Abstract
Background
Recurrent acute cholangitis (RAC) is a relatively uncommon entity that presents significant management difficulties. We present the case of a patient with RAC in whom the number of episodes was reduced after a novel therapeutic procedure.
Case report
A 93-year-old male who in June 2019 was admitted for chills without fever, shivering, epigastric abdominal pain and moderate jaundice. Both abdominal ultrasound and CT scan showed intrahepatic and extrahepatic duct dilatation up to the papilla with no evidence of mass at that level. Endoscopic retrograde cholangiopancreatography (ERCP) was performed and abundant biliary sludge was removed. E. coli was identified as the cause of several of the episodes. Some isolates were shown to produce extended spectrum beta-lactamase (ESBL). Papillotomy was performed and plastic prosthesis and later a metallic prosthesis were implanted. Several months later a surgical bypass of the biliary tract was performed due to persistent episodes of cholangitis. When the chronic suppressive antibiotic treatment subsequently instituted to prevent new episodes of cholangitis failed, it was decided to perform a fecal microbiota transplant from a healthy donor and to suspend the chronic suppressive treatment. Since then, she has not presented new episodes of RAC for more than 10 months of clinical follow-up. BLEE-producing E. coli in the gastrointestinal tract could not be eradicated.
Comment
Chronic colonization of the biliary tract by certain enterobacteria such as E. coli has been identified as a relevant pathogenic factor in cases of RAC. FMT may be a promising tool to improve the clinical course of patients with RAC.
Keywords: Fecal Microbiota Transplantation, Cholangitis, Escherichia coli, Reinfection, Biliary Tract
Recurrent acute cholangitis (RAC) is a relatively uncommon entity that presents significant management difficulties [1]. In addition to stone extraction or stricture resolution by biliary-enteric anastomosis, chronic administration of antibiotics, at reduced doses, is the main strategy to reduce these episodes [1], [2]. We present the case of a patient with RAC who reduced the number of episodes after a novel therapeutic procedure:
93-year-old male with a history of type II diabetes on treatment with metformin 850 mg/24 h, arterial hypertension and superficial bladder urothelial carcinoma in remission. In June 2019 he was admitted due to shivering without fever, tremor, epigastric abdominal pain, and moderate jaundice (serum bilirubin 4 mg/dl) with significant elevation of AST (383 U/l), ALT (195 U/l) GGT (448 U/l). Blood cultures were negative. Both an abdominal ultrasound and a CT scan showed dilatation of the intrahepatic and extrahepatic duct up to the papilla without evidence of a mass at that level. There was also discrete dilatation of the gallbladder without signs of cholecystitis. Magnetic resonance cholangiopancreatography did not show the cause of the distal common bile duct stenosis (Fig. 1a). He was successfully treated with amoxicillin/clavulanic acid first intravenously (1 g/8 h) and then orally 875 mg until 14 days of treatment in total. By means of endoscopic retrograde cholangiopancreatography (ERCP) y, abundant biliary sludge was extracted. Cytological samples were obtained by puncture of the stenotic region, which showed no malignancy. Papillotomy was performed and a plastic prosthesis was placed, which was replaced in December 2019 and again in March 2020. In June 2020, he was admitted again for fever and jaundice, with bacteremia by extended spectrum beta-lactamase (ESBL)-producing Escherichia coli. He received treatment with ertapenem 1 g/24 h for 10 days. The biliary tract was mechanically cleaned by ERCP and the plastic prosthesis was replaced by a metal one (Fig. 1b). In September and December 2020, he presented new episodes of fever due to incipient cholangitis, which were treated empirically with the combination of ciprofloxacin (500 mg/8 h po) and amoxicillin/clavulanic acid 875 mg/8 h po). In January 2021, he was admitted by cholangitis and although blood cultures were negative, ESBL-producing E. coli was isolated from bile in co-culture with Bacteroides fragilis).
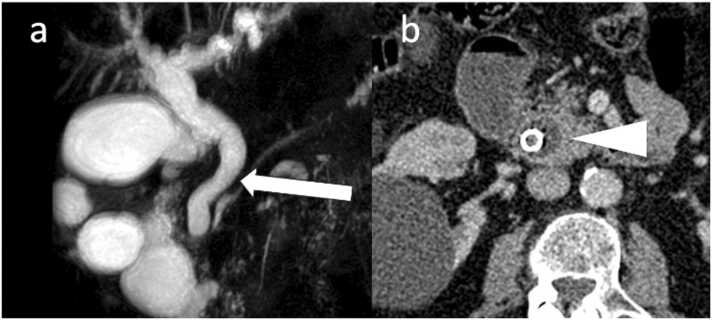
Fig. 1.
(a). Magnetic resonance cholangiopancreatography showing dilatation of the intrahepatic and extrahepatic bile duct (arrow). (b). Abdominal computed tomography showing metallic prosthesis inside the dilated common bile duct (arrowhead).
In February 2021, with the intention of preventing new infections, cholecystectomy and resection of the common bile duct with reconstruction of the transit through Roux-en-Y was performed. In June 2021 chronic suppressive treatment with cefixime 400 g po was started after a new episode of fever. Despite this strategy, the patient presented 2 episodes of fever in September and November 2022, that subsided with oral amoxicillin clavulanate empirically. In March 2023 the patient presented a new episode of cholangitis, obtaining again ESBL-producing E. coli in blood cultures. After hospital discharge, it was decided to perform fecal microbiota transplantation (FMT) from a healthy donor (after signing an informed consent document) and suspend chronic suppressive treatment. FMT was applied as compassionate use based on positive previously published results [5]. From a 50 g fresh faecal sample, the same protocol used for the treatment of C. difficile was performed, and after freeze-drying, 5 gastroresistant capsules were obtained and administered to the patient in a single dose. Since then, she has not presented new episodes of RAC for more than 11 months. Unfortunately, ESBL-producing E. coli was still identified in the stool. This was demonstrated by seeding a sample on ESBL agar (Biomérieux), a chromogenic, selective and differential agar for Gram-negative bacilli resistant to third-generation cephalosporins. Subsequently, a sensitivity study was performed on the colonies grown, using the Microscan Beckman coulter Combo 96 Panel, detecting ESBL-producing E. coli in the final reading.
Chronic colonization of the biliary tract by certain enterobacteria such as E. coli has been identified as a relevant pathogenic factor in cases of RAC [1]. FMT has been used to treat some infections, in addition to C. difficile infection, such as recurrent urinary tract infections with a clearly positive result [3]. The reduction of urinary tract infections with FMT in these patients has been related to the replacement of the uropathogens by less virulent bacteria as colonizing agents of the urinary tract.
FMT has been used in various gastrointestinal pathologies such as hepatic encephalopathy, alcoholic steatohepatitis, alcoholic hepatitis, irritable bowel syndrome and primary sclerosing cholangitis [4]. Of note is a case of primary sclerosing cholangitis in which FMT was successful in reducing the incidence of RAC [5]. The experience to date (2 published cases) and the one presented here could stimulate the performance of a clinical trial to evaluate the possible role of FMT in the prevention of RAC. As observed in recurrent urinary tract infection, the replacement in the gastrointestinal tract of certain pathogenic Enterobacterales by others that are less pathogenic and more physiologically diverse microbiota could be the cause of these promising results.
Among the limitations of this case report, we must point out that the clinical follow-up time after FMT has not been very long, so we cannot rule out that the evolution of the patient would have been the same without intervention. Likewise, we should note that the hypothesis of decolonization of enteropathogens is somewhat contradicted by the persistence of intestinal colonization by ESBL-producing E.coli.
Ethical approval
This study was approved by the appropiate institutional comiitttee (Internal Code: 124/24 Date: 09/05/24).
Author contribution
Study design: ARM, EM, RC. Data collections:ANF, MGH. Data analysis:ARM, JCP EM. Writing:ARM, JCP. All authors approved the final version of the manuscript.
Author statement
The authors state that all procedures were performed in accordance with relevant laws and institutional guidelines and have been approved by the appropriate institutional committee (Internal Code: 124/24 Date: 09/05/24).
We also confirm that informed consent was obtained from the patient.
Finally, we mention that the right to privacy of human subjects was guaranteed and respected.
CRediT authorship contribution statement
Antonio Ramos-Martinez: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. Elena Múñez: Writing – review & editing, Writing – original draft, Formal analysis, Conceptualization. Rosa del Campo: Writing – review & editing, Resources, Methodology. Alberto Nieto-Fernández: Writing – review & editing, Resources, Investigation, Data curation. Mariano Gonzálz-Haba: Writing – review & editing, Methodology, Formal analysis, Conceptualization. Jorge Calderón-Parra: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization.
Declaration of Competing Interest
All authors are free of conflicts of interest.
Footnotes
Comité de Ética de Investigación con Medicamentos. Instituto Investigación Sanitaria Puerta de Hierro. Majadahonda (Spain)
References
- 1.Li K., Hu X., Lu Q., Zhang H., Zhou J., Tian S., et al. Analysis of pathogenic bacteria distribution and related factors in recurrent acute cholangitis. Infect Drug Resist. 2023;Volume 16:4729–4740. doi: 10.2147/IDR.S418752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metwally O., Man K. The role of endoscopy in the management of recurrent pyogenic cholangitis: a review. J Community Hosp Intern Med Perspect. 2015;5(4):27858. doi: 10.3402/jchimp.v5.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramos-Martínez A., Martínez-Ruiz R., Múñez-Rubio E., Valencia-Alijo A., Ferre-Aracil C., Vera-Mendoza M.I. Effect of faecal microbiota transplantation on recurrent urinary tract infection in a patient with long-term suprapubic urinary catheter. J Hosp Infect. 2020;105(2):332–333. doi: 10.1016/j.jhin.2020.01.01. [DOI] [PubMed] [Google Scholar]
- 4.Núñez F.P., Quera R., Bay C., Thomson P. Fecal microbiota transplant, its usefulness beyond Clostridioides difficile in gastrointestinal diseases. Gastroenterol Hepatol. 2022;45(3):223–230. doi: 10.1016/j.gastrohep.2021.05. [DOI] [PubMed] [Google Scholar]
- 5.Philips C.A., Augustine P., Phadke N. Healthy donor fecal microbiota transplantation for recurrent bacterial cholangitis in primary sclerosing cholangitis – a single case report. J Clin Transl Hepatol. 2018;6(4):438–441. doi: 10.14218/JCTH.2018.00033. (ddi:) [DOI] [PMC free article] [PubMed] [Google Scholar]