Abstract
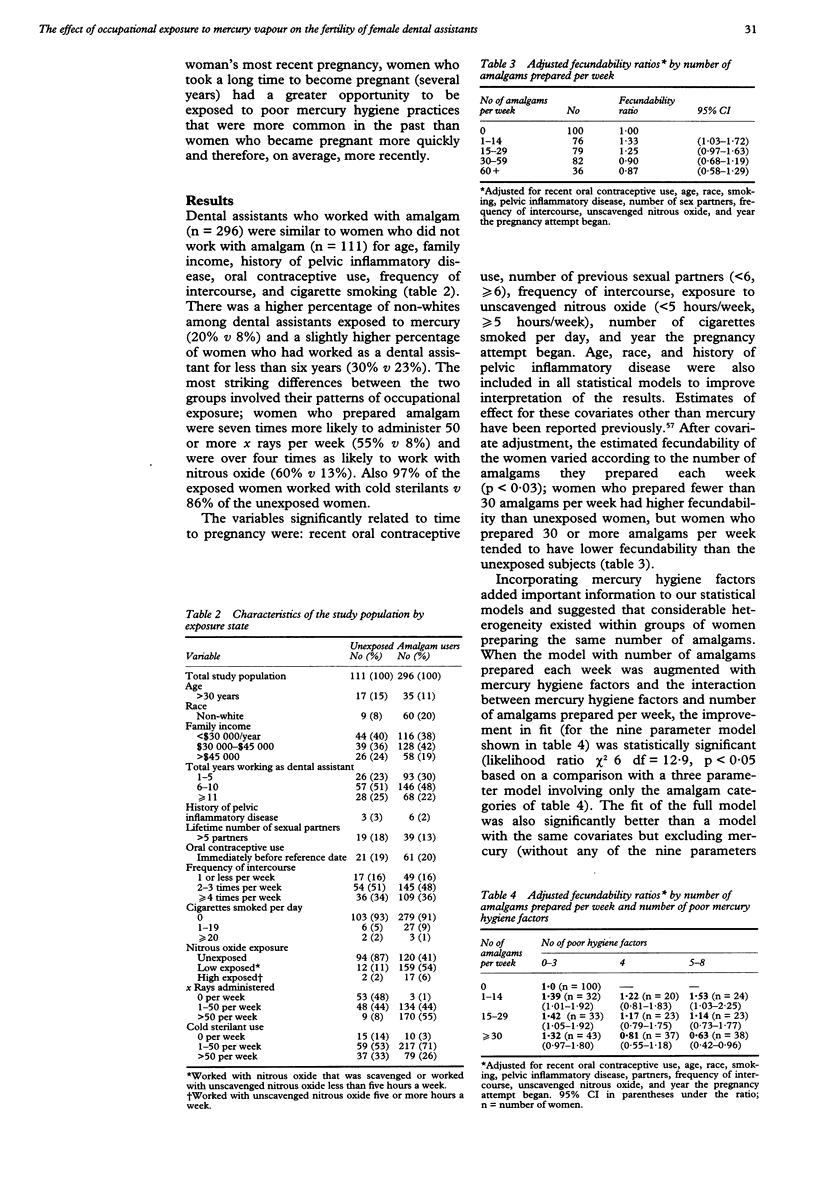
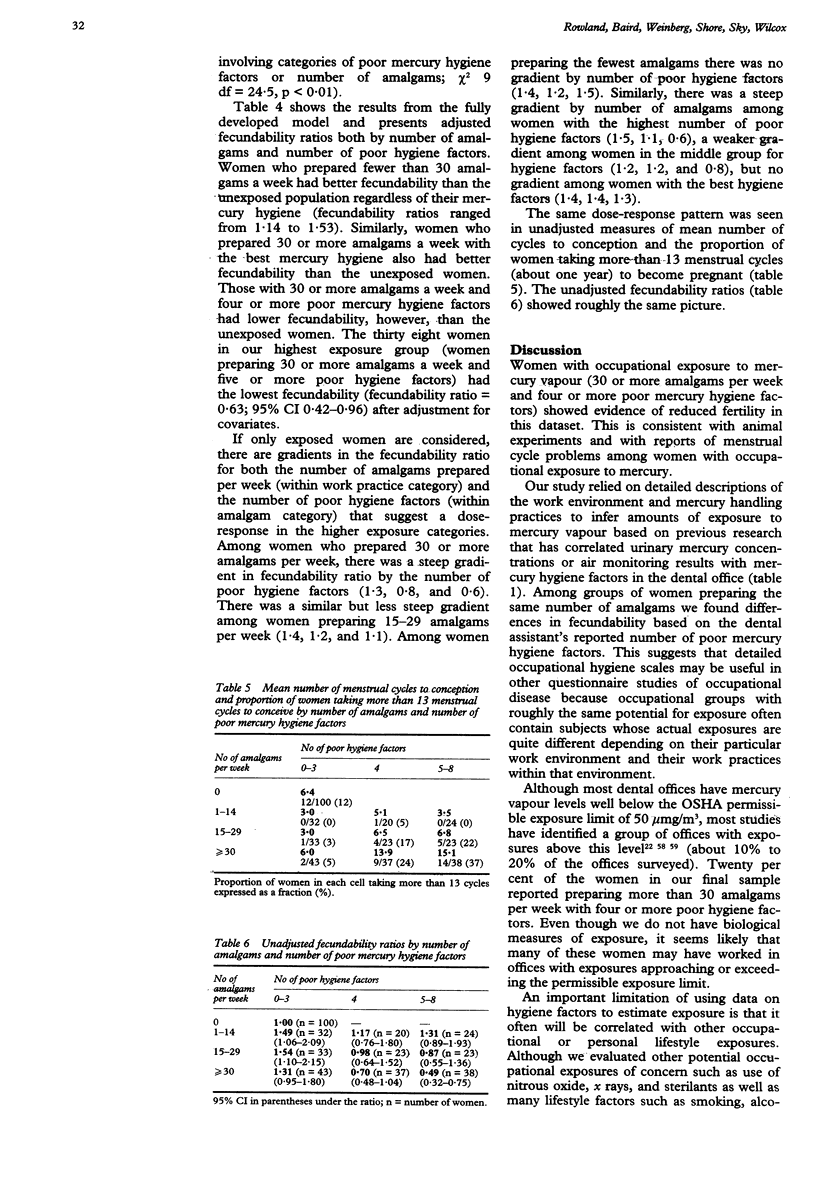
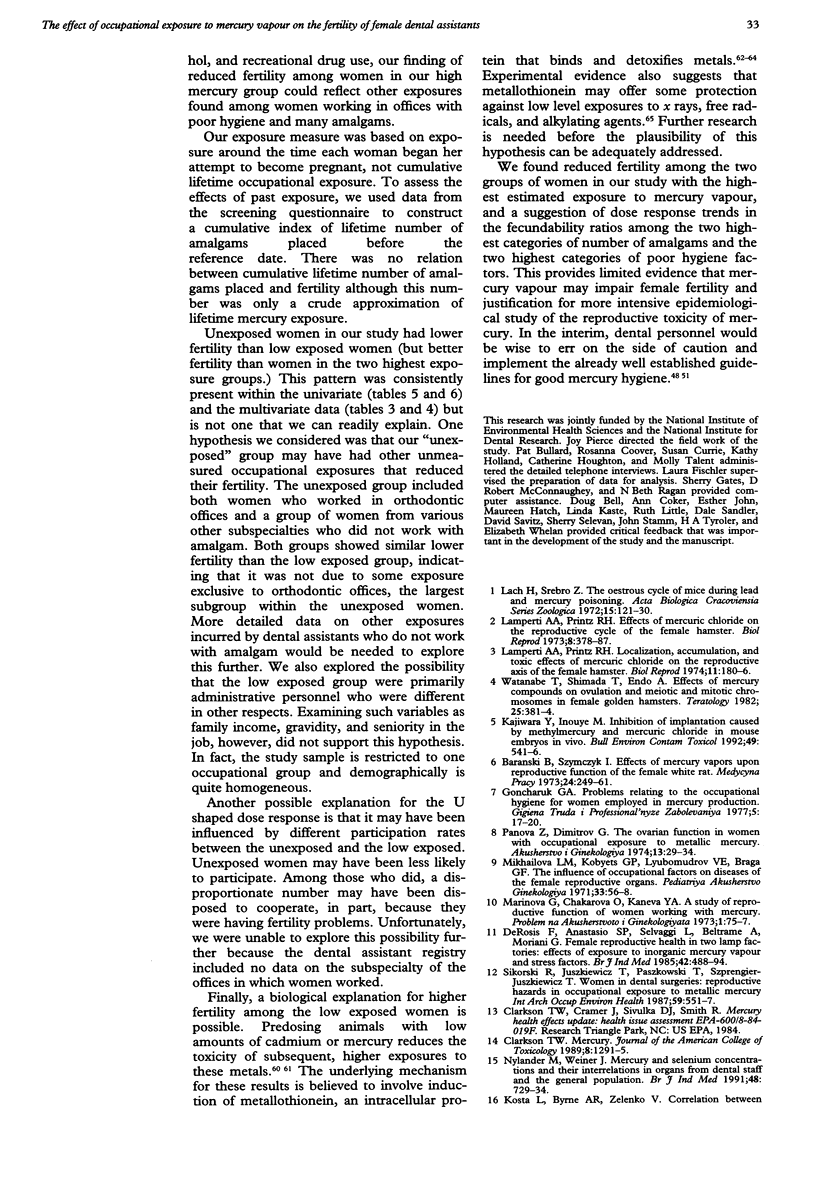
Exposure to mercury vapour or inorganic mercury compounds can impair fertility in laboratory animals. To study the effects of mercury vapour on fertility in women, eligibility questionnaires were sent to 7000 registered dental assistants in California. The final eligible sample of 418 women, who had become pregnant during the previous four years, were interviewed by telephone. Detailed information was collected on mercury handling practices and the number of menstrual cycles without contraception it had taken them to become pregnant. Dental assistants not working with amalgam served as unexposed controls. Women with high occupational exposure to mercury were less fertile than unexposed controls. The fecundability (probability of conception each menstrual cycle) of women who prepared 30 or more amalgams per week and who had five or more poor mercury hygiene factors was only 63% of that for unexposed women (95% CI 42%-96%) after controlling for covariates. Women with low exposure were more fertile, however, than unexposed controls. Possible explanations for the U shaped dose response and limitations of the exposure measure are discussed. Further investigation is needed that uses biological measures of mercury exposure.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baird D. D., Wilcox A. J. Cigarette smoking associated with delayed conception. JAMA. 1985 May 24;253(20):2979–2983. [PubMed] [Google Scholar]
- Baird D. D., Wilcox A. J., Weinberg C. R. Use of time to pregnancy to study environmental exposures. Am J Epidemiol. 1986 Sep;124(3):470–480. doi: 10.1093/oxfordjournals.aje.a114417. [DOI] [PubMed] [Google Scholar]
- Battistone G. C., Hefferren J. J., Miller R. A., Cutright D. E. Mercury: its relation to the dentist's health and dental practice characteristics. J Am Dent Assoc. 1976 Jun;92(6):1182–1188. doi: 10.14219/jada.archive.1976.0173. [DOI] [PubMed] [Google Scholar]
- Brady J. A., Gemmiti-Nunn D., Polan A. K., Mitchell D., Weil R., Vianna N. J. The relationship of dental practice characteristics to blood mercury levels. N Y State Dent J. 1980 Aug-Sep;46(7):420, 422-4. [PubMed] [Google Scholar]
- Brown D. Detection of mercury vapour in the dental surgery. An assessment of disposable monitoring discs. Br Dent J. 1983 Oct 8;155(7):237–240. doi: 10.1038/sj.bdj.4805189. [DOI] [PubMed] [Google Scholar]
- Brune D., Beltesbrekke H. Mercury vapor levels in a dental laboratory. Scand J Dent Res. 1978 Jul;86(4):300–302. doi: 10.1111/j.1600-0722.1978.tb00630.x. [DOI] [PubMed] [Google Scholar]
- Brune D., Hensten-Pettersen A., Beltesbrekke H. Exposure to mercury and silver during removal of amalgam restorations. Scand J Dent Res. 1980 Oct;88(5):460–463. doi: 10.1111/j.1600-0722.1980.tb01254.x. [DOI] [PubMed] [Google Scholar]
- Buchwald H. Exposure of dental workers to mercury. Am Ind Hyg Assoc J. 1972 Jul;33(7):492–502. doi: 10.1080/0002889728506692. [DOI] [PubMed] [Google Scholar]
- Cavanagh J. B. Long term persistence of mercury in the brain. Br J Ind Med. 1988 Oct;45(10):649–651. doi: 10.1136/oem.45.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rosis F., Anastasio S. P., Selvaggi L., Beltrame A., Moriani G. Female reproductive health in two lamp factories: effects of exposure to inorganic mercury vapour and stress factors. Br J Ind Med. 1985 Jul;42(7):488–494. doi: 10.1136/oem.42.7.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erfurth E. M., Schütz A., Nilsson A., Barregård L., Skerfving S. Normal pituitary hormone response to thyrotrophin and gonadotrophin releasing hormones in subjects exposed to elemental mercury vapour. Br J Ind Med. 1990 Sep;47(9):639–644. doi: 10.1136/oem.47.9.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris D., Nicols J. J., Stark R., Hill K. The dental working environment and the risk of mercury exposure. J Am Dent Assoc. 1978 Nov;97(5):811–815. doi: 10.14219/jada.archive.1978.0380. [DOI] [PubMed] [Google Scholar]
- Herber R. F., de Gee A. J., Wibowo A. A. Exposure of dentists and assistants to mercury: mercury levels in urine and hair related to conditions of practice. Community Dent Oral Epidemiol. 1988 Jun;16(3):153–158. doi: 10.1111/j.1600-0528.1988.tb00564.x. [DOI] [PubMed] [Google Scholar]
- Howe G., Westhoff C., Vessey M., Yeates D. Effects of age, cigarette smoking, and other factors on fertility: findings in a large prospective study. Br Med J (Clin Res Ed) 1985 Jun 8;290(6483):1697–1700. doi: 10.1136/bmj.290.6483.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokstad A. Mercury excretion and occupational exposure of dental personnel. Community Dent Oral Epidemiol. 1990 Jun;18(3):143–148. doi: 10.1111/j.1600-0528.1990.tb00040.x. [DOI] [PubMed] [Google Scholar]
- Jones D. W., Sutow E. J., Milne E. L. Survey of mercury vapour in dental offices in Atlantic Canada. J Can Dent Assoc. 1983 Jun;49(6):378–395. [PubMed] [Google Scholar]
- Joselow M. M., Goldwater L. J., Alvarez A., Herndon J. Absorption and excretion of mercury in man. XV. Occupational exposure among dentists. Arch Environ Health. 1968 Jul;17(1):39–44. [PubMed] [Google Scholar]
- Kajiwara Y., Inouye M. Inhibition of implantation caused by methylmercury and mercuric chloride in mouse embryos in vivo. Bull Environ Contam Toxicol. 1992 Oct;49(4):541–546. doi: 10.1007/BF00196296. [DOI] [PubMed] [Google Scholar]
- Kelman G. R. Urinary mercury excretion in dental personnel. Br J Ind Med. 1978 Aug;35(3):262–265. doi: 10.1136/oem.35.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosta L., Byrne A. R., Zelenko V. Correlation between selenium and mercury in man following exposure to inorganic mercury. Nature. 1975 Mar 20;254(5497):238–239. doi: 10.1038/254238a0. [DOI] [PubMed] [Google Scholar]
- Lamperti A. A., Printz R. H. Effects of mercuric chloride on the reproductive cycle of the female hamster. Biol Reprod. 1973 Apr;8(3):378–387. doi: 10.1093/biolreprod/8.3.378. [DOI] [PubMed] [Google Scholar]
- Lamperti A. A., Printz R. H. Localization, accumulation, and toxic effects of mercuric chloride on the reproductive axis of the female hamster. Biol Reprod. 1974 Sep;11(2):180–186. doi: 10.1095/biolreprod11.2.180. [DOI] [PubMed] [Google Scholar]
- Langan D. C., Fan P. L., Hoos A. A. The use of mercury in dentistry: a critical review of the recent literature. J Am Dent Assoc. 1987 Dec;115(6):867–880. doi: 10.14219/jada.archive.1987.0270. [DOI] [PubMed] [Google Scholar]
- Langworth S., Röjdmark S., Akesson A. Normal pituitary hormone response to thyrotrophin releasing hormone in dental personnel exposed to mercury. Swed Dent J. 1990;14(2):101–103. [PubMed] [Google Scholar]
- Lee Y. H., Shaikh Z. A., Tohyama C. Urinary metallothionein and tissue metal levels of rats injected with cadmium, mercury, lead, copper or zinc. Toxicology. 1983 Jul-Aug;27(3-4):337–345. doi: 10.1016/0300-483x(83)90029-x. [DOI] [PubMed] [Google Scholar]
- Linn S., Schoenbaum S. C., Monson R. R., Rosner B., Ryan K. J. Delay in conception for former 'pill' users. JAMA. 1982 Feb 5;247(5):629–632. [PubMed] [Google Scholar]
- Liu J., Kershaw W. C., Klaassen C. D. The protective effect of metallothionein on the toxicity of various metals in rat primary hepatocyte culture. Toxicol Appl Pharmacol. 1991 Jan;107(1):27–34. doi: 10.1016/0041-008x(91)90327-b. [DOI] [PubMed] [Google Scholar]
- McGregor A. J., Mason H. J. Occupational mercury vapour exposure and testicular, pituitary and thyroid endocrine function. Hum Exp Toxicol. 1991 May;10(3):199–203. doi: 10.1177/096032719101000309. [DOI] [PubMed] [Google Scholar]
- Möller-Madsen B., Hansen J. C., Kragstrup J. Mercury concentrations in blood from Danish dentists. Scand J Dent Res. 1988 Feb;96(1):56–59. doi: 10.1111/j.1600-0722.1988.tb01408.x. [DOI] [PubMed] [Google Scholar]
- Naleway C., Sakaguchi R., Mitchell E., Muller T., Ayer W. A., Hefferren J. J. Urinary mercury levels in US dentists, 1975-1983: review of Health Assessment Program. J Am Dent Assoc. 1985 Jul;111(1):37–42. doi: 10.14219/jada.archive.1985.0069. [DOI] [PubMed] [Google Scholar]
- Nilsson B., Nilsson B. Mercury in dental practice. II. Urinary mercury excretion in dental personnel. Swed Dent J. 1986;10(6):221–232. [PubMed] [Google Scholar]
- Nordberg G. F. Modulation of metal toxicity by metallothionein. Biol Trace Elem Res. 1989 Jul-Sep;21:131–135. doi: 10.1007/BF02917245. [DOI] [PubMed] [Google Scholar]
- Nylander M., Weiner J. Mercury and selenium concentrations and their interrelations in organs from dental staff and the general population. Br J Ind Med. 1991 Nov;48(11):729–734. doi: 10.1136/oem.48.11.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards J. M., Warren P. J. Mercury vapour released during the removal of old amalgam restorations. Br Dent J. 1985 Oct 5;159(7):231–232. doi: 10.1038/sj.bdj.4805688. [DOI] [PubMed] [Google Scholar]
- Rowland A. S., Baird D. D., Weinberg C. R., Shore D. L., Shy C. M., Wilcox A. J. Reduced fertility among women employed as dental assistants exposed to high levels of nitrous oxide. N Engl J Med. 1992 Oct 1;327(14):993–997. doi: 10.1056/NEJM199210013271405. [DOI] [PubMed] [Google Scholar]
- Roydhouse R. H., Ferg M. R., Knox R. P. Mercury in dental offices. Survey in Vancouver, B.C. J Can Dent Assoc. 1985 Feb;51(2):156–158. [PubMed] [Google Scholar]
- Schneider M. An environmental study of mercury contamination in dental offices. J Am Dent Assoc. 1974 Nov;89(5):1092–1098. doi: 10.14219/jada.archive.1974.0537. [DOI] [PubMed] [Google Scholar]
- Sikorski R., Juszkiewicz T., Paszkowski T., Szprengier-Juszkiewicz T. Women in dental surgeries: reproductive hazards in occupational exposure to metallic mercury. Int Arch Occup Environ Health. 1987;59(6):551–557. doi: 10.1007/BF00377918. [DOI] [PubMed] [Google Scholar]
- Skare I., Bergström T., Engqvist A., Weiner J. A. Mercury exposure of different origins among dentists and dental nurses. Scand J Work Environ Health. 1990 Oct;16(5):340–347. doi: 10.5271/sjweh.1774. [DOI] [PubMed] [Google Scholar]
- Smart E. R. The hazards of mercury in dentistry. Rev Environ Health. 1985;5(1):59–86. [PubMed] [Google Scholar]
- Smith D. C., Lewis D. W. Study calls for dental office investigations. Ont Dent. 1987 Jun;64(6):21–26. [PubMed] [Google Scholar]
- Templeton D. M., Cherian M. G. Toxicological significance of metallothionein. Methods Enzymol. 1991;205:11–24. doi: 10.1016/0076-6879(91)05079-b. [DOI] [PubMed] [Google Scholar]
- Votaw A. L., Zey J. Vacuuming a mercury-contaminated dental office may be hazardous to your health. Dent Assist. 1991 Jan-Feb;60(1):27–29. [PubMed] [Google Scholar]
- Waalkes M. P., Goering P. L. Metallothionein and other cadmium-binding proteins: recent developments. Chem Res Toxicol. 1990 Jul-Aug;3(4):281–288. doi: 10.1021/tx00016a001. [DOI] [PubMed] [Google Scholar]
- Watanabe T., Shimada T., Endo A. Effects of mercury compounds on ovulation and meiotic and mitotic chromosomes in female golden hamsters. Teratology. 1982 Jun;25(3):381–384. doi: 10.1002/tera.1420250315. [DOI] [PubMed] [Google Scholar]
- Weinberg C. R., Wilcox A. J., Baird D. D. Reduced fecundability in women with prenatal exposure to cigarette smoking. Am J Epidemiol. 1989 May;129(5):1072–1078. doi: 10.1093/oxfordjournals.aje.a115211. [DOI] [PubMed] [Google Scholar]


