Synopsis:
During the COVID-19 pandemic, crisis changes in clinical care significantly increased rates of delirium in the intensive care unit. Deep sedation, unfamiliar environments with visitor restrictions, and stalled uptake of the ABCDEF bundle due to high workload and health system strain contributed to the occurrence of delirium doubling in the ICU. As the pandemic wanes, healthcare systems and ICU leadership must emphasize post-pandemic recovery, integrating lessons learned about delirium management, evidence-based care, and family involvement. Strategies to empower clinicians, creatively deliver care, and integrate families pave the way forward for a more holistic and resilient approach to patient care in the post-pandemic era.
Keywords: delirium, COVID-19, ABCDEF bundle, family engagement
COVID-19: Clinical Case
In an intensive care unit (ICU) at the local community hospital, the team is caring for a 48-year-old male, ‘David’, with a history of chronic obstructive pulmonary disorder (COPD) who lives at home with his wife and two children, ages 16 and 17. David presented to the hospital via the emergency room with severe shortness of breath, worsening over the last day, and an initial oxygen saturation of 84%. Over the course of just a few hours, David transitioned from requiring oxygen via nasal cannula to being intubated on 80% FiO2 and a PEEP of 14 cm H20. The hospital is at capacity, with all ICU beds filled with patients with similar presentations. David was admitted to a makeshift ICU that was converted from a patient overflow space. It is an “all hands-on deck’ situation for staff, with attending physicians and trainees from non-critical care settings on board to help care for COVID-19 patients in the hospital’s ICU. As the day progresses, David’s oxygen levels remain low, and the team decides to place David in the prone position to enhance lung recruitment and medically paralyze him with cisatracurium to prevent him from breathing over the ventilator. The pharmacy is concerned about an impending shortage of propofol, so David is placed in a deep coma using midazolam and fentanyl. While David’s paralytics are turned off a couple of days later, he remains sedated and restrained in bed, with his intravenous pump and monitors set outside the room to reduce the need for entry by staff, who provide direct care when fully covered in personal protective equipment. The hospital has a strict no-visitors policy to prevent transmission of the novel coronavirus. Seven days later, David’s sedatives are titrated off and he self-extubates, thrashing in bed and unable to follow instructions. He is given haloperidol intravenously. Eight hours later he lies immobile in bed, unable to answer questions but maintaining eye contact.
Delirium: A Common and Complex Clinical Syndrome
The above clinical case describes a perfect recipe for the development of delirium during critical care. Delirium is an acute neurocognitive condition characterized by disturbed attention, awareness, and cognition. Predisposing factors (e.g., comorbidities and cognitive impairment) and precipitating factors (e.g., systemic illness and organ dysfunction, mechanical ventilation, benzodiazepines, opioids, immobilization, physical restraints) combine to increase the risk of delirium,1 which then contributes to greater mortality, functional disability, and long-term cognitive impairment.2,3 Throughout the COVID-19 pandemic, many patients, families, clinicians, and researchers in ICUs experienced severe distress due to the related devastation, which included increased rates of delirium. In this review, we describe the burden of delirium during the pandemic, the reversal of progress that had been made in delirium practices before the pandemic, and the journey we face to reduce this acute cognitive injury to critically ill patients moving forward.
Historical Recognition of Delirium in the ICU
In 1998, Dr. Thomas L. Petty from the University of Colorado Health Sciences Center editorialized in Chest that, despite prior care where patients were awake and alert in the ICU, he now saw, “paralyzed, sedated patients, lying without motion, appearing to be dead, except for the monitors that told [him] otherwise.” The practice of using sedative medications to keep patients in unresponsive states where they “appeared to be sleeping” was common, arising from clinicians’ benevolent desire that patients be comfortable on mechanical ventilation (or at least, forgetful of it), resulting in increased use of sedative-hypnotic agents in ICUs worldwide. Dr. Petty described the resultant complications of deep sedation, including a “clouded sensorium that often results in what has been termed as intensive care delirium.” Researchers then began to recognize this as an acute iatrogenic brain injury, now commonly known as delirium. The early 2000s yielded valid and easy-to-use ICU delirium assessment tools for adults (e.g., Confusion Assessment Method for the ICU [CAM-ICU], Intensive Care Delirium Screening Checklist [ICDSC]).4,5 A decade later pediatric ICU delirium screening tools were validated and published (e.g., Pediatric CAM-ICU, Cornell Assessment of Pediatric Delirium [CAPD]).6,7 The development of validated screening tools rapidly led to better understanding of ICU delirium prevalence, associated outcomes, and the development and testing of prevention and management interventions for both adults and children.8,9
Advent of the ABCDEF Bundle
In 2010, the ABCDEF bundle (A = assess, prevent, and manage pain; B = both spontaneous awakening trials and spontaneous breathing trials; C = choice of analgesia and sedation; D = assess, prevent, and manage delirium; E = early mobility and exercise; F = family engagement and empowerment) was proposed as a framework for ICU guideline implementation, integrating delirium assessment and management as part of this bundle of ICU evidence-based practices.10,11 The ABCDEF bundle was foundational in understanding the interdependency of delirium prevention and management on sedation and mobility practices in addition to considering long-term recovery beginning in the ICU. The ABCDEF bundle, applicable to all patients in the ICU regardless of their admitting diagnosis or ventilation status, has been proven to be safe, efficacious, and feasible, with more complete performance yielding greater reductions in delirium, ventilator, and ICU days.12 For example, in a study of over 15,000 critically ill adults, patients had a 40% lower likelihood of developing delirium when they received all components of the ABCDEF bundle compared with patients who received a lower proportion of bundled care.12 The bundle was later adapted to meet the need for age-appropriate bundled delirium care for critically ill children.13,14
COVID’s Disruption of ABCDEF Bundle Implementation
Due to strained staff, unprecedented patient volume, and limited resources, the COVID-19 pandemic disrupted progress made with ABCDEF bundle implementation. Not only did ABCDEF bundle adherence drop dramatically,15 but practices also trended toward increased rates of delirium. Prolonged and deep sedation was commonly employed during the pandemic to manage agitation and ventilator-patient dyssynchrony, while facilitating tolerance of higher positive end-expiratory pressure and prone positioning. These practices aligned with early advocacy for neuromuscular blockade, which is inseparable from deep sedation, in the management of COVID-19 acute respiratory distress syndrome.16 Consequently, patients with COVID-19 were prescribed higher doses of sedatives and analgesics than those without COVID-19. The percentage of physicians who regularly prescribed sedation increased from 86% to 94% and the percentage who performed daily awakening trials decreased from up to 66% to 30%.17,18 Reports of propofol shortages, prolonged neuromuscular blockade, prone ventilation, and concerns about propofol infusion syndrome also increased the reliance on benzodiazepines, a known deliriogenic drug, leading to patients with COVID-19 receiving benzodiazepines for a median of 7 (4–12) days.16
Along with increased sedative administration, patients had less physical and social contact with healthcare providers, were more often restrained in bed, were less mobile and unable to leave their rooms, and were cared for by stressed staff who were hard to recognize due to personal protective equipment (Figure 1). Clinicians may have also been advised by hospital leadership to limit patient interactions to conserve personal protective equipment.19 These factors combined with limited or nonexistent hospital visitation meant patients had fewer family members physically present with them, and likely contributed to increased use of physical restraints.20 Persistently elevated restraint use, which acutely increased at the beginning of the pandemic, was reported even months after the initial wave.21 Additionally, the pandemic intensified barriers to early mobilization, a practice that has positive and synergistic effects on ICU patient outcomes when paired with other ABCDEF bundle components. In an analysis of global ICU practices, COVID-19 infection was not itself a major barrier to mobilization; rather, mechanical ventilation and other associated clinical therapies (e.g., deep sedation) decreased the likelihood of mobilization.22
Figure 1.
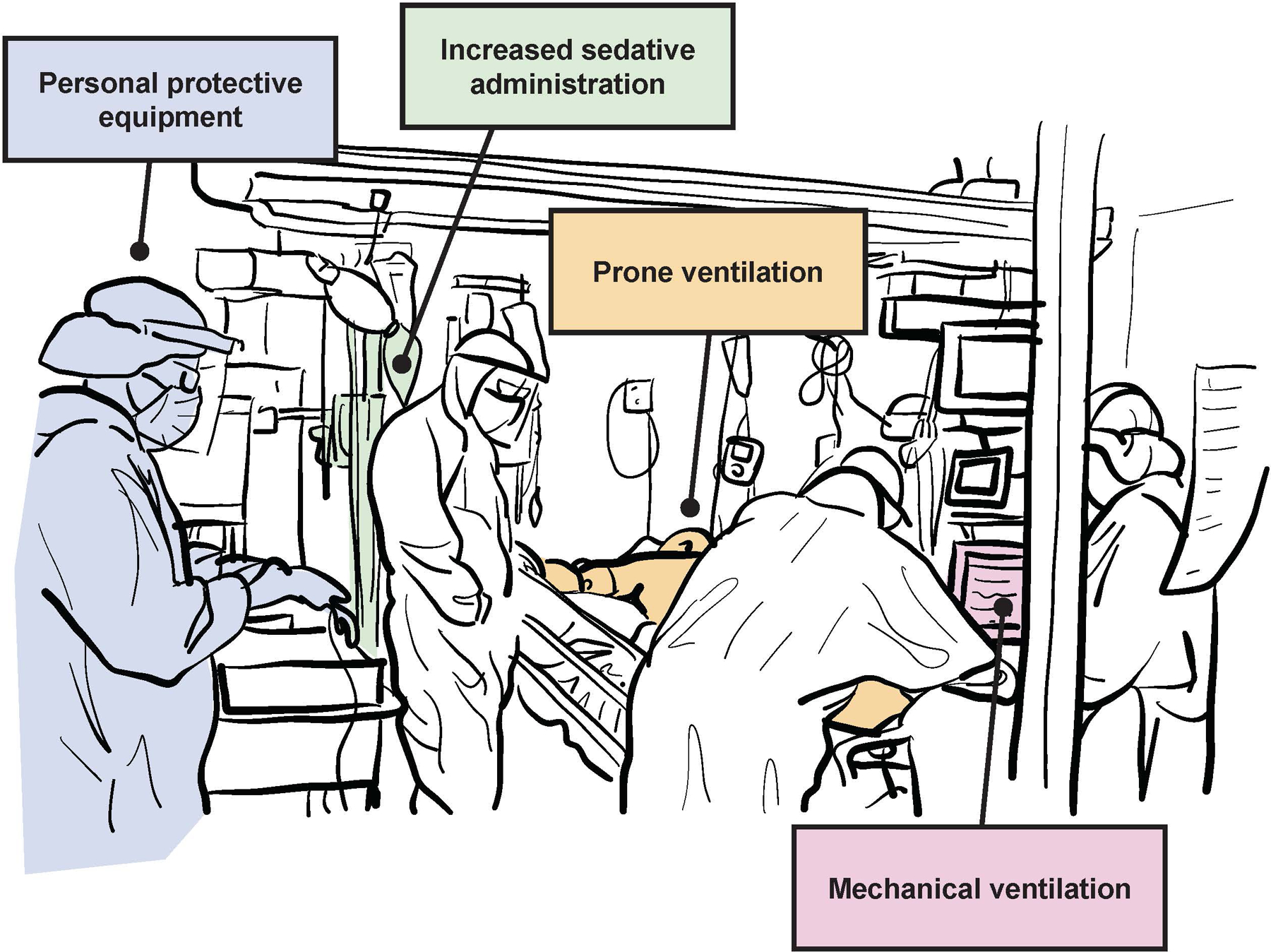
Crisis changes in clinical care during the COVID-19 pandemic, including increased use of personal protective equipment and deep sedation, prone ventilation, and mechanical ventilation, contributed to double the occurrence of delirium in the intensive care unit.
Thus, rates of delirium increased, affecting up to 84% of adult COVID-19 patients23–25 compared to up to 30% of critically ill patients pre-pandemic.26 Those diagnosed with COVID-19 had 4.42 (95% CI 2.69–7.26) greater odds of developing delirium as compared to non-COVID-19 patients, although delirium incidence did not differ among those with two or more days of mechanical ventilation.24 Likewise, COVID-19 patients with delirium also experienced worse outcomes than their non-delirious counterparts, with 3.2 (95%CI 2.1–4.8) greater odds of short-term mortality in those with delirium compared to those without.27
Similar trends occurred in the pediatric setting. The gains in evidence-based pediatric critical care using the ABCDEF bundle (64% pre-pandemic) were not sustained.28 While literature describing the influence of COVID-19 on pediatric ICU delirium care is scarce, reports indicate the rate of moderate to severe COVID-19 was dramatically less than in adults.29 Rather, children who had multiple comorbidities were more likely to have moderate to severe COVID-19 or Multisystemic Inflammatory Syndrome in Children that resulted in ICU care, although these cases represented less than 30% of all pediatric ICU cases.30 Still, pediatric patients experienced similar increase in immobilization, isolation, analgosedation, and visitor restrictions, contributing to worse disorientation and late recognition of delirium.31–33
Where Are We Now?
Now, nearly four years after the pandemic began, the healthcare system faces different challenges. While present COVID-19 surges are nothing compared to the high numbers in 2020, we still find ourselves navigating such surges and recovering from collateral damage from the height of the quarantine isolation and chaos of high volumes. Specifically, in many of our ICUs, we face significant staffing shortages leading to strained systems, high workload, and burnout. The strain on staff contributes to poor implementation and disconnect with evidence-based practice, including the ABCDEF bundle. Many ICUs continue practices started during the pandemic, originally intended to be exclusive to COVID-19 patients, with all patients, such as deep sedation, prone ventilation, and limited visitation hours. All these practices sustain the burden of delirium and coma during critical illness.
How Do We Move Forward?
Going forward, we make the same call as Dr. Petty in his editorial 25 years ago: “We must return to the basic principles of human caring and the fundamental principle of reason, as we try to guide desperately ill patients along the pathway to recovery.” While we have equipment and medication that can support critically ill patients in times of need, “supportive care” can also result in devastating cognitive impairment that persists for years after the acute illness. No pharmacological or mechanical advance “can begin to replace the caring physician, nurse, and therapist at the bedside to bring a patient from the threshold of death, back to the living.” Therefore, we call for the resuscitation of ABCDEF bundled care for adults and children by empowering clinical champions to promote uptake, implementing creative and novel care strategies to foster a team environment that promotes holistic recovery, and re-integrating patient-centered approaches in our new era of critical care (Figure 2).
Figure 2.
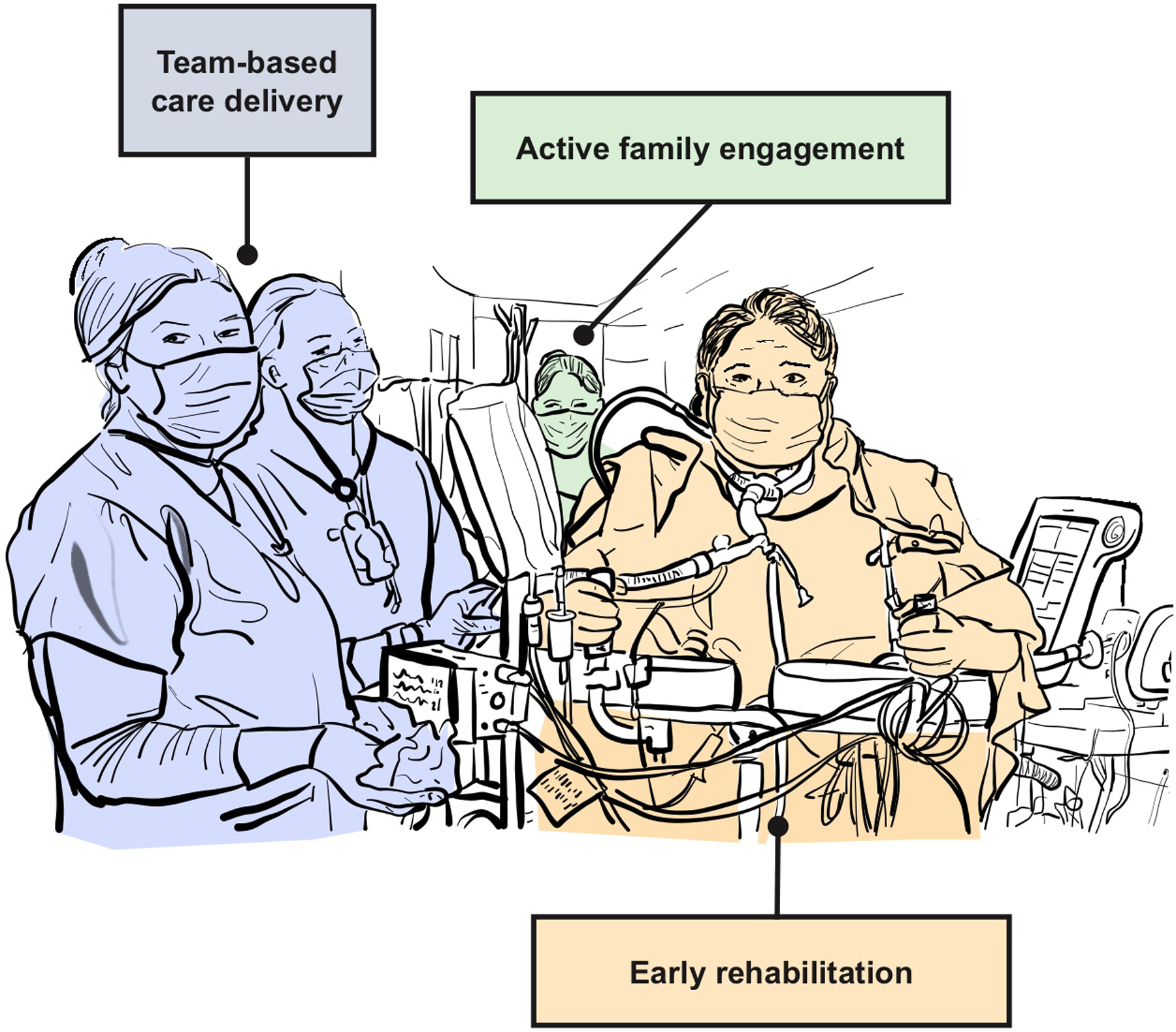
Resuscitation of patient-centered care after COVID-19 should emphasize motivating champions of the ABCDEF bundle, including the family as an active partner in care, and integrating novel care models that emphasize the strengths of the interprofessional team.
Motivating Champions of Care.
We must address the ongoing moral distress experienced by many healthcare workers to create a care environment where teams are motivated to pursue high-quality care. Persistent burnout, compassion fatigue, and low levels of personal accomplishment linger from the pandemic and negatively impact nurse professional commitment, clinical performance, and attitudes.34,35 However, renewed vigilance around the ABCDEF bundle could be a strategy to combat professional burnout. Mastery experiences, which include learning new things, are associated with higher work engagement for ICU nurses.36 Transforming nurses into delirium prevention experts could be a strategy to provide meaning, a sense of accomplishment, and increased work engagement. Creating experts begins with standardized education about ABCDEF bundle protocols. Standardized education equips nurses and other healthcare team members to advocate for high-quality, evidence-based patient care.37 Attention to the ABCDEF bundle may also transform exhaustion with the unwieldy problem of the pandemic into renewed energy directed at providing holistic care to individual human beings. The ABCDEF bundle provides tangible interventions to prevent delirium, a stark contrast to the distress of being under-equipped to proactively meet patient needs during the pandemic.38
Novel Care Strategies.
We must amplify what we have learned in past efforts to facilitate care coordination and implementation of evidence-based delirium care, while also recognizing that the critical care environment is different from its pre-pandemic state. Fatigue is common among ICU clinicians, and worse when compounded by burnout. Clinical decision support tools, like checklists and automated prompting may help facilitate adherence to evidence-based delirium care.39,40 Informatics and data science can be leveraged to reduce alert fatigue by providing customized feedback, prompts, or recommendations tailored to the clinician, patient, and setting. Thus, these systems may not add to the psychological burden faced by clinicians.41 The design of such systems should emphasize how clinicians interact with the computer, electronic health literacy, and education priorities to facilitate their use.42,43
Pre-pandemic, organizational factors were the most commonly reported barriers to ABCDEF bundle implementation, including team structure.44–46 When more members of the interdisciplinary team are involved in the individual components of the ABCDEF bundle, it is more likely that these components are implemented routinely yet rarely does this occur.47 Inclusion of the entire interprofessional team, including the family, social workers, pharmacists, psychologists, palliative care specialists, chaplains, and respiratory and rehabilitation therapists (physical, occupational, and speech), may help clinicians generate an optimal plan of care that promotes ABCDEF bundle implementation. However, given the turnover and structural changes among the ICU team since the pandemic, a robust analysis of how organizational factors and team dynamics influence individual contributions to ABCDEF implementation by healthcare team members is urgently needed to inform implementation strategy selection geared toward sustainability.
Both adult and pediatric patients who develop delirium are at high risk for post-intensive care syndrome (PICS),48–50 and should receive early referral to post-ICU recovery programs.51–53 ICU recovery care coordination via a multidisciplinary outpatient clinic, staffed by healthcare team members specializing in PICS, provides individualized evaluation, management, and referral to address ongoing needs often missed in standard ICU follow-up.54 Akin to a navigator program, ICU recovery clinics assist patients and family members with long-term recovery and provide support and guidance to those affected by delirium, aiding in adaptation to post-ICU life. More importantly, ICU staff involvement in ICU recovery programs offers benefits across the critical illness continuum by providing targets for ICU-based quality improvement initiatives, creating roles for ICU survivors to volunteer within the ICU setting, sensitizing ICU team members to the realities of PICS and the patient/family experience, and improving the meaningfulness of ICU work by creating a feedback loop.55
Reimagining Family Engagement.
Finally, we must reimagine opportunities for enhanced family inclusion in our ICUs – with an emphasis on the art, not just the science, of critical care.56 While COVID-19 highlighted deficiencies in hospital communication, in reality, these limitations have always existed. Nevertheless, family engagement and empowerment are integral components of the ABCDEF bundle of ICU care.
Families of critically ill patients may face barriers to in-person presence because of geographic distance, work or caregiving responsibilities, economic hardship, transportation challenges, or health limitations.57 Given pre-existing constraints on visitation, even without considering hospital restrictions, we must use best practices to communicate and facilitate family engagement and empowerment at a distance. While both the healthcare team and family members generally favor in-person conversations, empathy can successfully be conveyed via phone or video. Advanced logistical planning can also facilitate family engagement with programs like VoiceLove™, a virtual healthcare visitation system being researched and funded by the National Institute of Aging and the National Institute of Mental Health. Such technologies offer an opportunity to greatly enhance family connection while simultaneously relieving this time-consuming task from the nursing staff. Communication with family members at a distance can be further improved by assigning a point person to receive updates for continuity, frequently evaluating family understanding, allowing the family to view the patient and their surroundings via video, and offering time for the patient to interact with their family without healthcare team members present.57,58
When in-person, family members want to actively participate in care and prefer talking, providing music, reading aloud, hygiene- or medical-related activities, completing bed changes, bathing, or suctioning the patient over passive activities like receiving information.59 While there is limited evidence on the benefits of familiar voices for managing delirium, some investigators have concluded that auditory stimulation, particularly, direct auditory stimulation through talking to the patient, might be useful for improving the recovery of consciousness and increasing the arousal of comatose patients.60 In addition, others have indicated that family member voices can increase level of consciousness of comatose patients with traumatic brain injury and acute subdural hematoma.61 However, like how burnout and poor staffing impact implementation of the overall ABCDEF bundle, high staff-to-patient ratios and burnout influence how healthcare team members facilitate opportunities to activate family members. Managing barriers often must begin at the organizational level, but a facilitated understanding of the value of family presence (e.g., reduced delirium-related agitation and distress) may increase team member willingness to offer opportunities for family members to participate in care.62,63
Coordinated, early care pathways for family support also improve communication and patient- and family-centeredness, which are markers of improved decision-making that may contribute to value-concordant care. ICUs should develop policies and standards of care for identifying and addressing patient and family distress. Family members should be empowered with comprehensive education about delirium, emphasizing its presentation and potentially distressing symptoms, the family’s role in its management (e.g., assisting with orientation activities and mobility), and its significance in the care process. The “VALUE” mnemonic (Value family statements, Acknowledge emotions, Listen, Understand the patient as a person, and Elicit questions) can be implemented to enhance communication, foster empathy, and establish a collaborative atmosphere between the healthcare team and family.64 These strategies ensure the well-being of both patients and families is adequately considered and addressed, contributing to a holistic patient- and family-centered approach to ICU delirium care.
Moving Forward
Patients, families, and clinicians collectively confronted often overwhelming challenges because of the COVID-19 pandemic. Crisis changes in clinical practice resulted in increased sedation, isolation, restraint use, visitor restrictions, and de-adoption of the ABCDEF bundle, resulting in rates of delirium double those seen pre-pandemic. Clinicians, now burnt out and distressed, face the vital task of moving forward after the pandemic. Clinicians must be supported by their leadership and ICU environments to reenergize and champion the ABCDEF bundle, deliver critical care using models that facilitate recovery after critical illness without additional burden, and emphasize the art of clinical care. The path forward requires us to both look back to where we came from and move ahead with common goals in mind, including to reduce the burden of delirium and cognitive impairment among patients and to promote the well-being of their families.
Key Points:
Occurrence of delirium, an acute neurocognitive condition characterized by disturbed attention, awareness, and cognition and associated with poor long-term outcomes, increased significantly in intensive care units (ICU) during the COVID-19 pandemic due to increased sedation, immobilization, restraint use, isolation, and visitor restrictions.
Full delivery of the ABCDEF bundle in ICUs is associated with a 40% lower likelihood of delirium compared with patients who receive partial implementation of the ABCDEF bundle, but implementation of the bundle stalled during the COVID-19 pandemic.
Recruiting ABCDEF bundle champions may not only improve patient outcomes, but also provide meaning, a sense of accomplishment, and increased work engagement among ICU clinicians, all strategies that may combat professional burnout.
Novel care strategies that leverage informatics, the interprofessional team, and care coordination may facilitate better adherence to evidence-based care and reduce delirium and subsequent adverse outcomes among critically ill patients.
The family is a vital component of critical care, and active opportunities for families to engage with their loved ones should be provided by clinicians and will reduce delirium-related agitation and distress.
Clinics Care Points:
As a result of the COVID-19 pandemic, occurrence of delirium in the ICU has increased compared to pre-pandemic.
Routine use of deep sedation, immobilization, restraint use, and isolation and visitor restriction contribute to the burden of delirium and risks of mortality and long-term functional and cognitive impairment.
Resuscitation of patient-centered care requires ABCDEF bundle champions to promote uptake, novel care strategies that foster evidence-based and interprofessional care, and humane approaches that actively integrate the family as a necessary component of critical care.
Contributor Information
Kelly M. Potter, CRISMA Center, Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, PA, USA.
Brenda T. Pun, Department of Medicine, Pulmonary and Critical Care, Critical Illness, Brain dysfunction, and Survivorship Center, Vanderbilt University Medical Center, Nashville, TN, USA.
Kerri Maya, Sutter Health System, Sacramento, CA, USA.
Bethany Young, Hospital of the University of Pennsylvania, Philadelphia, PA, USA.
Stacey Williams, Monroe Carrell Jr Children’s Hospital at Vanderbilt, Nashville, TN, USA.
Marc Schiffman, Weill Cornell Medicine, New York, NY, USA.
Annmarie Hosie, School of Nursing & Midwifery Sydney, University of Notre Dame Australia, Sydney NSW, Australia; Cunningham Centre for Palliative Care, St Vincent’s Health Network Sydney, Sydney, NSW, Australia; IMPACCT- Improving Palliative, Aged and Chronic Care through Research and Translation, University of Technology Sydney, Sydney, NSW, Australia.
Leanne M. Boehm, School of Nursing, Vanderbilt University, Nashville, Tennessee, USA; Critical Illness, Brain dysfunction, and Survivorship (CIBS) Center, Vanderbilt University Medical Center, Nashville, TN, USA.
References
- 1.Ormseth C, LaHue S, Oldham M, Josephson S, Whitaker E, Douglas V. Predisposing and Precipitating Factors Associated With Delirium: A Systematic Review. JAMA Netw Open. 01/03/2023 2023;6(1):e2249950. doi: 10.1001/jamanetworkopen.2022.49950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ely E, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 04/14/2004 2004;291(14):1753–1762. doi: 10.1001/jama.291.14.1753 [DOI] [PubMed] [Google Scholar]
- 3.Pandharipande P, Girard T, Jackson J, et al. Long-term cognitive impairment after critical illness. The New England journal of medicine. 10/03/2013 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ely E, Inouye S, Bernard G, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 12/05/2001 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703 [DOI] [PubMed] [Google Scholar]
- 5.Bergeron N, Dubois M, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive care medicine. 2001 May 2001;27(5):859–864. doi: 10.1007/s001340100909 [DOI] [PubMed] [Google Scholar]
- 6.Smith H, Boyd J, Fuchs D, et al. Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit. Critical care medicine. 2011 Jan 2011;39(1):150–157. doi: 10.1097/CCM.0b013e3181feb489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Traube C, Silver G, Kearney J, et al. Cornell Assessment of Pediatric Delirium: a valid, rapid, observational tool for screening delirium in the PICU*. Critical care medicine. 2014 Mar 2014;42(3):656–663. doi: 10.1097/CCM.0b013e3182a66b76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalvas L, Harrison T. State of the science in pediatric ICU delirium: An integrative review. Res Nurs Health. 2020 Aug 2020;43(4):341–355. doi: 10.1002/nur.22054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van den Boogaard M, Slooter A. Delirium in critically ill patients: current knowledge and future perspectives. BJA Educ. 2019 Dec 2019;19(12):398–404. doi: 10.1016/j.bjae.2019.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devlin JW, Skrobik Y, Gelinas C, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. Sep 2018;46(9):e825–e873. doi: 10.1097/ccm.0000000000003299 [DOI] [PubMed] [Google Scholar]
- 11.Vasilevskis EE, Ely EW, Speroff T, et al. Reducing iatrogenic risks: ICU-acquired delirium and weakness--crossing the quality chasm. CHEST. 2010;138(5):1224–1233. doi: 10.1378/chest.10-0466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pun B, Balas M, Barnes-Daly M, et al. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Crit Care Med. 2019;47(1):3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Engel J, von B F, Baumgartner I, et al. Modified ABCDEF-Bundles for Critically Ill Pediatric Patients - What Could They Look Like? Front Pediatr. 05/02/2022 2022;10:886334. doi: 10.3389/fped.2022.886334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith H, Besunder J, Betters K, et al. 2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility. Pediatr Crit Care Med. 02/01/2022 2022;23(2):e74–e110. doi: 10.1097/PCC.0000000000002873 [DOI] [PubMed] [Google Scholar]
- 15.Liu K, Nakamura K, Katsukawa H, et al. Implementation of the ABCDEF Bundle for Critically Ill ICU Patients During the COVID-19 Pandemic: A Multi-National 1-Day Point Prevalence Study. Front Med (Lausanne). 10/28/2021 2021;8:735860. doi: 10.3389/fmed.2021.735860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pun B, Badenes R, Heras L, Calle G, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. The Lancet Respiratory medicine. 2021 Mar 2021;9(3):239–250. doi: 10.1016/S2213-2600(20)30552-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morandi A, Piva S, Ely E, et al. Worldwide Survey of the “Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Drugs, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Empowerment” (ABCDEF) Bundle. Critical care medicine. 2017 Nov 2017;45(11)doi: 10.1097/CCM.0000000000002640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luz M, Brandão B B, de C REV, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Annals of intensive care. 02/04/2022 2022;12(1):9. doi: 10.1186/s13613-022-00985-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosen A, Carter D, Applebaum J, et al. Critical Care Clinicians’ Experiences of Patient Safety During the COVID-19 Pandemic. J Patient Saf. 12/01/2022 2022;18(8):e1219–e1225. doi: 10.1097/PTS.0000000000001060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Font R, Quintana S, Monistrol O. Impact of family restrictions during COVID-19 pandemic on the use of physical restraint in an acute hospital: An observational study. J Healthc Qual Res. 2021 Sep-Oct 2021;36(5):263–268. doi: 10.1016/j.jhqr.2021.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones A, Goodarzi Z, Lee J, et al. Chemical and physical restraint use during acute care hospitalization of older adults: A retrospective cohort study and time series analysis. PLoS One. 10/26/2022 2022;17(10):e0276504. doi: 10.1371/journal.pone.0276504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu K, Nakamura K, Kudchadkar S, et al. Mobilization and Rehabilitation Practice in ICUs During the COVID-19 Pandemic. J Intensive Care Med. 2022 Sep 2022;37(9):1256–1264. doi: 10.1177/08850666221097644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Helms J, Kremer S, Merdji H, et al. Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. Crit Care. 08/08/2020 2020;24(1):s13054-020-03200-1. doi: 10.1186/s13054-020-03200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Westphal G, Fernandes R, Pereira A, Moerschberger M, Pereira M, Gonçalves A. Incidence of Delirium in Critically Ill Patients With and Without COVID-19. Journal of intensive care medicine. 2023 Aug 2023;38(8):751–759. doi: 10.1177/08850666231162805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernard-Valnet R, Favre E, Bernini A, et al. Delirium in Adults With COVID-19-Related Acute Respiratory Distress Syndrome: Comparison With Other Etiologies. Neurology. 11/15/2022 2022;99(20):e2326–e2335. doi: 10.1212/WNL.0000000000201162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krewulak K, Stelfox H, Leigh J, Ely E, Fiest K. Incidence and Prevalence of Delirium Subtypes in an Adult ICU: A Systematic Review and Meta-Analysis. Critical care medicine. 2018 Dec 2018;46(12):2029–2035. doi: 10.1097/CCM.0000000000003402 [DOI] [PubMed] [Google Scholar]
- 27.Shao S, Lai C, Chen Y, Chen Y, Hung M, Liao S. Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis. Age and ageing. 09/11/2021 2021;50(5):1445–1453. doi: 10.1093/ageing/afab103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ista E, Redivo J, Kananur P, et al. ABCDEF Bundle Practices for Critically Ill Children: An International Survey of 161 PICUs in 18 Countries. Crit Care Med. 01/01/2022 2022;50(1):114–125. doi: 10.1097/CCM.0000000000005168 [DOI] [PubMed] [Google Scholar]
- 29.Kim L, Whitaker M, O’Halloran A, et al. Hospitalization rates and characteristics of children aged< 18 years hospitalized with laboratory-confirmed COVID-19—COVID-NET, 14 states, March 1–July 25, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kompaniyets L, Agathis N, Nelson J, et al. Underlying Medical Conditions Associated With Severe COVID-19 Illness Among Children. JAMA Netw Open. 06/01/2021 2021;4(6):e2111182. doi: 10.1001/jamanetworkopen.2021.11182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castro R, Rodríguez-Rubio M, Magalhães-Barbosa M, Prata-Barbosa A. Pediatric delirium in times of COVID-19. Rev Bras Ter Intensiva. 01/24/2022 2022;33(4):483–486. doi: 10.5935/0103-507X.20210070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sisk B, Cull W, Harris JM, Rothenburger A, Olson L. National trends of cases of COVID-19 in children based on US state health department data. Pediatrics. 2020;146(6) [DOI] [PubMed] [Google Scholar]
- 33.Pumphrey K, Bouzaher A, Achuff B-J, Traube C. Sedation Practices in the PICU: An Unexpected Casualty of COVID-19. Critical Care Explorations. 2022;4(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020 Aug 2020;29(15–16):2762–2764. doi: 10.1111/jocn.15314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021 Aug 2021;77(8):3286–3302. doi: 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haruna Y, Shiromaru M, Sumikawa M. Factors related to intensive care unit Nurses’ work engagement: A web-based survey. Nurs Health Sci. 2023 Sep 2023;25(3):445–455. doi: 10.1111/nhs.13041 [DOI] [PubMed] [Google Scholar]
- 37.Albert B Prevention as Intervention: Reducing Incident Delirium in Heart Failure. J Dr Nurs Pract. 10/01/2019 2019;12(2):159–188. doi: 10.1891/2380-9418.12.2.159 [DOI] [PubMed] [Google Scholar]
- 38.González-Gil M, González-Blázquez C, Parro-Moreno A, et al. Nurses’ perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive Crit Care Nurs. 2021 Feb 2021;62:102966. doi: 10.1016/j.iccn.2020.102966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.King A, Potter K, Seaman J, et al. Measuring Performance on the ABCDEF Bundle During Interprofessional Rounds via a Nurse-Based Assessment Tool. Am J Crit Care. 03/01/2023 2023;32(2):92–99. doi: 10.4037/ajcc2023755 [DOI] [PubMed] [Google Scholar]
- 40.King A, Angus D, Cooper G, et al. A voice-based digital assistant for intelligent prompting of evidence-based practices during ICU rounds. J Biomed Inform. 2023 Oct 2023;146:104483. doi: 10.1016/j.jbi.2023.104483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.King A, Kahn J. The Role of Data Science in Closing the Implementation Gap. Crit Care Clin. 2023 Oct 2023;39(4):701–716. doi: 10.1016/j.ccc.2023.03.005 [DOI] [PubMed] [Google Scholar]
- 42.Gray K, Slavotinek J, Dimaguila G, Choo D. Artificial Intelligence Education for the Health Workforce: Expert Survey of Approaches and Needs. JMIR Med Educ. 04/04/2022 2022;8(2):e35223. doi: 10.2196/35223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Malerbi F, Nakayama L, Gayle D R, et al. Digital Education for the Deployment of Artificial Intelligence in Health Care. J Med Internet Res. 06/22/2023 2023;25:e43333. doi: 10.2196/43333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boehm L, Pun B, Stollings J, et al. A multisite study of nurse-reported perceptions and practice of ABCDEF bundle components. Intensive Crit Care Nurs. 2020 Oct 2020;60:102872. doi: 10.1016/j.iccn.2020.102872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Costa DK, White MR, Ginier E, et al. Identifying Barriers to Delivering the Awakening and Breathing Coordination, Delirium, and Early Exercise/Mobility Bundle to Minimize Adverse Outcomes for Mechanically Ventilated Patients: A Systematic Review. Chest. Aug 2017;152(2):304–311. doi: 10.1016/j.chest.2017.03.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boltey E, Iwashyna T, Hyzy R, Watson S, Ross C, Costa D. Ability to predict team members’ behaviors in ICU teams is associated with routine ABCDE implementation. J Crit Care. 2019 Jun 2019;51:192–197. doi: 10.1016/j.jcrc.2019.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Costa D, Valley T, Miller M, et al. ICU team composition and its association with ABCDE implementation in a quality collaborative. J Crit Care. 2018 Apr 2018;44:1–6. doi: 10.1016/j.jcrc.2017.09.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manning J, Pinto N, Rennick J, Colville G, Curley M. Conceptualizing Post Intensive Care Syndrome in Children-The PICS-p Framework. Pediatr Crit Care Med. 2018 Apr 2018;19(4):298–300. doi: 10.1097/PCC.0000000000001476 [DOI] [PubMed] [Google Scholar]
- 49.Watson R, Choong K, Colville G, et al. Life after Critical Illness in Children-Toward an Understanding of Pediatric Post-intensive Care Syndrome. J Pediatr. 2018 Jul 2018;198:16–24. doi: 10.1016/j.jpeds.2017.12.084 [DOI] [PubMed] [Google Scholar]
- 50.Hiser S, Fatima A, Ali M, Needham D. Post-intensive care syndrome (PICS): recent updates. J Intensive Care. 05/23/2023 2023;11(1):23. doi: 10.1186/s40560-023-00670-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sayde G, Stefanescu A, Hammer R. Interdisciplinary Treatment for Survivors of Critical Illness due to COVID-19: Expanding the Post-Intensive Care Recovery Model and Impact on Psychiatric Outcomes. J Acad Consult Liaison Psychiatry. 2023 May-Jun 2023;64(3):226–235. doi: 10.1016/j.jaclp.2023.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mikkelsen M, Still M, Anderson B, et al. Society of Critical Care Medicine’s International Consensus Conference on Prediction and Identification of Long-Term Impairments After Critical Illness. Critical care medicine. 2020 Nov 2020;48(11)doi: 10.1097/CCM.0000000000004586 [DOI] [PubMed] [Google Scholar]
- 53.Hall TA, Greene RK, Lee JB, et al. Post-intensive care syndrome in a cohort of school-aged children and adolescent ICU survivors: The importance of follow-up in the acute recovery phase. Journal of Pediatric Intensive Care. 2022; [Google Scholar]
- 54.Bloom S, Stollings J, Kirkpatrick O, et al. Randomized Clinical Trial of an ICU Recovery Pilot Program for Survivors of Critical Illness. Crit Care Med. 2019 Oct 2019;47(10):1337–1345. doi: 10.1097/CCM.0000000000003909 [DOI] [PubMed] [Google Scholar]
- 55.Haines KJ, Sevin CM, Hibbert E, et al. Key mechanisms by which post-ICU activities can improve in-ICU care: results of the international THRIVE collaboratives. Intensive Care Med. 2019;45(7):939–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.MA H The Arts Unique to Critical Care Nursing: Hard to Measure But Breathtakingly Manifest in a Pandemic. Dimens Crit Care Nurs. 2020 Sep/Oct 2020;39(5):287–289. doi: 10.1097/DCC.0000000000000437 [DOI] [PubMed] [Google Scholar]
- 57.Milner K Evolution of Visiting the Intensive Care Unit. Crit Care Clin. 2023 Jul 2023;39(3):541–558. doi: 10.1016/j.ccc.2023.01.005 [DOI] [PubMed] [Google Scholar]
- 58.Kennedy N, Steinberg A, Arnold R, et al. Perspectives on Telephone and Video Communication in the Intensive Care Unit during COVID-19. Annals of the American Thoracic Society. 2021 May 2021;18(5):838–847. doi: 10.1513/AnnalsATS.202006-729OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hetland B, McAndrew N, Kupzyk K, et al. Family Caregiver Preferences and Contributions Related to Patient Care in the ICU. West J Nurs Res. 2022 Mar 2022;44(3):214–226. doi: 10.1177/01939459211062954 [DOI] [PubMed] [Google Scholar]
- 60.Park S, Davis A. Effectiveness of direct and non-direct auditory stimulation on coma arousal after traumatic brain injury. Int J Nurs Pract. 2016 Aug 2016;22(4):391–396. doi: 10.1111/ijn.12448 [DOI] [PubMed] [Google Scholar]
- 61.Tavangar H, Shahriary-Kalantary M, Salimi T, Jarahzadeh M, Sarebanhassanabadi M. Effect of family members’ voice on level of consciousness of comatose patients admitted to the intensive care unit: A single-blind randomized controlled trial. Adv Biomed Res. 05/29/2015 2015;4:106. doi: 10.4103/2277-9175.157806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Eggenberger S, Sanders M. A family nursing educational intervention supports nurses and families in an adult intensive care unit. Aust Crit Care. 2016 Nov 2016;29(4):217–223. doi: 10.1016/j.aucc.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 63.Lee Y, Lee J, Kim J, Jung Y. Non-Pharmacological Nursing Interventions for Prevention and Treatment of Delirium in Hospitalized Adult Patients: Systematic Review of Randomized Controlled Trials. Int J Environ Res Public Health. 08/22/2021 2021;18(16):8853. doi: 10.3390/ijerph18168853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davidson J, Aslakson R, Long A, et al. Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med. 2017 Jan 2017;45(1):103–128. doi: 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]


