Abstract
Since the earliest days, people have been employing herbal treatments extensively around the world. The development of phytochemical and phytopharmacological sciences has made it possible to understand the chemical composition and biological properties of a number of medicinal plant products. Due to certain challenges like large molecular weight and low bioavailability, some components of herbal extracts are not utilized for therapeutic purposes. It has been suggested that herbal medicine and nanotechnology can be combined to enhance the benefits of plant extracts by lowering dosage requirements and adverse effects and increasing therapeutic activity. Using nanotechnology, the active ingredient can be delivered in an adequate concentration and transported to the targeted site of action. Conventional therapy does not fulfill these requirements. This review focuses on different skin diseases and nanotechnology-based herbal medicines that have been utilized to treat them.
Keywords: skin, herbal formulations, skin diseases, drug delivery system, nanoparticles, ethosomes
1. Introduction
The skin is the largest organ of the human body. The skin acts as the initial defense line. The skin has several different cells and structures. The three main layers are the dermis, hypodermis, and epidermis. Every layer has a different role to play in the overall functionality of the skin. Every layer on the body varies in thickness. It is the thickest on the palms and soles and thinnest on the eyelids. The position of the skin affects the dermis’s thickness as well. Beneath the dermis is the hypodermis or subcutaneous connective tissue. The subcutaneous layer varies in thickness from person to person and throughout the body. The primary skin appendages are sweat glands, oil glands, and hair follicles. The skin covers and protects the interior organs, bones, muscles, and ligaments. Hairy skin and glabrous skin are the two basic types of skin [1]. The skin can also be pale, sensitive, dry, sagging, and worn out.
Skin is essential for defending the body from infections as well as water loss [1,2]. Other roles include water resistance, insulation, temperature control, sensations, storage, and vitamin D synthesis by ultraviolet (UV) light. It also protects vitamin B folates and aids in the absorption of various medications [3]. Scar tissue formation is an attempt by skin to heal from severe wounds. Frequently, this is depigmented and dingy [4].
For both the treatment and prevention of numerous diseases, natural products and conventional pharmaceuticals are beneficial [5]. They are becoming more popular as complementary therapies for typical skin diseases [6]. Plant-based natural medicines have grown in popularity throughout time because of their many advantages, such as few side effects, low cost, and long-term acceptability. Additionally, medicinal plants can be used as raw materials in the creation of novel therapeutic medicines. Calendula officinalis, Azadirachta A. Juss., Portulaca amilis, Aloe vera, and many more plants have been studied for the treatment of various skin conditions ranging from itching to skin cancer and they have been reported to be effective in managing a number of skin conditions [4,7]. Numerous traditional medical systems, including Chinese Medicine, Ayurveda, Siddha, and the Unani System of Medicine, have extensive documentation on the therapeutic use of plants. Nearly a third part of the most popular medications in the market today come from plants or alternative natural sources [8,9]. Herbal medications have unique properties that conventional drug administration methods like capsules, syrups, and decoctions cannot match. Nonetheless, using nanotechnology to deliver herbal medications has proven to be highly effective [10].
Herbal technology has proven useful in a number of medical sciences sectors, including organ and tissue imaging, artificial implants, nanorobotics, biosensors, and enhanced drug delivery systems, such as regulated or sustained drug delivery. Herbal nanomedicines are nanosized pharmaceuticals that include extracts, concentrated fractions, or biomarker elements of herbal medications. Due to their higher bioavailability and lower toxicity, herbal nanomedicines possess a number of advantages [11]. With improved bioavailability and fewer toxicities, combining herbal medicine with nanotechnology may be a valuable resource for the development of herbal formulations [12]. Overall, it is well-established that herbal nanomedicines are safer, more bioavailable, and have greater therapeutic value than traditional herbal and synthetic pharmaceuticals [11].
Although the contributions of nanotechnology are helpful in a number of medical fields, it is important to draw attention to specific drawbacks. Common concerns related to nano-sized particles including the potential to cause hazardous lung diseases and lead to other diseases that might cause changes in homeostasis or even mortality, have been cited by clinical researchers [13]. Other negative factors mentioned include difficulties in scaling up procedures and high cost [14]. This review outlines the application of several herbal nanoformulations, along with different skin conditions and herbal drugs used to treat them. Additionally, it shows several patents that have been published on skin conditions. This paper explains how the popularity of herbal products has increased interest among researchers and enhanced productivity by preventing several skin conditions.
2. Skin Diseases
The human body’s largest and most varied organ is the skin. The general state of one’s skin is significant for both cosmetic and health reasons. The patient’s psychological state is impacted by its unfavorable appearance due to dermatitis, and both of these elements are crucial in the development and management of chronic skin illnesses [15]. Increased awareness of one’s body and appearance, especially among young people, exacerbates anxiety [16]. A number of variables, including gender, race, personal cleanliness, the standard of skincare, the environment, and diet, influence the occurrence and incidence of cutaneous illnesses in young people [17]. In certain cases, patients seem to manifest lesions of the skin due to the tensions brought on by interpersonal disputes and unresolved emotional issues [16]. The different skin diseases are shown in Figure 1 [18].
Figure 1.
Various types of skin diseases. Reproduced with permission from [18] Creative Commons Attribution License 4.0.
2.1. Common Skin Problems
Skin conditions are a prevalent ailment that can injure a person in various ways and affect people of all ages. Despite the fact there are over more than one thousand illnesses that can damage the skin, the main categories of skin diseases are discussed below [4].
2.1.1. Rashes
A rash is a collection of several patches or a specific area of irritated skin surface. It can be brought on by infections, allergies, and overactive oil glands, which can result in psoriasis, dermatitis, eczema, and acne [19].
2.1.2. Viral Infections
Viral skin disorders affect persons of all ages and range from straightforward exanthems to intricate systemic illnesses. Most exanthems of viral origin are self-limiting. Warts, herpes simplex, and herpes zoster are a few examples of viral skin infections [20].
2.1.3. Bacterial Infections
Acute bacterial and skin structure infections are two categories of bacterial skin infections, along with skin and soft tissue infections. Both cellulitis and erythrasma are complicated bacterial illnesses that are impacted by fat. Other complex bacterial illnesses include erysipelas, wound infections, and severe cutaneous abscesses.
2.1.4. Fungal Infection
Moisture and maceration in intertriginous zones create a perfect habitat for yeasts to grow, including Candida species. This causes inflammation and redness, as well as satellite lesions in the inguinal area, beneath the breasts, and in the abdominal folds. An important part of the growth of candidiasis is friction and maceration. Although less common, obese people can also have candidal folliculitis. While oral medications like fluconazole or itraconazole or topical antifungals like ketoconazole and econazole creams can effectively treat the illness, they cannot stop recurrences.
2.1.5. Pigmentation Problems
Patients with abnormal pigmentation, such as those with vitiligo, melasma, and post-inflammatory hyperpigmentation (PIHP), may also have serious concerns. Pigment loss, commonly in the lips and fingertips, is called vitiligo. Melasma, which is characterized by symmetrical regions of hyperpigmentation, can result from a variety of factors, such as exposure to high UV radiation levels, chemical agents, female hormone imbalances, or genetic abnormalities [21]. PIHP is commonly associated with skin inflammation and may manifest during surgery, laser ablation, dermatitis flare-ups, or in patients treated with photosensitizing medications [22,23].
2.1.6. Cancers
Skin cells can be harmed by excessive sun exposure or other UV radiation, leading to the development of skin cancer. Skin cancer can be classified into three primary types: melanoma, squamous cell carcinoma (SCC), and basal cell carcinoma (BCC). Even though melanoma is the rarest form of skin cancer, its high rate of metastasis makes it the deadliest. However, keratinocyte malignancies, such as BCC and SCC, account for the majority of cases of skin cancer [24].
2.1.7. Others
Among the problems that cannot be clearly characterized are wrinkles, rosacea, spider veins, and varicose veins. The breakdown of collagen and elastin in the dermis results in drooping skin, ultimately giving rise to wrinkles. Rosacea is a chronic condition that causes the skin of the human face to grow red, develop lesions and pimples, and, less frequently, expand the nose. Its origin is a mystery. When blood vessels develop and become apparent through the skin’s surface, spider veins and varicose veins are evident [4]. Erythema is the outcome of an inflamed cutaneous reaction linked to conditions including psoriasis, acne, fever from systemic disorders, and sunburn from exposure to certain electromagnetic wave bands, primarily ultraviolet radiation [22].
3. Herbal Drugs for Skin Diseases
The use of synthetic molecules and chemical compounds can result in skin toxicity from safety concerns with long-term use. The demand for herbal drugs has skyrocketed due to an increased awareness of the photoaging and carcinogenic consequences and socioeconomic advancement [25,26]. Overall, there is an increase in demand for plant-based medications, health goods, food supplements, and cosmetics. The cause of this is the rising understanding that natural products are harmless, have few adverse effects, and are widely accessible at low costs [27]. All scientific communities are concentrating their study on understanding the chemical constitution of plants with medicinal properties and their common usage. With fewer adverse effects than current medications, this research could result in increasingly ingenious products [14,28].
According to the World Health Organization, herbal medications are fully developed and labeled pharmaceuticals that contain combinations of aerial, subterranean, or other plant elements, as well as active ingredients [27]. Natural drugs made from plants are becoming increasingly popular because of a number of advantages, such as frequently fewer side effects, increased patient compliance, being comparatively cheaper, and being widely accepted due to a long history of use. Herbal treatments also provide sensible approaches to address a range of ailments that are incurable or difficult to cure with traditional medical procedures. These factors have led to studies on a variety of plants as possible remedies for skin disorders ranging from skin cancer to itching. Over the previous years of research, more than 31 plants have so far been reported to be beneficial in treating a variety of skin conditions [4]. Various herbal drugs used for different skin diseases are discussed below.
3.1. Atopic Dermatitis
An inflammatory, itchy, and chronic skin condition is known as atopic dermatitis [29].
Licorice
A thorough analysis summarizes the anti-inflammatory properties of licorice, i.e., Glycyrrhiza glabra L. and Glycyrrhiza uralensis. Glycyrrhetinic acid, the triterpenes of licorice, and glycyrrhizin were used in the skin investigations [30,31]. Nevertheless, several components, such as the chalcone licochalcone A [32] and the flavonoid isoliquiritigenin [33], also have anti-inflammatory properties. Licochalcone A-containing cream showed better anti-inflammatory effects in placebo-controlled research including 26 individuals [34]. Furthermore, a placebo-controlled double-blind UV-erythema evaluation study demonstrated anti-inflammatory effects with an herbal composition, containing 0.1% root extract of Glycyrrhiza uralensis and 0.6% glycyrrhizinic acid as the main active ingredients, at 48 h after irradiation and cream application. The medication made of licorice was just as successful as 1% hydrocortisone acetate. A non-interventional pilot study also resulted in a reduction in the severity score in ten atopic dermatitis patients given this medication twice daily for two weeks [35].
-
b.
Tormentil and Evening Primrose
Since ancient times, dermatologists have empirically employed tannins from black tea and oak bark. Tannins are applied topically as local baths or wet-lipid wraps to treat oozing and acute eczema [36]. Due to the high γ-linolenic acid content in evening primrose oil, it is good for atopic dermatitis. It finds applications in topical products as well as in products for internal use [36]. After 48 h, an occlusive patch test revealed that a cream with 2% tannins obtained from the roots of tormentil had a vasoconstrictive effect similar to that of a corticoid [37].
3.2. Psoriasis
Herbal medicines are also applied topically to treat psoriasis. Long-term immune-mediated psoriasis is characterized by scaly, red, burning, and itchy skin patches [36].
Araroba tree
The anthracene derivative dithranol is the most effective topical therapy for psoriasis. Dithranol prevents keratinocyte growth and the secretion of pro-inflammatory cytokines. When compared to the standard treatment of calcipotriol ointment, a randomized multicenter study involving 106 psoriasis patients with chronic psoriasis plaques showed significantly better therapeutic efficaciousness [38].
-
b.
Indigo
An essential treatment in Traditional Chinese Medicine is “Indigo naturalis”. It is a blue powder made by grinding, fermenting, and adding lime to the plant Baphicacanthus cusia [36]. Numerous psoriasis trials have been conducted using indigo extract. Applying indigo extract twice daily for eight weeks proved to be effective in reducing psoriasis in 100 patients, based on a recently conducted double-blind, randomized, placebo-controlled trial. Both the 200 µg/g and 50 µg/g of indigo extract decreased the PASI by 70% and 50%, respectively. Some patients experienced local erythema, upper respiratory tract infections, and nasopharyngitis as side effects. Punch biopsies taken prior to and following an 8-week course of therapy demonstrated downregulation and a restoration of skin morphology [39].
-
c.
Turmeric
In both Traditional Chinese Medicine and Ayurvedic medicine, turmeric is crucial. Turmeric, with its main active component, curcumin, has anti-inflammatory, antibacterial, and antioxidative qualities in vitro [40]. In recent years, a number of clinical and laboratory investigations have looked into curcumin’s potential as a treatment for psoriasis. Curcumin has the potential to alleviate psoriasis through its inhibition of phosphorylase kinase [41], reduction of pro-inflammatory cytokines like TNF-α and IL-17, and enhancement of the epidermis barrier through the in vitro induction of involucrin and filaggrin production [42].
-
d.
Olibanum
Galen, Hippocrates, and Dioscorides all prescribed olibanum-containing ointments during the Greco–Roman era to treat a variety of skin conditions, including warts, psoriasis, bleeding, burns, and wounds. A total of 200 individuals with intermediate to mild psoriasis underwent three daily doses of an olibanum ointment containing 5% of 3-O-Acetyl-11-keto-β-boswellic acid for a period of 12 weeks in an open-label application study. The PASI dropped dramatically [36,43].
3.3. Herpes Simplex
Almost any area of the skin can develop blisters and sores due to the virus that causes herpes simplex. These sores typically appear on the genitalia and buttocks or around the mouth and nose. Numerous extracts, such as licorice extract and Boswellia serrata oleo gum, were reported to have antiviral action [44,45]. Clinical research utilizing these plant-based products is still lacking [36].
Lemon balm
In a randomized, double-blind, placebo-controlled study, 66 individuals who had persistent herpes simplex labialis were evaluated with lemon balm cream. For five days, the test cream—a 1% dried Melissa officinalis extract—was applied four times a day. Lemon balm cream caused the lesions to resolve far more quickly, and the patients experienced less pain and blistering [46].
3.4. Wound Healing
Wound healing is an intricate interplay between the vascular system, cytokines, and various cell types, such as keratin cells, fibroblasts, and immune cells, that stop bleeding, eliminate pathogens, and initiate the process of re-epithelialization. Most traditionally used herbal remedies for wound healing have not been investigated as part of closely supervised clinical research [47].
Birch bark
The molecular elucidation of betulin’s wound-healing characteristics demonstrates a positive impact on all three stages of wound healing [48]. In a split-thickness wound examination, the first clinical evidence for betulin’s wound healing properties was achieved through the topical application of a water-free betulin oleogel [49]. Following that, betulin oleogel was used in a number of multicentric, controlled, randomized clinical trials on second-degree burns and superficial wounds [50,51].
Similarly, other plants such as Psidium guajava and Eucalyptus camaldulensis also possess wound healing properties [52,53].
-
b.
Allium cepa (Onion)
An onion extract was tested for its effect on scar formation in 58 participants who had minor skin surgeries, such as punch biopsies or the removal of skin tumors, in a randomized placebo-controlled study. Following three weeks of primary wound healing, the patients were given either onion extract or a placebo twice a day for ten weeks. When compared to a placebo, onion extract dramatically improved the scars’ overall appearance, smoothness, texture, and redness [54].
3.5. Acne Vulgaris
Perifollicular inflammation, the hyperproliferation of the epidermis, and hyperactive sebaceous glands are the hallmarks of acne vulgaris [36].
Green tea
It may be demonstrated that the main polyphenol in green tea, epigallocatechin-3-gallate, has anti-inflammatory, sebosuppressive, and apoptotic properties on human sebocytes. Additionally, it exhibits antimicrobial properties against Propionibacterium acnes. An eight-week randomized split-face clinical experiment including 35 patients receiving either 5% or 1% epigallocatechin-3-gallate solution two times daily showed considerable improvement in acne [55].
-
b.
Melaleuca alternifolia (Tea tree)
A randomized double-blind vehicle-controlled study comprising sixty patients with acne verified the effectiveness of a gel that included five percent tea tree oil when administered twice a day for forty-five days [56].
-
c.
Humulus lupulus (Hop)
Hop extract has anti-inflammatory and antioxidant properties. Furthermore, in the agar diffusion test, a gel formulation with 0.3% w/w hop extract exhibited antibacterial activity against Staphylococcus aureus and Propionibacterium acnes. Thus, hop extract needs to be investigated in clinical trials as a potential alternative treatment for skin prone to acne [36,57].
3.6. Skin Cancer
Skin cancers, being the most prevalent cancers, are identified in Caucasians globally, and as a result of increased exposure to ultraviolet radiation, their incidence is steadily rising. Skin cancer is defined by an imbalance that favors either excessive cell survival and proliferation in the epidermis or insufficient apoptosis [58,59].
Panax ginseng
In this study, red ginseng extracts applied topically were shown to suppress chemically produced skin cancers in mice [60].
-
b.
Rosmarinus officinalis (Rosemary)
Extracts from rosemary (Rosmarinus officinalis) are said to possess antioxidant properties. The effects of a leaf methanol extract on mouse skin cancers were assessed. In mice given recognized chemical carcinogens, it was discovered that topically applied rosemary reduced the formation and growth of skin cancers. It seems that multiple extract constituents play a significant role in this process, even if the precise mechanism of action is currently being investigated. According to this research, antioxidant qualities were not the only thing that helped prevent skin cancers [61,62]. Some other plants used in skin disorders are listed in Table 1.
Table 1.
Plants used for skin diseases.
| Name of Plant | Part of Plant | Use | Research | Ref. |
|---|---|---|---|---|
| Oryza sativa | Seeds | Antioxidant and anti-inflammatory activity, antibacterial effect, antifungal effect, psoriasis, and anti-aging agent | Palungwachira et al. evaluated the cellular activity of anthocyanins, which will be useful in the creation of new products that promote natural healing. Based on the modulation of type-I collagen gene expression and the suppression of H2O2-induced activation of necrosis factor-B in skin fibroblasts, the data indicated that anthocyanins from Oryza sativa have anti-inflammatory and anti-aging potential. | [63] |
| Nicotiana tabacum | Leaves | Antibacterial, antifungal, wound healing, and anti-aphthous activity | Sharma et al. used a Wistar rat model to examine the wound-healing properties of an ethanolic extract of stems of Nicotiana tabacum. Studies conducted in vitro and in vivo have shown the high efficiency of ethanolic extracts in wound healing, suggesting that they could be applied topically as herbal medicine. | [64] |
| Knema globularia | Seeds, leaves | Cytotoxic activity and antioxidant activity | Thinh et al. determined the antioxidant effect of the leaves of Knema globularia. The findings demonstrated the potent antioxidant qualities of the methanol essential oil of Knema globularia, suggesting that they may offer a novel and dependable supply of naturally occurring antioxidants. | [65] |
| Senna macranthera | Flowers | Antifungal activity | Nascimento et al. evaluated the antifungal and cytotoxic effects of flowers of senna species. The current findings indicated that flowers of Senna macranthera are a promising source of novel antifungal compounds. | [66] |
| Punica granatum | Pericarp | Anti-melanoma, anti-inflammatory, antibacterial, and wound healing | Saini et al. utilized the peel extract of Punica granatum and evaluated its antibacterial activity against multidrug-resistant bacteria. Strong antibacterial activity was observed in the interaction with Punica granatum peel extract, with a minimum inhibitory concentration of 780–6250 μg/mL and a zone of inhibition measuring 24.33 mm. | [67] |
| Aloe vera | Leaves | Insect bites, sunburns, wound infections, scabies, wound healing, burns, itching, and swelling [19] | Padmakar et al. evaluated natural aloe vera’s safety and effectiveness in treating stable vitiligo. It was found that using natural aloe vera to treat stable vitiligo was both effective and safe. However, in order to confirm the effectiveness and safety of Aloe vera in the management of vitiligo, higher sample sizes for randomized controlled trials are advised. | [68] |
| Jatropha curcas | Seeds, roots, leaves | Wound healing and skin lesions [19] | An herbal ointment with pro-wound healing properties was developed and tested, incorporating the methanol leaf extract of Jatropha curcas. The application of the ointment batch containing the maximum amount of Jatropha curcas extract showed the highest rate of wound closure in comparison to the blank ointment, which had an epithelialization duration of 18.8 days. | [69] |
| Glycyrrhiza glabra | Root | Allergic dermatitis, depigmentation, and atopic dermatitis [19] | Jan et al. isolated different polyphenols from the extract of Glycyrrhiza glabra and found flavonoids and other compounds showing antioxidant activity. | [70] |
| Ficus carica | Fruit | Skin ulcers, acne, hyperpigmentation, eczema [19] | Khan et al. sought to determine the effect of cream containing fruit extract from Ficus carica on skin parameters such as erythema, sebum, moisture content, trans-epidermal water loss, and skin pigmentation. The pigment melanin, trans-epidermal water loss, and skin sebum were all considerably reduced by the formulation and had a negligible impact on skin erythema while greatly increasing skin moisture. | [71] |
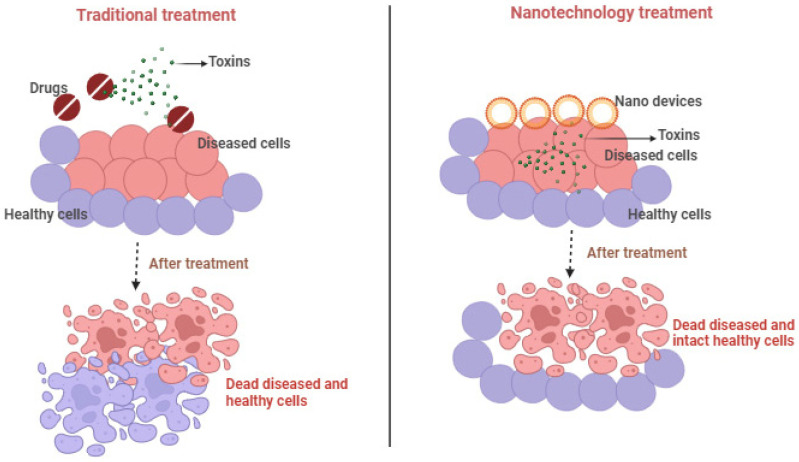
4. Traditional Treatment vs. Nanotechnology-Based Treatment
Nanotechnology uses nanoscale particles, nanofiber, and nanodevices to deliver drugs and other substances to specific cells in the human body. This is done for the purpose of treating diseases or injuries within the targeted cells and minimizing damage to other cells. Nanoparticulate medications have a number of benefits over traditional drug formulations, including improved bioavailability, a quicker onset of action, dosage homogeneity, and less variability between fasting and feeding, as discussed in Table 2. Nanomedicine has brought advancement in drug delivery and discovery.
Table 2.
Traditional vs. nanotechnological approach.
| Features | Traditional Herbal Formulation | Nanotechnological Herbal Formulation |
|---|---|---|
| Particle Size | Larger | Nano-size |
| Solubility | Limited Solubility | Higher solubility |
| Bioavailability | Limited Bioavailability | Higher bioavailability due to small size |
| Targeted Delivery | No | Provides targeted delivery to specific cells |
| Dosing Precision | Less precise | More precise |
| Surface Area | Less surface area for interaction | More surface area for interaction |
| Production Process | Simple | Complex |
| Allergic Reactions | More allergic reactions to extract | Less, as the drug is enclosed in nanoformulation |
| Interaction with other drugs | Possible | It may or may not be possible |
| Skin Irritation | Yes | No |
| Efficacy | Low | High |
Research and development advances are reflected in nanotechnology, which enhances product efficacy. In order to get around some of the drawbacks of conventional goods, nanotechnology is being used more and more in the cosmeceutical industry. Nano cosmeceuticals are now widely utilized to treat a variety of skin problems, including wrinkles, acne, photoaging, hyperpigmentation, etc. [72]. Lohani et al. recently analyzed a few nanoproducts made by a limited number of companies, such as Skin Caviar Ampoules, Hydra Zen Cream, and Revitalift, which use different nanotechnologies to manufacture phytocompounds. Vegetable oils and curcumin, two phyto bioactive substances that are nanosized, improve the appearance of skin through a variety of antioxidative processes. The products described above guard against premature aging and oxidative stress-induced skin aging [73]. Herbal cosmeceuticals are used to maintain the health and hygienic conditions of the skin. These products improve the skin’s condition and revitalize it at the cellular and molecular levels. The daily use of cosmeceuticals for skin care includes antioxidants, anti-inflammatories, skin rejuvenation agents, etc. [72]. Recent studies depict that phyto-based nano cosmeceuticals, which have improved protection, aesthetic, and health benefits, will certainly play an increasingly multifunctional role in the near future.
Herbal medicines have been used since ancient times for the treatment of various diseases, including skin diseases, but they also cause damage to normal cells as they do not provide targeted delivery. The nanotechnology-based delivery of herbal drugs provides targeted delivery and does not cause any harm to the uninfected or normal cells of the body [74]. The comparison between traditional and nanotechnology-based treatment on the basis of targeting is depicted in Figure 2.
Figure 2.
Comparison between traditional and nanotechnology-based treatment [75].
5. Herbal Nanotechnology
The use of nanotechnology in combination with herbal extracts has been extensively documented in the literature due to the potential for nanostructured systems to increase the benefits of plant-based extracts, enhance the prolonged absorption of active ingredients, lower dosage requirements, lessen adverse effects, and enhance efficacy [76,77]. Many nanotechnological methods are being employed, such as liposomes, liquid crystal systems, polymeric nanoparticles, and precursor systems for liquid crystals [78]. These techniques enable the use of materials with various properties in a single formulation and may even alter a material’s properties and behavior in a biological environment. The delivery of drugs has been transformed by these technical advancements [79].
The ability to reintroduce inactive substances that were previously removed because they were inappropriate for formulation, in addition to increasing the strength of the active ingredients, is provided by the new drug delivery techniques [80]. The ability to improve novel compounds prior to their commercial release or medical application makes this approach even more alluring. Raising selectivity as well as efficacy, protecting against heat and photodegradation, reducing negative effects, and controlling the diffusion of active ingredients are a few instances of such improvements [81]. Various nanotechnological systems and their use are depicted in Figure 3 [82].
Figure 3.
Various nanotechnology-based delivery systems and their uses for topical dermatological therapy. Adapted with permission from ref. [82] under Creative Commons Attribution License 4.0 (https://creativecommons.org/licenses/by/4.0/).
There is a need for improvements in nanotechnology and nanoscience, which pertain to the utilization of nanoscale materials, which, to date, have only been the focus of the cosmetics sector, along with advancements in recent decades connected to medical research. Scientific innovations can transform and improve approaches to solve challenging formulation preparation issues [83]. Nanostructures can successfully combine active ingredients with varying degrees of hydrophilicity and lipophilicity, as well as enhance the solubility and stability of active ingredients. The movement of a chemical to particular tissues or organs can also be targeted using this method [84].
To boost the absorption of the active ingredients, Bhattacharya and Ghosh utilized lipid-based systems and added green tea and ginseng (Araliaceae) extracts to several formulations [85]. Artemisia arborescens was used by Sinico et al. to create liposomes which showed that the technique assisted the active ingredients (β-thyjon and camphor, derivatives of azulene) from the plant in crossing the cytoplasmic viral barrier [86]. Ocimum sanctum L. (Lamiaceae) methanolic extract was used to create nanoparticles by Rajendran et al. They reported that when examined against Bacillus subtilis, Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus, the antibacterial activity of the encapsulated extract was superior to that of the free-form formulation [77]. Skin soft-tissue infections and scars can be efficiently treated using Rhodomyrtus tomentosa leaf-loaded transferosomes, which are natural biomedicines [87,88]. Similarly, other nano formulations such as phytosome-loaded shape memory gels for skin aging [89] and the microemulsion of the oil of Kaempferia galanga for UV ray protection [90] have been formulated. It is an intriguing strategy to enhance a formulation’s most appealing characteristics by using various drug delivery systems that utilize nanotechnology. Additionally, nanoscale particles might be an indication of the time when activity is guaranteed and issues with employing medicinal plants are resolved [14].
The different herbal formulations based on different nanotechnology-based systems are as follows.
5.1. Polymeric Nanoparticles
The harungana of Madagascar Lam. Ex Poir is well renowned for its ability to fight off viruses, fungi, and bacteria. The antibacterial efficacy of an ethanol-based extract of HLE (Harungana madagascariensis) leaf combined with poly (D, L-lactide-co-glycolide) nanoparticles, i.e., PLG-NPs, was assessed and compared by Moulari et al. Two Gram-positive strains of S. epidermidis and Micrococcus luteus, as well as a Gram-negative strain of Moraxella species, were evaluated ex vivo against one concentration of HLE, while two concentrations of HLE—500 g/mL and 1000 g/mL—were taken into consideration for the in vivo experiment. An artificial contamination technique was used to determine the ex vivo antibacterial characteristics of S. epidermidis CIP 55109. The bacterium was injected into the human skin surface for 12 h. Studies conducted in vitro demonstrated that both formulations totally inhibited the growth of all tested bacterial strains. Four hours after artificial contamination, ex vivo testing revealed that the HLE-PLG-NPs had more antibacterial properties than the HLE solution. Incorporating extracts into polymeric nanoparticles led to better results. The thin-layer chromatography study showed peaks of only two compounds in the case of nanoparticles, demonstrating greater efficacy by loading in the form of a nanocarrier system. The main anti-bacterial activity was due to presence of the flavonoid heteroside [14,91].
Sun and coworkers examined the aqueous solubility, chemical stability, resolution of the epidermal barrier, and in vivo anti-psoriatic activity of curcumin in PLGA (polylactic-co-glycolic acid) nanoparticles. The results show that PLGA nanoparticles distribute and safeguard curcumin during the delivery procedure and enable it to reach the dermis. Therapeutic benefits are influenced by sustained medication release and the compatibility of skin and skin layer penetration. Better therapeutic benefits are demonstrated with the incorporation of curcumin into PLGA nanoparticles, showing sustained medication release, compatibility of the skin, and skin layer penetration [92]. In order to target heat shock protein 70-1, Raghuwanshi and coworkers employed the flower extract of Woodfordia fructicosa heat shock protein 70-1, which has the potential to be inhibited in the therapy of psoriasis. The authors developed Woodfordia fructicosa extract-based biogenic gold nanoparticles containing ellagic acid, quercetin, and myricetin as the main therapeutic components and came to the conclusion that the resulting biologically produced nanostructured formulation would be an effective substitute for treating psoriasis. The results depicted the targeted release of nanoparticles as compared to conventional formulation [93,94].
Lee et al. created an siRNA delivery system based on poly lactic-co-glycolic acid nanoparticles and paired it with a functional laser to enhance the absorption of skin for topical psoriasis treatment. The ability of the nanocarriers to reduce IL-6 expression was demonstrated by their low cytotoxicity and simple cellular absorption. The nanoformulation that included a cationic nature surfactant for ion coupling with siRNA was successful in knocking down IL-6 in keratinocytes and macrophages with 66% and 77% efficiency, respectively. The lasers improved the naked siRNA’s permeability by 3.7–5.0 times. The combination of the laser and nanosystem reduced epidermal hyperplasia and macrophage infiltration, according to the histological analysis. Naked siRNA distribution that was passive or aided by laser had less success at reducing dermatitis. In mice, a topical administration of fractional laser-assisted nanoparticles caused a 56% decrease in IL-6. The study depicts that the efficacy of SiRNA increased when loaded into nanoparticles, but were found to show a cytotoxic effect in the naked form [95].
Lin et al. developed nanocarriers of polylactic-co-glycolic acid containing dictamnine. The results showed that the nanocarrier system penetrated the dermal layer more effectively than bare dictamnine, and it also reduced in vivo inflammatory cytokine expression and the symptoms of dermatitis. The formulation enhanced the anti-inflammatory potential of dictamnine by providing prolonged release with greater penetration [96]. Other research-based evidence for herbal nanoformulation using polymeric nanoparticles is summarized in Table 3.
Table 3.
Herbal formulations based on polymeric nanoparticles for skin diseases.
| Plants | Approaches | Techniques | Skin Disease | Types of Study | Outcomes | Ref. |
|---|---|---|---|---|---|---|
| Thespesia populnea | Nanoparticles | Aqueous and methanolic extraction methods | Skin infection |
|
|
[97] |
|
Alpinia calcarata (diterpenoids, flavonoids and phenols) |
Nanoparticles | Aqueous and methanolic extraction methods | Skin cancer |
|
|
[98] |
|
Fumaria officinalis (stylopine, sanguinarine) |
Nanoparticles | Ionotropic gelation method | Wound healing |
|
|
[99] |
| Praecitrullus fistulosus | Silver nanoparticles | Solvent casting method | Wound healing |
|
|
[100] |
|
Moringa oleifera (phenolic compounds and flavonoids) |
ZnO nanoparticles | Sonicate method | Anti-acne |
|
|
[101] |
|
Fragaria ananassa (flavonols, flavan-3-ols, anthocyanins, hydrolyzable tannins) |
Copper nanoparticles | ---- | Skin wounds |
|
|
[102] |
|
Ximenia americana L. (rutin, epicatechin, catechin, myricetin) |
Silver nanoparticles | Solvent casting method | Wound healing |
|
|
[103] |
5.2. Solid Lipid Nanoparticles Nanostructured Lipid Carriers (NLCs)
In order to assess the formulation’s viability as a dermal delivery system, Guo et al. added quercetin to NLCs (QU-NLCs). The formulation was created utilizing the method of emulsion evaporation–solidification at lower temperatures and includes quercetin, stearic acid, glyceryl monostearate, and soy lecithin. The mean size of the nanoparticles was 215.2 nm, and their average entrapment effectiveness was 89.95% ± 0.16%. They were spherically formed. As a result, the inclusion was successful in promoting quercetin penetration, increasing the amount of quercetin maintained in the dermis and epidermis, and enhancing the flavonoid’s anti-inflammatory and antioxidant activities. Further evidence from this study showed that NLCs have excellent dermal delivery potential, targeting capability, and a delayed release [14,104].
Agrawal et al. formulated nanostructured lipid carriers of capsaicin derived from Capsicum annum for treating psoriasis. In the case of psoriasis, NLCs exhibit increased skin permeation through tough and hyperproliferative skin. Since no skin irritation symptoms have been noticed, the scientists hypothesized that both types of lipid nanoparticles would be suitable for cutaneous administration [105,106].
Recently, Montenegro and colleagues suggested using nano-encapsulated rosemary essential oil to increase skin hydration and elasticity. After being loaded into lipid nanoparticles and added to Carbopol hydrophilic gels, an essential oil with well-known antibacterial, antioxidant, wound healing, and hydration capabilities was used on human volunteers. Cetyl palmitate served as the solid component of the nanoparticles, and rosemary essential oil served as the liquid component, creating nanostructured lipid carriers as a result. Skin hydration and elasticity changes were seen after the application of rosemary essential oil combined with nanostructured gel for a week. In comparison to ordinary gels, nanostructured gels caused better skin hydration and elasticity. In the event of skin dehydration, the researchers have proposed the use of a nanostructured gel containing rosemary essential oil [107].
The effectiveness of NLC containing thymol as a topical vehicle for the treatment of skin inflammation and wound healing has been examined by Pivetta and colleagues. Since the produced gel revealed an anti-inflammatory effect in two different animal models, it proved suitable for the management of inflammatory skin conditions. Additionally, the imiquimod-induced psoriasis mouse model’s healing was enhanced by the thymol-containing nanostructured gel [108].
Eugenol-loaded SLN was created, manufactured, and defined by Garg and Singh. The integration of SLN into a Carbopol hydrogel produced a nanostructured vehicle that may be used to administer SLN topically. In comparison to a medicinal oil solution, a greater eugenol accumulation was seen in the epidermis. In addition, compared to an ordinary gel or untreated skin, an occlusion investigation showed that human cadaver skin was more hydrated after the application of the nanostructured gel. The scientists have proposed using a nanostructured gel that contains eugenol for the treatment of cutaneous fungal infections [109,110].
The different studies performed by researchers using NLCs or SLNs of herbal drugs showed that the NLC or SLN preparations had better potential than their traditional formulations. Moreover, it can be concluded that formulating NLCs or SLNs and loading them into gel could provide enhanced penetration, prolonged release, and better efficacy.
5.3. Ethosomes
The ethosomes of curcumin from Curcuma longa were formulated in a study using hyaluronic acid for treating psoriasis. The results demonstrated a decrease in drug leakage as well as an improved penetration and retention of curcumin. Similarly, ethosomes of thymoquinone, an anti-psoriatic molecule derived from Nigella sativa, showed positive outcomes for psoriasis treatment with enhanced solubility and penetration [106,111]. In a study by Sun and coworkers, which was discussed in the section on polymeric nanoparticles, the curcumin nanoparticles enhanced penetration and provided sustained release, while the formulation of ethosomes of curcumin demonstrated enhanced solubility and decreased leakage of the drug along with greater and prolonged penetration.
In order to obtain lycopene-rich extracts from tomatoes, Ascenso and colleagues developed their dispersion. As bilayer softeners, the dispersions contained Tween 80 with soybean phosphatidylcholine for transferosomes and ethanol for the ethosomes. In particular, the skin permeation and retention investigation showed that ethosomes containing lycopene were retained in the skin for a longer time, whereas confocal microscopy images showed that transferosomes containing fluorescent rhodamine were taken up by HaCat cells. Lycopene-containing vesicles were applied to an ear edema model induced by anthralin to examine their ability to penetrate inflamed skin. In comparison to the simple lycopene extract, transferosomes and ethosomes were both able to lower the levels of inflammatory cell infiltration and epidermal hyperplasia. Vesicles possibly improved lycopene retention in the skin by enhancing carrier-mediated lycopene skin delivery, which probably improved skin retention and increased the therapeutic impact [110,112].
Vitamins A, E, and C were used in conjunction to create ethosomes by Koli and Lin. Due to the synergistic effects of all vitamins, as well as their distribution to the innermost layers of the skin, the prepared formulation demonstrated stronger antioxidant properties in comparison to the usual drug delivery system [113,114].
5.4. Liposomes
Lin et al. investigated camptothecin-containing liposomes coupled to α-melanocyte-stimulating hormone (α-MSH) to preferentially target melanoma cells. The camptothecin release may be managed by the liposomes, which were based on stearylamine, phosphatidylcholine, and cholesterol. In comparison to non-targeted liposomes and free camptothecin, greater cell endocytosis was seen in the α-MSH liposomes using fluorescent microscopy. Notably, the scientists showed that α-MSH liposomes were primarily internalized in the cytoplasm. The capacity of α-MSH liposomes to target tumors showed that they may be able to increase the effectiveness of camptothecin against melanoma [110,115]. The study depicts the targeted release of camptothecin-loaded liposomes providing better efficacy against melanoma as compared to the non-targeted formulation.
Using a murine model, researchers examined the anti-inflammation characteristics of liposomes intended for the topical application of curcumin and quercetin. They found that adding penetration enhancers to liposomes greatly increased these characteristics while also postponing the development of TPA-induced (12-O-tetradecanoylphorbol-13-acetate) wounds [114,116].
The evaluation of the usnic acid-loaded liposomes in gelatin by Rabelo et al., led to favorable findings for the treatment of wounds. According to these findings, the liposome membrane plays a significant role in controlling second-grade infections in the pig model. Additionally, the liposomal membrane-treated group showed deposition on cellularized granulation tissue, which, in contrast to one of the commercial products, increased the maturation of granulation tissue and mended the wounds (Figure 4) [117].
Figure 4.
Macroscopy of the wound treatment at 8, 18, and 30 days with silver sulfadiazine (SDZ), DuoDerme® (GDU), and a gelatin layer loaded with usnic acid liposomes (UAL). Adapted with permission from [117].
The above two studies done by researchers for the treatment of wounds demonstrate that the application of nanotechnology in the formulation increased their therapeutic effect and penetration and also prevented the development of other induced wounds in the future.
5.5. Nanoemulsions
Mahdi et al. created nanoemulsions that included Phyllanthus urinaria extract using esters made from palm kernel oil. These showed DPPH radical neutralizing action, the neutralization of reactive oxygen species, and the prevention of oxidative damage brought on by UV light when they were tested for their anti-aging effects due to the presence of polyphenols in the extract (gallic acid, geraniin, and ellagic acid) [114,118]. The formulation of nano emulsion-based cream increased the antioxidant potential activity along with permeation, providing a better anti-aging effect. The partitioning of the drug into two phases enhanced the solubility and drug release.
Vater et al. formulated nano emulsions of spruce balm and birch bark extract using lecithin for wound healing properties. The nanoemulsions loaded with either birch bark or spruce balm extract resulted in greater fibroblast and keratinocyte cell viability rates. After the treatment, there was increased keratinocyte and fibroblast proliferative activity, which is necessary for wound repair. Our research suggests that nanoemulsions of herbal extracts are remarkable wound-healing medications, and their use in lecithin-based nanoemulsions may be a useful wound-care therapy [119]. Kreutz et al. formulated a hydroxyethyl cellulose hydrogel of the nanoemulsion of Aniba canelilla to evaluate its anti-inflammatory activity on the skin. Aniba canelilla essential oil-containing hydroxyethyl cellulose-hydrogel thickened nano emulsion appeared to be an effective formulation because it demonstrated a clear anti-inflammatory potential with decreased myeloperoxidase activity. It acted by reducing polymorphonuclear leukocyte movement, decreasing edema and reducing the release of inflammatory mediators. 1-nitro-2-phenylethane and methyleugenol were found to be the components of essential oils responsible for activity [120].
Luu et al. through the use of an oil-in-water emulsion, formulated a topical cream based on a nanoformulation of Chromolaena odorata leaves with a fraction of ethyl acetate extract. The cream was formulated by loading active ingredients (flavonoids and tannins) in pluronic micelles. The formulated cream demonstrated high homogeneity, a sufficient pH level, the sustained release of phenolics, and satisfactory stability for prolonged storage. When DPPH was incubated with cream for 15 min to 5 h, the amount of free radical scavengers decreased from 10% to 80%. Additionally, the cream encouraged the movement of fibroblast cells through the appropriate release of phenolic chemicals, but the extract in the same quantity caused toxic effects and prevented wound closure [121]. The results of the formulated nano-emulsion-based topical cream are depicted in Figure 5.
Figure 5.
Nanoparticle-loaded cream of Chromolaena odorata for the treatment of wounds by controlling TPC (total phenolic compound) release, enhancing fibroblast migration. Adapted with permission from [121].
Chlorogenic acid nanoemulsions were developed by Budama-klinic et al. for hyperpigmentation. The in vitro cell survival result, the Ames test result, and the formulation’s non-mutagenicity were used to demonstrate that the formulation was suitable for transdermal application. The finished chlorogenic acid nano emulsion formulation was found to decrease the activity of tyrosinase and melanogenesis during efficacy tests on melanoma B16 cells [122]. The therapeutic efficacy of chlorogenic acid is limited due to poor penetration, which was improved by formulating its nanoformulation, providing greater intradermal delivery. The prepared nanoemulsion increased the efficacy and safety of chlorogenic acid in hyperpigmentation. The other emulsion-based nanoformulations are detailed in Table 4.
Table 4.
Herbal formulations based on nanoemulsions for skin diseases.
| Plants | Approaches | Techniques | Skin Disease | Types of Study | Outcomes | Ref. |
|---|---|---|---|---|---|---|
| Garlic (dialkyl polysulphides) and ginger (zingiberene, curcumene, and β-bisabolene) |
Nanoemulsion | Ultrasonic cavitation | Skin wound healing |
|
|
[123] |
|
Chromolaena odorata
(flavanoids, tannins) |
Oil-in-water emulsion Pluronic micelles |
----- | Burn wound healing |
|
|
[121] |
| Chlorogenic acid | Nanoemulsion | Ultrasonic homogenization method. | Hyperpigmentation disorder |
|
|
[122] |
|
Aniba canelilla (Kunth) (1-nitro-2-phenylethane and methyleugenol) |
Nanoemulsion | ---- | Skin disorders |
|
|
[120] |
|
Alpinia galanga extract (1-acetoxychavicol acetate) |
Nanoemulsion | ---- | Psoriasis |
|
|
[124] |
|
Brosimum Gaudichaudii
(furanocoumarins bergapten and psoralen) |
Microemulsions | ---- | Vitiligo |
|
|
[125] |
| Linseed oil | Nanoemulsion | Ultrasonic emulsification method | Atopic dermatitis |
|
|
[126] |
5.6. Niosomes
In order to create a topical gel, Priprem et al. created niosomes that encapsulated a concentrate of Zingiber cassumunar. Improved chemical stability and skin permeability were seen. The anti-inflammatory effects due to the presence of active compound(E)-4-(3′,4′-dimethoxyphenyl) but-3-en-1-ol were comparable to the ones of commercially available hydrocortisone cream and Piroxicam gel [127]. It can be concluded that in comparison to steroids and other conventional gel formulations, the noisome-loaded gel of Zingiber cassumunar provided better stability, increased anti-inflammatory effect, and enhanced permeation.
In different vesicular forms, including ethosomes, liposomes, and transferosomes, an alcohol-based extract of Curcuma longa was produced. The most effective cream was the one filled with Curcuma longa transferosomal extract containing curcumin; it was followed, in order of effectiveness, by ethosomal, liposomal, and Curcuma longa extract creams. When these forms were coupled with the cream, the skin damaged by UV radiation showed improved recovery [114,128].
Meng et al. created niosomes of Celastrol incorporating Span 20, 60, and cholesterol by a thin-film hydration method. For prolonging the effects of the topical medication on the skin and preserving subcutaneous hydration, the hydrogel was utilized as a core carrier. In comparison to the Celastrol hydrogel, the drug concentration of the Celastrol niosomal gel was shown to be about 13 times higher in the skin in an in vitro penetration assay (Figure 6). Erythema and scaling on the lateral skin were further improved [129].
Figure 6.
(A) Images of dorsal skin of mice after administration of Imiquimod (IMQ). (B) Staining with H&E demonstrating the changes in inner skin after the application of tacrolimus ointment, blank niosomal gel, and Celastrol gel (positive control). (C) An enlarged view of the IMQ-treated group (right) and normal (left) groups. Adapted with permission from [129].
5.7. Nanofibers
Nanofibers operate as a sheet that enhances the tissues since they are made of indestructible chains of polymers of both synthetic and natural substances [130]. Emodin, an anthraquinone compound that can be found in the rhizomes of Rheum officinale L., is widely used for wound healing because of its antibacterial and anti-inflammatory properties. When applied to severe skin injuries, it had a beneficial outcome [131]. In comparison to the pure substance, the emodin nanofibers in polyvinylpyrrolidone were non-toxic, anti-allergenic, bioactive, and disintegrated quickly. Re-epithelization was demonstrated to have taken place at the site of injury, accelerating the healing process [132]. Emodin was added to cellulose acetate nanostructure fibers to bring the collagen content of human cells to 100%. Through the incorporation of herbal components into cellulose acetate nanofibers, wound healing is accelerated by the use of biological nanomaterials [133]. Chitosan nanofibers that had been loaded with bromelain led to successful wound healing. Positive effects were seen for second-degree burns. When compared to chitosan 4% w/v bromelain, the chitosan 2% w/v bromelain produced better physiochemical outcomes and was successful in minimizing burn-induced damage [133,134]. The different nanofiber-based formulations of emodin discussed above show better outcomes than those of its pure form. The loading of emodin in nanofibers increased wound healing activity and decreased the associated side effects. Nanofiber-based herbal nanoformulations for skin diseases are listed in Table 5.
Table 5.
Herbal formulations based on nanofibers for skin diseases.
| Plants | Approaches | Techniques | Skin Disease | Types of Study | Outcomes | Ref. |
|---|---|---|---|---|---|---|
|
Malva sylvestris (mucilage and flavonoids) |
Nanofibers | Maceration method | Wound dressings |
|
|
[135] |
|
Ananas comosus (bromelain) |
Nanofibers | Electrospinning method | Wound healing |
|
|
[136] |
5.8. Hydrogels and Nanogels
Hydrogels made of sodium alginate and polyvinyl alcohol were created by Esposito et al. as a novel delivery mechanism, primarily to treat inflammation and skin aging. A hydrogel that was loaded with quercetin showed a respectable swelling and viscosity profile. The obtained outcomes demonstrated that a quercetin-loaded hydrogel reduces the rate of infiltration and increases the penetration and duration of the drug–skin interface, consequently enhancing the action of quercetin [137]. Jangde et al. used liposomes loaded with quercetin to construct a multiphase hydrogel system and assessed its structure, swelling index, water vapor transfer rate, stability evaluation, hemocompatibility, and in vitro and in vivo testing (Figure 7). The results showed that the hydrogel considerably accelerated the process of wound closure and enhanced wound healing applications [138].
Figure 7.
Illustration depicting images of animal skin: (a) untreated; (b) standard treatment; and (c) quercetin-loaded liposome treatment. Adapted with permission from [138].
Bagde et al. produced a topical nanogel loaded with quercetin and TiO2, and they used the Box–Behnken design to optimize the low and high concentrations of quercetin nanocrystals. Over 70% of the medication was released within 24 h using combined nanogels. The new combination of quercetin and titanium dioxide nanogel inhibits the inflammatory and cell cycle pathways, as demonstrated by the in vivo animal model. Overall findings, therefore, indicated that the proposed nanoformulation could enhance skin deposition and can be used as an innovative pharmaceutical delivery strategy against UVB-induced skin cancer [139]. The different formulations of quercetin formulated by researchers, either as a hydrogel or nanogel, show their improved efficacy in the treatment of skin problems. The formulation by Jangde et al. depicts increased bioavailability along with faster wound healing in comparison to other formulations. The other nanogel-based herbal nanoformulations are summarized in Table 6.
Table 6.
Herbal formulations based on nanogels for skin diseases.
| Plants | Approaches | Techniques | Skin Disease | Types of Study | Outcomes | Ref. |
|---|---|---|---|---|---|---|
|
Calotropis procera (flavones, tannins, and alkaloids) |
Nanogel | Diffusion technique | Skin acne and skin cancer |
|
|
[140] |
| Sesame oil (lignans and sesamol) |
Hydrogel | --------- | Skin hyperpigmentation |
|
|
[141] |
|
Smilax china and Salix alba (quercetin) |
Nano lipid carrier-based gel | Sonication method | Psoriasis |
|
|
[142] |
5.9. Others
The nanocomplexes were created by Nirmal et al. by loading gold nanorods and isatin into a polylactic-co-glycolic acid matrix. This combination has been found to have synergistic anti-psoriatic activity. The combined nanocomplexes with near-infrared prevented epidermal hyperplasia and neutrophil infiltration, according to the in vivo psoriasis murine model. After photothermal treatment, the elevated cytokines in the area of injury could return to their baseline levels. For at least five days, the subcutaneous nanocomplexes persisted in the skin. The skin and liver of normal mice had no harm from the nanocomposites [143]. A 6-Gingerol-loaded self-nano emulsifying drug delivery system as a nano emulgel was developed by Ahmad et al. in order to enhance topical administration through improved solubility and skin penetration for the control of wound healing and anti-inflammatory processes. In order to improve skin permeability, a nano emulgel was utilized, and the dermatokinetic results revealed a substantial improvement in the treated skin as compared to a conventional gel. It increased skin permeability and solubility. The topical application of the nano emulgel demonstrated improved wound healing and anti-inflammatory effects [144].
Amer et al. formulated aspasomes (quercetin loaded in nanovesicles of vitamin C) for the treatment of acne. Quercetin’s antioxidant activity was preserved by aspasomes, which also demonstrated a markedly greater antibacterial impact towards Propionibacterium than quercetin alone and was safe on fibroblastic cells. In the clinical study of 20 acne patients, quercetin aspasomes showed decreased percentages of 77.9%, 11.8%, and 55.3% for inflammatory lesions, comedones, and total lesions, respectively [145].
Other nanoformulations for the treatment of various skin diseases are outlined in Table 7.
Table 7.
Herbal nano formulations for skin diseases.
| Plants | Approaches | Techniques | Skin Disease | Types of Study | Outcomes | Ref. |
|---|---|---|---|---|---|---|
|
Zataria multiflora (carvacrol, thymol) |
Nanostructured lipid carriers | Ultrasonic probe | Cutaneous dermatophytosis |
|
|
[146] |
| Aloe vera | Nanoflowers | ----- | Wound healing |
|
|
[147] |
|
Sideroxylon mascatense (quercetine, berberine, and myricetin) |
Synthetic gel | --- | Wound healing |
|
|
[148] |
|
Phyllanthus emblica L. (sinapic and ferulic acid) |
Topical gel | Rotary Evaporator |
Anti-aging |
|
|
[149] |
|
Olea europaea and Spirodela polyrhiza (oleuropein, luteolin, and apigenin) |
Topical oil | ---- | Atopic dermatitis |
|
|
[150] |
| Berberine | Gel-core oleosomes | Modified ethanol injection technique | Vitiligo |
|
|
[151] |
| Azadirachta indica | Nanocapsule | Sonochemical method | Bacterial diseases |
|
|
[152] |
The different studies discussed above show the potential of herbal nano formulations in treating skin diseases and the increased popularity of herbal products. The application of nanotechnology in the development of various formulations will help in effectively curing various life-threatening skin disorders by providing targeted and prolonged effect with decreased side effects.
6. Patents
The different patents published on herbal nanoformulations for the treatment of skin diseases in the last 15 years are discussed in Table 8.
Table 8.
Patents on herbal formulations for skin diseases.
| Title | Patent No. | Publication Date | Current Assignee | Ref. |
|---|---|---|---|---|
| Herbal nanoformulations for treating psoriasis and other skin conditions | WO2017172648A1 | 5 October 2017 | Sirbal Ltd. | [153] |
| Topical nano liposome formulation, including extracted purified herbal mixture whitening cosmetics using this formulation | KR20050117958A | 15 December 2005 | SK Chemicals Co. Ltd. | [154] |
| Cosmetic composition for preventing skin aging comprising nano liposome of Torilis japonica fruit | KR100733334B1 | 29 June 2007 | KT&G Co., Ltd., Korea Ginseng Corporation Co., Ltd. | [155] |
| Nano-sponge loaded topical gel of Curcumin and babchi oil for enhanced treatment of psoriasis. | DE202023101592U1 | 2 May 2023 | Individual | [156] |
| Anti-acne nano preparation, gel composition, and preparation method thereof | CN115634165A | 24 January 2023 | Jiangsu Jicui New Pharmaceutical Preparation Technology Research Institute Co. Ltd. | [157] |
| Compound traditional Chinese medicine nano gel for treating dermatophytosis and tinea pedis and preparation method thereof | CN115300576A | 8 November 2022 | Changsha Medical University | [158] |
| Natural gel preparation of traditional Chinese medicine compound extract coated by nanoparticles, preparation method, and application thereof | CN115337282A | 15 November 2022 | Individual | [159] |
| Rigida pine bark extract with improved stability encapsulated nanoparticles and manufacturing method, a cosmetic composition comprising the same | KR20220152865A | 17 November 2022 | Kim Yu-mi and Jang Ki-hyeon | [160] |
| In-situ Gel Extraction, Formulation and Evaluation for Treating Fungal Skin Infection | AU2021107001A4 | 16 December 2021 | Bhati Priyanka Ms. Khatoon Rizwana Mrs. Kumar Amrish Dr. Rahate Kalpana Dr. Sharma Akhil Dr. Sharma Shaweta Dr. Singh Veena Dr. Singh Vijay Dr. Sudha Anjali Ms | [161] |
| Novel Punica granatum Extracts-Zinc oxide Nanoparticles and its use | KR20220117942A | 25 September 2023 | Yeungnam University Industry-Academic Cooperation Foundation | [162] |
| Natural polysaccharide Nano-hydrogel mask based on hollow nanoparticles preparation method thereof | CN114010555A | 8 February 2022 | Luoyang Normal University | [163] |
| Berberis extract nanoformulation and process of preparation thereof | WO2022168124A1 | 11 August 2022 | Panjab University, Chandigarh | [164] |
| Nanoparticle system for treating skin diseases and preparation method and preparation thereof | CN113081948A | 9 July 2021 | Anhui University of Traditional Chinese Medicine AHUTCM | [165] |
| Cosmetic preparation for the care and treatment of facial skin | DE202021106363U1 | 15 December 2021 | Jassen GmbH | [166] |
7. Current Challenges and Future Perspectives
Herbal medicine delivery systems using nanoscale technology may enhance biological activity and address problems with plant-based pharmaceuticals. Yet, there are still numerous challenges in this discipline to overcome before implementing clinically sound treatments. One of the biggest challenges in converting this technology into medicines is testing novel ways to control how nanomaterials interact with biological systems. The potential for obtaining multifunctional systems to satisfy various biological and therapeutic requirements, as well as the viability of the increased production of processes that quickly bring creative therapeutic technology to market, are novel obstacles in the design of nanotechnology-based systems for drug delivery. Investigating the targeting effectiveness of nanoparticles and meeting global criteria for their toxicological and biocompatibility are some additional emerging issues. A better method of delivering medications to the target site at a dosage that does not modify the way the disease is currently being treated must be developed. It is obvious that more studies are required to determine the effectiveness, safety, and ideal applications of herbal treatments and establish standards for them. Researchers also need to concentrate on creating biocompatible and biodegradable nanomaterials. Continued research and successful pre-clinical and clinical studies are required to provide better alternatives to conventional formulations. Along with this, the contribution of health professionals and the general public is necessary to increase the acceptance of herbal nanoformulations for various skin diseases all over the world.
8. Conclusions
The data compiled in this research have shown that treating skin diseases with herbal medicines based on nanotechnology is a novel approach. In fact, there are many clinical advantages of applying herbal medicines via nanotechnology systems to the skin. The ability to use a formulation that is entirely biocompatible guarantees the consumer a “green” approach and virtually zero side effects when administered topically. Several nanotechnology-based approaches, such as liposomes and solid lipid nanoparticles, have been recommended for topical administration, indicating their potential in inflammatory phenomena, wound healing, fungus infections, and skin aging. In general, the various investigations presented here have indicated that the topical application of nanosystems provides a longer release and efficacy of the loaded herbal compounds. Regardless, a lot more research needs to be done and addressed to understand more about the interaction of nanosystems with the skin.
Acknowledgments
Priyanka Jurel, Rohitas Deshmukh, and Ranjit Kumar Harwansh are thankful to the GLA University, Mathura, India for providing the necessary facilities to accomplish this work. Akash Garg and Rutvi Agrawal are thankful to the management of the Rajiv Academy for pharmacy, Mathura, India, for providing the necessary facilities to accomplish the paper. Arun Kumar acknowledges the management of Sharda University, Greater Noida for the support provided to carry out this work. Moreover, Ashwini Kumar acknowledges the management of the Manav Rachna International Institute of Research and Studies, Faridabad for the support provided to carry out this work. Moreover, Ajay Guru acknowledges the Department of Cariology, Saveetha Dental Collegeand Hospital, Saveetha University, Chennai, India for the support provided to carry out this work. Moreover, this work was partially supported by University Kebangsaan Malaysia, “Contract No. GGPM-2023-020” for Vinoth Kumaraswamy and CMU Proactive Researcher Scheme (2023), Chiang Mai University, “Contract No. 933/2566” for Sudarshan Singh.
Author Contributions
Conceptualization, R.D.; Validation, R.K.H.; Formal analysis, A.K. (Ashwini Kumar); Investigation, P.J. and R.A.; Resources, A.K. (Arun Kumar); Writing—Review and editing, R.A.; Writing—Original Draft preparation, P.J.; Project administration, A.G. (Ajay Guru), P.J. and R.A.; Supervision, R.D. and R.K.H.; Visualization, A.G. (Ajay Guru) and A.G. (Akash Garg); Funding acquisition, V.K., S.S. and A.K. (Ashwini Kumar). All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Data can be made available on request to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This study was supported via funding from University Kebangsaan Malaysia, GGPM Grant (GGPM-2023-020).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Madison K.C. Barrier function of the skin: “La raison d’être” of the epidermis. J. Investig. Dermatol. 2003;121:231–241. doi: 10.1046/j.1523-1747.2003.12359.x. [DOI] [PubMed] [Google Scholar]
- 2.Proksch E., Brandner J.M., Jensen J.M. The skin: An indispensable barrier. Exp. Dermatol. 2008;17:1063–1072. doi: 10.1111/j.1600-0625.2008.00786.x. [DOI] [PubMed] [Google Scholar]
- 3.Grice E.A., Kong H.H., Conlan S., Deming C.B., Davis J., Young A.C., Bouffard G.G., Blakesley R.W., Murray P.R., Green E.D., et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009;324:1190–1192. doi: 10.1126/science.1171700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tabassum N., Hamdani M. Plants used to treat skin diseases. Pharmacogn. Rev. 2014;8:52–60. doi: 10.4103/0973-7847.125531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan H., Ma Q., Ye L., Piao G. The Traditional Medicine and Modern Medicine from Natural Products. Molecules. 2016;21:559. doi: 10.3390/molecules21050559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones V.A., Patel P.M., Wilson C., Wang H., Ashack K.A. Complementary and alternative medicine treatments for common skin diseases: A systematic review and meta-analysis. JAAD Int. 2021;2:76–93. doi: 10.1016/j.jdin.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saising J., Maneenoon K., Sakulkeo O., Limsuwan S., Götz F., Voravuthikunchai S.P. Ethnomedicinal Plants in Herbal Remedies Used for Treatment of Skin Diseases by Traditional Healers in Songkhla Province, Thailand. Plants. 2022;11:880. doi: 10.3390/plants11070880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atanasov A.G., Waltenberger B., Pferschy-Wenzig E.M., Linder T., Wawrosch C., Uhrin P., Temml V., Wang L., Schwaiger S., Heiss E.H., et al. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015;33:1582–1614. doi: 10.1016/j.biotechadv.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caesar L.K., Cech N.B. Synergy and antagonism in natural product extracts: When 1 + 1 does not equal 2. Nat. Prod. Rep. 2019;36:869–888. doi: 10.1039/C9NP00011A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ansari S.H., Islam F., Sameem M. Influence of nanotechnology on herbal drugs: A Review. J. Adv. Pharm. Technol. Res. 2012;3:142–146. doi: 10.4103/2231-4040.101006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teja P.K., Mithiya J., Kate A.S., Bairwa K., Chauthe S.K. Herbal nanomedicines: Recent advancements, challenges, opportunities and regulatory overview. Phytomedicine. 2022;96:153890. doi: 10.1016/j.phymed.2021.153890. [DOI] [PubMed] [Google Scholar]
- 12.Dewi M.K., Chaerunisaa A.Y., Muhaimin M., Joni I.M. Improved Activity of Herbal Medicines through Nanotechnology. Nanomaterials. 2022;12:4073. doi: 10.3390/nano12224073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yadav A., Ghune M., Jain D. Nano-medicine based drug delivery system. J Adv. Pharm. Educ. Res. 2011;1:201–213. [Google Scholar]
- 14.Bonifácio B.V., Silva P.B., Ramos M.A., Negri K.M., Bauab T.M., Chorilli M. Nanotechnology-based drug delivery systems and herbal medicines: A review. Int. J. Nanomed. 2014;9:1–15. doi: 10.2147/ijn.S52634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawid-Pać R. Medicinal plants used in treatment of inflammatory skin diseases. Postep. Dermatol. Alergol. 2013;30:170–177. doi: 10.5114/pdia.2013.35620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph N., Kumar G.S., Nelliyanil M. Skin diseases and conditions among students of a medical college in southern India. Indian Dermatol. Online J. 2014;5:19–24. doi: 10.4103/2229-5178.126023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunwell P., Rose A. Study of the skin disease spectrum occurring in an Afro-Caribbean population. Int. J. Dermatol. 2003;42:287–289. doi: 10.1046/j.1365-4362.2003.01358.x. [DOI] [PubMed] [Google Scholar]
- 18.Zhang B., Zhou X., Luo Y., Zhang H., Yang H., Ma J., Ma L. Opportunities and Challenges: Classification of Skin Disease Based on Deep Learning. Chin. J. Mech. Eng. 2021;34:112. doi: 10.1186/s10033-021-00629-5. [DOI] [Google Scholar]
- 19.Ahuja A., Gupta J., Gupta R. Miracles of Herbal Phytomedicines in Treatment of Skin Disorders: Natural Healthcare Perspective. Infect. Disord. Drug Targets. 2021;21:328–338. doi: 10.2174/1871526520666200622142710. [DOI] [PubMed] [Google Scholar]
- 20.Ramdass P., Mullick S., Farber H.F. Viral Skin Diseases. Prim. Care. 2015;42:517–567. doi: 10.1016/j.pop.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Schalka S. New data on hyperpigmentation disorders. J. Eur. Acad. Dermatol. Venereol. JEADV. 2017;31((Suppl. S5)):18–21. doi: 10.1111/jdv.14411. [DOI] [PubMed] [Google Scholar]
- 22.Abdlaty R., Hayward J., Farrell T., Fang Q. Skin erythema and pigmentation: A review of optical assessment techniques. Photodiagnosis Photodyn. Ther. 2021;33:102127. doi: 10.1016/j.pdpdt.2020.102127. [DOI] [PubMed] [Google Scholar]
- 23.Kuzmina I., Diebele I., Spigulis J., Valeine L., Berzina A., Abelite A. Contact and contactless diffuse reflectance spectroscopy: Potential for recovery monitoring of vascular lesions after intense pulsed light treatment. J. Biomed. Opt. 2011;16:040505. doi: 10.1117/1.3569119. [DOI] [PubMed] [Google Scholar]
- 24.Pacheco A.G.C., Krohling R.A. The impact of patient clinical information on automated skin cancer detection. Comput. Biol. Med. 2020;116:103545. doi: 10.1016/j.compbiomed.2019.103545. [DOI] [PubMed] [Google Scholar]
- 25.Sharma R.R., Deep A., Abdullah S.T. Herbal products as skincare therapeutic agents against ultraviolet radiation-induced skin disorders. J. Ayurveda Integr. Med. 2022;13:100500. doi: 10.1016/j.jaim.2021.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karlsson I., Hillerström L., Stenfeldt A.L., Mårtensson J., Börje A. Photodegradation of dibenzoylmethanes: Potential cause of photocontact allergy to sunscreens. Chem. Res. Toxicol. 2009;22:1881–1892. doi: 10.1021/tx900284e. [DOI] [PubMed] [Google Scholar]
- 27.Ahmad Khan M.S., Ahmad I. Chapter 1—Herbal Medicine: Current Trends and Future Prospects. In: Ahmad Khan M.S., Ahmad I., Chattopadhyay D., editors. New Look to Phytomedicine. Academic Press; Cambridge, MA, USA: 2019. pp. 3–13. [DOI] [Google Scholar]
- 28.Costa E.M.M.d.B., Barbosa A.S., Arruda T.A.d., Oliveira P.T.d., Dametto F.R., Carvalho R.A.d., Melo M.d.D. Estudo in vitro da ação antimicrobiana de extratos de plantas contra Enterococcus faecalis. J. Bras. Patol. Med. Lab. 2010;46:1–15. doi: 10.1590/S1676-24442010000300004. [DOI] [Google Scholar]
- 29.Vieira B.L., Lim N.R., Lohman M.E., Lio P.A. Complementary and Alternative Medicine for Atopic Dermatitis: An Evidence-Based Review. Am. J. Clin. Dermatol. 2016;17:557–581. doi: 10.1007/s40257-016-0209-1. [DOI] [PubMed] [Google Scholar]
- 30.Lee Y.M., Hirota S., Jippo-Kanemoto T., Kim H.R., Shin T.Y., Yeom Y., Lee K.K., Kitamura Y., Nomura S., Kim H.M. Inhibition of histamine synthesis by glycyrrhetinic acid in mast cells cocultured with Swiss 3T3 fibroblasts. Int. Arch. Allergy Immunol. 1996;110:272–277. doi: 10.1159/000237298. [DOI] [PubMed] [Google Scholar]
- 31.Farrukh M.R., Nissar U.A., Kaiser P.J., Afnan Q., Sharma P.R., Bhushan S., Tasduq S.A. Glycyrrhizic acid (GA) inhibits reactive oxygen Species mediated photodamage by blocking ER stress and MAPK pathway in UV-B irradiated human skin fibroblasts. J. Photochem. Photobiol. B Biol. 2015;148:351–357. doi: 10.1016/j.jphotobiol.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 32.Song N.R., Kim J.E., Park J.S., Kim J.R., Kang H., Lee E., Kang Y.G., Son J.E., Seo S.G., Heo Y.S., et al. Licochalcone A, a polyphenol present in licorice, suppresses UV-induced COX-2 expression by targeting PI3K, MEK1, and B-Raf. Int. J. Mol. Sci. 2015;16:4453–4470. doi: 10.3390/ijms16034453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdullah Z.W., Dong Y., Davies I.J., Barbhuiya S. PVA, PVA Blends, and Their Nanocomposites for Biodegradable Packaging Application. Polym.-Plast. Technol. Eng. 2017;56:1307–1344. doi: 10.1080/03602559.2016.1275684. [DOI] [Google Scholar]
- 34.Angelova-Fischer I., Rippke F., Richter D., Filbry A., Arrowitz C., Weber T., Fischer T.W., Zillikens D. Stand-alone Emollient Treatment Reduces Flares After Discontinuation of Topical Steroid Treatment in Atopic Dermatitis: A Double-blind, Randomized, Vehicle-controlled, Left-right Comparison Study. Acta Derm.-Venereol. 2018;98:517–523. doi: 10.2340/00015555-2882. [DOI] [PubMed] [Google Scholar]
- 35.Seiwerth J., Tasiopoulou G., Hoffmann J., Wölfle U., Schwabe K., Quirin K.W., Schempp C.M. Anti-Inflammatory Effect of a Novel Topical Herbal Composition (VEL-091604) Consisting of Gentian Root, Licorice Root and Willow Bark Extract. Planta Medica. 2019;85:608–614. doi: 10.1055/a-0835-6806. [DOI] [PubMed] [Google Scholar]
- 36.Hoffmann J., Gendrisch F., Schempp C.M., Wölfle U. New Herbal Biomedicines for the Topical Treatment of Dermatological Disorders. Biomedicines. 2020;8:27. doi: 10.3390/biomedicines8020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wölfle U., Hoffmann J., Haarhaus B., Rao Mittapalli V., Schempp C.M. Anti-inflammatory and vasoconstrictive properties of Potentilla erecta—A traditional medicinal plant from the northern hemisphere. J. Ethnopharmacol. 2017;204:86–94. doi: 10.1016/j.jep.2017.03.058. [DOI] [PubMed] [Google Scholar]
- 38.van de Kerkhof P.C., van der Valk P.G., Swinkels O.Q., Kucharekova M., de Rie M.A., de Vries H.J., Damstra R., Oranje A.P., de Waard-van der Spek F.B., van Neer P., et al. A comparison of twice-daily calcipotriol ointment with once-daily short-contact dithranol cream therapy: A randomized controlled trial of supervised treatment of psoriasis vulgaris in a day-care setting. Br. J. Dermatol. 2006;155:800–807. doi: 10.1111/j.1365-2133.2006.07393.x. [DOI] [PubMed] [Google Scholar]
- 39.Lin Y.K., See L.C., Huang Y.H., Chi C.C., Hui R.C. Comparison of indirubin concentrations in indigo naturalis ointment for psoriasis treatment: A randomized, double-blind, dosage-controlled trial. Br. J. Dermatol. 2018;178:124–131. doi: 10.1111/bjd.15894. [DOI] [PubMed] [Google Scholar]
- 40.Antiga E., Bonciolini V., Volpi W., Del Bianco E., Caproni M. Oral Curcumin (Meriva) Is Effective as an Adjuvant Treatment and Is Able to Reduce IL-22 Serum Levels in Patients with Psoriasis Vulgaris. BioMed Res. Int. 2015;2015:283634. doi: 10.1155/2015/283634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heng M.C., Song M.K., Harker J., Heng M.K. Drug-induced suppression of phosphorylase kinase activity correlates with resolution of psoriasis as assessed by clinical, histological and immunohistochemical parameters. Br. J. Dermatol. 2000;143:937–949. doi: 10.1046/j.1365-2133.2000.03767.x. [DOI] [PubMed] [Google Scholar]
- 42.Varma S.R., Sivaprakasam T.O., Mishra A., Prabhu S., Rafiq M., Rangesh P. Imiquimod-induced psoriasis-like inflammation in differentiated Human keratinocytes: Its evaluation using curcumin. Eur. J. Pharmacol. 2017;813:33–41. doi: 10.1016/j.ejphar.2017.07.040. [DOI] [PubMed] [Google Scholar]
- 43.Muhammed M., Nagabhushanam K., Sankaran N., Sood R.S., Karri S. Clinical evaluation of AKBBA in the management of psoriasis. Clin. Dermatol. 2014;2:17–24. doi: 10.11138/cderm/2014.2.1.017. [DOI] [Google Scholar]
- 44.Fukuchi K., Okudaira N., Adachi K., Odai-Ide R., Watanabe S., Ohno H., Yamamoto M., Kanamoto T., Terakubo S., Nakashima H., et al. Antiviral and Antitumor Activity of Licorice Root Extracts. In Vivo. 2016;30:777–785. doi: 10.21873/invivo.10994. [DOI] [PubMed] [Google Scholar]
- 45.Goswami D., Mahapatra A.D., Banerjee S., Kar A., Ojha D., Mukherjee P.K., Chattopadhyay D. Boswellia serrata oleo-gum-resin and β-boswellic acid inhibits HSV-1 infection in vitro through modulation of NF-кB and p38 MAP kinase signaling. Phytomed. Int. J. Phytother. Phytopharm. 2018;51:94–103. doi: 10.1016/j.phymed.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 46.Koytchev R., Alken R.G., Dundarov S. Balm mint extract (Lo-701) for topical treatment of recurring herpes labialis. Phytomed. Int. J. Phytother. Phytopharm. 1999;6:225–230. doi: 10.1016/S0944-7113(99)80013-0. [DOI] [PubMed] [Google Scholar]
- 47.Pazyar N., Yaghoobi R., Rafiee E., Mehrabian A., Feily A. Skin wound healing and phytomedicine: A review. Skin Pharmacol. Physiol. 2014;27:303–310. doi: 10.1159/000357477. [DOI] [PubMed] [Google Scholar]
- 48.Ebeling S., Naumann K., Pollok S., Wardecki T., Vidal Y.S.S., Nascimento J.M., Boerries M., Schmidt G., Brandner J.M., Merfort I. From a traditional medicinal plant to a rational drug: Understanding the clinically proven wound healing efficacy of birch bark extract. PLoS ONE. 2014;9:e86147. doi: 10.1371/journal.pone.0086147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Metelmann H.R., Brandner J.M., Schumann H., Bross F., Fimmers R., Böttger K., Scheffler A., Podmelle F. Accelerated reepithelialization by triterpenes: Proof of concept in the healing of surgical skin lesions. Skin Pharmacol. Physiol. 2015;28:1–11. doi: 10.1159/000357501. [DOI] [PubMed] [Google Scholar]
- 50.Frew Q., Rennekampff H.O., Dziewulski P., Moiemen N., Zahn T., Hartmann B. Betulin wound gel accelerated healing of superficial partial thickness burns: Results of a randomized, intra-individually controlled, phase III trial with 12-months follow-up. Burn. J. Int. Soc. Burn Inj. 2019;45:876–890. doi: 10.1016/j.burns.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 51.Barret J.P., Podmelle F., Lipový B., Rennekampff H.O., Schumann H., Schwieger-Briel A., Zahn T.R., Metelmann H.R. Accelerated re-epithelialization of partial-thickness skin wounds by a topical betulin gel: Results of a randomized phase III clinical trials program. Burn. J. Int. Soc. Burn Inj. 2017;43:1284–1294. doi: 10.1016/j.burns.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 52.Singh S., Chidrawar V.R., Hermawan D., Nwabor O.F., Olatunde O.O., Jayeoye T.J., Samee W., Ontong J.C., Chittasupho C. Solvent-assisted dechlorophyllization of Psidium guajava leaf extract: Effects on the polyphenol content, cytocompatibility, antibacterial, anti-inflammatory, and anticancer activities. S. Afr. J. Bot. 2023;158:166–179. doi: 10.1016/j.sajb.2023.04.029. [DOI] [Google Scholar]
- 53.Chidrawar V.R., Singh S., Jayeoye T.J., Dodiya R., Samee W., Chittasupho C. Porous Swellable Hypromellose Composite Fortified with Eucalyptus camaldulensis Leaf Hydrophobic/Hydrophilic Phenolic-rich Extract to Mitigate Dermal Wound Infections. J. Polym. Environ. 2023;31:3841–3856. doi: 10.1007/s10924-023-02860-8. [DOI] [Google Scholar]
- 54.Draelos Z.D. The ability of onion extract gel to improve the cosmetic appearance of postsurgical scars. J. Cosmet. Dermatol. 2008;7:101–104. doi: 10.1111/j.1473-2165.2008.00371.x. [DOI] [PubMed] [Google Scholar]
- 55.Yoon J.Y., Kwon H.H., Min S.U., Thiboutot D.M., Suh D.H. Epigallocatechin-3-gallate improves acne in humans by modulating intracellular molecular targets and inhibiting P. acnes. J. Investig. Dermatol. 2013;133:429–440. doi: 10.1038/jid.2012.292. [DOI] [PubMed] [Google Scholar]
- 56.Enshaieh S., Jooya A., Siadat A.H., Iraji F. The efficacy of 5% topical tea tree oil gel in mild to moderate acne vulgaris: A randomized, double-blind placebo-controlled study. Indian J. Dermatol. Venereol. Leprol. 2007;73:22–25. doi: 10.4103/0378-6323.30646. [DOI] [PubMed] [Google Scholar]
- 57.Weber N., Biehler K., Schwabe K., Haarhaus B., Quirin K.W., Frank U., Schempp C.M., Wölfle U. Hop Extract Acts as an Antioxidant with Antimicrobial Effects against Propionibacterium acnes and Staphylococcus aureus. Molecules. 2019;24:223. doi: 10.3390/molecules24020223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chinembiri T.N., du Plessis L.H., Gerber M., Hamman J.H., du Plessis J. Review of natural compounds for potential skin cancer treatment. Molecules. 2014;19:11679–11721. doi: 10.3390/molecules190811679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lippens S., Hoste E., Vandenabeele P., Agostinis P., Declercq W. Cell death in the skin. Apoptosis Int. J. Program. Cell Death. 2009;14:549–569. doi: 10.1007/s10495-009-0324-z. [DOI] [PubMed] [Google Scholar]
- 60.Xiaoguang C., Hongyan L., Xiaohong L., Zhaodi F., Yan L., Lihua T., Rui H. Cancer chemopreventive and therapeutic activities of red ginseng. J. Ethnopharmacol. 1998;60:71–78. doi: 10.1016/S0378-8741(97)00133-5. [DOI] [PubMed] [Google Scholar]
- 61.Huang M.T., Ho C.T., Wang Z.Y., Ferraro T., Lou Y.R., Stauber K., Ma W., Georgiadis C., Laskin J.D., Conney A.H. Inhibition of skin tumorigenesis by rosemary and its constituents carnosol and ursolic acid. Cancer Res. 1994;54:701–708. [PubMed] [Google Scholar]
- 62.Shenefelt P.D. Herbal Treatment for Dermatologic Disorders. CRC Press/Taylor & Francis; Boca Raton, FL, USA: 2011. [PubMed] [Google Scholar]
- 63.Palungwachira P., Tancharoen S., Phruksaniyom C., Klungsaeng S., Srichan R., Kikuchi K., Nararatwanchai T. Antioxidant and Anti-Inflammatory Properties of Anthocyanins Extracted from Oryza sativa L. in Primary Dermal Fibroblasts. Oxidative Med. Cell. Longev. 2019;2019:2089817. doi: 10.1155/2019/2089817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sharma Y., Kaur A., Bhardwaj R., Srivastava N., Lal M., Madan S., Bala K. Preclinical assessment of stem of Nicotiana tabacum on excision wound model. Bioorg. Chem. 2021;109:104731. doi: 10.1016/j.bioorg.2021.104731. [DOI] [PubMed] [Google Scholar]
- 65.Thinh B.B., Khoi N.T., Doudkin R.V., Thin D.B., Ogunwande I.A. Chemical composition of essential oil and antioxidant activity of the essential oil and methanol extracts of Knema globularia (Lam.) Warb. from Vietnam. Nat. Prod. Res. 2023;37:1625–1631. doi: 10.1080/14786419.2022.2103698. [DOI] [PubMed] [Google Scholar]
- 66.do Nascimento M.N.G., Machado Martins M., Scalon Cunha L.C., de Souza Santos P., Goulart L.R., de Souza Silva T., Gomes Martins C.H., de Morais S.A.L., Pivatto M. Antimicrobial and cytotoxic activities of Senna and Cassia species (Fabaceae) extracts. Ind. Crops Prod. 2020;148:112081. doi: 10.1016/j.indcrop.2019.112081. [DOI] [Google Scholar]
- 67.Saini S., Mishra P., Balhara M., Dutta D., Ghosh S., Chaudhuri S. Antimicrobial potency of Punica granatum peel extract: Against multidrug resistant clinical isolates. Gene Rep. 2023;30:101744. doi: 10.1016/j.genrep.2023.101744. [DOI] [Google Scholar]
- 68.Padmakar S., Kumar G.A., Khurana N., Kumari S., Pal B. Efficacy and safety of natural Aloe Vera gel in the treatment of stable vitiligo. Clin. Epidemiol. Glob. Health. 2023;22:101332. doi: 10.1016/j.cegh.2023.101332. [DOI] [Google Scholar]
- 69.Esimone C.O., Nworu C., Jackson C. Cutaneous wound healing activity of a herbal ointment containing the leaf extract of Jatropha curcas L. (Euphorbiaceae) Int. J. Appl. Res. Nat. Prod. 2008;1:1–4. [Google Scholar]
- 70.Jan R., Gani A., Masarat Dar M., Bhat N.A. Bioactive characterization of ultrasonicated ginger (Zingiber officinale) and licorice (Glycyrrhiza glabra) freeze dried extracts. Ultrason. Sonochem. 2022;88:106048. doi: 10.1016/j.ultsonch.2022.106048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Khan H., Akhtar N., Ali A. Effects of Cream Containing Ficus carica L. Fruit Extract on Skin Parameters: In Vivo Evaluation. Indian J. Pharm. Sci. 2014;76:560–564. [PMC free article] [PubMed] [Google Scholar]
- 72.Chaudhuri A., Aqil M., Qadir A. Herbal cosmeceuticals: New opportunities in cosmetology. Trends Phytochem. Res. 2021;4:117–142. [Google Scholar]
- 73.Lohani A., Verma A., Joshi H., Yadav N., Karki N. Nanotechnology-based cosmeceuticals. ISRN Dermatol. 2014;2014:843687. doi: 10.1155/2014/843687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ahmed M. An Overview of Nanomedicine. J. Med. Res. Inst. 2006;27:248–254. [Google Scholar]
- 75.Sindura C., Babu N.C., Vinod Unbounding the Future: Nanobiotechnology in Detection and Treatment of Oral Cancer. J. Adv. Med. Dent. Sci. 2013;1:66–77. [Google Scholar]
- 76.Ghosh V., Saranya S., Mukherjee A., Chandrasekaran N. Antibacterial microemulsion prevents sepsis and triggers healing of wound in wistar rats. Colloids Surf. B Biointerfaces. 2013;105:152–157. doi: 10.1016/j.colsurfb.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 77.Rajendran R., Radhai R., Kotresh T.M., Csiszar E. Development of antimicrobial cotton fabrics using herb loaded nanoparticles. Carbohydr. Polym. 2013;91:613–617. doi: 10.1016/j.carbpol.2012.08.064. [DOI] [PubMed] [Google Scholar]
- 78.Mainardes R.M., Urban M.C., Cinto P.O., Chaud M.V., Evangelista R.C., Gremião M.P. Liposomes and micro/nanoparticles as colloidal carriers for nasal drug delivery. Curr. Drug Deliv. 2006;3:275–285. doi: 10.2174/156720106777731019. [DOI] [PubMed] [Google Scholar]
- 79.Grill A.E., Johnston N.W., Sadhukha T., Panyam J. A review of select recent patents on novel nanocarriers. Recent Pat. Drug Deliv. Formul. 2009;3:137–142. doi: 10.2174/187221109788452276. [DOI] [PubMed] [Google Scholar]
- 80.Venugopal J., Prabhakaran M.P., Low S., Choon A.T., Deepika G., Dev V.R., Ramakrishna S. Continuous nanostructures for the controlled release of drugs. Curr. Pharm. Des. 2009;15:1799–1808. doi: 10.2174/138161209788186344. [DOI] [PubMed] [Google Scholar]
- 81.Chorilli M., Brizante A.C., Rodrigues C.A., Salgado H.R.N. Aspectos gerais em sistemas transdérmicos de liberação de fármacos General aspects in transdermal systems of drugs release. Infarma. 2007;88:7–13. [Google Scholar]
- 82.Raszewska-Famielec M., Flieger J. Nanoparticles for Topical Application in the Treatment of Skin Dysfunctions-An Overview of Dermo-Cosmetic and Dermatological Products. Int. J. Mol. Sci. 2022;23:15980. doi: 10.3390/ijms232415980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bailey M.M., Berkland C.J. Nanoparticle formulations in pulmonary drug delivery. Med. Res. Rev. 2009;29:196–212. doi: 10.1002/med.20140. [DOI] [PubMed] [Google Scholar]
- 84.Chen Y., Lin X., Park H., Greever R. Study of artemisinin nanocapsules as anticancer drug delivery systems. Nanomedicine. 2009;5:316–322. doi: 10.1016/j.nano.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 85.Bhattacharya S., Ghosh A.K. Phytosomes: The Emerging Technology for Enhancement of Bioavailability of Botanicals and Nutraceuticals. Int. J. Aesthetic. Antiaging Med. 2009;2:87–91. [Google Scholar]
- 86.Sinico C., De Logu A., Lai F., Valenti D., Manconi M., Loy G., Bonsignore L., Fadda A.M. Liposomal incorporation of Artemisia arborescens L. essential oil and in vitro antiviral activity. Eur. J. Pharm. Biopharm. 2005;59:161–168. doi: 10.1016/j.ejpb.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 87.Ontong J.C., Singh S., Siriyong T., Voravuthikunchai S.P. Transferosomes stabilized hydrogel incorporated rhodomyrtone-rich extract from Rhodomyrtus tomentosa leaf fortified with phosphatidylcholine for the management of skin and soft-tissue infections. Biotechnol. Lett. 2024;46:127–142. doi: 10.1007/s10529-023-03452-1. [DOI] [PubMed] [Google Scholar]
- 88.Chorachoo Ontong J., Singh S., Nwabor O.F., Chusri S., Kaewnam W., Kanokwiroon K., Septama A.W., Panichayupakaranant P., Voravuthikunchai S.P. Microwave-assisted extract of rhodomyrtone from rhodomyrtus tomentosa leaf: Anti-inflammatory, antibacterial, antioxidant, and safety assessment of topical rhodomyrtone formulation. Sep. Sci. Technol. 2023;58:929–943. doi: 10.1080/01496395.2023.2169162. [DOI] [Google Scholar]
- 89.Chittasupho C., Chaobankrang K., Sarawungkad A., Samee W., Singh S., Hemsuwimon K., Okonogi S., Kheawfu K., Kiattisin K., Chaiyana W. Antioxidant, Anti-Inflammatory and Attenuating Intracellular Reactive Oxygen Species Activities of Nicotiana tabacum var. Virginia Leaf Extract Phytosomes and Shape Memory Gel Formulation. Gels. 2023;9:78. doi: 10.3390/gels9020078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chittasupho C., Ditsri S., Singh S., Kanlayavattanakul M., Duangnin N., Ruksiriwanich W., Athikomkulchai S. Ultraviolet Radiation Protective and Anti-Inflammatory Effects of Kaempferia galanga L. Rhizome Oil and Microemulsion: Formulation, Characterization, and Hydrogel Preparation. Gels. 2022;8:639. doi: 10.3390/gels8100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Moulari B., Lboutounne H., Pellequer Y., Guillaume Y.C., Millet J., Pirot F. Vectorization of Harungana madagascariensis Lam. ex Poir. (Hypericaceae) ethanolic leaf extract by using PLG-nanoparticles: Antibacterial activity assessment. Drug Dev. Res. 2005;65:26–33. doi: 10.1002/ddr.20004. [DOI] [Google Scholar]
- 92.Sun L., Liu Z., Wang L., Cun D., Tong H.H.Y., Yan R., Chen X., Wang R., Zheng Y. Enhanced topical penetration, system exposure and anti-psoriasis activity of two particle-sized, curcumin-loaded PLGA nanoparticles in hydrogel. J. Control. Release. 2017;254:44–54. doi: 10.1016/j.jconrel.2017.03.385. [DOI] [PubMed] [Google Scholar]
- 93.Raghuwanshi N., Yadav T.C., Srivastava A.K., Raj U., Varadwaj P., Pruthi V. Structure-based drug designing and identification of Woodfordia fruticosa inhibitors targeted against heat shock protein (HSP70-1) as suppressor for Imiquimod-induced psoriasis like skin inflammation in mice model. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;95:57–71. doi: 10.1016/j.msec.2018.10.061. [DOI] [PubMed] [Google Scholar]
- 94.Biswasroy P., Pradhan D., Haldar J., Kar B., Ghosh G., Rath G. Recent Advancements in Herbal Bioactive-based Nanoformulations for the Treatment of Psoriasis. Curr. Bioact. Compd. 2023;19:94–103. doi: 10.2174/1573407218666220823112843. [DOI] [Google Scholar]
- 95.Lee W.-R., Chou W.-L., Lin Z.-C., Sung C.T., Lin C.-Y., Fang J.-Y. Laser-assisted nanocarrier delivery to achieve cutaneous siRNA targeting for attenuating psoriasiform dermatitis. J. Control. Release. 2022;347:590–606. doi: 10.1016/j.jconrel.2022.05.032. [DOI] [PubMed] [Google Scholar]
- 96.Lin C.-Y., Hsieh Y.-T., Chan L.Y., Yang T.-Y., Maeda T., Chang T.-M., Huang H.-C. Dictamnine delivered by PLGA nanocarriers ameliorated inflammation in an oxazolone-induced dermatitis mouse model. J. Control. Release. 2021;329:731–742. doi: 10.1016/j.jconrel.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 97.Narayanan M., hussain F.A.J., Srinivasan B., Sambantham M.T., Al-Keridis L.A., Al-Mekhlafi F.A. Green synthesizes and characterization of copper-oxide nanoparticles by Thespesia populnea against skin-infection causing microbes. J. King Saud Univ. Sci. 2022;34:101885. doi: 10.1016/j.jksus.2022.101885. [DOI] [Google Scholar]
- 98.Chelladurai M., Sahadevan R., Margavelu G., Vijayakumar S., González-Sánchez Z.I., Vijayan K., Balaji K.C.D. Anti-skin cancer activity of Alpinia calcarata ZnO nanoparticles: Characterization and potential antimicrobial effects. J. Drug Deliv. Sci. Technol. 2021;61:102180. doi: 10.1016/j.jddst.2020.102180. [DOI] [Google Scholar]
- 99.Yang X., Mo W., Shi Y., Fang X., Xu Y., He X., Xu Y. Fumaria officinalis-loaded chitosan nanoparticles dispersed in an alginate hydrogel promote diabetic wounds healing by upregulating VEGF, TGF-β, and b-FGF genes: A preclinical investigation. Heliyon. 2023;9:e17704. doi: 10.1016/j.heliyon.2023.e17704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sheokand B., Pathak S.R., Srivastava C.M., Kumar A., Bahadur I., Vats M. Green silver nanoparticles functionalised gelatin nanocomposite film for wound healing: Construction and characterization. J. Mol. Liq. 2022;368:120561. doi: 10.1016/j.molliq.2022.120561. [DOI] [Google Scholar]
- 101.Bhalla N., Ingle N., Jayaprakash A., Patel H., Patri S.V., Haranath D. Green approach to synthesize nano zinc oxide via Moringa oleifera leaves for enhanced anti-oxidant, anti-acne and anti-bacterial properties for health & wellness applications. Arab. J. Chem. 2023;16:104506. doi: 10.1016/j.arabjc.2022.104506. [DOI] [Google Scholar]
- 102.Hemmati S., Ahmeda A., Salehabadi Y., Zangeneh A., Zangeneh M.M. Synthesis, characterization, and evaluation of cytotoxicity, antioxidant, antifungal, antibacterial, and cutaneous wound healing effects of copper nanoparticles using the aqueous extract of Strawberry fruit and l-Ascorbic acid. Polyhedron. 2020;180:114425. doi: 10.1016/j.poly.2020.114425. [DOI] [Google Scholar]
- 103.Carneiro R.d.S., Canuto M.R., Ribeiro L.K., Ferreira D.C.L., Assunção A.F.C., Costa C.A.C.B., de Freitas J.D., Rai M., Cavalcante L.S., Alves W.d.S., et al. Novel antibacterial efficacy of ZnO nanocrystals/Ag nanoparticles loaded with extract of Ximenia americana L. stem bark for wound healing. S. Afr. J. Bot. 2022;151:18–32. doi: 10.1016/j.sajb.2022.09.030. [DOI] [Google Scholar]
- 104.Guo C., Yang C., Li Q., Qi T., Xi Y., Liu W., Zhai G. Development of a quercetin-loaded nanostructured lipid carrier formulation for topical delivery. Int. J. Pharm. 2012;430:292–298. doi: 10.1016/j.ijpharm.2012.03.042. [DOI] [PubMed] [Google Scholar]
- 105.Agrawal U., Gupta M., Vyas S.P. Capsaicin delivery into the skin with lipidic nanoparticles for the treatment of psoriasis. Artif. Cells Nanomed. Biotechnol. 2015;43:33–39. doi: 10.3109/21691401.2013.832683. [DOI] [PubMed] [Google Scholar]
- 106.Khan A., Qadir A., Ali F., Aqil M. Phytoconstituents based nanomedicines for the management of psoriasis. J. Drug Deliv. Sci. Technol. 2021;64:102663. doi: 10.1016/j.jddst.2021.102663. [DOI] [Google Scholar]
- 107.Montenegro L., Pasquinucci L., Zappalà A., Chiechio S., Turnaturi R., Parenti C. Rosemary Essential Oil-Loaded Lipid Nanoparticles: In Vivo Topical Activity from Gel Vehicles. Pharmaceutics. 2017;9:48. doi: 10.3390/pharmaceutics9040048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pivetta T.P., Simões S., Araújo M.M., Carvalho T., Arruda C., Marcato P.D. Development of nanoparticles from natural lipids for topical delivery of thymol: Investigation of its anti-inflammatory properties. Colloids Surf. B Biointerfaces. 2018;164:281–290. doi: 10.1016/j.colsurfb.2018.01.053. [DOI] [PubMed] [Google Scholar]
- 109.Garg A., Singh S. Targeting of eugenol-loaded solid lipid nanoparticles to the epidermal layer of human skin. Nanomedicine. 2014;9:1223–1238. doi: 10.2217/nnm.13.33. [DOI] [PubMed] [Google Scholar]
- 110.Esposito E., Nastruzzi C., Sguizzato M., Cortesi R. Nanomedicines to Treat Skin Pathologies with Natural Molecules. Curr. Pharm. Des. 2019;25:2323–2337. doi: 10.2174/1381612825666190709210703. [DOI] [PubMed] [Google Scholar]
- 111.Zhang Y., Xia Q., Li Y., He Z., Li Z., Guo T., Wu Z., Feng N. CD44 Assists the Topical Anti-Psoriatic Efficacy of Curcumin-Loaded Hyaluronan-Modified Ethosomes: A New Strategy for Clustering Drug in Inflammatory Skin. Theranostics. 2019;9:48–64. doi: 10.7150/thno.29715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ascenso A., Pinho S., Eleutério C., Praça F.G., Bentley M.V., Oliveira H., Santos C., Silva O., Simões S. Lycopene from tomatoes: Vesicular nanocarrier formulations for dermal delivery. J. Agric. Food Chem. 2013;61:7284–7293. doi: 10.1021/jf401368w. [DOI] [PubMed] [Google Scholar]
- 113.Koli J.R., Lin S. Development of anti-oxidant ethosomes for topical delivery utilizing the synergistic properties of Vit A palmitate, Vit E and Vit C. AAPS Pharm. Sci. Technol. 2009;11:1–8. [Google Scholar]
- 114.Khogta S., Patel J., Barve K., Londhe V. Herbal nano-formulations for topical delivery. J. Herb. Med. 2020;20:100300. doi: 10.1016/j.hermed.2019.100300. [DOI] [Google Scholar]
- 115.Lin C.H., Al-Suwayeh S.A., Hung C.F., Chen C.C., Fang J.Y. Camptothecin-Loaded Liposomes with α-Melanocyte-Stimulating Hormone Enhance Cytotoxicity Toward and Cellular Uptake by Melanomas: An Application of Nanomedicine on Natural Product. J. Tradit. Complement. Med. 2013;3:102–109. doi: 10.4103/2225-4110.110423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Di Marzio L., Ventura C.A., Cosco D., Paolino D., Di Stefano A., Stancanelli R., Tommasini S., Cannavà C., Celia C., Fresta M. Nanotherapeutics for anti-inflammatory delivery. J. Drug Deliv. Sci. Technol. 2016;32:174–191. doi: 10.1016/j.jddst.2015.10.011. [DOI] [Google Scholar]
- 117.Nunes P., Rabelo A., Souza J., Santana B., Silva T., Serafini M., Menezes P., Lima B., Cardoso J., Alves J., et al. Gelatin-based membrane containing usnic acid-loaded liposome improves dermal burn healing in a porcine model. Int. J. Pharm. 2016;513:473–482. doi: 10.1016/j.ijpharm.2016.09.040. [DOI] [PubMed] [Google Scholar]
- 118.Mahdi E.S., Noor A.M., Sakeena M.H., Abdullah G.Z., Abdulkarim M.F., Sattar M.A. Formulation and in vitro release evaluation of newly synthesized palm kernel oil esters-based nanoemulsion delivery system for 30% ethanolic dried extract derived from local Phyllanthus urinaria for skin antiaging. Int. J. Nanomed. 2011;6:2499–2512. doi: 10.2147/IJN.S22337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vater C., Bosch L., Mitter A., Göls T., Seiser S., Heiss E., Elbe-Bürger A., Wirth M., Valenta C., Klang V. Lecithin-based nanoemulsions of traditional herbal wound healing agents and their effect on human skin cells. Eur. J. Pharm. Biopharm. 2022;170:1–9. doi: 10.1016/j.ejpb.2021.11.004. [DOI] [PubMed] [Google Scholar]
- 120.Kreutz T., Lucca L.G., Carneiro S.B., Limberger R.P., Veiga-Junior V.F., de Araújo B.V., Teixeira H.F., Koester L.S. Hydrogel-thickened nanoemulsion containing amazonian Aniba canelilla (Kunth) Mez essential oil: Skin permeation and in vivo anti-inflammatory efficacy. J. Drug Deliv. Sci. Technol. 2023;87:104771. doi: 10.1016/j.jddst.2023.104771. [DOI] [Google Scholar]
- 121.Huynh Luu N.-D., Dang L.H., Vo Le T.-V., Ngoc Do T.-D., Thi Nguyen T.-T., Thi Nguyen T.T., Nguyen T.P., Hoang L.S., Tran N.Q. Topical cream based on nanoformulation of Chromolaena odorata extract for accelerating burn wound healing. J. Drug Deliv. Sci. Technol. 2023;82:104360. doi: 10.1016/j.jddst.2023.104360. [DOI] [Google Scholar]
- 122.Budama-Kilinc Y., Gok B., Kecel-Gunduz S., Altuntas E. Development of nanoformulation for hyperpigmentation disorders: Experimental evaluations, in vitro efficacy and in silico molecular docking studies. Arab. J. Chem. 2022;15:104362. doi: 10.1016/j.arabjc.2022.104362. [DOI] [Google Scholar]
- 123.Ibrar M., Ayub Y., Nazir R., Irshad M., Hussain N., Saleem Y., Ahmad M. Garlic and ginger essential oil-based neomycin nano-emulsions as effective and accelerated treatment for skin wounds’ healing and inflammation: In-vivo and in-vitro studies. Saudi Pharm. J. 2022;30:1700–1709. doi: 10.1016/j.jsps.2022.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ramanunny A.K., Wadhwa S., Kumar Singh S., Kumar B., Gulati M., Kumar A., Almawash S., Al Saqr A., Gowthamarajan K., Dua K., et al. Topical non-aqueous nanoemulsion of Alpinia galanga extract for effective treatment in psoriasis: In vitro and in vivo evaluation. Int. J. Pharm. 2022;624:121882. doi: 10.1016/j.ijpharm.2022.121882. [DOI] [PubMed] [Google Scholar]
- 125.Quintão W., Alencar-Silva T., Borin M., Rezende K., Albernaz L., Cunha Filho M., Gratieri T., Carvalho J., Sá-Barreto L., Gelfuso G. Microemulsions incorporating Brosimum gaudichaudii extracts as a topical treatment for vitiligo: In vitro stimulation of melanocyte migration and pigmentation. J. Mol. Liq. 2019;294:111685. doi: 10.1016/j.molliq.2019.111685. [DOI] [Google Scholar]
- 126.Kildaci I., Budama-Kilinc Y., Kecel-Gunduz S., Altuntas E. Linseed Oil Nanoemulsions for treatment of Atopic Dermatitis disease: Formulation, characterization, in vitro and in silico evaluations. J. Drug Deliv. Sci. Technol. 2021;64:102652. doi: 10.1016/j.jddst.2021.102652. [DOI] [Google Scholar]
- 127.Priprem A., Janpim K., Nualkaew S., Mahakunakorn P. Topical Niosome Gel of Zingiber cassumunar Roxb. Extract for Anti-inflammatory Activity Enhanced Skin Permeation and Stability of Compound D. AAPS PharmSciTech. 2016;17:631–639. doi: 10.1208/s12249-015-0376-z. [DOI] [PubMed] [Google Scholar]
- 128.Kaur C.D., Saraf S. Topical vesicular formulations of Curcuma longa extract on recuperating the ultraviolet radiation-damaged skin. J. Cosmet. Dermatol. 2011;10:260–265. doi: 10.1111/j.1473-2165.2011.00586.x. [DOI] [PubMed] [Google Scholar]
- 129.Meng S., Sun L., Wang L., Lin Z., Liu Z., Xi L., Wang Z., Zheng Y. Loading of water-insoluble celastrol into niosome hydrogels for improved topical permeation and anti-psoriasis activity. Colloids Surf. B Biointerfaces. 2019;182:110352. doi: 10.1016/j.colsurfb.2019.110352. [DOI] [PubMed] [Google Scholar]
- 130.Hromadka M., Collins J.B., Reed C., Han L., Kolappa K.K., Cairns B.A., Andrady T., van Aalst J.A. Nanofiber applications for burn care. J. Burn Care Res. 2008;29:695–703. doi: 10.1097/BCR.0b013e31818480c9. [DOI] [PubMed] [Google Scholar]
- 131.Tang T., Yin L., Yang J., Shan G. Emodin, an anthraquinone derivative from Rheum officinale Baill, enhances cutaneous wound healing in rats. Eur. J. Pharmacol. 2007;567:177–185. doi: 10.1016/j.ejphar.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 132.Dai X.Y., Nie W., Wang Y.C., Shen Y., Li Y., Gan S.J. Electrospun emodin polyvinylpyrrolidone blended nanofibrous membrane: A novel medicated biomaterial for drug delivery and accelerated wound healing. J. Mater. Sci. Mater. Med. 2012;23:2709–2716. doi: 10.1007/s10856-012-4728-x. [DOI] [PubMed] [Google Scholar]
- 133.Qadir A., Jahan S., Aqil M., Warsi M.H., Alhakamy N.A., Alfaleh M.A., Khan N., Ali A. Phytochemical-Based Nano-Pharmacotherapeutics for Management of Burn Wound Healing. Gels. 2021;7:209. doi: 10.3390/gels7040209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tokuda M., Yamane M., Thickett S.C., Minami H., Zetterlund P.B. Synthesis of polymeric nanoparticles containing reduced graphene oxide nanosheets stabilized by poly(ionic liquid) using miniemulsion polymerization. Soft Matter. 2016;12:3955–3962. doi: 10.1039/C6SM00269B. [DOI] [PubMed] [Google Scholar]
- 135.Almasian A., Najafi F., Eftekhari M., Ardekani M.R.S., Sharifzadeh M., Khanavi M. Polyurethane/carboxymethylcellulose nanofibers containing Malva sylvestris extract for healing diabetic wounds: Preparation, characterization, in vitro and in vivo studies. Mater. Sci. Eng. C. 2020;114:111039. doi: 10.1016/j.msec.2020.111039. [DOI] [PubMed] [Google Scholar]
- 136.Bayat S., Amiri N., Pishavar E., Kalalinia F., Movaffagh J., Hashemi M. Bromelain-loaded chitosan nanofibers prepared by electrospinning method for burn wound healing in animal models. Life Sci. 2019;229:57–66. doi: 10.1016/j.lfs.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 137.Esposito L., Barbosa A.I., Moniz T., Costa Lima S., Costa P., Celia C., Reis S. Design and Characterization of Sodium Alginate and Poly(vinyl) Alcohol Hydrogels for Enhanced Skin Delivery of Quercetin. Pharmaceutics. 2020;12:1149. doi: 10.3390/pharmaceutics12121149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jangde R., Srivastava S., Singh M.R., Singh D. In vitro and In vivo characterization of quercetin loaded multiphase hydrogel for wound healing application. Int. J. Biol. Macromol. 2018;115:1211–1217. doi: 10.1016/j.ijbiomac.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 139.Bagde A., Patel K., Mondal A., Kutlehria S., Chowdhury N., Gebeyehu A., Patel N., Kumar N., Singh M. Combination of UVB Absorbing Titanium Dioxide and Quercetin Nanogel for Skin Cancer Chemoprevention. AAPS PharmSciTech. 2019;20:240. doi: 10.1208/s12249-019-1424-x. [DOI] [PubMed] [Google Scholar]
- 140.Raj S., Muthu D., Isaac R.S.R., Ramakrishnan S., Anooj E., Vallinayagam S. Nanomedicinary evaluation of calotropis procera mediated silver nanoparticle on skin cancer cell line for microbes-front line analysis. J. Mol. Struct. 2021;1235:130237. doi: 10.1016/j.molstruc.2021.130237. [DOI] [Google Scholar]
- 141.Ghorbanzadeh M., Farhadian N., Golmohammadzadeh S., Karimi M., Ebrahimi M. Formulation, clinical and histopathological assessment of microemulsion based hydrogel for UV protection of skin. Colloids Surf. B Biointerfaces. 2019;179:393–404. doi: 10.1016/j.colsurfb.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 142.Qadir A., Aqil M., Ali A., Warsi M.H., Mujeeb M., Ahmad F.J., Ahmad S., Beg S. Nanostructured lipidic carriers for dual drug delivery in the management of psoriasis: Systematic optimization, dermatokinetic and preclinical evaluation. J. Drug Deliv. Sci. Technol. 2020;57:101775. doi: 10.1016/j.jddst.2020.101775. [DOI] [Google Scholar]
- 143.Nirmal G.R., Lin Z.-C., Tsai M.-J., Yang S.-C., Alalaiwe A., Fang J.-Y. Photothermal treatment by PLGA–gold nanorod–isatin nanocomplexes under near-infrared irradiation for alleviating psoriasiform hyperproliferation. J. Control. Release. 2021;333:487–499. doi: 10.1016/j.jconrel.2021.04.005. [DOI] [PubMed] [Google Scholar]
- 144.Ahmad N., Khalid M.S., Khan M.F., Ullah Z. Beneficial effects of topical 6-gingerol loaded nanoemulsion gel for wound and inflammation management with their comparative dermatokinetic. J. Drug Deliv. Sci. Technol. 2023;80:104094. doi: 10.1016/j.jddst.2022.104094. [DOI] [Google Scholar]
- 145.Amer S.S., Nasr M., Abdel-Aziz R.T.A., Moftah N.H., El Shaer A., Polycarpou E., Mamdouh W., Sammour O. Cosm-nutraceutical nanovesicles for acne treatment: Physicochemical characterization and exploratory clinical experimentation. Int. J. Pharm. 2020;577:119092. doi: 10.1016/j.ijpharm.2020.119092. [DOI] [PubMed] [Google Scholar]
- 146.Nasirzadeh Fard Y., Kelidari H., Kazeminejad A., Mousavi S.J., Hedayati M.T., Mosayebi E., Nabili M., Faeli L., Asare-Addo K., Nokhodchi A., et al. Enhanced treatment in cutaneous dermatophytosis management by Zataria multiflora-loaded nanostructured lipid carrier topical gel: A randomized double-blind placebo-controlled clinical trial. J. Drug Deliv. Sci. Technol. 2023;80:104132. doi: 10.1016/j.jddst.2022.104132. [DOI] [Google Scholar]
- 147.Altinkaynak C., Haciosmanoglu E., Ekremoglu M., Hacioglu M., Özdemir N. Anti-microbial, anti-oxidant and wound healing capabilities of Aloe vera-incorporated hybrid nanoflowers. J. Biosci. Bioeng. 2023;135:321–330. doi: 10.1016/j.jbiosc.2023.01.004. [DOI] [PubMed] [Google Scholar]
- 148.Hayat M., Nawaz A., Chinnam S., Muzammal M., Latif M.S., Yasin M., Ashique S., Zengin G., Farid A. Formulation development and optimization of herbo synthetic gel: In vitro biological evaluation and in vivo wound healing studies. Process Biochem. 2023;130:116–126. doi: 10.1016/j.procbio.2023.04.010. [DOI] [Google Scholar]
- 149.Chaikul P., Kanlayavattanakul M., Somkumnerd J., Lourith N. Phyllanthus emblica L. (amla) branch: A safe and effective ingredient against skin aging. J. Tradit. Complement. Med. 2021;11:390–399. doi: 10.1016/j.jtcme.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lee Y.-S., Ryu H.W., Yang W.-K., Park M.H., Park Y.-C., Kim D.-Y., Kwon H.J., Kim S.-Y., Oh S.-R., Kim S.-H. A combination of Olea europaea leaf extract and Spirodela polyrhiza extract alleviates atopic dermatitis by modulating immune balance and skin barrier function in a 1-chloro-2,4-dinitrobenzene-induced murine model. Phytomedicine. 2021;82:153407. doi: 10.1016/j.phymed.2020.153407. [DOI] [PubMed] [Google Scholar]
- 151.Elhalmoushy P.M., Elsheikh M.A., Matar N.A., El-Hadidy W.F., Kamel M.A., Omran G.A., Elnaggar Y.S.R. Elaboration of novel gel-core oleosomes encapsulating phytoconstituent for targeted topical delivery in a vitiligo-induced mouse model: Focus on antioxidant and anti-inflammatory pathways. J. Drug Deliv. Sci. Technol. 2023;80:104119. doi: 10.1016/j.jddst.2022.104119. [DOI] [Google Scholar]
- 152.Ibrahim R.E., Elshopakey G.E., Abdelwarith A.A., Younis E.M., Ismail S.H., Ahmed A.I., El-Saber M.M., Abdelhamid A.E., Davies S.J., El-Murr A., et al. Chitosan neem nanocapsule enhances immunity and disease resistance in Nile tilapia (Oreochromis niloticus) Heliyon. 2023;9:e19354. doi: 10.1016/j.heliyon.2023.e19354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nadav S., Steinberg E., Jaggi M., Singh A.T., Verma R., Madaan A. Herbal Nanoformulations for Treating Psoriasis and Other Skin Conditions. No. WO2017172648A1. Patent. 2017 October 5;
- 154.Lee S., Kim J., Yoon S., Jo Y., Han C., Pyo S., Shin J. Topical Nano Liposome Formulation Including Extracted Purified Herbal Mixture and Whitening Cosmetics Using This Formulation. No. KR20050117958A. Patent. 2005 December 15;
- 155.Kim N., Yang J., Do J., Lee J., Kang B. Cosmetic Composition for Preventing Skin Aging Comporising Nanoliposome of Torilis japonica Fruit. No. KR100733334B1. [(accessed on 26 June 2024)];Patent. 2007 June 29; Available online: https://patents.google.com/patent/KR100733334B1/en?q=(Cosmetic+composition+for+preventing+skin+aging+nano+liposome+Torilis+japonica+fruit)&oq=Cosmetic+composition+for+preventing+skin+aging+comprising+nano+liposome+of+Torilis+japonica+fruit.
- 156.Ramar A., Sherbudeen S.B., Abdulrahim M.I., Mehta F., Janarthanan M., Ramanathan R., Rajagopalan S. Nano-Sponge Loaded Topical Gel of Curcumin and Babchi Oil for Enhanced Treatment of Psoriasis. No. DE202023101592U1. [(accessed on 26 June 2024)];Patent. 2023 May 2; Available online: https://patents.google.com/patent/DE202023101592U1/en?q=(Nano-sponge+loaded+topical+gel+of+curcumin+and+babchi+oil+enhanced+treatment+of+psoriasis)&oq=Nano-sponge+loaded+topical+gel+of+curcumin+and+babchi+oil+for+enhanced+treatment+of+psoriasis.
- 157.Quan D., Qin M. Anti-Acne Nano Preparation, Gel Composition and Preparation Method Thereof. No. CN115634165A. [(accessed on 26 June 2024)];Patent. 2023 January 24; Available online: https://patents.google.com/patent/CN115634165A/en?q=(Anti-acne+nano+preparation%2c+gel+composition+and+preparation+method+Jiangsu+Jicui+New+Pharmaceutical+Preparation+Technology+Research+Institute+Co)&oq=Anti-acne+nano+preparation%2c+gel+composition+and+preparation+method+thereof+Jiangsu+Jicui+New+Pharmaceutical+Preparation+Technology+Research+Institute+Co+ltd.
- 158.He B., Zhou J., Zhou W., Tang T., Bing P., Zhang H., Xu M. Compound Traditional Chinese Medicine Nano Gel for Treating Dermatophytosis and Tinea Pedis and Preparation Method Thereof. No. CN115300576A. [(accessed on 26 June 2024)];Patent. 2022 November 8; Available online: https://patents.google.com/patent/CN115300576A/en?q=(Compound+traditional+Chinese+medicine+nano+gel+for+treating+dermatophytosis+and+tinea+pedis+and+preparation+method+Changsha+Medical+University)&oq=Compound+traditional+Chinese+medicine+nano+gel+for+treating+dermatophytosis+and+tinea+pedis+and+preparation+method+thereof+Changsha+Medical+University.
- 159.Ni X., Xie J., Fan L. Natural Gel Preparation of Traditional Chinese Medicine Compound Extract Coated by Nanoparticles, Preparation Method and Application thereof. No. CN115337282A. [(accessed on 26 June 2024)];Patent. 2022 November 15; Available online: https://patents.google.com/patent/CN115337282A/en?oq=Natural+gel+preparation+of+traditional+Chinese+medicine+compound+extract+coated+by+nanoparticles%2c+preparation+method+and+application+thereof+CN115337282A.
- 160.Kim Y., Jang K. Rigida Pine Bark Extract with Improved Stability Encapsulated Nanoparticles and Manufacturing Method, Cosmetic Composition Comprising the Same. No. KR20220152865A. [(accessed on 26 June 2024)];Patent. 2022 November 17; Available online: https://patents.google.com/patent/KR20220152865A/en?oq=Rigida+pine+bark+extract+with+improved+stability+encapsulated+nanoparticles+and+manufacturing+meth-od%2c+cosmetic+composition+comprising+the+same++KR20220152865A.
- 161.Alam M., Bhati P., Kaushik N., Khatoon R., Kumar A., Rahate K., Sharma A., Sharma S., Singh V., Singh V., et al. In-Situ Gel Extraction, Formulation and Evaluation for Treating Fungal Skin Infection. No. AU2021107001A4. [(accessed on 26 June 2024)];Patent. 2021 December 16; Available online: https://patents.google.com/patent/AU2021107001A4/en?oq=In-situ+Gel+Extraction%2c+Formulation+and+Evaluation+for+Treating+Fungal+Skin+Infection+AU2021107001A4.
- 162.Kang S. Novel Punica granatum Extracts-Zinc Oxide Nanoparticles and Its Use. No. KR20220117942A. [(accessed on 26 June 2024)];Patent. 2023 September 25; Available online: https://patents.google.com/patent/KR20220117942A/en?oq=Novel+Punica+granatum+Extracts-Zinc+oxide+Nanoparticles+and+its+use+KR20220117942A.
- 163.Zhang P., Han L., Sun S., Du M. Natural Polysaccharide Nano Hydrogel Mask Based on Hollow Nanoparticles and Preparation Method Thereof. No. CN114010555A. [(accessed on 26 June 2024)];Patent. 2022 February 8; Available online: https://patents.google.com/patent/CN114010555A/en?oq=Natural+polysaccharide+nano+hydrogel+mask+based+on+hollow+nanoparticles+and+preparation+method+thereof+CN114010555A.
- 164.Karan M., Vasisht K., Sharma N., Kaur I.P., Gautam V., Sandhu S.K., Kaur J. Berberis Extract Nano-Formulation and Process of Preparation Thereof. No. WO2022168124A1. [(accessed on 26 June 2024)];Patent. 2022 August 11; Available online: https://patents.google.com/patent/WO2022168124A1/en?oq=Berberis+extract+nano-formulation+and+process+of+preparation+thereof+WO2022168124A1.
- 165.Zhang C., Zhang R., Gao F., Hu S. Nanoparticle System for Treating Skin Diseases and Preparation Method and Preparation Thereof. No. CN113081948A. [(accessed on 26 June 2024)];Patent. 2021 July 9; Available online: https://patents.google.com/patent/CN113081948A/en?oq=Nanoparticle+system+for+treating+skin+diseases+and+preparation+method+and+preparation+thereof+CN113081948A.
- 166.Jassen GmbH Cosmetic Preparation for the Care and Treatment of Facial Skin. No. DE202021106363U1. [(accessed on 26 June 2024)];Patent. 2021 December 15; Available online: https://patents.google.com/patent/DE202021106363U1/en?oq=Cosmetic+preparation+for+the+care+and+treatment+of+facial+skin+DE202021106363U1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be made available on request to the corresponding authors.