Abstract
The aim of the study was to compare the efficacy of Mathieu combined urethral plate incision (Mathieu-IP) versus onlay island flap urethroplasty in patients with distal hypospadias complicated by urethral stenosis. The clinical data of 70 patients with distal hypospadias complicated by urethral plate stenosis treated in the Department of Urology, Anhui Provincial Children’s Hospital (Hefei, China), from May 2019 to May 2022, were retrospectively analyzed. Thirty-eight patients underwent Mathieu-IP (Mathieu-IP group) and 32 underwent onlay island flap urethroplasty (Onlay group). Follow-ups at 1 month, 6 months, and 12 months postoperatively assessed operative time, complications, urethral meatus morphology, and family satisfaction. The Mathieu-IP group had significantly shorter operative time (mean ± standard deviation [s.d.]: 81.58 ± 5.18 min) versus the Onlay group (mean ± s.d.: 110.75 ± 6.05 min; P < 0.05). Surgical success rates were 78.9% (Mathieu-IP group) and 75.0% (Onlay group), with no significant difference (P > 0.05). Complications were comparable between the groups. The Mathieu-IP group resulted in a vertical slit-shaped urethral meatus in 89.5% versus 13.8% in the Onlay group (P < 0.05). Family satisfaction with general penile appearance and skin shape showed no significant differences, but the Mathieu-IP group had higher satisfaction with meatal position (P < 0.05). Mathieu-IP offers simplicity, safety, and shorter operative time compared to Onlay. Both the techniques effectively treat urethral plate stenosis in distal hypospadias, with reduced postoperative complications compared to tubularized incised plate urethroplasty. Mathieu-IP results in a vertical slit-shaped urethral meatus which enhances urinary stream, indicating its potential for broader adoption.
Keywords: longitudinal urethral plate incision, Mathieu, onlay island flap urethroplasty, urethral stenosis
INTRODUCTION
Hypospadias is one of the most common congenital abnormalities affecting male infants,1 with the distal type accounting for more than half of all cases.2 Since the first report of tubularized incised plate (TIP) urethroplasty by Snodgrass in 1994, this procedure has been widely used in the initial treatment of distal hypospadias because it can achieve a slit shape of the urethral meatus, better penile appearance, and minimal complications. However, with the extension of TIP indications and long-term follow-up studies, the limitations of TIP have gradually been revealed. Postoperative stenosis and/or fistula is a common concern,3,4 especially in patients with a flat glans and narrow urethral plate, which are associated with an increased risk of complications.5 Univariate analysis suggested that the navicular fossa width and postlongitudinal incision width of the urethral plate were risk factors for post-TIP complications. For every 1-mm increase in the width of the urethral plate after a longitudinal incision, the risk of postoperative complications decreased by 16.4%.6 Holland and Smith7 suggested that a urethral plate width of <8 mm increased the incidence of urethral stenosis, urinary fistula, and glandular dehiscence after TIP. Sarhan et al.5 reported that complications were more common among patients with a urethral plate width of <8 mm than among those with a width of >8 mm.
Many studies have demonstrated that the Mathieu and onlay island flap urethroplasties can reduce the tension on the formed urethra by capping the urethra with a free flap. Therefore, these procedures are more suitable for patients with distal hypospadias complicated by urethral stenosis compared with TIP.8,9 Some scholars have reported good outcomes with the Mathieu technique combined urethral plate incision (Mathieu-IP).10,11 This study evaluated the Mathieu-IP for distal hypospadias with associated urethral plate stenosis and compared the efficacy with onlay island flap urethroplasty (Onlay). Outcomes were analyzed and compared between the two techniques.
PARTICIPANTS AND METHODS
General information
Data for 70 children with hypospadias admitted to Anhui Provincial Children’s Hospital (Hefei, China) from May 2019 to May 2022 were retrospectively analyzed. The inclusion criteria were as follows: (1) children diagnosed with hypospadias who underwent surgery for the first time; (2) urethral plate width <8 mm (average value of the upper, middle, and lower parts of the urethral plate); (3) distal hypospadias (coronal, subcoronal, and distal penile) involving a urethral defect of <2 cm; and (4) no or mild chordee. The exclusion criteria were as follows: (1) severe chordee; (2) history of circumcision and urethroplasty; (3) distal hypoplasia (transparent skin proximal to the meatus); or (4) unable to cooperate with the completion of the study and follow-ups. Depending on the type of surgical procedure, the children were divided into two groups: the Mathieu-IP group underwent Mathieu combined urethral plate incision urethroplasty, while the Onlay group underwent conventional onlay island flap urethroplasty. The selection of Mathieu-IP and onlay island flap urethroplasty was randomized. Nonsignificant differences were noted in the general information between the two groups (all P > 0.05; Table 1), which showed intergroup comparability. The surgery was performed by the same surgeon (TZ) in the Department of Urology, Anhui Provincial Children’s Hospital. The study was approved by the Ethics Committee of Anhui Provincial Children’s Hospital in 2023 (Approval No. ETYY-2023-049), and informed consent of all patients’ parents was obtained.
Table 1.
Comparison of general information between Mathieu-IP and Onlay groups
| Group | Patient (n) | Age (year), mean±s.d. | Penile length (cm), mean±s.d. | Glanular width (cm), mean±s.d. | Urethral defect length (cm), mean±s.d. | Urethral plate width (cm), mean±s.d. |
|---|---|---|---|---|---|---|
| Mathieu-IP | 38 | 2.32±1.25 | 2.35±0.54 | 1.21±0.23 | 1.32±0.58 | 5.73±1.78 |
| Onlay | 32 | 2.28±1.31 | 2.46±0.42 | 1.32±0.28 | 1.25±0.32 | 5.66±1.64 |
| P | 0.452 | 0.256 | 0.835 | 0.152 | 0.752 |
Mathieu-IP: Mathieu combined urethral plate incision; Onlay: onlay island flap urethroplasty; s.d.: standard deviation
Surgical methods
In the Mathieu-IP group, intravenous combined general anesthesia (laryngeal mask) and single caudal block were performed in the supine position, and a traction suture of 4-0 polylactic-co-glycolic acid (PGLA) was fixed at the posterior glans. The width of the urethral plate was then measured (Figure 1a). Based on the measurement of the distance between the tip of the glans and the meatus, a U-shaped incision was made around the urethral meatus, extending from the proximal end to the length of the urethral defect, with the distal end of the flap slightly narrower than the proximal end (Figure 1b). The shaft of the penis reached Buck’s fascia (a separately prepared rubber glove tourniquet was placed at the root of the penis and released once in 20 min). After exposing the tunica albuginea (abundant soft tissues were present under the inverted flap), the coronary sulcus was horizontally and circumferentially incised, and the skin was degloved to the bottom of the penis, which facilitated chordee correction. The corpus cavernosum was injected with 0.9% saline to observe penile straightening (Figure 1c). In cases in which chordee persisted, dorsal plication with 6-0 PGLA suture was performed, and before plication, the neurovascular bundles were elevated. Parallel incisions were made on both sides of the urethral plate, extending to the glans tip, reaching the tunica albuginea of the corpus cavernosum, and adequately freeing the wings of the glans. A longitudinal midline urethral plate incision was made, which was extended from the original urethral meatus to the glandular terminal, reaching the corpus cavernosum. A 6-Fr catheter was inserted, and the dartos flap around the urethral plate margin was sutured continuously or interrupted with 6-0 single-strand suture (Figure 1d and 1e), from the vicinity of the urethral meatus to the glandular terminal. The neourethra was separated dorsally, and the preputial dartos flap was rotated ventrally to cover both suture lines. Using a 6-0 single-strand suture, the urethral meatus was fixed at the 3-o’clock and 9-o’clock positions of the glans. The apex of the flap was elevated with forceps at the 6-o’clock position of the meatus, and the excess flap was trimmed along the glans contour. The first suture in the glans closure sutured the top ends of the well-freed glans wings to the trimmed 6-o’clock position of the urethral meatus. The two wings of the glans were then closed symmetrically in two layers (mattress suture on the medial side using a 5-0 single-strand suture). The appearance of the urethral meatus was then elliptical and vertical (Figure 1f). Finally, the ventral side was covered with the penile dorsal skin (Figure 1g) and covered with Mepitel film (Mölnlycke Health Care AB, Gothenburg, Sweden) and an elastic bandage.
Figure 1.
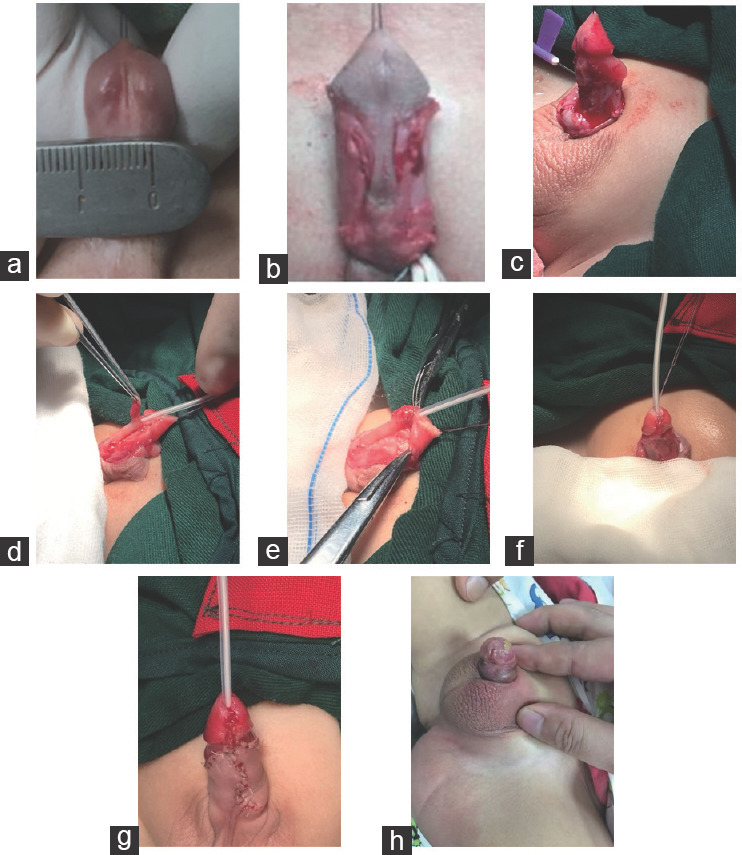
Urethroplasty procedure and postoperative urethral meatus shape of the Mathieu-IP group. (a) Measurement of urethral plate width. (b) A U-shaped incision was made around the urethral meatus, extending from the proximal end to the length of the urethral defect. (c) Straighten the penis. (d) A longitudinal midline urethral plate incision was made, which was extended from the original urethral meatus to the glandular terminal, reaching the corpus cavernosum. (e) Turn the free flap over and suture the urethra. (f) Urethral and glans formation. (g) Postoperative appearance. (h) Postoperative follow-up urethral meatus shape. Mathieu-IP: Mathieu combined urethral plate incision.
In the Onlay group, patients received intravenous combined anesthesia and were placed in the supine position. A traction suture (4-0 PGLA) was placed in the glans. The urethral plate was incised parallel from the meatus to the navicular fossa at a width of 0.6 cm–0.8 cm and then incised circumferentially 1 cm from the coronary sulcus. The skin of the penis was degloved to the bottom of the penis (dorsal tunica albuginea plication was performed if chordee was present). The length of the urethral defect was measured, and an approximately 0.8-cm-wide pedicled flap with corresponding length was created at the inner preputial flap of the dorsal penis or at the junction between the inner and outer plates. The pedicled flap was rotated to the ventral side of the penis and anastomosed with the urethral plate in a U-shape. After continuous or interrupted suturing with 6-0 single-strand suture, also using a 6-0 single-strand suture, the urethral meatus was fixed at the 3-o’clock and 9-o’clock positions of the glans. The apex of the flap was elevated with forceps at the 6 o’clock position of the meatus, and the excess flap was trimmed along the glans contour. The first suture in the glans closure sutured the top ends of the well-freed glans wings to the trimmed 6-o’clock position of the urethral meatus. The glans was sutured closed using 5-0 single-strand mattress sutures. The dorsal preputial dartos flap was separated and rotated to the ventral side to cover the neourethra, and the ventral side was covered with the penile dorsal skin followed by application of Mepitel film (Mölnlycke Health Care AB) and an elastic bandage.
Postoperative treatment and follow-ups
After surgery, cephalosporin antibiotics were administered routinely to prevent infection. The dressing was removed 5 days postoperatively, and the catheter was withdrawn 3–4 weeks postoperatively. The patients were followed up at 1 month, 6 months, and 12 months postoperatively.
Outcome measures
Intraoperative blood loss and operative time were compared between the two groups. Both the groups of children were followed up for 12 months to evaluate the surgical success rate as per the following criteria: penile appearance was basically normal, chordee was completely corrected, the meatal opening was in the normal position at the anterior glans tip, the glans shape was conical, and the children could urinate when standing normally, without complications, such as urethral stenosis or fistula. Otherwise, the operation was considered to have failed. The urethral opening and postoperative complications, such as urethral stenosis, fistula, diverticulum, and glandular dehiscence, were evaluated. A standardized questionnaire was created to record family members’ satisfaction with the meatal position, general penile appearance, and skin shape.
Statistical analyses
Data were analyzed using SPSS 25 (IBM Corp., Armonk, NY, USA). Measurement data with a normal distribution were presented as mean ± standard deviation (s.d.). Intragroup comparisons before and after treatment were analyzed using the paired samples t-test, while intergroup comparisons were analyzed using the independent samples t-test. Measurement data with a skewed distribution were presented as medians, and intergroup comparisons were analyzed using the Wilcoxon signed rank test. Numerical data were presented as percentage (%), and intergroup comparisons were analyzed using the Chi-square test. Differences were considered statistically significant at P < 0.05.
RESULTS
Intergroup comparisons of intraoperative blood loss and operative time
The Mathieu-IP group had significantly shorter operative time than that of the Onlay group (P < 0.05). Intraoperative blood loss for the Mathieu-IP group was less than that of the Onlay group, although the difference was nonsignificant (P > 0.05), as shown in Table 2.
Table 2.
Comparison of surgical data between Mathieu-IP and Onlay groups
| Group | Patient (n) | Intraoperative blood loss (ml), mean±s.d. | Operative time (min), mean±s.d. |
|---|---|---|---|
| Mathieu-IP | 38 | 16.30±1.31 | 81.58±5.18 |
| Onlay | 32 | 16.63±1.16 | 110.75±6.05 |
| P | 0.275 | <0.05 |
Mathieu-IP: Mathieu combined urethral plate incision; Onlay: onlay island flap urethroplasty; s.d.: standard deviation
Intergroup comparisons of the surgical success rate
According to the follow-up data, the surgical success rate was 78.9% (30/38) in the Mathieu-IP group and 75.0% (24/32) in the Onlay group, with no significant difference (P > 0.05; Table 3).
Table 3.
Comparison of surgical success rates between Mathieu-IP and Onlay groups
| Group | Patient (n) | Successful case (n) | Success rate (%) |
|---|---|---|---|
| Mathieu-IP | 38 | 30 | 78.9 |
| Onlay | 32 | 24 | 75.0 |
| P | 0.695 |
Mathieu-IP: Mathieu combined urethral plate incision; Onlay: onlay island flap urethroplasty
Intergroup comparisons of urethral meatal shape and postoperative complications
There were 34 cases of a vertical slit-shaped urethral meatus and 2 cases of a horizontal round urethral meatus in the Mathieu-IP group (Figure 1h). In the Onlay group, there were 6 cases of a vertical slit-shaped urethral meatus and 23 cases of a horizontal round urethral meatus. There was a significant statistical difference between the two groups (P < 0.05). There were two cases of glandular dehiscence in the Mathieu-IP group and three cases in the Onlay group, with no significant difference (P > 0.05). TIP repair was performed 6–12 months postoperatively for all glandular dehiscence cases. There were four cases of fistula (coronal sulcus) in the Mathieu-IP group and three cases in the Onlay group (repaired between 6 months and 12 months postoperatively), with no significant difference between the groups (P > 0.05). Each group had two cases of urethral stenosis, with no significant intergroup difference (P > 0.05). The two cases in the Mathieu-IP group were treated successfully by urethral dilation (dilator or catheter), and in the Onlay group, dilation attempts for 2 cases with urethral stenosis were unsuccessful, followed by incision of the narrowed segment. Subsequently, Duplay urethroplasty performed 6–12 months later resulted in successful repair. No urethral diverticulum was noted in either group (Table 4).
Table 4.
Comparison of the shape of the urethral meatus and postoperative complications between Mathieu-IP and Onlay groups
| Characteristic | Mathieu-IP (n=38) | Onlay (n=32) | P |
|---|---|---|---|
| Urethral meatus, n (%) | <0.05 | ||
| Dehiscence | 2 (5.3) | 3 (9.4) | |
| Vertical slit-like | 32 (84.2) | 6 (18.8) | |
| Horizontal round | 4 (10.5) | 23 (71.9) | |
| Postoperative fistula, n (%) | 0.873 | ||
| No fistula | 34 (89.5) | 29 (90.6) | |
| Fistula | 4 (10.5) | 3 (9.4) | |
| Postoperative stenosis, n (%) | 0.859 | ||
| No stenosis | 36 (94.7) | 30 (93.8) | |
| Stenosis | 2 (5.3) | 2 (6.3) | |
| Urethral diverticulum, n (%) | >0.05 | ||
| No diverticulum | 38 (100.0) | 32 (100.0) | |
| Diverticulum | 0 (0) | 0 (0) |
Mathieu-IP: Mathieu combined urethral plate incision; Onlay: onlay island flap urethroplasty
Intergroup comparisons of family members’ satisfaction with the urinary stream, general penile appearance, and skin shape
In the follow-up evaluation, a standardized questionnaire was used to record family members’ satisfaction with three aspects: urinary stream, general penile appearance, and skin shape. Most family members were satisfied with the postoperative general penile appearance and the skin shape, with no significant intergroup differences (P > 0.05), even with the presence of distortion for some children in the Onlay group. Regarding the urinary stream, the family members of the patients in the Mathieu-IP group reported significantly higher satisfaction compared with the Onlay group according to the questionnaire data (P=0.031; Table 5).
Table 5.
Comparison of family member’s satisfaction with the patient’s urinary stream, general penile shape, and skin shape between Mathieu-IP and Onlay groups
| Patient satisfaction | Mathieu-IP (n=38) | Onlay (n=32) | P |
|---|---|---|---|
| Urination line, n (%) | 0.031 | ||
| Very dissatisfied | 2 (5.3) | 2 (6.3) | |
| Dissatisfied | 3 (7.9) | 18 (56.3) | |
| Satisfied | 12 (31.6) | 8 (25.0) | |
| Very satisfied | 21 (55.3) | 4 (12.5) | |
| General penile appearance, n (%) | 0.944 | ||
| Very dissatisfied | 0 (0) | 0 (0) | |
| Dissatisfied | 5 (13.1) | 4 (12.5) | |
| Satisfied | 20 (52.6) | 18 (56.3) | |
| Very satisfied | 13 (34.2) | 10 (31.3) | |
| Skin shape, n (%) | 0.694 | ||
| Very dissatisfied | 0 (0) | 0 (0) | |
| Dissatisfied | 4 (10.5) | 5 (15.6) | |
| Satisfied | 23 (60.5) | 20 (62.5) | |
| Very satisfied | 11 (28.9) | 7 (21.9) |
Mathieu-IP: Mathieu combined urethral plate incision; Onlay: onlay island flap urethroplasty
DISCUSSION
Owing to anatomical traits and physiological factors, surgical treatment of distal hypospadias complicated by urethral stenosis is challenging because complications, such as urethral stenosis, urethral fistula, and glandular dehiscence, are likely to happen postoperatively.12 The urethral plate has a dense distribution of blood vessels and nerves, which is closely attached to the penile corpus cavernosum as urethral mucosal tissue. Currently, the urethral plate is considered a good urethroplasty material owing to its flat structure, regular appearance, and flexibility.13,14 Mathieu urethroplasty involves the creation of a pedicled flap to form the urethra,15 which, similar to onlay island flap urethroplasty,16 caps the flap to reduce tension on the urethra when preserving the original urethral plate. Mathieu urethroplasty has been proposed and performed to treat distal hypospadias complicated by urethral stenosis, achieving clinical efficacy, which can effectively reduce complications.17,18 We proposed the use of Mathieu-IP for distal hypospadias complicated by urethral stenosis, based on the Mathieu technique. The core principle of this approach is to enlarge the urethral plate and meatus in one step, so that the meatal shape can be transformed from horizontal to a vertical slit-like shape, thereby improving the meatal shape and penile appearance.
The comparative analysis of the Mathieu-IP group (38 cases) with the Onlay group (32 cases) in this study revealed that the mean operative time was significantly shorter for the Mathieu-IP group (mean±s.d.: 81.58 ± 5.18 min) than that for the Onlay group (mean±s.d.: 110.75 ± 6.05 min; P< 0.05). With onlay urethroplasty, a transverse pedicled preputial island flap must be applied on the urethral plate and sutured to the urethra. Thus, the dorsal prepuce must be abundant, and the superficial dorsal penile vessels should be properly protected during the separation of vascular pedicle tissue, making the surgical operation complicated and time-consuming. In contrast, with the Mathieu-IP procedure, the free urethral meatal base flap is flipped and applied on the urethral plate. This relatively simple operation can significantly shorten the operative time and is associated with a short learning curve.12
In this study, the surgical success rate was 78.9% (30/38) in the Mathieu-IP group compared with 75.0% (24/32) in the Onlay group, with no significant difference (P > 0.05). Holland and Smith7 reported an increased incidence of complications after TIP among patients with a urethral plate width of <8 mm, including urethral fistula (55%) and urethral stenosis (18%). Sarhan et al.5 reported that, among 80 patients who underwent TIP urethroplasty, 39 with a urethral plate width of <8 mm experienced significantly higher postoperative complication rates compared with those with a wider urethral plate. Both of the surgical procedures in this study showed a good efficacy in the treatment of urethral stenosis, which significantly reduced the postoperative complication rate compared with TIP. We performed a detailed comparison of the postoperative complications, including glandular dehiscence, urethral fistula, and stenosis between the Mathieu-IP and Onlay groups, and found no significant intergroup differences (P > 0.05). Glandular dehiscence in four cases might have been associated with poor glandular development, insufficient intraoperative release of the bilateral wings, and excessive suture tension during glans formation. There were two cases of urethral stenosis in the Mathieu-IP and Onlay groups each. The two cases in the Mathieu-IP group were treated successfully by urethral dilation (dilator or catheter), while the two cases in the Onlay group were treated unsuccessfully (stenosis incision and Duplay urethroplasty between 6 months and 12 months postoperatively). Hyperplastic scar tissue was found during the incision of the stenotic segment in the two cases in the Onlay group, which was likely associated with failure to protect the vasa vasorum during intraoperative isolation of the dorsal island flap, resulting in flap necrosis and hyperplastic scar tissue. The urethral plate width of all four patients with urethral stenosis was <5 mm. When the width of the urethral plate is <5 mm, it can be widened through embedding of the intrapreputial plate and buccal mucosa, thereby lowering the incidence of urethral stenosis.19,20 This is beneficial because urethral stenosis is often difficult to repair.21
The “V” incision sutured at the urethral meatus is crucial for forming a vertical slit-like appearance.22 However, for patients with urethral plate stenosis, it is necessary to extend the urethral plate incision to the glans to increase the width of the urethral meatus; otherwise, excessive trimming may lead to narrowing of the urethral meatus. Although both the groups of patients underwent “V” incision suturing at the urethral meatus, a urethral plate longitudinal incision was not performed in the Onlay group, which restricted the amount of trimming that was possible. As a result, for some patients, the surgeon was unable to form a vertical slit-like appearance at the urethral meatus. The vertical slit-like appearance of the urethral meatus is closely related to the urinary stream. In this study, the family members of the patients in the Mathieu-IP group reported significantly enhanced satisfaction with the meatal shape and position compared with the Onlay group (P < 0.05). There were five cases of penile distortion in the Onlay group and only one case in the Mathieu-IP group. Considering that intraoperative asymmetrical rotation of the flap caused penile distortion during the onlay procedure, adequate vascular pedicle length of the onlay island flap should be ensured as much as possible.23
The advantages of the Mathieu-IP procedure are as follows: (1) vertical slit-like urethral meatus; (2) the procedure facilitates formation of a reasonable glandular aperture; (3) tension-free suturing of the urethra and glans reduces the incidence of urethral stenosis and fistula, which is suitable for children with urethral stenosis; and (4) the Mathieu-IP procedure is a simple operation with a short learning curve; the procedure is easy to perform by experienced surgeons. Although the onlay island flap procedure is more complex compared with the Mathieu technique, onlay urethroplasty is not a challenge for proficient surgeons. There are increasing reports of its application in cases of urethral plate stenosis.12,24 Furthermore, compared with the Mathieu technique, onlay urethroplasty has a broader range of indications, especially in cases of mid-to-proximal hypospadias.
The postoperative urethral complications in this study are likely associated with poor urethral development, insufficient blood supply in local urethral tissue, and incomplete urethral coverage. Accordingly, the following should be noted when performing the Mathieu-IP procedure. (1) The separation and length of the pedicled flap should be sufficient to avoid high tension and damage to the vascular pedicles, which improves the flap survival rate and increases the surgical success rate. (2) Because children with distal hypospadias complicated by urethral stenosis often have a small glans, the bilateral glandular wings must be fully isolated during the longitudinal urethral plate incision to reduce tension during suturing. (3) Tissue at the coronal sulcus is relatively weak and prone to fistula formation. Thus, the longitudinal incision depth at the coronal sulcus can be appropriately increased, and part of the dartos tissue can be sutured with the penile tunica albuginea for coverage to prevent urethral fistula. Both of the urethral fistula cases in the Mathieu-IP group occurred at the coronal sulcus, which was presumably attributed to insufficient intraoperative coverage. Both the cases were cured after surgical repair. (4) The dartos fascia of the Mathieu flap acts as a second layer to cover the neourethra (note: the vascular pedicle dartos covers the two ventral sutures) to increase the coverage layers. (5) The urethral plate longitudinal incision must be extended to the tip of the glans to widen the longitudinal diameter of the urethral meatus. When shaping the urethral meatus, the tip of the flap must be trimmed to a V-shape.
For distal hypospadias with concurrent urethral plate stenosis, both the Mathieu-IP and onlay island flap procedures have shown good outcomes. The choice of surgery depends not only on the patient’s objective conditions but also on the surgeon’s preference and understanding of the procedure, leading to individualized treatment approaches. Unfortunately, owing to equipment limitations, we were unable to perform postoperative urinary flow rate assessments and comparative data analysis between the two groups of patients. Additionally, long-term follow-up is necessary to observe the postoperative outcomes of hypospadias repair. Our results require extensive and prolonged follow-up to be validated on a large scale.
AUTHOR CONTRIBUTIONS
YSC and TZ designed this study. YSC and ABZ supervised the research. CKM and TZ wrote the manuscript and analyzed the data. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Fisch H, Hyun G, Hensle TW. Rising hypospadias rates:disproving a myth. J Pediatr Urol. 2010;6:37–9. doi: 10.1016/j.jpurol.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Canon S, Mosley B, Chipollini J, Purifoy JA, Hobbs C. Epidemiological assessment of hypospadiasby degree of severity. J Urol. 2012;188:2362–6. doi: 10.1016/j.juro.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Elbakry A. Further experience with the tubularized-incised urethral plate technique for hypospadias repair. BJU Int. 2002;89:291–4. doi: 10.1046/j.1464-4096.2001.01525.x. [DOI] [PubMed] [Google Scholar]
- 4.Karakaya AE, Doğan AB, Güler AG. Use of a stent in distal hypospadias repaired by tubularized incised plate urethroplasty:a comparative study. Urol Int. 2019;102:336–40. doi: 10.1159/000497062. [DOI] [PubMed] [Google Scholar]
- 5.Sarhan O, Saad M, Helmy T, Hafez A. Effect of suturing technique and urethral plate characteristics on complication rate following hypospadias repair:a prospective randomized study. J Urol. 2009;182:682–6. doi: 10.1016/j.juro.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 6.Fang YH, Song HC, Sun N, Zhang WP, Tang YM, et al. A multicenter study on surgical procedure selection and risk factor analysis of postoperative complications after TIP and Duckett hypospadias repair. BMC Urol. 2022;22:131. doi: 10.1186/s12894-022-01051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holland AJ, Smith GH. Effect of the depth and width of the urethral plate on tubularized incised plate urethroplasty. J Urol. 2000;164:489–91. [PubMed] [Google Scholar]
- 8.Wilkinson DJ, Farrelly P, Kenny SE. Outcomes in distal hypospadias:a systematic review of the Mathieu and tubularized incised plate repairs. J Pediatr Urol. 2012;8:307–12. doi: 10.1016/j.jpurol.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Zhu XJ, Deng YJ, Wang J, Guo YF, Ge Z. Modified onlay island flap versus tubularized incised plate urethroplasty for hypospadias reoperation. Asian J Androl. 2023;25:583–6. doi: 10.4103/aja20235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiss A, Nyirády P, Pirót L, Merksz M. Combined use of perimeatal-based flap urethroplasty (Mathieu) with midline incision or urethral plate in hypospadias repair. Eur J Pediatr Surg. 2003;13:383–5. doi: 10.1055/s-2003-44727. [DOI] [PubMed] [Google Scholar]
- 11.Khalil M, Gharib T, El Shaer W, Sebaey A, Elmohamady B, Elgamal K. Mathieu technique with incision of the urethral plate versus standard tubularised incised-plate urethroplasty in primary repair of distal hypospadias:a prospective randomised study. Arab J Urol. 2017;15:242–7. doi: 10.1016/j.aju.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali MM, Anwar AZ, Mohamed MS, Abdelgawad AH, Rohiem MF, et al. Comparative outcomes among inlay grafted incised plate, onlay preputial flap and tubularized incised plate urethroplasty for the repair of distal penile hypospadias with a narrow urethral plate. World J Urol. 2023;41:3643–50. doi: 10.1007/s00345-023-04690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang PQ, Zheng RY. Efficacy comparison between tolterodine and solifenacin in improving the lower urinary tract symptoms caused by ureteral stents. Health Med Res Pract. 2019;16:46–50. [Google Scholar]
- 14.Abbas TO, Braga LH, Spinoit AF, Salle JP. Urethral plate quality assessment and its impact on hypospadias repair outcomes:a systematic review and quality assessment. J Pediatr Urol. 2021;17:316–25. doi: 10.1016/j.jpurol.2021.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Zor M, Topac H, Ors O. A new technique for adult hypospadias repair:a combination of TIPU and Mathieu techniques. Kaohsiung J Med Sci. 2018;34:120–1. doi: 10.1016/j.kjms.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Singal AK, Dubey M, Jain V. Transverse preputial onlay island flap urethroplasty for single-stage correction of proximal hypospadias. World J Urol. 2016;34:1019–24. doi: 10.1007/s00345-015-1686-1. [DOI] [PubMed] [Google Scholar]
- 17.Oswald J, Körner I, Riccabona M. Comparison of the perimeatal-based flap (Mathieu) and the tubularized incised-plate urethroplasty (Snodgrass) in primary distal hypospadias. BJU Int. 2000;85:725–7. doi: 10.1046/j.1464-410x.2000.00479.x. [DOI] [PubMed] [Google Scholar]
- 18.El Helaly HA, Youssof HA, Ibrahim HM, Aldaqadossi HA, Abdalla OM, et al. Distal hypospadias repair:comparative study between Snodgrass and transverse preputial onlay flap. J Pediatr Urol. 2022;18:610.e1–6. doi: 10.1016/j.jpurol.2022.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Shimotakahara A, Nakazawa N, Wada A, Nagata S, Koga H, et al. Tubularized incised plate urethroplasty with dorsal inlay graft prevents meatal/neourethral stenosis:a single surgeon's experience. J Pediatr Surg. 2011;46:2370–2. doi: 10.1016/j.jpedsurg.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 20.Barbagli G, Balò S, Montorsi F, Sansalone S, Lazzeri M. History and evolution of the use of oral mucosa for urethral reconstruction. Asian J Urol. 2017;4:96–101. doi: 10.1016/j.ajur.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xie QG, Xia K, Li XP, Luo P, Li ZQ, et al. Application of the Mathieu combined tunnel technique for repairing glans dehiscence after failed hypospadias repair. Asian J Androl. 2022;24:311–6. doi: 10.4103/aja202163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boddy SA, Samuel M. Mathieu and 'V'incision sutured (MAVIS) results in a natural glanular meatus. J Pediatr Surg. 2000;35:494–6. doi: 10.1016/s0022-3468(00)90220-3. [DOI] [PubMed] [Google Scholar]
- 23.Djordjevic ML, Perovic SV, Slavkovic Z, Djakovic N. Longitudinal dorsal dartos flap for prevention of fistula after a Snodgrass hypospadias procedure. Eur Urol. 2006;50:53–7. doi: 10.1016/j.eururo.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 24.Omar RG, Khalil MM, Shereef HW, Al Ashram MR, Elshaer A. Dorsal inlay inner preputial graft repair versus ventral-only preputial graft repair in primary distal penile hypospadias with narrow urethral plate. Urol Ann. 2023;15:271–7. doi: 10.4103/ua.ua_14_23. [DOI] [PMC free article] [PubMed] [Google Scholar]


