Abstract
Introduction
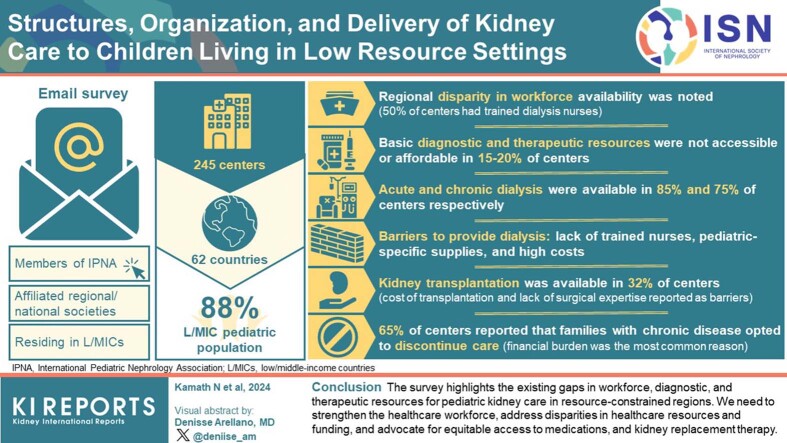
There is a disparity in the availability of health care for children in resource-constrained countries. The International Pediatric Nephrology Association (IPNA) commissioned an initiative exploring the challenges in the care of children with kidney disease in low- or middle-income countries (LMICs) with a focus on human, diagnostic, and therapeutic resources.
Methods
A survey was sent by e-mail to all members of IPNA and its affiliated regional or national societies residing in LMICs. Data were extracted from individual responses after merging duplicate data. Descriptive analysis was done using Microsoft Excel.
Results
Responses were obtained from 245 centers across 62 countries representing 88% of the LMIC pediatric population. Regional disparity in the availability of basic diagnostic and therapeutic resources was noted. Even when resources were available, they were not accessible or affordable in 15% to 20% of centers. Acute and chronic dialysis were available in 85% and 75% of centers respectively. Lack of trained nurses, pediatric-specific supplies, and high costs were barriers to providing dialysis in these regions. Kidney transplantation was available in 32% of centers, with the cost of transplantation and lack of surgical expertise reported as barriers. About 65% of centers reported that families with chronic disease opted to discontinue care, with financial burden as the most common reason cited.
Conclusion
The survey highlights the existing gaps in workforce, diagnostic, and therapeutic resources for pediatric kidney care in resource-constrained regions. We need to strengthen the health care workforce, address disparities in health care resources and funding, and advocate for equitable access to medications, and kidney replacement therapy (KRT).
Keywords: barriers, challenges, dialysis, low and middle-income countries, pediatric kidney care resources
Graphical abstract
The spectrum of kidney disease in children is wide and encompasses a diverse group of congenital and acquired diseases from in utero to adolescence.1 The disparity in the diagnosis, treatment, and care of kidney disease between high-income countries and LMICs is documented by projects such as the Global Kidney Health Atlas2,3 and the Global Burden of Disease Study.4 The available resources and access to care for children with kidney disease compared to adults are even more disparate.5,6 The challenge in providing care has been described on national or regional levels for nondialysis chronic kidney disease,7 dialysis,8 and transplant care,9,10 with reports of high rates of discontinuation of care in children with kidney failure.11 However, there remains a paucity of robust and comprehensive data focusing on the spectrum of pediatric kidney care (nondialysis chronic kidney disease, dialysis, and transplantation), and the barriers faced in LMICs globally. The IPNA commissioned a Priorities in Low Resource Countries Committee initiative under the IPNA Special Projects Committee to map the existing resources for the care of children with kidney disease in LMICs with a focus on the workforce, availability of health care technologies and medications, and the ability of patients to access these resources.
Methods
Setting
The survey aimed to assess the resources for the care of children with kidney diseases in low-, lower-middle, and upper-middle-income countries as defined by the World Bank classification based on gross national income12 (Supplementary Table S1).
Survey Development
The Priorities in Low Resource Countries Committee conducted a cross-sectional survey to assess the nature of, availability, and accessibility of pediatric nephrology resources in LMICs.
The survey was designed by 5 subgroups of the Priorities in Low Resource Countries Committee through an iterative process. Each subgroup focused on the development of questions within 1 of the following domains of the survey: human resources, diagnostic resources, therapeutic resources, and financial support. The subgroups prepared a questionnaire for their domain, which was then discussed and approved by the entire group. The preliminary survey was scrutinized by senior members of the committee. The survey was reviewed by the peers of other subgroups for content validity and comprehensiveness. A pilot run was conducted by 3 members of the Priorities in Low Resource Countries Committee to identify any logistic or feasibility issues and based on the feedback obtained the final questionnaire was refined and approved by all members. The survey (survey questionnaire) included geographical details such as the name of the center, city, and country. The survey explored the details of the center’s human resources (physicians, surgeons, nurses, and allied health) as well as the availability; affordability; and accessibility of basic diagnostic resources such as pediatric nephrology clinics, sphygmomanometers, urine dipsticks, microscopy, biochemistry; and of advanced resources such as imaging (ultrasound, voiding cystourethrograms), pathology (light microscopy and immunofluorescence), and complement testing). The availability, affordability, and accessibility of therapeutic resources such as basic medications (antihypertensives, immunosuppressives, antimicrobials, diuretics, and albumin), acute and chronic dialysis, and kidney transplantation were also explored. Finally, the survey explored reasons for care being discontinued.
Survey Administration
The survey was conducted from March 2021 through February 2022. An electronic version of the survey, created on SurveyMonkey (Survey Questionnaire), was sent to all participants via e-mail. This was accompanied by a letter of invitation to participate in the survey, which informed the participants that their response to the survey implied consent to publish the data. A maximum of 3 email reminders were sent to members who had not responded to the survey. The survey was sent to clinicians in 86 LMICs.
Snowball sampling methods were used to recruit participants. All members of IPNA from LMICs were invited to participate in the study and to invite members from their local and national pediatric nephrology associations. In addition, the survey was sent to representatives of the regional societies of IPNA (Asian Pediatric Nephrology Association, African Pediatric Nephrology Association, Latin American Association of Pediatric Nephrology, European Society for Pediatric Nephrology, and Australian and New Zealand Paediatric Nephrology Association) to send to their members. The survey was also sent through local contacts to pediatricians and adult nephrologists providing care to children with kidney disease, even if they were not members of IPNA or its regional societies. Only 1 health care provider from each center was requested to respond to the survey and no patient-level data was obtained.
Data Handling and Analysis
Data from individual surveys were extracted and checked for completeness with duplicated center entries merged. Any discrepancies regarding the presence of resources were adjudicated by 2 authors with the positive response being deemed correct. Country-level data were vetted by a senior clinician from IPNA regional societies familiar with each country. The centers were grouped based on their countries and were further grouped into the following 5 regions: Africa, Asia, Europe, Latin America, and Oceania. The countries were also classified as low-income, lower-middle-income, and upper-middle-income using the World Bank classification based on gross national income.12 The data were reported as numbers and percentages. Descriptive statistical analysis was done using Microsoft Excel.
Ethics and Privacy
The participants were physicians taking care of children in their respective centers, the data did not include individual patient information. This study was assessed by the New Zealand Health and Disability Ethics Committee and Auckland District Health Board Research Office and found to be low-risk and not requiring full New Zealand Health and Disability Ethics Committee or ethics review.
Results
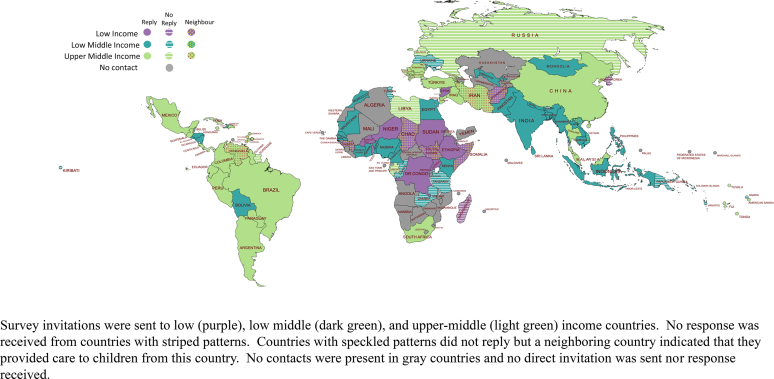
After consolidating duplicate data from 28 centers, responses were received from a total of 245 centers in 62 countries (Supplementary Table S1). The response rate represents 72% of the LMICs surveyed and 82% of the global pediatric population in LMICs. Some centers reported the provision of care to children from neighboring countries which, when included, brought the potential LMIC pediatric population captured by our survey to 88%. Responses were obtained from 7 low-income countries, 27 lower-middle-income countries, and 28 upper-middle-income countries. The target countries based on gross national income and response status are illustrated in Figure 1.
Figure 1.
Low and middle-income countries and survey uptake.
Availability of Workforce for Kidney Care
Trained pediatric nephrologists were present in 231 centers (94.3%), Oceania had no pediatric nephrologists at responding centers (Table 1). In some centers that had pediatric nephrologists, children with kidney diseases were also taken care of by adult nephrologists (n = 77, 31.4%). Children with kidney disease were cared for by a general pediatrician alone in 8 centers (3.3%) and by a general pediatrician along with an adult nephrologist in 5 (2.0%) responding centers. A pediatric nephrology clinic was present in 187 centers (76.3%).
Table 1.
Availability of human resources at centers providing pediatric nephrology care
| Human resources | All regions (N = 245) | Africa (n = 32) | Asia (n = 133) | Europe (n = 7) | Latin America (n = 70) | Oceania (n = 3) |
|---|---|---|---|---|---|---|
| Pediatric nephrologist | 231 (94.3%) | 28 (87.5%) | 131 (98.5%) | 7 (100%) | 65 (93%) | 0 |
| Pediatric HD nurse | 128 (52.2%) | 11 (34.3%) | 84 (63.2%) | 5 (71.4%) | 28 (40%) | 0 |
| Shared HD nurse | 131 (53.5%) | 18 (56.3%) | 74 (55.6%) | 4 (57.3%) | 33 (47.1%) | 2 (66.6%) |
| Pediatric PD nurse | 128 (52.2%) | 13 (40.6%) | 75 (56.4%) | 5 (71.4%) | 35 (50%) | 0 |
| Shared PD nurse | 78 (31.8%) | 6 (18.8%) | 49 (36.8%) | 0 | 23 (32.8%) | 0 |
| Pediatric ICU | 204 (83.3%) | 16 (50%) | 121 (91.1%) | 6 (85.7%) | 60 (85.7%) | 1 (33.3%) |
| Pediatric surgery | 223 (91%) | 28 (87.5%) | 126 (94.7%) | 5 (71.4%) | 62 (88.5%) | 2 (66.6%) |
| Radiology | 228 (93.1%) | 30 (93.7%) | 127 (95.5%) | 7 (100%) | 61 (87.1%) | 3 (100%) |
| Pathology | 189 (77.1%) | 22 (68.7%) | 118 (88.7%) | 7 (100%) | 40 (57.1%) | 2 (66.6%) |
| Social worker | 160 (65.3%) | 21 (65.6%) | 74 (55.6%) | 5 (71.4%) | 58 (82.8%) | 2 (66.6%) |
| Nutritionist | 189 (77.1%) | 20 (62.5%) | 99 (74.4%) | 2 (28.5%) | 65 (92.8%) | 3 (100%) |
HD, hemodialysis; ICU, intensive care unit; PD, peritoneal dialysis.
Availability of human resources for the care of children with kidney disease. The number of centers and the percentage of the total number of responding centers in the region are reported.
Despite the availability of pediatric nephrologists, children with kidney disease were most often managed by pediatricians in 56 centers (26%), adult nephrologists in 7 centers (3.3%), and general practitioners in 6 centers (2.8%).
About 50% of centers had trained pediatric nurses to provide hemodialysis (n = 128) and peritoneal dialysis (PD) (n = 128) (Table 1). Centers from Africa, Latin America, and Oceania had a lower availability of nurses than centers from Asia and Europe.
Support from collaborative specialties such as pediatric intensive care, pediatric surgery, and radiology was available in more than 80% of centers. Regional disparities were observed in the availability of pathologists, social workers, and nutritionists (Table 1).
Availability of Diagnostic Services
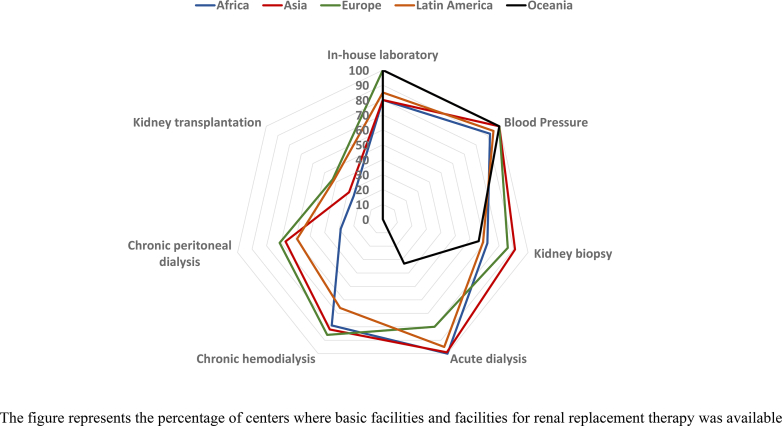
Standard in-house laboratory facilities were available in 181 of 218 centers (83.0%) in 52 countries. Blood pressure measurement was available for children in 213 of 218 centers (97.7%) in 60 countries. Capacity to perform kidney biopsies was reported in 179 of 218 centers (82.1%), though this was lower in centers from Latin America (43/62, 69%) and Oceania (2/3, 66%) (Figure 2).
Figure 2.
The availability of basic facilities, acute and chronic dialysis, and kidney transplantation in various regions.
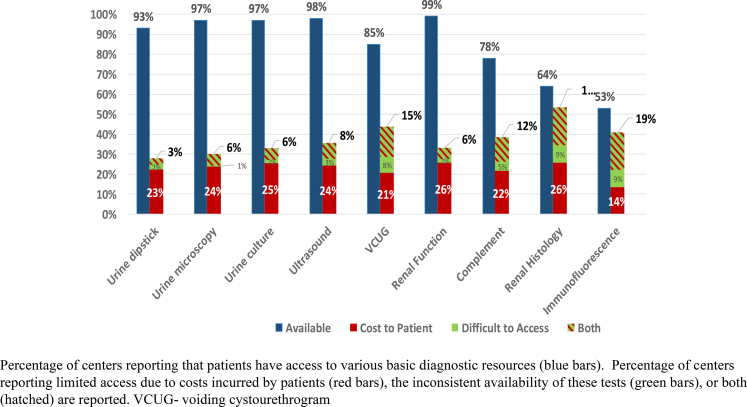
The availability of basic laboratory services such as urine dipstick analysis (n = 199, 93.4%), microscopy (n = 207, 97.1%), urine culture (n = 206, 96.7%), serum creatinine (n = 211, 99.1%), and kidney ultrasonography (n = 208, 97.7%) were commonly available with more specialized diagnostics such as complement (C3 and C4) testing, renal histology, and immunofluorescence being less available (Table 2), with African, Latin American, and Oceanic centers reporting the least availability. Even when these laboratory services were available either in-house or in other nearby centers, access to them was restricted by cost to patients in approximately one-third of centers, inconsistent availability in 5% to 10% of centers or both in 10% to 20% of centers (Figure 3). The most important reasons for difficulty in availing diagnostic facilities even when they were available were reported to be the need to send samples to another center or city, long turnaround time, lack of trained personnel to perform the tests, poor maintenance of equipment, high maintenance costs, and unreliable supply of consumables.
Table 2.
Diagnostic resources at centers providing pediatric nephrology care
| Diagnostics | All regions (N = 213) | Africa (n = 25) | Asia (n = 116) | Europe (n = 7) | Latin America (n = 62) | Oceania (n = 3) |
|---|---|---|---|---|---|---|
| Urine dipstick | 199 (93.4%) | 24 (96%) | 107 (92.2%) | 7 (100%) | 58 (93.4%) | 3 (100%) |
| Urine microscopy | 207 (97.1%) | 24 (96%) | 115 (99.1%) | 7 (100%) | 58 (93.4%) | 3 (100%) |
| Urine culture | 206 (96.7%) | 23 (92%) | 113 (97.4%) | 7 (100%) | 60 (96.8%) | 3 (100%) |
| Serum creatinine | 211 (99.1%) | 25 (100%) | 116 (100%) | 7 (100%) | 60 (96.8%) | 3 (100%) |
| Ultrasound | 208 (97.7%) | 23 (92%) | 116 (100%) | 7 (100%) | 59 (96.6%) | 3 (100%) |
| VCUG | 181 (85.3%) | 18 (72%) | 109 (94.0%) | 7 (100%) | 44 (71.0%) | 3 (100%) |
| Complement | 167 (78.4%) | 7 (28%) | 100 (86.2%) | 6 (85.7%) | 54 (87.1%) | 0 (0%) |
| Renal histology | 137 (64.3%) | 13 (52%) | 84 (72.4%) | 4 (57.1%) | 35 (56.5%) | 1 (33.3%) |
| Immunofluorescence | 113 (53.1%) | 5 (20%) | 74 (63.8%) | 4 (57.1%) | 30 (48.3%) | 0 (0%) |
VCUG, voiding cystourethrogram.
Availability of basic diagnostic resources required for the evaluation of kidney disease in children displayed as the number of centers responding in the affirmative (percentage).
Figure 3.
Challenges in access to diagnostic resources.
Therapeutic Resources
Medications
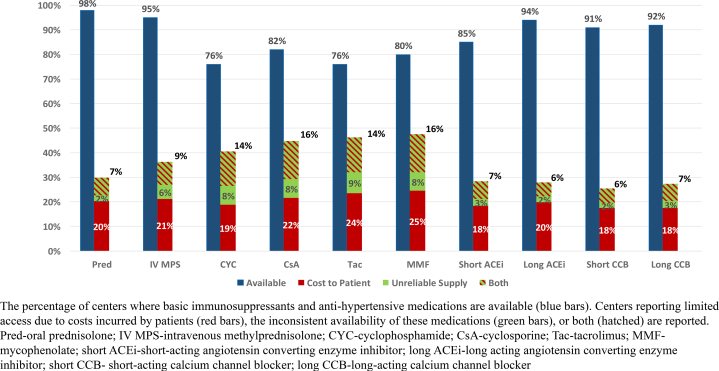
Immunosuppressive, diuretic, and antihypertensive medications were available in over 75% of centers. There was regional variation, particularly in the availability of immunosuppressive medications which were less available to centers in Oceania and Latin America, compared to centers in Asia and Europe (Table 3).
Table 3.
Availability of common medications used in pediatric nephrology care
| Medications | All regions (N = 212) | Africa (n = 25) | Asia (n = 117) | Europe (n = 7) | Latin America (n = 60) | Oceania (n = 3) |
|---|---|---|---|---|---|---|
| Immunosuppressants | ||||||
| Prednisolone | 208 (98.1%) | 25 (100%) | 114 (97.4%) | 6 (85.7%) | 60 (100%) | 3 (100%) |
| Methylprednisolone | 201 (94.8%) | 22 (88.0%) | 112 (95.7%) | 7 (100%) | 58 (96.2%) | 2 (66.7%) |
| Cyclophosphamide | 162 (76.4%) | 20 (80.0%) | 94 (80.3%) | 6 (85.7%) | 41 (68.3%) | 1 (33.3%) |
| Cyclosporine | 173 (81.6%) | 15 (60.0%) | 105 (89.0%) | 7 (100%) | 45 (75.0%) | 1 (33.3%) |
| Tacrolimus | 162 (76.4%) | 14 (56.0%) | 104 (88.9%) | 5 (71.4%) | 39 (65%) | 0 (0%) |
| Mycophenolate | 170 (80.2%) | 17 (68.0%) | 105 (89.7%) | 6 (85.7%) | 41 (68.3%) | 1 (33.3%) |
| Antihypertensives | ||||||
| Captopril | 181 (85.4%) | 22 (88.0%) | 99 (84.6%) | 6 (85.7%) | 52 (86.7%) | 2 (66.7%) |
| Enalapril | 200 (94.3%) | 22 (88.0%) | 110 (94.0%) | 6 (85.7%) | 59 (98.3%) | 3 (100%) |
| Nifedipine | 193 (91.0%) | 22 (88.0%) | 109 (93.2%) | 6 (85.7%) | 53 (88.3%) | 3 (100%) |
| Amlodipine | 195 (92.0%) | 22 (88.0%) | 110 (94.0%) | 6 (85.7%) | 54 (90.0%) | 3 (100%) |
| Other drugs | ||||||
| Furosemide | 191 (90.1%) | 22 (88.0%) | 106 (90.6%) | 7 (100%) | 54 (90.0%) | 3 (100%) |
| Albumin (20%–25%) | 186 (87.7%) | 18 (72.0%) | 108 (92.3%) | 7 (100%) | 53 (88.3%) | 1 (33.3%) |
| Trimethoprim-sulfamethoxazole | 195 (92.0%) | 25 (100%) | 103 (88.0%) | 6 (85.7%) | 58 (96.7%) | 3 (100%) |
The table describes the availability of basic medications used to treat children with kidney disease. The percentage of centers where the medications are available to the total number of centers that responded to the survey are reported.
Although these standard pediatric nephrology medications may be available in many countries, the ability of the patient to pay for the medications, unreliable supply chains, or both limited access to the medications (Figure 4). The need to export medications, lack of regular availability in public sector hospitals, availability as adult formulations or doses that were not suitable for children, drugs for kidney disease not being included in the country’s essential drug list, poor insurance coverage, and unfavorable health care policies were the most common reasons cited for the difficulty in obtaining medications even when they were available.
Figure 4.
Challenges with access to medications.
KRT
Ten centers (4.1%) in 7 countries did not offer any form of KRT, either dialysis (acute or chronic) or transplantation. However, the majority of these centers had locations within their country that they could send their patients to for KRT. Only 4 countries, Timor-Leste, American Samoa, and Tonga, report needing to transfer children out of the country for KRT.
Facilities for pediatric dialysis for acute kidney injury (AKI) were available in 200 of 217 centers (97%) in 53 countries. For dialytic management of AKI, manual PD (74%) was more commonly available than automated PD (43%) (Supplementary Table S2). Although almost half of the centers (mainly in Asia and Europe) had continuous KRT available, sustained low-efficiency dialysis was performed only in a quarter of the centers. Acute intermittent hemodialysis was available in 79% of centers.
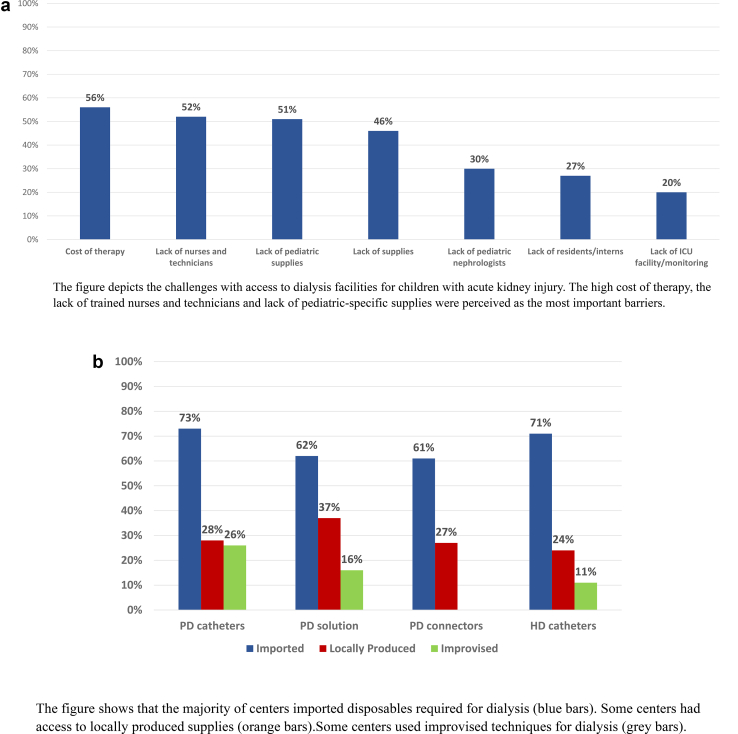
The cost of therapy was the major barrier to providing KRT for AKI even when it was available. Lack of trained nurses or technicians and nonavailability or difficulty in procuring pediatric-specific supplies for KRT were reasons reported in about 50% of centers as barriers to providing this care (Figure 5a).
Figure 5.
(a) Challenges with access to kidney replacement therapy for acute kidney injury (n = 217). (b) Availability of disposables for acute dialysis (n = 210).
Although commercially prepared and imported disposables were accessed by several centers, a large proportion of centers (24%–37%) reported local production, and 11% to 26% reported the use of improvised techniques (15) (Figure 5b). Rigid PD catheters were the only catheters available in 57 centers (26%).
Chronic PD was available in 147 centers (68%) and chronic hemodialysis in 165 centers (76%). Fewer centers in Africa (n = 7/24, 29%) and no centers in Oceania had chronic PD (Figure 2; Supplementary Table 2). Chronic hemodialysis was less available in Latin America (n = 41/62, 66%) when compared to other regions (82%) and not provided at all in Oceania (Figure 2). Nine centers report no access to chronic dialysis within their countries.
Pediatric kidney transplantation was available in about a third of centers (n = 72/217); however, again fewer centers in Africa (n = 6/24, 25%), Asia (n = 36/120, 30%), and no centers in Oceania offered transplantation. Among centers with kidney transplant facilities, a living-related transplantation program was present in 62 centers (94%), whereas a deceased donor program was present in 47 centers (71%). Twenty-nine centers in 21 countries reported not having the ability to perform pediatric kidney transplantation and needing to refer to centers outside of the country or having no center to refer patients to. Seven centers in 3 countries reported an inability to refer patients for transplants despite having transplantation services in other centers in their country.
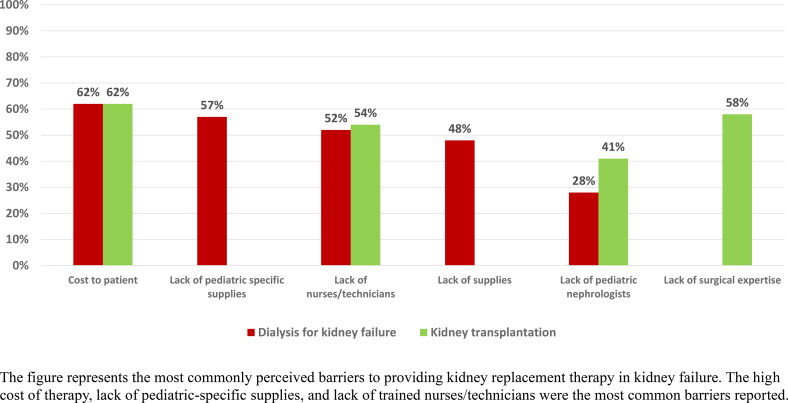
The cost of therapy and lack of pediatric-specific supplies were the major challenges for providing chronic dialysis, whereas the cost of therapy and lack of surgical expertise were the major challenges for providing kidney transplantation for children with kidney failure (Figure 6).
Figure 6.
Challenges with access to kidney replacement therapy/chronic dialysis for kidney failure (n = 210) and kidney transplantation (n = 186).
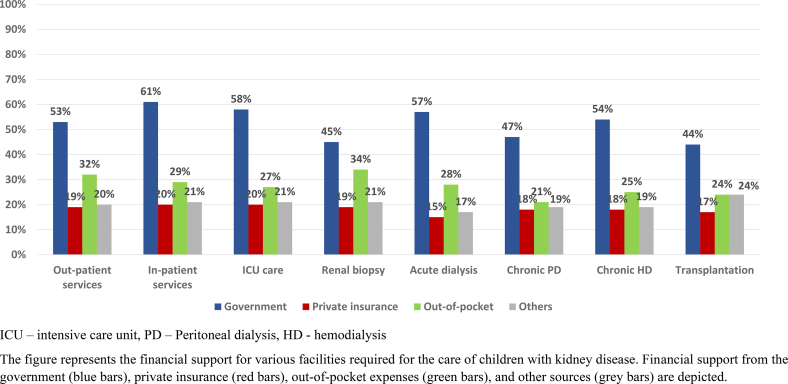
Funding for Pediatric Kidney Care Centers
Several funding models were reported, with 15 countries (24.2%) reporting multiple sources within the country. Two-thirds of centers, in 55 countries, were government-funded (n = 164, 66.9%). Thirty-three centers (13.5%) were privately funded, 15 (6.1%) were supported by a trust, 8 (3.3%) received support from other sources. Sixteen (6.5%) centers reported receiving funding from multiple sources. In most of the centers in Latin America (95%–100%) and all centers in Europe where chronic dialysis and kidney transplantation were available, it was supported by the government. However, in Africa and Asia, only 66 % of chronic dialysis centers were government-only supported, this increased to 90% in transplant centers. In about a third of centers, patients had to pay out-of-pocket for clinical services, including dialysis and transplantation. Private insurance was available to some patients in about 20% of centers and 20% of centers received support from trusts and other sources (Figure 7).
Figure 7.
Financial support for care for kidney disease in children (n = 207).
Challenges With Providing Chronic Care
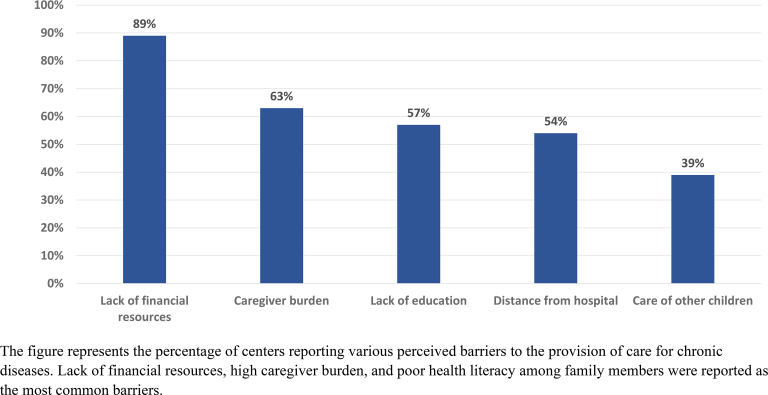
About 134 of 207 (64.7%) centers reported that some families opted to discontinue care for children with chronic diseases. Discontinuation of chronic care was opted for by some families in 21 centers (91.3%) in Africa, 80 centers (70.2%) in Asia, 3 centers (50%) in Europe, 28 centers (45.9%) in Latin America, and 2 centers (66.6%) in Oceania. Lack of family financial resources was reported as the reason for discontinuing care in about 90% of centers. High caregiver burden, lack of education among caregivers, and distance from the hospital were the other major reasons reported for discontinuation of care (Figure 8).
Figure 8.
Factors responsible for discontinuation of care in children with chronic disease (n = 207).
Discussion
To the best of our knowledge, this is the most comprehensive, pediatric-focused assessment of kidney care in LMICs with participation from countries covering about 88% of the LMICs population. This survey highlights the plethora of challenges in providing optimal care to children with kidney disease in LMICs and the regional disparities in the availability of resources. It describes the lack of pediatric-trained nurses, dialysis technicians, social workers, and nutritionists in some regions. Although basic diagnostic tests and medications were available in most centers, access to them was restricted by limited supplies and affordability. Regional disparities in availability, cost of therapy, and lack of pediatric-specific supplies were important barriers to providing dialysis to children with AKI. Access to chronic PD and kidney transplantation was limited by high costs, lack of consistent supply of disposables, and surgical expertise. The burden of out-of-pocket expenses was large and limited support from private insurance was available. Financial constraints forced some families of children with chronic diseases to opt for discontinuation of care in many centers.
A global survey of pediatric nephrologists found that 67% of respondents perceived a pediatric nephrologist workforce shortage. More severe shortages were perceived by those in regions with high numbers of LMICs.13 Our survey reported that even in centers that had pediatric nephrologists, adult nephrologists worked with them to provide care to children. In many countries, adult nephrologists, who lack training in pediatric-specific disease management and pediatrics in general, are tasked with providing pediatric nephrology care.5
A recent analysis of pediatric nephrology training in Africa emphasized the importance of training in regional centers and hands-on training in improving the provision of care in resource-limited regions.14 The focus placed on developing this training by IPNA and the International Society of Nephrology has resulted in more pediatric nephrology-trained physicians in LMICs and our ability to survey so many LMICs captures this success. However, many of these physicians are in groups of 1 or 2 pediatric nephrologists and the lack of institutional or government support is seen as the primary barrier to recruiting more pediatric nephrologists in regions such as Africa, Asia, the Middle East, and Latin America.13 This lack of systemic nephrology support has been well-described in LMICs.15,16
Poor systemic support was further highlighted by the lack of allied health professionals such as nurses, dietitians, and dialysis technicians, all critical components of pediatric kidney care. To provide sustainable care to children in these countries, efforts need to be made by governments and international organizations to develop capacity in pediatric nephrology care. It may fall on physician-based associations to enhance their nonphysician memberships with the interest of fostering networks to support the development of these disciplines in LMICs.
The ability to access diagnostic and therapeutic resources is critical to pediatric nephrology care. This survey and a previous survey of IPNA members17 showed that basic diagnostics like urine analysis, ultrasound, and serum creatinine were available in most centers. However, specialty investigations required to diagnose common problems in children, such as fluoroscopy, histopathology, and immunofluorescence were not available in many centers.17 Our survey also highlighted that even when basic laboratory facilities were available, access was limited due to financial and logistical barriers. This is consistent with adult-centered studies which reported low affordability of basic diagnostics.18
Similarly, basic medications such as steroids and antihypertensive medications were not uniformly accessible even when they were available. In-country regional variations in access to medications have been described, with lower access in nontertiary care centers.19 Inefficient supply chains, lack of storage facilities, and inadequate numbers of health care workers were reported as the key barriers.20
Acute dialysis is a life-saving intervention, but our survey shows that the provision of acute dialysis in children is fraught with concerns both technical and financial. A global snapshot of the management of AKI showed that even when dialysis was indicated, it was not initiated in lower-income countries due to financial constraints and a lack of trained staff.20 Pediatric dialysis units are scarce in low-income countries, with adult nephrologists providing dialysis for AKI in children due to the lack of pediatric nephrologists.21,22
Internationally, dialysis provision is very resource-intensive and this is complicated in low-income settings by erratic medical supplies, poor infrastructure, and lack of financial support. Our results support similar observations of improvised catheters and fluids being used in many centers due to a lack of access to standard equipment.14,22 Important initiatives such as the International Society of Nephrology 0by25 initiative23 and Saving Young Lives Program have enhanced workforce capacity in some regions and continued to expand particularly in low-income countries.23,24 However, knowledge needs to be partnered with the provision of a reliable supply of pediatric-specific equipment at reasonable costs that do not fall on the patient. Supporting local production of supplies required for dialysis will enhance availability and reduce costs.
Chronic dialysis for children entails additional challenges and we have shown that it is less frequently available than acute dialysis. Chronic dialysis facilities, even when available, are not accessible to children with kidney failure in LMICs, thereby highlighting the inequity of care for children with chronic kidney disease.2,14 PD, the preferred modality for chronic pediatric dialysis, is rarely available in LMICs. Lack of government funding for dialysis, especially PD, lack of medical and technical expertise, poor availability of pediatric-specific supplies, and poor access to transplantation were reported as important barriers in our study and others.2,5,25
Although transplantation is the best form of KRT, children with kidney failure have limited access to transplantation.3,5 Only a third of centers reported in the survey were able to provide kidney transplantation. Lack of expertise in medical and surgical aspects of pediatric transplantation, availability of transplantation only in a few tertiary centers which are inaccessible due to logistical issues, high costs of transplantation and posttransplant immunosuppression, poor financial support from the government, and poorly developed deceased donor programs were barriers across LMICs in our study, as in others3,10,26,27 Focused efforts to make kidney transplantation available and accessible to children are required in LMICs.
The outcome of a child with kidney failure is bleak in most resource-limited settings, with reports of a high mortality rate and a significant proportion abandoning treatment.11 We report that the lack of resources for kidney care and the poor financial support compel many families to abandon care for their children with chronic disease in LMICs. Health literacy of the family, socioeconomic status, and geographical remoteness have been reported as important barriers.6,28,29 Though unmeasured and poorly reported, it is implied that most of these children who abandon care succumb to their kidney disease.
The survey included low-income and middle-income countries (lower and upper middle income) and demonstrated that gross national income is not the sole determinant of health care. Many factors such as the proportion of GDP spent on health, health care policies, geographic isolation, government funding, insurance coverage, and health literacy are important factors that influence the availability of healthcare.
We recognize that this survey relied upon responses from centers where there were known pediatric nephrology providers and likely represents the best case scenario within a country and that in-country disparities may be overlooked. The findings of the survey are based on the responding physicians’ perspectives and the data provided is not verified at each center. The survey aimed at obtaining a bird’s eye view of the availability of resources for pediatric kidney care and details of each service or resource is not available. Even so, the survey identified widespread deficits and disparities in the provision of kidney care to children in LMICs. The impact of childhood kidney disease on health in adulthood should be underscored30 and our data can be used in informing policy development and action plans for addressing regional challenges and supporting IPNA in its effort to strengthen pediatric kidney care globally. Optimally, the survey will serve as a platform for regional and international collaborative efforts that address system-level and kidney disease-specific barriers, allowing for prioritization of resources focused on the needs of the population, and involving stakeholders to formulate solutions tailored to regional needs.31
In conclusion, the survey highlights a deficit in the workforce for the care of children with kidney disease in resource-constrained regions of the world. A wide gap exists in the availability, accessibility, and affordability of basic diagnostic, therapeutic, and financial resources in these regions. The survey emphasizes the urgent need for IPNA to collaborate with other global bodies to advocate for better health care facilities for children, advocate for equitable access to medications and dialysis, and appeal to policymakers to take measures to address disparities in health care resources and funding.
Disclosure
All the authors declared no competing interests.
Acknowledgments
We are grateful to Valerie Luyckx and Aminu Bello for their critical appraisal of the manuscript and intellectual contributions.
Abstract published: R. Erickson, N. Kamath, H. Safouh, G. Montini, M. Bonilla-Félix, Wcn23-0888 Pediatric Nephrology Resources in Low and Middle Income (LMI) Countries: A Survey from The IPNA Priorities in Low Resource Countries Committee (LRCC). Kidney Int Rep. 8(3); S178-S179. https://doi.org/10.1016/j.ekir.2023.02.398
Footnotes
Survey questionnaire.
Table S1. Distribution and response to the survey from low and middle-income countries.
Table S2. The availability of various modalities of kidney replacement therapy for acute kidney injury and kidney failure.
Supplementary Material
Survey questionnaire. Table S1. Distribution and response to the survey from low and middle-income countries. Table S2. The availability of various modalities of kidney replacement therapy for acute kidney injury and kidney failure.
References
- 1.Harambat J., Madden I. What is the true burden of chronic kidney disease in children worldwide? Pediatr Nephrol. 2023;38:1389–1393. doi: 10.1007/s00467-022-05816-7. [DOI] [PubMed] [Google Scholar]
- 2.International Society of Nephrology Global kidney health atlas 2023. www.theisn.org/global-atlas
- 3.International Society of Nephrology Global Kidney Health Atlas 2019. https://archive.theisn.org/global-atlas
- 4.James S.L., Abate D., Abate K.H. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lalji R., Francis A., Wong G., et al. Disparities in end-stage kidney disease care for children: a global survey. Kidney Int. 2020;98:527–532. doi: 10.1016/j.kint.2020.04.058. [DOI] [PubMed] [Google Scholar]
- 6.Lalji R., Francis A., Johnson D.W., McCulloch M. Health disparities in access to kidney replacement therapy amongst children and adolescents with end-stage kidney disease in low- and lower-middle-income countries. Kidney Int. 2020;97:463–465. doi: 10.1016/j.kint.2019.11.030. [DOI] [PubMed] [Google Scholar]
- 7.Harambat J., Van Stralen K.J., Kim J.J., Tizard E.J. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27:363–373. doi: 10.1007/s00467-011-1939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCulloch M., Luyckx V.A., Cullis B., et al. Challenges of access to kidney care for children in low-resource settings. Nat Rev Nephrol. 2021;17:33–45. doi: 10.1038/s41581-020-00338-7. [DOI] [PubMed] [Google Scholar]
- 9.Iyengar A., Mcculloch M.I. Paediatric kidney transplantation in under-resourced regions-a panoramic view. Pediatr Nephrol. 2022;37:745–755. doi: 10.1007/s00467-021-05070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sethi S.K., Sinha R., Rohatgi S., Kher V., Iyengar A., Bagga A. Pediatric renal transplant practices in India. Pediatr Transplant. 2017;21 doi: 10.1111/petr.12892. [DOI] [PubMed] [Google Scholar]
- 11.Ashuntantang G., Osafo C., Olowu W.A., et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5:e408–e417. doi: 10.1016/S2214-109X(17)30057-8. [DOI] [PubMed] [Google Scholar]
- 12.World bank Group World Bank Open Data. https://data.worldbank.org
- 13.Glenn D., Ocegueda S., Nazareth M., et al. The global pediatric nephrology workforce: a survey of the International Pediatric Nephrology Association. BMC Nephrol. 2016;17:83. doi: 10.1186/s12882-016-0299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nourse P., Cullis B., Finkelstein F., et al. ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 Update (paediatrics) Perit Dial Int. 2021;41:139–157. doi: 10.1177/0896860820982120. [DOI] [PubMed] [Google Scholar]
- 15.McCulloch M.I., Argent A.C., Morrow B., et al. Lessons learned from regional training of paediatric nephrology fellows in Africa. Pediatr Nephrol. 2023;38:3757–3768. doi: 10.1007/s00467-023-06022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okpechi I.G., Bello A.K., Luyckx V.A., Wearne N., Swanepoel C.R., Jha V. Building optimal and sustainable kidney care in low resource settings: the role of healthcare systems. Nephrology (Carlton) 2021;26:948–960. doi: 10.1111/nep.13935. [DOI] [PubMed] [Google Scholar]
- 17.Banerjee S., Kamath N., Antwi S., Bonilla-Felix M. Paediatric nephrology in under-resourced areas. Pediatr Nephrol. 2022;37:959–972. doi: 10.1007/s00467-021-05059-y. [DOI] [PubMed] [Google Scholar]
- 18.Tummalapalli S.L., Shlipak M.G., Damster S., et al. Availability and affordability of kidney health laboratory tests around the globe. Am J Nephrol. 2021;51:959–965. doi: 10.1159/000511848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francis A., Abdul Hafidz M.I., Ekrikpo U.E., et al. Barriers to accessing essential medicines for kidney disease in low- and lower-middle-income countries. Kidney Int. 2022;102:969–973. doi: 10.1016/j.kint.2022.07.029. [DOI] [PubMed] [Google Scholar]
- 20.Macedo E., Cerdá J., Hingorani S., et al. Recognition and management of acute kidney injury in children: the ISN 0by25 global snapshot study. PLoS One. 2018;13:1–15. doi: 10.1371/journal.pone.0196586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olowu W.A., Niang A., Osafo C., et al. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2016;4:e242–e250. doi: 10.1016/S2214-109X(15)00322-8. [DOI] [PubMed] [Google Scholar]
- 22.Raina R., Chauvin A.M., Bunchman T., et al. Treatment of AKI in developing and developed countries: an international survey of pediatric dialysis modalities. PLoS One. 2017;12 doi: 10.1371/journal.pone.0178233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehta R.L., Cerdá J., Burdmann E.A., et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385:2616–2643. doi: 10.1016/S0140-6736(15)60126-X. [DOI] [PubMed] [Google Scholar]
- 24.Nkoy A.B., Ndiyo Y.M., Matoka T.T., et al. A promising pediatric peritoneal dialysis experience in a resource-limited setting with the support of saving young lives program. Perit Dial Int. 2020;40:504–508. doi: 10.1177/0896860819887286. [DOI] [PubMed] [Google Scholar]
- 25.Niang A., Iyengar A., Luyckx V.A. Hemodialysis versus peritoneal dialysis in resource-limited settings. Curr Opin Nephrol Hypertens. 2018;27:463–471. doi: 10.1097/MNH.0000000000000455. [DOI] [PubMed] [Google Scholar]
- 26.Hasan Rizvi S.A., Naqvi S.A., Hussain Z., et al. Renal transplantation in developing countries. Kidney Int Suppl. 2003;83:S96–S100. doi: 10.1046/j.1523-1755.63.s83.20.x. [DOI] [PubMed] [Google Scholar]
- 27.Spearman C.W.N., McCulloch M.I. Challenges for paediatric transplantation in Africa. Pediatr Transplant. 2014;18:668–674. doi: 10.1111/petr.12333. [DOI] [PubMed] [Google Scholar]
- 28.Pais P., Blydt-Hansen T.D., Michael Raj J.A., Dello Strologo L., Iyengar A. Low renal transplantation rates in children with end-stage kidney disease: a study of barriers in a low-resource setting. Pediatr Transplant. 2021;25 doi: 10.1111/petr.13867. [DOI] [PubMed] [Google Scholar]
- 29.Cao B., Adler J.T., Bababekov Y.J., Markmann J.F., Chang D.C., Yeh H. Pediatric kidney transplantation and mortality: distance to transplant center matters. Pediatr Transplant. 2018;22 doi: 10.1111/petr.13120. [DOI] [PubMed] [Google Scholar]
- 30.Bernardes R. de P., Bresolin N.L., Guimarães Penido M.G.M. Prevention of pediatric chronic kidney disease. Urology & Nephrology Open Access Journal. 2020;8:139–146. doi: 10.15406/unoaj.2020.08.00293. [DOI] [Google Scholar]
- 31.Luyckx V.A., Moosa M.R. Priority setting as an ethical imperative in managing global dialysis access and improving kidney care. Semin Nephrol. 2021;41:230–241. doi: 10.1016/j.semnephrol.2021.05.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey questionnaire. Table S1. Distribution and response to the survey from low and middle-income countries. Table S2. The availability of various modalities of kidney replacement therapy for acute kidney injury and kidney failure.