiovascular disease, n. (%) | 16 (20.0) |
| Dyslipidemia, n. (%) | 12 (15.0) |
| Kidney disease, n. (%) | 5 (6.3) |
| Previous treatment | |
| Previous therapy with NSAIDs n. (%) | 39 (48.8) |
| Previous therapy with GCs n. (%) | 45 (56.3) |
| Previous therapy with csDMARDs n. (%) | 65 (81.3) |
| Previous therapy with MTX n. (%) | 61 (76.3) |
| Previous therapy with bDMARDs n. (%) | 49 (61.3) |
| Previous therapy with tsDMARDs n. (%) | 6 (7.5) |
| Previous TNFi n. (%) | 46 (57.5) |
| Previous IL-12/23i n. (%) | 4 (5.0) |
| Previous IL-17i n. (%) | 12 (15.0) |
| Previous tsDMARDs n. (%) | 9 (11.3) |
| Failure to 1 bDMARD/tsDMARD n. (%) | 32 (40.0) |
| Failure to 2 bDMARDs/tsDMARDs n. (%) | 15 (18.8) |
| Failure to 3 or more bDMARDs/tsDMARDs n. (%) | 9 (11.3) |
| Ixekizumab treatment | |
| Ongoing at the last observation n. (%) | 43 (53.8) |
| Discontinuation due to inefficacy n. (%) | 25 (31.3) |
| Discontinuation due to primary inefficacy n. (%) | 9 (11.3) |
| Discontinuation due to secondary inefficacy n. (%) | 16 (20.0) |
| Discontinuation due to AEs n. (%) | 12 (15.0) |
Footnotes: PsA, psoriatic arthritis; BMI, body mass index; SD, standard deviation; IQR, interquartile range; HLA, Human Leukocyte Antigen; NSAID, non-steroidal anti-inflammatory drugs; GCs, Glucocorticoids; csDMARDs, conventional synthetic Disease-Modifying Antirheumatic Drugs; MTX, methotrexate; bDMARDs, biologic Disease-Modifying Antirheumatic Drugs; tsDMARDs, targeted synthetic Disease-Modifying Antirheumatic Drugs; TNFi, tumor necrosis factor inhibitor; IL-12/23i, interleukin 12/23 inhibitor; IL-17i, interleukin 17 inhibitor; AEs, adverse events.
At the first observation, the mean age was 50.1 ± 11.8 years. Twenty-four (30.0%) of the patients were male, twenty-seven (33.8%) were obese, and twenty-two (27.5%) were smokers.
Forty-six (57.5%) patients presented comorbidities, and the main comorbidities were high blood pressure (n. 36, 45.0%), type 2 diabetes (n. 17, 21.3%), fatty liver disease (n. 17, 21.3%), cardiovascular disease (n. 16, 20.0%), dyslipidemia (n. 12, 15.0%), and kidney disease (n. 5, 6.3%).
The median disease duration was 4 (IQR 9) years. All patients presented peripheral joint involvement; in addition, 25 (31.3%) displayed axial and 35 (43.8%) enthesis involvement. Sixty-eight (85%) showed skin involvement, and nineteen (23.8%) psoriatic onychopathy.
All patients received ixekizumab at a dose of 160 mg by subcutaneous injection at baseline, followed by 80 mg every four weeks thereafter.
Sixty-five (81.3%) patients had received csDMARDs before ixekizumab, with the majority (n. 61, 76.3%) receiving methotrexate. Forty-six (57.5%) patients had received at least one TNFi, four (5%) received one interleukin 12/23 inhibitor (IL-12/23i), nine (11.3%) received a tsDMARDs, and twelve (15%) had already been treated with an IL-17i medication. Among patients previously treated with secukinumab, five (41.7%) discontinued ixekizumab during follow-up, of whom three (25%) ended the treatment because of ineffectiveness. Fifty-six (70.1%) had experienced a failure with at least one bDMARD/tsDMARD and nine (11.3%) to three or more bDMARDs/tsDMARDs before ixekizumab.
Forty-three (53.8%) patients were on ixekizumab at the last follow-up visit. Among those who discontinued the treatment, 25 (31.3%) did so due to inefficacy, with 9 (11.3%) experiencing primary inefficacy and 10 (12.5%) experiencing secondary inefficacy, while 12 (15%) discontinued treatment due to AEs (Table 1).
3.1. Drug Retention Rate
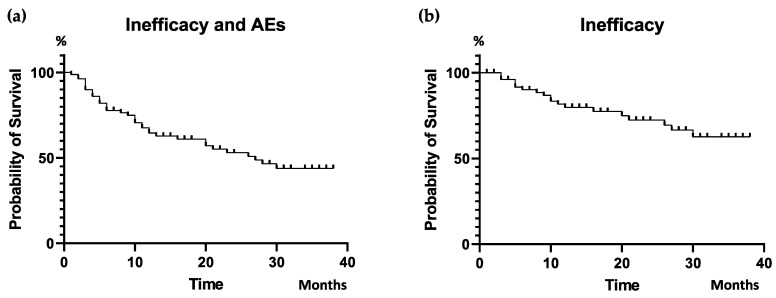
Ixekizumab was administered in our cohort for a median of 12 (IQR 23.2) months. Taking follow-up into account, the cumulative 38 month DRR of ixekizumab was estimated to be 43.8%, considering the discontinuation for both inefficacy and side effects, whereas in 62.6%, the interruption was only due to inefficacy (Figure 1).
Figure 1.
Cumulative DRR of ixekizumab: Inefficacy and AEs (a) and Inefficacy (b). DRR, drug retention rate; AEs, adverse events.
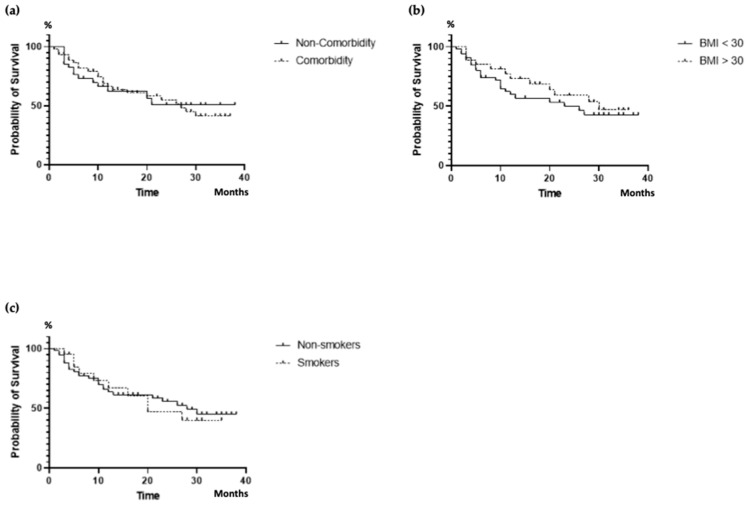
After stratifying the results, it was evident that the DRR of ixekizumab was unaffected by concomitant comorbidities (p = 0.993), obesity (p = 0.665), and smoking habit (p = 0.884) (Figure 2).
Figure 2.
DRR of ixekizumab according to comorbidities (a), obesity (b), and smoking (c). DRR, drug retention rate; BMI, body mass index.
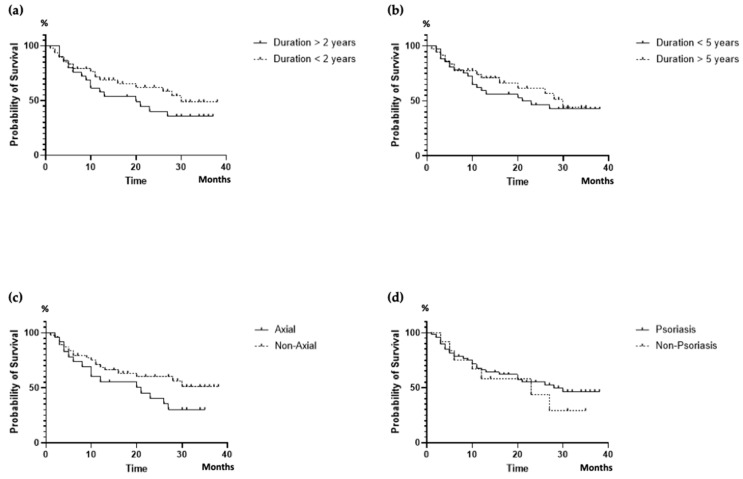
Despite a positive trend noted in patients with a disease duration ≤ 2 years (p = 0.071), the DRR did not appear to be significantly influenced by the disease duration. DRR was not significantly different (p = 0.062) between patients with axial and peripheral involvement (p = 0.131), despite a numerically higher proportion of patients with peripheral involvement persisted on treatment in the long term. Skin involvement did not influence the DRR of ixekizumab (p = 0.460) (Figure 3).
Figure 3.
DRR of ixekizumab according to disease duration (a,b), axial disease (c), and skin involvement (d). DRR, drug retention rate.
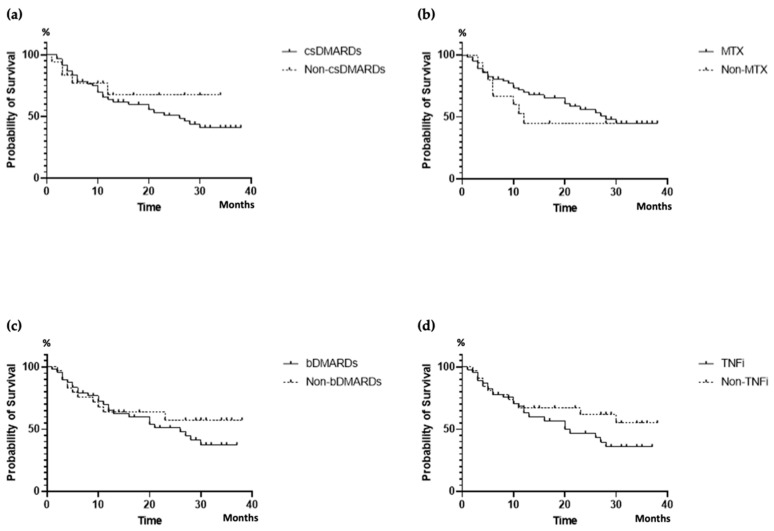
In addition, the DRR did not seem to be influenced by previous therapies, including csDMARDs (p = 0.504), methotrexate (p = 0.396), bDMARDs (p = 0.474), and previous TNFi (p = 0.247) (Figure 4). The number of previous bDMARDs/tsDMARDs was found to be correlated with patients’ age (r = 0.310, p = 0.005) and disease duration (r = 0.265, p value 0.018), while it did not appear to affect the duration (r = 0.106, p = 0.349) or discontinuation (r = 0.042, p = 0.896) of ixekizumab therapy.
Figure 4.
DRR of ixekizumab according to previous therapies: csDMARDs (a), MTX (b), bDMARDs (c), TNFi (d). csDMARDs, conventional synthetic Disease-Modifying Antirheumatic Drugs; MTX, methotrexate; bDMARDs, biologic Disease-Modifying Antirheumatic Drugs; TNFi, tumor necrosis factor inhibitor; DRR, drug retention rate.
When conducting multivariate explorative analyses to evaluate the possible predictive role of selected baseline clinical variables in the likelihood of ixekizumab discontinuation, none of these variables reached statistical significance (Table 2). Disease duration and the presence of HLA-B27 were not found to be predictive of ixekizumab discontinuation. Similarly, patient clinical characteristics (i.e., comorbidities, obesity, axial disease, and skin involvement) did not appear to influence drug discontinuation. In addition, the prior therapies with csDMARDs and bDMARDs were not identified as predictors of ixekizumab discontinuation.
Table 2.
Baseline clinical predictors of ixekizumab discontinuation through multivariate analysis.
| Clinical Variables | OR | 95%CI | p Value |
|---|---|---|---|
| Discontinuation of Ixekizumab | |||
| Multivariate analysis | |||
| Age | 0.99 | 0.97–1.03 | 0.980 |
| Male Sex | 1.21 | 0.60–2.27 | 0.591 |
| Disease duration ≤ 2 years | 1.51 | 0.76–2.99 | 0.235 |
| HLA-B27 | 2.72 | 0.90–8.23 | 0.076 |
| Multivariate analysis | |||
| Age | 0.99 | 0.96–1.02 | 0.991 |
| Male Sex | 1.42 | 0.64–3.16 | 0.386 |
| Comorbidity | 1.10 | 0.47–2.57 | 0.825 |
| Obesity | 0.78 | 0.37–1.64 | 0.511 |
| Multivariate analysis | |||
| Age | 1.01 | 0.98–1.03 | 0.922 |
| Male Sex | 1.09 | 0.53–2.25 | 0.811 |
| Axial Disease | 1.67 | 0.86–3.25 | 0.133 |
| Skin involvement | 0.89 | 0.38–2.07 | 0.791 |
| Multivariate analysis | |||
| Age | 0.99 | 0.97–1.03 | 0.989 |
| Male Sex | 1.17 | 0.57–2.43 | 0.664 |
| Previous csDMARDs | 1.26 | 0.49–3.28 | 0.630 |
| Previous bDMARDs | 1.07 | 0.52–2.19 | 0.852 |
Footnotes: OR, odds ratio; CI, confidence interval; HLA, Human Leukocyte antigen; csDMARDs, conventional synthetic Disease Modifying Antirheumatic Drugs; bDMARDs, biologic Disease Modifying Antirheumatic Drugs.
3.2. Adverse Events
The most frequent AEs leading to the discontinuation of ixekizumab (Table S1) were skin reactions, including localized reactions at the injection site (four cases, 5.0%) or diffuse skin reactions (three cases, 3.75%). Three (3.75%) patients discontinued the treatment due to diarrhea, and one of these was thereafter diagnosed with microscopic colitis. This patient had previously presented with diarrhea and gastrointestinal intolerance to csDMARDs. Another patient received a concomitant diagnosis of lung malignancy just after the initiation of therapy, despite prior screening. Only one patient had to discontinue ixekizumab due to an infection (i.e., persistent oral candidiasis). Eight (10%) patients experienced SARS-CoV-2 infection, which was not severe in all cases. A single case of localized Herpes Zoster and 1 pyelonephritis was reported.
4. Discussion
The majority of real-world data in the literature focus on patients with PsO, while fewer studies concentrate on those affected by PsA [58].
In this study, we showed that ixekizumab entails a good DRR in a real-life PsA cohort, with a good safety profile.
Taking into account the complete follow-up period of our cohort, a 38-month cumulative DRR was seen in 43.8%, where discontinuation was due to both inefficacy and AEs, whereas in 62.6%, interruption was due to inefficacy only. These findings are consistent with previous real-life data in PsA patients treated with ixekizumab. Recently, Braña et al. observed a 12-month DRR of 65% in a retrospective monocentric cohort of 72 patients [44]; similarly, an analysis of administrative claims databases from the USA highlighted that 52.8% of patients maintained ixekizumab therapy for a 12 months follow-up period [59]. Glintborg et al., drawing from data across five Nordic biologics registries, outlined a 12-month DRR of 57–65% for 361 treatment courses [45]. Joven et al. instead highlighted a drug persistence rate of 68.5% at two years [43]. In a monocenter cohort study conducted in the UK involving spondyloarthritis patients undergoing therapy with the IL-17i ixekizumab and secukinumab, drug survival rates were found to be 69% at 12 months and 60% at 24 months [49]. Takami et al. reported a 10-year DRR of 50% for ixekizumab in a long-term follow-up study [50].
In the literature, the DRR of ixekizumab has been found to be comparable to that of other biologics, with the exception of a higher DRR compared to infliximab [42].
Our PsA patient cohort exhibited a high rate of obesity and several comorbidities, primarily cardio-metabolic, which aligns with previous research findings [40,43,60]. Nevertheless, when analyzing factors that may influence the DRR of ixekizumab, it became evident that obesity had no significant effect, as previously noted in the literature [43,44]. Similarly, in our study, the presence of comorbidities and smoking habits, as previously documented by Braña et al., did not show any significant influence on the DRR of ixekizumab [44].
All our patients presented with peripheral involvement. Interestingly, axial involvement appeared to influence the DRR with a negative, albeit non-significant, trend, whereas this was not observed when considering skin involvement. It is necessary, nevertheless, to confirm this trend on larger cohorts, as the evaluation of these factors is crucial when tailoring PsA patients’ treatment, given their different phenotypes and multiple comorbidities [60].
Moreover, we highlighted a positive, but not statistically significant, trend for a higher DRR in patients with a disease duration shorter than 2 years. Braña et al. noted, however, that disease duration did not influence drug persistence [44].
The majority of our patients (70.1%) had encountered prior treatment failure with at least one bDMARD/tsDMARD, and 30.1% had experienced multiple treatment failures. Moreover, 15% had already been treated with an IL-17i. However, prior treatments with csDMARDs, including methotrexate, bDMARD/tsDMARD, or even a number of previous bDMARD/tsDMARD treatments, did not exert a significant impact on the DRR. Similarly, in the PRO-STIP study, it was observed that the number of previous DMARDs did not affect the drug persistence [43]. Braña et al. noted that previous therapies with bDMARDs did not influence drug persistence, whereas the prior use of methotrexate, in contrast with our study, was linked to a higher ixekizumab discontinuation [44]. Weddell et al. reported additionally comparable drug survival rates in PsA patients treated with IL-17 inhibitors, regardless of whether they were bDMARD-naïve or had prior exposure to bDMARDs [49].
These characteristics were analyzed to create multivariate analyses aimed at identifying factors that might affect DRR. However, it seems that even when using these models, they do not appear to predict improved DRR.
In our cohort of patients characterized with multiple comorbidities, many of whom had experienced treatment failure with second-line therapies, ixekizumab furthermore exhibited a favorable safety profile.
The discontinuation due to AEs occurred in 15.0% of patients, a higher percentage compared to the literature [58]. However, it is important to note that the AEs were not severe. Indeed, the most common AEs that resulted in the discontinuation of treatment were localized or diffuse skin reactions, which, however, were not severe and were in line with the expectations, as they had been already previously described in previous randomized controlled trials and real life data (SPIRIT-P1, SPIRIT-P2, SPIRIT-P3, and SPIRIT-H2H) [14,15,17,58,61,62].
Notably, our study revealed no severe infections. Similarly, Bastard et al. described serious infections in only 2.9% of the 344 patients treated with ixekizumab [52]. No severe infections were detected even among patients who were tested positive for SARS-CoV-2. Also, this finding aligns with the existing literature, which does not exhibit an increased risk of SARS-CoV-2-associated hospitalization or mortality in patients undergoing treatment with IL-17i [63]. Only one patient had to discontinue treatment due to an infectious disease, specifically persistent oral candidiasis. Chronic fungal diseases were also described in the study of Weddell et al. [49]. Localized candida infections were reported in a low proportion of patients treated with ixekizumab, likely related to the function of IL-17A in defense against these pathogens [44,62]. An analysis of administrative claims in the USA revealed that the risk of serious infection in patients treated with IL-17i appears to be similar to that in patients treated with TNFi [41].
Within our cohort, one patient exposed to ixekizumab developed microscopic colitis. Cases of microscopic colitis occurring during IL-17i therapy have already been documented in the worldwide pharmacovigilance database [64], and IL-17i were previously associated with increased rates of AEs and the exacerbation of symptoms related to Crohn’s disease [65,66]. A rate of new cases of Crohn’s disease and ulcerative colitis of less than 1% were documented in PsO patients [67]. As seen from a pooled analysis of the open-label period of SPIRIT-P1, SPIRIT-P2, and SPIRIT-P3, the rate of chronic inflammatory bowel diseases among PsA patients treated with ixekizumab was 0.2% [68]. Hence, although the evidence suggests a low rate of new onset of inflammatory bowel disease among patients exposed to ixekizumab, careful screening seems relevant especially in presence of symptoms suspicious for IBD. Considering real-life data, comparable findings were presented by Braña et al., where the predominant AEs were cutaneous and gastrointestinal, including a new diagnosis of Crohn’s disease [44].
Lastly, a patient received a diagnosis of lung cancer shortly after beginning therapy, despite screening performed prior to prescription with a chest X-ray. However, the diagnosis occurred soon after the induction period, so a direct link to ixekizumab administration seems unlikely.
Our study has certain limitations, primarily due to its retrospective monocentric design, which led to a lack of data concerning minor AEs, especially those that did not result in treatment discontinuation, as well as in the assessment of disease activity.
On the other hand, based on the current literature in the field, our cohort is among the largest and most well-characterized monocentric real-world cohorts of patients on ixekizumab so far, thereby offering valuable real-life insights on ixekizumab use in PsA patients and providing important data about DRR and safety, particularly among patients with multiple comorbidities.
In conclusion, in our study, ixekizumab revealed a good DRR and safety profile, even among patients with multiple treatment failures, comorbidities, and obesity, which are common in PsA patients. The prior use of methotrexate did not affect DRR in our study, in contrast to previous findings [44]. Additionally, we observed comparable efficacy in both peripheral and axial phenotypes, despite a negative trend in the latter. Moreover, our data suggest that initiating ixekizumab earlier may provide additional benefits. However, addressing these points will require larger sample sizes and further studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm14070716/s1. Table S1: Adverse events that led to discontinuation.
Author Contributions
Conceptualization, E.B., P.R. and A.I.; methodology, E.B. and P.R.; software, P.R.; formal analysis, E.B., P.R. and A.I.; investigation, all; data curation, E.B., P.R., D.D., G.C., V.D., M.G. (Marinella Gammino), M.G. (Mariele Gatto), V.G., C.L., E.M. and M.S.; writing—original draft preparation, E.B. and A.I.; writing—review and editing, all; visualization, E.B. and A.I.; supervision, E.B. and A.I.; project administration, A.I. All authors have read and agreed to the published version of the manuscript. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Interagency Territorial Ethics Committee A.O.U. Città della Salute e della Scienza, protocol code No 139/2023, date of approval 21 April 2023.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, and further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare the following conflicts of interest. E.B.: Honoraria: BMS, Novartis. P.R.: Honoraria: Abbvie, BMS, Ely Lilly, Janssen Novartis, Sobi; educational grants: BMS; research support: Pfizer. D.D.: Honoraria: Janssen. G.C.: advisory boards: Novartis, AbbVie, Alfa-sigma; speakers’ bureau: Janssen, Galapagos, Eli-Lilly, BMS. V.D.: no conflict of interest. M. Gammino: no conflict of interest. M. Gatto: Honoraria, speakers bureau from: GSK, Astrazeneca, Janssen. V.G.: no conflict of interest. C.L.: Honoraria, advisory boards, speakers’ bureau, educational grants, research support from: BMS, Pfizer, AbbVie, Janssen, Eli-Lilly. E.M.: no conflict of interest; M.S.: no conflict of interest. A.I.: Honoraria, advisory boards, speakers’ bureau, educational grants, research support from: AbbVie, Alfa-sigma, BMS, Celgene, Celltrion, Eli-Lilly, Galapagos, Gilead, MSD, Janssen, Novartis, Pfizer, Sanofi Genzyme, SOBI.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Rida M.A., Chandran V. Challenges in the Clinical Diagnosis of Psoriatic Arthritis. Clin. Immunol. 2020;214:108390. doi: 10.1016/j.clim.2020.108390. [DOI] [PubMed] [Google Scholar]
- 2.Haroon M., Kirby B., FitzGerald O. High Prevalence of Psoriatic Arthritis in Patients with Severe Psoriasis with Suboptimal Performance of Screening Questionnaires. Ann. Rheum. Dis. 2013;72:736–740. doi: 10.1136/annrheumdis-2012-201706. [DOI] [PubMed] [Google Scholar]
- 3.Moshrif A., Mosallam A., Mohamed E.E.M., Gouda W., Doma M. Subclinical Enthesopathy in Patients with Psoriasis and Its Association with Other Disease Parameters: A Power Doppler Ultrasonographic Study. Eur. J. Rheumatol. 2017;4:24–28. doi: 10.5152/eurjrheum.2017.16049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naredo E., Moller I., De Miguel E., Batlle-Gualda E., Acebes C., Brito E., Mayordomo L., Moragues C., Uson J., De Agustin J.J., et al. High Prevalence of Ultrasonographic Synovitis and Enthesopathy in Patients with Psoriasis without Psoriatic Arthritis: A Prospective Case-Control Study. Rheumatology. 2011;50:1838–1848. doi: 10.1093/rheumatology/ker078. [DOI] [PubMed] [Google Scholar]
- 5.Zuliani F., Zabotti A., Errichetti E., Tinazzi I., Zanetti A., Carrara G., Quartuccio L., Sacco S., Giovannini I., Stinco G., et al. Ultrasonographic Detection of Subclinical Enthesitis and Synovitis: A Possible Stratification of Psoriatic Patients without Clinical Musculoskeletal Involvement. Clin. Exp. Rheumatol. 2019;37:593–599. [PubMed] [Google Scholar]
- 6.Ribeiro A.L., Eder L. From Psoriasis to Psoriatic Arthritis: Ultrasound Insights Connecting Psoriasis with Subclinical Musculoskeletal Inflammation and the Path to Psoriatic Arthritis. Curr. Rheumatol. Rep. 2024;26:235–247. doi: 10.1007/s11926-024-01146-9. [DOI] [PubMed] [Google Scholar]
- 7.Kirkham B., de Vlam K., Li W., Boggs R., Mallbris L., Nab H.W., Tarallo M. Early Treatment of Psoriatic Arthritis Is Associated with Improved Patient-Reported Outcomes: Findings from the Etanercept PRESTA Trial. Clin. Exp. Rheumatol. 2015;33:11–19. [PubMed] [Google Scholar]
- 8.Kampylafka E., Simon D., d’Oliveira I., Linz C., Lerchen V., Englbrecht M., Rech J., Kleyer A., Sticherling M., Schett G., et al. Disease Interception with Interleukin-17 Inhibition in High-Risk Psoriasis Patients with Subclinical Joint Inflammation—Data from the Prospective IVEPSA Study. Arthritis Res. Ther. 2019;21:178. doi: 10.1186/s13075-019-1957-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panagiotopoulos A., Fragoulis G.E. Comorbidities in Psoriatic Arthritis: A Narrative Review. Clin. Ther. 2023;45:177–189. doi: 10.1016/j.clinthera.2023.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Schett G., Rahman P., Ritchlin C., McInnes I.B., Elewaut D., Scher J.U. Psoriatic Arthritis from a Mechanistic Perspective. Nat. Rev. Rheumatol. 2022;18:311–325. doi: 10.1038/s41584-022-00776-6. [DOI] [PubMed] [Google Scholar]
- 11.Blauvelt A., Chiricozzi A. The Immunologic Role of IL-17 in Psoriasis and Psoriatic Arthritis Pathogenesis. Clin. Rev. Allergy Immunol. 2018;55:379–390. doi: 10.1007/s12016-018-8702-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu L., Kikly K., Lu J., Allan B., Tang Y., Tetreault J., Chow C.-K., Barmettler B., Nelson J., Bina H., et al. Generation and Characterization of Ixekizumab, a Humanized Monoclonal Antibody That Neutralizes Interleukin-17A. J. Inflamm. Res. 2016;39:39–50. doi: 10.2147/JIR.S100940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.European Medicines Agency [Internet] Taltz: EPAR—Product Information. [(accessed on 30 June 2024)]; Available online: https://www.ema.europa.eu/en/documents/product-information/taltz-epar-product-information_en.pdf.
- 14.Mease P.J., van der Heijde D., Ritchlin C.T., Okada M., Cuchacovich R.S., Shuler C.L., Lin C.-Y., Braun D.K., Lee C.H., Gladman D.D. Ixekizumab, an Interleukin-17A Specific Monoclonal Antibody, for the Treatment of Biologic-Naive Patients with Active Psoriatic Arthritis: Results from the 24-Week Randomised, Double-Blind, Placebo-Controlled and Active (Adalimumab)-Controlled Period of the Phase III Trial SPIRIT-P1. Ann. Rheum. Dis. 2017;76:79–87. doi: 10.1136/annrheumdis-2016-209709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mease P.J., Smolen J.S., Behrens F., Nash P., Liu Leage S., Li L., Tahir H., Gooderham M., Krishnan E., Liu-Seifert H., et al. A Head-to-Head Comparison of the Efficacy and Safety of Ixekizumab and Adalimumab in Biological-Naïve Patients with Active Psoriatic Arthritis: 24-Week Results of a Randomised, Open-Label, Blinded-Assessor Trial. Ann. Rheum. Dis. 2020;79:123–131. doi: 10.1136/annrheumdis-2019-215386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smolen J.S., Mease P., Tahir H., Schulze-Koops H., De La Torre I., Li L., Hojnik M., Sapin C., Okada M., Caporali R., et al. Multicentre, Randomised, Open-Label, Parallel-Group Study Evaluating the Efficacy and Safety of Ixekizumab versus Adalimumab in Patients with Psoriatic Arthritis Naïve to Biological Disease-Modifying Antirheumatic Drug: Final Results by Week 52. Ann. Rheum. Dis. 2020;79:1310–1319. doi: 10.1136/annrheumdis-2020-217372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nash P., Kirkham B., Okada M., Rahman P., Combe B., Burmester G.-R., Adams D.H., Kerr L., Lee C., Shuler C.L., et al. Ixekizumab for the Treatment of Patients with Active Psoriatic Arthritis and an Inadequate Response to Tumour Necrosis Factor Inhibitors: Results from the 24-Week Randomised, Double-Blind, Placebo-Controlled Period of the SPIRIT-P2 Phase 3 Trial. Lancet. 2017;389:2317–2327. doi: 10.1016/S0140-6736(17)31429-0. [DOI] [PubMed] [Google Scholar]
- 18.Genovese M.C., Combe B., Kremer J.M., Tsai T.-F., Behrens F., Adams D.H., Lee C., Kerr L., Nash P. Safety and Efficacy of Ixekizumab in Patients with PsA and Previous Inadequate Response to TNF Inhibitors: Week 52 Results from SPIRIT-P2. Rheumatology. 2018;57:2001–2011. doi: 10.1093/rheumatology/key182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kavanaugh A., Marzo-Ortega H., Vender R., Wei C.-C., Birt J., Adams D.H., Benichou O., Lin C.-Y., Nash P. Ixekizumab Improves Patient-Reported Outcomes in Patients with Active Psoriatic Arthritis and Inadequate Response to Tumour Necrosis Factor Inhibitors: SPIRIT-P2 Results to 52 Weeks. Clin. Exp. Rheumatol. 2019;37:566–574. [PubMed] [Google Scholar]
- 20.Gordon K.B., Blauvelt A., Papp K.A., Langley R.G., Luger T., Ohtsuki M., Reich K., Amato D., Ball S.G., Braun D.K., et al. Phase 3 Trials of Ixekizumab in Moderate-to-Severe Plaque Psoriasis. N. Engl. J. Med. 2016;375:345–356. doi: 10.1056/NEJMoa1512711. [DOI] [PubMed] [Google Scholar]
- 21.Strober B., Leonardi C., Papp K.A., Mrowietz U., Ohtsuki M., Bissonnette R., Ferris L.K., Paul C., Lebwohl M., Braun D.K., et al. Short- and Long-Term Safety Outcomes with Ixekizumab from 7 Clinical Trials in Psoriasis: Etanercept Comparisons and Integrated Data. J. Am. Acad. Dermatol. 2017;76:432–440. doi: 10.1016/j.jaad.2016.09.026. [DOI] [PubMed] [Google Scholar]
- 22.Calianno G., Esposito M., Fidanza R., Palmieri M., Fargnoli M.C. Ixekizumab Improves Disease Severity, Clinical Symptoms and Quality of Life in Patients with Genital Psoriasis: A 24-week Real-life Experience. Dermatol. Ther. 2021;34:e14993. doi: 10.1111/dth.14993. [DOI] [PubMed] [Google Scholar]
- 23.Magdaleno-Tapial J., Carmena-Ramón R., Valenzuela-Oñate C., Ortiz-Salvador J.M., Sabater-Abad J., Hernández-Bel P., Gimeno-Carpio E., Sánchez-Carazo J.L., Pérez-Ferriols A. Eficacia y seguridad de ixekizumab en la práctica clínica habitual: Estudio retrospectivo bicéntrico. Actas Dermo-Sifiliográficas. 2019;110:585–589. doi: 10.1016/j.ad.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Gottlieb A.B., Burge R., Malatestinic W.N., Zhu B., Zhao Y., McCormack J., Kimel M., Merola J.F. Ixekizumab Real-World Effectiveness at 24 Weeks in Patients with Psoriasis: Data from the United States Taltz Customer Support Program. Dermatol. Ther. 2023;13:1831–1846. doi: 10.1007/s13555-023-00969-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gulliver W., Gooderham M.J., Zhu B., Jossart C., Montmayeur S., Burge R., Reed C. Treatment Persistence of Ixekizumab in Adults with Moderate-to-Severe Plaque Psoriasis Participating in the Canadian Patient Support Program. Dermatol. Ther. 2023;13:235–244. doi: 10.1007/s13555-022-00853-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caldarola G., Chiricozzi A., Megna M., Dapavo P., Giunta A., Burlando M., Malagoli P., Dini V., Mariani M., Fabbrocini G., et al. Real-Life Experience with Ixekizumab in Plaque Psoriasis: A Multi-Center, Retrospective, 3-Year Study. Expert Opin. Biol. Ther. 2023;23:365–370. doi: 10.1080/14712598.2023.2193288. [DOI] [PubMed] [Google Scholar]
- 27.Armstrong A., González-Cantero A., Khattri S., Muzy G., Malatestinic W.N., Lampropoulou A., Feely M., See S.K., Mert C., Blauvelt A. Comparing Achievement of National Psoriasis Foundation Treatment Targets among Patients with Plaque Psoriasis Treated with Ixekizumab versus Other Biologics in Clinical and Real-World Studies. Dermatol. Ther. 2024;14:933–952. doi: 10.1007/s13555-024-01136-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schots L., Soenen R., Blanquart B., Thomas D., Lambert J. Blocking Interleukin-17 in Psoriasis: Real-world Experience from the PsoPlus Cohort. Acad. Dermatol. Venereol. 2023;37:698–710. doi: 10.1111/jdv.18827. [DOI] [PubMed] [Google Scholar]
- 29.Ying L., Suyun J., Yanhua L., Yunsheng L., Li D., Lin D., Chengzhi L., Bingjiang L., Furen Z., Wendi S., et al. Safety and Efficacy of Ixekizumab in Chinese Adults with Moderate-to-Severe Plaque Psoriasis: A Prospective, Multicenter, Observational Study. Adv. Ther. 2023;40:5464–5474. doi: 10.1007/s12325-023-02672-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gargiulo L., Ibba L., Malagoli P., Balato A., Bardazzi F., Burlando M., Carrera C.G., Damiani G., Dapavo P., Dini V., et al. Drug Survival of IL-12/23, IL-17 and IL-23 Inhibitors for Moderate-to-Severe Plaque Psoriasis: A Retrospective Multicenter Real-World Experience on 5932 Treatment Courses—IL PSO (Italian Landscape Psoriasis) Front. Immunol. 2023;14:1341708. doi: 10.3389/fimmu.2023.1341708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiricozzi A., Megna M., Giunta A., Carrera C.G., Dapavo P., Balato A., Malagoli P., Mazzoccoli S., Parodi A., Sabatino S., et al. Ixekizumab Is Effective in the Long-Term Management in Moderate-to-Severe Plaque Psoriasis: Results from an Italian Retrospective Cohort Study (the LOTIXE Study) J. Dermatol. Treat. 2023;34:2246606. doi: 10.1080/09546634.2023.2246606. [DOI] [PubMed] [Google Scholar]
- 32.Fitzgerald T., Zhdanava M., Pilon D., Shah A., Hilts A., Lefebvre P., Feldman S.R. Long-Term Psoriasis Control with Guselkumab, Adalimumab, Secukinumab, or Ixekizumab in the USA. Dermatol. Ther. 2023;13:1053–1068. doi: 10.1007/s13555-023-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mastorino L., Dapavo P., Burzi L., Rosset F., Giunipero di Corteranzo I., Leo F., Verrone A., Stroppiana E., Ortoncelli M., Ribero S., et al. Drug Survival, Effectiveness and Safety of Ixekizumab for Moderate-to-Severe Psoriasis up to 5 Years. J. Eur. Acad. Dermatol. Venereol. 2024;38:568–575. doi: 10.1111/jdv.19682. [DOI] [PubMed] [Google Scholar]
- 34.Wang C., Torisu-Itakura H., Hanada T., Matsuo T., Cai Z., Osaga S., Aranishi T. Treatment Persistence of Interleukin-17 Inhibitor Class Drugs among Patients with Psoriasis in Japan: A Retrospective Database Study. J. Dermatol. Treat. 2023;34:2229465. doi: 10.1080/09546634.2023.2229465. [DOI] [PubMed] [Google Scholar]
- 35.Burlando M., Salvi I., Castelli R., Herzum A., Cozzani E., Parodi A. Long-Term Clinical Efficacy and Safety of Ixekizumab for Psoriatic Patients: A Single-Center Experience. Eur. Rev. Med. Pharmacol. Sci. 2023;27:4060–4064. doi: 10.26355/eurrev_202305_32312. [DOI] [PubMed] [Google Scholar]
- 36.Pinter A., Costanzo A., Khattri S., Smith S.D., Carrascosa J.M., Tada Y., Riedl E., Reich A., Brnabic A., Haustrup N., et al. Comparative Effectiveness and Durability of Biologics in Clinical Practice: Month 12 Outcomes from the International, Observational Psoriasis Study of Health Outcomes (PSoHO) Dermatol. Ther. 2023;14:1479–1493. doi: 10.1007/s13555-023-01086-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Travaglini M., Maul J.-T., Kors C., Zaheri S., Gerwien J., Müller M., Brnabic A., Sabatino S., Schuster C., Tsai T.-F. Effectiveness of Biologics, Patient-Reported Outcomes, and Clinical Photography in a Subset of Patients with Moderate-to-Severe Psoriasis: Week 12 Results from the Psoriasis Study of Health Outcomes (PSoHO) Clin. Cosmet. Investig. Dermatol. 2023;16:2971–2983. doi: 10.2147/CCID.S426972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ting S., Lowe P., Smith A., Fernández-Peñas P. Drug Survival of Biologics in Psoriasis: An Australian Multicentre Retrospective Study. Australas. J. Dermatol. 2024;65:350–357. doi: 10.1111/ajd.14254. [DOI] [PubMed] [Google Scholar]
- 39.Zhdanava M., Fitzgerald T., Pilon D., Teneralli R.E., Shah A., Diaz L., Lefebvre P., Feldman S.R. Comparative Analysis of Persistence and Remission with Guselkumab versus Secukinumab and Ixekizumab in the United States. J. Dermatol. Treat. 2024;35:2349658. doi: 10.1080/09546634.2024.2349658. [DOI] [PubMed] [Google Scholar]
- 40.Manfreda V., Chimenti M.S., Canofari C., Esposito M., Perricone R., Bianchi L., Giunta A. Efficacy and Safety of Ixekizumab in Psoriatic Arthritis: A Retrospective, Single-Centre, Observational Study in a Real-Life Clinical Setting. Clin. Exp. Rheumatol. 2020;38:581–582. [PubMed] [Google Scholar]
- 41.Li X., Andersen K.M., Chang H.-Y., Curtis J.R., Alexander G.C. Comparative Risk of Serious Infections among Real-World Users of Biologics for Psoriasis or Psoriatic Arthritis. Ann. Rheum. Dis. 2020;79:285–291. doi: 10.1136/annrheumdis-2019-216102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egeberg A., Rosenø N.A.L., Aagaard D., Lørup E.H., Nielsen M.-L., Nymand L., Kristensen L.E., Thyssen J.P., Thomsen S.F., Cordtz R.L., et al. Drug Survival of Biologics and Novel Immunomodulators for Rheumatoid Arthritis, Axial Spondyloarthritis, Psoriatic Arthritis, and Psoriasis—A Nationwide Cohort Study from the DANBIO and DERMBIO Registries. Semin. Arthritis Rheum. 2022;53:151979. doi: 10.1016/j.semarthrit.2022.151979. [DOI] [PubMed] [Google Scholar]
- 43.Joven B., Hernández Sánchez R., Pérez-Pampín E., Aragón Díez Á., Almodóvar R., Martínez-Ferrer Á., Belzunegui J., Rubio E., Díaz-Cerezo S., Moyano S., et al. Persistence and Use of Ixekizumab in Patients with Psoriatic Arthritis in Real-World Practice in Spain. The PRO-STIP Study. Rheumatol. Ther. 2023;10:1319–1333. doi: 10.1007/s40744-023-00584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Braña I., Pardo E., Burger S., González Del Pozo P., Alperi M., Queiro R. Treatment Retention and Safety of Ixekizumab in Psoriatic Arthritis: A Real Life Single-Center Experience. J. Clin. Med. 2023;12:467. doi: 10.3390/jcm12020467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Glintborg B., Di Giuseppe D., Wallman J.K., Nordström D.C., Gudbjornsson B., Hetland M.L., Askling J., Grondal G., Sokka T., Provan S.A., et al. Uptake and Effectiveness of Newer Biologic and Targeted Synthetic Disease-Modifying Antirheumatic Drugs in Psoriatic Arthritis: Results from Five Nordic Biologics Registries. Ann. Rheum. Dis. 2023;82:820–828. doi: 10.1136/ard-2022-223650. [DOI] [PubMed] [Google Scholar]
- 46.Berman J., Furer V., Berman M., Isakov O., Zisman D., Haddad A., Elkayam O. Treatment with Ixekizumab Following Secukinumab Failure in Patients with Psoriatic Arthritis: Real-Life Experience from a Resistant Population. Biol. Targets Ther. 2021;15:463–470. doi: 10.2147/BTT.S326792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tillett W., Birt J., Cavanaugh C., Jung Y., Vadhariya A., Ross S., Paulus J., Lubrano E. Changes in Musculoskeletal Disease Activity and Patient-Reported Outcomes in Patients with Psoriatic Arthritis Treated with Ixekizumab: Results from a Real-World US Cohort. Front. Med. 2023;10:1184028. doi: 10.3389/fmed.2023.1184028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rohekar S., Vadhariya A., Ross S., Malatestinic W., Janos B., Massey N., Hughes M., Weatherby S., Birt J., Sebba A. Real-World Treatment Patterns, Clinical Outcomes, and Symptom Burden in Patients with Psoriatic Arthritis Prescribed Ixekizumab in the United States. ACR Open Rheumatol. 2024:acr2.11676. doi: 10.1002/acr2.11676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weddell J., Din N.R.A., Harrison S.R., Michelena X., McGonagle D., Barr A., Vandevelde C., Freeston J., Marzo-Ortega H. Real-World Experience of IL-17Ai Drug Survival in a Large Cohort of Axial Spondyloarthritis and Psoriatic Arthritis. Rheumatol. Adv. Pract. 2024;8:rkae018. doi: 10.1093/rap/rkae018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Takami K., Tsuji S., Sato S., Akaji K., Yamashita C., Hiroumi S., Konaka H., Hayashi M., Higashiyama M. Long-Term Retention Rates of Anti-Tumour Necrosis Factor and Anti-Interleukin-17 Antibodies for Patients with Psoriatic Arthritis. Mod. Rheumatol. 2023:road111. doi: 10.1093/mr/road111. [DOI] [PubMed] [Google Scholar]
- 51.Panagiotopoulos A., Koutsianas C., Kougkas N., Moschou D., Bournia V.-K., Gazi S., Tektonidou M.G., Vassilopoulos D., Sfikakis P.P., Fragoulis G.E. Ixekizumab Therapy Following Secukinumab Inadequate Response in Psoriatic Arthritis: A Case Series Focusing on Axial Disease. Rheumatol. Int. 2023;43:969–973. doi: 10.1007/s00296-023-05289-3. [DOI] [PubMed] [Google Scholar]
- 52.Bastard L., Claudepierre P., Penso L., Sbidian E., Pina Vegas L. Risk of Serious Infection Associated with Different Classes of Targeted Therapies Used in Psoriatic Arthritis: A Nationwide Cohort Study from the French Health Insurance Database (SNDS) RMD Open. 2024;10:e003865. doi: 10.1136/rmdopen-2023-003865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barnish M., Turner S. The Value of Pragmatic and Observational Studies in Health Care and Public Health. Pragmatic Obs. Res. 2017;8:49–55. doi: 10.2147/POR.S137701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fortin M. Randomized Controlled Trials: Do They Have External Validity for Patients With Multiple Comorbidities? Ann. Fam. Med. 2006;4:104–108. doi: 10.1370/afm.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taylor W., Gladman D., Helliwell P., Marchesoni A., Mease P., Mielants H., CASPAR Study Group Classification Criteria for Psoriatic Arthritis: Development of New Criteria from a Large International Study. Arthritis Rheum. 2006;54:2665–2673. doi: 10.1002/art.21972. [DOI] [PubMed] [Google Scholar]
- 56.Zabotti A., De Marco G., Gossec L., Baraliakos X., Aletaha D., Iagnocco A., Gisondi P., Balint P.V., Bertheussen H., Boehncke W.-H., et al. EULAR Points to Consider for the Definition of Clinical and Imaging Features Suspicious for Progression from Psoriasis to Psoriatic Arthritis. Ann. Rheum. Dis. 2023;82:1162–1170. doi: 10.1136/ard-2023-224148. [DOI] [PubMed] [Google Scholar]
- 57.Mekhail C., Chouk M., Prati C., Wendling D., Verhoeven F. Prognostic Factors of Good Response to DMARDs in Psoriatic Arthritis: A Narrative Review. Expert Rev. Clin. Pharmacol. 2020;13:505–519. doi: 10.1080/17512433.2020.1758556. [DOI] [PubMed] [Google Scholar]
- 58.Reich A., Reed C., Schuster C., Robert C., Treuer T., Lubrano E. Real-World Evidence for Ixekizumab in the Treatment of Psoriasis and Psoriatic Arthritis: Literature Review 2016–2021. J. Dermatol. Treat. 2023;34:2160196. doi: 10.1080/09546634.2022.2160196. [DOI] [PubMed] [Google Scholar]
- 59.Murage M.J., Princic N., Park J., Malatestinic W., Zhu B., Atiya B., Kern S.A., Stenger K.B., Sprabery A.T., Ogdie A. Real-World Treatment Patterns and Healthcare Costs in Patients with Psoriatic Arthritis Treated with Ixekizumab: A Retrospective Study. ACR Open Rheumatol. 2021;3:879–887. doi: 10.1002/acr2.11347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta S., Syrimi Z., Hughes D.M., Zhao S.S. Comorbidities in Psoriatic Arthritis: A Systematic Review and Meta-Analysis. Rheumatol. Int. 2021;41:275–284. doi: 10.1007/s00296-020-04775-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coates L.C., Pillai S.G., Tahir H., Valter I., Chandran V., Kameda H., Okada M., Kerr L., Alves D., Park S.Y., et al. Withdrawing Ixekizumab in Patients With Psoriatic Arthritis Who Achieved Minimal Disease Activity: Results From a Randomized, Double-Blind Withdrawal Study. Arthritis Rheumatol. 2021;73:1663–1672. doi: 10.1002/art.41716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Deodhar A.A., Combe B., Accioly A.P., Bolce R., Zhu D., Gellett A.M., Sprabery A.T., Burmester G.-R.R. Safety of Ixekizumab in Patients with Psoriatic Arthritis: Data from Four Clinical Trials with over 2000 Patient-Years of Exposure. Ann. Rheum. Dis. 2022;81:944–950. doi: 10.1136/annrheumdis-2021-222027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kridin K., Schonmann Y., Solomon A., Damiani G., Tzur Bitan D., Onn E., Weinstein O., Cohen A.D. Risk of COVID-19 Infection, Hospitalization, and Mortality in Patients with Psoriasis Treated by Interleukin-17 Inhibitors. J. Dermatol. Treat. 2022;33:2014–2020. doi: 10.1080/09546634.2021.1905766. [DOI] [PubMed] [Google Scholar]
- 64.Petitpain N., D’Amico F., Yelehe-Okouma M., Jouzeau J., Netter P., Peyrin-Biroulet L., Gillet P. IL-17 Inhibitors and Inflammatory Bowel Diseases: A Postmarketing Study in Vigibase. Clin. Pharmacol. Ther. 2021;110:159–168. doi: 10.1002/cpt.2155. [DOI] [PubMed] [Google Scholar]
- 65.Hueber W., Sands B.E., Lewitzky S., Vandemeulebroecke M., Reinisch W., Higgins P.D.R., Wehkamp J., Feagan B.G., Yao M.D., Karczewski M., et al. Secukinumab, a Human Anti-IL-17A Monoclonal Antibody, for Moderate to Severe Crohn’s Disease: Unexpected Results of a Randomised, Double-Blind Placebo-Controlled Trial. Gut. 2012;61:1693–1700. doi: 10.1136/gutjnl-2011-301668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Targan S.R., Feagan B., Vermeire S., Panaccione R., Melmed G.Y., Landers C., Li D., Russell C., Newmark R., Zhang N., et al. A Randomized, Double-Blind, Placebo-Controlled Phase 2 Study of Brodalumab in Patients with Moderate-to-Severe Crohn’s Disease. Am. J. Gastroenterol. 2016;111:1599–1607. doi: 10.1038/ajg.2016.298. [DOI] [PubMed] [Google Scholar]
- 67.Reich K., Leonardi C., Langley R.G., Warren R.B., Bachelez H., Romiti R., Ohtsuki M., Xu W., Acharya N., Solotkin K., et al. Inflammatory Bowel Disease among Patients with Psoriasis Treated with Ixekizumab: A Presentation of Adjudicated Data from an Integrated Database of 7 Randomized Controlled and Uncontrolled Trials. J. Am. Acad. Dermatol. 2017;76:441–448. doi: 10.1016/j.jaad.2016.10.027. [DOI] [PubMed] [Google Scholar]
- 68.Mease P., Roussou E., Burmester G.-R., Goupille P., Gottlieb A., Moriarty S.R., Benichou O., Adams D.H., Xu W., Nash P. Safety of Ixekizumab in Patients with Psoriatic Arthritis: Results From a Pooled Analysis of Three Clinical Trials. Arthritis Care Res. 2019;71:367–378. doi: 10.1002/acr.23738. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, and further inquiries can be directed to the corresponding author.