See Clinical Research on Page 2134
Sex (reflecting biological, reproductive differences between males and females) and gender (reflecting social and cultural differences between men and women) inequities exist in numerous societal and medical contexts, including in kidney care. Adequate kidney care requires awareness of kidney disease, consultation by a nephrologist, evaluation of underlying disease, a patient management plan, and periodic follow-up. Societal pressures, particularly in heavily patriarchal cultures, disproportionately burden women to overcome others’ unmet essential needs, often making a woman’s self-care the last priority. Common barriers across the globe in access to pertinent health care for women include financial dependency, culture norms, maternal obligations, such as those of family and childcare. In the health care setting, gender favoritism can negatively affect women’s access to care.1
The major social determinants of health include economic stability, political/legal factors, social and community context, health care provision, education, and neighborhood factors, each of which affects women and females’ access to kidney care.2 Social and community factors include availability and access to resources, family obligations and child care responsibilities. Health care provision may be affected by internalized sexism, because women may deny or ignore their symptoms and not seek screening or treatment owing to internalized biases learned through cultural expectations. Though political and legal regulations may affirm sex and gender equity on paper, in practice gaps still exist.
Globally, the prevalence of chronic kidney disease (CKD) tends to be higher in women/females compared to men/males. Lewandowski et al.,S1 analyzed the prevalence of CKD from outpatient clinics in Austria and CKD prevalence was 12.3% among females and 6.1% among males. A systematic review and meta-analysis from Hockham et al.,S2 reported CKD prevalence of 13% in females and 12% in males in Asia. Hill et al.,S3 in a systematic review also observed increased CKD prevalence in females (14.6%) versus males (12.8%). The International Society of Nephrology reported the CKD prevalence in women of ∼11.8% compared with 10.4% in men.S4
Sex and gender-based disparities do not always disadvantage females/women. Working in high ambient temperatures, a burden more often shouldered by men, is known to predispose individuals to CDK. A meta-analysis by Neugarten provides evidence of faster progression of CKD to end-stage kidney disease in men than women.S5 This accelerated disease progression in men may explain, in part, why males comprise the majority of recipients of both forms of renal replacement therapy, dialysis and transplantation.
Disparities in access to care by biological, demographic, and socioeconomic factors have the potential to arise within any of the many steps between developing kidney failure and potentially receiving the optimal treatment, an organ transplant. Females’ access to transplantation may be disproportionately affected by biological barriers, including preformed HLA antibodies after pregnancy, autoimmune diseases, and poor physical health due to frailty. Using the United States Renal Data System, Schold et al.,3 showed that <30% of patients diagnosed with renal failure are either waitlisted or receive a transplant within 4 years. In addition, <10% of patients with end-stage kidney disease are pre-emptively waitlisted or receive transplant. Access to transplantation among patients with end-stage kidney disease was also inequitable, varying substantially by factors including median household income, geographic region, and sex.
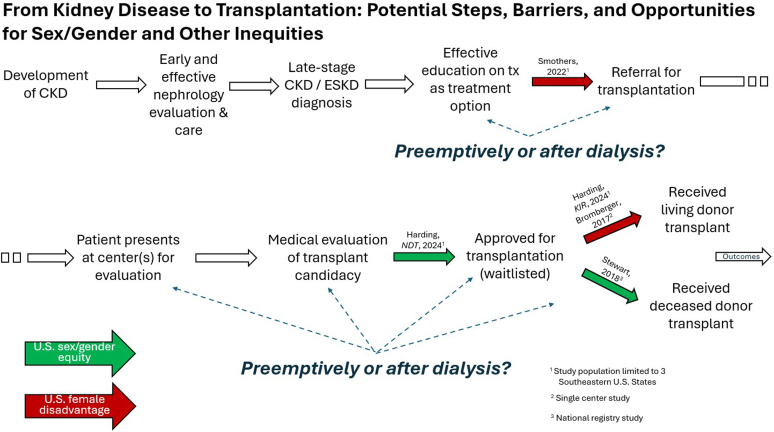
Several North American studies have assessed sex and/or gender disparities at various stages of the end-stage kidney disease-to-transplantation pathway. Kucirka et al.,S6 found that specific factors hindering women’s progression toward transplantation included increased age, intolerance to surgery, withdrawal of consent, and transplantation knowledge deficits. A study from Canada by Kim et al.,S7 found that females had 12% less access to transplantation than males. Using the first-of-its-kind, Early Steps to Transplant Access Registry,4 Harding recently found that among patients evaluated by a transplant center, the odds of being waitlisted were approximately the same by sex/gender in the Southeastern US.5 A national study found that once waitlisted, the rate of deceased donor transplantation was no different by birth sex (males versus females: adjusted relative risk = 1.0, 95% confidence interval: 0.92–1.08).6 By contrast, other studies have identified disadvantages for women/females in the likelihood of being referred for transplantation7 or receiving a living donor transplant.8,9 (Figure 1)
Figure 1.
Disparities in access to adequate and equitable care can hinder patients with severe kidney disease from progressing toward the optimal treatment, organ transplantation. Depending on social, biological, and individual factors, patients with imminent kidney failure may be evaluated for a transplant, and even receive a transplant, pre-emptively, whereas other patients may endure years of dialysis before even being properly educated and referred. Several steps are highlighted for which studies have found either equitable (green arrows) or disparate (red arrows) access by patient sex and/or gender. Comprehensive, national data are needed to fully inform policymakers and health providers about opportunities to address ongoing disparities in access to optimal kidney care.
The present issue of Kidney International Reports includes the latest edition in the early steps to transplant access registry series, a study by Harding et al.8 that aims to assess sex/gender-based disparities specifically in pre-emptive referral, as well as whether pre-emptive listing mitigates the aforementioned disparities. Discouragingly, the study found that even among patients who were pre-emptively referred, women were still 25% less likely to receive a living donor transplant, suggesting factors other than delayed referral underlie this disparity.9,S8 However, the large magnitude of this disparity is based on relatively small studies of limited geographic scope and does not appear to translate nationally. In 2021 to 2023, 22% of female (based on birth sex) kidney recipients in the United States received a living donor kidney, only slightly <24% of male recipients who received a kidney from a living donor.S9
Encouragingly, this study found essentially no differences by sex/gender in unadjusted odds of having been preemptively listed. After adjusting for medical and socioeconomic factors, women had ∼10% higher odds than men of having been listed preemptively. An insightful, supplementary analysis explored effect mediators that help explain the drivers behind the difference in unadjusted and adjusted results. For example, women were more likely to have severe obesity and be covered by public insurance, factors which are both associated with a markedly lower likelihood of having been preemptively listed. Adjusting for such factors essentially assumes that they are equally distributed for men and women, which is appropriate for assessing evidence for “disparate treatment” by sex in preemptive listing. On the other hand, risk adjustment masks that these factors disproportionately affect women in a way that could have caused (but, in this case, did not, as evidenced by the 0.99 crude odds ratio) a “disparate impact.S10 Supplementary Table S3 of Harding et al.,8 nicely highlights the value in presenting both unadjusted and adjusted findings.
The Southeastern Kidney Transplant Coalition was ahead of its time when it began a quality improvement initiative in 2010 to better understand disparities in access to transplantation, particularly those beginning well “upstream” of being added to the waiting list, an interim step many never reach. Patients, regulators, and others in the transplantation community have increasingly echoed the importance of measuring how well the US healthcare system is (or is not) serving all patients with end-stage organ failure, not just those fortunate enough to find their way onto the waiting list.S11,S12 The US health resources and services administration recently directed the OPTN to collect prelisting data to evaluate variations in listing rates among patients referred to transplant hospitals.S13 The early steps to transplant access registry database spawned from the Southeastern collaborative provides a template for expanding the collection of prelisting data beyond just 3 states to the cover the entire nation. The OPTN should incorporate lessons learned from early steps to transplant access registry, while exploring avenues for collecting data even further upstream. Collecting data even earlier in the process is needed to better understand which patients with organ failure are falling through the cracks well before being considered for the waiting list, for example those not adequately educated about transplantation as an option, never referred, or referred but never evaluated.
Only with complete, end-to-end transparency into the successes and shortcomings of a nation’s organ transplantation system will it be able to fully realize the promise of equity in organ transplantation.S12
Disclosure
Darren Stewart discloses his past employment with the USA Organ Procurement & Transplantation Network (OPTN) contractor, United Network for Organ Sharing (UNOS). All the authors declared no competing interests.
Footnotes
Supplementary References.
Supplementary Material
Supplementary References.
References
- 1.Mauvais-Jarvis F., Bairey Merz N., Barnes P.J., et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396:565–582. doi: 10.1016/S0140-6736(20)31561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anandh U., Meena P., Karam S., Luyckx V. Social, political and legal determinants of kidney health: perspectives from lower- and middle-income countries with a focus on India. Front Nephrol. 2022;2 doi: 10.3389/fneph.2022.1024667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schold J.D., Mohan S., Huml A., et al. Failure to advance access to kidney transplantation over two decades in the United States. J Am Soc Nephrol. 2021;32:913–926. doi: 10.1681/ASN.2020060888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patzer R.E., Retzloff S., Buford J., et al. Community engagement to improve equity in kidney transplantation from the ground up: the southeastern kidney transplant coalition. Curr Transplant Rep. 2021;8:324–332. doi: 10.1007/s40472-021-00346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harding J.L., Di M., Pastan S.O., et al. Examination of sex/gender disparities across the continuum of kidney transplant steps. Nephrol Dial Transplant. 2024;39:717–719. doi: 10.1093/ndt/gfad242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart D.E., Wilk A.R., Toll A.E., et al. Measuring and monitoring equity in access to deceased donor kidney transplantation. Am J Transplant. 2018;18:1924–1935. doi: 10.1111/ajt.14922. [DOI] [PubMed] [Google Scholar]
- 7.Smothers L., Patzer R.E., Pastan S.O., DuBay D., Harding J.L. Gender disparities in kidney transplantation referral vary by age and race: a multiregional cohort study in the Southeast United States. Kidney Int Rep. 2022;7:1248–1257. doi: 10.1016/j.ekir.2022.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harding J.L., Gompers A., Di M., et al. Sex/gender disparities in preemptive referrals for kidney transplantation. Kidney Int Rep. 2024;9:2134–2145. doi: 10.1016/j.ekir.2024.04.025. [DOI] [Google Scholar]
- 9.Bromberger B., Spragan D., Hashmi S., et al. Pregnancy-induced sensitization promotes sex disparity in living donor kidney transplantation. J Am Soc Nephrol. 2017;28:3025–3033. doi: 10.1681/ASN.2016101059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary References.