Abstract
Introduction:
Blood culture is the gold standard for diagnosing bacteremia and direct the physicians to select appropriate antimicrobials. In hospitals, blood culture contamination (BCC) is a common problem that has a detrimental effect on patient outcomes. Hence, we implemented strategies in our tertiary care setup, for training phlebotomists and nurses in proper blood sampling techniques, and assessed their effectiveness in reducing BCC rates.
Methods:
This interventional study was conducted at the Indus Hospital, Karachi, Pakistan from 1st January 2021 to 30th June 2023. All blood cultures received from different departments of the hospital were included. The 2.5-year study period was divided into pre-intervention and intervention periods, with monthly monitoring of BCC. The BCC data between 1st January 2021 and 31st December 2021 was taken as the baseline pre-intervention period and the next 1.5 years comprised the intervention period (1st January 2022-30th June 2023). To improve compliance, various strategies were implemented, such as regular training sessions, didactic sessions, and re-competencies.
Results:
A total of 86 774 Blood cultures were received from all departments of the hospital, out of which n = 30 672 were received in the pre-intervention period whereas, n = 56 102 were received in the intervention period. Mean BCC rate in the pre-intervention period was found to be 4.6%. However, after the implementation of different measures to reduce BCC, the contamination rate decreased to a mean of 3.1% by the end of the intervention period. Emergency department accounted for the highest proportion of BCC in the pre-intervention and intervention periods.
Conclusion:
We decreased BCC in our tertiary care setup by implementing a simple and inexpensive collaborative intervention, and came to the conclusion that the higher incidence of BCC was probably caused by factors unique to the emergency department and provided measures to successfully address them.
Keywords: Blood culture, contamination, intervention, quality improvement
Introduction
Blood culture is the gold standard for diagnosing bacteremia and direct the physicians to select appropriate antimicrobials, greatly improving patient outcome. 1 An accurate blood culture result in this regard mostly depends on appropriate specimen collection procedures. 2 Blood culture contamination (BCC) is a prevalent issue in hospitals and is broadly characterized as the introduction of any microorganism into the culture during specimen collection or processing that may not be pathogenic to the patient. Coagulase-negative Staphylococci (CoNS), aerobic spore-bearing bacilli (ASB), viridans group Streptococci, Corynebacterium spp., Propionibacterium spp., Micrococcus spp., and Clostridium perfringens are among the organisms that are frequently isolated as contaminants in blood cultures. 3 The majority of these organisms exist as common commensal flora on the skin.
False positive blood cultures can result in incorrect diagnoses, which can have a negative impact on patients. The negative effects could include overuse of antibiotics, extended hospital stays, increased workload due to recollection and higher testing expenses. 4 Deviation from the standard protocol of sample collection is an important reason for BCC. As per the recommendations of American Society for Microbiology (ASM) and Clinical Laboratory Standards Institute (CLSI), the overall BCC rate should not exceed 3%. 5 Although it is not possible to completely eliminate BCC, it is essential to keep it within the benchmark. The efficiency of the sampling technique determines the quality of the blood culture, which can be improved by a number of ways such as the use of appropriate skin preparation kits, compliance with standard operating protocols (SOPs) and a trained phlebotomy team. 2
Hence, we conducted this study at the Indus Hospital and Health Network, a tertiary care hospital in Karachi, Pakistan, to assess the effectiveness of implementing strategies for training phlebotomists and nurses in proper blood sampling techniques, in reducing BCC rates.
Methods
Study setting and design
This interventional study was conducted at a tertiary care hospital in Karachi from 1st January 2021 to 30th June 2023. All blood cultures received from different departments of the hospital were included. The 2.5-year study period was divided into pre-intervention and intervention periods, with monthly monitoring of BCC. The pre-intervention period was set to assess the baseline rate of BCC in cultures received from all major departments of the hospital and this data was compared with the BCC rates after the interventions were introduced in the study’s intervention period. The blood culture contamination data between 1st January 2021 to 31st December 2021 was taken as the baseline pre-intervention period and the next 1.5 years comprised the intervention period from 1st January 2022 to 30th June 2023.
Blood culture contamination
The study only included blood samples that were received in multiple sets; single set of blood cultures were excluded because it is not possible to reliably detect contamination in such scenario. Furthermore, only multiple sets of blood cultures which were collected from peripheral lines were included in the study and those from central lines were excluded so as to obtain a uniform set of blood culture population in which the contamination can be reliably determined. For the purpose of our study, we classified the organisms in to 2 groups: (i) organisms that, in almost all cases, represent a true infection; and (ii) common contaminants that, in some clinical cases, may be important. Coagulase-negative Staphylococci (CoNS), aerobic spore-bearing bacilli (ASB), viridans group Streptococci, Corynebacterium spp., Propionibacterium spp., Micrococcus spp., and Clostridium perfringens are some of the most common contaminants isolated from blood cultures and hence, are included in the second group.
The number of blood culture sets that grow a particular organism when expressed as a function of the total number of blood culture sets, is a useful tool for classifying blood cultures as contaminated in order to evaluate the clinical significance of positive blood cultures. Organisms from the first category were deemed to be clinically significant if they were isolated from any of the blood culture sets. The second category of organisms, on the other hand, were only deemed clinically significant if they were isolated from 2 or more blood culture sets and grew organisms with the same antibiogram and biochemical profile; otherwise they were regarded as contaminants.
Blood culture collection
The following Standard Operating Procedure (SOP) was employed for the collection of blood cultures:
(1) Identification of the patient using a minimum of 2 distinct, patient-specific identifiers.
(2) Applying 70% isopropyl alcohol to the venipuncture site to disinfect it.
(3) Using 70% isopropyl alcohol to disinfect the rubber septum on the blood culture bottles.
(4) The initial blood culture set collection, which typically consists of 1 anaerobic and 1 aerobic bottle.
(5) Collecting 10 mL of blood in each bottle to reach the target of 20 mL of blood per set (40 mL if 2 blood culture sets are collected).
(6) Measuring and recording the amount of blood collected in each bottle.
(7) Recording the anatomic location from where the blood sample was collected.
(8) Keeping a record of the employee who took the blood cultures.
(9) Documenting the location of the hospital in which the blood cultures were collected.
(10) To obtain the second blood culture set, repeating the above process with 1 aerobic and 1 anaerobic bottle.
(11) Sending the blood culture sets to the laboratory immediately for processing.
Interventions
The pre-intervention data was divided department wise to determine the contribution of each department to the volume of blood cultures as well as contamination rates. A root cause analysis (RCA) was conducted to identify several factors responsible for contamination. It was found that the nursing staff and phlebotomists, who are primarily responsible for blood sample collection, were not following the SOP for blood culture collection in circumstances of overcrowding and high patient turnover. To improve compliance, various strategies were implemented, such as regular training sessions, didactic sessions, and re-competencies. Experienced personnel from phlebotomy team with the history of least BCC rate were designated as master trainers for the purpose of re-training of all phlebotomy staff. All staff were re-trained in collecting blood cultures as per the described SOP and then competencies of each staff was assessed independently by 2 master trainers for proper blood collection. The staff competency assessment form for the collection of blood cultures is given as a supplement with this study (Supplemental file).
The master trainers worked in collaboration with the Microbiology laboratory providing data on individual staff competencies. As the name of each staff was documented when collecting blood cultures, contamination rates for each staff were reviewed on weekly basis to further re-evaluate individual competency for each staff. Also, BCC rate is made a key performance indicator collectively for the Microbiology laboratory which is monitored monthly and the feedback provided to the head of nursing and the phlebotomy staff.
Additional measures taken to ensure a decrease in the BCC rate included assigning nursing staff and phlebotomists to fixed shifts so they could monitor contamination rates, recording the number of contaminated blood cultures per staff member, and using BCC data as a key performance indicator for each employee. Also, pictorial flyer explaining blood culture collection procedure were pasted in blood culture collection areas.
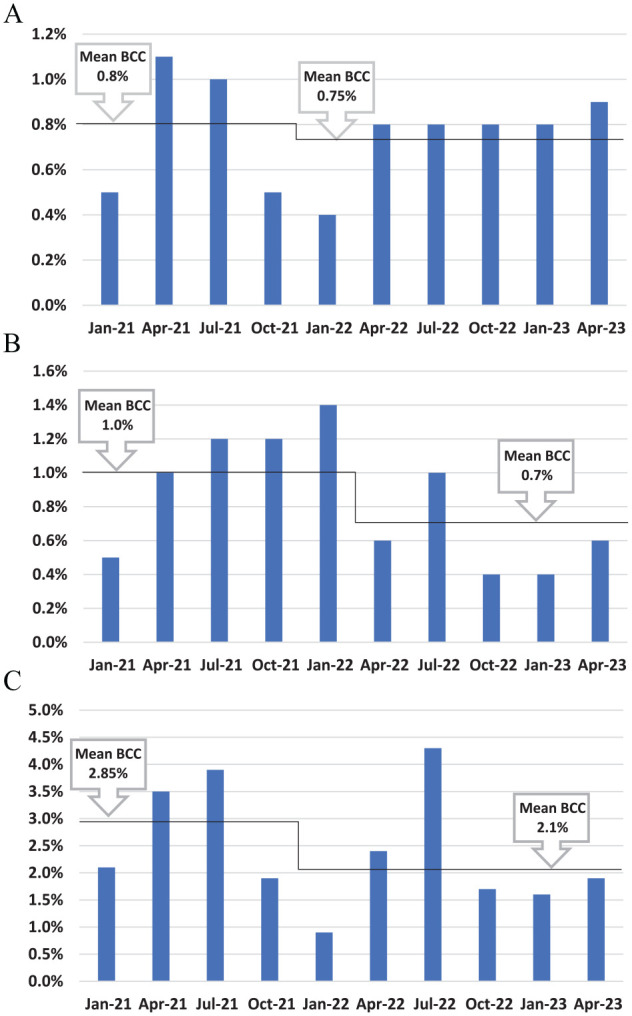
Statistical analysis
Data regarding the total number of blood cultures received during the study period, number of blood cultures received from different departments of the hospital and from different patient populations viz. pediatric and adult population was recorded on a standardized proforma. BCC rate during the pre-intervention and intervention periods, from different departments of the hospital and from different patient populations was also documented. For the purpose of statistical analysis, all data was entered in Microsoft Excel software (Microsoft Excel 2013 {15.0.5553.1000} 32-bit). The quarterly BCC rates were plotted on a run chart to demonstrate the effect of the interventions on the overall reduction of BCC between the pre-intervention and intervention periods. Furthermore, an interrupted time-series analysis using segmented regression was used to assess the effectiveness of the implemented interventions, which allowed the evaluation of the intervention impact while accounting for the time trend and autocorrelation present in subsequent observations.
Results
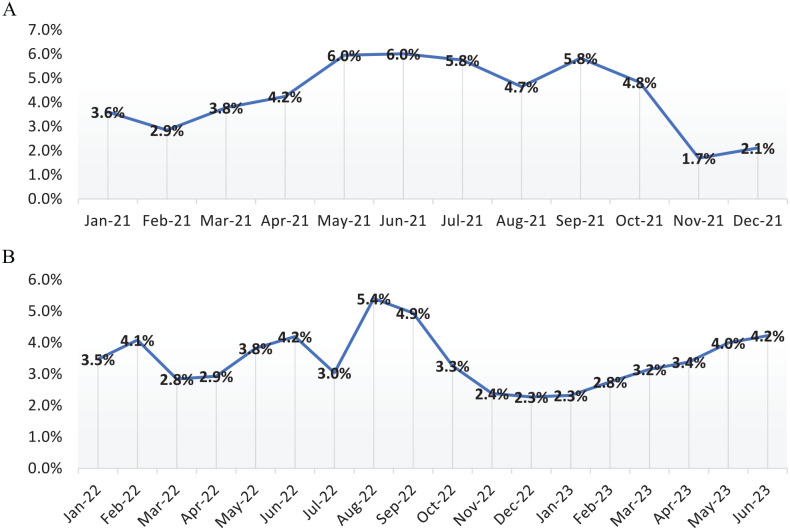
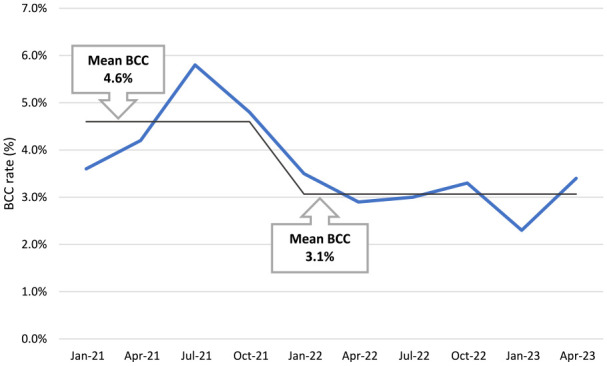
A total of 86 774 blood cultures were received from all departments of the hospital during the study period, out of which 45 122 were from adult patients and 41 652 from pediatric patients. In the pre-intervention period (1st January 2021-31st December 2021), 30 672 blood cultures were received whereas, 56 102 blood cultures were received in the intervention period (1st January 2022-30th June 2023). Overall, BCC was seen in 3306 (3.8%) blood cultures, of which 1582 (48%) were from pediatric patients and, 1724 (52%) from adult patients. BCC rate in the pre-intervention period was found to be 4.6%. However, after the implementation of different measures to reduce BCC, the contamination rate decreased to 3.1% by the end of the intervention period. Monthly BCC rate in the pre-intervention and intervention periods is shown in Figure 1. The run chart of quarterly BCC rates over the study period depicts the reduction in BCC rate between the baseline pre-intervention period and the intervention period (Figure 2).
Figure 1.
(A) Monthly BCC rate in the pre-intervention period. (B) Monthly blood culture contamination rate in the intervention period.
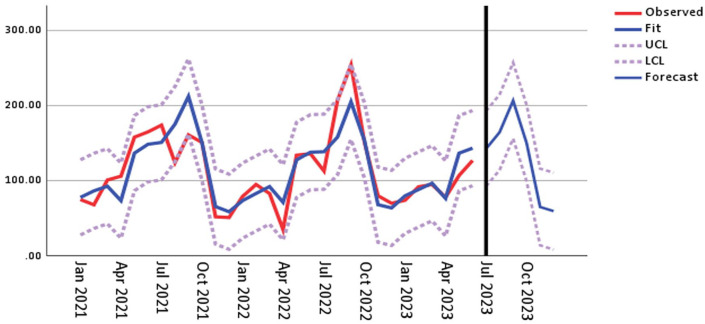
Figure 2.
Run chart of quarterly blood culture contamination (BCC) rates over the study period (Jan 2021-Jun 2023); pre-intervention (Jan 2021-Dec 2021) and intervention periods (Jan 2022-Jun 2023).
The contamination rate varied among different departments viz. emergency (ER), in-patient (IPD) and out-patient (OPD) departments. ER accounted for the highest proportion of BCC (2.4%) throughout the study period, followed by OPD (0.8%) and IPD (0.75%). The effect of interventions in reducing the BCC rate was most observed in blood cultures received from ER, which showed a decline of BCC from a mean rate of 2.85% in the pre-intervention period to 2.1% at the end of the intervention period. Department wise distribution of quarterly BCC rates in the pre-intervention and interventions periods is shown in Figure 3.
Figure 3.
Department wise distribution of quarterly BCC rates over the pre-intervention (Jan 2021-Dec 2021) and intervention periods (Jan 2022-Jun 2023) in (A) in-patient department (IPD) (B) out-patient department (OPD) & (C) emergency department (ER).
The time series analysis demonstrated that the educational intervention (R2 = 0.35) had an effect on the BCC rate, with a reduction in level change (P ⩽ .05) noted 2 months after the intervention. The observed quarterly BCC rates were approximately within range of the upper and lower control limits throughout the study period. Moreover, an expected trend of BCC in the 6-month post-study forecast was observed to be within the control limits (Figure 4).
Figure 4.
Interrupted time series analysis for quarterly BCC rates among positive blood cultures in the pre-intervention and intervention periods [where y-axis—number of contaminated blood cultures among positive cultures & x-axis—quarterly intervals in the study period (Abbreviations: LCL, lower control limit; UCL, upper control limit)].
Discussion
This study demonstrates that a persistent team effort can effectively address the problem of blood culture contamination in a hospital unit that experiences high patient turnover. The findings of this study are relevant as it originates from a developing nation with limited resources.
Most BCCs were associated with the ER, according to our findings. Periods of crowding and stressful working environment are some of factors that have been linked to considerable increases in BCCs from the ER. Similar findings were observed in different studies conducted worldwide.6 -8
Pakistan is a sub-tropical country and typically exhibit hot and humid weather from May to August and cold and dry weather from November to February each year. The weather of Karachi in the humid months can cause increased perspiration in the patients, which can alter normal skin microbiota resulting in poor skin hygiene. This, in turn, may increase the probability of contamination during specimen collection. 9 This fact was evident with the abrupt increase in the BCC rate seen in the pre-intervention period as seen from May to September 2021, in our study (Figure 1A). Furthermore, while rigorous interventions were in place, a creep in BCC rate was still observed in the intervention period from May 2022 and then a steep decline from September 2022 onward, when the weather began to dry and the patients were less likely to perspire. The rise in BCC rate was again observed in the intervention period from May 2023 onward (Figure 1B). While, the effects of changing weather are increasingly evident from these findings, it is noteworthy that the overall BCC rates after the initiation of interventions exhibited a significant decline from 4.6% in the pre-intervention to 3.1% by the end of the intervention period (Figure 2).
Several studies have indicated that a trained phlebotomy team could decrease BCC rates. A study conducted in the emergency department, compared the contamination rate between blood cultures collected by dedicated phlebotomists and non-phlebotomist staff. Significantly higher contamination rate was observed in blood cultures collected by non-phlebotomist staff. The study took place during the COVID-19 pandemic, when phlebotomy staff dedicated to blood culture collections were temporarily disbanded, and blood culture collection was performed by non-phlebotomist staff. 10 For reducing contamination rates especially from departments contributing to the highest proportion of BCC, we discouraged rotational duties and implemented fixed duties. Each staff member’s performance was monitored based on the number of contaminated blood samples versus the total blood samples drawn. To ensure better compliance among phlebotomists and nursing staff, BCC was introduced as one of their key performance indicators on the basis of which they were appraised. After implementing appropriate measures, we observed a steady decline in the contamination rate in the first intervention period (2022) which continued to decrease over the next 6 months of the second intervention period (2023).
It is challenging to maintain specimen quality to international standards while offering the best possible patient care in health setups with limited resources. A strategic approach to quality control measures and ongoing monitoring are needed to achieve this goal. Even with limited resources, adherence to these standards improves the accuracy of research and diagnosis.
There were few limitations in our study. We didn’t measure the impact of blood culture contamination on patient care and health outcomes, and the expenses associated with it. However, the authors intend to conduct a multi-center study in the future, which would incorporate a wider understanding of specimen contamination on the overall care of patients and the health setup. Furthermore, a more targeted study is needed in this regard to assess the precise intervention which has the most impact in reducing sample contamination rates.
Conclusion
We decreased blood culture contamination in our tertiary care setup by implementing a simple and inexpensive collaborative intervention, and came to the conclusion that the higher incidence of blood culture contamination was probably caused by factors unique to the emergency department and provided measures to successfully address them.
Supplemental Material
Supplemental material, sj-docx-1-pat-10.1177_2632010X241265857 for Safeguarding Accuracy: The Impact of Interventions on Reducing Blood Culture Contamination by Fareeha Adnan, Nazia Khursheed, Moiz Ahmed Khan and Nazia Parveen in Clinical Pathology
Acknowledgments
None
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: F.A. - Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – original draft
N.K. - Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – review & editing
M.A.K. - Formal Analysis, Investigation, Software, Visualization, Writing – review & editing
N.P. - Data curation, Formal Analysis, Investigation, Validation, Visualization
Ethical Approval: This study was exempted from ethical approval by the Institutional Review Board (IHHN-IRB#1) of the Indus Hospital & Health Network (Ref # IHHN_IRB_2023_08_022).
Consent: As the study was part of the institutional quality improvement project and did not involve any specific intervention on humans or animals therefore, no consent was applicable.
ORCID iD: Moiz Ahmed Khan  https://orcid.org/0009-0004-2726-277X
https://orcid.org/0009-0004-2726-277X
Availability of Data and Materials: All data generated or analyzed during this study are included in this published article.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. López-Pintor JM, Sánchez-López J, Navarro-San Francisco C, et al. Real life clinical impact of antimicrobial stewardship actions on the blood culture workflow from a microbiology laboratory. Antibiotics. 2021;10:1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Preventing adult blood culture contamination: a quality tool for clinical laboratory professionals. Cdc.gov 2024. Accessed May 25, 2024. https://www.cdc.gov/labquality/blood-culture-contamination-prevention.html
- 3. Doern GV, Carroll KC, Diekema DJ, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev. 2019;33:e00009-e00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19:788-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sacchetti B, Travis J, Steed LL, Webb G. Identification of the main contributors to blood culture contamination at a tertiary care academic medical center. Infect Prev Pr. 2022;4:100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marcelino C, Shepard J. A quality improvement initiative on reducing blood culture contamination in the emergency department. J Emerg Nurs. 2023;49:162-171. [DOI] [PubMed] [Google Scholar]
- 7. Burnie J, Vining S. Clinical nurse specialist practice: impact on emergency department blood culture contamination. Clin Nurse Spec. 2021;35:314-317. [DOI] [PubMed] [Google Scholar]
- 8. McLeod CG. Reducing blood culture contamination in the emergency department. J Nurs Care Qual. 2020;35:245-251. [DOI] [PubMed] [Google Scholar]
- 9. Qiu Y, Zhou Y, Chang Y, et al. The effects of ventilation, humidity, and temperature on bacterial growth and bacterial genera distribution. Int J Environ Res Public Health. 2022;19:15345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Esquer Garrigos Z, Wingler MJB, Svoronos PA, et al. Increased rates of blood culture contamination during the coronavirus disease 2019 pandemic. Infect Control Hosp Epidemiol. 2022;43:1719-1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pat-10.1177_2632010X241265857 for Safeguarding Accuracy: The Impact of Interventions on Reducing Blood Culture Contamination by Fareeha Adnan, Nazia Khursheed, Moiz Ahmed Khan and Nazia Parveen in Clinical Pathology