Abstract
Objectives:
Returns to the Emergency Department (ED) and unplanned readmissions within 90 days of shoulder arthroplasty represent a significant financial burden to healthcare systems. Identifying the reasons and risk factors could potentially reduce their prevalence.
Methods:
A retrospective review of primary anatomic (aTSA) and reverse shoulder arthroplasty (rTSA) cases from January 2016 through August 2023 was performed. Demographic patient and surgical data, including age, diagnosis of anxiety or depression, body mass index (BMI), smoking status, age-adjusted Charlson Comorbidity Index (ACCI), modified 5-item fragility index (mFI-5), and hospital length of stay (LOS) was collected. Patient visits to the ED within 12 months prior to surgery were recorded. Predictors for return to the ED within 90 days postoperatively and any readmissions were determined.
Results:
There were 338 cases (167 aTSA and 171 rTSA), of which 225 (67%) were women. Patients with anxiety (OR=2.44, 95% CI 1.11–5.33; P=0.026), surgical postoperative complications (OR=3.22, 95% CI 1.36–7.58; P=0.008), ED visit within 3 months prior to surgery (OR=3.80, 95% CI 1.71–8.45; P=0.001), ED visit 3 to 6 months prior to surgery (OR=2.60, 95% CI 1.12–6.05; P=0.027), and ED visit 6 to 12 months prior to surgery (OR=2.12, 95% CI 1.02–4.41; P=0.045) were more likely to have ED visit within 90 days postoperatively. Patients with prior ipsilateral shoulder surgery (OR=3.32, 95% CI 1.21–9.09; P=0.02), surgical postoperative complications (OR=13.92, 95% CI 5.04–38.42; P<0.001), an ED visit within 3 to 6 months preoperatively (OR=8.47, 95% CI 2.84–25.27; P<0.001), and an mFI-5 ≥2 (OR=3.66, 95% CI 1.35–9.91; P=0.011) were more likely to be readmitted within 90 days.
Conclusion:
Patients who present to the ED within 12 months prior to shoulder arthroplasty, those with anxiety, those with surgical complications and those with higher fragility should be monitored closely during the early postoperative period to minimize returns to the ED and/or unplanned readmissions.
Key Words: 90-day readmission, Modified fragility index, Return to emergency department, Risk factors
Introduction
The incidence of shoulder arthroplasty in the United States has been projected to experience a significant increase compared with both hip and knee arthroplasty.1 This expanded utilization has been demonstrated for both anatomic (aTSA) and reverse total shoulder arthroplasty (rTSA).2,3 Return visits to the ED and unplanned hospital readmissions during the 90-day postoperative global period following primary TSA represent key quality metrics, in addition to being significant drivers of the cumulative cost of care.4,5 The recent inclusion of outpatient total shoulder arthroplasty in the Centers for Medicare & Medicaid Services (CMS) Bundled Payments for Care Improvement Advanced (BPCIa) program has been associated with decreased implant and day of surgery total costs.6,7 The bundled payment program refers to an alternative payment model that centers on providing a single payment to institutions for all services provided during a patient’s total episode of care, which includes the 90-day post-discharge period.8 As private insurers inevitably transition to bundled payment models following shoulder arthroplasty, it is imperative that healthcare systems continue to focus on controlling the costs associated with each episode of care (EOC). Gowd et al., using a readmissions database, reported an 8.7% incidence of all-cause readmission following primary aTSA and rTSA, and calculated the average cost for readmission at nearly $14000.4 A similar mean cost of readmission has been demonstrated by others.7
Identifying modifiable factors associated with all-cause ED visits and readmissions could potentially result in the development of interventions to better optimize patients preoperatively and ease the cost burden on hospitals. Werner et al. found that approximately 9% of patients who underwent TSA experienced a postoperative ED visit within 90 days of surgery.5 Furthermore, the authors determined that more frequent presentations to the ED in the 12 months prior to TSA were significantly associated with an increasing risk for postoperative 90-day ED visits though the reason for the ED return visits could not be determined. With regards to 90-day readmissions, Pezzulo et al. reported a readmission incidence of 3.6% and further determined that an elevated medical risk was independently associated with increased readmission.7 Male gender and older age have also been demonstrated to be independently associated with readmission following TSA.9
Chung et al., in a study of aTSA using a national readmissions database, identified a Medicare payer status, transfer to skilled nursing facility (SNF), and chronic obstructive pulmonary disease as being associated with an increased risk for 90-day readmission, whereas female gender was associated with a lower risk for 90-day readmission.10 In a database study of rTSA from the same institution, the authors reported that the presence of diabetes, paralysis, hypertension, and a solid tumor without metastasis were independent predictors of 90-day readmission.11 In both studies, the incidence for readmission was reported at 1.7%.10,11 Finally, several studies have reported a significant association between increased patient frailty and readmission following TSA.12,13 Medical complications have been shown to represent a higher proportion of readmitted cases compared with surgical complications.14
The primary objectives of the current study were to: 1) determine the prevalence of all-cause 90-day ED visits and readmissions following primary TSA; 2) identify independent risk factors for all cause 90-day ED visits and readmissions following primary TSA; and 3) determine the reasons for the all-cause 90-day ED visit and readmissions. We hypothesized that patients who have at least one preoperative ED visit, those with an inpatient medical complication and those with a postoperative surgical complication were more likely to have an ED visit and/or readmission within 90 days.
Materials and Methods
We performed a retrospective assessment of all primary elective anatomic (aTSA) and reverse total shoulder arthroplasties (rTSA) conducted by a fellowship-trained orthopaedic surgeon from January 2016 through August 2023 at a single tertiary-referral teaching hospital. This study was approved by our institutional review board [#2024-15617]. Inclusion criteria included all patients who underwent an elective primary aTSA or rTSA who underwent surgery with a minimum 90-day follow-up period. Any patient who underwent a revision TSA, an arthroplasty for acute fracture, or an arthroplasty following prior fracture fixation was excluded.
We reviewed electronic health records (EHRs) to gather patient demographic data including age, sex, body mass index (BMI), marital status, preferred language (English vs. Spanish vs. Other), insurance type (Commercial vs. Medicare vs. Medicaid), self-identified race, smoking status (current vs. former vs. never smoked), age-adjusted Charlson Comorbidity Index (ACCI), modified 5-item Frailty Index (mFI-5), the distance from home-to-clinic, clinically diagnosed depression and/or anxiety, 12-month preoperative and 90-day postoperative visits to the ED along with presentation diagnoses, and 90-day unplanned postoperative readmissions. We collated sociodemographic status via utilization of the Area Deprivation Index (ADI), a tool that ranks neighborhoods by socioeconomic disadvantage at both the state and national level. The ADI tool is a multifaceted, evidence-based model that utilizes income, education, employment, and housing quality, amongst a multitude of other characteristics, to categorize and score the regions.15,16 At the state level, the data are given in deciles (1-10), with a score of 1 indicating the least disadvantaged and 10 indicating the most disadvantaged. At the national level, the data are given as percentiles, with the lower values representing the least disadvantaged. The ACCI is a validated instrument for predicting mortality based on underlying patient comorbid disease including peripheral vascular disease, myocardial infarction (MI), and chronic obstructive pulmonary disease (COPD), and was a modification of the original CCI by adjusting risk by age.17 The mFI-5 is a validated 5-item risk stratification tool that serves as a marker of physiologic decline and that has previously been demonstrated to be an accurate predictor of adverse outcomes and readmission following total shoulder arthroplasty.12,13
With regards to surgical data, we obtained the preoperative diagnosis, arthroplasty type (aTSA vs rTSA), American Society of Anesthesiologists (ASA) score, history of prior non-arthroplasty ipsilateral shoulder surgery, prior contralateral TSA, hospital length of stay, intraoperative complications, postsurgical complications within 4 weeks of surgery, in-hospital complications, operative time, intraoperative total blood volume loss (ITBVL), need for intra- or postoperative transfusion, and both postoperative day 1 and discharge visual analogue scale (VAS) pain assessment. We categorized the mFI-5 as <2 versus ≥2 as described previously in the literature.12 For the purpose of this study, we combined the medical- and surgical-related 90-day ED visits and readmission data given the low number of cases present. With regards to return to the ED, each visit was categorized as medical or surgical, and the specific reason was recorded. Surgically-related reasons included wound complications, intractable surgical site pain, or periprosthetic fractures/dislocations. Medical reasons were categorized based on the major organ system involved and those deemed to have a low prevalence were listed as “other”. A musculoskeletal (MSK) complaint with regards to 90-day return to the ED refers to any orthopaedic complaint not related to the surgical shoulder. With regards to return to the ED, if a patient was seen multiple times within the 90-day postoperative period, the tabulated reason for return (medical versus surgical) was categorized based on the diagnosis of the initial ED visit. Finally, we categorized the number of preoperative ED visits as 0, 1-2, or ≥3.
Statistical analysis
Continuous variables were presented as a median and associated inter-quartile range (IQR). Differences in demographic and medical characteristics between patients with and without ED visits or readmission within 90 days following surgery were compared using the Wilcoxon rank-sum test for continuous variables and chi-squared or Fisher’s exact tests for categorical variables. Logistic regression analysis was used to identify factors independently associated with 90-day ER visits and re-admission, and were presented as odds ratio (OR) with 95% confidence intervals (CI). Variables with P-value <0.25 in initial analyses were included in regression analysis.18 A P-value <0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4 (SAS, Inc., Cary, North Carolina).
Results
There were 338 total cases included in this study, of which 167 (49%) were aTSA and 171 (51%) were rTSA. Of the aTSA, there were 46 short-stem and 121 stemless humeral components. The median age of the cohort was 68 years (IQR 61, 73) and 225 (67%) were women. The median distance from home-to-clinic was 2.95 miles (IQR 2.2, 4.2) and the median national ADI percentile was 24 (IQR 17, 29). Forty-seven (14%) patients had previously undergone a contralateral TSA and 76 (22%) underwent prior ipsilateral non-fracture related shoulder surgery, with 65 (86%) having undergone a prior arthroscopy. In the 12 months prior to surgery, 111 (32.8%) patients were treated in the ED, of which 92 patients had either one or two visits and 19 had ≥3 visits. The total number of ED visits amongst the 111 patients was 212, of which 43 (20.2%) dealt primarily with a musculoskeletal complaint. The median number of preoperative ED visits within 12 months was 0 (IQR 0, 1).
90-day return to ED
There were 54 (15.9%) patients who experienced at least one return visit to the ED during the 90-day postoperative period for a total of 69 visits. Of these, 37 (68.5%) patients returned solely for medical reasons, 11 (20.4%) patients returned solely for surgical reasons and 6 (11.1%) patients presented for both a medical and surgical visit. Overall, 17 (31.5%) patients initially returned to the ED for a surgical-related reason and 37 (68.5%) returned for a medical-related reason. From the perspective of total postoperative ED visits, 18 (26%) visits were for surgical reasons and 51 (74%) were for medical reasons [Figures 1 and 2]. Following univariate analysis, having Medicaid insurance (P=0.014), a diagnosis of depression (P=0.003) or anxiety (P=0.001), a surgical complication within 4 weeks of surgery (P=0.012), and an ED visit within 12 months prior to shoulder arthroplasty (P<0.001) were significantly associated with an increased risk for all-cause 90-day ED visit [Table 1]. On logistic regression, patients with anxiety (OR 2.44), a surgical postoperative complications (OR 3.22), an ED visit within 3 months prior to surgery (OR 3.80), an ED visit within 3 to 6 months prior to surgery (OR 2.60), and an ED visit within 6 to 12 months prior to surgery (OR 2.12) were more likely to have an ED visit within 90 days after surgery [Table 2]. There was a significantly increased risk for 90-day ED return amongst patients with both 1-2 preoperative visits (OR 4.96) and ≥3 preoperative ED visits (OR 6.92) versus those without a preoperative ED visit.
Figure 1.
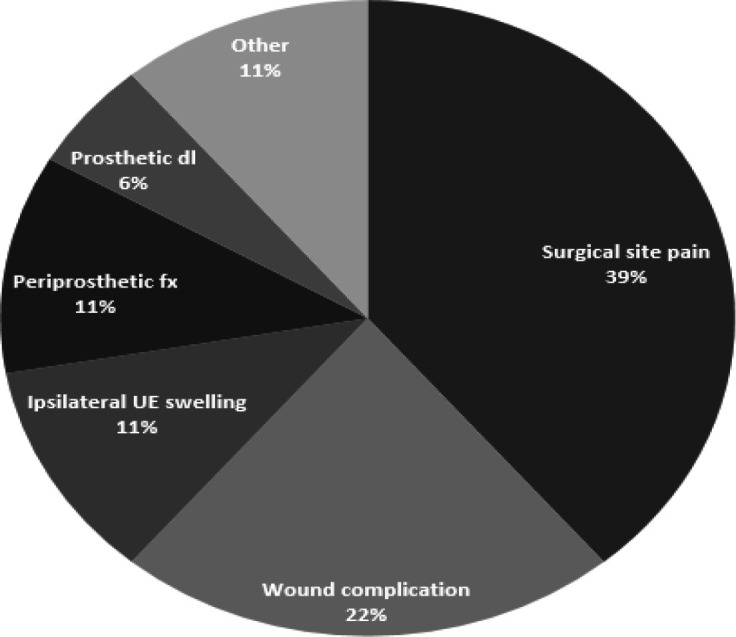
Surgery-related all-cause 90-day ED return (n=18) (UE: Upper Extremity; dl: dislocation; FX: fracture)
Table 1.
Characteristics and clinical variables for return to ED in 90 days post-surgery
| No return to ER in 90 days (N = 284) | Return to ER in 90 days (N = 54) | P values | |
|---|---|---|---|
|
Gender, n (%)
Female Male |
188 (66.2) 96 (33.8) |
37 (68.5) 17 (31.5) |
0.740 |
|
Preferred language, n (%)
English Spanish Other |
209 (73.6) 71 (25.0) 4 (1.4) |
39 (72.2) 14 (25.9) 1 (1.9) |
0.835 |
|
Insurance type, n (%)
Medicare Medicaid Commercial |
198 (69.7) 42 (14.8) 44 (15.5) |
38 (70.4) 14 (25.9) 2 (3.7) |
0.014 |
|
Race, n (%)
Caucasian Hispanic Black Asian |
50 (17.6) 144 (50.7) 86 (30.3) 4 (1.4) |
5 (9.3) 27 (50.0) 20 (37.0) 2 (3.7) |
0.211 |
|
Depression, n (%)
No Yes |
219 (77.1) 65 (22.9) |
31 (57.4) 23 (42.6) |
0.003 |
|
Anxiety, n (%)
No Yes |
248 (87.3) 36 (12.7) |
37 (68.5) 17 (31.5) |
0.001 |
|
ASA, n (%)
1,2 ≥3 |
136 (47.9) 148 (52.1) |
22 (40.7) 32 (59.3) |
0.335 |
|
MFI-5, n (%)
0-1 2-5 |
162 (57.0) 122 (43.0) |
29 (53.7) 25 (46.3) |
0.650 |
|
Smoking, n (%)
None Former Current |
141 (49.7) 108 (38.0) 35 (12.3) |
28 (51.8) 17 (31.5) 9 (16.7) |
0.541 |
|
Laterality, n (%)
Left Right |
121 (42.6) 163 (57.4) |
25 (46.3) 29 (53.7) |
0.616 |
|
Prior ipsilateral surgery, n (%)
No Yes |
225 (79.2) 59 (20.8) |
37 (68.5) 17 (31.5) |
0.084 |
|
Prior contralateral TSA, n (%)
No Yes |
243 (85.6) 41 (14.4) |
48 (88.9) 6 (11.1) |
0.517 |
|
Transfusion, n (%)
No Yes |
276 (97.2) 8 (2.8) |
53 (98.2) 1 (1.8) |
1.0 |
|
Hospital disposition, n (%)
Home Non-home |
260 (91.5) 24 (8.5) |
49 (90.7) 5 (9.3) |
0.794 |
|
Intraop complications, n (%)
No Yes |
278 (97.9) 6 (2.1) |
53 (98.2) 1 (1.8) |
1.0 |
|
Surgical postop complications in 4 weeks, n (%)
No Yes |
259 (91.2) 25 (8.8) |
43 (79.6) 11 (20.4) |
0.012 |
|
In hospital medical complications, n (%)
No Yes |
242 (85.2) 42 (14.8) |
43 (79.6) 11 (20.4) |
0.301 |
|
Surgical procedure, n (%)
SS ATSA Stemless ATSA SS RTSA |
40 (14.1) 103 (36.3) 141 (49.6) |
6 (11.1) 18 (33.3) 30 (55.6) |
0.790 |
|
ED visit in 1 year prior to surgery, n (%)
No Yes |
209 (73.6) 75 (26.4) |
18 (33.3) 36 (66.7) |
< 0.001 |
|
Number of ED visits in 1 year prior to surgery, n (%)
0 1-2 ≥3 |
209 (73.6) 65 (22.9) 10 (3.5) |
18 (33.3) 27 (50.0) 9 (16.7) |
< 0.001 |
|
ED visit in 3 months prior to surgery, n (%)
No Yes |
262 (92.2) 22 (7.8) |
36 (66.7) 18 (33.3) |
< 0.001 |
|
ED visit in 3 to 6 months prior to surgery, n (%)
No Yes |
259 (91.2) 25 (8.8) |
39 (72.2) 15 (27.8) |
< 0.001 |
|
ED visit in 6 to 12 months prior to surgery, n (%)
No Yes |
237 (83.4) 47 (16.6) |
32 (59.3) 22 (40.7) |
< 0.001 |
| Age, median (IQR) | 68.0 (61.0, 73.0) | 68.0 (62.0, 73.0) | 0.841 |
| Distance to clinic, median (IQR) | 2.9 (2.1, 4.23) | 3.0 (2.4, 4.2) | 0.751 |
| ADI state decile, median (IQR) | 6 (4, 6) | 5 (5, 6) | 0.605 |
| ADI national %, median (IQR) | 24 (17, 28.5) | 21.5 (17, 31) | 0.953 |
| Number of preop visits attended, median (IQR) | 3 (2, 4) | 2 (2, 4) | 0.532 |
| BMI, median (IQR) | 31.7 (27.6, 36.5) | 31.2 (27.6, 33.0) | 0.224 |
| ACCI, median (IQR) | 3 (2, 4) | 4 (2, 4) | 0.464 |
| Operative time, median (IQR) | 116 (98, 136) | 116 (101, 136) | 0.871 |
| ITBVL, median (IQR) | 219.0 (139.5, 318.9) | 217.2 (159.6, 340.2) | 0.643 |
| Hospital stay, median (IQR) | 2 (1, 2) | 2 (1, 2) | 0.777 |
| Pain POD1, median (IQR) | 4 (2, 7) | 3.5 (0, 7) | 0.977 |
| Pain at discharge, median (IQR) | 2 (0, 4) | 3 (0, 4) | 0.191 |
| Pain change from POD1 (pain at discharge – pain at day 1), median (IQR) | -1 (-4, 0) | 0 (-3, 0) | 0.348 |
ASA: American Society of Anesthesiologists; mFI-5: 5-item modified frailty index; TSA: total shoulder arthroplasty; SS ATSA: short-stem anatomic total shoulder arthroplasty; SS RTSA: short-stem reverse total shoulder arthroplasty; ED: emergency department; ADI: Area Deprivation Index; IQR: interquartile range; BMI: body mass index; ACCI: age-adjusted Charlson Comorbidity Index; ITBVL: intraoperative total blood volume loss; POD: postoperative day
Table 2.
Factors associated with return to ED in 90 days post-surgery following regression analysis
| Characteristic | Adjusted Odds Ratio (95% CI) | P value |
|---|---|---|
|
Anxiety
Yes No (reference) |
2.44 (1.11 – 5.33) 1 |
0.026 |
|
Surgical postop complication
Yes No (reference) |
3.22 (1.36 – 7.58) 1 |
0.008 |
|
ED visit in 3 months prior to surgery
Yes No (reference) |
3.80 (1.71 – 8.45) 1 |
0.001 |
|
ED visit in 3 to 6 months prior to surgery
Yes No (reference) |
2.60 (1.12 – 6.05) 1 |
0.027 |
|
ED visit in 6 to 12 months prior to surgery
Yes No (reference) |
2.12 (1.02 – 4.41) 1 |
0.045 |
Figure 2.
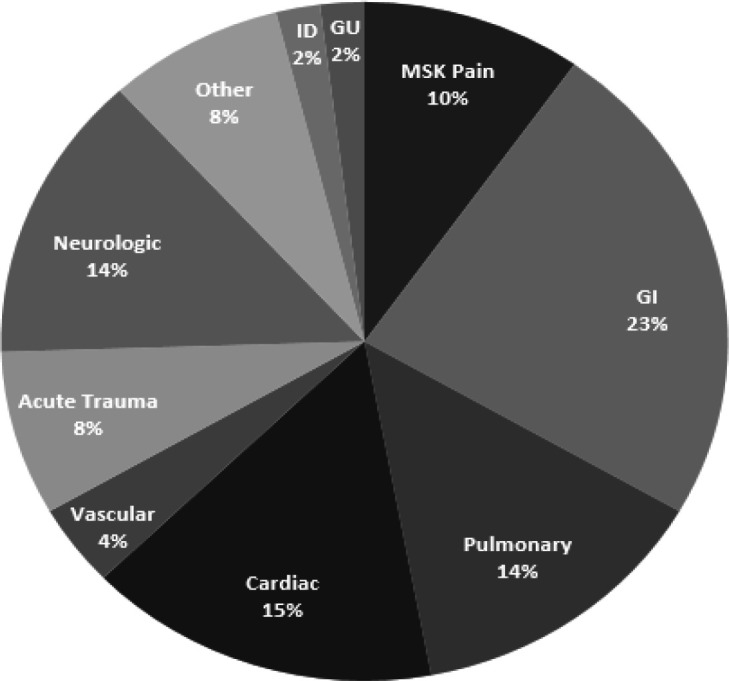
Medical-related all-cause 90-day ED return (n=51) (GU: Genitourinary; GI: Gastrointestinal; MSK: Musculoskeletal; ID: Infectious Disease)
90-day Readmission
There were 25 (7.4%) readmissions within 90 days following TSA and no patient was readmitted more than once. Of these, 12 (48%) were medically-related and 13 (52%) were surgically-related. The reasons for surgical readmission were hematoma (4), prosthetic instability (4), wound drainage (3) and periprosthetic fracture (2). Following univariate analysis, having undergone prior ipsilateral non-arthroplasty surgery (P=0.029), a surgical complication within 4 weeks of surgery (P<0.001), an in-hospital medical complication (P=0.02), or an ED visit within 3-6 months of surgery (P<0.001) were associated with an unplanned 90-day readmission [Table 3]. Following regression analysis, patients prior ipsilateral surgery (OR 3.32), surgical postoperative complications (OR 13.92), an ED visit in 3 to 6 months prior to surgery (OR 8.47), and an mFI-5 ≥2 (OR 3.66) were more likely to be readmitted within 90 days following TSA [Table 4].
Table 3.
Characteristics and clinical variables for 90-day all-cause readmission
| No readmission (N = 313) | Readmission (N = 25) | P values | |
|---|---|---|---|
|
Gender, n (%)
Female Male |
208 (66.5) 105 (33.5) |
17 (68.0) 8 (32.0) |
0.875 |
|
Preferred language, n (%)
English Spanish Other |
230 (73.5) 5 (1.6) 78 (24.9) |
18 (72.0) 0 7 (28.0) |
0.872 |
|
Insurance type, n (%)
Medicare Medicaid Commercial |
214 (68.4) 54 (17.2) 45 (14.4) |
22 (88.0) 2 (8.0) 1 (4.0) |
0.157 |
|
Race, n (%)
Caucasian Hispanic Black Asian |
53 (16.9) 161 (51.4) 94 (30.0) 5 (1.6) |
2 (8.0) 10 (40.0) 12 (48.0) 1 (4.0) |
0.139 |
|
Depression, n (%)
No Yes |
234 (74.8) 79 (25.2) |
16 (64.0) 9 (36.0) |
0.238 |
|
Anxiety, n (%)
No Yes |
265 (84.7) 48 (15.3) |
20 (80.0) 5 (20.0) |
0.566 |
|
ASA, n (%)
1,2 ≥3 |
147 (47.0)166 (53.0) | 11 (44.0) 14 (56.0) |
0.775 |
|
MFI-5, n (%)
0-1 2-5 |
182 (58.2) 131 (41.8) |
9 (36.0) 16 (64.0) |
0.032 |
|
Smoking, n (%)
None Former Current |
158 (50.5) 113 (36.1) 42 (13.4) |
11 (44.0) 12 (48.0) 2 (8.0) |
0.520 |
|
Laterality, n (%)
Left Right |
138 (44.1) 175 (55.9) |
8 (32.0)17 (68.0) | 0.240 |
|
Prior ipsilateral surgery, n (%)
No Yes |
247 (78.9) 66 (21.1) |
15 (60.0) 10 (40.0) |
0.029 |
|
Prior contralateral TSA, n (%)
No Yes |
270 (86.3) 43 (13.7) |
21 (84.0) 4 (16.0) |
0.763 |
|
Transfusion, n (%)
No Yes |
306 (97.8) 7 (2.2) |
23 (92.0) 2 (8.0) | 0.137 |
|
Hospital disposition, n (%)
Home Non-home |
287 (91.7) 26 (8.3) |
22 (88.0) 3 (12.0) |
0.462 |
|
Intraop complications, n (%)
No Yes |
306 (97.8) 7 (2.2) |
25 (100) 0 |
1.0 |
|
Surgical postop complications in 4 weeks, n (%)
No Yes |
289 (92.3) 24 (7.7) |
12 (48.0) 13 (52.0) |
< 0.001 |
|
In hospital medical complications, n (%)
No Yes |
268 (85.6) 45 (14.4) |
17 (68.0) 8 (32.0) |
0.020 |
|
Surgical procedure, n (%)
SS ATSA Stemless ATSA SS RTSA |
43 (13.7) 114 (36.4) 156 (49.8) |
3 (12.0) 7 (28.0) 15 (60.0) |
0.652 |
|
ER visit in 1 year prior to surgery, n (%)
No Yes |
214 (68.4) 99 (31.6) |
13 (52.0) 12 (48.0) |
0.094 |
|
Number of ER visits in 1 year prior to surgery, n (%)
0 1-2 3 or more |
214 (68.4) 83 (26.5) 16 (5.1) |
13 (52.0) 9 (36.0) 3 (12.0) |
0.117 |
|
ER visit in 3 months prior to surgery, n (%)
No Yes |
278 (88.8) 35 (11.2) |
20 (80.0) 5 (20.0) |
0.197 |
|
ER visit in 3 to 6 months prior to surgery, n (%)
No Yes |
282 (90.1) 31 (9.9) |
16 (64.0) 9 (36.0) |
< 0.001 |
|
ER visit in 6 to 12 months prior to surgery, n (%)
No Yes |
247 (78.9) 66 (21.1) |
22 (88.0) 3 (12.0) |
0.438 |
| Age, median (IQR) | 68.0 (61.0, 73.0) | 70.0 (66.0, 73.0) | 0.277 |
| Distance to clinic, median (IQR) | 3.0 (2.2, 4.3) | 2.6 (1.5, 3.5) | 0.120 |
| ADI state decile, median (IQR) | 6 (4, 6) | 6 (5, 7) | 0.195 |
| ADI national %, median (IQR) | 23 (17, 28) | 25 (17, 44) | 0.299 |
| Number of preop visits attended, median (IQR) | 3 (2, 4) | 3 (2, 4) | 0.286 |
| BMI, median (IQR) | 31.6 (27.7, 36.3) | 30.8 (26.9, 32.7) | 0.144 |
| ACCI, median (IQR) | 3 (2, 4) | 4 (3, 6) | 0.100 |
| Operative time, median (IQR) | 116 (99, 136) | 118 (99, 140) | 0.602 |
| ITBVL, median (IQR) | 218.0 (139.7, 319.4) | 218.7 (153.2, 324.4) | 0.694 |
| Hospital stay, median (IQR) | 2 (1, 2) | 2 (2, 3) | 0.118 |
| Pain POD1, median (IQR) | 4 (2, 7) | 3 (0, 7) | 0.826 |
| Pain at discharge, median (IQR) | 2 (0, 4) | 3 (1, 4) | 0.241 |
| Pain change from POD1 (pain at discharge – pain at day 1), median (IQR) | -1 (-4, 0) | 0 (-4, 1) | 0.275 |
ASA: American Society of Anesthesiologists; mFI-5: 5-item modified frailty index; TSA: total shoulder arthroplasty; SS ATSA: short-stem anatomic total shoulder arthroplasty; SS RTSA: short-stem reverse total shoulder arthroplasty; ED: emergency department; ADI: Area Deprivation Index; IQR: interquartile range; BMI: body mass index; ACCI: age-adjusted Charlson Comorbidity Index; ITBVL: intraoperative total blood volume loss; POD: postoperative day
Table 4.
Factors associated with 90-day all-cause readmission from ED following regression analysis
| Characteristic | Adjusted Odds Ratio (95% CI) | P value |
|---|---|---|
|
Prior ipsilateral surgery
Yes No (reference) |
3.32 (1.21 – 9.09) 1 |
0.020 |
|
Surgical postop complication
Yes No (reference) |
13.92 (5.04 – 38.42) 1 |
< 0.001 |
|
ED visit in 3 to 6 months prior to surgery
Yes No (reference) |
8.47 (2.84 – 25.27) 1 |
< 0.001 |
|
mFI-5
2-5 0-1 (reference) |
3.66 (1.35 – 9.91) 1 |
0.011 |
MFI-5: 5-item modified frailty index
Discussion
We conducted a retrospective analysis of a consecutive cohort of primary aTSA and rTSA performed at a single institution to determine the prevalence of and independent risk factors for 90-day return to the ED and unplanned readmissions. The main findings of this study were that, amongst patients who underwent elective TSA, a diagnosis of anxiety, the development of a postoperative surgical complication, and a preoperative visit to the ED within 12 months of surgery was independently predictive of a postoperative 90-day ED visit. The risk increased with visits that occurred nearer to the surgical date, in addition to a greater number of preoperative ED visits. Additionally, patients with prior ipsilateral non-arthroplasty shoulder surgery, the development of a surgical postoperative complication, increased frailty, and an ED visit in 3 to 6 months prior to surgery were independently predictive of a 90-day readmission following TSA.
We found that patients who were evaluated in the ED within 12 months of TSA were more likely to have a return to the ED within 90 days of surgery. The prevalence of a postoperative ED visit within 90 days of surgery in this study was nearly 16%, for which the reasons were predominately medical in nature. Werner et al., in a Medicare database study examining only aTSA, found that 8.6% of patients had a postoperative ED visit and that a preoperative ED visit within 12 months of surgery was an independent risk factor for 90-day postoperative ED visit.5 The authors, however, were unable to determine the cause of the return ED visits. We found that approximately 70% of the return visits dealt with medically-related diagnoses. In contrast to their finding that there was no association between the proximity of the preoperative ED visit and the risk for a 90-day postoperative visit, we found that an ED visit within 3 months of surgery had a nearly four times higher likelihood of ED return versus a visit within 6-12 months which had a two-fold higher likelihood. The difference may be a result of our inclusion of both aTSA and rTSA as opposed to just aTSA in their study. Similar to their results, we did identify a dose-dependent relationship between the number of preoperative ED visits and the risk for postoperative 90-day ED visits. Young et al. found that, amongst patients with a regular clinician, non-financial barriers such as the clinic not being open and no available or convenient clinic appointment represented significant reasons for ED visits.19 Proposed strategies to minimize the likelihood of postoperative ED visits following TSA should include educating patients as to actual urgent signs and symptoms requiring an ED visit and instructing them on the effective contact strategies with the outpatient surgical team for less urgent matters.
Furthermore, we found that a diagnosis of anxiety, but not depression, was significantly associated with a 90-day ED visit. Vinton et al. reported that a mental healthcare assessment in the prior 12 months was associated with both frequent (≥4 visits) and super-frequent (>10 visits) trips to the ED.20 Further, the authors found that a patient mentality that the ED was the place to go when sick was similarly associated with frequent and super-frequent ED use. In contrast, Kuhlmann et al. found no significant difference in postoperative ED visits following TSA in patients who had anxiety and/or major depressive disorder versus a control group.21 However, isolated analysis of either anxiety or depression was not undertaken as in our study, and multivariable analysis of independent associations with postoperative ED visits was not performed. Ensuring that any patient with anxiety disorder has been receiving the appropriate treatment, including the use of medication and outpatient follow-up with a mental health specialist, would be an important potential strategy for mitigating visits to the ED following shoulder arthroplasty.
With regards to readmissions, we found a 7.4% prevalence within 90 days, with over half of the cases being related to a surgical issue, split evenly between wound-related issues and implant-related issues. Our readmission incidence was somewhat higher than that previously shown by others which ranged from 1.7-2.7%.9-11 Similar to our findings, however, Lu et al., using the National Readmissions Database, found an all-cause 90-day readmission incidence of 7.76% and 4.37% for rTSA and aTSA, respectively, with even higher rates amongst inpatient- versus outpatient-performed procedures.22 Furthermore, Xu et al. demonstrated that two-thirds of the readmissions were medical in nature, with pneumonia and urinary tract infections being the most common etiologies.14 In contrast, Chung et al. reported that 73% of 90-day readmissions were complications related to the implant, with dislocations being the most common reason.10 We found that 52% of readmissions in the current study were surgical in nature with 46% directly related to the implant. The remainder was related to persistent wound drainage and enlarging hematomas. Finally, similar to the study by Chung et al., we did not find an association between CCI and risk for readmission. The apparent evolving trend towards surgical, as opposed to medical reasons for readmission, may be a result of more effective pre-surgical patient optimization.10
A history of prior ipsilateral shoulder surgery was found to be associated with increased risk for 90-day readmission. Our findings were discordant with a prior study by Malik et al., though that study focused solely on pre-arthroplasty arthroscopic procedures.23 this may be a result of the higher prevalence of shoulder arthroscopy (19.2%) prior to TSA in our study, and our inclusion of prior open (2%) and open/scope (1.2%) cases. We further found that an mFI-5 score of 2+ was significantly associated with a nearly four-fold increased risk for 90-day readmission, a particularly important result which may be underestimated given the overall low prevalence of readmissions in this cohort. Our results were similar to prior studies examining the effect of fragility on readmission following TSA.12,13 Holzgrefe et al. reported that frailty was significantly associated with 30-day readmission and that the effect was higher than that shown for patient age.12 Several studies have also reported that higher mFI-5 scores were independent predictors of postoperative adverse outcomes and mortality following TSA.12,13 This relationship between frailty and postoperative complications may explain our finding that a postoperative
surgical complication itself was a significant predictor of 90-day readmission. An assessment of frailty represents a straightforward means of stratifying a patient’s risk for potential postoperative readmission following TSA and a potential intervention point including judicious use of home healthcare services and involvement of patient family members during the early postoperative period.
There were certainly limitations to the current study including those that are inherent in the retrospective nature of the study. The incidence of visits to the ED could have been underestimated if patients had been evaluated in an Urgent Care Center or ED and did not bring this to the attention of the treating orthopaedic surgeon. Similarly, patients with emergent issues may have had readmission to another hospital outside of our health system, potentially underestimating the incidence of readmission. However, the vast majority of our patients receive all of their medical and orthopaedic care through our health system, and we believe this number to be negligible. Furthermore, these procedures were performed by a single fellowship-trained orthopaedic surgeon at a tertiary referral center and may not be generalizable to other surgeons practicing in different locations. Finally, the diagnosis of anxiety and depression was based on the diagnosis in the medical record as opposed to the use of validated patient reported outcomes measures. Strengths of the study include the numerous patient- and surgery-related predictive factors included. Furthermore, we included a validated assessment of a patient’s socioeconomic situation using the Area Deprivation Index.
Conclusion
Patients who had at least one preoperative visit to the ED are more likely to experience a return to the ED in the 90-day postoperative period after TSA, and the risk increases with a greater number of preoperative ED visits and a visit closer to the surgery date. Furthermore, those with increased frailty and those with a postoperative complication were more likely to experience readmission within 90-days. Knowledge of the risk factors for these adverse outcomes can drive interventions to reduce their incidence and result in decreased healthcare costs.
Acknowledgment
Not applicable
Authors Contribution:
Cameron Smith: Investigation, writing original draft
Robert Ades: Investigation
Yungtai Lo: Statistical Analysis
Savino Stallone: Investigation, conceptualization
Suhirad Khokhar: Writing original draft
Konrad Gruson: Writing original draft and revision, conceptualization.
Declaration of Conflict of Interest:
KIG is a paid consultant for Stryker Wright Medical. CS, RA, YL, SS, SK have no financial relationships to report.
Declaration of Funding:
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of Ethical Approval for Study:
Institutional Review Board approved study, Albert Einstein College of Medicine. IRB#2024-15617, approved 1/12/2024.
Declaration of Informed Consent:
Does not apply as none of the information in the submitted manuscript can be used to identify patients.
References
- 1.Wagner ER, Farley KX, Higgins I, Wilson JM, Daly CA, Gottschalk MB. The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg. 2020;29(12):2601–2609. doi: 10.1016/j.jse.2020.03.049. [DOI] [PubMed] [Google Scholar]
- 2.Dillon MT, Chan PH, Inacio MCS, Singh A, Yian EH, Navarro RA. Yearly trends in elective shoulder arthroplasty, 2005-2013. Arthritis Care Res (Hoboken). 2017;69(10):1574–1581. doi: 10.1002/acr.23167. [DOI] [PubMed] [Google Scholar]
- 3.Best MJ, Aziz KT, Wilckens JH, McFarland EG, Srikumaran U. Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2021;30(5):1159–1166. doi: 10.1016/j.jse.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Gowd AK, Agarwalla A, Beck EC, Rosas S, Waterman BR, Romeo AA, Liu JN. Prediction of total healthcare cost following total shoulder arthroplasty utilizing machine learning. J Shoulder Elbow Surg. 2022;31(12):2449–2456. doi: 10.1016/j.jse.2022.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Werner BC, Bustos FP, Gean RP, Deasey MJ. Emergency department visits in the year prior to total shoulder arthroplasty as a risk factor for postoperative emergency department visits. HSS J. 2021;17(2):200–206. doi: 10.1177/1556331621995775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walters JD, Walsh RN, Smith RA, Brolin TJ, Azar FM, Throckmorton TW. Bundled payment plans are associated with notable cost savings for ambulatory outpatient total shoulder arthroplasty. J Am Acad Orthop Surg. 2020;28(19):795–801. doi: 10.5435/JAAOS-D-19-00441. [DOI] [PubMed] [Google Scholar]
- 7.Pezzulo JD, Farronato DM, Rondon AJ, Sherman MB, Getz CL, Davis DE. Predicting hospital readmissions after total shoulder arthroplasty within a bundled payment cohort. J Am Acad Orthop Surg. 2023;31(4):199–204. doi: 10.5435/JAAOS-D-22-00449. [DOI] [PubMed] [Google Scholar]
- 8.Bosco JA, Harty JH, Iorio R. Bundled Payment Arrangements: Keys to Success. J Am Acad Orthop Surg. 2018;26(23):817–822. doi: 10.5435/JAAOS-D-17-00022. [DOI] [PubMed] [Google Scholar]
- 9.Cvetanovich GL, Bohl DD, Frank RM, Verma NN, Cole BJ, Nicholson GP, Romeo AA. Reasons for readmission following primary total shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 2018;47:7. doi: 10.12788/ajo.2018.0053. [DOI] [PubMed] [Google Scholar]
- 10.Chung AS, Makovicka JL, Hydrick T, Scott KL, Arvind V, Hattrup SJ. Analysis of 90-day readmissions after total shoulder arthroplasty. Orthop J Sports Med. 2019;7(9):2325967119868964. doi: 10.1177/2325967119868964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott KL, Chung AS, Makovicka JL, Pena AJ, Arvind V, Hattrup SJ. Ninety-day readmissions following reverse total shoulder arthroplasty. JSES Open Access. 2019;3(1):54–58. doi: 10.1016/j.jses.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holzgrefe RE, Wilson JM, Staley CA, Anderson TL, Wagner ER, Gottschalk MB. Modified frailty index is an effective risk-stratification tool for patients undergoing total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(7):1232–1240. doi: 10.1016/j.jse.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Traven SA, McGurk KM, Reeves RA, Walton ZJ, Woolf SK, Slone HS. Modified frailty index predicts medical complications, length of stay, readmission, and mortality following total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(10):1854–1860. doi: 10.1016/j.jse.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Xu S, Baker DK, Woods JC, Brabston EW 3rd, Ponce BA. Risk factors for early readmission after anatomical or reverse total shoulder arthroplasty. Am J Orthop (Belle Mead NJ). 2016;45(6):E386–E392. [PubMed] [Google Scholar]
- 15.Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl J Med. 2018;378: 2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.About the Neighborhood Atlas®.University of Wisconsin School of Medicine Public Health. Area Deprivation Index Datasets. [Accessed December 15, 2023]. Available at: https://www.neighborhoodatlas.medicine.wisc.edu/
- 17.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol . 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 18.Chowdhury MZI, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. FAM Med Community Health. 2020;8(1):e000262 . doi: 10.1136/fmch-2019-000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Young GP, Wagner MB, Kellermann AL, Ellis J, Bouley D. Ambulatory visits to hospital emergency departments Patterns and reasons for use 24 Hours in the ED Study Group. JAMA. 1996;276(6):460–465. doi: 10.1001/jama.276.6.460. [DOI] [PubMed] [Google Scholar]
- 20.Vinton DT, Capp R, Rooks SP, Abbott JT, Ginde AA. Frequent users of US emergency departments: characteristics and opportunities for intervention. Emerg Med J. 2014;31(7):526–532. doi: 10.1136/emermed-2013-202407. [DOI] [PubMed] [Google Scholar]
- 21.Kuhlmann NA, Franovic S, Burdick GB, et al. Shoulder arthroplasty outcomes in patients with major depressive disorder or generalized anxiety disorder. Seminars in Arthroplasty: JSES. 2023;33(4):722–726. [Google Scholar]
- 22.Lu Y, Oeding JF, Parkes C, Patel H, Berlinberg E, Forsythe B, Camp CL, Sanchez-Sotelo J. Incidence and 30- and 90-day readmission rates after primary shoulder arthroplasty in the United States: an analysis using the National Readmissions Database. J Shoulder Elbow Surg. 2023;32(6):1174–1184. doi: 10.1016/j.jse.2022.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Malik AT, Morris J, Bishop JY, Neviaser AS, Khan SN, Cvetanovich GL. Undergoing an arthroscopic procedure prior to shoulder arthroplasty is associated with greater risk of prosthetic joint infection. Arthroscopy. 2021;37(6):1748–1754. doi: 10.1016/j.arthro.2021.01.013. [DOI] [PubMed] [Google Scholar]


