Abstract
Background
As part of the fight against coronavirus disease, Nigeria received nearly 4 million doses of the COVID-19 vaccine via the COVID-19 Vaccines Global Access (COVAX) Facility, marking a historic step towards equitable global distribution of COVID-19 vaccines. Although evidence exists on COVID-19 hesitancy in Nigeria, yet, we are unaware of any study on the optimization of COVID-19 vaccination from the lenses of the mobile teams.
Objective
This study seeks to explore the perceptions and experiences of mobile teams in selected communities during the implementation of COVID-19 vaccination in Benue and Niger.
Methods
An exploratory approach was adopted, and the study was conducted in Niger and Benue states based on poor performance in COVID-19 vaccination. Focus Group Discussions (FDGs) were conducted among 12 mobile vaccination teams from 12 LGAs. The recorded discussions were transcribed and coded (inductively and deductively) using Dedoose software (v9.0). Four themes and seven sub-themes were generated from the participants’ responses.
Results
Seventy-two (72) health workers including vaccinators, validators, Electronic Management of Immunization Data (EMID) recorders, social mobilizers, and paper recorders participated in this study. Health workers’ perceptions and experiences were thematized using the health building blocks. The mobilization teams in Benue and Niger states perceived that their mobilization efforts contributed to improved coverage, increased accessibility, and reduced hesitancy among the community dwellers. Challenges reported by the teams were vaccine misconceptions, requests for incentives in exchange for vaccine uptake, poor network services, distance to communities, and vaccine stockout.
Conclusion
This study concluded that social mobilizers play key roles in vaccine uptake, especially at the community level. Their roles in creating awareness, sensitization, and bringing the vaccine closer to hard-to-reach communities contributed to the success attained in the fight against COVID-19 in both states.
Keywords: Perceptions, Mobile teams, Vaccine uptake, Community level
Background
The outbreak of COVID-19 led to the cessation of key economic activities, a decrease in well-being, and loss of human lives [1–3]. After adopting several non-pharmaceutical measures, prophylactic vaccines were developed to ameliorate the situation and improve the global population’s well-being [4, 5], in less than a year, resulting in the largest vaccination campaign in human history [6]. Nigeria received nearly 4 million doses of the COVID-19 vaccine, shipped via the COVID-19 Vaccines Global Access (COVAX) Facility, a partnership between CEPI, Gavi, UNICEF, and WHO, on March 2, 2021 [7]. This marked a historic step towards ensuring equitable distribution of COVID-19 vaccines globally in what is considered the largest vaccine procurement and supply operation the world has ever known [7]. Essentially, the first phase of vaccination targeted population groups at high risk of mortality from COVID-19, such as frontline health workers, social workers, individuals with comorbidities, and the elderly above 60 years of age [8, 9].
Consequently, the government of Nigeria through its health authority, the National Primary Healthcare Development Agency (NPHCDA), employed strategies to administer COVID-19 vaccines to the targeted populations [10–12]. This was executed in collaboration with multiple stakeholders at the national and sub-national levels [10]. Amidst the vaccination exercise at varying stages, reports revealed a high level of hesitancy among the country’s populace [9, 13, 14], particularly members of rural communities, and underserved populations [15]. Primarily, vaccine hesitancy is the delay in acceptance, reluctance, or refusal of vaccination despite the availability of vaccination services [16]. Studies reported the drivers of vaccine hesitancy to include religious beliefs [17–19] beliefs in conspiracy theories [20–22] low-risk perception influenced by self-denial [1, 12, 23], and misinformation [14, 24]. Furthermore, a lack of confidence in vaccine safety or its effectiveness and a lack of trust in authorities have also been considered as attributing factors to vaccine hesitancy among population members [12, 25–27].
While several determinants have been scientifically associated with COVID-19 vaccine hesitancy, many of these can be categorized under four of the Health Belief Model (HBM) components. HBM is a scientific psychological health behaviour model that posits the existence of six key predictors of health behavioural change and is often used as a tool for disease prevention and health promotion [28, 29]. These four components are perceived susceptibility (perceived threat to COVID-19), perceived severity (belief of consequences), perceived benefits (possible positive benefits to action), and perceived barriers (potential hindrances to action).
In Nigeria, several conspiracies exist around COVID-19 and the vaccine. Specifically, many Nigerians, particularly in rural settings believed that COVID-19 was a false tool created by the Nigerian government to siphon funds [30, 31], which in turn influenced their poor perceived susceptibility to the disease. Consequently, Nigerians, including health workers, believed that the vaccines were designed to incorporate microchips into the human body and alter DNAs [32], and in some cases reduce the global population, especially in Africa. Additionally, evidence exists on concerns about the COVID-19 vaccine among Nigerians including the efficacy of the vaccine, and potential side effects [33, 34]. These impediments played a significant role in the hesitancy of many Nigerians, especially residents of rural and underserved communities towards COVID-19 vaccination.
To address the issue of hesitancy, and to subsequently control and manage the prevalence of COVID-19 in Nigeria, the National Primary Healthcare Development Agency (NPHCDA) in collaboration with implementing partners locally and internationally, engaged ad-hoc health workers to facilitate outreaches in different communities and settlements that are situated in rural local government areas and usually habituated by the underserved populations. These ad-hoc health workers are often called “Mobile or Community Outreach teams”. Community outreach programs are typically adopted to reach underserved populations, optimize vaccine uptake, and ensure equity across a country’s population, even in developed countries, as evident in the literature [35, 36]. In several African health systems, health workers were designated in groups to various underserved communities to facilitate door-to-door COVID-19 vaccination campaigns as a strategy to improve the uptake of COVID-19 vaccines [37, 38].
Owing to the above, Sydani Group was one of many local implementing partners that collaborated with the NPHCDA to engage mobile teams, in Benue and Niger states. Over 150 mobile teams were engaged by the Sydani Group in 46 LGAs across the two states. This support provided to the two states helped in leap-frogging both states on COVID-19 vaccination coverage of the national log. Specifically, Benue state recorded a 14.2% increase in vaccination coverage (28.1% − 42.3$), while Niger state recorded a 20% increase in vaccination coverage (58.6 − 78.6%).
Based on the literature, evidence exists on COVID-19 vaccination and hesitancy in Nigeria [39, 40], and the role mobile vaccination teams play in increasing vaccine uptake [24, 41, 42], however, we are yet to explore the perceptions and experiences of the mobile teams concerning the acceptance and uptake of COVID-19 vaccination among underserved community residents in Nigeria. Against this backdrop, this study seeks to explore and document the perceptions and experiences of mobile teams in various communities in Benue and Niger states, Nigeria, during their implementation of COVID-19 vaccination.
Methods
This study was anchored on an exploratory research design to acquire qualitative data from purposively selected participants in two North Central (Niger, and Benue) states in Nigeria. Focus Group Discussions (FDGs) were conducted among 12 mobile vaccination teams from 12 LGAs across the two North Central states (6 mobile teams from each state) to elicit information from participants on the perception and experiences of mobile teams on COVID-19 vaccine uptake at the community level.
Study locations
The study was conducted in two North Central States: Benue and Niger (see Fig. 1). One of Nigeria’s six geopolitical regions, the North Central consists of several Middle Belt states. Seven states, including the Federal Capital Territory, make up this entity. The North Central region shares a border with Cameroon, and Benin, and spans the whole nation’s width.
Fig. 1.
Map of Nigeria indicating the study locations
Established from the previous Benue-Plateau State in 1976, Benue State shares international borders with Cameroon, and local borders with Nasarawa, Taraba, Kogi, Enugu, Ebonyi, Cross-Rivers, and Enugu states. The Tiv, Idoma, and Igede are the main ethnic groups that live there. Etulo, Igbo, and Jukun peoples are among the minority ethnic groups in Benue.
Niger State by landmass, is the largest state in Nigeria. It was established along with Sokoto State from the then North-Western State in 1976. The bulk of Niger State’s various indigenous tribes includes the Nupe, Gbagyi, Kamuku, Kambari, Gungawa, Hun-Saare, Hausa, and Koro. The river Niger inspired the state’s name.
Study participants and selections
The study participants were health workers at the ward level within a local government area. These health workers are regarded as community outreach teams or mobile teams. and are usually attached to the primary healthcare facility established in the political wards they inhabit. They are primarily engaged in the immunization unit of the primary health care agency through the facility, to the local government areas (LGAs) and state levels. The mobile team usually consists of professionally trained, and informal health workers [43]. More precisely, a mobile is a group of 6 people, with everyone assigned specific roles within the team to ease the delivery of services to community members. There are two (2) vaccinators (trained nurses), a paper/manual recorder, an electronic recorder, a validator, and a social mobilizer.
The study locations (Niger and Benue states) were selected purposively based on the outcome of the COVID-19 vaccination support funded by the US-CDC, and provided to the states, to meet up with the National target of 70% coverage for COVID-19 vaccination as stated by the National Primary Healthcare Development Agency (NPHCDA). Afterward, the LGA selection was based on the following criteria:
-
i.
Low/high reporting of COVID-19 vaccination rates.
-
ii.
Absence of insecurity issues.
-
iii.
The facility must have been active for at least 3 months before the study.
At the time of the study, there were a few mobile teams in each local government, depending on the number of facilities and wards in the LGA. In each state, 60 mobile teams (120 in the two states) were engaged by the Sydani group, spread across 23 local government areas in each state where support was provided. In each of the selected LGA, one mobile team was purposively selected based on proximity to the local government secretariat at the time of the study. For all the teams engaged in both states, there exist a total of 240 vaccinators, 120 paper recorders, 120 electronic recorders, 120 validators, and 120 social mobilizers.
Inclusion and exclusion criteria for selecting study participants
The participants were selected based on the conditions that they were engaged as a mobile team by the Sydani Group for the COVID-19 vaccination exercise. They must have also visited communities within their wards and local government areas to vaccinate people on COVID-19 vaccination and have been doing this for over three (3) months. On the other hand, participants were excluded if they were domiciled in the facility to administer COVID-19 vaccination to the populace.
Analytical framework
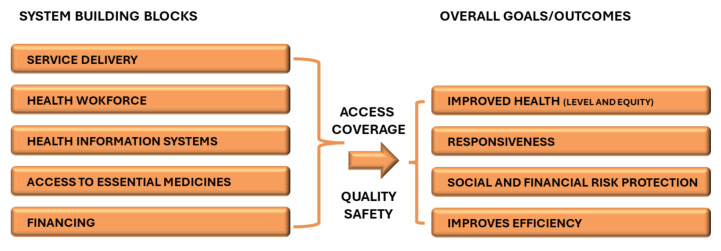
According to the WHO, Health systems consist of organizations, people, and actions to promote, restore, or maintain health [44, 45]. WHO emphasizes that the health system is a set of interconnected parts that must function together to be effective, and as a result proposed the six health system building blocks. Managing the interaction among these blocks translates to achieving more equitable and sustained improvements across health services and health outcomes.
The WHO Health System Building Framework was adapted in this study to scientifically and constructively guide the study tool design, data collection, and analysis [44]. The framework has six components and five were adapted for this study (see Fig. 2) as they are relevant to guiding the operationalization of our objectives.
Fig. 2.
Adapted WHO health systems framework
Ethical approval and consent to participate
The research protocols were reviewed and approved by the National Emergency Routine Immunization Coordinating Centre (NERICC), the Institutional (internal) Review Board of the National Primary Health Care Development Agency (NPHCDA) in Abuja, Nigeria. The research adhered to the principles outlined in the Helsinki Declaration. Additionally, written informed consent was obtained from each participant prior to the commencement of the research.
Data collection instrument
A semi-structured interview guide was developed using an adapted version of the WHO Health System Building Blocks Framework during the Focus Group Discussions in line with the study objectives [44]. Specifically, the study assessed participants’ perceptions and experiences on service delivery, health workforce, health information systems, finance, and vaccine logistics. These areas were focused on because the study participants operate at the Questions were generated for these thematic areas based on the sole objective of the study: to document the perceptions and experiences of the mobile teams. grassroots levels and the identified areas best apply to them. Questions such as: “How would you describe your contributions to (optimizing) COVID-19 vaccination in your various localities (through service delivery, health workforce, and health information system)?” and “Kindly describe your experiences briefly in terms of problems and challenges you encountered in the field, and how you dealt with it”.
Data collection procedure
Twelve (12) Focus group discussions (FGDs) were conducted among the mobile teams across Benue and Niger states (6 in each state). Each FGD session consisted of members of a single mobile team (2 vaccinators, 1 paper recorder, an electronic recorder, a validator, and a social mobilizer). Verbal consent was obtained from all the participants before the FGDs were conducted. All discussions were conducted in English language to ease communication within 30–60 min on an audio recording device.
Data analysis
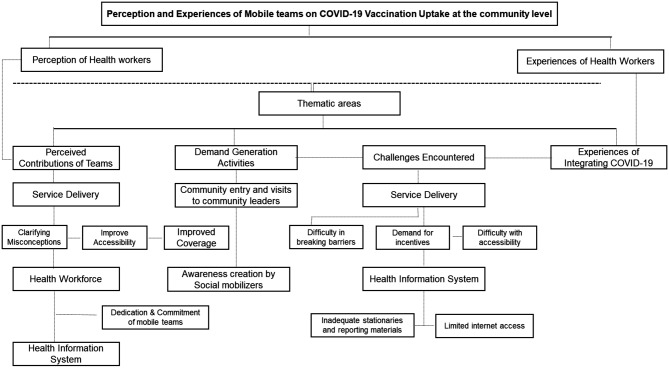
All audio recordings were transcribed in Word document files by professional and experienced transcribers. The research team reviewed the transcripts’ contents and developed the codebook with the adapted WHO health building blocks framework [44]. The transcripts were coded and managed on Dedoose software (Version 9.0) combining the inductive and deductive approaches [46]. A thematic analysis was conducted, and codes were synthesized to identify useful patterns in responding to the study objective. Four thematic areas were generated from the study including demand generation strategies, perceived contribution to COVID-19 optimization, challenges encountered, and experience in integration into extant health programs (see Fig. 3).
Fig. 3.
Thematic analysis of study findings
Results
Socio-demographics characteristics of participants
In total, 72 health workers participated in the study including vaccinators, validators, EMID recorders, social mobilizers, and paper recorders. About 3 out of every 5 (58.3%) participants were female by gender, as over one-quarter (27.8%) of the study participants are National Certificate Examination (NCE) degree holders. The mean age of the study participants is 34.3. About 2 out of every 5 (40.3%) study participants fall within the 29–38 age bracket (Please see Table 1).
Table 1.
Socio-demographic characteristics of participants
| Total (72) | Niger State N = 36 | Benue States N = 36 | |||
|---|---|---|---|---|---|
| Characteristics | n(%) | Frequency | Percent | Frequency | Percent |
| Gender | |||||
| Male | 30 (41.7) | 15 | 41.7 | 15 | 41.7 |
| Female | 42 (58.3) | 21 | 58.3 | 21 | 58.3 |
| Age group | |||||
| 19–28 | 22 (30.6) | 12 | 33.3 | 10 | 27.8 |
| 29–38 | 29 (40.3) | 11 | 30.6 | 18 | 50 |
| 39–48 | 13 (19.5) | 9 | 25 | 5 | 13.9 |
| 49–58 | 19.4 (9.7) | 4 | 11.1 | 3 | 8.3 |
| Educational attainment | |||||
| Secondary | 14 (19.5) | 8 | 22.3 | 6 | 16.7 |
| Post-secondary | 51 (70.9) | 24 | 66.7 | 27 | 75 |
| University | 3 (8.3) | 0 | - | 3 | 8.3 |
Perceptions and experiences of mobile teams on the uptake of COVID-19 vaccine at the community level
For proper delineation of the findings from the study, the result section is divided into two major parts. The first part of the findings highlights health workers’ perception of the services they have provided at the community level, and the second part thematically discusses health workers’ experiences during their provision of vaccine administration in the communities.
Perception of health workers
Perceived contributions of the mobile team to COVID-19 vaccination optimization
The adapted WHO Health System Building Blocks Framework guided the grouping of the emerging themes from the study findings under the relevant building blocks. The findings presented in this section provided insights into the perceived contributions of the mobile team toward the optimization of COVID-19 vaccination in the two selected states:
Service delivery
All the participants who participated in the discussion believed that through the work they did in several communities in their local government, they have been able to improve vaccination coverage in their states, while they were trying to support their people through the administration of COVID-19 vaccine as a prophylaxis for community members. The following are some of the thematic areas the mobile team provided service at the community level:
Clarification of misconceptions and beliefs
Before the teams visited the communities, many of the community dwellers held several misconceptions about the COVID-19 pandemic and the vaccination which had led to the hesitancy experienced in the vaccine uptake. Hence, part of the most essential services of the/ Community Outreach team was to unravel and clarify those misconceptions.
… Secondly, concerning issues that some of them were scared of, we gave clarification and explanation. A lot of them decided to be vaccinated having gotten the explanation and all that. (FGD/Mobile Team/ Wushishi LGA/Niger State)
Yes, what we did as a team was that we encouraged others to participate in the uptake of COVID-19, for example, if we go to any community, maybe some people have the intention of not taking it because of one thing or another or the wrong perception about it. We tell them that the vaccine is safe, that we as a team and the health workers that visited them have taken the vaccine before and nothing has happened to us. So, it’s how we encouraged them that the vaccine is safe for everybody to take. (FGD/Mobile Team/Ogbadibo LGA/Benue State)
My team’s contribution to the community or to the Otukpo Local government as a whole, vaccinating people, we are preventing them from having the illness that they are vaccinated against, 2) we are telling them the importance of what we are doing or what the government is helping them to do, because in other areas, we have heard about people that COVID-19 have killed, but by the special grace of God because of this program that is here, it help us that such a way that we don’t experience something like that, and based on the information that was given from the radio and our mobilizers going to talk to them, it gives them a kind of motivation, because at the first time people were scared of the vaccine that it’s not good, that it is this and it is that, but based on the information and the corporation form the team again, to the community, people have started coming out unlike before, so now I think this our services have helped the community with a lot of vaccine uptake (FGD/Mobile Team/Otukpo LGA/Benue State).
Improved service accessibility
The services provided by the mobile team at the community level are effective drivers of increased accessibility to the uptake of COVID-19 vaccines, as communal residents are usually reluctant to visit health facilities for vaccination based on certain conditions. Community dwellers who reside in communities far from the fixed vaccination centers face the challenge of transportation. However, the consistent activities of the mobile/community outreach team have helped bring the COVID-19 vaccination services closer to these groups.
In addition to what he has said, the proximity of the vaccine; You know ordinarily Most of them find it difficult to transport themselves to the health facility but our frequent going to their communities makes the vaccines closer to them, available to them without them spending transport to come. (FGD/Mobile Team/ Wushishi LGA/Niger State)
The work we did helped many people have access to vaccines, especially now that everything is costly. Eating is a big problem, but some people still want to be vaccinated. Like the place we visited today, a bike from this place (and none of us is even leaving around here), just to go is 300 naira coming back they would not even carry you for that 300 naira, and some people want to have access to the vaccine, but due to the economy we are facing now, they would not come, me I have looked at this work that has helped a very. It has gone a very long way in making people access the services even right on their doorsteps. So, this work has helped us a lot (FGD/Mobile Team/Otukpo LGA/Benue State).
Improved coverage
As a result of bringing COVID-19 vaccination service closer to the community dwellers the number of persons who took the vaccine increased in each of the respective LGAs. Hence, barriers such as misconceptions, vaccine safety, and distance to name a few, were addressed by the mobile team.
It helped because as part of the staff in the clinic, the work we did with people in the villages also increased the number of COVID-19 immunizations. We normally convince them that the vaccine is supposed to help them not to have COVID-19. You know some people do not believe that the disease is in Nigeria, and they will say that it is a lie, but because of our work in the villages, we save the stress of our people in the clinic. And we make sure that the village people are protected (FGD/Mobile Team/ BOSSO LGA/Niger State).
Our work affected vaccination coverage in the sense that, many people were not available to go to the fixed post for vaccination but since we have been going out, we have been getting them there in their various settlements. At least some of them will say that they cannot come to the facility. There are a lot of things they have been saying about COVID-19 and even the vaccine, but when we move close to them, we explain to them the benefits of this, So many of them if we explain to them, they would then decide to take the vaccine (FGD/Mobile Team/Makurdi LGA/Benue State).
Health workforce
Dedication and commitment of the mobile teams
All participants involved in the discussion agreed and believed that their engagement as mobile teams strengthened and improved the capacity of the health workforce, by optimizing COVID-19 vaccination tremendously through increased coverage in various communities, especially the hard-to-reach communities, in their respective local government areas. This, according to them was attained through their visitations to these communities and their provision of door-to-door vaccination services. Participants also stressed that they were usually committed to the work irrespective of the few deterrents the work presented to them. This was evident in the expression of teams who emphasized that:
For me, I say to them that they should not be worried. We are doing it for a community purpose. We are helping ourselves, our fathers, mothers, and brothers. We don’t have to earn something, anything. Sometimes you do work, it’s only God who will reward you. Let’s just help ourselves and help the community. We don’t give our (FGD/Mobile Team/Katsina-Ala LGA Benue State).
I think the work we did in the community really helped our people in the facility, and it even made the number of COVID-19 go up very well. Like now, we always go and convince people, and even go and block them when they are going to farms. We also gave people vaccines immediately after morning prayer in the mosque. (FGD/Mobile Team/Edatti LGA/ Niger State)
Health information system
A structured paper and electronic-based form of data reporting
Participants expressed that they adopt a bottom-to-top-level reporting structure, as they relay their collected data to the ward focal person, who in turn forwards the reported data to the monitoring and evaluation officer at the local government level, and this goes to the state-level officer, who is likely to report the data in the National Call-in Data platform for COVID-19 vaccination. Participants equally expressed that team leads re-evaluate the submission of data through the appropriate channels to ensure sustainability from the team, as the implication for reporting is to attest to the increased coverage of the vaccinated populace in the various local government areas across the two states.
One thing is that once we get the details of the client, and then we, on our EMID app. Once we do it, automatically it synchronizes and saves. Then the whole thing is shifted to the validator, afterward then I think it’s a done deal already. We do ask them their names, ages, numbers date of birth, then vaccination date and time. We then send a report first from the unit to the ward focal person, from the ward focal person to the M&E, from the M&E to the local government officer, and then to the state, just like once we finish any session. Like today’s job, we make sure that everybody that is acquainted with their position, we make sure that they send it like the person that is responsible in our team, to send it, the thing keep going gradually, from our team now, from the unit to the ward focal person and the focal person would also do his work and gradually till it gets to the climax of the whole thing (FGD/Mobile Team/Otukpo LGA/Benue State).
Let’s assume this man is already immunized, and he came to me as an EMID. I will ask him what his name is. Since he is a male, there’s no need to ask for his sex, I will put in M and ask him for his date of birth, I will ask him ward and the community. So, I later go to the vaccine section if it is Moderna or Pfizer, so I will now register him, ask him to give you his phone number, and later do it. At the end of all our vaccinations, I will synchronize my data and send the report to the focal person and the M&E in the LGA, and the M&E in the LGA now send it to the state. I think the state now sends it to the national level. I will also send my report through the ODK to Sydani. And if there is no data, I used to tell my team people and they will contribute money for me to buy data so that I can send the vaccine report (FGD/Mobile Team/Edatti LGA/Niger State).
Experiences of health workers
Demand generation strategies deployed by the mobile team
Community entry and visit to the community leader
Generally, evidence-based practices have revealed that vaccinations and/or immunizations are driven either by fixed posts or outreach teams. However, outreach teams are significantly integral to optimizing immunization/vaccination services, especially in communities with limited access to healthcare services. Recognizing the value of mobile teams, our study inquired from the teams how they carry out their activities and ensure seamless operations within the communities. The mobile teams interviewed emphasized that their first step in conducting their vaccination activities was visiting the community leaders. Community leaders are informed on why the teams are in the community and are then leveraged to get community members informed and vaccinated for COVID-19.
Like, in my team, I’m the supervisor. Let me say it like that. When we go out to the community, we go straight to the community’s chief. We let the chief know that this is what we are coming here for. We tell the chief about how we intend to take the vaccine to the people, the potential side effects of the vaccine, and what next steps they can take should they experience it. The chief will either tell us to go ahead or send any of the villagers to inform others that this is what these people are here for. They are not here to harm. They will allow our town announcer to announce for them so that we can take the vaccination to them. (FGD/Mobile Team/Katsina-Ala LGA/Benue State)
When we go to the community as my other person said, we will make sure that we go to Mai Angwa, and when there is a palace there, we go to the palace too to tell the king who we are and what we want to do there. We tell them “we are from the health center in the ward”, and “we want to vaccinate people for COVID-19 in the community”. They mostly tell us to come back the following day and before we come, they will inform their community members. They even use to tell us to come early so that we can meet people at home that many people will go to farm (FGD/Mobile Team/Wushishi LGA/Niger State).
Awareness creation at the community by social mobilizer
The second layer of demand generation activities deployed by the mobile team is to engage a social mobilizer who goes from street to street, household to household to sensitize the community dwellers, especially in their local dialects about the need to avail themselves of the vaccination exercise. The social mobilizer provides details on the visit of the mobile team for the vaccination exercise, the venue, days, times, and duration.
So, first of all, if we want to go to the community for vaccination, first we arrange for the week, within the weekend we arrange the community we’re supposed to go day by day. So, if we have to go to this same community, we inform our Mobilizer to go to the community and mobilize them before the day we are supposed to go. OK, the information that was given to them, we have come for COVID-19 vaccination. Give them some information that is going around about the vaccination…… We try our best to convince them, to tell them that the vaccine is effective, safe and there’s nothing about the vaccine. So we try and convince them with the help of God, some of them will accept and take the vaccine. That’s what I have to say. (FGD/ Mobile team BOSSO LGA/Niger State)
Whenever we are going into a community, first we send our mobilizer to go ahead of us so that he go and clear the ground for us and then we go after him, then we sensitize the people by educating them, giving education concerning COVID and other related diseases, then we vaccinate them. Not only that, we sometimes cooperate with the KNCV team now that they are on the ground we collect some of the material like BP apparatus and then HPSL machines, and then we test the proof of blood sugar and then high BP (FGD/ Mobile team Makurdi LGA/Benue State).
The teams engaged in highly coordinated activities by structurally planning their locations in a community on the first day of the week, before entering the community. Additionally, the teams drive their vaccination activities through the key stakeholders at the grassroots level and sensitize not only the stakeholders, but also the community members on the value, and potential benefits accepting the vaccine offers to community members. The sensitization of community residents is equally an approach to addressing misconceptions and conspiracy theories that pervaded the communities where mobile teams found themselves.
Challenges encountered during vaccination exercise
The study equally adapted the Health Systems Framework to document the challenges of the health workers conducting outreaches in various communities across different LGAs in Benue and Niger states.
Service delivery
Difficulty in breaking the barrier of misconception and vaccine safety
Despite the efforts made by the team to clarify the misconceptions, and beliefs around COVID-19 and vaccine safety, some of the community dwellers in certain instances still proved difficult as they stuck to what they previously knew. Hence, reaching such a community might require a special form of understudying. Below is feedback from our study participants:
Whenever there is a misconception about COVID-19, when we come there, we see a lot of stories about the vaccine, and even when we correct them, some of them are still spreading the stories. So, we find it very difficult to convince people, there are some places we go and break barriers, but there are places we cannot go once and break barriers (FGD/Mobile Team/Makurdi LGA/Benue State).
Demand for incentives by the locals
The demand for financial incentives and other consumable items by the locals was another challenge encountered by the mobile/community. Some community dwellers were not willing to avail themselves of the vaccine, except the vaccine comes with incentives attached to it. Findings from the Focus Group Discussion are presented below:
We have had many challenges when we go for the field, in many settlements to discuss, sometimes when they come around, they will say, “Is it because of the town announcement that was made, you are here?” Why are you not bringing money or even if it is Maggi, why are you not bringing anything for us to share for the people? (FGD/Mobile Team/Edatti LGA/Niger State)
We used to get challenges because before they come if you ask them to come and take the vaccine, they will say, is this money that we intend to give them? This vaccine is not beneficial to them. Is it food? If there is no food, we should go, we cannot give them vaccines. We will then visit the place again. Then, the social mobilizer will help us to explain to them so that they will understand and come and take the vaccine (FGD/Mobile Team/Chachanga LGA/Niger State).
Difficulty with accessibility and transportation
Participants also mentioned the challenges they experienced with reaching people, especially those in hard-to-reach communities. There are situations where the roads are not motorable, limited means of transportation, and hikes in transportation fares during rainy seasons to such areas. They emphasized these outlined issues as significant hindrances to vaccination coverage.
First of all, the challenge that we’ve had at times is farther communities that are not close to the health facility, therefore you must look for a way to go ahead of the vaccination team to tell the people. Sometimes, if logistics are not provided, we would have challenges getting to these places because they are very far places. Sometimes we spend our money on going to that place and it is not good for us, because our transport allowance will not cover it (FGD/Mobile Team/Wushishi LGA/Niger State).
Another challenge we encounter is mobility, one thing we do is enter villages, where these people, the poor masses that cannot afford to take these vaccines, or where transport issues might be a problem to come to the primary health care to access these vaccines (FGD/Mobile Team/Otukpo LGA/Benue State).
Although the distance to communities and mobility issues, particularly during the rainy seasons were a major impediment for health workers (mobile teams) to access communities for the optimization of COVID-19 vaccination, however, the teams are usually committed to ensuring that they get to the communities by any means available to them.
Health information system
Inadequate stationaries and reporting materials
According to the participants, two major threats to the documentation and reporting of vaccination data from the field activities among mobile teams during their COVID-19 vaccination exercise. These were paper-based documentation and technological-related challenges. Participants revealed that the documentation of the vaccination exercise is usually affected by a lack of registers and a shortage of writing tools. These eventually result in inconvenience for the team, as they temporarily substitute the absence of registers with an exercise book which would require them to re-document the information on the registers when they become available. Additionally, the health workers expressed that they experienced significant challenges that are directly and indirectly related to technology or in this case, electronic documentation. The following excerpts from the study interview provide more evidence for this section:
My major challenge is my writing tool; which is my pen because I am doing more of writing as a paper recorder and I always have to document everything on paper and cards. However, sometimes my pen will stop working and sometimes the ink will finish, and there will be no place to buy another pen nearby. Also, when the cards that given we will give to the people we vaccinate, it affects us and is another challenge that we face. (FGD/Mobile Team_/Ogbadibo LGA/Benue State)
Sometimes we do not have cards that can help us scan the QR code, and it used to affect us in the field. Now that there are no registers, we use exercise books to register people that are coming. One, getting all the information in the register transferred to the notebook is not easy and the notebook is sometimes too small for the two spread pages to contain it all. It is a challenge there and you know exercise book can tear quicker than the register and it can easily get lost (FGD/Mobile Team/Ushongo LGA/Benue State).
Limited internet access
Participants emphasized that they experienced several challenges related to entering and submitting their data electronically. Essentially, limited power supply in their communities had a negative influence on electronic gadgets used for collecting clients’ information and reporting daily coverage data. Additionally, participants also experienced network issues in certain distant communities during some of the outreach visits. Similarly, there were concerns over issues associated with accessing and operating the electronic app adopted to report COVID-19 vaccination data at the national and sub-national levels. Evidence from the discussion sessions with the mobile teams is presented below:
The challenge I have sometimes is with my data. If I enter where I want to synchronize sometimes, I just see off I can’t see any clearance line, to tell me or show that it’s sent or done, I can’t see it. So sometimes when am confused I later tell my oga (boss) they use to call the LIO, and he will give us advice on what to do if we go to a place that doesn’t have a network (FGD/Mobile Team/Edatti LGA/Niger state).
For more than four months we don’t have light. When we go to outreaches, we go with our phone and the charger, to charge them, because sometimes as you see us like this we are going to the settlements for a whole day. So, when we finish like this, I am a validator because NG is the identification number for the people we want to vaccinate. So, I will type out all the NGs on my Kobo Collect one by one. So, after typing this one back into my phone, I will send it before the battery I have left on my phone is finished/Mobile Team/Wushishi LGA/Niger State)
We met our LIO one time telling them we don’t have data money because this work consumes data a lot and at times the money … in fact, there was a time they sent 2300 naira to our account each When we consider our transportation, our feeding money and how can we cope to even buy the data. So, they should if they can support and be sending the data directly to us. To subscribe for us directly, so, that it would save the work (FGD/Mobile Team/Bosso LGA/Niger State).
Sending this vaccination information needs resources, which is an internet data subscription. So, you must have your internet data subscription. If you don’t have your internet data, your reports are not going to be delivered. So, we use an internet data subscription for sending this report (FGD/Moile Team/Katsina Ala LGA/Benue State).
In addition to that one other major challenge is the fluctuation in the network. Sometimes you go to a community where you have a cluster of people after explaining to them the need to be vaccinated and it’s well accepted, trying to get their details captured is a problem because sometimes network fluctuates and it becomes a problem after a while some times we can go ahead and capture these guys and then give to them the vaccine (FGD/Mobile Team/Otukpo LGA/Benue State).
Mobile team experiences on covid–19 vaccine integration into extant health structures
Interestingly, all the study participants emphasized that they integrated COVID-19 vaccination into at least one extant public health intervention in their respective localities. While some participants leverage the routine immunization services offered through the outreach services, others utilize other public health services like HIV/TB testing services.
Participants exuded that integration was slightly challenging for the teams when they experienced certain hindrances. Teams partnering with other implementing partners expressed that the occasional; unavailability of their partnering team affects their performance, as they seem to have established a symbiotic relationship with them, and as such performance tends to be limited when the other team is unavailable. Additionally, teams who leveraged routine immunization are sometimes troubled by the absence of COVID-19 vaccines, while the RI antigens are available.
To get to more people what we did was that we were doing RI and COVID-19. So, we combined all vaccinations every day for the RI and the COVID-19 vaccine. So by the time we start, we call the town announcer to explain to them, Even the child, we tell the caregiver to bring the child, those aged zero to 59 months, 0–11 months, so everybody came, so like our vaccinator, we arrange the vaccine for each of the category of people we want to vaccinate ( not audible) if they have the card for the RI they can bring it and we give the child the RI vaccine. We also ask the caregiver if she has received the COVID-19 vaccine. For those who said “no”, we would administer the vaccination to them (FGD /Mobile Team/Edatti LGA/Niger State).
Okay, so in our team, we work with teams from other partners, and we used to integrate. We go to the HIV clinic with the Breakthrough team and do awareness campaigns with them too, and we also work with KNCV. This influences because like, KNCV, the BP apparatus that we are using, most people will not intend to take the vaccine, but once they see that they will check their BP, it will motivate them to come for it and at times, if they check their BP, we will tell them that as you have check your BP it’s good that you take the COVID − 19 vaccine also (FGD/Mobile Team/Makurdi LGA/Benue State).
The study participants took the initiative, either on their own, or through the stakeholders at the LGA and state levels, and/or partners working with the state health authorities, to ensure the optimization of COVID-19 vaccination. This strategy equally adopted integrated campaigns of public health interventions to leverage and drive vaccination exercises in the communities. The adopted strategy is therefore highly plausible for similar interventions that may occur in posterity. Furthermore, participants expressed that the little challenge that comes with integration may be impactful.
The only challenge is that when one is not there, to some extent it might affect the work. Just like for instance, the breakthrough is not there. Maybe we are going to a particular community and then Breakthrough has not come to play the role they are to play to some extent. The uptake of vaccination will not be as it should have been. So, when they come, just like we said when they play music and all that attracts, it draws people’s attention. So, the moment they’re not there, it will then turn up will be encouraging not as it should have been, because at that level it’s only the mobilizer that is doing it, and he has to go from one door to another so it, to some extent, it’s not that easy (FGD/Mobile Team/Makurdi LGA//Benue State).
The challenge is that when we want to go to the community to go and vaccinate the community, we go and collect vaccines. they can have Penta and BCG, but they will not have COVID-19 and we cannot go to the community alone with RI vaccines. (FGD/Mobile Team/Bosso LGA/Niger State)
Discussion
Our study assessed the perceptions and experiences of health workers who operated as mobile teams for COVID-19 vaccination uptake in Benue and Niger states. To explore their perception of optimizing COVID-19 vaccination and the challenges encountered, the study adapted the WHO Health Building Blocks Framework across key areas that align with the study objective.
Our study found that mobile health workers generally hold the perception that they have made significant contributions to the optimization and attained the success of COVID-19 vaccination in Benue and Niger states. Specifically, the mobile teams opined that their visitation to communities, and their door-to-door campaigns and administration of COVID-19 vaccines in various settlements of the local government areas in the selected states are the major drivers of optimizing COVID-19, as well as increasing community residents’ accessibility to the vaccines. This corroborates the findings of [47] who reported that Volunteer Community Mobilizers (VCM) adopted innovative strategies including door-to-door campaigns, community dialogues, compound meetings, and community health camps to optimize vaccination in 5 states across 31 LGAs.
This thought may be premised on the notion that many of the community residents did not prioritize the need to visit health facilities to be administered the COVID-19 vaccine either because of perceived low-risk infection, conspiracies and myths around the vaccines, and the distance that these facilities have to their location. However, the mobile teams successfully located them in their communities and convinced these locals to accept and take the vaccines. The mobile health workers also reported that they are well acquainted with and inclined about the rules and ethics expected of them to maintain the vaccine potency to ensure its efficacy. Although the team spent hours on the field during outreaches, they endeavoured to optimize the capacity of the ice pack inside the Geostar to maintain the vaccine potency. Subsequently, they return unused vaccines to the refrigerator in the cold chain unit as a necessity to preserve the vaccines.
Our study findings also revealed that mobile health workers hold the perception that their engagement as extra hands to support fixed health workers (i.e., health workers domiciled in the facilities), significantly influenced the optimization of COVID-19 vaccination in Benue and Niger states because they were actively engaged in reaching the nooks and crannies of their local government areas to address misconceptions about COVID-19 and educate community residents on the benefits of taking COVID-19 vaccines while they are also getting people vaccinated. This claim alludes to the outcomes of “The Maximizing Uptake Programme” [48] in the Southwest of England, where outreach service was used to vaccinate underserved populations such as homeless people, refugees, and asylum seekers who are highly susceptible to COVID-19 and/or have limited access to vaccination centers. The perception held by the teams may be based on the possibility of observing a high level of hesitancy among community residents, particularly residents domiciled in underserved communities of the various LGAs where the mobile teams operate.
Our study also found that the adopted reporting structure by the mobile teams was a Bottom-top approach wherein data collected in the communities on COVID-19 vaccination are entered into the tally sheets and registers, which will eventually be submitted to the facility once the sheet and registers are filled. The data are subsequently entered electronically on the EMID platform while on the field. This is then submitted and shared with the LGA level officials who then share with the state officials. This method of reporting may have been adopted to ensure data validity and reliability before pushing such data to the national level where the coverage for each state is reported in a hierarchical structure in an ascending order. This reporting approach alludes to the assertion of Kanma-Okafor et al. [49] that vaccination exercises in Nigeria are premised on a bottom-top approach.
Findings from our study revealed that mobile teams deployed certain strategies in reaching the targeted population for vaccination, including advocacy visits to the community leaders to unveil their intentions and mission in the community which helps to gain the buy-in of the ruler. Secondly, engage the service of a social mobilizer who visits the community dwellers to create awareness and sensitize them before the vaccination on the purpose, venue, and duration of the vaccination activities. This is similar to the approach adopted by the outreach teams created by the health ministry in Iraq with support from UNICEF to optimize COVID-19 vaccination, where a team of health workers attached to a primary health facility, go to villages to vaccinate people [41].
In documenting the challenges experienced by the mobile teams, this study revealed that prevailing misconceptions around the COVID-19 vaccines, desired incentives for vaccines among community residents, and adverse events following immunizations acted as a clog in the wheel in the teams’ quest to get people vaccinated with COVID-19 vaccines. This alludes to the studies of Zhuang et al. [50–52], who reported misconceptions about the COVID-19 vaccine, and the adverse events following immunization as drivers of COVID-19 vaccine hesitancy respectively. Contrarily, Berger et al. [53] reported a significant relationship, establishing that increased perceived severity (of COVID-19 disease), and perceived benefits (of COVID-19 vaccine) increase the likelihood of being vaccinated. Consequently, these challenges experienced by the health workers regarding COVID-19 vaccination in the communities, influence the communal residents’ perceived benefits and perceived barriers towards the COVID-19 vaccine. This corroborates the report of Limbu et al. [54] who found that perceived benefits and perceived barriers are the most common HBM constructs associated with vaccine hesitancy. Although participants asserted that they were able to diffuse the situations, however, these challenges, particularly the desire for incentives by community residents might have been influenced by the government’s claims to provide palliatives for the disadvantaged populace, regarding people in underserved communities, and the residents experiencing renege on the part of the government.
Findings from our study equally revealed that the distance of facilities to the communities, and the unavailability of a free transportation system for the teams to get to these distant communities were the major barriers experienced in ensuring communal residents’ accessibility to the COVID-19 vaccines. These challenges, particularly the distance, might be due to the large landmass of the two selected states. Niger state, for instance, has the largest landmass in Nigeria [55], and many of the scattered settlements in the local government areas of the state are more than 5 km from their nearest health facilities making it difficult to access health facilities. This has also been compounded by the recent removal of subsidies for petroleum products, in the country, as the cost of a litter of fuel has tripled the extant price at the inception of the vaccination exercise in the country [56]. This is because the outreach vaccination exercises were still on at the time of the sudden removal of the subsidy for petroleum products by the president of the Federal Republic of Nigeria.
Our study findings revealed that mobile health workers experienced several challenges vis-à-vis paper-based information documentation of the vaccinees. The teams experienced inadequate availability of registers required for manual documentation of the vaccination details including the number of vaccinees and this was a menace to the team as they found it difficult to record the information of the intending vaccinees. On the other hand, challenges such as poor network, malfunction of the EMID app, and inadequate power supply to charge gadgets were the issues experienced by the mobile teams in the course of their duties. This is similar to the study of Mbunge et al. [57] who reported infrastructural and technological challenges such as poor internet access and app malfunctions as barriers to digital health services employed in South Africa during COVID-19. However, the health workers did not let the experiences affect their work and performance, as the team innovatively developed solutions such as temporarily using exercise books to replace unavailable registers, charging their gadgets with small amounts in a charging center, and logging into the app in areas with a quality network, while data are entered offline, and subsequently synchronizing the data after securing a quality network.
Finally, findings from our study revealed that the mobile teams adopted an integration strategy to optimize COVID-19 vaccination in both Benue and Niger states. Integration was done across other extant public health interventions in their states and the specific local government areas where they find themselves. This is in line with the strategy employed by UNICEF (Hopkins et al., 2023) with the outreach teams in Iraq through an approach tagged the 3Is’ (Intensive, Integrated, and Immunization), to address the sub-optimal routine immunization while also ensuring increased COVID-19 vaccination coverage. However, this success did not come without its challenges, as our study found that the absence of other intervention teams in the environment where mobile teams were optimizing COVID-19 vaccination resulted in slowed-pace vaccination campaigns, as what used to be a double barrel technique was no longer such due to the absence of the complementing team.
Limitations of the study
Although, the study was designed to include two local government areas per senatorial district, security challenges reported in the state across some LGAs (including two of our initially selected LGAs) at the time of the study influenced the replacement of two LGAs in our study, resulting in a skewed LGA selection process.
Conclusion and recommendations
Generally, the integral role played by mobile health workers in the optimization of COVID-19 vaccination and other public health interventions cannot be overemphasized. Over the years, mobile health workers have consistently proven to be a force to be reckoned with and a strategy that intervention implementers can always fall back on to optimize public health interventions, specifically, COVID-19 vaccination.
Ultimately, as a team, they are bound to experience successes and challenges, that are within and outside their control. Using the adapted WHO Health System Building Block framework, it is obvious that the majority of the challenges experienced are not directly within their controls, and as such it is pertinent to involve all stakeholders: across all levels, particularly at the community level, and within the health industry, that are directly and indirectly involved with community health interventions to support the (mobile) health workers by ensuring that all necessary strategies and/or prerequisites are put in place to facilitate optimum performance from advocacy visit to the communities to drive the implementation of public health interventions.
Recommendations
Based on the findings from the study, recommendations include but are not limited to; first, the need for an upward review in the stipends paid to these teams, which subsequently, will aid selfless service delivery, especially in locating hard-to-reach populations. Secondly, there is the need to consider other data reporting options suitable for the kind of remote environment visited by the outreach team to ease data reporting for improved decision-making in the future. Lastly, it is important to consider involving additional implementing partners in the drive to reach more people with the vaccination message and to effectively integrate COVID-19 vaccination into extant health structures in these states and communities.
Acknowledgements
We would like to acknowledge the United States Center for Disease Control (US-CDC) for providing the support and funding of the project intervention on the optimization of COVID–19 vaccination in Benue and Niger states through our organization (Sydani Initiative for International Development, Nigeria). We also want to extend our appreciation to the National Primary Healthcare Development Board (NPHCDA) and the State Primary Healthcare Board of Benue and Niger states for their support during the project phases.
Author contributions
The article was conceptualized by SDI and SN, who conducted the qualitative analysis and drafted the manuscript. OWS reviewed the manuscript and made direct edits on the manuscript. SA and AUJ conducted a programmatic review of the paper to approve any program discussions from the paper. SS oversaw the intervention support provided to the two states. VD, JCD, IO, and ZA participated in project implementation in the two states.
Funding
This study did not receive any external funding or grant from any funding agency in the public, commercial, or non-profit sectors.
Data availability
The data supporting the findings will be available from the corresponding author upon request following a 1-year embargo from the publication date. Requests will be examined and considered on a case-by-case basis.
Declarations
Ethical approval and consent to participate
The research protocols were reviewed and approved by the National Emergency Routine Immunization Coordinating Centre (NERICC), the Institutional (internal) Review Board of the National Primary Health Care Development Agency (NPHCDA) in Abuja, Nigeria. The research adhered to the principles outlined in the Helsinki Declaration. Additionally, written informed consent was obtained from each participant prior to the commencement of the research.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oleribe O, Ezechi O, Osita-Oleribe P, Olawepo O, Musa AZ, Omoluabi A, Fertleman M, Salako BL, Taylor-Robinson SD. Public perception of COVID-19 management and response in Nigeria: a cross-sectional survey. BMJ Open. 2020;10(10):e041936. 10.1136/bmjopen-2020-041936. PMID: 33055123; PMCID: PMC7559048. 10.1136/bmjopen-2020-041936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gill S, Adenan AM, Ali A, Ismail NAS. Living through the COVID-19 pandemic: Impact and lessons on Dietary Behavior and Physical Well-Being. Int J Environ Res Public Health. 2022;19(2):642. 10.3390/ijerph19020642. PMID: 35055469; PMCID: PMC8775925. 10.3390/ijerph19020642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haffejee S, Vostanis P, O’Reilly M, Law E, Eruyar S, Fleury J, Hassan S, Getanda E. Disruptions, adjustments and hopes: the impact of the COVID-19 pandemic on child well-being in five Majority World Countries. Child Soc 2022 Mar 31:10.1111/chso.12563. doi: 10.1111/chso.12563. Epub ahead of print. PMID: 35602421; PMCID: PMC9111791. [DOI] [PMC free article] [PubMed]
- 4.Moore S, Hill EM, Tildesley MJ, Dyson L, Keeling MJ. Vaccination and non-pharmaceutical interventions for COVID-19: a mathematical modelling study. Lancet Infect Dis. 2021;21(6):793–802. doi: 10.1016/S1473-3099(21)00143-2. Epub 2021 Mar 18. PMID: 33743847; PMCID: PMC7972312. [DOI] [PMC free article] [PubMed]
- 5.So B, Kwon KH. The impact of physical activity on well-being, lifestyle and health promotion in an era of COVID-19 and SARS-CoV-2 variant. Postgrad Med. 2022;134(4):349–58. Epub 2022 Mar 30. PMID: 35285767. 10.1080/00325481.2022.2052467 [DOI] [PubMed] [Google Scholar]
- 6.Tatar M, Wilson FA. The largest vaccination campaign in history: a golden opportunity for bundling public health interventions. J Glob Health. 2021;11:03076. 10.7189/jogh.11.03076. PMID: 34055326; PMCID: PMC8141326. 10.7189/jogh.11.03076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations International Children Emergency Funds (UNICEF). COVID-19 Vaccines shipped by COVAX arrive in Nigeria. https://www.unicef.org/wca/press-releases/covid-19-vaccines-shipped-covax-arrive-nigeria#:~:text=Abuja%2C%202%20March%202021%20%2D%20Today,%2C%20Gavi%2C%20UNICEF%20and%20WHO. Last Accessed 28 October 2023.
- 8.Chapman LAC, Shukla P, Rodríguez-Barraquer I, Shete PB, León TM, Bibbins-Domingo K, Rutherford GW, Schechter R, Lo NC. Risk factor targeting for vaccine prioritization during the COVID-19 pandemic. Sci Rep. 2022;12(1):3055. 10.1038/s41598-022-06971-5. PMID: 35197495; PMCID: PMC8866501. 10.1038/s41598-022-06971-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nomhwange T, Wariri O, Nkereuwem E, Olanrewaju S, Nwosu N, Adamu U, Danjuma E, Onuaguluchi N, Enegela J, Nomhwange E, Jean Baptiste AE, Mulombo WK. COVID-19 vaccine hesitancy amongst healthcare workers: an assessment of its magnitude and determinants during the initial phase of national vaccine deployment in Nigeria. EClinicalMedicine. 2022;50:101499. 10.1016/j.eclinm.2022.101499. PMID: 35770256; PMCID: PMC9233171. 10.1016/j.eclinm.2022.101499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chukwuocha UM, Emerole CO, Iwuoha GN, Dozie UW, Njoku PU, Akanazu CO, Eteike PO, Hemingway C. Stakeholders’ hopes and concerns about the COVID-19 vaccines in Southeastern Nigeria: a qualitative study. BMC Public Health. 2022;22(1):330. 10.1186/s12889-022-12754-4. PMID: 35172789; PMCID: PMC8848682. 10.1186/s12889-022-12754-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emeka C, Edu B, Ekpenyong J, Getachew B, Chabo J, Abdurhaman UP, Ntui NB, Chukwu E, Ekpenyong N. COVID-19 vaccine roll-out at the community level in developing countries: lessons learnt from Cross River State, Nigeria. Public Health Pract (Oxf). 2022;4:100273. Epub 2022 May 21. PMID: 35614950; PMCID: PMC9123799. 10.1016/j.puhip.2022.100273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eguavoen A, Larson HJ, Chinye-Nwoko F, Ojeniyi T, Reducing. COVID-19 vaccine hesitancy and improving vaccine uptake in Nigeria. J Public Health Afr. 2023;14(5):2290. 10.4081/jphia.2023.2290. PMID: 37492424; PMCID: PMC10365642. 10.4081/jphia.2023.2290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zwawua O, Kor E. Factors Associated with COVID-19 vaccine hesitancy among a rural sample in Benue State, Nigeria: a qualitative study. Nigerian J Hlth Promotion. 2022; 15(1).
- 14.Uroko FC, Okwuosa L. The link between aphorisms on jewish eschatological expectation of the anti-christ and COVID-19 vaccine hesitancy among pentecostal christians in Makurdi, Nigeria. Theologia Viatorum. 2022;46(1):150. 10.4102/tv.v46i1.150 [DOI] [Google Scholar]
- 15.Alcendor DJ. Targeting COVID Vaccine Hesitancy in Rural communities in Tennessee: implications for extending the COVID-19 pandemic in the South. Vaccines (Basel). 2021;9(11):1279. 10.3390/vaccines9111279. PMID: 34835210; PMCID: PMC8621887. 10.3390/vaccines9111279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO). Vaccine hesitancy: A growing challenge for immunization programmes. 2020. https://www.who.int/news/item/18-08-2015-vaccine-hesitancy-a-growing-challenge-for-immunization-programmes#:~:text=Vaccine%20hesitancy%20refers%20to%20delay,%2C%20complacency%2C%20convenience%20and%20confidence. Last Accessed October 12, 2023.
- 17.Hassen HD, Welde M, Menebo MM. Understanding determinants of COVID-19 vaccine hesitancy; an emphasis on the role of religious affiliation and individual’s reliance on traditional remedy. BMC Public Health. 2022;22(1):1142. 10.1186/s12889-022-13485-2. PMID: 35672720; PMCID: PMC9172606. 10.1186/s12889-022-13485-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atoi EN. The scourge of coronavirus (COVID-19) and religious beliefs in Nigeria: matters arising. J Relig Hum Relations. 2022;14(1):1–20. 10.4314/jrhr.v14i1.1 [DOI] [Google Scholar]
- 19.Chilanga E, Dzimbiri M, Mwanjawala P, Keller A, Mbeya RA. Religion, politics and COVID-19 risk perception among urban residents in Malawi. BMC Public Health. 2022;22(1):1430. 10.1186/s12889-022-13858-7. PMID: 35897087; PMCID: PMC9326149. 10.1186/s12889-022-13858-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Enders AM, Uscinski J, Klofstad C, Stoler J. On the relationship between conspiracy theory beliefs, misinformation, and vaccine hesitancy. PLoS ONE. 2022;17(10):e0276082. 10.1371/journal.pone.0276082. PMID: 36288357; PMCID: PMC9604946. 10.1371/journal.pone.0276082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pivetti M, Melotti G, Bonomo M, Hakoköngäs E. Conspiracy beliefs and Acceptance of COVID-Vaccine: an exploratory study in Italy. Social Sci. 2021;10(3):108. 10.3390/socsci10030108. 10.3390/socsci10030108 [DOI] [Google Scholar]
- 22.Milošević Đorđević J, Mari S, Vdović M, Milošević A. Links between conspiracy beliefs, vaccine knowledge, and trust: anti-vaccine behavior of Serbian adults. Soc Sci Med. 2021;277:113930. 10.1016/j.socscimed.2021.113930. Epub 2021 Apr 13. PMID: 33873008; PMCID: PMC8634900. 10.1016/j.socscimed.2021.113930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Afolabi MO, Wariri O, Saidu Y, Otu A, Omoleke SA, Ebenso B, Adebiyi A, Ooko M, Ahinkorah BO, Ameyaw EK, Seidu AA, Agogo E, Nomhwange T, Salami K, Mohammed NI, Yaya S. Tracking the uptake and trajectory of COVID-19 vaccination coverage in 15 west African countries: an interim analysis. BMJ Glob Health. 2021;6(12):e007518. 10.1136/bmjgh-2021-007518. PMID: 34906987; PMCID: PMC8718349. 10.1136/bmjgh-2021-007518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Betsch C, Schmid P, Verger P, Lewandowsky S, Soveri A, Hertwig R, Fasce A, Holford D, De Raeve P, Gagneur A, Vuolanto P, Correia T, Tavoschi L, Declich S, Marceca M, Linos A, Karnaki P, Karlsson L, Garrison A. A call for immediate action to increase COVID-19 vaccination uptake to prepare for the third pandemic winter. Nat Commun. 2022;13(1):7511. 10.1038/s41467-022-34995-y. PMID: 36473855; PMCID: PMC9726862. 10.1038/s41467-022-34995-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ezeibe CC, Ilo C, Ezeibe EN, Oguonu CN, Nwankwo NA, Ajaero CK, Osadebe N. Political distrust and the spread of COVID-19 in Nigeria. Glob Public Health. 2020;15(12):1753–66. Epub 2020 Oct 6. PMID: 33019916. 10.1080/17441692.2020.1828987 [DOI] [PubMed] [Google Scholar]
- 26.Adigwe OP. COVID-19 vaccine hesitancy and willingness to pay: emergent factors from a cross-sectional study in Nigeria. Vaccine X. 2021;9:100112. 10.1016/j.jvacx.2021.100112. Epub 2021 Sep 3. PMID: 34494000; PMCID: PMC8413098. 10.1016/j.jvacx.2021.100112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ekstrand ML, Heylen E, Gandhi M, Steward WT, Pereira M, Srinivasan K. COVID-19 vaccine hesitancy among PLWH in South India: implications for Vaccination campaigns. J Acquir Immune Defic Syndr. 2021;88(5):421–5. PMID: 34757971; PMCID: PMC8575086. 10.1097/QAI.0000000000002803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barattucci M, Pagliaro S, Ballone C, Teresi M, Consoli C, Garofalo A, De Giorgio A, Ramaci T. Trust in Science as a possible mediator between different antecedents and COVID-19 booster vaccination intention: an integration of Health Belief Model (HBM) and theory of planned behavior (TPB). Vaccines (Basel). 2022;10(7):1099. 10.3390/vaccines10071099. PMID: 35891265; PMCID: PMC9320855. 10.3390/vaccines10071099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zampetakis LA, Melas C. The health belief model predicts vaccination intentions against COVID-19: a survey experiment approach. Appl Psychol Health Well Being. 2021;13(2):469–84. 10.1111/aphw.12262. Epub 2021 Feb 26. PMID: 33634930; PMCID: PMC8014148. 10.1111/aphw.12262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wonodi C, Obi-Jeff C, Adewumi F, Keluo-Udeke SC, Gur-Arie R, Krubiner C, Jaffe EF, Bamiduro T, Karron R, Faden R. Conspiracy theories and misinformation about COVID-19 in Nigeria: implications for vaccine demand generation communications. Vaccine. 2022;40(13):2114–21. Epub 2022 Feb 7. PMID: 35153088; PMCID: PMC8830779. 10.1016/j.vaccine.2022.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olu-Abiodun O, Abiodun O, Okafor N. COVID-19 vaccination in Nigeria: a rapid review of vaccine acceptance rate and the associated factors. PLoS ONE. 2022;17(5):e0267691. 10.1371/journal.pone.0267691. PMID: 35544545; PMCID: PMC9094528. 10.1371/journal.pone.0267691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oyeyemi SO, Fagbemi S, Busari II, Wynn R. Belief in COVID-19 conspiracy theories, level of Trust in Government Information, and willingness to take COVID-19 vaccines among Health Care workers in Nigeria: Survey Study. JMIR Form Res. 2023;7:e41925. 10.2196/41925. PMID: 37068055; PMCID: PMC10189621. 10.2196/41925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ojewale LY, Mukumbang FC. COVID-19 vaccine hesitancy among nigerians living with non-communicable diseases: a qualitative study. BMJ Open. 2023;13(2):e065901. 10.1136/bmjopen-2022-065901. PMID: 36731928; PMCID: PMC9895914. 10.1136/bmjopen-2022-065901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iliyasu Z, Umar AA, Abdullahi HM, Kwaku AA, Amole TG, Tsiga-Ahmed FI, Garba RM, Salihu HM, Aliyu MH. They have produced a vaccine, but we doubt if COVID-19 exists: correlates of COVID-19 vaccine acceptability among adults in Kano, Nigeria. Hum Vaccin Immunother. 2021;17(11):4057–64. Epub 2021 Oct 6. PMID: 34613864; PMCID: PMC8828136. 10.1080/21645515.2021.1974796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Demeke J, Ramos SR, McFadden SM, Dada D, Nguemo Djiometio J, Vlahov D, Wilton L, Wang M, Nelson LE. Strategies that promote equity in COVID-19 Vaccine Uptake for Latinx communities: a review. J Racial Ethn Health Disparities. 2023;10(3):1349–57. 10.1007/s40615-022-01320-8. Epub 2022 May 6. PMID: 35524004; PMCID: PMC9075141. 10.1007/s40615-022-01320-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dada D, Djiometio JN, McFadden SM, Demeke J, Vlahov D, Wilton L, Wang M, Nelson LE. Strategies that promote equity in COVID-19 Vaccine Uptake for Black communities: a review. J Urban Health. 2022;99(1):15–27. 10.1007/s11524-021-00594-3. Epub 2022 Jan 11. PMID: 35018612; PMCID: PMC8751469. 10.1007/s11524-021-00594-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sethy G, Chisema MN, Sharma L, Singhal S, Joshi K, Nicks PO, Laher B, Mamba KC, Deokar K, Damte T, Phuka J. ‘Vaccinate my village’ strategy in Malawi: an effort to boost COVID-19 vaccination. Expert Rev Vaccines. 2023 Jan-Dec;22(1):180–185. doi: 10.1080/14760584.2023.2171398. PMID: 36688599. [DOI] [PubMed]
- 38.Falope O, Nyaku MK, O’Rourke C, Hermany LV, Plavchak B, Mauskopf J, Hartley L, Kruk ME. Resilience learning from the COVID-19 pandemic and its relevance for routine immunization programs. Expert Rev Vaccines. 2022;21(11):1621–1636. doi: 10.1080/14760584.2022.2116007. Epub 2022 Sep 5. PMID: 36063485. [DOI] [PubMed]
- 39.Ogunbosi BO, Alao MA, Ibrahim OR, Ayuk AC, Ibraheem RM, Odimegwu CL, Ikwuka DC, Akintan P, Morakinyo O, Adeyemi AT, Jega RM, Olowookere TF, Bello OE, Owolabi BI, Chukwuyem A, Bukar LM, Rasaki A, Issa A, Ewa AU, Oladokun R, Akinyinka OO. COVID-19 vaccine hesitancy in six geopolitical zones in Nigeria: a cross-sectional survey. Pan Afr Med J. 2022;42:179. 10.11604/pamj.2022.42.179.34135. PMID: 36187029; PMCID: PMC9482243. 10.11604/pamj.2022.42.179.34135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sato R. COVID-19 vaccine hesitancy and trust in government in Nigeria. Vaccines (Basel). 2022;10(7):1008. 10.3390/vaccines10071008. PMID: 35891171; PMCID: PMC9317906. 10.3390/vaccines10071008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hopkins KL, Underwood T, Iddrisu I, Woldemeskel H, Bon HB, Brouwers S, De Almeida S, Fol N, Malhotra A, Prasad S, Bharadwaj S, Bhatnagar A, Knobler S, Lihemo G. Community-based approaches to increase COVID-19 vaccine uptake and demand: lessons learned from four UNICEF-Supported interventions. Vaccines (Basel). 2023;11(7):1180. 10.3390/vaccines11071180. PMID: 37514996; PMCID: PMC10384848. 10.3390/vaccines11071180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kulle AC, Schumacher S, von Bieberstein F. Make it easy: Lowering transaction costs substantially increases COVID-19 vaccinations. 2022. Available at SSRN 4166827.
- 43.Schleiff MJ, Aitken I, Alam MA, Damtew ZA, Perry HB. Community health workers at the dawn of a new era: 6. Recruitment, training, and continuing education. Health Res Policy Syst. 2021;19(Suppl 3):113. 10.1186/s12961-021-00757-3. PMID: 34641898; PMCID: PMC8506097. 10.1186/s12961-021-00757-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization (WHO). Health Systems Governance. 2020. https://www.who.int/india/health-topics/health-systems-governance. Last Accessed June 15, 2024.
- 45.World Health Organization (WHO). Monitoring the Building Blocks of Health System: A Handbook of Indicators and their Measurement Strategies. 2010. https://iris.who.int/bitstream/handle/10665/258734/9789241564052-eng.pdf. Last Accessed June 15, 2024.
- 46.Paulus TM. Hum Res Dev Rev. 2023;22(1):139–48. 10.1177/15344843221138381. Using Qualitative Data Analysis Software to Support Digital Research Workflows. 10.1177/15344843221138381 [DOI]
- 47.Duru JI, Usman S, Adeosun O, Stamidis KV, Bologna L. Contributions of Volunteer Community mobilizers to Polio Eradication in Nigeria: the experiences of non-governmental and Civil Society Organizations. Am J Trop Med Hyg. 2019;101(4Suppl):74–84. 10.4269/ajtmh.19-0068. PMID: 31760970; PMCID: PMC6776094. 10.4269/ajtmh.19-0068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berrou I, Hamilton K, Cook C, Armour C, Hughes S, Hancock J, Quigg S, Hajinur H, Srivastava S, Kenward C, Ali A, Hobbs L, Milani E, Walsh N. Leaving no one behind: interventions and outcomes of the COVID-19 Vaccine Maximising Uptake Programme. Vaccines (Basel). 2022;10(6):840. 10.3390/vaccines10060840. PMID: 35746447; PMCID: PMC9227842. 10.3390/vaccines10060840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kanma-Okafor O, Odusolu Y, Abayomi A, Shuaib F, Adeyeye M, Mustapha I, Ogboye S, Lajide D, Abdur-Razzaq H, Okafor U, Elemuwa U, Osibogun A. A qualitative analysis of the COVID-19 vaccination rollout in Lagos, Nigeria: client and provider perspectives on the plan, the process and the progress. PLOS Glob Public Health. 2022;2(11):e0000486. 10.1371/journal.pgph.0000486. PMID: 36962511; PMCID: PMC10021997. 10.1371/journal.pgph.0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhuang W, Zhang J, Wei P, Lan Z, Chen R, Zeng C, Shi Q, Qiao G. Misconception contributed to COVID-19 vaccine hesitancy in patients with lung cancer or ground-glass opacity: a cross-sectional study of 324 Chinese patients. Hum Vaccin Immunother. 2021;17(12):5016–23. Epub 2021 Oct 29. PMID: 34715002; PMCID: PMC8903957. 10.1080/21645515.2021.1992212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kowalska-Duplaga K, Duplaga M. The association of conspiracy beliefs and the uptake of COVID-19 vaccination: a cross-sectional study. BMC Public Health. 2023;23(1):672. 10.1186/s12889-023-15603-0. PMID: 37041546; PMCID: PMC10088115. 10.1186/s12889-023-15603-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Babaee E, Amirkafi A, Tehrani-Banihashemi A, SoleimanvandiAzar N, Eshrati B, Rampisheh Z, Asadi-Aliabadi M, Nojomi M. Adverse effects following COVID-19 vaccination in Iran. BMC Infect Dis. 2022;22(1):476. 10.1186/s12879-022-07411-5. PMID: 35585518; PMCID: PMC9116064. 10.1186/s12879-022-07411-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berger C, Ben-Shalom U, Tarant Z, Longo J, DeDonno M. The influence of the Health Belief Model on the decision to get the COVID-19 vaccine: an International Survey Study of College Students. INQUIRY: J Health Care Organ Provis Financing. 2023;60. 10.1177/00469580231164229. [DOI] [PMC free article] [PubMed]
- 54.Limbu YB, Gautam RK, Pham L. The Health Belief Model Applied to COVID-19 vaccine hesitancy: a systematic review. Vaccines (Basel). 2022;10(6):973. 10.3390/vaccines10060973. PMID: 35746581; PMCID: PMC9227551. 10.3390/vaccines10060973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adenle AA, Boillat S, Speranza CI. Key dimensions of land users’ perceptions of Land Degradation and Sustainable Land Management in Niger State, Nigeria. Environ Challenges. 2022;8. 10.1016/j.envc.2022.100544.
- 56.Yunusa E, Yakubu Y, Emeje YA, Ibrahim YB, Stephen E, Egbunu DA. Fuel subsidy removal and poverty in Nigeria: A literature review. Int J App Mgt Sci. 2023;4(9):14–27. 10.5281/zenodo.8409907. 10.5281/zenodo.8409907 [DOI] [Google Scholar]
- 57.Mbunge E, Batani J, Gaobotse G, Muchemwa B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Glob Health J. 2022;6(2):102–13. 10.1016/j.glohj.2022.03.001. Epub 2022 Mar 5. PMID: 35282399; PMCID: PMC8897959. 10.1016/j.glohj.2022.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Paulus TM. Hum Res Dev Rev. 2023;22(1):139–48. 10.1177/15344843221138381. Using Qualitative Data Analysis Software to Support Digital Research Workflows. 10.1177/15344843221138381 [DOI]
Data Availability Statement
The data supporting the findings will be available from the corresponding author upon request following a 1-year embargo from the publication date. Requests will be examined and considered on a case-by-case basis.