The most common type of cardiac tumour found in children is a rhabdomyoma. These benign masses are commonly associated with the tuberous sclerosis complex, an autosomal dominant neurocutaneous disorder that affects multiple organs. We present 2 paediatric cases with an atypical location of cardiac rhabdomyoma associated with the unusual presenting feature of arrhythmia.
Cardiac tumours in children are rare, and the most common type found in children is a rhabdomyoma.1 These benign masses are commonly associated with the tuberous sclerosis complex (TSC), an autosomal dominant neurocutaneous disorder that affects multiple organs.2 We present 2 paediatric cases with an atypical location of cardiac rhabdomyoma associated with the unusual presenting feature of arrhythmia.
Case Descriptions
Case 1
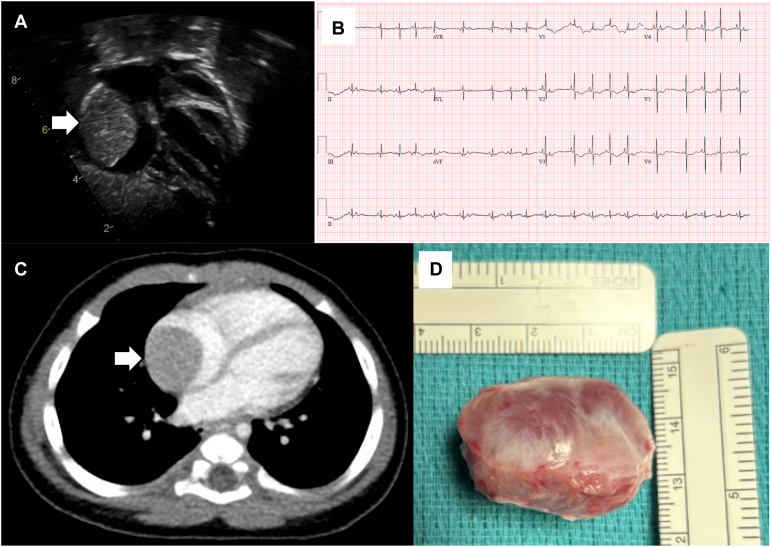
A female infant was seen as an outpatient at 4 months of age for follow-up. She had been diagnosed antenatally with frequent premature atrial ectopic contractions (PACs) causing bradycardia. A fetal echocardiogram was reported as being structurally normal. She was the product of a twin pregnancy (dichorionic and diamniotic) and delivered prematurely at 33 weeks and 3 days’ gestational age. During hospitalization in the neonatal intensive care unit, she was noted to have frequent isolated PACs. An echocardiogram performed on the first day of life was reported as being within normal limits. After discharge, feeding and growth were normal. At her outpatient appointment, physical examination was normal, but her echocardiogram demonstrated a large (2 × 2 cm) right atrial tumour (Fig. 1A). A retrospective review of the previous echocardiogram identified a small right atrial mass measuring 0.5 × 0.5 cm. An electrocardiogram (ECG) (Fig. 1B) and a 24-hour Holter monitor demonstrated frequent (20%) isolated PACs. A computed tomography scan demonstrated a sharply circumscribed 2.0 × 2.2 × 3.1 cm tumour within the right atrium (Fig. 1C). She underwent surgery for resection of the mass at 5 months of age. The tumour was quite adherent to the atrial wall with a broad base and a firm consistency (Fig. 1D). She developed a persistent junctional rhythm postoperatively, and she was discharged home on postoperative day 5. A Holter monitor performed 2 weeks postoperatively showed predominantly junctional rhythm with an average heart rate of 81 beats per minute with examples of sinus rhythm. There was no significant ectopy with just 8 isolated PACs. At 8 months of follow-up, she was found to have both sinus and junctional beats. Pathology determined the tumour to be a benign and well-differentiated cardiac rhabdomyoma. She was referred to Genetics for evaluation of TSC. No clinical features of TSC were identified. No reportable variants were detected in TSC1 or TSC2, and the chromosomal microarray was normal. She is demonstrating progressive recovery of sinus rhythm.
Figure 1.
Case 1 presenting arrhythmia and imaging findings. (A) Echocardiogram demonstrated a large right atrial tumour (arrow). (B) Frequent isolated premature atrial contractions. (C) Computed tomography image of the mass (arrow). (D) Appearance of the resected mass.
Case 2
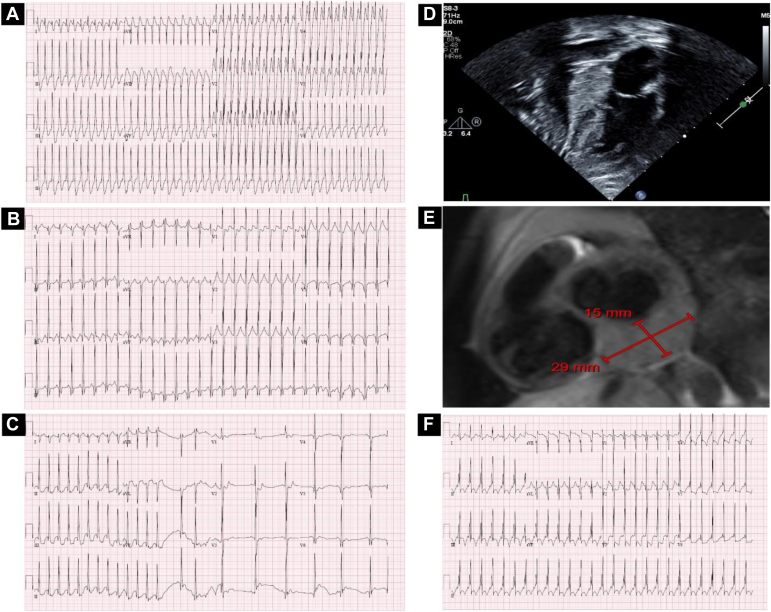
A previously healthy female patient presented at 2 years of age with fever, vomiting, and supraventricular tachycardia with a heart rate of >280 beats per minute (Fig. 2A). She was diagnosed with COVID-19 pneumonia and converted to sinus rhythm with adenosine and oral propranolol (Fig. 2B and C). Her ECG demonstrated intermittent pre-excitation. An echocardiogram revealed a large (1.8 × 2.7 cm) homogeneous and echogenic mass behind the left ventricle (Fig. 2D). There was normal cardiac function, and no other cardiac abnormalities were identified. She was started on atenolol. A computed tomography scan showed a homogeneous soft tissue mass adjacent to the left atrium and left ventricle. A cardiac magnetic resonance imaging (Fig. 2E) identified abnormal tissue involving the inferior surface of the basal left ventricular myocardium and extending slightly above the left atrioventricular groove, posterior to the left atrium. The mass (2.8 × 2.9 × 1.5 cm) was contained within the pericardium, and T1 and T2 signal intensities of the mass were similar to the myocardium with no late gadolinium enhancement. Signal characteristics were consistent with a rhabdomyoma. An ultrasound demonstrated small echogenicities in the left renal cortex. Given the cardiac mass and hypopigmented skin lesions, she was referred to Genetics. Testing identified a pathogenic de novo mutation in TSC2 (c.4951A>C, p.Asn1651His) compatible with a diagnosis of TSC. Growth and development have been normal, and she has had no seizures and no recurrence of arrhythmia on atenolol. Her ECG continues to demonstrate intermittent pre-excitation consistent with Wolff-Parkinson-White syndrome (Fig. 2F).
Figure 2.
Case 2 presenting arrhythmia, imaging, and pathology findings. (A) Presenting tachycardia. (B) Subsequent electrocardiogram (ECG) (obtained on the same day as presenting ECG) showing sinus tachycardia with a short PR interval. (C) ECG showing supraventricular tachycardia converting to sinus rhythm. (D) Echocardiographic imaging of the mass behind the left atrium. (E) Cardiac magnetic resonance T1-weighted imaging of the mass measuring 15 × 29 mm. (F) ECG demonstrating pre-excitation consistent with Wolff-Parkinson-White syndrome.
Discussion
Cardiac rhabdomyomas are usually found within the myocardium and can be associated with outflow tract obstruction and/or interference with valvar function.1 Atypical locations of rhabdomyomas can occur, as shown in both our cases. Cardiac rhabdomyomas may be identified incidentally or during investigations for TSC.2 In our patients, cardiac arrhythmia was the presenting feature, and investigations diagnosed a benign isolated rhabdomyoma and TSC. Most rhabdomyomas resolve spontaneously, and the enlargement that we observed in case 1 is rare.3,4 The junctional rhythm experienced by the patient in the postoperative period appears to have been secondary to intraoperative injury to the sinus node at the time of tumour resection but is fortunately showing signs of resolution. In case 1, there was preoperative diagnostic uncertainty about the type of tumour, but pathology identified a rhabdomyoma and genetic testing confirmed that the tumour was not related to TSC.
In case 2, the cardiac mass was outside of the heart but created a manifest accessory pathway that enabled the development of supraventricular tachycardia. In case 2, magnetic resonance imaging tissue characterization was consistent with a rhabdomyoma, and diagnosis of TSC caused by a novel variant in TSC2 confirmed the diagnosis.
Novel Teaching Points.
-
•
Although most commonly associated with tuberous sclerosis complex and usually embedded within the myocardium, rhabdomyomas can present with arrhythmia and unusual location.
-
•
Spontaneous resolution is the most common outcome, but progressive enlargement is possible.
-
•
Cardiac magnetic resonance imaging is helpful in characterizing the mass with additional investigations required to identify the underlying etiology.
Acknowledgments
Ethics Statement
The research reported in this case report has adhered to all relevant ethical guidelines.
Patient Consent
The patients’ parents provided informed consent for the preparation and publication of this case report.
Funding Sources
No funding was received for this study.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Amonkar G.P., Kandalkar B.M., Balasubramanian M. Cardiac rhabdomyoma. Cardiovasc Pathol. 2009;18:313–314. doi: 10.1016/j.carpath.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Randle S.C. Tuberous sclerosis complex: a review. Pediatr Ann. 2017;46:e166–e171. doi: 10.3928/19382359-20170320-01. [DOI] [PubMed] [Google Scholar]
- 3.Kiztanir H., Sulu A., Akin T., Kosger P., Ucar B. Fetal and postnatal diagnosis and management of cardiac rhabdomyomas and association with tuberous sclerosis complex. Cir Cardiovasc. 2023;30:294–299. [Google Scholar]
- 4.Bader R.S., Chitayat D., Kelly E., et al. Fetal rhabdomyoma: prenatal diagnosis, clinical outcome, and incidence of associated tuberous sclerosis complex. J Pediatr. 2003;143:620–624. doi: 10.1067/S0022-3476(03)00494-3. [DOI] [PubMed] [Google Scholar]