Abstract
Background:
Arthrodesis of the first metatarsophalangeal joint is an effective treatment of advanced hallux rigidus. Numerous options have been described for performing this intervention. The aim of this study was to evaluate the outcomes following a consistent surgical technique of joint preparation with hand tools and fixation with 2 crossed screws and a dorsal compression plate.
Methods:
Thirteen patients (16 feet) who underwent primary isolated arthrodesis of the first metatarsophalangeal joint between March 2019 and June 2021 were available for clinical, radiologic, and pedobarographic evaluation at a minimum of 12 months after surgery. American Orthopaedic Foot & Ankle Society scores, numerical pain rating scale, the radiologic hallux valgus and intermetatarsal 1-2 angles as well as the distribution of plantar pressure during gait were compared between the pre- and postoperative conditions.
Results:
After an average follow-up period of 26 months, union was achieved in all cases and the mean AOFAS score raised significantly by 39 points. All the patients were satisfied with the result. Only 1 patient complained of mild residual pain at walk. Hardware removal was performed in 2 cases. The mean hallux valgus angle dropped from 12.3 to 6.3 degrees. The mean postoperative dorsiflexion angle was 21.6 degrees. After the procedure, peak pressure was significantly higher beneath the first metatarsal head and heel, whereas pressure-time integral was significantly lower beneath the hallux and medial lesser toes.
Conclusion:
Arthrodesis of the first metatarsophalangeal joint with 2 crossed screws and a dorsal compression plate is a safe and effective treatment of advanced hallux rigidus. This procedure provides adequate pain relief and functional improvement of gait.
Level of Evidence:
Level IV, therapeutic, retrospective case series.
Keywords: dorsiflexion angle, dynamic pedobarography, fusion, gait, osteoarthritis of the first metatarsophalangeal joint
Introduction
First metatarsophalangeal (MTP) joint arthrodesis is a reliable surgical treatment for pain and functional disability caused by various disorders of the first ray. Indications include end-stage MTP osteoarthritis, selected cases of hallux valgus, inflammatory arthritis, and failed first MTP joint surgery.8,10,23,47,50 The procedure is commonly performed in patients with advanced hallux rigidus. 22 In such cases, arthrodesis is supposed to provide more effective pain relief when compared to several motion-preserving alternatives.14,37,43 Satisfactory outcomes have been reported with various surgical techniques to achieve first MTP fusion.8,10,17,18,20,23,38,47,50 Options essentially concern the surgical approach, joint preparation, and the fixation method. Controversy remains on the optimal strategy to provide the best possible outcomes. According to the general consensus, a stable fixation in proper alignment is of paramount importance. Practically, the choice of the appropriate surgical method depends mainly on the surgeon’s individual experience and the availability of material and instrumentation.
The aim of this study was to assess the outcomes following isolated first MTP joint arthrodesis when the preparation of the surfaces is performed with hand tools and the fixation is achieved with 2 crossed screws and a dorsal compression plate. In addition, we measured the effect of the procedure on the distribution of load over the sole of the foot during gait by means of dynamic pedobarography.
Patients and Methods
Patients
We reviewed our medical database to identify all the patients who underwent primary arthrodesis of the first MTP joint at our institution. Between March 2019 and June 2021, 35 such procedures were performed by the senior author, always using the same surgical technique and fixation material. All patients underwent clinical, radiologic, and pedobarographic evaluation prior to the surgery. The operative indication was intractable pain and severe stiffness (mobility of less than 30 degrees) of the first MTP joint associated with radiologic evidence of severe MTP osteoarthritis (grade 3 or 4 according to the Coughlin and Shurnas’s classification of hallux rigidus). 13 Concomitant foot pathologies were treated simultaneously with additional procedures at the time of surgery in 12 cases, which were excluded from the study. Three patients were lost to follow-up and 1 patient moved abroad. One patient was excluded because of recent ipsilateral tibial osteotomy at the time of follow-up. Thus, 13 patients (16 feet) were available for clinical, radiologic, and pedobarographic assessment at a minimum of 12 months after surgery. The procedure was performed simultaneously on both sides in 3 patients. The mean age at the time of surgery was 54.9 (range, 38-72) years. No patient had prior ipsilateral foot surgery. Participants gave written informed consent, and institutional review board approval was obtained according to the Declaration of Helsinki (Cantonal Commission for Ethics in Research on Human Beings: CER-VD, BASEC ref. no. 2023-00286). Patient demographics are listed in Table 1.
Table 1.
Patient Demographics.
| Case | Age | Gender | Side | History |
|---|---|---|---|---|
| 1 | 51 | Female | Right | |
| 2 | 41 | Female | Right | |
| 3 | 45 | Female | Right | |
| 4 | Left | |||
| 5 | 53 | Male | Right | |
| 6 | 72 | Male | Right | |
| 7 | 48 | Male | Right | |
| 8 | Left | |||
| 9 | 38 | Male | Left | Hallux P1 fracture |
| 10 | 67 | Female | Right | Parkinson, left first MTP joint arthrodesis |
| 11 | 65 | Male | Left | |
| 12 | 50 | Female | Right | |
| 13 | 57 | Male | Right | Bilateral tibial osteotomy |
| 14 | Left | |||
| 15 | 63 | Male | Right | Bilateral total knee replacement |
| 16 | 65 | Female | Left | Right first MTP joint arthrodesis |
Abbreviation: MTP, metatarsophalangeal; P1, proximal phalanx.
Surgical Technique
The patients were operated in the supine position under general or spinal anesthesia. Antibiotic prophylaxis was administered prior to the exsanguination of the limb and a tourniquet was applied to the thigh. A 5-cm medial longitudinal incision was centered over the first MTP joint, and a medial longitudinal capsulotomy was performed in line with the skin incision. Subperiosteal dissection was carried out to allow complete exposure of the metatarsal head and base of the proximal phalanx, preserving the plantar attachment of the capsule. Osteophytes were resected and the joint surfaces were carefully prepared by hand, using bone chisel, curette, and rongeur. Preparation was achieved deep to the subchondral zone. Multiple 1.5- or 1.8-mm drills were then made through both surfaces to enhance vitality at the site of fusion. The position of fixation in the sagittal plane was assessed clinically, simulating the loadbearing condition with a flat plate applied on the plantar aspect of the foot. The transverse position of the hallux in slight valgus was adapted in relation to the second toe. The first metatarsal and the proximal phalanx of the hallux were fixed using 2 crossed 2.7-mm screws (CompactFoot, Johnson & Johnson, New Brunswick, NJ). The osteosynthesis was stabilized with a manually contoured 2.4-mm 4- or 6-hole titanium plate (CompactFoot) fixed dorsally in compression mode. Proper positioning of arthrodesis and material was confirmed with fluoroscopy. The medial protuberance of the first metatarsal head was resected using a powered saw. Capsule closure and subcutaneous adaptation were obtained with single monofilament stitches. The skin was closed with a continuous suture and an elastic bandage was applied. From the first postoperative day, patients were allowed to walk with protected full weightbearing, using a stiff sole shoe (Darco, Huntington, WV) for 6 weeks.
Clinical Evaluation
All patients underwent a detailed interview and physical examination of the foot before and after the surgery. Routine follow-up visits were planned approximately 6 weeks, 3 months, and 1 year after the operation to assess the functional recovery and detect any potential complication related to the procedure. To quantify the clinical outcome, we used the American Orthopaedic Foot & Ankle Society hallux metatarsal-interphalangeal (AOFAS-HMI) score. 29 As arthrodesis suppresses motion of the MTP joint, the maximum score was 90 points. Pain intensity was also reported on a numeric rating scale (NRS) from 0 (no pain) to 10 (worst pain ever experienced). 46 In addition, patients were asked to express their overall level of satisfaction (excellent, good, fair, or poor) and to score their appreciation of the aesthetic result, from 0 to 10 (10 describing a “perfectly normal appearance of the foot”).
Radiologic Evaluation
Anteroposterior and lateral weightbearing radiographs of the foot were routinely taken prior to surgery, at the first postoperative day and at 6 weeks and 12 months after surgery. Hallux valgus angle (HVA) and intermetatarsal 1-2 angle (IMA) were measured on the most recent preoperative and final postoperative radiographs. 12 Radiologic union was defined by the presence of at least 3 cortices bridging the focus of arthrodesis, and by the evidence of crossing trabeculae on both views. The dorsiflexion angle (DFA) was measured as described by Coughlin on the lateral radiograph at final follow-up. 11
Pedobarographic Evaluation
Dynamic pedobarographic exams were performed prior to surgery and at final follow-up, using the Wintrack system (Medicapteurs, Balma, France). This device consists of a 652 × 1610-mm walking platform that includes 12 288 resistive sensors. The data collected from the platform with a sampling rate of up to 200 Hz are processed by the Wintrack software to record podometric and space-time parameters of gait. Patients were asked to walk barefoot over the platform at a self-selected speed. The 2-step method was applied as described by Bryant et al. 7 At least 3 trials were done per exam to ensure a reproducible sequence of 3 recorded steps for each trial. 40 To assess the distribution of the plantar pressure during gait, the numeric footprint was divided into 12 regions of interest, following the lines of Bessou. 21 For each zone, peak pressure (PP) and pressure-time integral (PTI) 35 were compared between the pre- and postoperative states.
Statistical Analysis
A priori power analysis based on the mean values and standard deviations of the AOFAS-HMI scores reported in previous studies3,6,8,19,20,25 was performed using G*Power software (version 3.1.9.6), aiming for a power of 80% and level of significance of 5%. Pre- and postoperative values of continuous variables were tested for normal distribution. Accordingly, the Wilcoxon signed rank test was used for statistical analysis of the pre- and postoperative AOFAS-HMI and pain NRS scores, whereas HVA values were analyzed using a unilateral Welch test and IMA values with a Student paired t test.
Similarly, the normally distributed pedobarographic parameters were analyzed using a Student paired t test, whereas the Wilcoxon rank sum test was used for nonnormally distributed data. Finally, Spearman and Pearson coefficients were calculated between various parameters to seek for correlations.
Results
Clinical Results
After an average follow-up period of 26 (range, 12-35) months, the mean AOFAS-HMI score increased significantly from 47.5 ± 13.8 (range, 28-65) points preoperatively to 86.5 ± 6.7 (range, 65-90) points postoperatively (P < .001), and the mean pain NRS score decreased from 6.73 ± 1.62 (range, 5-10) preoperatively to 0.41 ± 1.64 (range, 0-4) postoperatively (P < .001) (Table 2). All patients reported complete pain relief at rest. Only 1 patient complained of mild residual pain during walking. This patient underwent simultaneous bilateral surgery and had former bilateral tibial osteotomy. Complications were met in 3 cases. One patient had a postoperative wound dehiscence that underwent uneventful secondary healing. Two patients complained of disturbance from hardware that required removal 12 and 14 months after the primary procedure, respectively. One of these 2 patients developed a dorsal hyperkeratosis that was treated with surgical excision at the time of material withdrawal. At the time of final follow-up, all the patients were satisfied and would undergo the procedure again. Twelve patients reported on excellent result and 1 patient described a good result. The mean subjective aesthetic rating score of the operated foot was 8.8 (range, 5-10).
Table 2.
Clinical Scores.
| Case | Follow-up, mo |
AOFAS Score | Pain NRS Score | ||
|---|---|---|---|---|---|
| Preoperative | Follow-up | Preoperative | Follow-up | ||
| 1 | 35 | 60 | 87 | 5.5 | 0 |
| 2 | 35 | 39 | 90 | 7.7 | 0 |
| 3 | 33 | 62 | 85 | 5 | 0 |
| 4 | 33 | 62 | 85 | 5 | 0 |
| 5 | 33 | 65 | 90 | 7 | 0 |
| 6 | 28 | 60 | 90 | 5 | 0 |
| 7 | 28 | 47 | 90 | 5 | 0 |
| 8 | 28 | 47 | 90 | 5 | 0 |
| 9 | 28 | 47 | 90 | 8.5 | 0 |
| 10 | 27 | 34 | 85 | 7 | 0 |
| 11 | 26 | 62 | 90 | 8 | 0 |
| 12 | 20 | 25 | 90 | 10 | 0 |
| 13 | 20 | 28 | 65 | 8 | 4 |
| 14 | 20 | 34 | 77 | 8 | 2.5 |
| 15 | 15 | 33 | 90 | 8 | 0 |
| 16 | 12 | 55 | 90 | 5 | 0 |
| Mean | 26 | 47.5 | 86.5 | 6.7 | 0.4 |
| P | <.001 | <.001 | |||
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; NRS, numeric rating scale.
Radiologic Results
Fusion was achieved in all cases at final follow-up (Figure 1). The mean dorsiflexion angle was 21.6 ± 2.7 (range, 15.9-26.9) degrees. The mean HVA dropped significantly from 12.3 ± 5.6 (range, 2.9-20.7) degrees preoperatively to 6.3 ± 3.0 (range, 1.2-12.8) degrees postoperatively (P < .001). HVA was corrected after the procedure in all the 6 cases with preoperative HVA higher than 15 degrees. We also observed a nonsignificant reduction of the mean IMA (Table 3).
Figure 1.
(A) Anteroposterior and (B) lateral weightbearing radiographs 12 months after the procedure in a 65-year-old patient.
Table 3.
Radiographic Angles (Degrees). a
| Case | HVA | IMA | Final DFA | ||
|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||
| 1 | 9.9 | 9.0 | 8.9 | 7.5 | 24.0 |
| 2 | 19.4 | 10 | 8.8 | 6.5 | 19.7 |
| 3 | NA | 5.5 | NA | 7.4 | 24.6 |
| 4 | NA | 3.1 | NA | 7.4 | 22.5 |
| 5 | 20.7 | 9.9 | 8.7 | 10.1 | 24.2 |
| 6 | 15.5 | 4.1 | 8.5 | 8.2 | 21.1 |
| 7 | 9.3 | 6.7 | 9.9 | 9.4 | 20.5 |
| 8 | 5.9 | 3.4 | 5.8 | 7.3 | 19.5 |
| 9 | 2.9 | 3.2 | 6.2 | 3.6 | 15.9 |
| 10 | 9.0 | 1.2 | 10.1 | 7.7 | 20.6 |
| 11 | 17.3 | 12.8 | 10.6 | 12.4 | 20.5 |
| 12 | 17.8 | 5.5 | 10.6 | 9.5 | 26.9 |
| 13 | 12.3 | 7.8 | 9.7 | 9.9 | 24.5 |
| 14 | 8.4 | 5.1 | 9.5 | 11.6 | 20.4 |
| 15 | 7.1 | 7.1 | 11.7 | 10.4 | 20.0 |
| 16 | 16.9 | 6.4 | 12.4 | 10.9 | 20.0 |
| Mean | 12.3 | 6.3 | 9.4 | 8.7 | 21.6 |
Abbreviations: DFA, dorsiflexion angle; HVA, Hallux valgus angle; IMA, intermetatarsal angle.
P < .001.
Pedobarographic Results
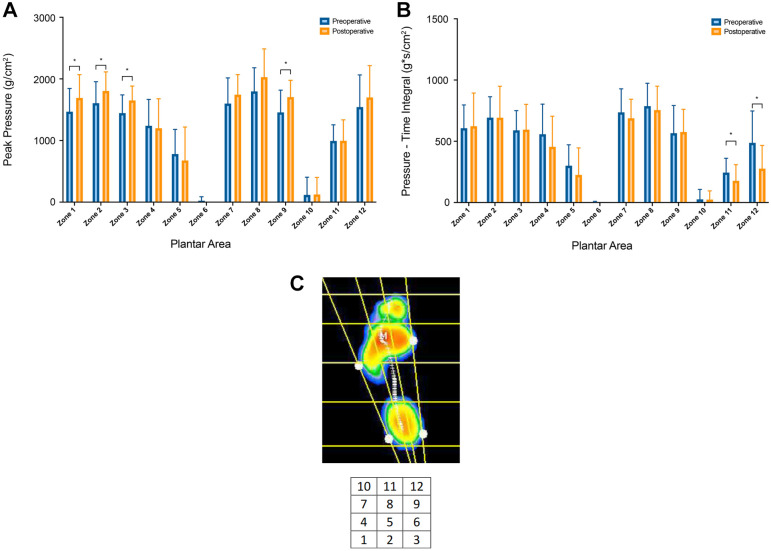
After the procedure, PP was significantly higher under the head of the first metatarsal (P = .013) and heel (from medial to lateral: P = .008, .015, and .014, respectively), as shown in Figure 2. PTI was significantly lower under the hallux (P = .002) and medial lesser toes (P = .012). There was a negative correlation between DFA and PTI over the lateral side of the heel (r = −0.68, P = .004).
Figure 2.
Comparison of (A) peak pressure and (B) pressure-time integral between the pre- and postoperative conditions for the 12 plantar zones of interest. Significant differences are indicated with *. (C) Location of the 12 zones of interest over the footprint.
Discussion
In this study, we observed successful outcomes of first-MTP joint arthrodesis in terms of functional improvement and pain relief, as shown by the significant shift of the mean AOFAS-HMI and pain NRS scores. Clinical and radiologic union was achieved in all cases without major complication. However, reoperation was required in 2 patients because of symptomatic prominence of hardware. The operative risk and cost involved in this additional procedure should not be ignored.
Preparation, alignment, and stability are technical factors that may impact the outcomes following arthrodesis of the first MTP joint. 32 In this respect, our surgical technique is supported by previous clinical and experimental evidence. Adequate joint preparation must preserve vitality and limit shortening. Powered reamers are widely used to perform the preparation of the surfaces. 31 Instead, the use of curettes and rongeurs may improve the union rate. 30 We assume that this avoids unnecessary bone heating and additional damage to the soft tissues. According to Prat et al, 39 in situ preparation of the articular surfaces causes less shortening of the first ray when compared to flat cuts performed with a powered saw.
The position of fusion is a major issue during surgery. Persistent postoperative hallux valgus deformity carries a higher risk of nonunion. 50 Pronation must be avoided. Excessive or insufficient dorsiflexion can lead to footwear problems. In their series including 153 patients, Weber et al 49 found that higher DFAs were associated with a higher fusion rate. Coughlin et al 11 reported on increased prevalence of interphalangeal arthritis with a DFA of less than 20 degrees. Yet no association was found between the sagittal position of fusion and the clinical outcomes in other studies that addressed this question.1,26,36,47 Nor was it the case in our study. By contrast, a relationship between DFA and distribution of plantar load during gait is suggested by 2 studies. Using a cadaveric model, Bayomy et al 5 found that PP and PTI under the hallux and first metatarsal head were minimized with fixed DFA of 24.7 and 21.3 degrees respectively. In a cross-sectional study of 15 patients with fused first MTP joint, Alentorn-Geli et al 2 found a positive correlation between DFA and mean dynamic plantar pressure under the first metatarsal head. A more recent investigation found no association between the radiologic position of fusion and the plantar pressure under the hallux. 34 The position of dorsiflexion generally recommended in the literature ranges from 10 to 30 degrees.1,5,17,26,36 To determine the position of fusion in the sagittal plane during the procedure, we apply the widely reported and reproductible method of simulating the contact with the floor with the application of a flat surface against the sole of the foot. 45
The hardware and method of fixation may affect the fusion rate following first MTP joint arthrodesis. 9 There is strong evidence in favor of using a plate and screws to perform the procedure. Dorsal plating with compression screws is currently acknowledged as the most stable method of fixation. 4 According to a recent systematic review, plating techniques yield better overall results in terms of functional outcome and complication rate, although techniques with staples may achieve higher union rates. 28 Nonunion is not necessarily determinant of poor outcome, as several authors reported on variable rates of asymptomatic nonunions.8,17,38,41 Surgeons placing dorsal plates should consider that the type of plate and its relative position in the longitudinal axis of the dorsal side may affect the final DFA.16,33
The effect of first MTP fusion on the distribution of load over the foot during gait remains controversial. Previous investigations with dynamic pedobarography acknowledged that first MTP arthrodesis provides some restoration of the loadbearing role of the first ray during gait.8,14,24,48 However, this statement was challenged by Stevens et al. 44 In their study comparing patients with first MTP arthrodesis to healthy controls, they found higher PP beneath the lesser toes and lateral metatarsal heads in the arthrodesis group, whereas PTI was lower beneath the hallux and higher beneath the fourth metatarsal head. 44 They concluded to a load transfer from the first ray toward the lesser metatarsals. To our knowledge, our study was the first to compare the distribution of plantar pressure over the entire foot between the pre- and postoperative states in patients who underwent first MTP arthrodesis. Indeed, we found reduced cumulative load under the hallux during gait when the first MTP joint is fused. But concurrently after the procedure, the area of the first metatarsal head reached significantly higher values of pressure. This indicates an improved loadbearing capacity of the first ray in our patients.
The main limitations of our study are inherent to its retrospective nature and small sample size. However, our restrictive exclusion criterion allowed to evaluate the arthrodesis in isolation. Most clinical studies include several indications, patients with additional pathologies of lesser rays, and different methods of fixation. In our study, all patients were operated by the same surgeon with the same procedure. The AOFAS-HMI score may not be the optimal tool to measure the clinical outcome in patients with first MTP fusion; nevertheless, it has remained widely used in clinical studies until recent years, allowing a priori power analysis.3,6,8,15,19,20,23,25 -27,36,42,48,51
In conclusion, we found that first MTP joint arthrodesis performed with in situ preparation of the joint and fixation with 2 crossed screws and a dorsal compression plate is a safe and effective procedure for patients with severe hallux rigidus. However, the possible need for subsequent hardware removal must be considered with this technique. First MTP fusion may improve the loadbearing function of the first ray during gait in patients with severe hallux rigidus. Further prospective clinical investigations should use validated measurement tools to assess the functional outcome in patients undergoing first MTP joint arthrodesis.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114241265344 for Primary Isolated Arthrodesis of the First Metatarsophalangeal Joint for Hallux Rigidus: Clinical, Radiologic, and Pedobarographic Evaluation by Nicolas Fragnière, Maeva Kameni-Hekam, Amadou Cissé and Patrick Vienne in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: Ethical approval for this study was obtained from our institutional review board: Commission d’éthique cantonale de la recherche sur l’être humain (CER-VD, Switzerland), approval number ID: BASEC 2023-00286.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Disclosure forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Nicolas Fragnière,  https://orcid.org/0009-0006-5831-0126
https://orcid.org/0009-0006-5831-0126
Amadou Cissé,  https://orcid.org/0000-0001-6239-236X
https://orcid.org/0000-0001-6239-236X
Supplemental Material: Supplementary material is available online with this article.
References
- 1. Aas M, Johnsen TM, Finsen V. Arthrodesis of the first metatarsophalangeal joint for hallux rigidus—optimal position of fusion. Foot (Edinb). 2008;18(3):131-135. doi: 10.1016/j.foot.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 2. Alentorn-Geli E, Gil S, Bascuas I, et al. Correlation of dorsiflexion angle and plantar pressure following arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int. 2013;34(4):504-511. doi: 10.1177/1071100713477386 [DOI] [PubMed] [Google Scholar]
- 3. Ballas R, Edouard P, Philippot R, Farizon F, Delangle F, Peyrot N. Ground-reactive forces after hallux valgus surgery: comparison of scarf osteotomy and arthrodesis of the first metatarsophalangeal joint. Bone Joint J. 2016;98-B(5):641-646. doi: 10.1302/0301-620X.98B5.36406 [DOI] [PubMed] [Google Scholar]
- 4. Balu AR, Baumann AN, Tsang T, et al. Evaluating the biomechanical integrity of various constructs utilized for first metatarsophalangeal joint arthrodesis: a systematic review. Materials (Basel). 2023;16(19):6562. doi: 10.3390/ma16196562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bayomy AF, Aubin PM, Sangeorzan BJ, Ledoux WR. Arthrodesis of the first metatarsophalangeal joint: a robotic cadaver study of the dorsiflexion angle. J Bone Joint Surg Am. 2010;92(8):1754-1764. doi: 10.2106/JBJS.I.00984 [DOI] [PubMed] [Google Scholar]
- 6. Bei C, Gross CE, Adams S, Parekh SG. Dual plating with bone block arthrodesis of the first metatarsophalangeal joint: a clinical retrospective review. Foot Ankle Surg. 2015;21(4):235-239. doi: 10.1016/j.fas.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 7. Bryant AR, Tinley P, Singer KP. Normal values of plantar pressure measurements determined using the EMED-SF system. J Am Podiatr Med Assoc. 2000;90(6):295-299. doi: 10.7547/87507315-90-6-295 [DOI] [PubMed] [Google Scholar]
- 8. Chraim M, Bock P, Alrabai HM, Trnka HJ. Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int Orthop. 2016;40(11):2401-2408. doi: 10.1007/s00264-016-3277-1 [DOI] [PubMed] [Google Scholar]
- 9. Cichero MJ, Yates BJ, Joyce ASD, Williamson DM, Walsh TP. Different fixation constructs and the risk of non-union following first metatarsophalangeal joint arthrodesis. Foot Ankle Surg. 2021;27(7):789-792. doi: 10.1016/j.fas.2020.10.006 [DOI] [PubMed] [Google Scholar]
- 10. Coughlin MJ. Rheumatoid forefoot reconstruction. A long-term follow-up study. J Bone Joint Surg Am. 2000;82(3):322-341. [PubMed] [Google Scholar]
- 11. Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26(10):783-792. doi: 10.1177/107110070502601001 [DOI] [PubMed] [Google Scholar]
- 12. Coughlin MJ, Saltzman CL, Nunley JA, 2nd. Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002;23(1):68-74. doi: 10.1177/107110070202300114 [DOI] [PubMed] [Google Scholar]
- 13. Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85(11):2072-2088. [PubMed] [Google Scholar]
- 14. de Bot RTAL, Veldman HD, Eurlings R, Stevens J, Hermus JPS, Witlox AM. Metallic hemiarthroplasty or arthrodesis of the first metatarsophalangeal joint as treatment for hallux rigidus: a systematic review and meta-analysis. Foot Ankle Surg. 2022;28(2):139-152. doi: 10.1016/j.fas.2021.03.004 [DOI] [PubMed] [Google Scholar]
- 15. DeFrino PF, Brodsky JW, Pollo FE, Crenshaw SJ, Beischer AD. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002;23(6):496-502. doi: 10.1177/107110070202300605 [DOI] [PubMed] [Google Scholar]
- 16. DeOrio JK. Technique tip: arthrodesis of the first metatarsophalangeal joint - prevention of excessive dorsiflexion. Foot Ankle Int. 2007;28(6):746-747. doi: 10.3113/FAI.2007.0746 [DOI] [PubMed] [Google Scholar]
- 17. Donegan RJ, Blume PA. Functional results and patient satisfaction of first metatarsophalangeal joint arthrodesis using dual crossed screw fixation. J Foot Ankle Surg. 2017;56(2):291-297. doi: 10.1053/j.jfas.2016.10.021 [DOI] [PubMed] [Google Scholar]
- 18. Fanous RN, Ridgers S, Sott AH. Minimally invasive arthrodesis of the first metatarsophalangeal joint for hallux rigidus. Foot Ankle Surg. 2014;20(3):170-173. doi: 10.1016/j.fas.2014.03.004 [DOI] [PubMed] [Google Scholar]
- 19. Fazal MA, Wong JH, Rahman L. First metatarsophalangeal joint arthrodesis with two orthogonal two hole plates. Acta Orthop Traumatol Turc. 2018;52(5):363-366. doi: 10.1016/j.aott.2018.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Filomeno P, Lopez J. First metatarsophalangeal joint arthrodesis: functional outcomes using 2 different fixation techniques. Is more expensive better? Foot Ankle Orthop. 2023;8(3):24730114231193424. doi: 10.1177/24730114231193424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gaillet JC, Biraud JC, Bessou M, Bessou P. Modifications of baropodograms after transcutaneous electric stimulation of the abductor hallucis muscle in humans standing erect. Clin Biomech (Bristol, Avon). 2004;19(10):1066-1069. doi: 10.1016/j.clinbiomech.2004.03.005 [DOI] [PubMed] [Google Scholar]
- 22. Galois L, Hemmer J, Ray V, Sirveaux F. Surgical options for hallux rigidus: state of the art and review of the literature. Eur J Orthop Surg Traumatol. 2020;30(1):57-65. doi: 10.1007/s00590-019-02528-x [DOI] [PubMed] [Google Scholar]
- 23. Garcia-Ortiz MT, Talavera-Gosalbez JJ, Moril-Peñalver L, Fernandez-Ruiz MD, Alonso-Montero C, Lizaur-Utrilla A. First metatarsophalangeal arthrodesis after failed distal chevron osteotomy for hallux valgus. Foot Ankle Int. 2021;42(4):425-430. doi: 10.1177/1071100720968831 [DOI] [PubMed] [Google Scholar]
- 24. Gibson JN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26(9):680-690. doi: 10.1177/107110070502600904 [DOI] [PubMed] [Google Scholar]
- 25. Gross CE, Bei C, Gay T, Parekh SG. A short-term retrospective of first metatarsophalangeal joint arthrodesis using a plate with pocketlock fixation. Foot Ankle Spec. 2015;8(6):466-471. doi: 10.1177/1938640015585968 [DOI] [PubMed] [Google Scholar]
- 26. Hoveidaei AH, Roshanshad A, Vosoughi AR. Clinical and radiological outcomes after arthrodesis of the first metatarsophalangeal joint. Int Orthop. 2021;45(3):711-719. doi: 10.1007/s00264-020-04807-3 [DOI] [PubMed] [Google Scholar]
- 27. Hunt KJ, Lakey E. Patient-reported outcomes in foot and ankle surgery. Orthop Clin North Am. 2018;49(2):277-289. doi: 10.1016/j.ocl.2017.11.014 [DOI] [PubMed] [Google Scholar]
- 28. Kang YS, Bridgen A. First metatarsophalangeal joint arthrodesis/fusion: a systematic review of modern fixation techniques. J Foot Ankle Res. 2022;15(1):30. doi: 10.1186/s13047-022-00540-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349-353. doi: 10.1177/107110079401500701 [DOI] [PubMed] [Google Scholar]
- 30. Korim MT, Mahadevan D, Ghosh A, Mangwani J. Effect of joint pathology, surface preparation and fixation methods on union frequency after first metatarsophalangeal joint arthrodesis: a systematic review of the English literature. Foot Ankle Surg. 2017;23(3):189-194. doi: 10.1016/j.fas.2016.05.317 [DOI] [PubMed] [Google Scholar]
- 31. Koutsouradis P, Savvidou OD, Stamatis ED. Arthrodesis of the first metatarsophalangeal joint: the “when and how.” World J Orthop. 2021;12(7):485-494. doi: 10.5312/wjo.v12.i7.485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Latif A, Dhinsa BS, Lau B, Abbasian A. First metatarsophalangeal fusion using joint specific dorsal plate with interfragmentary screw augmentation: clinical and radiological outcomes. Foot Ankle Surg. 2019;25(2):132-136. doi: 10.1016/j.fas.2017.09.005 [DOI] [PubMed] [Google Scholar]
- 33. Lewis JT, Hanselman AE, Lalli TA, Daigre JL, Santrock RD. Effect of dorsal plate positioning on dorsiflexion angle in arthrodesis of the first metatarsophalangeal joint: a cadaveric study. Foot Ankle Int. 2014;35(8):802-808. doi: 10.1177/1071100714534419 [DOI] [PubMed] [Google Scholar]
- 34. Matsumoto T, Takeda R, Kasai T, et al. Clinical outcomes after first metatarsophalangeal joint arthrodesis by flat cut joint preparation with individual adjustment for sagittal alignment. J Foot Ankle Surg. 2022;61(1):60-66. doi: 10.1053/j.jfas.2020.10.015 [DOI] [PubMed] [Google Scholar]
- 35. Melai T, IJzerman TH, Schaper NC, et al. Calculation of plantar pressure time integral, an alternative approach. Gait Posture. 2011;34(3):379-383. doi: 10.1016/j.gaitpost.2011.06.005 [DOI] [PubMed] [Google Scholar]
- 36. Paredes-Carnero X, Fernández-Cebrián AM, Villardefrancos-Gil S. Do postoperative hallux angles correlate with outcome in MP1 fusion? Our experience with 71 cases. Foot Ankle Spec. Published online January 1, 2018. doi: 10.1177/1938640017751186 [DOI] [PubMed] [Google Scholar]
- 37. Park YH, Jung JH, Kang SH, Choi GW, Kim HJ. Implant arthroplasty versus arthrodesis for the treatment of advanced hallux rigidus: a meta-analysis of comparative studies. J Foot Ankle Surg. 2019;58(1):137-143. doi: 10.1053/j.jfas.2018.08.045 [DOI] [PubMed] [Google Scholar]
- 38. Patel S, Garg P, Fazal MA, Ray PS. First metatarsophalangeal joint arthrodesis using an intraosseous post and lag screw with immediate bearing of weight. J Foot Ankle Surg. 2019;58(6):1091-1094. doi: 10.1053/j.jfas.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 39. Prat D, Sourugeon Y, Haghverdian BA, et al. “In Situ” joint preparation technique for first metatarsophalangeal arthrodesis: a retrospective comparative review of 388 cases. J Foot Ankle Surg. 2023;62(5):855-861. doi: 10.1053/j.jfas.2023.05.004 [DOI] [PubMed] [Google Scholar]
- 40. Ramachandra P, Maiya AG, Kumar P. Test-retest reliability of the Win-Track platform in analyzing the gait parameters and plantar pressures during barefoot walking in healthy adults. Foot Ankle Spec. 2012;5(5):306-312. doi: 10.1177/1938640012457680 [DOI] [PubMed] [Google Scholar]
- 41. Roukis TS. Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. J Foot Ankle Surg. 2011;50(6):710-713. doi: 10.1053/j.jfas.2011.06.012 [DOI] [PubMed] [Google Scholar]
- 42. Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. A systematic review of the outcome evaluation tools for the foot and ankle. Foot Ankle Spec. 2019;12(5):461-470. doi: 10.1177/1938640018803747 [DOI] [PubMed] [Google Scholar]
- 43. Stevens J, de Bot RTAL, Hermus JPS, van Rhijn LW, Witlox AM. Clinical outcome following total joint replacement and arthrodesis for hallux rigidus: a systematic review. JBJS Rev. 2017;5(11):e2. doi: 10.2106/JBJS.RVW.17.00032 [DOI] [PubMed] [Google Scholar]
- 44. Stevens J, Meijer K, Bijnens W, et al. Gait analysis of foot compensation after arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int. 2017;38(2):181-191. doi: 10.1177/1071100716674310 [DOI] [PubMed] [Google Scholar]
- 45. Strony JT, Rascoe AS, Marcus RE. Validation of the artificial floor technique in first metatarsophalangeal joint arthrodesis. Clin Orthop Relat Res. 2022;480(10):2002-2009. doi: 10.1097/CORR.0000000000002248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18(1):99-107. doi: 10.1515/sjpain-2018-0012 [DOI] [PubMed] [Google Scholar]
- 47. van Doeselaar DJ, Heesterbeek PJ, Louwerens JW, Swierstra BA. Foot function after fusion of the first metatarsophalangeal joint. Foot Ankle Int. 2010;31(8):670-675. doi: 10.3113/FAI.2010.0670 [DOI] [PubMed] [Google Scholar]
- 48. Vienne P, Sukthankar A, Favre P, Werner CM, Baumer A, Zingg PO. Metatarsophalangeal joint arthrodesis after failed Keller-Brandes procedure. Foot Ankle Int. 2006;27(11):894-901. doi: 10.1177/107110070602701105 [DOI] [PubMed] [Google Scholar]
- 49. Weber C, Yao D, Schwarze M, et al. Risk analysis of nonunion after first metatarsophalangeal joint arthrodesis. Foot Ankle Spec. 2021;14(2):120-125. doi: 10.1177/1938640019899829 [DOI] [PubMed] [Google Scholar]
- 50. Weigelt L, Redfern J, Heyes GJ, Butcher C, Molloy A, Mason L. Risk factors for nonunion after first metatarsophalangeal joint arthrodesis with a dorsal locking plate and compression screw construct: correction of hallux valgus is key. J Foot Ankle Surg. 2021;60(6):1179-1183. doi: 10.1053/j.jfas.2020.12.007 [DOI] [PubMed] [Google Scholar]
- 51. Wood EV, Walker CR, Hennessy MS. First metatarsophalangeal arthrodesis for hallux valgus. Foot Ankle Clin. 2014;19(2):245-258. doi: 10.1016/j.fcl.2014.02.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114241265344 for Primary Isolated Arthrodesis of the First Metatarsophalangeal Joint for Hallux Rigidus: Clinical, Radiologic, and Pedobarographic Evaluation by Nicolas Fragnière, Maeva Kameni-Hekam, Amadou Cissé and Patrick Vienne in Foot & Ankle Orthopaedics