Abstract
Objective
This article aims to examine the impact of nursing workforce skill-mix (percentage of critical care registered nurses [CCRN]) in the intensive care unit (ICU) during a patient's stay.
Design
Registry linked cohort study of the Australian and New Zealand Intensive Care Society Adult Patient Database and the Critical Health Resources Information System using real-time nursing workforce data.
Settings
Fifteen public and 5 private hospital ICUs in Victoria, Australia.
Participants
There were 16,618 adult patients admitted between 1 December 2021 and 30 September 2022.
Main outcome measures
Primary outcome: in-hospital mortality. Secondary outcomes: in-ICU mortality, development of delirium, pressure injury, duration of stay in-ICU and hospital, after-hours discharge from ICU and readmission to ICU.
Results
In total, 6563 (39.5%) patients were cared for in ICUs with >75% CCRN, 7695 (46.3%) in ICUs with 50–75% CCRN, and 2360 (14.2%) in ICUs with <50% CCRN. In-hospital mortality was 534 (8.1%) vs. 859 (11.2%) vs. 252 (10.7%) respectively. After adjusting for confounders, patients cared for in ICUs with 50–75% CCRN (adjusted OR 1.21 [95% CI 1.02–1.45]) were more likely to die compared to patients in ICUs with >75% CCRN. A similar but non-significant trend was seen in ICUs with <50% CCRN (adjusted OR 1.21 [95% CI 0.94–1.55]), when compared to patients in ICUs with >75% CCRN. In-ICU mortality, delirium, pressure injuries, after-hours discharge and ICU length of stay were lower in ICUs with CCRN>75%.
Conclusion
The nursing skill-mix in ICU impacts outcomes and should be routinely monitored. Health system regulators, hospital administrators and ICU leaders should ensure nursing workforce planning and education align with these findings to maximise patient outcomes.
Keywords: Critical care, ICU, Intensive care, Mortality, Nurses, Nursing staff, Patient harm, Patient safety, Skill-mix, Workforce
1. Introduction
In Australia, national nursing workforce standards for intensive care provide an evidence-informed framework for staffing, and include nursing skill-mix recommendations.1 In the intensive care unit (ICU), skill-mix refers to the percentage of registered nurses that hold postgraduate specialist qualification in critical care nursing. These standards recommend a minimum skill-mix of 50% critical care nurses, with the optimal percentage of 75% critical care qualified staff.2,3 These skill-mix standards have been in place for over 20 years with no real substantial change over this time despite changes to healthcare systems and pandemic events.4,5 It is recognised Australian ICU patients experience excellent outcomes in comparison to other health systems.6
International studies have shown that the education level, and number of nursing staff are associated with patient outcomes, such as mortality and adverse events.[7], [8], [9] A single centre Australian ICU study demonstrated an inverse association between the percentage of critical care nurses and the risk of adverse events occurring.10 There are no published multi-centre studies which examine the impact of nursing workforce skill-mix in Australian ICUs on patient outcomes.
2. Objectives
The aim of this study was to examine the association between nursing skill-mix and ICU patient outcomes. The hypothesis was that outcomes would be better when a patient is cared for in an ICU which has a higher percentage of trained critical care nurses.
3. Methods
3.1. Design and setting
We conducted a registry linked cohort study at fifteen public and five private Victorian hospital adult ICUs between 1 December 2021 and 30 September 2022 (303 days).
3.2. Data sources
Individual patient demographic, diagnostic and outcome data were extracted from the Australia and New Zealand Intensive Care Society (ANZICS) Adult Patient Database. The ANZICS Adult Patient Database is a dataset held by the ANZICS Centre for Outcomes and Resources Evaluation Clinical Quality Registry for purposes of benchmarking ICU outcomes in Australia and New Zealand. All ICUs in Victoria submit individual patient data on a quarterly basis. Illness severity was assessed using the Australian and New Zealand Risk of Death.11 This is a highly discriminatory and well-calibrated risk model which combines age, acute physiological and biochemical disturbance, chronic comorbidities, treatment limitations, elective surgical status and source of admission with individual predictive equations for each admission diagnosis, into a single mortality risk estimate for each patient. It does not include sex, frailty or a prediction equation for COVID-19.11 Readmission episodes to ICU, palliative admissions, children (<16 years), patients still in ICU at time of data extraction and those with missing information about mortality outcomes or length of stay in ICU were excluded.
ICU staffing data were extracted from the Critical Health Resources Information System (CHRIS), a real-time dashboard of ICU activity, acuity and resources, developed and implemented nationally in response to the Coronavirus disease 2019 (COVID-19) pandemic by ANZICS, Ambulance Victoria, the Australian Government Department of Health, and Telstra Purple™. ICUs contribute summary ‘snapshot’ information about ICU resources and activity at least twice daily for the purposes of monitoring provision of critical care services.
In November 2021, all Victorian ICUs were invited to voluntarily contribute additional data about the nursing staff providing direct patient care within each ICU. This study examined a convenience sample of ICUs where more than 60% of admissions could be linked to staffing data. Nursing workforce skill-mix was categorised into four groups as defined by the Safer Care Victoria COVID-19 surge workforce guideline.12,13
-
•
Group One: postgraduate qualified critical care registered nurses (CCRN) or general registered nurses with five plus years of current/continuous ICU experience (referred to collectively as CCRN).
-
•
Group Two: early career general registered nursing staff including foundation year/transition to ICU speciality nurses, 2021–2022 postgraduate critical care nursing students, nurses with critical care experience not normally working in ICU pre-pandemic.
-
•
Group Three: redeployed nursing staff with no ICU experience (novice to ICU).
-
•
Group Four: registered undergraduate students of nursing, enrolled nurses and allied health staff providing direct patient care.
3.3. Exposure
Our exposure of interest was the overall mean proportion of CCRNs (group one) throughout the patient's ICU stay. This was calculated as the sum of CCRNs at every site, divided by the total nursing staff providing direct patient care (groups one to four) for that 24-h period. Daily values from ICU admission up until discharge/death, were then summed and divided by the total available days of data. The percentage of CCRN was categorised into three groups (>75%, 50%–75%, <50%) reflecting ‘ideal’, ‘minimum recommended’ and ‘less than ideal’ staffing levels as designated by national critical care organisations (Australian College of Critical Care Nurses and College of Intensive Care Medicine).2,3
3.4. Outcomes
The primary outcome was in-hospital mortality. Secondary outcomes were in-ICU mortality, development of delirium, pressure injury in ICU, duration of ICU stay (days), ratio of observed to predicted length of ICU stay, after-hours discharge from ICU and duration of stay in hospital.
3.5. Subgroups
The primary outcome of in-hospital mortality was also examined in the following subgroups: patients who required one or more critical care therapy (invasive ventilation, renal replacement, extracorporeal membrane oxygenation [ECMO]), patients who did not receive any of these therapies, and only patients in public hospitals.
3.6. Statistical analysis
All data were analysed using Stata version 16.1, College Station, Texas.14 Results are presented as number (%), median (interquartile range) or mean (standard deviation) as appropriate depending on type and distribution of data. Chi-square, t-test, analysis of variance (ANOVA), Wilcoxon rank-sum and Kruskal–Wallis tests were used to compare groups depending on the type of data, and number of groups examined. Mixed effects hierarchical multivariable logistic regression (with patients clustered by site and site entered as a random effect) was used to determine variables independently associated with the primary outcome (in-hospital mortality). Patients admitted to ICUs with CCRN >75% were the reference category. Potential confounders were identified through univariable comparison of survivors and deaths (Appendix Table 1). The Activity index of the ICU on the day of the patient's admission was included.15 The Activity index combines overall patient acuity and staffing within the ICU into a single measure where higher values represent increasing levels of strain within the unit. Additional information about the Activity index is provided in Appendix Table 2. Colinear variables were identified using variance inflation factor, with the best model selected using Akaike and Bayesian information criteria. Marginal risk-adjusted probabilities of death are reported for all patients and for subgroups after holding other parameters constant using the margins command in Stata. Sensitivity analyses were undertaken, modelling the exposure (CCRN percentage) with restricted cubic splines. No imputation for missing data was performed. A two-sided p value of <0.05 was considered statistically significant.
3.7. Ethical approval
Ethics was approved by The Alfred Health Human Research and Ethics Committee (HREC 246/22). The study was unfunded research undertaken by the authors.
4. Results
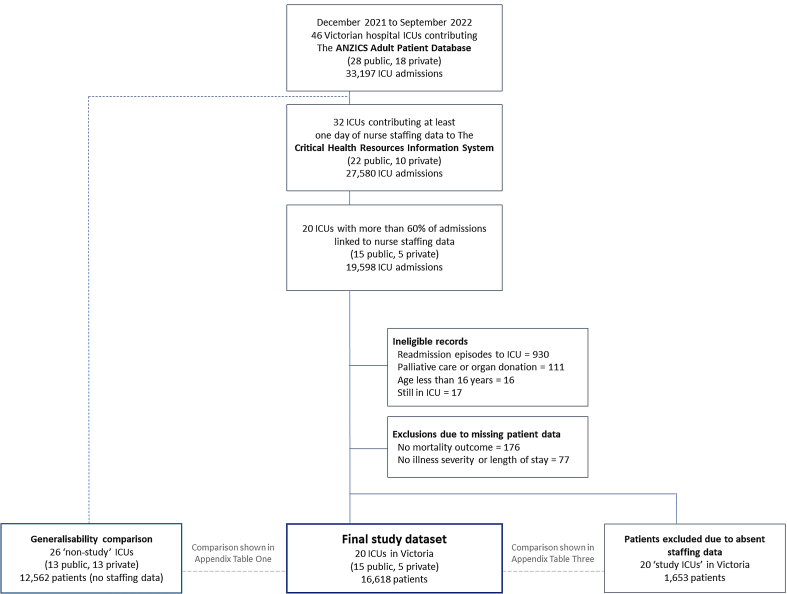
There were 19,598 admissions to the 20 study ICUs, of which 16,618 patients met inclusion criteria (Appendix Figs. 1 and 2). There were 6563 (39.5%) patients cared for in ICUs where the CCRN was >75%, 7695 (46.3%) where this was 50–75% and 2360 (14.2%) with CCRN <50%. Study ICUs were larger public units, with younger patients, more invasive therapies and higher mortality than ICUs in other Victorian hospitals (Appendix Tables 3 and 4).
Patients in the highest CCRN percentage category were older, had lower illness severity scores and less commonly received renal replacement therapy or ECMO. There was no difference in the proportion receiving invasive mechanical ventilation. Although medical patients were the most common diagnostic category overall, a relatively greater proportion of patients in the highest CCRN percentage category were planned admissions to ICU following elective surgery or admitted following cardiac surgery. COVID-19 patients were most common in ICUs in the lowest CCRN percentage category (Table 1).
Table 1.
Characteristics of patients and intensive care units (ICUs) by category of percentage of critical care registered nurses in each ICU.
| <50 % CCRN | 50–75% CCRN | >75% CCRN | p value | |
|---|---|---|---|---|
| Patient characteristics | N = 2360 | N = 7695 | N = 6563 | |
| Age in yearsa | 60.7 (18.0) | 61.1 (17.5) | 62.1 (17.2) | <0.001 |
| Men | 1401 (59.4%) | 4482 (58.2%) | 3768 (57.4%) | 0.24 |
| ICU admission category | <0.001 | |||
| Medical admission | 1594 (67.5%) | 4970 (64.6%) | 3113 (47.4%) | |
| Emergency surgical admission | 406 (17.2%) | 1379 (17.9%) | 1065 (16.2%) | |
| Elective surgery with planned ICU admission | 360 (15.3%) | 1346 (17.5%) | 2385 (36.3%) | |
| ICU admission diagnosis | <0.001 | |||
| Cardiac medical diagnoses | 305 (12.9%) | 960 (12.5%) | 611 (9.3%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 212 (9.0%) | 660 (8.6%) | 334 (5.1%) | |
| Sepsis and other infections (incl. pneumonia) | 424 (18.0%) | 1378 (17.9%) | 844 (12.9%) | |
| Other medical diagnoses | 361 (15.3%) | 1191 (15.5%) | 738 (11.2%) | |
| Cardiothoracic & vascular surgery | 140 (5.9%) | 540 (7.0%) | 568 (8.7%) | |
| Coronary Artery Bypass Grafting and/or valve surgery | 134 (5.7%) | 514 (6.7%) | 882 (13.4%) | |
| Gastro-intestinal surgery | 204 (8.6%) | 733 (9.5%) | 799 (12.2%) | |
| Neurological and neurosurgical diagnoses | 118 (5.0%) | 502 (6.5%) | 529 (8.1%) | |
| Orthopaedic surgery | 44 (1.9%) | 183 (2.4%) | 392 (6.0%) | |
| Trauma | 271 (11.5%) | 565 (7.3%) | 363 (5.5%) | |
| Other surgical diagnoses | 147 (6.2%) | 469 (6.1%) | 503 (7.7%) | |
| COVID-19 pneumonitis | 105 (4.4%) | 297 (3.9%) | 106 (1.6%) | <0.001 |
| Illness severity scores | ||||
| Acute Physiology and Chronic Health Evaluation (APACHE) III/IV scorea | 54.1 (25.7) | 56.2 (25.2) | 52.0 (23.6) | <0.001 |
| Australian & New Zealand Risk of Death (ANZROD) percent (mean, median [IQR]) | 10.8, 2.9 (0.7–11.2) | 11.5, 3.1 (0.8–12.8) | 9.4, 1.8 (0.5–8.3) | <0.001 |
| Therapies provided in ICU | ||||
| Invasive ventilation | 903 (38.3%) | 3101 (40.3%) | 2639 (40.2%) | 0.19 |
| Renal replacement therapy | 163 (7.0%) | 562 (7.6%) | 291 (5.4%) | <0.001 |
| Extracorporeal membrane oxygenation | 32 (1.4%) | 44 (0.6%) | 13 (0.2%) | <0.001 |
| Inotropes | 1034 (44.2%) | 3763 (50.9%) | 2431 (45.4%) | <0.001 |
| Invasive ventilation, renal replacement or ECMO | 952 (40.3%) | 3297 (42.8%) | 2751 (41.9%) | 0.09 |
| Intensive Care Unit Characteristics | ||||
| Hospital classification | <0.001 | |||
| Public rural/regional (4 ICUs) | 702 (30%) | 1179 (15%) | 190 (3%) | |
| Public metropolitan (6 ICUs) | 748 (32%) | 2599 (34%) | 676 (10%) | |
| Public tertiary (5 ICUs) | 900 (38%) | 3496 (45%) | 3311 (50%) | |
| Private (5 ICUs) | 10 (0%) | 421 (5%) | 2386 (36%) | |
| Characteristics of the ICU and nursing skill-mix profile on the day of patient's admission to ICU (unless otherwise stated) | ||||
| Activity index of the ICU | 1.3 (0.5–1.7) | 1.4 (0.9–1.6) | 1.2 (0.7–1.5) | <0.001 |
| Occupancy (%)b | 88 (67–95) | 90 (77–95) | 85 (73–93) | <0.001 |
| Number of baseline ‘business as usual’ ICU bedsb | 10.0 (6.0–46.0) | 14.0 (10.0–25.0) | 17.0 (11.0–26.0) | <0.001 |
| Number of patients receiving 1:1 nursing in ICUb | 7.0 (2.0–47.7) | 8.5 (4.0–23.3) | 10.0 (3.0–21.3) | <0.001 |
| Number of COVID-19 patients in ICU on day of admissionb | 2.0 (0.0–6.7) | 1.3 (0.0–3.8) | 0.8 (0.0–2.0) | <0.001 |
| Number of Critical Care Registered Nursesb | 6.0 (3.0–28.0) | 9.0 (6.0–20.0) | 13.0 (7.0–22.0) | <0.001 |
| Number of early career/in training critical care nursesb | 5.0 (3.0–26.0) | 4.0 (2.0–9.0) | 2.0 (1.0–4.0) | <0.001 |
| Number of nurses without ICU experience redeployed into ICUb | 1.0 (0.0–5.0) | 0.0 (0.0–2.0) | 0.0 (0.0–0.0) | <0.001 |
| Number of nursing students & ‘non-nursing’ staff providing ICU bedside careb | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | <0.001 |
| Percentage of CCRN as proportion of all staff providing bed-side ICU careb | 44.1 (36.4–49.3) | 62.1 (54.5–70.0) | 84.6 (77.8–93.8) | <0.001 |
| Percentage of CCRN throughout patient's ICU admissionb | 44.5 (39.5–47.7) | 62.7 (55.6–69.1) | 83.3 (78.7–90.4) | <0.001 |
CCRN, Critical Care Registered Nurses; ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
Data reported as mean (standard deviation).
Median (interquartile range); all other data reported as number (percentage).
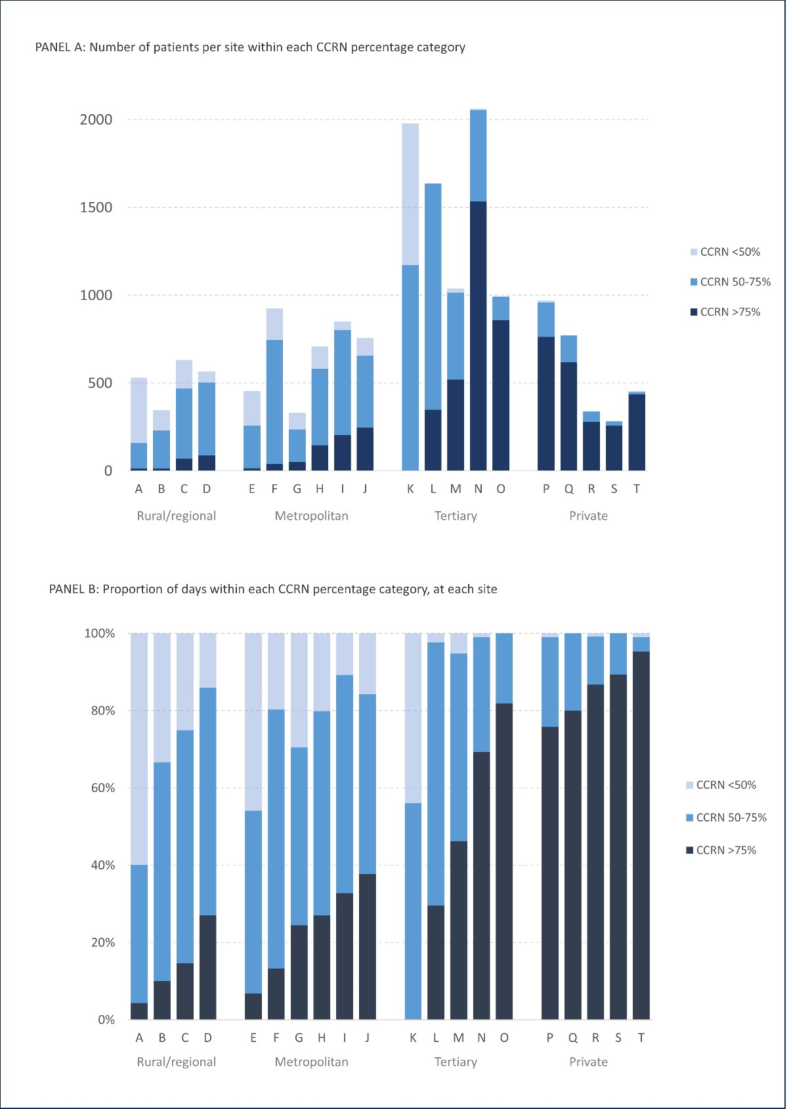
Patients in the highest CCRN percentage category were cared for in larger ICUs (more baseline ICU beds, more total patients already in ICU needing 1:1 nursing) with lower occupancy. As a proportion of the total number of patients admitted to each hospital type, 2386 (85%) patients in private hospitals were cared for in ICUs where the CCRN percentage was >75%, compared to 3311 (43%) in tertiary ICUs, 676 (17%) in metropolitan ICUs and 190 (9%) in rural/regional ICUs (Table 1). Private hospital ICUs had the greatest proportion of days with skill-mix >75% CCRN, followed by tertiary ICUs, then metropolitan ICUs, with the lowest seen in rural/regional ICUs (Fig. 1).
Fig. 1.
Number of patients within each critical care registered nurse (CCRN) percentage category (Panel A) and proportion of days within each CCRN percentage category (Panel B) at each site.
4.1. Primary outcome – in-hospital mortality
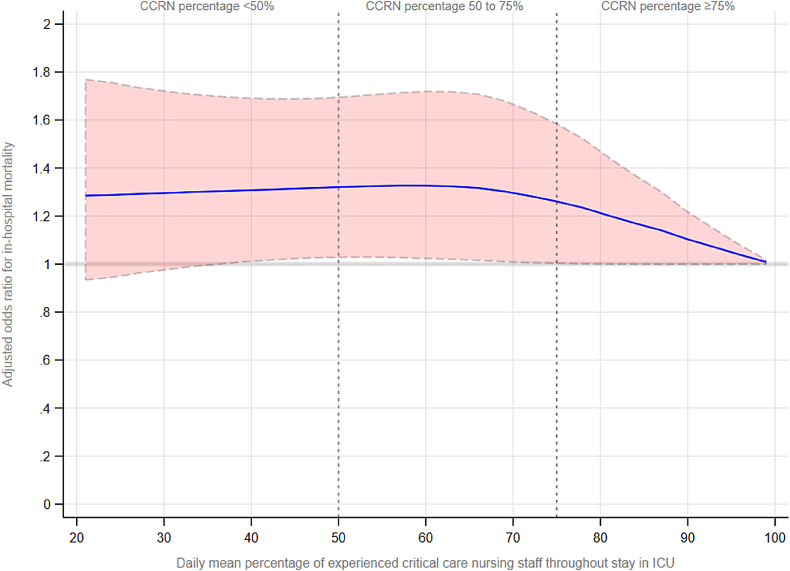
Observed in-hospital mortality was lowest when patients were cared for in ICUs with the highest nursing skill-mix category CCRN >75% (n = 534, 8.1%) vs. CCRN 50–75% (n = 859, 11.2%) vs. CCRN <50% (n = 252, 10.7%) (Table 2). After adjusting for confounders including illness severity, sex, COVID-19, frailty, ICU Activity index, and hospital type, patients in ICUs with CCRN 50–75% were more likely to die (adjusted OR 1.21 [95% Confidence Interval 1.02–1.45]) than those in ICUs with a higher CCRN percentage. Although the point estimate for patients in ICUs with CCRN <50% (adjusted Odds Ratio 1.21 [95% CI 0.94–1.55]) suggested a potential signal for harm, this did not reach statistical significance (Table 3) and (Appendix Table 5). The mortality risk associated with the percentage of CCRN, modelled using cubic splines is shown in Fig. 2.
Table 2.
Unadjusted primary and secondary outcomes of patients by category of critical care registered nurses in each intensive care unit.
| <50% CCRN |
50–75% CCRN |
>75% CCRN |
p value | |
|---|---|---|---|---|
| N = 2360 | N = 7695 | N = 6563 | ||
| Primary outcome | ||||
| In-hospital mortality | 252 (10.7%) | 859 (11.2%) | 534 (8.1%) | <0.001 |
| Secondary outcomes | ||||
| In-ICU mortality | 180 (7.6%) | 594 (7.7%) | 351 (5.3%) | <0.001 |
| Delirium in ICU | 258 (12.8%) | 618 (10.0%) | 150 (4.1%) | <0.001 |
| Pressure injury developed in ICU | 57 (2.7%) | 135 (2.1%) | 46 (1.2%) | <0.001 |
| Duration of ICU stay (days) | 2.2 (1.1–4.8) | 2.1 (1.1–4.2) | 1.8 (0.9–3.2) | <0.001 |
| Ratio of observed to predicted length of ICU stayb | 1.18 (0.66–2.16) | 1.11 (0.65–1.93) | 1.01 (0.64–1.63) | <0.001 |
| Duration of stay in hospital (days) | 7.8 (3.8–14.8) | 8.3 (4.3–15.8) | 8.0 (4.3–14.6) | <0.001 |
| After-hours discharge from ICUa | 552 (25.3%) | 1576 (22.2%) | 831 (13.4%) | <0.001 |
CCRN, Critical Care Registered Nurse; ICU, Intensive Care Unit.
ICU survivors only.
Predicted length of ICU stay is derived from the ANZICS prediction model to estimate expected ICU length of stay. A ratio >1 represents an ICU stay that is longer than predicted.
Table 3.
Mixed effects hierarchical multivariable logistic regression for in-hospital mortality adjusted for sex, illness severity, COVID-19 status, frailty, ICU activity index and hospital type (with site as random effect) in all patients and in subgroups categorised by a. invasive therapies (invasive ventilation, renal replacement or ECMO), b. no invasive therapies and c. patients in public hospital ICUs.
| Patient category | CCRN group | No. of patients | Observed mortality | Adjusted Odds Ratio (95% CI) | p value |
|---|---|---|---|---|---|
| All patients | CCRN >75% | (n = 6563) | 534 (8.1%) | Reference value | |
| CCRN 50–75% | (n = 7695) | 859 (11.2%) | 1.21 (1.02–1.45) | 0.032 | |
| CCRN <50% | (n = 2360) | 252 (10.7%) | 1.21 (0.94–1.55) | 0.14 | |
| Subgroups | |||||
| a. Invasive ventilation, renal replacement or ECMO | CCRN >75% | (n = 2751) | 352 (12.8%) | Reference value | |
| CCRN 50–75% | (n = 3297) | 602 (18.3%) | 1.35 (1.11–1.64) | 0.003 | |
| CCRN <50% | (n = 952) | 169 (17.8%) | 1.28 (0.98–1.66) | 0.07 | |
| b. No invasive ventilation, renal replacement or ECMO | CCRN >75% | (n = 3812) | 182 (4.8%) | Reference value | |
| CCRN 50–75% | (n = 4398) | 257 (5.8%) | 1.05 (0.79–1.39) | 0.76 | |
| CCRN <50% | (n = 1408) | 83 (5.9%) | 1.14 (0.76–1.71) | 0.52 | |
| c. Public hospital ICUs | CCRN >75% | (n = 4177) | 425 (10.2%) | Reference value | |
| CCRN 50–75% | (n = 7274) | 844 (11.6%) | 1.27 (1.06–1.52) | 0.011 | |
| CCRN <50% | (n = 2350) | 251 (10.7%) | 1.24 (0.97–1.59) | 0.08 | |
For full multivariable models see Appendix Table 5. CCRN, Critical Care Registered Nurse; CI, Confidence interval; ECMO, Extracorporeal membrane oxygenation; ICU, Intensive Care Unit.
Fig. 2.
Adjusted odds of in-hospital mortality plotted across the mean daily percentage of critical care registered nurses (CCRN) over the duration of the patient stay in ICU.
4.2. Secondary outcomes
In-ICU mortality, delirium, pressure injuries, after-hours discharge, ICU length of stay and ratio of observed to predicted length of ICU stay were all lower amongst patients admitted to ICUs with CCRN >75%, compared to the other skill-mix categories (Table 2).
4.3. Subgroup and sensitivity analyses
Amongst patients who received invasive ventilation, renal replacement or ECMO, observed in-hospital mortality was lowest amongst patients cared for in ICUs with the highest nursing skill-mix category CCRN >75% (n = 352, 12.8%) vs. CCRN 50–75% (n = 602, 18.3%) vs. CCRN <50% (n = 169, 17.8%) (Appendix Table 6). After adjusting for confounders, those admitted to ICUs with a CCRN 50–75% were more likely to die (adjusted OR 1.35 [95% CI 1.11–1.64]) when compared to patients in ICUs with CCRN >75%. A similar but non-significant trend was seen in ICUs with CCRN <50% (adjusted OR 1.28 [95% CI 0.98–1.66]) (Table 3, Appendix Table 5). In-ICU mortality, delirium, pressure injuries, after-hours discharge, and ICU and hospital length of stay were also all lower amongst patients admitted to ICUs with CCRN>75% (Appendix Table 6).
Amongst the subgroup who did not receive invasive ventilation, renal replacement or ECMO, there was no difference in observed or adjusted in-hospital mortality between patients in each of the skill-mix categories (Appendix Tables 5 and 7). However, unadjusted in-ICU mortality, delirium, after-hours discharge, and ICU length of stay were lower amongst patients in ICUs with CCRN >75% (Appendix Table 7).
Amongst the subgroup who were in public hospital ICUs, unadjusted in-ICU mortality, delirium, after-hours discharge, and ICU length of stay were lower amongst patients in ICUs with CCRN >75% (Appendix Table 8). After adjusting for confounders, those admitted to ICUs with a CCRN 50–75% were more likely to die (adjusted OR 1.27 [95%CI 1.06–1.52]) (Appendix Tables 5 and 8).
5. Discussion
This study of 16,618 patients admitted to 20 ICUs in Victoria, Australia between December 2021 and September 2022, demonstrated that patients cared for in ICUs with 50–75% CCRN were more likely to die in hospital than patients in ICUs with a higher CCRN skill-mix. This effect on mortality was predominantly accounted for by those who required critical care therapies such as invasive mechanical ventilation, renal replacement or ECMO and was consistent when only patients in public hospital ICUs were analysed. In addition, patients admitted to ICUs with CCRN >75% were observed to have lower in-ICU mortality, delirium, pressure injuries, after-hours discharge, and reduced ICU length of stay.
Studies that have examined nurse staffing and level of education on ICU patient outcomes have been limited by the use of static or aggregated data from sources which do not measure daily or shift by shift variation in workforce.9,16,17 Although the impact of overall staff resources on ICU patient mortality and morbidity has been described, the effect of experience and training level of ICU nurses has limited evidence. A cross-sectional study of 303 acute care hospitals in the USA found that a 10% increase in nurses with a bachelor's degree was associated with a 2% reduction in the odds of 30-day mortality in mechanically ventilated patients.18 Additionally, fewer nursing resources in ICU contribute to adverse events such as increase healthcare associated infections,19 poorer quality of care, and reduced adherence to guidelines and protocols.20,21 Organisational factors, such as appropriate nursing workforce levels directly influence quality of care, with increased missed or omitted nursing care interventions reported.22,23 Our study suggests that improvements in patient mortality and patient quality care outcomes might be achieved by increasing the percentage of postgraduate qualified critical care nurses within an ICU.
Excluding patients admitted for COVID-19, the all-cause mortality has increased in Australian ICUs for the first time in five years.24 The COVID-19 pandemic required an adaptable nursing workforce with nursing redeployment, rapid upskilling and changed models of staffing.13 The COVID-19 pandemic impacted health and healthcare delivery, with workforce shortages, especially in critical care environments continuing to be a global challenge for healthcare systems.[25], [26], [27] Pandemic models of care may have influenced healthcare systems and patient outcomes.28 Our study covered the COVID-19 peak which affected Victoria between the end of 2021 and early 2022, when many hospitals relied on nursing staff without critical care experience redeployed into ICU.13 While it is likely that this is an important factor in our findings, it is also important to note that without redeployment to increase total ICU staffing levels over the peak pandemic demand, it is possible mortality would have been even higher.
Chronic shortages of postgraduate qualified critical care nurses existed pre-pandemic and continue to challenge health systems' ability to respond to critical care demand through sustainable training, education, recruitment, and retention strategies.29,30 These were exacerbated during the COVID-19 pandemic. Our study raises the possibility that inadequate numbers of critical care trained nurses may have contributed to excess mortality during the pandemic and also potentially to the ongoing reversal of the annual reduction in mortality presently reported in Australian ICUs.24,31 The consistency of our findings after adjusting for the ICU Activity index, which is a measure of overall ICU strain combining patient acuity and staffing, suggests that the skill-mix itself is an independent factor influencing patient outcomes which goes beyond the absolute number of nursing staff available and the overall acuity of the ICU. Our finding that CCRN skill-mix was not associated with outcomes in those who did not receive invasive ventilation, renal replacement or ECMO, has important implications to the allocation of nurse staffing. Our study also highlights the need to continue to gather nursing workforce skill-mix data so that changes to ICU models of care and staffing can be properly evaluated. We recommend classifying post-graduate ICU educated nurses as CCRN in future data collection with years of experience as a different construct.
5.1. Strengths
Our study included a large number of patients from 20 hospitals representing a majority of ICU admissions in Victoria, all hospital types and all major diagnostic groups. We controlled for confounding factors, including severity of illness, gender, frailty, COVID-19, Activity index, and hospital type. We have accounted for ICU strain which is recognised as an important factor influencing access to ICU and patient outcomes.31,32 Subgroup and sensitivity analyses showed the relationship between the percentage of CCRN and mortality was predominantly confined to patients requiring invasive ICU therapies in whom critical care expertise is most needed. This supports a causal relationship between nursing skill-mix and patient outcomes.
5.2. Limitations
The Safer Care Victoria COVID-19 ICU Group One staffing classification combined nurses with a specialist postgraduate qualification with general registered nurses who had at least five years of ICU experience.12 Thus, we cannot determine whether years of experience or formal critical care training with a qualification has a greater effect on patient outcomes. The influence of advanced clinical nursing roles such as nurse practitioners, clinical nurse educator, charge nurse/associate nurse unit manager and clinical coordinator/patient access nurse is unknown as they were not identifiable in our skill-mix calculations. We cannot tell whether the lack of effect seen in the group with the lowest CCRN percentage contains a true effect which we failed to detect in this smaller group, or if there were strategies in place to support patients looked after in these ICUs to mitigate any adverse outcomes. This study has all the limitations of retrospective data, with the potential for residual unmeasured confounding leading to over-estimation of the effect of nursing skill-mix in the primary risk-adjusted analysis. Generalisability of our findings to other parts of Australia and healthcare systems in other countries is uncertain. It is possible that Victorian ICUs which were invited to participate but did not provide staffing data, were those with fewer staffing resources and could thus not collect the required information. Our study was limited to reporting ICU-only workforce data and not other components of the hospital system. The primary outcome of in-hospital mortality may also have been impacted by the levels and experience of ward nursing staff. Other potential factors such as organisational culture, impact of the COVID-19 pandemic on healthcare professionals' work practices, well-being, burnout and attrition were unknown. Finally, we did not have data on ICU medical or allied health staffing.
6. Conclusion
The nursing skill-mix in ICU impacts patient outcomes and should be routinely monitored. Addressing CCRN shortages is likely to lead to improved patient outcomes. Health system regulators, hospital administrators and leaders in Australian ICUs should ensure nursing workforce planning and education align with these findings to maximise patient outcomes.
Conflict of interest
Conflicts of interests and relevant funding are also disclosed as part of this statement.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Paul Ross: Conceptualisation of the project; Contributed to the development and design of methodology; contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Nil conflict of interests to report. Rose Jaspers: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Rose Jaspers represents the Australian College of Critical Care Nurses (ACCCN) for the Victorian ICU Nurse Unit Manager Community of Practice group. Jason Watterson: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Jason Watterson is an ICU NUM and contributed data to CHRIS. Michelle Topple: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Michelle Topple is an ICU NUM and contributed data to CHRIS. Tania Birthisel: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Tania Birthisel is an ICU NUM and contributed data to CHRIS. Melissa Rosenow: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Melissa Rosenow is a member of the management committee of the Critical Health Resources Information System (CHRIS). Jason McClure: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Conflict of interests to report: Jason McClure is the Director of Adult Retrieval Victoria and member of the management committee of the Critical Health Resources Information System (CHRIS). Ged Williams: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Nil conflict of interests to report. Wendy Pollock: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Nil conflict of interests to report. David Pilcher: Conceptualisation of the project; Contributed to the development and design of methodology; Contributed to the achievement of the project design, objectives, deliverables, and outcomes; Participated in project meetings; Contributed to HREC application, data collection tool, ethics preparation and application, data analysis and interpretation and reports; Contributed to the validation and formal analysis of results; Contributed in the preparation, review and editing of the manuscript; Contribute to publication and dissemination; No funding relevant to the article; Nil conflict of interests to report.
Acknowledgement
We acknowledge the Australia New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE) for providing the data used in the current study. The authors and the ANZICS CORE management committee would like to thank clinicians, managers, data collectors, and researchers at the contributing sites presented in Appendix Table 9. The authors gratefully acknowledge the contribution and work of the following nurse unit managers without whom this study would not have been possible: Samantha Angiolella, Tania Birthisel, Andrea Bock, Nikki Harrison, Dacielle Johnson, Michelle Spence, Penny Spencer, Michelle Topple, Kate Vasallo and Jason Watterson.
Contributor Information
Paul Ross, Email: P.Ross@alfred.org.au.
Rose Jaspers, Email: rose.jaspers@monash.edu.
Jason Watterson, Email: Jason.Watterson@latrobe.edu.au.
Michelle Topple, Email: Michelle.Topple@austin.org.au.
Tania Birthisel, Email: t.birthisel@alfred.org.au.
Melissa Rosenow, Email: melissa.rosenow@ambulance.vic.gov.au.
Jason McClure, Email: j.mcclure@alfred.org.au.
Ged Williams, Email: ged.williams@alfred.org.au.
Wendy Pollock, Email: Wendy.Pollock@monash.edu.
David Pilcher, Email: David.Pilcher@monash.edu.
Appendix.
Table A1.
Comparison of survivors to those who died in-hospital
| Patient characteristics | Alive |
Dead |
p value |
|---|---|---|---|
| N = 14,973 | N = 1645 | ||
| Critical Care Registered Nurse percentage | 70.0 (55.2–81.1) | 66.7 (54.6–77.7) | <0.001 |
| Critical Care Registered Nurse group | <0.001 | ||
| CCRN >75% | 6029 (40.3%) | 534 (32.5%) | |
| CCRN 50–75% | 6836 (45.7%) | 859 (52.2%) | |
| CCRN <50% | 2108 (14.1%) | 252 (15.3%) | |
| Age in years | 60.8 (17.6) | 67.7 (14.7) | <0.001 |
| Men | 8587 (57.3%) | 1064 (64.7%) | <0.001 |
| Source of admission to ICU | <0.001 | ||
| Operating theatre | 6458 (43.1%) | 308 (18.7%) | |
| Emergency department | 5311 (35.5%) | 689 (41.9%) | |
| Hospital ward | 1959 (13.1%) | 473 (28.8%) | |
| Other hospital | 1196 (8.0%) | 174 (10.6%) | |
| Other/unknown admission source | 49 (0.3%) | 1 (0.1%) | |
| Admission category | <0.001 | ||
| Emergency surgical admission | 2590 (17.3%) | 260 (15.8%) | |
| Medical ICU admission | 8343 (55.7%) | 1334 (81.1%) | |
| Planned ICU admission after elective surgery | 4040 (27.0%) | 51 (3.1%) | |
| ICU admission diagnosis | <0.001 | ||
| Cardiac medical diagnoses | 1454 (9.7%) | 422 (25.7%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 1075 (7.2%) | 131 (8.0%) | |
| Sepsis and other infections (incl. pneumonia) | 2182 (14.6%) | 464 (28.2%) | |
| Other medical diagnoses (incl. overdose) | 2139 (14.3%) | 151 (9.2%) | |
| Cardiothoracic & vascular surgery | 1176 (7.9%) | 72 (4.4%) | |
| Coronary artery bypass and/or valve surgery | 1511 (10.1%) | 19 (1.2%) | |
| Gastro-intestinal surgery | 1641 (11.0%) | 95 (5.8%) | |
| Neurological and neurosurgical diagnoses | 1000 (6.7%) | 149 (9.1%) | |
| Orthopaedic surgery | 606 (4.0%) | 13 (0.8%) | |
| Trauma | 1101 (7.4%) | 98 (6.0%) | |
| COVID-19 pneumonitis | 391 (2.6%) | 117 (7.1%) | <0.001 |
| Comorbidities and frailty | |||
| Diabetes | 3468 (23.2%) | 436 (26.5%) | 0.002 |
| Chronic - cardiovascular | 813 (5.4%) | 119 (7.2%) | 0.003 |
| Chronic - respiratory | 1080 (7.2%) | 166 (10.1%) | <0.001 |
| Chronic - dialysis dependent | 524 (3.5%) | 89 (5.4%) | <0.001 |
| Chronic - liver disease (cirrhosis) | 382 (2.6%) | 104 (6.3%) | <0.001 |
| Frailty category (clinical frailty scale – CFS) | <0.001 | ||
| Not frail (CFS <5) | 7565 (50.5%) | 612 (37.2%) | |
| Pre-frail (CFS 5 or 6) | 3970 (26.5%) | 604 (36.7%) | |
| Frail (CFS >6) | 814 (5.4%) | 222 (13.5%) | |
| Frailty score missing | 2624 (17.5%) | 207 (12.6%) | |
| Illness severity scores | |||
| APACHE III/IV score | 50.8 (21.4) | 85.9 (30.0) | <0.001 |
| ANZROD percent (mean, median [IQR]) | 7.2, 1.9 (0.6–7.3) | 41.1, 36.1 (15.4–65.5) | <0.001 |
| Therapies provided in ICU | |||
| Invasive ventilation | 5591 (37.3%) | 1052 (64.0%) | <0.001 |
| Renal replacement therapy | 657 (4.8%) | 359 (23.5%) | <0.001 |
| Extracorporeal membrane oxygenation | 61 (0.5%) | 28 (1.9%) | <0.001 |
| Inotropes | 6056 (44.6%) | 1172 (77.2%) | <0.001 |
| Invasive ventilation, renal replacement or ECMO | 5877 (39.3%) | 1123 (68.3%) | <0.001 |
| Daily staffing characteristics of the ICU | |||
| Overall daily percentage of experienced CCRNs throughout admission | 70.0 (55.2–81.1) | 66.7 (54.5–77.7) | <0.001 |
| Percentage of experienced CCRNs on day of admission | 69.7 (54.8–82.5) | 66.7 (53.8–78.9) | <0.001 |
| Critical care trained nurses | 12.0 (6.0–25.0) | 10.0 (5.0–22.0) | <0.001 |
| Early career/in training critical care nurses | 3.0 (1.0–7.0) | 4.0 (2.0–8.0) | <0.001 |
| Nurses without ICU experience redeployed into ICU | 0.0 (0.0–1.0) | 0.0 (0.0–2.0) | <0.001 |
| Nursing students & ‘non-nursing’ staff providing bedside care in ICU | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.71 |
| Hospital classification | <0.001 | ||
| Public rural/regional (4 ICUs) | 1894 (13%) | 177 (11%) | |
| Public metropolitan (6 ICUs) | 3555 (24%) | 468 (28%) | |
| Public tertiary (5 ICUs) | 6832 (46%) | 875 (53%) | |
| Private (5 ICUs) | 2692 (18%) | 125 (8%) | |
| Characteristics of the ICU on day of admission | |||
| Baseline business as usual ICU beds | 17.0 (10.0–26.0) | 17.0 (10.0–32.0) | <0.001 |
| Number of open available ICU beds | 12.0 (7.5–27.0) | 14.0 (9.0–32.0) | <0.001 |
| Number of vacant ICU beds | 1.9 (0.9–3.3) | 1.8 (0.8–3.0) | 0.12 |
| Occupancy | 87.0 (75.0–94.0) | 90.0 (79.0–95.0) | <0.001 |
| Activity Index of the ICU | |||
| Number of patients receiving 1:1 nursing in ICU | 8.8 (3.0–23.7) | 11.0 (5.0–28.0) | <0.001 |
| Number of ventilated patients in ICU | 4.0 (1.0–13.3) | 6.0 (2.0–15.3) | <0.001 |
| Number of COVID-19 patients in ICU | 1.0 (0.0–3.0) | 1.6 (0.0–4.5) | <0.001 |
| Number of patients on renal replacement therapy in ICU | 1.0 (0.0–2.0) | 1.0 (0.0–3.0) | <0.001 |
| Number of 1:2/HDU patients in ICU | 3.0 (1.3–5.0) | 3.0 (1.0–5.3) | 0.064 |
| Outcomes | |||
| In-ICU mortality | 0 (0.0%) | 1125 (68.4%) | N/A |
| Delirium in ICU | 885 (8.2%) | 141 (12.9%) | <0.001 |
| Pressure injury developed in ICU | 169 (1.5%) | 69 (5.9%) | <0.001 |
| Duration of ICU stay (days) | 1.9 (1.0–3.7) | 3.3 (1.2–6.9) | <0.001 |
| Ratio of observed to predicted length of ICU stay | 1.05 (0.65–1.77) | 1.37 (0.64–2.98) | <0.001 |
| Duration of stay in hospital (days) | 8.2 (4.4–15.1) | 7.0 (2.8–14.8) | <0.001 |
| After-hours discharge from ICU (ICU survivors only) | 2838 (19.0%) | 121 (23.3%) | 0.014 |
APACHE, Acute Physiology and Chronic Health Evaluation; ANZROD, Australian & New Zealand Risk of Death. CCRN, Critical Care Registered Nurse; HDU, high-dependency unit; ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
Table A2.
Supplementary methods information about the ICU Activity index
| A high Activity Index is a marker of ICU strain. The Activity index of the ICU was extracted from The Critical Health Resources Information System (CHRIS).33 It combines markers of aggregate patient acuity with overall available nursing resources to staff open beds within the ICU. The Activity index was calculated as: where 1:1 nursing = number of patients requiring 1:1 nurse to patient ratio; MV = number of ICU patients receiving invasive ventilation; RRT = number of ICU patients receiving renal replacement therapy; ECMO = number of ICU patients receiving extracorporeal membrane oxygenation (ECMO); COVIDs = number of ‘active’ COVID-19 patients requiring isolation within the ICU; and staffed ICU beds = total number of available, equipped and staffed bed spaces in the ICU, including any open additional surge beds. The number of staffed ICU beds is equal to the total number of nurses available to provide 1:1 care to ICU patients. Activity indices for each day at every site were summed and divided by the total number of values available for that 24-h period, to create a mean daily Activity index on the day of each patient's admission to ICU. For example, the Activity index of a ten-bed ICU where five beds were occupied by ventilated patients (five points) requiring 1:1 nursing (five points), of whom two were isolated for COVID-19 (two points), one bed was occupied by a non-ventilated patient requiring 1:1 nursing (one point) and there were four non-ventilated patients requiring 1:2 nursing (zero points) including one who had COVID-19 but was no longer in isolation precautions (zero points), had a value of 1.3. Patients in an ICU with a high Activity Index have an increased risk of death, afterhours discharge, readmission, and transfer to another ICU.15 |
Table A3.
Characteristics of study ICUs compared to ICUs in all other Victorian hospitals
| Other Victorian hospitals |
Study hospitals |
p value | |
|---|---|---|---|
| N = 26 | N = 20 | ||
| Number of patients per site | 438 (303–685) | 758 (562–1044) | 0.001 |
| Hospital type: n (%) | 0.063 | ||
| Public rural/regional | 8 (31%) | 4 (20%) | |
| Public metropolitan | 4 (15%) | 6 (30%) | |
| Public tertiary | 1 (4%) | 5 (25%) | |
| Private | 13 (50%) | 5 (25%) | |
| Demographics | |||
| Age in years | 65.4 (61.8–68.4) | 61.6 (59.6–64.8) | 0.019 |
| Proportion male (%) | 55.2 (52.1–57.4) | 56.9 (53.5–59.0) | 0.44 |
| Proportion elective surgical admissions (%) | 30.3 (6.5–67.5) | 16.6 (12.4–47.5) | 0.56 |
| Proportion medical admissions (%) | 57.2 (22.3–81.1) | 65.3 (40.4–70.7) | 0.86 |
| Proportion cardiac surgery (%) | 0 (0–18.2) | 0 (0–14.4) | 0.75 |
| Therapies (number of patients per site) | |||
| Invasive ventilation | 81 (14–211) | 235 (107–531) | 0.005 |
| Renal replacement therapy | 3 (0–17) | 37 (9–73) | <0.001 |
| Ventilated, renal replacement or ECMO | 89 (16–216) | 257 (114–553) | 0.005 |
| Illness severity and frailty scores | |||
| Frailty score (clinical frailty scale) | 3.4 (3.2–3.8) | 3.5 (3.3–3.7) | 0.79 |
| APACHE II score | 14.1 (12.3–16.1) | 15.9 (13.7–16.8) | 0.088 |
| APACHE III score | 48.1 (43.7–52.6) | 52.9 (46.8–57.4) | 0.13 |
| Predicted risk of death | 5.5 (3.6–9.7) | 10.5 (5.1–12.4) | 0.076 |
| Outcomes | |||
| In-hospital mortality | 5.6 (1.9–8.4) | 10.3 (5.3–11.6) | 0.012 |
| In-ICU mortality | 2.5 (0.7–4.8) | 6.4 (2.9–8.3) | 0.015 |
| Readmission to ICU | 3.0 (1.5–4.4) | 3.5 (2.1–4.5) | 0.71 |
| ICU length of stay in days | 1.8 (1.5–2.1) | 2.0 (1.7–2.2) | 0.23 |
| Hospital length of stay in days | 6.4 (4.4–8.6) | 7.6 (5.5–8.6) | 0.18 |
All statistics are median and interquartile value for sites during the study period (Dec 2021 to Sept 2022) unless otherwise stated. APACHE, Acute Physiological and Chronic Health Evaluation; ECMO, Extracorporeal membrane oxygenation.
Table A4.
Comparison of patients at participating sites who could be linked to staffing data to those where linkage was not possible (admitted on days went no staffing information was submitted.
| No Staffing Data |
Staffing Data Available |
p value | |
|---|---|---|---|
| N = 1653 | N = 16,618 | ||
| Age in years | 62.6 (17.5) | 61.5 (17.4) | 0.012 |
| Men | 994 (60.1%) | 9651 (58.1%) | 0.11 |
| Source of admission to ICU | <0.001 | ||
| Operating theatre | 893 (54.0%) | 6766 (40.7%) | |
| Emergency department | 473 (28.6%) | 6000 (36.1%) | |
| Hospital ward | 193 (11.7%) | 2432 (14.6%) | |
| Other hospital | 83 (5.0%) | 1370 (8.2%) | |
| Other/unknown admission source | 11 (0.7%) | 50 (0.3%) | |
| Admission category | <0.001 | ||
| Emergency surgical admission | 264 (16.0%) | 2850 (17.2%) | |
| Medical ICU admission | 757 (45.8%) | 9677 (58.2%) | |
| Planned ICU admission after elective surgery | 632 (38.2%) | 4091 (24.6%) | |
| ICU admission diagnosis | <0.001 | ||
| Cardiac medical diagnoses | 116 (7.0%) | 1876 (11.3%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 108 (6.5%) | 1206 (7.3%) | |
| Sepsis and other infections (incl. pneumonia) | 208 (12.6%) | 2646 (15.9%) | |
| Other medical diagnoses (incl. overdose) | 181 (10.9%) | 2290 (13.8%) | |
| Cardiothoracic & vascular surgery | 136 (8.2%) | 1248 (7.5%) | |
| Coronary artery bypass and/or valve surgery | 241 (14.6%) | 1530 (9.2%) | |
| Gastro-intestinal surgery | 193 (11.7%) | 1736 (10.4%) | |
| Neurological and neurosurgical diagnoses | 128 (7.7%) | 1149 (6.9%) | |
| Orthopaedic surgery | 129 (7.8%) | 619 (3.7%) | |
| Trauma | 131 (7.9%) | 1199 (7.2%) | |
| Other surgical diagnoses | 82 (5.0%) | 1119 (6.7%) | |
| COVID-19 pneumonitis | 42 (2.5%) | 508 (3.1%) | 0.24 |
| Comorbidities and frailty | |||
| Diabetes | 342 (20.7%) | 3904 (23.5%) | 0.010 |
| Chronic - cardiovascular | 163 (9.9%) | 932 (5.6%) | <0.001 |
| Chronic - respiratory | 115 (7.0%) | 1246 (7.5%) | 0.42 |
| Chronic - dialysis dependent | 42 (2.5%) | 613 (3.7%) | 0.017 |
| Chronic - liver disease (cirrhosis) | 21 (1.3%) | 486 (2.9%) | <0.001 |
| Frailty category | <0.001 | ||
| Not frail (CFS1-3) | 731 (44.2%) | 8177 (49.2%) | |
| Pre-frail (CFS 4,5) | 416 (25.2%) | 4574 (27.5%) | |
| Frail (CFS 6–8) | 98 (5.9%) | 1036 (6.2%) | |
| Frailty unknown | 408 (24.7%) | 2831 (17.0%) | |
| Illness severity scores | |||
| APACHE III/IV score | 52.2 (23.7) | 54.2 (24.7) | 0.002 |
| ANZROD percent | 7.7 (15.7) | 10.6 (18.4) | <0.001 |
| Hours in hospital prior to ICU admission | 10.1 (5.4–26.9) | 9.4 (4.8–24.5) | <0.001 |
| Therapies provided in ICU | |||
| Invasive ventilation | 654 (39.6%) | 6643 (40.0%) | 0.75 |
| Renal replacement therapy | 71 (4.7%) | 1016 (6.7%) | 0.002 |
| ECMO | 5 (0.3%) | 89 (0.6%) | 0.20 |
| Invasive ventilation, renal replacement or ECMO | 672 (40.7%) | 7000 (42.1%) | 0.25 |
| Inotropes | 658 (42.8%) | 7228 (47.9%) | <0.001 |
| No ventilation, renal replacement or ECMO | 981 (59.3%) | 9618 (57.9%) | 0.25 |
| Hospital classification | <0.001 | ||
| Public rural/regional (4 ICUs) | 180 (11%) | 2071 (12%) | |
| Public metropolitan (6 ICUs) | 266 (16%) | 4023 (24%) | |
| Public tertiary (5 ICUs) | 420 (25%) | 7707 (46%) | |
| Private (5 ICUs) | 787 (48%) | 2817 (17%) | |
| Characteristics of the ICU on day of admission | |||
| Baseline business-as-usual ICU beds | 11.0 (7.0–26.0) | 17.0 (10.0–26.0) | <0.001 |
| Number of open available ICU beds | 10.5 (6.0–17.0) | 12.3 (8.0–27.3) | <0.001 |
| Number of vacant ICU beds | 2.5 (1.3–4.3) | 1.8 (0.9–3.3) | <0.001 |
| Occupancy | 80.0 (66.0–91.0) | 88.0 (75.0–94.0) | <0.001 |
| Activity Index of the ICU | 1.0 (0.5–1.5) | 1.3 (0.8–1.6) | <0.001 |
| Number of ‘ICU equivalents' | 8.0 (3.5–14.0) | 10.5 (5.5–25.5) | <0.001 |
| Number of patients receiving 1:1 nursing in ICU | 6.0 (1.5–12.5) | 9.0 (3.5–24.0) | <0.001 |
| Number of ventilated patients in ICU | 2.0 (1.0–6.0) | 4.5 (1.3–13.5) | <0.001 |
| Number of COVID-19 patients in ICU | 1.0 (0.0–3.5) | 1.0 (0.0–3.0) | <0.001 |
| Number of patients on renal replacement therapy in ICU | 0.0 (0.0–2.0) | 1.0 (0.0–2.0) | <0.001 |
| Number of 1:2/HDU patients in ICU | 3.0 (1.7–5.0) | 3.0 (1.3–5.0) | 0.047 |
| Outcomes | |||
| In-hospital mortality | 143 (8.7%) | 1645 (9.9%) | 0.10 |
| In-ICU mortality | 103 (6.2%) | 1125 (6.8%) | 0.40 |
| Delirium in ICU | 117 (8.6%) | 1026 (8.6%) | 0.94 |
| Pressure injury developed in ICU | 30 (2.2%) | 238 (1.9%) | 0.52 |
| Duration of ICU stay (days) | 1.9 (1.0–3.4) | 2.0 (1.0–3.9) | 0.006 |
| Ratio of observed to predicted length of ICU stay | 1.09 (0.71–1.76) | 1.07 (0.65–1.84) | 0.36 |
| Duration of stay in hospital (days) | 8.5 (4.9–14.4) | 8.1 (4.2–15.1) | 0.25 |
| After-hours discharge from ICU (ICU survivors only) | 228 (14.7%) | 2959 (19.1%) | <0.001 |
APACHE, Acute Physiology and Chronic Health Evaluation; ANZROD, Australian & New Zealand Risk of Death. CCRN, Critical Care Registered Nurse; HDU, high-dependency unit; ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
Table A5.
Mixed effects hierarchical multivariable logistic regression for in-hospital mortality adjusted for sex, illness severity, COVID-19 status, frailty, ICU activity index and hospital type (with site as random effect) in all patients and in subgroups categorised by a. invasive therapies (invasive ventilation, renal replacement or ECMO), b. no invasive therapies and c. patients in public hospital ICUs.
| Whole study cohort |
Subgroups |
|||||||
|---|---|---|---|---|---|---|---|---|
| All patients |
a. Invasive ventilation, renal replacement, ECMO |
b. No invasive ventilation, renal replacement, ECMO |
c. Public Hospital ICUs |
|||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| CCRN >75% | Reference value | Reference value | Reference value | Reference value | ||||
| CCRN 50–75% | 1.21 (1.02–1.45) | 0.032 | 1.35 (1.11–1.64) | 0.003 | 1.05 (0.79–1.39) | 0.76 | 1.27 (1.06–1.52) | 0.011 |
| CCRN <50% | 1.21 (0.94–1.55) | 0.14 | 1.28 (0.98–1.66) | 0.07 | 1.14 (0.76–1.71) | 0.52 | 1.24 (0.97–1.59) | 0.08 |
| Male | 1.29 (1.13–1.46) | <0.001 | 1.07 (.91–1.26) | 0.41 | 1.51 (1.22–1.87) | <0.001 | 1.28 (1.12–1.47) | <0.001 |
| Australian & New Zealand Risk of Death (%) | 1.06 (1.06–1.07) | <0.001 | 1.06 (1.05–1.06) | <0.001 | 1.07 (1.07–1.08) | <0.001 | 1.06 (1.06–1.06) | <0.001 |
| COVID-19 patient | 2.61 (2.11–3.21) | <0.001 | 2.92 (2.21–3.86) | <0.001 | 2.48 (1.77–3.46) | <0.001 | 2.59 (2.10–3.20) | <0.001 |
| Frailty category (clinical frailty scale – CFS) | ||||||||
| Not frail (CFS <5) | Reference value | Reference value | Reference value | Reference value | ||||
| Pre-frail (CFS 5 or 6) | 1.67 (1.44–1.94) | <0.001 | 1.54 (1.29–1.85) | <0.001 | 2.62 (1.96–3.49) | <0.001 | 1.62 (1.40–1.89) | <0.001 |
| Frail (CFS >6) | 2.89 (2.34–3.57) | <0.001 | 1.99 (1.44–2.75) | <0.001 | 6.10 (4.39–8.48) | <0.001 | 2.60 (2.10–3.23) | <0.001 |
| Frailty score missing | 1.49 (1.08–2.03) | 0.014 | 0.86 (0.64–1.14) | 0.29 | 3.18 (1.98–5.11) | <0.001 | 1.09 (0.77–1.55) | 0.62 |
| ICU activity index | 1.03 (0.86–1.24) | 0.72 | 0.95 (0.76–1.19) | 0.65 | 1.01 (0.76–1.34) | 0.96 | 1.01 (0.84–1.22) | 0.91 |
| Hospital classification | ||||||||
| Tertiary (5 ICUs) | Reference value | Reference value | Reference value | Reference value | ||||
| Metropolitan (6 ICUs) | 1.09 (0.83–1.44) | 0.54 | 1.06 (0.85–1.33) | 0.59 | 1.38 (0.90–2.12) | 0.14 | 1.02 (0.80–1.29) | 0.89 |
| Rural/regional (4 ICUs) | 1.03 (0.71–1.49) | 0.89 | 1.18 (0.81–1.73) | 0.39 | 1.25 (0.72–2.17) | 0.43 | 0.94 (0.67–1.32) | 0.73 |
| Private (5 ICUs) | 0.94 (0.64–1.38) | 0.75 | 1.16 (0.76–1.76) | 0.48 | 1.04 (0.60–1.82) | 0.88 | Not applicable | |
| AUROC | 0.892 | 0.878 | 0.892 | 0.886 | ||||
| Brier score | 0.063 | 0.093 | 0.040 | 0.070 | ||||
Each column represents a separate multivariable hierarchical logistic regression model. The Australian and New Zealand Risk of Death (ANZROD) model includes age, acute physiological and biochemical disturbance, chronic comorbidities, treatment limitations, elective surgical status and source of admission with individual predictive equations for each ICU admission diagnosis. Sex, frailty and COVID-19 status were entered separately into each model because these are not included in ANZROD.
AUROC, Area under receiver operating characteristic curve; CCRN, Critical Care Registered Nurse; ECMO, Extra-corporeal Membrane Oxygenation, ICU, Intensive Care Unit: OR (95% CI), Adjusted odds ratio and 95% confidence interval.
Table A6.
Subgroup of 7000 patients who received invasive critical care therapies (invasive ventilation, renal replacement, or extracorporeal membrane oxygenation) – baseline characteristics by category of percentage of critical care registered nurses (CCRN) in each ICU.
| <50 % CCRN |
50–75% CCRN |
>75% CCRN |
p value | |
|---|---|---|---|---|
| N = 952 | N = 3297 | N = 2751 | ||
| Age in yearsa | 57.5 (17.3) | 58.8 (16.9) | 60.3 (16.9) | <0.001 |
| Men | 616 (64.7%) | 2138 (64.8%) | 1818 (66.1%) | 0.55 |
| Source of admission to ICU | <0.001 | |||
| Operating theatre | 377 (39.6%) | 1290 (39.1%) | 1465 (53.3%) | |
| Emergency department | 366 (38.4%) | 1234 (37.4%) | 777 (28.2%) | |
| Hospital ward | 85 (8.9%) | 398 (12.1%) | 235 (8.5%) | |
| Other hospital | 121 (12.7%) | 362 (11.0%) | 265 (9.6%) | |
| Other/unknown admission source | 3 (0.3%) | 13 (0.4%) | 9 (0.3%) | |
| Admission category | <0.001 | |||
| Emergency surgical admission | 216 (22.7%) | 742 (22.5%) | 513 (18.6%) | |
| Medical ICU admission | 572 (60.1%) | 1984 (60.2%) | 1239 (45.0%) | |
| Planned ICU admission after elective surgery | 164 (17.2%) | 571 (17.3%) | 999 (36.3%) | |
| ICU admission diagnosis | <0.001 | |||
| Cardiac medical diagnoses | 122 (12.8%) | 422 (12.8%) | 252 (9.2%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 63 (6.6%) | 189 (5.7%) | 95 (3.5%) | |
| Sepsis and other infections (incl. pneumonia) | 145 (15.2%) | 503 (15.3%) | 269 (9.8%) | |
| Other medical diagnoses (incl. overdose) | 125 (13.1%) | 475 (14.4%) | 273 (9.9%) | |
| Cardiothoracic & vascular surgery | 68 (7.1%) | 232 (7.0%) | 206 (7.5%) | |
| Coronary artery bypass and/or valve surgery | 134 (14.1%) | 509 (15.4%) | 871 (31.7%) | |
| Gastro-intestinal surgery | 67 (7.0%) | 247 (7.5%) | 168 (6.1%) | |
| Neurological and neurosurgical diagnoses | 56 (5.9%) | 299 (9.1%) | 277 (10.1%) | |
| Orthopaedic surgery | 5 (0.5%) | 20 (0.6%) | 39 (1.4%) | |
| Trauma | 135 (14.2%) | 268 (8.1%) | 222 (8.1%) | |
| Other surgical diagnoses | 32 (3.4%) | 133 (4.0%) | 79 (2.9%) | |
| COVID-19 pneumonitis | 53 (5.6%) | 145 (4.4%) | 31 (1.1%) | <0.001 |
| Comorbidities and frailty | ||||
| Diabetes | 202 (21.2%) | 805 (24.4%) | 563 (20.5%) | <0.001 |
| Chronic - cardiovascular | 34 (3.6%) | 120 (3.6%) | 81 (2.9%) | 0.30 |
| Chronic - respiratory | 61 (6.4%) | 258 (7.8%) | 93 (3.4%) | <0.001 |
| Chronic - dialysis dependent | 29 (3.0%) | 170 (5.2%) | 89 (3.2%) | <0.001 |
| Chronic - liver disease (cirrhosis) | 18 (1.9%) | 174 (5.3%) | 79 (2.9%) | <0.001 |
| Frailty category | <0.001 | |||
| Not frail (CFS1-3) | 573 (60.2%) | 1952 (59.2%) | 1058 (38.5%) | |
| Pre-frail (CFS 4,5) | 323 (33.9%) | 934 (28.3%) | 597 (21.7%) | |
| Frail (CFS 6–8) | 37 (3.9%) | 188 (5.7%) | 77 (2.8%) | |
| Frailty unknown | 19 (2.0%) | 223 (6.8%) | 1019 (37.0%) | |
| Illness Severity Scores | ||||
| APACHE II scorea | 19.3 (8.4) | 19.5 (8.2) | 16.4 (8.3) | <0.001 |
| APACHE III scorea | 64.3 (29.1) | 65.2 (27.9) | 60.2 (26.5) | <0.001 |
| ANZROD percent (median IQR)b | 16.6 (23.6) | 17.0 (23.4) | 14.4 (22.9) | <0.001 |
| ANZROD percent (mean, SD)a | 5.2 (1.1–21.1) | 5.6 (1.2–23.3) | 3.0 (0.8–17.5) | <0.001 |
| Therapies provided in ICU | ||||
| Invasive ventilation | 903 (94.9%) | 3101 (94.1%) | 2639 (95.9%) | 0.004 |
| Renal replacement therapy | 163 (17.3%) | 562 (17.6%) | 291 (13.4%) | <0.001 |
| Extracorporeal membrane oxygenation | 32 (3.4%) | 44 (1.4%) | 13 (0.6%) | <0.001 |
| Inotropes | 697 (73.8%) | 2481 (77.8%) | 1669 (78.3%) | 0.015 |
| Hospital Classification | <0.001 | |||
| Public rural/regional (4 ICUs) | 108 (11%) | 292 (9%) | 45 (2%) | |
| Public metropolitan (6 ICUs) | 287 (30%) | 960 (29%) | 207 (8%) | |
| Public tertiary (5 ICUs) | 554 (58%) | 1941 (59%) | 1905 (69%) | |
| Private (5 ICUs) | 3 (0%) | 104 (3%) | 594 (22%) | |
| Primary outcome | ||||
| In-hospital mortality | 169 (17.8%) | 602 (18.3%) | 352 (12.8%) | <0.001 |
| Secondary outcomes | ||||
| In-ICU mortality | 137 (14.4%) | 462 (14.0%) | 284 (10.3%) | <0.001 |
| Delirium in ICU | 166 (21.3%) | 407 (15.9%) | 63 (5.4%) | <0.001 |
| Pressure injury developed in ICU | 52 (6.1%) | 121 (4.6%) | 39 (3.2%) | 0.007 |
| Duration of ICU stay (days) | 3.9 (1.8–8.1) | 3.4 (1.8–7.1) | 2.8 (1.7–5.0) | <0.001 |
| Ratio of observed to predicted length of ICU stay | 1.37 (0.69–2.58) | 1.24 (0.68–2.34) | 1.11 (0.65–1.87) | <0.001 |
| Duration of stay in hospital (days) | 11.1 (5.4–20.3) | 10.9 (5.8–20.8) | 9.8 (5.9–16.9) | <0.001 |
| After-hours discharge from ICUa | 348 (25.5%) | 960 (22.5%) | 461 (12.3%) | <0.001 |
APACHE, Acute Physiology and Chronic Health Evaluation; ANZROD, Australian & New Zealand Risk of Death. ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
aData reported as mean (standard deviation).
bmedian (interquartile range); all other data reported as number (percentage).
Table A7.
Subgroup of 9618 patients who did not receive invasive critical care therapies (i.e. no invasive ventilation, renal replacement or extracorporeal membrane oxygenation) – baseline characteristics by category of percentage of critical care registered nurses (CCRN) in each ICU.
| <50 % CCRN |
50–75% CCRN |
>75% CCRN |
p value | |
|---|---|---|---|---|
| N = 1408 | N = 4398 | N = 3812 | ||
| Age in years | 63.0 (18.1) | 62.9 (17.7) | 63.4 (17.3) | 0.39 |
| Men | 785 (55.8%) | 2344 (53.3%) | 1950 (51.2%) | 0.01 |
| Source of admission to ICU | <0.001 | |||
| Operating theatre | 380 (27.0%) | 1385 (31.5%) | 1869 (49.0%) | |
| Emergency department | 699 (49.6%) | 1924 (43.7%) | 1000 (26.2%) | |
| Hospital ward | 250 (17.8%) | 816 (18.6%) | 648 (17.0%) | |
| Other hospital | 75 (5.3%) | 265 (6.0%) | 282 (7.4%) | |
| Other/unknown admission source | 4 (0.3%) | 8 (0.2%) | 13 (0.3%) | |
| Admission category | <0.001 | |||
| Emergency surgical admission | 190 (13.5%) | 637 (14.5%) | 552 (14.5%) | |
| Medical ICU admission | 1022 (72.6%) | 2986 (67.9%) | 1874 (49.2%) | |
| Planned ICU admission after elective surgery | 196 (13.9%) | 775 (17.6%) | 1386 (36.4%) | |
| ICU admission diagnosis | <0.001 | |||
| Cardiac medical diagnoses | 183 (13.0%) | 538 (12.2%) | 359 (9.4%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 149 (10.6%) | 471 (10.7%) | 239 (6.3%) | |
| Sepsis and other infections (incl. pneumonia) | 279 (19.8%) | 875 (19.9%) | 575 (15.1%) | |
| Other medical diagnoses (incl. overdose) | 236 (16.8%) | 716 (16.3%) | 465 (12.2%) | |
| Cardiothoracic & vascular surgery | 72 (5.1%) | 308 (7.0%) | 362 (9.5%) | |
| Coronary artery bypass and/or valve surgery | 0 (0.0%) | 5 (0.1%) | 11 (0.3%) | |
| Gastro-intestinal surgery | 137 (9.7%) | 486 (11.1%) | 631 (16.6%) | |
| Neurological and neurosurgical diagnoses | 62 (4.4%) | 203 (4.6%) | 252 (6.6%) | |
| Orthopaedic surgery | 39 (2.8%) | 163 (3.7%) | 353 (9.3%) | |
| Trauma | 136 (9.7%) | 297 (6.8%) | 141 (3.7%) | |
| Other surgical diagnoses | 115 (8.2%) | 336 (7.6%) | 424 (11.1%) | |
| COVID-19 pneumonitis | 52 (3.7%) | 152 (3.5%) | 75 (2.0%) | <0.001 |
| Comorbidities and frailty | ||||
| Diabetes | 349 (24.8%) | 1171 (26.6%) | 814 (21.4%) | <0.001 |
| Chronic - cardiovascular | 115 (8.2%) | 292 (6.6%) | 290 (7.6%) | 0.09 |
| Chronic - respiratory | 137 (9.7%) | 467 (10.6%) | 230 (6.0%) | <0.001 |
| Chronic - dialysis dependent | 34 (2.4%) | 187 (4.3%) | 104 (2.7%) | <0.001 |
| Chronic - liver disease (cirrhosis) | 32 (2.3%) | 116 (2.6%) | 67 (1.8%) | 0.03 |
| Frailty category | <0.001 | |||
| Not frail (CFS1-3) | 824 (58.5%) | 2316 (52.7%) | 1454 (38.1%) | |
| Pre-frail (CFS 4,5) | 420 (29.8%) | 1342 (30.5%) | 958 (25.1%) | |
| Frail (CFS 6–8) | 131 (9.3%) | 389 (8.8%) | 214 (5.6%) | |
| Frailty unknown | 33 (2.3%) | 351 (8.0%) | 1186 (31.1%) | |
| Illness severity scores | ||||
| APACHE II scorea | 14.4 (6.4) | 14.6 (6.4) | 13.0 (6.2) | <0.001 |
| APACHE III scorea | 47.1 (20.5) | 49.4 (20.6) | 46.1 (19.2) | <0.001 |
| ANZROD percent (median IQR)b | 6.9 (12.5) | 7.4 (13.1) | 5.8 (11.8) | <0.001 |
| ANZROD percent (mean, SD)a | 2.1 (0.5–7.2) | 2.2 (0.6–7.4) | 1.3 (0.4–5.1) | <0.001 |
| Therapies provided in ICU | ||||
| Invasive ventilation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Renal replacement therapy | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Extracorporeal membrane oxygenation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Inotropes | 337 (24.2%) | 1282 (30.4%) | 762 (23.6%) | <0.001 |
| Hospital Classification | <0.001 | |||
| Public rural/regional (4 ICUs) | 594 (42%) | 887 (20%) | 145 (4%) | |
| Public metropolitan (6 ICUs) | 461 (33%) | 1639 (37%) | 469 (12%) | |
| Public tertiary (5 ICUs) | 346 (25%) | 1555 (35%) | 1406 (37%) | |
| Private (5 ICUs) | 7 (0%) | 317 (7%) | 1792 (47%) | |
| Primary outcome | ||||
| In-hospital mortality | 83 (5.9%) | 257 (5.8%) | 182 (4.8%) | 0.07 |
| Secondary outcomes | ||||
| In-ICU mortality | 43 (3.1%) | 132 (3.0%) | 67 (1.8%) | <0.001 |
| Delirium in ICU | 92 (7.5%) | 211 (5.8%) | 87 (3.4%) | <0.001 |
| Pressure injury developed in ICU | 5 (0.4%) | 14 (0.4%) | 7 (0.3%) | 0.75 |
| Duration of ICU stay (days) | 1.7 (0.9–3.1) | 1.7 (0.9–2.9) | 1.2 (0.8–2.2) | <0.001 |
| Ratio of observed to predicted length of ICU stay | 1.10 (0.64–1.91) | 1.02 (0.63–1.71) | 0.95 (0.64–1.50) | <0.001 |
| Duration of stay in hospital (days) | 6.3 (3.2–11.3) | 7.0 (3.9–12.7) | 7.0 (3.7–12.7) | <0.001 |
| After-hours discharge from ICUa | 348 (25.5%) | 960 (22.5%) | 461 (12.3%) | <0.001 |
APACHE, Acute Physiology and Chronic Health Evaluation; ANZROD, Australian & New Zealand Risk of Death; ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
aData reported as mean (standard deviation).
bMedian (interquartile range); all other data reported as number (percentage).
Table A8.
Subgroup of 13,801 patients who were treated in public hospital ICUs – baseline characteristics by category of percentage of critical care registered nurses (CCRN) in each ICU.
| <50 % CCRN |
50–75% CCRN |
>75% CCRN |
p value | |
|---|---|---|---|---|
| N = 2350 | N = 7274 | N = 4177 | ||
| Age in years | 60.7 (18.0) | 60.8 (17.5) | 59.1 (17.6) | <0.001 |
| Men | 1395 (59.4%) | 4245 (58.4%) | 2520 (60.3%) | 0.11 |
| Source of admission to ICU | <0.001 | |||
| Operating theatre | 749 (31.9%) | 2361 (32.5%) | 1521 (36.4%) | |
| Emergency department | 1064 (45.3%) | 3115 (42.8%) | 1577 (37.8%) | |
| Hospital ward | 334 (14.2%) | 1164 (16.0%) | 594 (14.2%) | |
| Other hospital | 196 (8.3%) | 613 (8.4%) | 467 (11.2%) | |
| Other/unknown admission source | 7 (0.3%) | 21 (0.3%) | 18 (0.4%) | |
| Admission category | <0.001 | |||
| Emergency surgical admission | 406 (17.3%) | 1320 (18.1%) | 780 (18.7%) | |
| Medical ICU admission | 1592 (67.7%) | 4864 (66.9%) | 2548 (61.0%) | |
| Planned ICU admission after elective surgery | 352 (15.0%) | 1090 (15.0%) | 849 (20.3%) | |
| ICU admission diagnosis | <0.001 | |||
| Cardiac medical diagnoses | 305 (13.0%) | 934 (12.8%) | 456 (10.9%) | |
| Respiratory medical diagnoses (excl. pneumonia) | 212 (9.0%) | 648 (8.9%) | 263 (6.3%) | |
| Sepsis and other infections (incl. pneumonia) | 423 (18.0%) | 1350 (18.6%) | 696 (16.7%) | |
| Other medical diagnoses (incl. overdose) | 360 (15.3%) | 1160 (15.9%) | 578 (13.8%) | |
| Cardiothoracic & vascular surgery | 139 (5.9%) | 484 (6.7%) | 312 (7.5%) | |
| Coronary artery bypass and/or valve surgery | 131 (5.6%) | 457 (6.3%) | 501 (12.0%) | |
| Gastro-intestinal surgery | 201 (8.6%) | 656 (9.0%) | 356 (8.5%) | |
| Neurological and neurosurgical diagnoses | 118 (5.0%) | 471 (6.5%) | 404 (9.7%) | |
| Orthopaedic surgery | 44 (1.9%) | 108 (1.5%) | 55 (1.3%) | |
| Trauma | 271 (11.5%) | 561 (7.7%) | 339 (8.1%) | |
| Other surgical diagnoses | 146 (6.2%) | 445 (6.1%) | 217 (5.2%) | |
| COVID-19 pneumonitis | 105 (4.5%) | 291 (4.0%) | 97 (2.3%) | <0.001 |
| Comorbidities and frailty | ||||
| Diabetes | 549 (23.4%) | 1918 (26.4%) | 1058 (25.3%) | 0.014 |
| Chronic - cardiovascular | 149 (6.3%) | 389 (5.3%) | 117 (2.8%) | <0.001 |
| Chronic - respiratory | 198 (8.4%) | 707 (9.7%) | 211 (5.1%) | <0.001 |
| Chronic - dialysis dependent | 63 (2.7%) | 346 (4.8%) | 138 (3.3%) | <0.001 |
| Chronic - liver disease (cirrhosis) | 50 (2.1%) | 288 (4.0%) | 141 (3.4%) | <0.001 |
| Frailty category | <0.001 | |||
| Not frail (CFS1-3) | 1394 (59.3%) | 4208 (57.8%) | 1976 (47.3%) | |
| Pre-frail (CFS 4,5) | 742 (31.6%) | 2233 (30.7%) | 1099 (26.3%) | |
| Frail (CFS 6–8) | 168 (7.1%) | 567 (7.8%) | 214 (5.1%) | |
| Frailty unknown | 46 (2.0%) | 266 (3.7%) | 888 (21.3%) | |
| Illness severity scores | ||||
| APACHE II score | 16.4 (7.7) | 16.9 (7.6) | 14.8 (8.1) | <0.001 |
| APACHE III score | 54.1 (25.8) | 56.8 (25.4) | 54.7 (25.5) | <0.001 |
| ANZROD percent | 10.9 (18.5) | 12.0 (19.1) | 12.6 (20.5) | 0.002 |
| ANZROD percent | 2.9 (0.7–11.2) | 3.4 (0.9–13.7) | 3.3 (0.9–13.7) | <0.001 |
| Therapies provided in ICU | ||||
| Invasive ventilation | 900 (38.3%) | 3002 (41.3%) | 2065 (49.4%) | <0.001 |
| Renal replacement therapy | 163 (7.0%) | 553 (7.8%) | 259 (7.7%) | 0.46 |
| ECMO | 32 (1.4%) | 44 (0.6%) | 12 (0.4%) | <0.001 |
| Inotropes | 1030 (44.2%) | 3668 (51.8%) | 1823 (55.2%) | <0.001 |
| Hospital Classification | <0.001 | |||
| Rural/regional (4 ICUs) | 702 (30%) | 1179 (16%) | 190 (5%) | |
| Metropolitan (6 ICUs) | 748 (32%) | 2599 (36%) | 676 (16%) | |
| Tertiary (5 ICUs) | 900 (38%) | 3496 (48%) | 3311 (79%) | |
| Primary outcome | ||||
| In-hospital mortality | 251 (10.7%) | 844 (11.6%) | 425 (10.2%) | 0.054 |
| Secondary outcomes | ||||
| In-ICU mortality | 179 (7.6%) | 586 (8.1%) | 314 (7.5%) | 0.54 |
| Delirium in ICU | 258 (12.9%) | 611 (10.4%) | 93 (5.6%) | <0.001 |
| Pressure injury developed in ICU | 57 (2.7%) | 135 (2.3%) | 44 (2.6%) | 0.46 |
| Duration of ICU stay (days) | 2.2 (1.1–4.8) | 2.2 (1.1–4.4) | 2.0 (1.0–3.7) | <0.001 |
| Ratio of observed to predicted length of ICU stay | 1.18 (0.66–2.16) | 1.12 (0.65–1.97) | 0.95 (0.56–1.62) | <0.001 |
| Duration of stay in hospital (days) | 7.8 (3.8–14.8) | 8.3 (4.3–15.9) | 8.3 (4.3–15.5) | <0.001 |
| After-hours discharge from ICUa | 552 (25.4%) | 1555 (23.3%) | 725 (18.8%) | <0.001 |
APACHE, Acute Physiology and Chronic Health Evaluation; ANZROD, Australian & New Zealand Risk of Death; ICU, Intensive Care Unit. A vacant ICU bed is one that is not occupied by a patient but is available, equipped and can be staffed with 1:1 nursing ratio. A staffed ICU bed is equipped and can be staffed with 1:1 nursing ratio but may or may not be filled by a patient.
aData reported as mean (standard deviation).
bMedian (interquartile range); all other data reported as number (percentage).
Table A9.
List of participating hospitals in the study.
| Alfred Hospital ICU |
| Angliss Hospital ICU |
| Austin Hospital ICU |
| Bendigo Health Care Group ICU |
| Dandenong Hospital ICU |
| Epworth Freemasons Hospital ICU |
| Epworth Geelong ICU |
| Epworth Hospital (Richmond) ICU |
| Footscray Hospital ICU |
| Frankston Hospital ICU |
| Latrobe Regional Hospital ICU |
| Mildura Base Public Hospital ICU |
| Northeast Health Wangaratta ICU |
| Peninsula Private Hospital ICU |
| Royal Melbourne Hospital ICU |
| St John of God Hospital (Bendigo) ICU |
| St Vincent's Hospital (Melbourne) ICU |
| Sunshine Hospital ICU |
| The Northern Hospital ICU |
| University Hospital Geelong ICU |
Fig. A1.
Inclusions & exclusions.
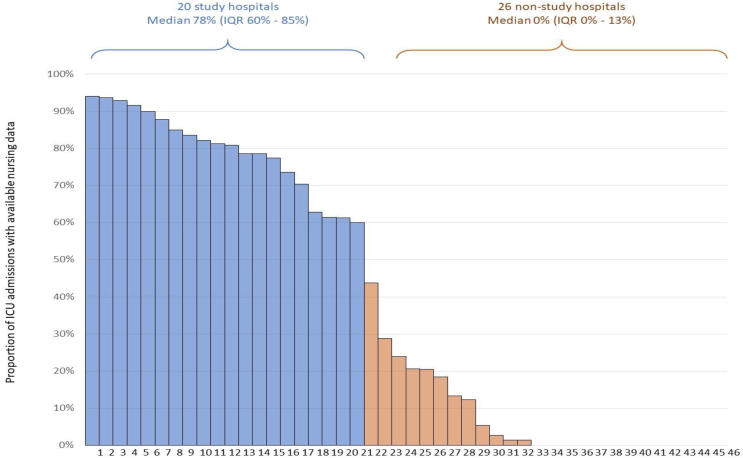
Fig. A2.
Proportion of nursing data per site.
References
- 1.Chamberlain D., Pollock W., Fulbrook P. ACCCN workforce standards for intensive care nursing: systematic and evidence review, development, and appraisal. Aust Crit Care. 2018;31:292–302. doi: 10.1016/j.aucc.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Australian College of Critical Care Nurses . 2016. ACCCN workforce standards for intensive care nursing. [DOI] [PubMed] [Google Scholar]
- 3.College of Intensive Care Medicine of Australia and New Zealand . 2016. Minimum standards for intensive care units. [Google Scholar]
- 4.Australian College of Critical Care Nurses . 2003. ACCCN ICU staffing position statement (2003) on intensive care nursing staffing. [Google Scholar]
- 5.Williams G., Clarke T. A consensus driven method to measure the required number of intensive care nurses in Australia. Aust Crit Care. 2001;14:106–115. doi: 10.1016/S1036-7314(01)80027-8. [DOI] [PubMed] [Google Scholar]
- 6.Bellomo R., Stow P.J., Hart G.K. Why is there such a difference in outcome between Australian intensive care units and others? Curr Opin Anesthesiol. 2007;20:100–105. doi: 10.1097/ACO.0b013e32802c7cd5. [DOI] [PubMed] [Google Scholar]
- 7.Neuraz A., Guérin C., Payet C., Polazzi S., Aubrun F., Dailler F., et al. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit Care Med. 2015;43:1587–1594. doi: 10.1097/CCM.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 8.Rae P.J., Pearce S., Greaves P.J., Dall’Ora C., Griffiths P., Endacott R. Outcomes sensitive to critical care nurse staffing levels: a systematic review. Intensive Crit Care Nurs. 2021;67:103110. doi: 10.1016/j.iccn.2021.103110. [DOI] [PubMed] [Google Scholar]
- 9.Driscoll A., Grant M.J., Carroll D., Dalton S., Deaton C., Jones I., et al. The effect of nurse-to-patient ratios on nurse-sensitive patient outcomes in acute specialist units: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2018;17:6–22. doi: 10.1177/1474515117721561. [DOI] [PubMed] [Google Scholar]
- 10.Ross P., Hodgson C.L., Ilic D., Watterson J., Gowland E., Collins K., et al. The impact of nursing skill-mix on adverse events in intensive care: a single centre cohort study. Contemp Nurse. 2023:1–13. doi: 10.1080/10376178.2023.2207687. ahead-of-print. [DOI] [PubMed] [Google Scholar]
- 11.Pilcher D., Paul E., Bailey M., Huckson S. The Australian and New Zealand Risk of Death (ANZROD) model: getting mortality prediction right for intensive care units. Crit Care Resusc. 2014;16:3–4. 2014/03/05. [PubMed] [Google Scholar]
- 12.Department of Health Victoria . 2021. Coronavirus (COVID-19) Intensive Care Unit surge workforce models of care delivery. [Google Scholar]
- 13.Topple M., Jaspers R., Watterson J., et al. Australian Critical Care; 2022. Nursing workforce deployment and intensive care unit strain during the COVID-19 pandemic in Victoria, Australia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Software SS . 2020. Stata version 16.1. Texas: College Station. [Google Scholar]
- 15.Pilcher D.V., Hensman T., Bihari S., Bailey M., McClure J., Nicholls M., et al. Measuring the impact of ICU strain on mortality, after-hours discharge, discharge delay, interhospital transfer, and readmission in Australia with the activity index. Crit Care Med. 2023;51:1623–1637. doi: 10.1097/CCM.0000000000005985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGahan M., Kucharski G., Coyer F. Nurse staffing levels and the incidence of mortality and morbidity in the adult intensive care unit: a literature review. Aust Crit Care. 2012;25:64–77. doi: 10.1016/j.aucc.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Ross P., Serpa-Neto A., Chee Tan S., Watterson J., Ilic D., Hodgson C.L., et al. The relationship between nursing skill mix and severity of illness of patients admitted in Australian and New Zealand intensive care units. Aust Crit Care. 2023 doi: 10.1016/j.aucc.2022.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Kelly D.M., Kutney-Lee A., McHugh M.D., Sloane D.M., Aiken L.H. Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults. Crit Care Med. 2014;42:1089–1095. doi: 10.1097/CCM.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Assadian O., Toma C.D., Rowley S.D. Implications of staffing ratios and workload limitations on healthcare-associated infections and the quality of patient care. Crit Care Med. 2007;35:296–298. doi: 10.1097/01.CCM.0000251291.65097.8A. [DOI] [PubMed] [Google Scholar]
- 20.Kleinpell R., Blot S., Boulanger C., Fulbrook P., Blackwood B. International critical care nursing considerations and quality indicators for the 2017 surviving sepsis campaign guidelines. Intensive Care Med. 2019;45:1663–1666. doi: 10.1007/s00134-019-05780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Midega T.D., Bozza F.A., Machado F.R., Guimarães H.P., Salluh J.I., Nassar A.P., et al. Organizational factors associated with adherence to low tidal volume ventilation: a secondary analysis of the CHECKLIST-ICU database. Ann Intensive Care. 2020;10:1–10. doi: 10.1186/s13613-020-00687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffiths P., Recio-Saucedo A., Dall’Ora C., Briggs J., Maruotti A., Meredith P., et al. The association between nurse staffing and omissions in nursing care: a systematic review. J Adv Nurs. 2018;74:1474–1487. doi: 10.1111/jan.13564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincelette C., D’Aragon F., Stevens L.-M., Rochefort C.M. The characteristics and factors associated with omitted nursing care in the intensive care unit: a cross-sectional study. Intensive Crit Care Nurs. 2022:103343. doi: 10.1016/j.iccn.2022.103343. [DOI] [PubMed] [Google Scholar]
- 24.Tan S.C., Evans T., Durie M.L., Secombe P.J., Pilcher D. Mortality among people admitted to Australian intensive care units for reasons other than COVID-19 during the COVID-19 pandemic: a retrospective cohort study. Med J Aust. 2023 doi: 10.5694/mja2.51933. [DOI] [PubMed] [Google Scholar]
- 25.Gibney R.T.N., Blackman C., Gauthier M., Fan E., Fowler R., Johnston C., et al. COVID-19 pandemic: the impact on Canada’s intensive care units. 2022. [Google Scholar]
- 26.McCarthy C., Boniol M., Daniels K., Cometto G., Diallo K., Lawani A., et al. State of the world’s nursing 2020: investing in education, jobs and leadership. World Health Organization; Geneva: 2020. Report no. 9789240003286 (print) [Google Scholar]
- 27.van Ginneken E., Siciliani L., Reed S., Eriksen A., Tille F., Zapata T. Addressing backlogs and managing waiting lists during and beyond the COVID-19 pandemic. TEN. 2022;28:35. [PubMed] [Google Scholar]
- 28.Arabi Y.M., Azoulay E., Al-Dorzi H.M., Phua J., Salluh J., Binnie A., et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med. 2021;47:282–291. doi: 10.1007/s00134-021-06352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams G. The true worth of a nurse … time to act. J Adv Nurs. 2020;76:2469–2470. doi: 10.1111/jan.14418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams G., Fulbrook P., Alberto L., Kleinpell R., Christensen M., Sitoula K., et al. Critical care nursing policy, practice, and research priorities: an international cross-sectional study. J Nurs Scholarsh. 2023 doi: 10.1111/jnu.12884. [DOI] [PubMed] [Google Scholar]
- 31.Bihari S., McElduff P., Pearse J., Cho O., Pilcher D. Intensive care unit strain and mortality risk in patients admitted from the ward in Australia and New Zealand. J Crit Care. 2022;68:136–140. doi: 10.1016/j.jcrc.2021.07.018. [DOI] [PubMed] [Google Scholar]
- 32.Tierney L.T., Conroy K.M. Optimal occupancy in the ICU: a literature review. Aust Crit Care. 2014;27:77–84. doi: 10.1016/j.aucc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Pilcher D., Coatsworth N.R., Rosenow M., McClure J. A national system for monitoring intensive care unit demand and capacity: the Critical Health Resources Information System (CHRIS) Med J Aust. 2021;214(7):297–298.e1. doi: 10.5694/mja2.50988. Epub 20210328. PubMed PMID: 33774832; PubMed Central PMCID: PMC8252483. [DOI] [PMC free article] [PubMed] [Google Scholar]



 @ICUnurses
@ICUnurses