Abstract
Objective:
Increasingly, states authorize pharmacists to prescribe hormonal contraception to patients without a prescription from another healthcare provider. The purpose of this review is to investigate pharmacist and patient perspectives on pharmacist-prescribed contraception in the United States.
Study design:
We searched Medline, Embase, PsycInfo, CINAHL, Scopus, and the Cochrane Library from inception through July 10, 2019. We included qualitative and mixed-methods studies, quantitative surveys, observational studies, and randomized trials in the United States. Risk of bias was assessed using tools for quantitative and qualitative studies.
Results:
Fifteen studies met inclusion criteria, including studies on pharmacists and student pharmacists (n = 9), patients (n = 5), and both (n = 1). Study samples ranged from local to national. Studies had moderate to high risk of bias, primarily due to low response rates and lack of validated instruments. Most pharmacists (57–96%) across four studies were interested in participating in pharmacist-prescribed contraception services. Among patients, 63–97% across three studies supported pharmacist-prescribed contraception, and 38–68% across four studies intended to participate in these services. At least half of pharmacists across four studies felt comfortable prescribing contraception, though pharmacists identified additional training needs. Pharmacists and patients identified several reasons for interest in pharmacist-prescribed contraception services, including increasing patient access, reducing unintended pregnancies, and offering professional development for pharmacists. They also identified barriers, including payment, time and resource constraints, liability, and patient health concerns.
Conclusions:
Most pharmacists and patients across 15 studies were interested in expanded access to contraception through pharmacist-prescribed contraception. Findings on facilitators and barriers may inform implementation efforts.
Implications:
Pharmacist-prescribed contraception is a strategy to expand patient access to contraception. Reducing barriers to implementation could improve participation among pharmacists and patients.
Keywords: Contraception, Pharmacy, Pharmacy access, Pharmacist-prescription, Systematic review
1. Introduction
Pharmacist-prescribed contraception laws and policies allow pharmacists to prescribe hormonal contraception (HC) to eligible patients. Pharmacists can safely prescribe contraception with appropriate screening for contraindications, and HC is generally safe for most women [1,2]. These laws and policies aim to improve access to contraception, as nearly 30% of US women have experienced difficulties obtaining, filling, or refilling a prescription [3,4]. Barriers include cost of a clinic appointment, lack of insurance, and challenges scheduling or attending an appointment [3,4].
In 2003, researchers demonstrated the success of pharmacist-prescribed contraception models in Washington through broad collaborative drug therapy agreements in place since 1979 [3]. In 2016, Oregon became the first state to implement legislation specific to pharmacist-prescribed contraception [5]. As of July 2020, 12 states and the District of Columbia (DC) have legislation specific to HC that authorizes pharmacist prescribing. Where HC-specific laws exist, pharmacist-prescribed contraception may occur through prescriptive authority under statewide protocols or collaborative practice agreements (CPAs) (Table 1) [6–11]. Statewide protocols allow pharmacists to prescribe medications under criteria defined by a state body, such as a Board of Pharmacy [12]. CPAs allow medication prescribing through a more formal arrangement, in which pharmacists partner with physicians or other authorized prescribers who broadly oversee their prescriptive authority [12]. Eleven states and DC allow pharmacist-prescribed contraception through statewide protocols, and one state through an HCspecific CPA (Tennessee) [6–11]. Two additional states have a broad CPA (Washington) or restricted prescriptive authority for pharmacists (Idaho) that allow for pharmacist-prescribed contraception, though contraception is not specified in their authorities [6–8,11].
Table 1.
States permitting pharmacist-prescribed contraception.a
| State | Year authority in effect | Prescriptive authority | Methods | Ages |
|---|---|---|---|---|
|
| ||||
| Washington | 1979 | * | No restrictions specified | No restrictions specified |
| California | 2016 | SP | Pill, patch, ring, injectable | All |
| Oregon | 2016 | SP | Pill, patch, ring, injectable | All |
| Colorado | 2017 | SP | Pill, patch | 18+ |
| Hawaii | 2017 (signed) | SP | Pill, patch, ring, injectable | All |
| New Mexico | 2017 | SP | Pill, patch, ring, injectable | All |
| Tennessee | 2018 | CPA | Pill, patch | 18+, or emancipated minors |
| Utah | 2018 | SP | Pill, patch, ring | 18+ |
| Idaho | 2019 | * | No restrictions specified | No restrictions specified |
| Maryland | 2019 | SP | Pill, patch, ring, injectable | All |
| New Hampshire | 2019 | SP | Pill, patch, ring | All |
| Washington, D.C. | 2019 | SP | Pill, patch, ring | All |
| West Virginia | 2019 | SP | Pill, patch, ring, injectable | 18+ |
| Minnesota | 2020 | SP | Pill, patch, ring | 18+, or <18 with a previous prescription from a non-pharmacist provider |
| Virginia | 2020 | SP | Pill, patch, ring, injectable | 18+ |
SP = Statewide Protocol.
CPA = Collaborative Practice Agreement.
These states do not have legislation specific to hormonal contraception (HC), but allow pharmacist-prescribed HC through a broad CPA (Washington) or restricted prescriptive authority for pharmacists (Idaho).
Tak CR, Kessler LT, Scott MA, Gunning KM. Pharmacist-prescribed hormonal contraception: a review of the current landscape. J Am Pharm Assoc 2019;59:633–41. Beal JL, Illingworth Plake KS. Social and legislative shaping of access to contraceptives and the pharmacist’s role: a literature review. Res Social Adm Pharm 2019. Rafie S, Landau S. Opening new doors to birth control: state efforts to expand access to contraception in community pharmacies. Birth Control Pharmacist. Available at https://birthcontrol-pharmacist.com/; 2019 [accessed 8 Jan 2020]. National Alliance of State Pharmacy Associations. Pharmacist prescribing: hormonal contraceptives. Available at https://naspa.us/resource/contraceptives/; 2020 [accessed 10 Sept 2020]. Association of State and Territorial Health Officials. States authorize pharmacists to prescribe and dispense contraceptives. Available at: https://www.astho.org/StatePublicHealth/States-Authorize-Pharmacists-to-Prescribe-Dispense-Contraceptives/06–06-19/; 2019 [accessed 8 Jan 2020]. Kooner M, Joseph H, Griffin B, Lynch S, Vest K, Stewart-Lynch A, et al. Hormonal contraception prescribing by pharmacists: 2019 update. J Am Pharm Assoc 2020;1544–3191.
In most of these states, pharmacists are required to complete a board-approved or pharmacy school-based training to participate [6,11]. Before prescribing contraception, pharmacists must provide a risk assessment screening to patients and measure their blood pressure to determine medical eligibility [6]. All states authorize pharmacists to prescribe the pill and patch; others also authorize the ring and injectables. Some states authorize pharmacist-prescription for only patients ages 18 years and older; others have no specified age or product limitations (Table 1) [6–11].
Early research suggests that pharmacist and patient participation in pharmacist-prescribed contraception services so far is relatively low [13–15]. For these services to improve access to contraception, both pharmacists and patients must be interested in participating, and barriers to participation must be minimized. The purpose of this systematic review is to understand pharmacist and patient perspectives on pharmacist-prescribed contraception in the United States. The results may help inform implementation of these laws and policies to improve access to contraception.
2. Methods
We report this systematic review according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [16]. The protocol for the review was published on the PROSPERO database in April 2019 (Registration Number: CRD42019130051) [17].
2.1. Search strategy and eligibility criteria
We searched Medline, Embase, PsycInfo, CINAHL, Scopus, and the Cochrane Library from database inception through July 10, 2019. We also searched references of relevant articles and protocols published on PROSPERO. We contacted authors of conference abstracts published online to identify additional published studies of interest. Only articles written in English were included, as the research intervention focused on the United States. Search strategies were developed in collaboration with a reference librarian (Table A.1).
We included primary reports of qualitative and mixed-methods studies, quantitative surveys, observational studies, and randomized trials. Conference abstracts, case reports and series, editorials, letters, and nonpublished results were excluded. We included only studies conducted in the United States. Studies were included from any US locality and state, encompassing those with and without implemented pharmacist-prescribed contraception.
We searched for studies that assessed pharmacist or patient perspectives on pharmacist-prescribed contraception. The pharmacist population included practicing pharmacists, student pharmacists, and pharmacy managers in the United States. The patient population included adult and adolescent women in the United States. The interventions of interest were policies and laws, including statewide protocols and CPAs, on pharmacist-prescribed contraception in the United States. We excluded studies exclusively on levonorgestrel emergency contraceptive pills, which have been FDA-approved for over-the-counter sale since 2013.
The outcomes for pharmacists and patients were: (1) interest in, (2) motivators for, (3) comfort with, and (4) barriers to pharmacist-prescribed contraception. “Interest” included outcomes related to support for and intention to participate in pharmacist-prescribed contraception services. “Motivators” included motivators for participating in and perceived benefits of pharmacist-prescribed contraception. “Comfort” for the pharmacist population included comfort, confidence, and training needs around pharmacist-prescribed contraception; “comfort” for the patient population included comfort and satisfaction with pharmacist-prescribed contraception. “Barriers” included barriers to participation and implementation.
2.2. Quality assessment
To assess the quality of the evidence, we considered risk of bias and generalizability. We used two risk of bias tools, one for quantitative and one for qualitative studies. For quantitative cross-sectional surveys, we used a modified version of the Clarity/McMaster “Risk of bias instrument for cross-sectional surveys of attitudes and practices” [18]. For quantitative longitudinal surveys, we also considered follow-up rates. For qualitative studies, we created a tool based on the Critical Appraisal Skills Programme (CASP) for qualitative research and the Mildred Blaxter “Criteria for the evaluation of qualitative research papers” [19,20]. For all study designs, we assessed selection bias (e.g. source of the sample, response rate, and assessment of differences between responders and non-responders), information bias (e.g. reliability and validity of data collection instruments and missing data), and appropriateness of analytic technique. Each risk of bias domain was scored low, medium, or high. Generalizability to the target population was assessed as good, fair, or poor.
2.3. Data synthesis
Abstract and full-text screening were completed by two authors (LE and AT), and disagreements were resolved by KC, using Covidence [21]. LE independently extracted data from each eligible study into prespecified evidence tables for pharmacist and patient perspectives. AT or KC reviewed each article in the evidence tables. Quality was assessed independently by two authors (LE and AT or KC), and disagreements were resolved by a third reviewer (AT or KC).
Results were summarized narratively and in evidence tables. Meta-analysis was not performed due to heterogeneity of the types of studies and outcomes.
The literature on this topic uses different terms for “pharmacist-prescribed contraception”, such as “pharmacy access to contraception” or “pharmacist-provided contraception”. In this paper, we use “pharmacist-prescribed contraception” or terms used in individual studies, when describing their results.
3. Results
We screened 1212 abstracts identified by our database search, from which we assessed 121 full-text publications (Fig. 1). In the full-text review, 13 studies from 14 publications met eligibility criteria; all others were excluded, primarily because they were not primary studies or were unpublished conference abstracts. We identified two additional full texts through references of relevant articles [22,23]. In total, 15 studies reported in 16 publications met inclusion criteria [2,3,13,22–34]. Nine studies (from 10 publications) included only pharmacists [13,24–32], five included only patients [3,22,23,33,34], and one included both pharmacists and patients [2].
Fig. 1.
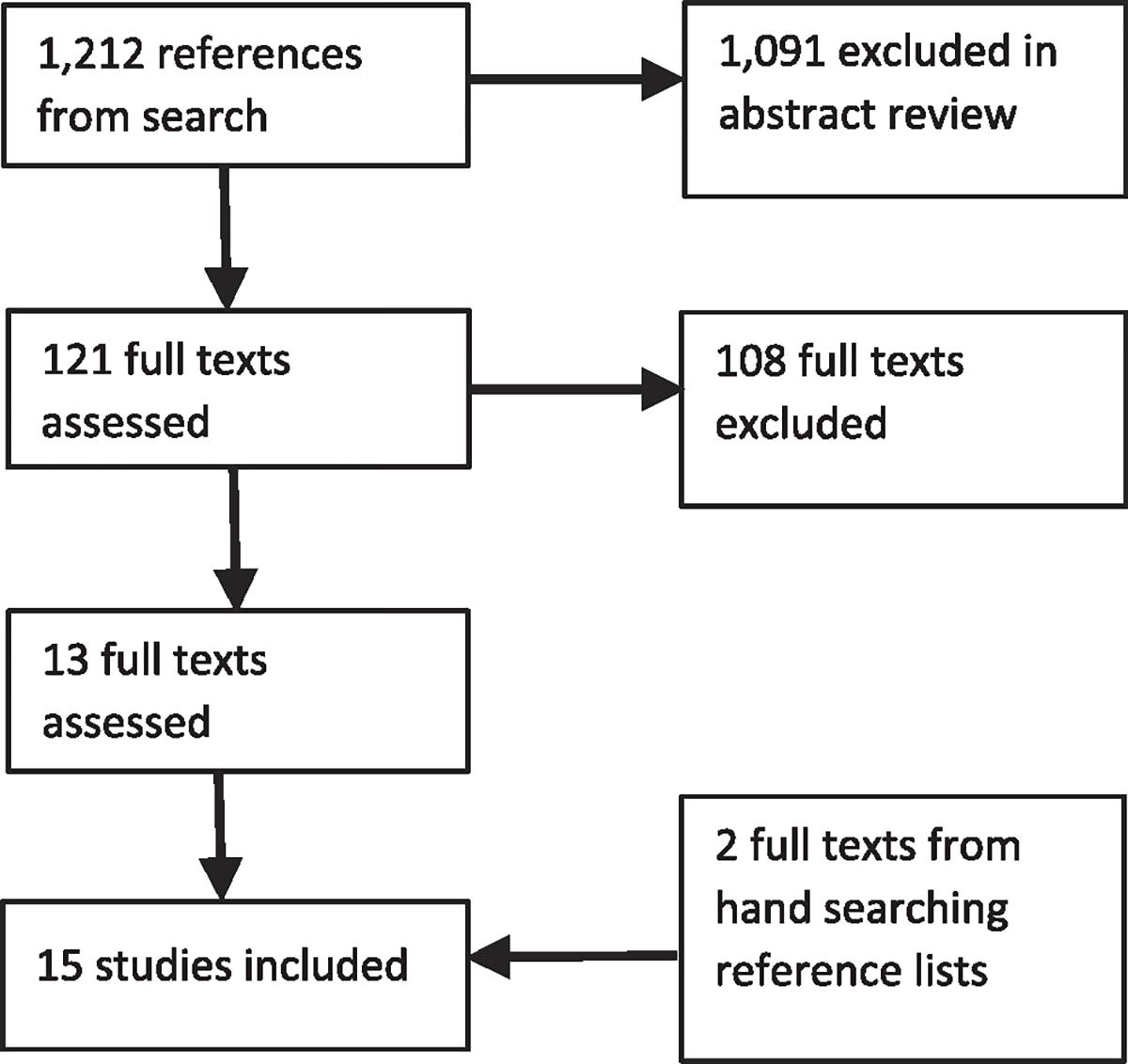
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart: flow diagram of study selection.
3.1. Pharmacist perspectives
3.1.1. Overview
Of the 10 studies that included pharmacists [2,13,24–32], eight were cross-sectional [24,26–31] or longitudinal [13,25] surveys, and two were interviews or focus groups [2,32] (Table 2; full evidence tables can be found in online appendix A.2). Six studies sampled participants from one state, [California (n = 3), Oregon (n = 2), Ohio (n = 1)] [13,24,26,29,30,32], two sampled from one locality (metropolitan Seattle, Washington and a pharmacy school in Illinois) [2,27], one sampled from multiple states [25], and one was a national sample [31]. The sample populations included student pharmacists in two studies [27–29] and practicing pharmacists in all other studies. Sample sizes ranged from nine student pharmacists in Illinois to 2725 pharmacists in a national study [27,31].
Table 2.
Evidence summary for studies on pharmacist-prescribed contraception: pharmacist perspectives (10 studies).
| Author, year | Study design | Population (response rate) | Law or policy | Outcomes | Quality |
|---|---|---|---|---|---|
|
| |||||
| Rodriguez, 2016 [24] | Cross-sectional electronic survey | Pharmacists, Oregon 509/3041 (17%) |
Pharmacist-prescribed contraception, after passage but prior to implementation of Oregon law | Interest Motivators Comfort Barriers |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Lio, 2018 [25] | Pre-post electronic survey | Pharmacists, Kroger pharmacies, 6 states in mid-Atlantic division 78/350 (22%) |
Pharmacist-prescribed contraception, not implemented in sampled states | Comfort Barriers |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Hilverding, 2017 [26] | Cross-sectional electronic survey | Pharmacists, direct patient care setting, Ohio 138/500 (28%) |
Pharmacist-prescribed contraception, not implemented in Ohio | Interest (support) Motivators Comfort Barriers |
Selection bias: Moderate Information bias: High Analysis bias: Low Generalizability: Poor |
| Lynch, 2018 [27] | Post-intervention cross-sectional electronic survey | Student pharmacists enrolled in women’s health elective, Illinois pharmacy school 9/11 (82%) |
Pharmacist-prescribed contraception, not implemented in Illinois | Comfort |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Rafie, 2011 and Rafie, 2014 [28,29] | Cross-sectional electronic or paper survey | Student pharmacists who had completed contraceptive curriculum, all pharmacy schools in California 502/803 (63%) |
Pharmacist-prescribed contraception, prior to passage of California law | Interest Motivators Comfort Barriers |
Selection bias: Moderate Information bias: Moderate Analysis bias: Low Generalizability: Fair |
| Vu, 2019 [30] | Cross-sectional electronic survey | Pharmacists, direct patient care setting, California 257/1774 (14%) responded, 121/257 (47%) eligible |
Pharmacist-prescribed contraception, after passage but prior to implementation of California law | Interest Motivators Comfort Barriers |
Selection bias: High Information bias: Moderate Analysis bias: Low Generalizability: Poor |
| Landau, 2009 [31] | Cross-sectional electronic survey | Pharmacists, American Pharmacists Association 2725/14,142 (19%) |
Pharmacist-prescribed contraception, prior to passage of laws in any state | Interest Motivators Comfort Barriers |
Selection bias: High Information bias: Moderate Analysis bias: Low Generalizability: Poor |
| Rodriguez, 2018 [13] | Longitudinal electronic survey | Pharmacists certified to prescribe contraception, Oregon 121/732 (17%) at 6 months, 62/121 (51%) at 12 months |
Pharmacist-prescribed contraception, 6 and 12 months after implementation of Oregon law | Interest Motivators Comfort |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Gardner, 2008 [2] | Interviews and focus groups in a longitudinal community-based intervention | Pharmacists, community pharmacies, Metropolitan Seattle n = 26 |
Direct access to contraception through collaborative drug therapy agreements, which Washington pharmacy act has allowed since 1979 | Interest Motivators Comfort |
Selection bias: High Information bias: High Analysis bias: High Generalizability: Poor |
| Gomez, 2019 [32] | Cross-sectional telephone interviews | Pharmacists, community-based, independent pharmacies, California n = 36 |
Pharmacist-prescribed contraception, after implementation of California law | Interest Motivators Barriers |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
Most studies (n = 7) included locations where pharmacist-prescribed contraception services were not implemented at the time of data collection [24–31]. However, pharmacist-prescribed contraception was in effect in two studies—a 2016 survey of Oregon pharmacists certified to provide HC [13] and a study in which 8 of 36 California pharmacists reported prescribing contraception during 2016–2017 interviews [32]. Another study evaluated a 2003–2005 pharmacy access to contraception intervention in metropolitan Seattle, in which 26 participating pharmacists prescribed contraception to eligible women [2].
The pharmacist studies had high [2,13,24,25,27,32] or moderate [26,28–31] risk of bias. Risk of selection bias was high, primarily due to low response rates and lack of information on non-responders. Response rates ranged from 14–82%, and most were lower than 30%. Some studies sampled their entire population of interest or used probability sampling and therefore had lower risk of sampling bias [13,24,26,28–32], while others used nonprobability sampling that increased their risk of sampling bias [2,25,27]. Risk of information bias was high because no studies reported reliability and validity of their quantitative or qualitative instruments. Risk of bias in the data analysis was low because most studies used appropriate descriptive and analytic techniques. Nine studies were likely not generalizable to their target populations due to the use of non-probability sampling or low response rates; one study may have been generalizable to its target population, California student pharmacists who had completed HC curricula [28,29].
3.1.2. Interest
Six studies found overall high levels of pharmacist interest in or intention to participate in pharmacist-prescribed contraception services [2,24,28,30–32]. In a national survey, 85% of US pharmacists were interested in providing pharmacy access to contraception [31]. In California studies, 65% of pharmacists and 96% of student pharmacists expressed interest [28,30]; 73% of pharmacists were “very” or “somewhat” likely to prescribe contraception under a statewide protocol [30]. In a qualitative survey after implementation of the California law, 96% of pharmacists expressed interest in completing HC training [32]. In Oregon, though 57% of respondents were interested in prescribing contraception, only 39% intended to prescribe after legislation went into effect [24]. All 15 Seattle pharmacists who gave feedback on a pharmacy access to contraception intervention wanted to continue providing contraception after study end [2].
In addition, five studies found that pharmacists were interested in several aspects of contraceptive care [13,24,28,30,31]. Studies found that 61% and 73% of pharmacists were interested in managing side effects [13,24], 54–73% were interested in managing method switching [24,30,31], and about 64% were interested in making formulation adjustments [30,31]. Over half of Oregon pharmacists (54%) and California student pharmacists (60%) were interested in prescribing to adolescents [13,28].
3.1.3. Motivators
Seven studies explored motivators for pharmacist interest in pharmacist-prescribed contraception [13,24,26,28,30–32]. Most pharmacists in a national survey (98%) and a California survey (90%) believed that pharmacy access was an important public health issue [30,31]. Most pharmacists (94%) in a qualitative California study believed that pharmacy access was an important health and community service [32]. Across four studies, 61–97% of pharmacists believed that pharmacy access would increase overall patient access to contraception [24,26,28,30]. Pharmacists (46% and 66%) in two studies believed that pharmacist-prescribed contraception services may reduce unintended pregnancies [24,26]. In Oregon and California studies that occurred after law implementation, increasing access to contraception and reducing unintended pregnancies were two of the most important motivators for pharmacists [13,32].
Nearly all pharmacists in a national survey (97%) and a California survey (91%) believed that prescribing contraception was a professional development opportunity [30,31]. Most of these US (97%) and California pharmacists (89%) would appreciate individual patient contact in the context of prescribing HC [30,31]. However, before implementation of the law in Oregon, only about 35% of pharmacists believed that prescribing contraception would increase their job satisfaction [24]. In two qualitative assessments after implementation of laws in Oregon and California, pharmacists generally were motivated to expand their scope of practice [13,32].
Anticipated positive impact on their businesses and on the healthcare system also motivated pharmacists. Pharmacists in a US survey (88%) and a California survey (77%) believed that pharmacist-prescribed contraception could help increase business [30,31]. Several of the pharmacists in these studies [US (59%) and California (44%)] believed the service could help recruit pharmacists to work at their pharmacies [30,31]. Regarding impact on the healthcare system, 47–96% of pharmacists across three studies thought that pharmacist-prescribed contraception could strengthen the relationship between pharmacists and other healthcare providers [24,30,31].
3.1.4. Comfort
Seven studies investigated pharmacist comfort and confidence with prescribing contraception [2,13,25,27,29–31]. In two of these studies, pharmacists were actively prescribing contraception [2,13]. In an Oregon study, 90% of pharmacists felt comfortable prescribing and counseling on contraception one year after implementation of the law [13]. In a Seattle intervention study, all 15 pharmacists who gave qualitative feedback reported confidence in initiating, counseling on, and managing contraception [2].
In five studies, pharmacists reported on their comfort and confidence with prescribing contraception, though pharmacist-prescribed contraception was not in effect in their practice areas [25,27,29–31]. Among pharmacists in a six-state sample, 65% and 46% felt comfortable prescribing contraception under a CPA or statewide protocol, respectively [25]. Only about 40% of these pharmacists were comfortable incorporating pharmacist-prescribed contraception services into their workflow [25]. Pharmacists in this sample felt most comfortable prescribing OCs (64%) and least comfortable prescribing injectables (43%) after completing HC training [25]. In samples of California student pharmacists and US pharmacists, most respondents (91% and 95%, respectfully) were comfortable screening patients for HC [29,31]. Across three studies, pharmacists and student pharmacists (63–94%) felt confident knowing when to refer a patient to a physician [25,27,29].
Despite the overall high levels of confidence in prescribing contraception, many pharmacists were interested in additional training. Among trained Oregon pharmacists surveyed after law implementation, 25–59% were interested in additional training on different prescribing and counseling topics [13]. Across several studies in locations without implemented laws, pharmacists and student pharmacists reported interest in specific training topics, such as identifying contraindications (46–84%) [24,29–31], counseling (51–69%) [24,29,30], and product selection (79–93%) [26,29–31]. Training for administering pharmacist-prescribed contraception was cited as the most important resource needed by pharmacists in a six-state study, and as a “must have” tool by 65% of pharmacists in Ohio [25,26].
3.1.5. Barriers
While many pharmacists were interested in and comfortable prescribing contraception, six studies explored barriers to implementation [24,26,28,30–32]. Several barriers were related to resource constraints. Lack of training was identified as a barrier by about 70% of Oregon pharmacists [24]. Limited time was identified by 56–96% of pharmacists and student pharmacists across three studies [28,30,31]. Limited staffing was identified by 75% of Oregon pharmacists [24]. Lack of private counseling areas in pharmacies was considered a barrier for some pharmacists across three studies (31–55%) [24,26,31] and most California student pharmacists (91%) [29]. In qualitative interviews with California pharmacists, limited time, limited staff, and lack of private counseling areas were also described as barriers [32].
Pharmacists were concerned about economic barriers. Inadequate or lack of reimbursement for prescribing contraception was a concern for 30–66% of pharmacists across three studies, and lack of appropriate incentive structure was a concern for 89% of student pharmacists in California [26,28,30,31]. Insurance reimbursement was reported as a barrier by pharmacists in qualitative interviews after implementation of the California law [32]. Costs, such as those to set up the service, were considered a barrier by 33% and about 55% of pharmacists in two studies [24,31].
Pharmacists reported pharmacy-level and system-level barriers to implementation. Liability was a concern for 45–88% of pharmacists across five quantitative studies and for California pharmacists in one qualitative study [24,26,28,30–32]. Lack of access to patient medical records was identified by some Ohio pharmacists (42%), most California student pharmacists (93%), and California pharmacists in a qualitative study [26,28,32]. Resistance from physicians was perceived as a barrier by 32–44% of pharmacists across three studies [24,26,31].
Regarding patient healthcare, 41% of Ohio pharmacists and 91% of California student pharmacists were concerned that women might neglect other aspects of their care if seeking contraception from a pharmacist [26,28]. A qualitative study also identified California pharmacists’ concern that patients may replace clinic visits with pharmacy visits [32]. Many pharmacists in California (76%) and national (88%) samples who reported disinterest in prescribing contraception believed that a pelvic exam and/or Pap smear was necessary for safely prescribing HC [30,31].
Four studies explored religious and personal beliefs and preferences. About 15% of Oregon pharmacists perceived religious objections to be an issue [24]. Among pharmacists in two studies who were disinterested in prescribing contraception, 21% and 54% reported that personal or religious beliefs were important [30,31]. In this sample, 21% and 54% also reported disinterest in providing any clinical service, not specific to contraceptive care [30,31].
3.2. Patient perspectives
3.2.1. Overview
Of the six studies that included patients, four were cross-sectional surveys [3,22,23,33], and two were interviews [2,34] (Table 3; full evidence tables can be found in online appendix A.3). One study sampled from one state (California) [34], one sampled from one locality (Seattle) [2], one sampled from multiple states [33], and three were national samples [3,22,23]. Sample sizes ranged from 30 adolescent women in California to 2,046 women at-risk for unintended pregnancy in a national survey [23,34]. Four studies sampled women of reproductive age, ranging from 15 to 46 years old [2,3,23,33], and two sampled only adolescent women, ranging from 14 to 19 years old [22,34]. Pharmacist-prescribed contraception services were in effect in only one study, a Seattle intervention study [2].
Table 3.
Evidence summary for studies on pharmacist-prescribed contraception: patient perspectives (6 studies).
| Author, year | Study design | Population (response rate) | Law or policy | Outcomes | Quality |
|---|---|---|---|---|---|
|
| |||||
| Landau, 2006 [3] | Cross-sectional telephone survey | Women at risk for unintended pregnancy, ages 18–44, US 811 (37%) |
Pharmacist-prescribed contraception, prior to passage of laws in any state | Interest (support) Motivators Barriers |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Grindlay, 2014 [33] | Cross-sectional electronic survey | Women seeking abortion, ages 15–46, urban abortion clinics, 6 states 651/757 (86%) |
Pharmacist-prescribed contraception, prior to passage of laws in any state | Interest |
Selection bias: Moderate Information bias: High Analysis bias: Low Generalizability: Fair |
| Wilkinson, 2018 [34] | Telephone interviews | Adolescent women, ages 18–19, California n =30 | Pharmacist-prescribed contraception, prior to implementation of California law | Interest (support) Motivators Barriers |
Selection bias: High Information bias: High Analysis bias: Low Generalizability: Poor |
| Gardner, 2008 [2] | Interviews in a longitudinal community-based intervention | Women, ages 18–44, Metropolitan Seattle 175/195 (90%) at 1-month follow-up, 127/195 (65%) at 12-month follow-up |
Direct access to contraception through collaborative drug therapy agreements, which Washington pharmacy act has allowed since 1979 | Motivators Comfort |
Selection bias: High Information bias: High Analysis bias: High Generalizability: Poor |
| Manski, 2015 [22] | Cross-sectional electronic survey | Adolescent women, ages 14–17, US n = 348 |
Pharmacist-prescribed oral contraception, prior to passage of laws in any state | Interest (support) |
Selection bias: High Information bias: Moderate Analysis bias: Low Generalizability: Poor |
| Grossman, 2013 [23] | Cross-sectional electronic survey | Women at risk for unintended pregnancy, ages 18–44, US 4487/7989 (56%) at initial screening, 2120/4487 (47%) met inclusion criteria, 2046/2120 (97%) participated |
Pharmacist-prescribed oral contraception, prior to passage of laws in any state | Interest |
Selection bias: High Information bias: Moderate Analysis bias: Low Generalizability: Poor |
The patient studies had high [2,3,22,34] or moderate [23,33] risk of bias. Similar to the pharmacist studies, the patient studies had high risk of selection bias. Four of six studies had high risk of sampling bias because they used non-probability samples [2,22,33,34]. Response rates could not be calculated for three studies due to lack of clear sampling frames [2,22,34]; response rates for the other three studies varied from 37% to 86% [3,23,33]. Similar to the pharmacist studies, risk of information bias was high due to unvalidated data collection instruments, while risk of bias in the data analysis was low. Five studies were likely not generalizable to their target populations due to the use of non-probability sampling or low response rates; one study of patients in six states seeking abortions may have been generalizable to its target population.
3.2.2. Interest
Five studies found an overall high level of patient support for and interest in pharmacist-prescribed contraception [3,22,23,33,34]. Support ranged from 63% in a national sample of women at-risk for unintended pregnancy [3] to 79% and 97% in samples of adolescent women [22,34]. Interest among women in two national samples ranged from 38% interested in pharmacy access to OCs to 68% interested in pharmacy access to contraception [3,23]. Likelihood of using pharmacy access ranged from 57% of teenage women in a national survey to 62% of women across six states seeking an abortion [22,33]. Factors associated with women’s interest in using pharmacy access included: being low-income, being uninsured, prior problems obtaining a prescription, and prior unintended pregnancy or pregnancy scare [3,33]. Studies found mixed results for association of race and insurance status with likelihood of using pharmacy access [3,33].
A national sample investigated interest in pharmacist-prescribed contraception by current contraceptive use and demographics [3]. Among women not using contraception, 41% said they would begin using contraception if available through pharmacist-prescription. Among women already using contraception, 66% said they would like to receive their method through pharmacist-prescription. Among uninsured and low-income women not using contraception, 47% and 40%, respectively, said they would begin using contraception through these services [3].
3.2.3. Motivators
Three studies explored motivators for patient interest in pharmacist-prescribed contraception [2,3,34] In a national sample, many women thought that pharmacy access would be personally beneficial due to pharmacies’ convenient hours (85%) and locations (84%) and not paying for a clinic visit [3]. Compared to white women, African American and Latina women were more likely to believe that pharmacy access would be personally beneficial [3]. In Seattle, women were motivated to participate in a pharmacy access to contraception intervention because it was convenient (62%), and some did not wish to have a pelvic exam to obtain contraception (30%) [2]. Adolescent women in a qualitative study in California also described how pharmacies are convenient and accessible [34].
In addition to personal benefits, patients identified public health benefits. In a national sample, 72% of women believed that pharmacy access would lead to fewer unintended pregnancies; 72% believed that more low-income women would use contraception [3]. Adolescent women in a qualitative study in California believed that pharmacy access would help normalize contraceptive use and enhance contraceptive decision-making [34].
3.2.4. Comfort
One study examined patient comfort and satisfaction with a pharmacy access intervention in Seattle. At 1-month follow-up, 98% of participants were “satisfied” or “very satisfied” with the pharmacist-prescribed contraception program and 98% felt that the program was convenient. At 12-month follow-up, 97% were comfortable continuing to receive contraception from a pharmacist after study end [2].
3.2.5. Barriers
While many women were interested in pharmacist-prescribed contraception, two studies described their concerns. In a national sample, women were concerned about patient health, including contraceptive safety (83%) and fewer women getting Pap smears (77%) [3]. In a national survey of adolescent women, while 97% of interested patients were willing to pay for pharmacist-prescribed contraception, only 36% were willing to pay over $20 [22]. Among adolescent women in California, some interviewees reported that pharmacies should have confidential spaces and be youth-friendly [34]. They also described the importance of patient safety, confidentiality from parents, and limiting out-of-pocket costs [34].
4. Discussion
Most pharmacists and patients across 15 US studies supported and were interested in pharmacist-prescribed contraception. Pharmacists felt comfortable prescribing contraception; patients who participated in a pharmacist-prescribed contraception intervention were satisfied with the service. Pharmacists and patients were motivated to participate for several reasons, including expanding access to contraception, reducing unintended pregnancies, and expanding scope of practice for pharmacists. They also identified barriers to participation. Pharmacists were concerned about reimbursement, resource constraints, liability, and patient health; patients were concerned about costs, confidentiality, and patient health. This US-focused systematic review on pharmacist-prescribed contraception of all HC methods expands upon findings of a global systematic review on pharmacy access and over-the-counter access to OCs [35].
Addressing the identified barriers may improve implementation of pharmacist-prescribed contraception. This review described economic barriers, including patient out-of-pocket costs and payment for pharmacist services [22,24,26,28,30–32,34]. One year after law implementation, less than half of pharmacist-prescribed contraception visits in Oregon were billed to insurance, and 68% of pharmacies in California had fees for service [13,15]. The average fees were $40–45 [13,15]. Currently, few state laws require insurance to cover the costs of the service. Improving insurance coverage may increase patient and pharmacist participation.
We also identified resource constraints related to training, time, and physical layouts of pharmacies [13,24–26,28–32,34]. Pharmacists were concerned about lack of training and desired additional training [13,24–26,29–31]. Evaluation of training curricula and pharmacist competency with contraceptive prescribing are areas for future research. Pharmacists were also concerned about the time commitment for the service. Studies have found that pharmacists spent 18–30 min with each patient to prescribe contraception [13,36]. To address this barrier, utilization of pharmacy technicians in administrative tasks related to contraceptive prescribing or general pharmacy workflow may allow additional time for pharmacists to focus on clinical activities [37]. Additionally, patients and pharmacists desired private counseling areas for the service, though not all pharmacy layouts have appropriate space. A survey-based Australian study investigating the characteristics of community pharmacies that provided clinical services found that the presence of private counseling areas in pharmacies was positively associated with the provision of clinical pharmacy services [38]. Implementation research in the United States could investigate how pharmacies can incorporate technicians and private spaces for pharmacist-prescribed contraception services.
Some pharmacists believed that physicians may be resistant to pharmacist-prescribed contraception [24,26,31]. However, a national survey found that 74% of healthcare providers supported pharmacist-prescribed contraception for several HC methods [39]. Surveys have found that providers expressed similar motivators to pharmacists and patients, such as expanding access to contraception and reducing unintended pregnancies [39,40]. Although a majority of healthcare providers support pharmacist-prescribed contraception, some pharmacists may perceive lack of support due to historical or anecdotal experiences of physician resistance [41].
Pharmacists and patients both identified barriers of patient health concerns, and pharmacists identified the associated liability [3,26,28,30–32,34]. However, HC is safe for most patients [1], and studies have found that only 2–7% of US women seeking contraception have contraindications [42–44]. Women are able to accurately self-screen for contraindications [45], and pharmacists in a Seattle intervention study assessed for contraindications with high accuracy [2]. Some patients and pharmacists thought that women may neglect other aspects of their healthcare if receiving contraception from a pharmacist. However, research has found that about 90% of women receiving pharmacist-prescribed contraception had seen a primary care provider in the past year [43].
4.1. Limitations
This review has several limitations. First, summarizing the results was challenging as there were many different and inconsistent outcome measures across studies. Validating data collection instruments could help standardize survey questions and prioritize outcome measures for future research. Next, most studies addressed patient and pharmacist perspectives on pharmacist-prescribed contraception in states where laws and policies were not implemented; perspectives may change if these services become a reality. Additionally, all studies had moderate to high risk of bias, primarily due to low response rates on surveys and lack of validated instruments. Most studies also lacked generalizability to their target populations. Most of the pharmacist studies included participants from just one jurisdiction, primarily on the west coast, so results may lack generalizability to states without study data. Finally, there were fewer findings on patient perspectives compared to pharmacist perspectives, as less research exists on the patient population.
5. Conclusion
Widespread pharmacist-prescribed contraception may be an important strategy for increasing access to contraception in the United States. While there is emerging evidence evaluating early participation in pharmacist-prescribed contraception services [13–15,42], this review suggests that pharmacists and patients support and are interested in these services. Despite interest and comfort, pharmacists and patients acknowledge barriers, such as payment and patient health concerns; pharmacists also identify resource constraints, liability concerns, and additional training needs. As states continue to adopt pharmacist-prescribed contraception laws and policies, this evidence on facilitators and barriers can be used to inform implementation. Further research can explore best practices for maximizing implementation and participation.
Supplementary Material
Acknowledgements
The authors would like to thank Joanna Taliano, MA, MLS, for helping to build the literature search strategy and running the searches. The authors would also like to thank Jenny Sewell, JD, MPA, for helping to search for and interpret state laws and policies.
This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention.
Funding:
This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention.
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, Oak Ridge Institute for Science and Education, or Duquesne University.
Footnotes
Declaration of interest: Dr. Stewart-Lynch has received honoraria from Pfizer, Inc unrelated to the current project, and her spouse is an employee of Pfizer, Inc. The other authors of this paper have nothing to disclose.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.contraception.2020.10.012.
References
- [1].Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, et al. U. S. Medical Eligibility Criteria for contraceptive use, 2016. MMWR Recomm Rep 2016;65:1–103. [DOI] [PubMed] [Google Scholar]
- [2].Gardner JS, Downing DF, Blough D, Miller L, Le S, Shotorbani S. Pharmacist prescribing of hormonal contraceptives: results of the Direct Access study. J Am Pharm Assoc 2008;48:212–26. [DOI] [PubMed] [Google Scholar]
- [3].Landau SC, Tapias MP, McGhee BT. Birth control within reach: a national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception 2006;74:463–70. [DOI] [PubMed] [Google Scholar]
- [4].Grindlay K, Grossman D. Prescription birth control access among U.S. Women at risk of unintended pregnancy. J Women’s Health 2016;25:249–54. [DOI] [PubMed] [Google Scholar]
- [5].Or. Rev. Stat. 689. Prescription and dispensation of certain contraceptives. Available at https://www.oregonlegislature.gov/bills_laws/lawsstatutes/2015orLaw0649.pdf; 2015. [accessed 6 Apr 2020].
- [6].Tak CR, Kessler LT, Scott MA, Gunning KM. Pharmacist-prescribed hormonal contraception: a review of the current landscape. J Am Pharm Assoc 2019;59:633–41. [DOI] [PubMed] [Google Scholar]
- [7].Beal JL, Illingworth Plake KS. Social and legislative shaping of access to contraceptives and the pharmacist’s role: a literature review. Res Social Adm Pharm 2019. [DOI] [PubMed] [Google Scholar]
- [8].Rafie S, Landau S. Opening new doors to birth control: state efforts to expand access to contraception in community pharmacies. Birth Control Pharmacist. Available at https://birthcontrol-pharmacist.com/; 2019. [accessed 8 Jan 2020]. [Google Scholar]
- [9].National Alliance of State Pharmacy Associations. Pharmacist prescribing: hormonal contraceptives. Available at https://naspa.us/resource/contraceptives/; 2020. [accessed 10 Sept 2020].
- [10].Association of State and Territorial Health Officials. States authorize pharmacists to prescribe and dispense contraceptives. Available at: https://www.astho.org/StatePublicHealth/States-Authorize-Pharmacists-to-Prescribe-Dispense-Contraceptives/06-06-19/; 2019. [accessed 8 Jan 2020].
- [11].Kooner M, Joseph H, Griffin B, Lynch S, Vest K, Stewart-Lynch A, et al. Hormonal contraception prescribing by pharmacists: 2019 update. J Am Pharm Assoc 2020:1544–3191. [DOI] [PubMed] [Google Scholar]
- [12].Adams AJ, Weaver KK. The continuum of pharmacist prescriptive authority. Ann Pharmacother 2016;50:778–84. [DOI] [PubMed] [Google Scholar]
- [13].Rodriguez MI, Biel FM, Swartz JJ, Anderson L, Edelman AB. Pharmacists’ experience with prescribing hormonal contraception in Oregon. J Am Pharm Assoc 2018;58:608–13. [DOI] [PubMed] [Google Scholar]
- [14].Batra P, Rafie S, Zhang Z, Singh AV, Bird CE, Sridhar A, et al. An evaluation of the implementation of pharmacist-prescribed hormonal contraceptives in California. Obstet Gynecol 2018;131:850–5. [DOI] [PubMed] [Google Scholar]
- [15].Gomez AM. Availability of pharmacist-prescribed contraception in California, 2017. JAMA 2017;318:2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Eckhaus L, Ti A, Stewart-Lynch A, Curtis K, Whiteman M. Patient and pharmacist perspectives on pharmacist-prescribed contraception: a systematic review. PROSPERO. Available at https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=130051; 2019. [accessed 1 May 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].CLARITY Group at McMaster University. Risk of bias in cross-sectional surveys of attitudes and practices. Available at https://www.evidencepartners.com/wp-content/uploads/2017/09/Risk-of-Bias-Instrument-for-Cross-SectionalSurveys-of-Attitudes-and-Practices.pdf; 2017. [accessed 22 Apr 2019].
- [19].Critical Appraisal Skills Programme. CASP qualitative checklist. Available at https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf; 2018. [accessed 22 Apr 2019].
- [20].Blaxter M Criteria for the evaluation of qualitative research papers. Med Sociol online 2013;7. [Google Scholar]
- [21].Covidence systematic review software. Veritas Health Innovation. Melbourne, Australia. Available at https://www.covidence.org. [Google Scholar]
- [22].Manski R, Kottke M. A survey of teenagers’ attitudes toward moving oral contraceptives over the counter. Perspect Sex Repro Health 2015;47:123–9. [DOI] [PubMed] [Google Scholar]
- [23].Grossman D, Grindlay K, Li R, Potter JE, Trussell J, Blanchard K. Interest in overthe-counter access to oral contraceptives among women in the United States. Contraception 2013;88:544–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rodriguez MI, McConnell KJ, Swartz J, Edelman AB. Pharmacist prescription of hormonal contraception in Oregon: baseline knowledge and interest in provision. J Am Pharm Assoc 2016;56:521–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lio I, Remines J, Nadpara PA, Goode J-V. Pharmacists’ comfort level and knowledge about prescribing hormonal contraception in a supermarket chain pharmacy. J Am Pharm Assoc 2018;58:S89–93. [DOI] [PubMed] [Google Scholar]
- [26].Hilverding AT, DiPietro Mager NA. Pharmacists’ attitudes regarding provision of sexual and reproductive health services. J Am Pharm Assoc 2017;57:493–7. [DOI] [PubMed] [Google Scholar]
- [27].Lynch SE, Griffin BL, Vest KM. Assessment of a simulated contraceptive prescribing activity for pharmacy students. Curr Pharm Teach Learn 2018;10:178–84. [DOI] [PubMed] [Google Scholar]
- [28].Rafie S, El-Ibiary SY. Student pharmacist perspectives on providing pharmacy-access hormonal contraception services. J Am Pharm Assoc 2011;51:762–5. [DOI] [PubMed] [Google Scholar]
- [29].Rafie S, El-Ibiary SY. California pharmacy student perceptions of confidence and curricular education to provide direct pharmacy access to hormonal contraception. Pharm Educ 2014;14:31–6. [Google Scholar]
- [30].Vu K, Rafie S, Grindlay K, Gutierrez H, Grossman D. Pharmacist intentions to prescribe hormonal contraception following new legislative authority in California. J Pharm Pract 2019;32:54–61. [DOI] [PubMed] [Google Scholar]
- [31].Landau S, Besinque K, Chung F, Dries-Daffner I, Maderes NM, McGhee BT, et al. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J Am Pharm Assoc 2009;49:43–50. [DOI] [PubMed] [Google Scholar]
- [32].Gomez AM, McCullough C, Fadda R, Ganguly B, Gustafson E, Severson N, et al. Facilitators and barriers to implementing pharmacist-prescribed hormonal contraception in California independent pharmacies. Women Health 2020;60:249–59. [DOI] [PubMed] [Google Scholar]
- [33].Grindlay K, Foster DG, Grossman D. Attitudes toward over-the-counter access to oral contraceptives among a sample of abortion clients in the United States. Perspect Sex Repro Health 2014;46:83–9. [DOI] [PubMed] [Google Scholar]
- [34].Wilkinson TA, Miller C, Rafie S, Landau SC, Rafie S. Older teen attitudes toward birth control access in pharmacies: a qualitative study. Contraception 2018;97:249–55. [DOI] [PubMed] [Google Scholar]
- [35].Kennedy CE, Yeh PT, Gonsalves L, Jafri H, Gaffield ME, Kiarie J, et al. Should oral contraceptive pills be available without a prescription? A systematic review of over-the-counter and pharmacy access availability. BMJ Glob Health 2019;4: e001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Frost TP, Klepser DG, Small DC, Doyle IC. Time and motion study of pharmacist prescribing of oral hormonal contraceptives in Oregon community pharmacies. J Am Pharm Assoc 2019;59:222–7. [DOI] [PubMed] [Google Scholar]
- [37].Koehler T, Brown A. Documenting the evolution of the relationship between the pharmacy support workforce and pharmacists to support patient care. Res Social Adm Pharm 2017;13:280–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Sim TF, Wright B, Hattingh L, Parsons R, Sunderland B, Czarniak P. A cross-sectional survey of enhanced and extended professional services in community pharmacies: a pharmacy perspective. Res Social Adm Pharm 2020;16:511–21. [DOI] [PubMed] [Google Scholar]
- [39].Rafie S, Kelly S, Gray EK, Wong M, Gibbs S, Harper CC. Provider opinions regarding expanding access to hormonal contraception in pharmacies. Women’s Health Issues 2016;26:153–60. [DOI] [PubMed] [Google Scholar]
- [40].Rafie S, Haycock M, Rafie S, Yen S, Harper CC. Direct pharmacy access to hormonal contraception: California physician and advanced practice clinician views. Contraception 2012;86:687–93. [DOI] [PubMed] [Google Scholar]
- [41].Majercak KR. Advancing pharmacist prescribing privileges: Is it time?. J Am Pharm Assoc 2019;59:783–6. [DOI] [PubMed] [Google Scholar]
- [42].Anderson L, Hartung DM, Middleton L, Rodriguez MI. Pharmacist provision of hormonal contraception in the Oregon Medicaid population. Obstet Gynecol 2019;133:1231–7. [DOI] [PubMed] [Google Scholar]
- [43].Lu S, Rafie S, Hamper J, Strauss R, Kroon L. Characterizing pharmacist-prescribed hormonal contraception services and users in California and Oregon pharmacies. Contraception 2019;99:239–43. [DOI] [PubMed] [Google Scholar]
- [44].Xu H, Eisenberg DL, Madden T, Secura GM, Peipert JF. Medical contraindications in women seeking combined hormonal contraception. Am J Obstet Gynecol 2014;210:210.e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Shotorbani S, Miller L, Blough DK, Gardner J. Agreement between women’s and providers’ assessment of hormonal contraceptive risk factors. Contraception 2006;73:501–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


