Abstract
Abstract
Background and objective
Pelvic organ prolapse (POP) affects 40% of women, with a 12%–19% lifetime surgical risk. Italy showed high practice variation in POP surgery, possibly impacting equity of access to healthcare services, a central goal of Beveridge-like health systems. According to the literature, unwarranted variation, influenced by physician attitudes or resource allocation, must be reduced. We aimed to identify determinants influencing women’s choice when asked whether they prefer surgical or conservative POP management.
Design, setting and population
In this nationwide prospective study, we distributed a Qualtrics questionnaire via social media to any Italian women over 18 years old who voluntarily decided to participate in the survey.
Intervention
A grade 3 POP scenario was presented. Women were asked how likely they would have surgery. Each woman randomly received only 1 question out of 11: 1 question was the reference question (‘How likely would you have surgery?’) while 10 questions contained a potential determinant influencing woman’s choice (‘How likely would you have surgery if…?’).
Outcome
The outcome was the chance of choosing surgery expressed as a percentage. We analysed the effect of each factor on the outcome by using adjusted beta regression models.
Results
Respondents (n=222) opted for surgery with a median probability of 61.5%. Factors significantly increasing the chance of choosing surgery were advice from physicians, the presence of a trusted physician during hospitalisation, surgical approach with low complication rates, uterine-sparing surgery, the absence of postoperative abdominal scars and nearby hospital.
Conclusions
Our findings provide health managers and policy-makers with new evidence to better understand women’s decision-making and partly capture the determinants of unwarranted variation. These inputs may also be used as attributes for a future discrete choice experiment.
Keywords: urogynaecology, health services, public health, qualitative research
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study explores women’s preferences in pelvic organ prolapse (POP) management in Italy by using data from an online survey developed with expert physicians, validated through a convenient pilot sample and administered to the general population of women.
The findings of this study rely on a strong methodology, based on a randomisation technique for the initial question that allowed for providing a foundation for drawing hypotheses and potential testing through subsequent survey studies.
Results rely on strong statistical methods such as adjusted regression models and multiple imputation tools.
However, the study is prone to a self-selection bias since women voluntarily joined the survey, thus resulting in participants who were younger, more educated and of higher socioeconomic status than the typical POP-affected population.
Finally, there might have been additional factors potentially influencing the women’s choice for surgery that we have not considered, such as the impact on sexual function or the role of minimally invasive surgery.
Introduction
Pelvic floor dysfunctions are very common among elderly women, with a continuously increasing incidence related to the growing life expectancy. These conditions deteriorate from the menopause due to the related endocrine modifications and the ageing process, leading to negative consequences on quality of life, daily functionality and social interactions. Pelvic organ prolapse (POP), defined as the downward descent of pelvic organs towards the vagina, affects up to 40% of women, with a 12%–19% lifetime surgical risk.1 2 POP is not a life-threatening disease but has no self-limited course, so often the decision for surgery depends on women’s choices, preferences, needs and symptoms.3 4
Conservative management strategies for POP offer non-surgical alternatives aimed at alleviating symptoms and enhancing the well-being of affected individuals. These approaches include the use of pessaries to support the prolapsed organs, lifestyle modifications such as weight management and dietary adjustments, patient education and support groups.5 Despite the benefits of conservative treatment, 30% of women will undergo surgery within 1–2 years.6 On the other hand, POP surgery consists of various surgical procedures designed to anatomically repair and restore pelvic organ support, thus providing long-term relief from POP-related symptoms and renewing the structural integrity of the pelvic floor.7
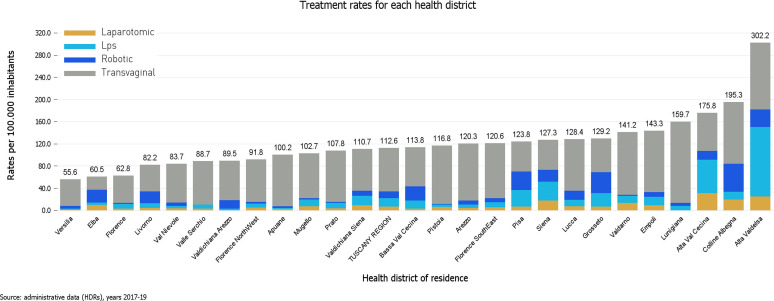
POP surgery is one of the most frequent elective surgical procedures in Western Countries: in the UK, 20% of women on the waiting lists for major gynaecological surgery suffer from POP.8 POP surgery is subject to practise variation since there are no clear and uniform indications for surgical treatment. In fact, a survey-based study on members of the International Urogynecological Association showed that much of the practice patterns in the treatment of POP depended on academic affiliation and geographic location.9 In addition, the spread of new technologies—such as robotic surgery—may exacerbate practice variation, as it may precede a robust cost-effectiveness evaluation, thus providing surgical options that are not consistently embraced by physicians.10 As a matter of fact, high regional variation in POP surgical practice has been documented in Tuscany, Italy (figure 1). However, between-hospital differences could explain only part of such variation.11
Figure 1. Variation in POP treatment rates across the 26 health districts of the Tuscany Region, Italy, with a 5.4-fold difference between the health districts with highest and the lowest treatment rates (Ferrari et al32). POP, pelvic organ prolapse.
According to JE Wennberg, variation in elective surgery is mainly due to supply-sensitive factors (use influenced by the resource allocation) and preference-sensitive factors (choice determined by patient’s and/or physician’s preferences).12 Variation is considered as unwarranted when it is not justified by real differences in patients’ needs, but rather by physicians’ attitudes and prescribing behaviour or different resource allocation. Unwarranted variation should be reduced, as it conflicts with the increasingly emerging patient-centred medical approach and the three pillars of public health systems pursuing universal coverage: quality, equity and sustainability.13
However, to define variation as unwarranted, a more comprehensive understanding of women’s decision-making process is needed.12 Since very little evidence is available from the literature about this topic, in this article, we aimed to explore the main determinants of practice variation at the woman’s level when asked whether she potentially prefers surgical or conservative management of POP. This may help policy-makers, health managers and researchers intercept patients’ opinions, choices and preferences, thereby providing new insights into the potential causes of unwarranted variation and guiding resource allocation to align health goals with women’s needs.14
Methods
Study design and setting
This was a survey-based prospective study which was carried out in Italy. The Italian National Health Service represents a Beveridge-style healthcare framework characterised by the provision of comprehensive and cost-free healthcare coverage to all citizens. This system adheres to a decentralised paradigm, whereby the central government assumes responsibility for establishing overarching financial prerequisites and objectives, as well as guaranteeing the equitable distribution of healthcare services throughout the nation. In contrast, individual regions are entrusted with the organisation and delivery of healthcare services within their respective jurisdictions, enjoying a substantial degree of administrative, political, legislative and fiscal self-governance.
Participants and data source
In this survey-based prospective study, we implemented an online questionnaire using the Qualtrics Survey Tool (Qualtrics, Provo, Utah, USA). Participants from the general population were invited via social media with an electronic link to access the online survey. The link was disseminated through social channels and participants were kindly asked to forward the link in turn. Embedded in the link was a message explicitly stating that the questionnaire addressed any woman over 18 years old. By clicking the link, participants accessed the first page that described the purpose of the study, disclosed the authors’ affiliation and informed women of the complete anonymity of the data collected and the possibility of not answering questions and dropping out of the survey at any time. By clicking the ‘forward’ button, women provided their implicit consent to participate. At the end of the survey, a link to a Google Forms survey was provided to collect the email address to which the participant could be recontacted, without the email address being associated with the Qualtrics survey response.
We intentionally chose to enrol women from the general population rather than women at higher risk of or suffering from POP. This decision allowed us to identify factors influencing women’s choices at an early stage of the decision-making process before the disease manifested leading to medical consultation. By that time, a doctor might have already provided some input or guidance that could have somehow biased the decision-making process. As our specific research objective was to explore how determinants influencing women’s choices affected practice variations, we necessarily had to select this study population to answer our research question.
The questionnaire
The questionnaire presented women with a clinical scenario of grade 3 POP (with uterus protruding out of the vagina). The two therapeutic alternatives (surgery or conservative management) were offered. Also, their advantages and disadvantages were detailed, for instance, the questionnaire explained how conservative management allows for symptom alleviation or resolution in a good percentage of cases, but—unlike surgery—cannot guarantee correction of the anatomical defect. Women were then asked how likely from 1 to 99 they would decide to undergo surgery. Each woman received only 1 question out of 11 in a randomised manner and then received the other 10 questions without randomisation on a different webpage. Out of the 11 questions, 1 was the reference question containing no additional factors (‘How likely would you choose surgery?’) while the other 10 questions contained a factor possibly influencing the woman’s choice for surgery (‘How likely would you choose surgery if…?’). We also included as a control question ‘Would you use epidural analgesia during childbirth?’ to assess survey’s reliability (online supplemental table S1).
The 10 factors were advice from the gynaecologist, advice from the general practitioner (GP), advice from two physicians, presence of the trusted gynaecologist during hospitalisation, advice from friends or relatives, short postoperative recovery time, low risk of complications, uterine-sparing surgery, no abdominal scarring and short travel times. The first question was always randomised to avoid response bias, related to the inevitable influence of the answer to the first question on the answer to the following questions. However, women further received the other 10 questions in a non-randomised manner. At the end of the questionnaire, sociodemographic data of women were also collected.
The survey content (eg, specification of the clinical scenario, factors or determinants of choice, description of the two treatment alternatives) was developed through an extensive literature review which was performed through computerised databases including PubMed, Embase, Google Scholar and the Cochrane Library. However, there was very little, evidence on this specific topic, so we had to draw this information from previous articles addressing different clinical scenarios, diseases or treatments. To consolidate our choices, we further carried out a focus group with a team of gynaecologists from the Division of Obstetrics and Gynaecology at the University of Pisa, a leading centre in Italy for pelvic floor surgery. The focus group was conducted in the presence of five gynaecologists by two authors who acted as moderator and assistant moderator. For the focus group, researchers created a script with the topics to be addressed and the questions to be asked. Following this script, the moderator asked the gynaecologists to comment on the survey content and all the factors that had been selected, choosing the most relevant ones and discarding the less important ones. We also asked them if any descriptive detail or additional factors to be considered had been left out. The interviews were recorded, and the focus group data were analysed with content analysis.
Before disseminating the study, we sent via Google Form a preview of the questionnaire to a convenient sample of 33 women to validate it by determining whether the questionnaire was simple and easily understandable on a 1–5 scale. 97% of the women responded that the questionnaire was either well understandable (4 out of 5) or totally understandable (5 out of 5). We also asked women to indicate the most difficult parts of the text to be interpreted. Finally, we asked them whether they thought any of the determinants of choice we proposed were unnecessary, and whether they would propose other factors or determinants of choice that we had not considered. For instance, the factor ‘advice from two physicians’ was added following women’s advice.
Outcome and statistical analyses
The outcome of our study was the response to the first randomised question, which was expressed as a percentage from 1% to 99% (converted to a 0.01–0.99 scale). To explore the effect of each factor on the probability of choosing surgery compared with the situation in which woman receive no additional input, we modelled unadjusted and adjusted beta regression models. We used the probability of choice as the dependent variable, and the first randomised factor as the main independent variable.
Adjustment was performed using all the available sociodemographic data, and missing data were handled through chained equation multiple imputation, generating 10 imputed data sets (see table 1 and online supplemental table S2 for further information). As a subanalysis of the study, we also ran multilevel beta regression models for repeated measures to investigate the effect of each factor on the probability of choice within each single respondent, using the woman’s anonymous identifier as the higher-level grouping variable. Statistical analyses were carried out on Stata Software V.17.0 (StataCorp). Statistical significance was set at a p<0.05.
Table 1. Baseline characteristics of respondents (n=222).
| Age, median (IQR) | 44.5 (31.0–55.0) |
| Perceived health status, median (IQR) | 4.0 (4.0–4.0) |
| Education level, n (%) | |
| Elementary/middle school | 7 (3.3) |
| High school | 86 (41.1) |
| University | 116 (55.5) |
| Work condition, n (%) | |
| Employed | 117 (56.3) |
| Unemployed | 22 (10.6) |
| Student | 9 (4.3) |
| Health worker | 60 (28.8) |
| Children, n (%) | |
| No one | 76 (36.4) |
| Just one | 76 (36.4) |
| Two or more | 57 (27.3) |
| Physical activity, n (%) | |
| Never | 33 (15.9) |
| Sometimes | 111 (53.4) |
| Often | 64 (30.8) |
| Civil status, n (%) | |
| With partner | 172 (82.7) |
| Without partner | 36 (17.3) |
| Assumed family support, n (%) | |
| Excellent | 113 (54.1) |
| Good | 76 (36.4) |
| Poor | 20 (9.6) |
| Chronic diseases, n (%) | |
| No one | 148 (70.8) |
| Just one | 50 (23.9) |
| Two or more | 11 (5.3) |
| Urinary incontinence knowledge, n (%) | |
| No | 5 (2.4) |
| Yes | 190 (90.9) |
| Yes: affected | 14 (6.7) |
| Pelvic organ prolapse knowledge, n (%) | |
| No | 21 (10.0) |
| Yes | 179 (85.6) |
| Yes: affected | 9 (4.3) |
Missing data were handled by using chained equation multiple imputation, generating 10 imputed data sets. Multiple imputation is an iterative form of stochastic imputation that – —instead of filling in a single value – —uses the distribution of the observed data to estimate multiple values that reflect the uncertainty around the true (missing) value. We included in the multiple imputation model the dependent and independent variables of the regression models, and all women’s sociodemographic data.
Patient and public involvement
As described above, the public was involved in the pilot phase of the study (convenient sample). The pilot phase served (1) to check the clarity of the text (particularly, of the clinical scenario and treatment options); (2) to modify the text according to the women’s suggestions and (3) to confirm the determinants of choice selected through literature review and expert focus group and possibly suggest additional factors to be considered.
Results
Characteristics of respondents
As shown in table 1, we obtained 222 participants, with a response rate of 89% (250 women opened the link). The region of residence of our respondents is shown in online supplemental table S3. The median age of our study population was 44.5 years, and the median perceived health status was 4.0 (out of 5.0). More than half of women had a university degree and were employed. About 36% of women had no children while 64% had at least one child, and 80% of women lived with a partner. Half of our respondents reported that they did physical activity only occasionally and that they could receive excellent family support when needed. Around 70% of women had no chronic comorbidities. Finally, 85%–90% of respondents were aware of urinary incontinence and POP despite not suffering from it.
As shown in table 2, each of the 11 questions appeared as the first randomised factor for about 8%–10% of the women. In the overall population (n=222), the median probability of choosing surgical treatment was 61.5%, regardless of which of the 11 questions was asked first. However, women who had received the reference question without any factor (n=20) responded that they would have surgery with a median probability of 39% (online supplemental figure S1). This percentage rose to about 80% when women received, as input, advice for surgery from two physicians (n=18) or the presence of a referral hospital for POP surgery within a 20 min drive (n=17). A slightly lower probability (70%–75%) of choosing surgery was observed in women who were told that the intervention was recommended by their gynaecologist (n=18) and that the surgery ensured the lowest possible complication rates (n=23).
Table 2. All randomised factors and median probability of choosing surgery for each factor.
| Randomised factor | N (%) | Response to the first answer, median (IQR) |
| Any factor (all respondents) | 222 (100) | 61.5 (42.0–84.0) |
| Reference | 20 (9.0) | 39.0 (6.5–69.0) |
| Gynaecologist’s advice | 18 (8.1) | 75.5 (60.0–90.0) |
| General practitioner’s advice | 20 (9.0) | 60.0 (49.5–82.0) |
| Two physicians’ advice | 18 (8.1) | 79.5 (61.0–84.0) |
| Trusted physician’s presence | 20 (9.0) | 61.0 (50.0–75.5) |
| Friends/relatives’ advice | 23 (10.4) | 50.0 (28.0–52.0) |
| Short postsurgical recovery | 23 (10.4) | 61.0 (30.0–80.0) |
| Low complication rates | 23 (10.4) | 71.0 (60.0–90.0) |
| Uterine sparing surgery | 23 (10.4) | 62.0 (28.0–100.0) |
| No abdominal scars | 17 (7.7) | 65.0 (51.0–84.0) |
| Nearby hospital | 17 (7.7) | 80.0 (50.0–97.0) |
Women who answered the control question (n=203) stating that they would choose to use epidural analgesia during childbirth numbered 71 (32.0%), consistently with data provided by the 2022 regional reports of Tuscany (31.3%) and Emilia-Romagna (31.4%).15 16
Primary outcome
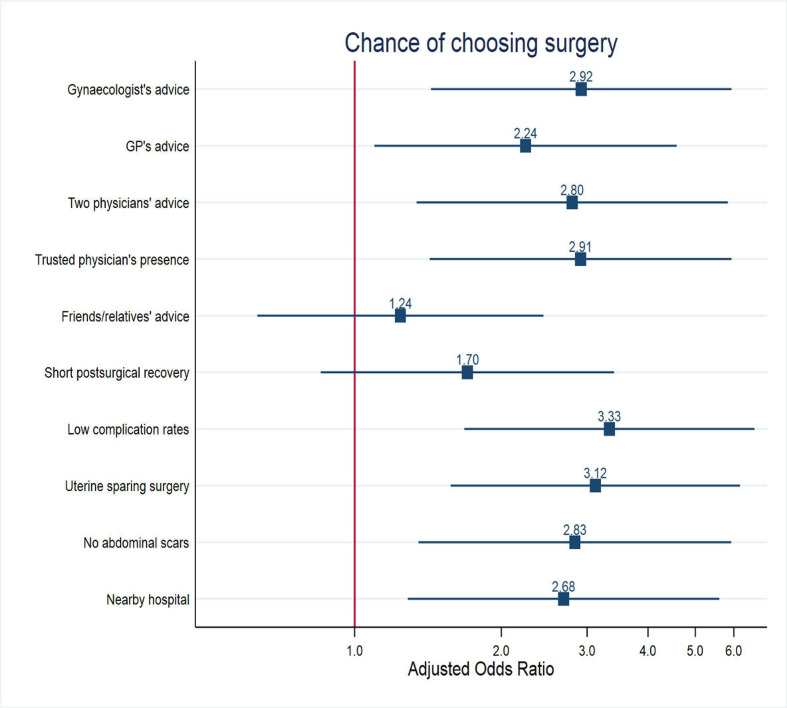
Both unadjusted and adjusted beta regression models (figure 2, online supplemental figure S2 and table S4) revealed that compared with the reference question in which women were given no further indication than those described in the scenario, all factors—except ‘advice from friends or relatives’ and ‘short postoperative recovery time’—significantly increased the likelihood of choosing surgical treatment. In the adjusted model, the highest OR (>3.0) was observed for the following factors: ‘surgery with the lowest possible complication rate’ and ‘uterine-sparing surgery’. Furthermore, the OR was significant also for the factors ‘presence of the trusted physician during hospitalisation for surgery’, ‘advice from gynaecologist’, ‘advice from two physicians’ and ‘absence of postoperative abdominal scars’. Finally, the factors ‘advice from general practitioner’ and ‘nearby referral hospital’, although significant, had the lowest effect.
Figure 2. Adjusted beta regression model for the primary outcome. The coefficients of the model are expressed in exponential form as ORs (and 95% CI). Please, see online supplemental table S4 for non-exponential coefficients. GP, general practitioner.
Subanalysis
Multilevel models for repeated measures (online supplemental figure S3) showed that, within the same subject, the factors that most increased the likelihood of choosing surgery were ‘advice from gynaecologist/two physicians’, ‘presence of trusted physician during hospitalisation’, ‘lowest possible complication rate’ and ‘uterine-sparing surgery’.
Discussion
Main findings
In this study, we presented a clinical scenario of grade 3 POP to women from the general population, with two different treatment alternatives (surgery or conservative management), and we asked them to express by what percentage they would decide to undergo surgery. We documented that the median probability of choosing surgery in our study population (n=222) was 61.5%. However, when receiving no further input than those given in the clinical scenario, women decided to have surgery with a 39% median probability. This percentage increased to ≈80% when the woman received specific inputs, such as the advice from two physicians and the presence of a nearby referral hospital. Previous clinical studies showed that the choice rate for POP surgery versus conservative management was slightly lower than in our study (from 33% to 44%)17 18 while a survey-based study reported a choice rate of 48%.19 Also, women who had a heavier symptom burden were found to be more likely to opt for surgery.20
Regression models showed that, compared with the situation in which the woman received no input, all the factors or determinants of choice considered (except two) resulted in a significant increase in the probability of choosing surgery. By far, the strongest effect, both in the overall population and within the same respondent, was observed for the following four factors: ‘advice from gynaecologist’, ‘presence of trusted physician during hospitalisation’, ‘surgery with lowest possible complication rate’ and ‘uterine-sparing surgery’.
Although there is little evidence from the literature on the same topic, our findings are consistent with previous articles that have explored the determinants influencing women’s preferences towards specific treatment options for gynaecological diseases. First, we showed that the role of the gynaecologist is crucial in guiding women’s decision-making. Similarly, Lyatoshinskaya et al reported that women from Vienna and Moscow would prefer to obtain information about POP from medical specialists.21 Also, women choosing between levonorgestrel intrauterine system and endometrial ablation for heavy menstrual bleeding preferred to be treated by a gynaecologist rather than the GP.22 Finally, Janda et al found that gynaecologists were the most influential source for women seeking information about hysterectomy.23
In line with our findings, uterus preservation has been reported to be a key determinant influencing women’s choices, but its influence depends greatly on how the anatomic success rate is communicated compared with hysterectomy-based surgery.24 For instance, van IJsselmuiden et al found that Dutch women were more likely in favour of uterus preservation over hysterectomy when assuming similar functional and anatomical outcomes for both procedures.25 Differently, a survey-based study by Urdzík et al showed that female gynaecologists from Czech Republic, Slovenia and Slovakia, would opt for hysterectomy as a treatment option when they were told that hysterectomy provided more satisfactory anatomical outcomes.26
We also found that surgery with a low risk of postoperative complications may drive women’s choice. This finding is coherent with previous articles, which however explored patient’s preferences between two different surgical techniques for POP rather than between surgical and conservative management.27 Consistently, for women seeking treatment for symptomatic uterine fibroids, repeat treatment and complications were found to be the leading factors in fostering surgical treatment options.28
We also showed that other factors such as the absence of postsurgical abdominal scars may increase the chance of choosing surgery. Similarly, a previous study showed that women would favour the laparoscopic approach for POP surgery due to the cosmetic appearance of the skin incision.29 The evidence that a favourable cosmetic outcome can influence women’s choices may foster, in the future, a wider diffusion of surgical techniques such as transvaginal natural orifice transluminal endoscopic surgery, which provide both anatomically and cosmetically satisfactory outcomes.30
As for travel times, there is a large body of previous literature demonstrating the influence of travel distances on the likelihood of receiving treatment.31 32 Similarly, we found that women, when told that a referral hospital for POP surgery was within a maximum of a 20 min car ride away, were more likely to choose surgery.
Limitations and strengths
This study presents some limitations. First, the study sample was selected from the general population using a link forwarded via social media, so the recruitment of participants was subject to a self-selection bias, whereby women who decided to participate had a lower average age than women who normally suffer from POP and had a higher educational level and socioeconomic status than the general population. Thus, our sample was not representative of the general population. In addition, the study was only in Italian so it was not possible to recruit women who were not proficient in the language. Also, we did not quantitatively investigate the readability of the text,33 but only asked qualitatively whether the clinical scenario was easily understandable, so some women may have responded without fully grasping the content of the study. Furthermore, there was no clear distinction between reconstructive and obliterative surgery among the determinants of choice, although there was a specific question about vaginal versus abdominal surgery. Finally, there may be additional determinants influencing the choice of the individual women that we have not considered, such as the impact on sexual function or the role of minimally invasive surgery.
However, despite its limitations, this study has multiple strengths. First, to the best of our knowledge, it was the first study to investigate women’s preferences for POP management while also trying to identify the factors that most influenced such preferences. These factors can thus be used for further investigations, for example, as attributes for a future discrete choice experiment (DCE). While the choice to include women from the general population instead of women at higher risk of or suffering from POP might seem to be a limitation of this study, it is instead justified by the rationale of our study. In fact, this allowed us to identify the determinants influencing women’s choices at an early stage before the condition occurred and the women had visited a health professional. By that time, the woman may have already received input that in some way may influence her choice of treatment. Since our main purpose was to investigate the effect of determinants influencing women’s choice on practice variation, we inevitably had to choose this type of population to answer the research question. Moreover, the study applied a robust methodology related to the randomisation of the first question (and the first factor) that allowed us to draw hypotheses on women preferences that could be tested through other survey studies. Finally, it was the first study to suggest a link between unwarranted practice variation in POP surgery and some determinants of choice at the individual level.
Implications
This study provides implications at different levels.
At the clinical level, the results from this study suggest that variation in POP surgery is strictly related to the physician advice. We found that less than half of women (around 40%) would choose to have surgery if no additional prompting or advice was provided. This percentage doubles (OR around 2.9–3.0) when external factors that influence a woman’s choice intervene.
This increase hinges on two core components related to the clinical dimension: the advice from gynaecologists and a proper information on clinical outcomes (complications, uterine sparing and abdominal scars). Thus, the influence of physicians’ attitudes and prescriptive behaviours, which are highly dependent on the surgical training and the affiliation, may have a great influence on women’s choice and, ultimately, on variation in treatment rates. For example, an excessive tendency to recommend surgery even when unnecessary could lead to unwarranted variation in terms of overuse. Hence, the need to establish more uniform international and national guidelines and recommendations, and to standardise care across different providers by developing defined care pathways.34
From an organisational point of view, our study revealed that, when women are aware of beneficial clinical outcomes (low complication rates, uterine-sparing surgery, favourable cosmetic outcomes), they are more likely to choose surgery. Therefore, to avoid non-justified underuse of surgery, a robust doctor–patient communication and a well-informed shared decision-making (SDM) process should be fostered. As a result, women would be equipped with comprehensive information about the spectrum of available treatment options to make choices aligned with their preferences and needs.
Indeed, previous literature has shown the positive effect of SDM, defined as the process of interacting with patients to reach informed and value-based choices, in reducing practice variations, improving the quality of decisions and preventing treatment overuse that patients may not welcome.35 36 Some authors have suggested that a tipping point is needed to truly put patients at the centre of healthcare as the norm of medical practice, although some issues remain unresolved, with a perception-reality gap.37 For example, SDM is a process that applies more to women with higher socioeconomic status, coming from high-income countries and having higher levels of literacy.
Also, SDM could be a process involving not only the doctor–patient relationship, but also family members, friends and social context.38 This is why, for instance, some authors might have not observed a significant decrease in the level of decision conflict with the addition of a decision aid to standard counselling for the management of POP.39 In any case, empirical studies have shown that decision aid, active support from nurses and the offer of reimbursement could both reduce unwarranted variation between hospitals and change variation patterns within hospitals,37 40 contributing to the ‘physiological’ variation rate that depends on patient preferences and should be valued. This has also recently been described for female pelvic floor reconstructive medicine and surgery.41
At the policy level, significant factor influencing women’s decisions regarding POP management is the proximity of a referral hospital. Travel times play a pivotal role, as women are more inclined to opt for surgery when such facilities are within a short car ride. In other words, the closer the hospital, the higher the probability of choosing POP surgery by women. This shows that even this surgical intervention is sensitive to the supply, thus highlighting the critical role of healthcare infrastructure and accessibility in shaping patient choices to avoid underuse of surgery. Policy-makers should consider this evidence when designing healthcare services and facilities. It should be valued if and why these women are forgoing the surgery. If it is for a settlement reason, other solutions have to be found in order to reduce the dreadful trade-off between access to care and financial sustainability.
Finally, at the academic level, this study paves the way for future investigations into patient preferences and decision-making processes. Findings of this paper provided essential preliminary knowledge to accurately specify the factors required for further advanced statistical analyses. For instance, the attributes analysed in this study may be used to design DCEs which are quasi-experimental survey acknowledged for their ability to elicit preferences and choices among alternative scenarios, making them a powerful tool in various fields.
Conclusion
In summary, this work provided valuable insights into the determinants influencing the individual women’s choice for surgical management of POP. If a woman who receives no input would have surgery in 40% of cases, but when receiving specific inputs (such as the determinants of choice analysed in this article) she would have surgery in 80% of cases, then this difference could explain some of the observed variation. The potential causes of such a variation have been explored at the user level, and they emerged to be mainly related to physicians’ advice, surgical outcomes and logistic factors such as travel distances. Health managers and policy-makers should consider these findings to better understand women’s decision-making and partly capture the determinants of unwarranted variation in terms of underuse or overuse, eventually ensuring that patients receive care aligned with their individual needs and preferences, regardless of their geographical location. The development of standardised guidelines and clinical pathways for pelvic prolapse may help tackle unwarranted practice variation to advance the cause of patient-centred, equitable, sustainable and effective healthcare services for women.
supplementary material
The Tuscany Region had no role in research question development, study design, data collection and analysis or writing and submitting the article for publication.
Footnotes
Funding: The data sources and the publication charges were funded as part of the research activities of the Sant’Anna School of Advanced Studies. Such activities were funded by the Regional Health Authority of Tuscany under a collaboration agreement with Sant’Anna School.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-084034).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: Participation in the survey was voluntary, and women gave informed consent before answering the questionnaire. They also provided consent to be recontacted for possible further questions. The study was exempt from ethics committee approval by the Institutional Review Board of Sant’Anna School of Advanced Studies since data were totally anonymous and voluntarily provided by the participants.
Data availability free text: The datasets used and/or analysed during the current study and the Stata scripts are available from the corresponding author on reasonable request.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Amerigo Ferrari, Email: amerigo.ferrari@santannapisa.it.
Nicola Bellè, Email: nicola.belle@santannapisa.it.
Andrea Giannini, Email: andrea.giannini@unipi.it.
Tommaso Simoncini, Email: tommaso.simoncini@unipi.it.
Milena Vainieri, Email: milena.vainieri@santannapisa.it.
Data availability statement
Data are available on reasonable request.
References
- 1.Smith FJ, Holman CDJ, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116:1096–100. doi: 10.1097/AOG.0b013e3181f73729. [DOI] [PubMed] [Google Scholar]
- 2.Collins SA, O’Shea M, Dykes N, et al. International urogynecological consultation: clinical definition of pelvic organ prolapse. Int Urogynecol J. 2021;32:2011–9. doi: 10.1007/s00192-021-04875-y. [DOI] [PubMed] [Google Scholar]
- 3.Mannella P, Giannini A, Russo E, et al. Personalizing pelvic floor reconstructive surgery in aging women. Maturitas. 2015;82:109–15. doi: 10.1016/j.maturitas.2015.06.032. [DOI] [PubMed] [Google Scholar]
- 4.Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027–38. doi: 10.1016/S0140-6736(07)60462-0. [DOI] [PubMed] [Google Scholar]
- 5.Hagen S, Thakar R. Conservative management of pelvic organ prolapse. Obstet Gynaecol Reprod Med. 2012;22:118–22. doi: 10.1016/j.ogrm.2012.02.003. [DOI] [Google Scholar]
- 6.Patnam R, Sripad AA, Dengler E, et al. Moving on: how many women opt for surgery after pessary use for prolapse? Female Pelvic Med Reconstr Surg . 2020;26:387–90. doi: 10.1097/SPV.0000000000000731. [DOI] [PubMed] [Google Scholar]
- 7.Hudson CO, Northington GM, Lyles RH, et al. Outcomes of robotic sacrocolpopexy: a systematic review and meta-analysis. Female Pelvic Med Reconstr Surg. 2014;20:252–60. doi: 10.1097/SPV.0000000000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan GA, Purandare NC, Ganeriwal SA, et al. Conservative management of pelvic organ prolapse: indian contribution. J Obstet Gynaecol India . 2021;71:3–10. doi: 10.1007/s13224-020-01406-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kammerer-Doak D, Svabik K, Bazi T. Variability in practice patterns in stress urinary incontinence and pelvic organ prolapse: results of an IUGA survey. Int Urogynecol J. 2017;28:735–44. doi: 10.1007/s00192-016-3174-6. [DOI] [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Reames BN, McCulloch P, et al. Understanding of regional variation in the use of surgery. Lancet. 2013;382:1121–9. doi: 10.1016/S0140-6736(13)61215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrari A, Giannini A, Seghieri C, et al. Regional practice variation in pelvic organ prolapse surgery in tuscany, italy: a retrospective cohort study on administrative health data. BMJ Open. 2023;13:e068145. doi: 10.1136/bmjopen-2022-068145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wennberg JE. Time to tackle unwarranted variations in practice. BMJ. 2011;342:bmj.d1513. doi: 10.1136/bmj.d1513. [DOI] [PubMed] [Google Scholar]
- 13.Lungu DA, Grillo Ruggieri T, Nuti S. Decision making tools for managing waiting times and treatment rates in elective surgery. BMC Health Serv Res. 2019;19:369. doi: 10.1186/s12913-019-4199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nuti S, De Rosis S, Bonciani M, et al. Rethinking healthcare performance evaluation systems towards the people-centredness approach: their pathways, their experience, their evaluation. Healthc Pap. 2017;17:56–64. doi: 10.12927/hcpap.2017.25408. [DOI] [PubMed] [Google Scholar]
- 15.Puglia M, Pacifici M, Voller F, et al. Gravidanza e parto in Toscana. 2022. https://www.epicentro.iss.it/territorio/toscana/pdf/Incifre_20_Gravidanza_parto_2022_rev_22_dic.pdf Available.
- 16.Perrone E, Formisano D, Gargano G, et al. La nascita in Emilia-Romagna: 20° Rapporto sui dati del Certificato di Assistenza al Parto (CedAP) 2022. https://salute.regione.emilia-romagna.it/siseps/sanita/cedap/files/la-nascita-in-emilia-romagna_rapporto-cedap-dati-anno-2022.pdf/@@download/file/La Available.
- 17.Sullivan SA, Davidson ERW, Bretschneider CE, et al. Patient characteristics associated with treatment choice for pelvic organ prolapse and urinary incontinence. Int Urogynecol J. 2016;27:811–6. doi: 10.1007/s00192-015-2907-2. [DOI] [PubMed] [Google Scholar]
- 18.Kapoor DS, Thakar R, Sultan AH, et al. Conservative versus surgical management of prolapse: what dictates patient choice? Int Urogynecol J. 2009;20:1157–61. doi: 10.1007/s00192-009-0930-x. [DOI] [PubMed] [Google Scholar]
- 19.Thys SD, Roovers JP, Geomini PM, et al. Do patients prefer a pessary or surgery as primary treatment for pelvic organ prolapse. Gynecol Obstet Invest. 2012;74:6–12. doi: 10.1159/000336634. [DOI] [PubMed] [Google Scholar]
- 20.Chan SSC, Cheung RYK, Yiu KW, et al. Symptoms, quality of life, and factors affecting women’s treatment decisions regarding pelvic organ prolapse. Int Urogynecol J. 2012;23:1027–33. doi: 10.1007/s00192-012-1698-y. [DOI] [PubMed] [Google Scholar]
- 21.Lyatoshinskaya P, Gumina D, Popov A, et al. Knowledge of pelvic organ prolapse in patients and their information-seeking preferences: comparing vienna and moscow. Int Urogynecol J. 2016;27:1673–80. doi: 10.1007/s00192-016-3018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Brink MJ, Beelen P, Herman MC, et al. Women’s preferences for the levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding. Eur J Obstet Gynecol Reprod Biol. 2018;228:143–7. doi: 10.1016/j.ejogrb.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 23.Janda M, Armfield NR, Page K, et al. Factors influencing women’s decision making in hysterectomy. Patient Educ Couns. 2018;101:504–10. doi: 10.1016/j.pec.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209:S0002-9378(13)00821-1. doi: 10.1016/j.ajog.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 25.van IJsselmuiden MN, Detollenaere RJ, Gerritse MBE, et al. Dutch women’s attitudes towards hysterectomy and uterus preservation in surgical treatment of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2018;220:79–83. doi: 10.1016/j.ejogrb.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 26.Urdzík P, Kalis V, Blaganje M, et al. Pelvic organ prolapse and uterine preservation: a survey of female gynecologists (POP-UP survey) BMC Womens Health. 2020;20:241. doi: 10.1186/s12905-020-01105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schulten SFM, Essers B, Notten KJB, et al. Patient’s preference for sacrospinous hysteropexy or modified manchester operation: A discrete choice experiment. BJOG. 2023;130:99–106. doi: 10.1111/1471-0528.17280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Babalola O, Gebben D, Tarver ME, et al. Patient preferences regarding surgical treatment methods for symptomatic uterine fibroids. Ther Innov Regul Sci. 2023;57:976–86. doi: 10.1007/s43441-023-00525-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noor N, Rahimi S, Pereira E, et al. Patient preferences for abdominal incisions used for pelvic organ prolapse surgery. Female Pelvic Med Reconstr Surg. 2015;21:348–54. doi: 10.1097/SPV.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 30.Interdonato ML, Scollo P, Bignardi T, et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery: an italian initial experience. Front Med (Lausanne) 2022;9:1018232.:1018232. doi: 10.3389/fmed.2022.1018232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunivan GC, Fairchild PS, Cichowski SB, et al. The association between distances traveled for care and treatment choices for pelvic floor disorders in a rural southwestern population. J Health Dispar Res Pract. 2014;7:23–32. [PMC free article] [PubMed] [Google Scholar]
- 32.Ferrari A, Seghieri C, Giannini A, et al. Driving time drives the hospital choice: choice models for pelvic organ prolapse surgery in italy. Eur J Health Econ . 2023;24:1575–86. doi: 10.1007/s10198-022-01563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferrari A, Pirrotta L, Bonciani M, et al. Higher readability of institutional websites drives the correct fruition of the abortion pathway: A cross-sectional study. PLoS One. 2022;17:e0277342. doi: 10.1371/journal.pone.0277342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caldwell L, Papermaster AE, Halder GE, et al. Evidence-based pelvic floor disorder care pathways optimize shared decision making between patients and surgeons. Int Urogynecol J. 2022;33:2841–7. doi: 10.1007/s00192-021-05021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Health Aff (Millwood) 2004;23:VAR–63. doi: 10.1377/hlthaff.var.63. [DOI] [PubMed] [Google Scholar]
- 36.O’Connor AM, Wennberg JE, Legare F, et al. Toward the ‘tipping point’: decision aids and informed patient choice. Health Aff (Millwood) 2007;26:716–25. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- 37.Stiggelbout AM, Van der Weijden T, De Wit MPT, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:bmj.e256. doi: 10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- 38.Greer AL, Goodwin JS, Freeman JL, et al. Bringing the patient back in. guidelines, practice variations, and the social context of medical practice. Int J Technol Assess Health Care. 2002;18:747–61. doi: 10.1017/s0266462302000569. [DOI] [PubMed] [Google Scholar]
- 39.Brazell HD, O’Sullivan DM, Forrest A, et al. Effect of a decision aid on decision making for the treatment of pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2015;21:231–5. doi: 10.1097/SPV.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 40.Brabers AEM, van Dijk L, Groenewegen PP, et al. Does A strategy to promote shared decision-making reduce medical practice variation in the choice of either single or double embryo transfer after in vitro fertilisation? A secondary analysis of A randomised controlled trial. BMJ Open. 2016;6:e010894. doi: 10.1136/bmjopen-2015-010894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ossin DA, Carter EC, Cartwright R, et al. Shared decision-making in urology and female pelvic floor medicine and reconstructive surgery. Nat Rev Urol. 2022;19:161–70. doi: 10.1038/s41585-021-00551-4. [DOI] [PubMed] [Google Scholar]