Abstract
Background
Acupuncture is commonly undertaken during an assisted reproductive technology (ART) cycle although its role in improving live birth and pregnancy rates is unclear.
Objectives
To determine the effectiveness and safety of acupuncture as an adjunct to ART cycles for male and female subfertility.
Search methods
All reports which described randomised controlled trials of acupuncture in assisted conception were obtained through searches of the Menstrual Disorders and Subfertility Group Specialised Register, CENTRAL, Ovid MEDLINE, EMBASE, CINAHL (Cumulative Index to Nursing & Allied Health Literature), AMED , www.clinicaltrials.gov (all from inception to July 2013), National Research Register, and the Chinese clinical trial database (all to November 2012).
Selection criteria
Randomised controlled trials of acupuncture for couples who were undergoing ART, comparing acupuncture treatment alone or acupuncture with concurrent ART versus no treatment, placebo or sham acupuncture plus ART for the treatment of primary and secondary infertility. Women with medical illness that was deemed to contraindicate ART or acupuncture were excluded.
Data collection and analysis
Twenty randomised controlled trials were included in the review and nine were excluded. Study selection, quality assessment and data extraction were performed independently by two review authors. Meta‐analysis was performed using odds ratio (OR) and 95% confidence intervals (CI). The outcome measures were live birth rate, clinical ongoing pregnancy rate, miscarriage rate, and any reported side effects of treatment. The quality of the evidence for the primary outcome (live birth) was rated using GRADE methods.
Main results
This updated meta‐analysis showed no evidence of overall benefit of acupuncture for improving live birth rate (LBR) regardless of whether acupuncture was performed around the time of oocyte retrieval (OR 0.87, 95% CI 0.59 to 1.29, 2 studies, n = 464, I2 = 0%, low quality evidence) or around the day of embryo transfer (ET) (OR 1.22, 95% CI 0.87 to 1.70, 8 studies, n = 2505, I2 = 69%, low quality evidence). There was no evidence that acupuncture had any effect on pregnancy or miscarriage rates, or had significant side effects.
Authors' conclusions
There is no evidence that acupuncture improves live birth or pregnancy rates in assisted conception.
Keywords: Female; Humans; Male; Pregnancy; Acupuncture Therapy; Live Birth; Pregnancy Rate; Reproductive Techniques, Assisted; Embryo Transfer; Oocyte Retrieval; Randomized Controlled Trials as Topic; Time Factors
Plain language summary
Acupuncture and assisted conception
Review question: does acupuncture improve the outcomes of assisted reproduction?
Background: one in seven couples suffer from subfertility and many will seek help in the form of assisted reproductive technology (ART). Although the use of acupuncture has gained popularity, the use of this traditional Chinese medical treatment in conjunction with ART treatments is still controversial. This review summarised the evidence from well designed studies and evaluated the effectiveness and safety of acupuncture in assisted conception.
Search date: the evidence is current to July 2013.
Study characteristics: there were 20 randomised controlled studies identified. Six studies compared acupuncture at the time of egg collection (912 women) and 14 studies compared acupuncture in assisted conception (3632 women). The studies were further divided into those which used placebo needles in their control groups versus those that had controls who did not undergo any treatment. All the studies identified involved participants undertaking in vitro fertilization (IVF); there were no studies reporting the effect of acupuncture in ovulation induction or intrauterine insemination.
Funding of included studies: no included studies had external funding.
Key results: there is no evidence of benefit for the use of acupuncture in participants undergoing assisted conception treatment around the time of embryo transfer or at egg collection in terms of improving the live birth rate, ongoing or clinical pregnancy rate. There is also no evidence that acupuncture has any effect on miscarriage rate or had significant side effects.
Quality of the evidence: overall, the results are not similar across the studies. This was due to different study designs including the use of different types of control groups that could have introduced bias. More research is needed before recommendations can be made, including studies in which some controls receive placebo needling and others receive no intervention.
Summary of findings
Summary of findings for the main comparison. Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture) for women undergoing ART.
| Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture) for women undergoing assisted reproductive technology (ART) | ||||||
| Population: women undergoing ART Intervention: Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture) | |||||
| Live birth rate | 357 per 1000 | 326 per 1000 (247 to 418) | OR 0.87 (0.59 to 1.29) | 464 (2 studies) | ⊕⊕⊝⊝ low1,2 | No significant difference in live birth rate was found between the two groups |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Neither study clearly reported method of random sequence generation, one did not clearly describe method of allocation concealment 2 Only two studies (n=464), wide confidence intervals.
Summary of findings 2. Acupuncture on the day of ET versus control for women undergoing ART.
| Acupuncture on the day of embryo transfer (ET) versus control for women undergoing assisted reproductive technology (ART) | ||||||
| Population: women undergoing ART Intervention: Acupuncture on the day of ET versus control (sham, placebo, no acupuncture) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture on the day of ET versus control | |||||
| Live birth rate | 281 per 1000 | 323 per 1000 (254 to 399) | OR 1.22 (0.87 to 1.7) | 2505 (8 studies) | ⊕⊕⊝⊝ low1,2,3 | No significant difference in live birth rate was found between the two groups |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Two studies did not describe method of random sequence generation; six did not clearly describe method of allocation concealment 2 High statistical heterogeneity (I‐squared =69%) 3 Wide confidence intervals
Background
Description of the condition
One in seven to 10 couples in industrialised countries suffer from subfertility (Boivin 2007; Schmidt 1995). Many will seek medical help in the form of assisted reproductive technologies (ART), including controlled ovarian stimulation (COS) with or without intrauterine insemination (IUI) and in vitro fertilisation (IVF) treatment. The use of acupuncture has increasing gained popularity (Fisher 1994; Klein 2012; Thomas 2001) although its use as an adjuvant treatment to assisted conception is still controversial (El‐Toukhy 2010; Huang 2011; Meldrum 2013).
Description of the intervention
Acupuncture is an integral part of traditional Chinese medicine (TCM) and can be dated back at least 3000 years. In Europe, from consumer surveys (Fisher 1994; Klein 2012; Thomas 2001) between 7% and 19% of the population report using acupuncture for various reasons, and studies have shown promising results for its efficacy in adult postoperative and chemotherapy induced nausea and vomiting (Garcia 2013; Holmer 2012; NIH Consensus 1998).
In its original form, acupuncture is based on the principles of TCM and involves the insertion of fine needles into the skin along the meridians, providing a means of altering the flow of energy through the body (Vickers 1999). In a typical treatment, between four to 10 points are needled for 10 to 30 minutes. Needles can be stimulated by manual twirling or with a small electric current, as electro‐acupuncture (EA). There have been few studies of the physiological effects of acupuncture on the male or female reproductive tract, although for many years acupuncture has been widely used as an adjuvant to ART. Opinion about the effectiveness of acupuncture in women undergoing assisted conception varies considerably. Some regard the traditional Chinese treatment as effective (Zheng 2012) whilst others consider acupuncture as primarily a placebo treatment (Meldrum 2013) or even as a treatment that is unscientific and futile (El‐Toukhy 2010). It is, therefore, critical to examine the current evidence available using stringent methodology and analysis to evaluate the effectiveness of acupuncture in couples undertaking ART.
How the intervention might work
The mechanisms of action of acupuncture are largely unknown. Its influence on plasma beta‐endorphin levels via the hypothalamic‐pituitary‐adrenal (HPA) axis (Chen 2004; Stener‐Victorin 2000; Stener‐Victorin 2001), on uterine artery blood flow (Stener‐Victorin 1996) and analgesic actions have been described (Stener‐Victorin 1999).
Why it is important to do this review
Given the controversy surrounding this topic, it is important to perform an up‐to‐date review so that subfertile couples, fertility practitioners and general practitioners are better informed of the benefits or harm of acupuncture in assisted conception.
Objectives
To determine the effectiveness and safety of acupuncture as an adjunct to ART cycles for male and female subfertility.
Methods
Criteria for considering studies for this review
Types of studies
Published and unpublished randomised controlled trials (RCTs) were included in the review. We excluded non‐randomised studies (for example studies with evidence of inadequate sequence generation such as alternate days, patient numbers) as they are associated with a high risk of bias. We did not include crossover trials with no first phase data.
Types of participants
Participants in the trials had to meet all the following criteria to be included in the review.
Inclusion criteria:
primary (subfertility in couples who have never conceived) or secondary subfertility (couples who have subfertility after previously having children);
women undergoing ART;
any type of acupuncture at any or all time points before, during, or after ART with the intention to improve the ART outcome.
Exclusion criteria:
participants with any medical illness deemed a contraindication for ART or acupuncture treatment;
quasi‐randomised controlled trials; or
crossover randomised controlled trials that did not provide pre‐crossover data.
Types of interventions
RCTs comparing acupuncture treatment of participants (men or women, or both) versus no treatment, placebo or sham acupuncture during controlled ovarian stimulation (COS) with or without artificial stimulation by partner (± artificial insemination by husband (AIH)), IVF, or frozen‐thawed embryo transfer (FET) treatment were considered.
We included studies using either traditional acupuncture, in which needles were inserted in classical meridian points, or contemporary acupuncture in which the needles were inserted in non‐meridian or trigger points. The source of stimulation could be the hand, fine needle, moxibustion with warming needle, or electrical stimulation. We excluded studies of acupuncture treatment without needling, such as point injection, acupressure, laser acupuncture, tap‐pricking, or cupping on pricked superficial blood vessels. We excluded trials comparing different acupuncture treatments alone.
The timing of acupuncture treatment was generally either around the time of oocyte retrieval or around the time of embryo transfer (ET) (a few days before, the day of, and a few days after).
Needling in the control groups could either be with a sham needle (for example Streitberger placebo needle, Asiamed, Pullach, Germany, where skin penetration does not occur because the tip of the needle is blunted) or normal acupuncture needles, needling an area not recommended by TCM practitioners for fertility treatment. The other type of control group had no needling treatment.
Specific interventions to be considered:
acupuncture + ART versus no treatment, placebo, sham acupuncture + ART; i.e. all women received ART;
acupuncture alone versus no treatment, placebo, sham acupuncture + ART;
acupuncture versus acupuncture + ART.
Types of outcome measures
Primary outcomes
1. Live birth rate, defined as delivery of a live fetus after 20 completed weeks gestational age
Secondary outcomes
1. Ongoing pregnancy rate, defined as evidence of a gestational sac with fetal heart motion at greater than 12 weeks (12 to 18 weeks), confirmed with ultrasound
2. Clinical pregnancy rate, defined as evidence of a gestational sac with fetal heart motion measured at seven to eight weeks, confirmed with ultrasound
3. Adverse events including miscarriage, ectopic pregnancy, fetal abnormalities, side effects, ovarian hyperstimulation syndrome (OHSS) and infection
All rates were per woman randomised.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases, trials registers and web sites.
Menstrual Disorders and Subfertility Group (MDSG) Specialised Register (inception to 22.7.13).
Ovid Cochrane Central Register of Controlled Trials (CENTRAL) (inception to 22.7.13).
Ovid MEDLINE® In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE® (inception to22.7.13).
Ovid EMBASE (01.01.10 to 22.7.13). EMBASE was only searched for recent records as the UK Cochrane Centre has handsearched EMBASE to this point and these trials are already in CENTRAL.
Ovid PsycINFO (inception to 22.7.13).
Ovid AMED (inception to 22.7.13).
Other electronic sources of trials included:
Database of Abstracts of Reviews of Effects (DARE) in The Cochrane Library (http://www.cochrane.org/index.htm);
ClinicalTrials.gov (http://clinicaltrials.gov/ct2/home);
World Health Organization International Clinical Trials Registry Platform search portal (http://apps.who.int/trialsearch/);
OpenSigle for Grey literature from Europe (http://opensigle.inist.fr/);
China Academic Journal Electronic full text Database in China National Knowledge Infrastructure;
Index to Chinese Periodical Literature.
There was no language restriction in these searches. The search strings are in the appendices.
Searching other resources
We also handsearched reference lists of articles retrieved by the search and contacted experts in the field to obtain additional data when required. We handsearched relevant journals and conference abstracts that are not covered in the MDSG register, in liaison with the Trials Search Co‐ordinator.
Data collection and analysis
Selection of studies
After an initial screening of titles and abstracts that were retrieved by the search, conducted by YC and SD, the full texts of all potentially eligible studies were retrieved. Two review authors (YC and SD) independently examined these full text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review. We corresponded with study investigators to clarify study data and eligibility. Disagreements as to study eligibility were resolved by discussion without requiring referral to a third review author (WL). Study investigators were contacted for further data on methods or results, as required.
The selection process is documented with a PRISMA flow chart in Figure 1.
1.
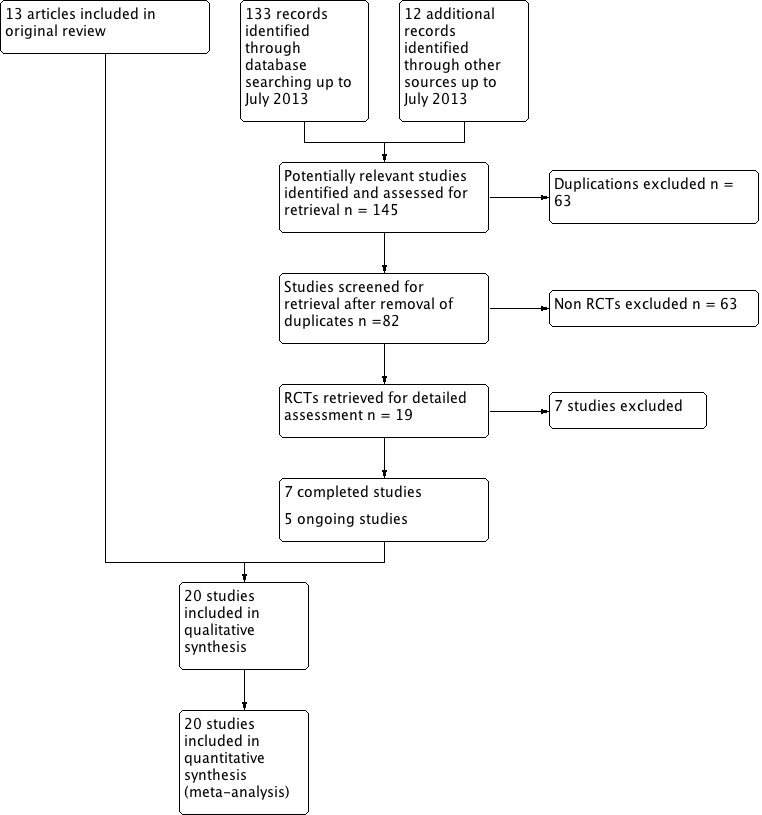
Study selection PRISMA flow diagram.
Data extraction and management
Two review authors (YC and SD) independently extracted data and assessed trial quality using forms designed according to Cochrane guidelines. Disagreements as to study eligibility were resolved by discussion without requiring referral to a third review author (WL). Where studies had multiple publications, the main trial report was used as the reference and additional details were derived from secondary papers. We corresponded with study investigators to clarify further data on methods and results.
Assessment of risk of bias in included studies
The included studies were assessed for risk of bias using the Cochrane risk of bias assessment tool (Cochrane Handbook for Systematic Reviews of Interventions Version 5.1) to assess the following domains: random sequence generation; allocation concealment; blinding; incomplete outcome data; selective reporting; and other bias.
Two authors (YC and SD) independently assessed these six domains, with any disagreements resolved by consensus or by discussion with the third author (WL).
As this was a review of surgical studies, where blinding was not possible, absence of blinding was not considered a significant source of bias. Risk of bias assessment is summarised (Figure 2 and Figure 3).
2.
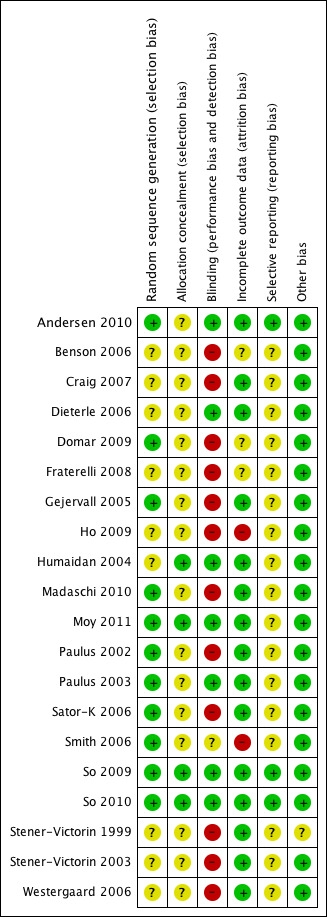
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
3.
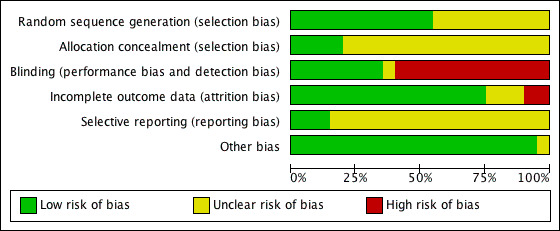
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
We took care to search for within trial selective reporting.
Measures of treatment effect
We performed statistical analysis in accordance with the guidelines and methods developed by The Cochrane Collaboration (Higgins 2011). All data were dichotomous. We expressed results for each study as odds ratio (OR) with 95% confidence interval (CI).
Unit of analysis issues
The unit of analysis was per participant and not per cycle. Multiple live births were counted as one live birth event.
Dealing with missing data
The data was analysed on an intention‐to‐treat basis and we have attempted to obtain missing data from the original trialists. Where these were unobtainable, imputation of individual values was undertaken for the primary outcomes only. Live births were assumed not to have occurred in participants without a reported outcome. For other outcomes, only the available data were analysed.
Assessment of heterogeneity
Heterogeneity was assessed using the I2 statistic, according to the guidelines set out in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). An I2 value greater than 50% indicated substantial heterogeneity.
Assessment of reporting biases
In view of the difficulty in detecting and correcting for publication bias and other reporting bias, we minimised their potential impact by ensuring a comprehensive search for eligible studies and by being aware of duplicated data. In the case where 10 or more studies were present in our analysis, we used a funnel plot to explore the possibility of a small study effect.
Data synthesis
Where possible, we pooled the outcomes and combined them for meta‐analysis. Dichotomous data for primary and secondary outcomes in studies that were sufficiently similar were combined with RevMan software using the Peto‐modified Mantel‐Haenszel method and fixed‐effect and random‐effects models in the following comparisons.
1. Acupuncture around the time of oocyte retrieval versus control (changed for consistency).
2. Acupuncture on the day of ET versus control.
We used a fixed‐effect model and examined heterogeneity between the results of different studies by inspecting the scatter in the data points, the overlap in their CIs, and more formally by checking the results of the Chi2 test and the I2 statistic. An I2 greater than 50% was taken to indicate substantial heterogeneity and in that case a random‐effects analysis was used.
Subgroup analysis and investigation of heterogeneity
The analysis was stratified to examine the separate evidence within the following subgroups:
1) studies with control groups that had sham or needling acupuncture;
2) studies with control groups that had no acupuncture.
Sensitivity analysis
None applicable
Results
Description of studies
See the tables Characteristics of included studies and Characteristics of excluded studies.
Results of the search
In the original review, 16 randomised trials were identified involving acupuncture and assisted conception; 13 met the inclusion criteria and three were excluded. In the updated search, 14 further randomised trials were identified, giving a total of 30. In total, 20 trials were included and nine were excluded; see Figure 1. Five ongoing studies were also identified (ACTRN12611000226909; IRCT201011275181N4; NCT00317317; NCT01449396; NCT01608048).
Included studies
Study design and setting
Twenty randomised controlled trials were included in this review. Four of the trial reports were abstracts (Benson 2006; Craig 2007; Fraterelli 2008; Paulus 2003). All 20 trials had a parallel design (Andersen 2010; Benson 2006; Craig 2007; Dieterle 2006; Domar 2009; Fraterelli 2008; Gejervall 2005; Ho 2009; Humaidan 2004; Madaschi 2010; Moy 2011; Paulus 2002; Paulus 2003; Sator‐K 2006; Smith 2006; So 2009; So 2010; Stener‐Victorin 1999; Stener‐Victorin 2003; Westergaard 2006).
Participants
The studies included a total of 4544 participants. All were women undergoing IVF and intracytoplasmic sperm injection (ICSI). The characteristics of the participants can be found in the table Characteristics of included studies.
Interventions
Six of the 20 trials were designed with the primary objective of assessing the effect of acupuncture as an analgesic during oocyte retrieval, but had pregnancy rate as one of the primary outcomes (Gejervall 2005; Ho 2009; Humaidan 2004; Smith 2006; Stener‐Victorin 1999; Stener‐Victorin 2003).
Fourteen of the 20 trials were designed to examine the fertility outcome of acupuncture performed around the time of ET (Andersen 2010; Benson 2006; Craig 2007; Dieterle 2006; Domar 2009; Fraterelli 2008; Madaschi 2010; Moy 2011; Paulus 2002; Paulus 2003; Smith 2006; So 2009; So 2010; Westergaard 2006), although two of these studies also included acupuncture two to three days after ET (Dieterle 2006; Westergaard 2006).
A summary of the acupuncture points used in the various studies is provided in Table 3.
1. Table 1. Summary of acupuncture points used.
| Acupuncture points | Craig 2007 | Westergaard 2006 | Dieterle 2006 | Paulus 2002Paulus 2003Andersen 2010; Domar 2009 | Madaschi 2010 | Ho 2009 | Moy 2011 | Smith 2006 | So 2009 | So 2010 | Stener‐Victorin 1999 | Stener‐Victorin 2003 | Gejervall 2005 | Humaidan 2004 | Sator‐K 2006 |
| Cv6 (Qi Hai) | Y (before ET) | Y | |||||||||||||
| Cx6 (Neiguan) | Y | Y | Y | ||||||||||||
| DU 20 (bai hui) |
Y | ||||||||||||||
| GV 20 (Baihui) | Y | Y (around ET and ET + 2) | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Liv 2 (Xingjian) | |||||||||||||||
| Liv 3 (Taichong) | Y | Y | Y | Y | |||||||||||
| LI 4 (Hegu) | Y | Y ( ET + 2) | Y (ET + 3) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |
| LI 10 (Shoushanli) | Y | ||||||||||||||
| LR 3 (Taichong) | Y | Y | Y | Y | |||||||||||
| LU 7 (lieque) |
Y | ||||||||||||||
| SP 6 (Sanyinjiao) | Y | Y ( ET + 2) | Y (ET + 3) | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| SP 8 (Diji) | Y | Y | Y | Y | Y | Y | Y | Y | |||||||
| SP 10 (Xuehai) | Y | Y | Y | Y | Y | Y | Y | Y | |||||||
| ST28 | Y | ||||||||||||||
| ST29 (Guilai) | Y | Y (ET and ET + 2) | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| ST36 (Zushanli) | Y | Y (ET + 3) | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| PC6 (Neiguan) | Y | Y | Y | Y | |||||||||||
| Ren 3 (Zhongji) | Y (ET + 2) | ||||||||||||||
| RN 4 (Guanyuan) | Y | Y | |||||||||||||
| RN6 (Qihai) | Y | Y | |||||||||||||
| K3 (Tai Xi) | Y (after ET) | ||||||||||||||
| K13 (Taxiu) | Y (ET + 3) | ||||||||||||||
| K1 11(Henggu) | Y | Y | |||||||||||||
| TE 5 (Weiguan) | Y | ||||||||||||||
| EX‐CA 1 (Zigong) | Y |
Control groups
No sham or needling:
eight studies had a no intervention control group (Benson 2006; Craig 2007; Domar 2009; Fraterelli 2008; Ho 2009; Madaschi 2010; Paulus 2002; Westergaard 2006);
five studies had control groups with conventional medical analgesia (Gejervall 2005; Humaidan 2004; Sator‐K 2006; Stener‐Victorin 1999; Stener‐Victorin 2003).
With sham or needling:
6/20 had a sham acupuncture needle control group using Strietberger sham acupuncture needles (Andersen 2010; Moy 2011; Paulus 2003; Smith 2006; So 2009; So 2010). Smith 2006 needled close to but not on real acupuncture points whilst Andersen 2010, Paulus 2003, So 2009 and So 2010 needled at the same acupoints as for the intervention group. Moy 2011 had acupuncture control groups that were needled at pre‐determined, non‐qui lines and auricular points not used for fertility;
one study had control groups with needling at non‐acupuncture points (Dieterle 2006) using normal acupuncture needles.
Outcomes
11/20 studies reported on live birth rate
11/20 studies reported on ongoing pregnancy rate
20/20 studies reported on clinical pregnancy rate
2/20 studies reported on multiple pregnancy rates
0/20 studies reported on rates of OHSS
9/20 studies reported on miscarriage rates
4/20 studies reported on side effects arising from use of acupuncture
Further details of the included studies can be found in the table Characteristics of included studies.
Excluded studies
Ten studies were excluded from the review for the following reasons:
Quintero 2004 was excluded due to the lack of first phase results in its crossover design;
Cui 2011 randomised women with polycystic ovary syndrome (PCOS) undergoing ET to either electro‐acupuncture (n = 34) or the control of no treatment (n = 32). However, the description of the randomisation process showed a high risk of bias with an inadequate randomisation process, based on odd or even numbers;
Chen 2004; Chen 2009; Cui 2007; Evans 2005; Feliciani 2011; Li 2009 and Omodei 2010 were excluded because they were apparently not randomised.
Chen 2012 reported on supplementary analgesia and improvement of adverse reactions induced by dolantin in oocyte retrieval, which were not outcoems of interest in the review
Characteristics of excluded studies can be found in the table Characteristics of excluded studies.
Risk of bias in included studies
Risk of bias assessment focused on six main domains: random sequence generation, allocation concealment, blinding, incomplete data outcome, selective reporting and other potential bias. Details of the findings can be found in the relevant risk of bias summary figures (Figure 2; Figure 3) and the Characteristics of included studies table.
Allocation
Sequence generation
Eleven trials were at low risk of selection bias related to sequence generation (Andersen 2010; ; Domar 2009; Gejervall 2005; Madaschi 2010; Moy 2011; Paulus 2002; Paulus 2003; Sator‐K 2006; Smith 2006; So 2009; So 2010; ). The other nine trials (Benson 2006; Craig 2007; Dieterle 2006; Fraterelli 2008; Ho 2009; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003; Westergaard 2006)were at an unclear risk due to a lack of detail of their methods of sequence generation.
Allocation concealment
Four trials were at low risk of bias for allocations concealment (Humaidan 2004; Moy 2011; So 2009; So 2010). The other sixteen trials (Andersen 2010; Benson 2006; Craig 2007; Dieterle 2006; Domar 2009; Fraterelli 2008; Gejervall 2005; Ho 2009; Madaschi 2010; Paulus 2002; Paulus 2003; Sator‐K 2006; Smith 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Westergaard 2006) were at unclear risk of bias for allocation concealment.
Blinding
Due to the nature of the studies, double blinding was often not possible. Eleven trials (Benson 2006; Craig 2007; Domar 2009; Gejervall 2005; Ho 2009; Madaschi 2010; Paulus 2002; Sator‐K 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Westergaard 2006) had no sham acupuncture intervention for the control group and so were at high risk of performance and detection bias. Five trials (Andersen 2010; Humaidan 2004; Paulus 2003; So 2009; So 2010) were low risk of performance and detection bias due to the use of sham acupuncture controls for blinding. Moy 2011 and Dieterle 2006 used an actual needling procedure on acupoints that were not considered to affect fertility and so were also low risk. Smith 2006 used sham acupuncture for the control groups but was deemed at an unclear risk of performance and detection bias as, after the 3rd session, 24 in the treatment group and 10 in the control group had guessed their allocation correctly.
Incomplete outcome data
Fifteen trials were at low risk of attrition bias without significant incomplete outcome data (Andersen 2010; Craig 2007; Dieterle 2006; Gejervall 2005; Humaidan 2004; Madaschi 2010; Moy 2011; Paulus 2002; Paulus 2003; Sator‐K 2006; So 2009; So 2010; Stener‐Victorin 1999; Stener‐Victorin 2003; Westergaard 2006). In three trials the risk was unclear as they did not report on the number of participants who completed the study (Benson 2006; Domar 2009; Fraterelli 2008). Ho 2009 had a high risk of attrition bias as 12 of the 26 control group participants dropped out of the trial. Smith 2006 also had a high risk of attrition bias as 36 women (15%) were withdrawn from the trial after randomisation.
Selective reporting
Three trials (Andersen 2010; So 2009; So 2010) were at low risk of reporting bias as they reported live birth data as prestated outcomes. Seven trials (Dieterle 2006; Humaidan 2004; Madaschi 2010; Paulus 2002; Paulus 2003; Stener‐Victorin 2003; Westergaard 2006) were at unclear risk of reporting bias as they reported live birth data but it was not a prestated outcome. The remaining 10 trials (Benson 2006; Craig 2007; Domar 2009; Fraterelli 2008; Gejervall 2005; Ho 2009; Moy 2011; Sator‐K 2006; Smith 2006; Stener‐Victorin 1999) did not report on live birth rate outcomes and so were also at unclear risk.
Other potential sources of bias
One study (Stener‐Victorin 1999) was rated as at unclear risk of other potential bias, related to co‐intervention in some women. The other studies were rated as at low risk of bias in this domain.
Effects of interventions
Overall, 20 studies were included in the meta‐analysis. The most commonly used acupuncture points were: GV 20, LI 4, SP6, and ST 29 (Table 3). A summary of the intended treatment with the various acupuncture points is given in Table 4.
2. Table 2. Summary of the treatment intended for the respective acupuncture points.
| Acupuncture points | Intended treatment |
| Cx6 (Neiguan) | Location: 2 cun above the transverse crease of the wrist, between the tendons of muscle palmaris longus and muscle flexor radialis. Indications Cardiac pain, palpitation, stuffy chest, pain in the hypochondriac region, stomach ache, nausea, vomiting, hiccups, mental disorders, epilepsy, insomnia, febrile diseases, irritability, malaria, contracture and pain in elbow and arm. Traditional action Opens the chest, regulates heart Qi and blood, regulates and clears the Triple Burner, calms the mind, regulates the terminal Yin, harmonizes the stomach. |
| GV 20 (Baihui) | Location: on the midline of the head, 7 cun directly above the posterior hairline, approximately on the midpoint of the line connecting the apexes of the two auricles. Indications Headache, vertigo, tinnitus, nasal obstruction, aphasia by apoplexy, coma, mental disorders, prolapse of the rectum and the uterus. Traditional action Clears the mind, lifts the spirits, tonifies yang, strengthens the ascending function of the spleen, eliminates interior wind, promotes resuscitation. |
| Liv 2 (Xingjian) | Location: on the dorsum of the foot between the 1st and 2nd toes, proximal to the margin of the web at the junction of the red and white skin. Point associations: Ying Spring point Fire point Actions and effects: Generally, clears LV Fire ‐ extreme irritability, red face, eyes, tongue. Clears heat from the lower Jiao ‐ burning urination. Useful for "true heat, false cold" ‐ lack of Qi flow to the extremities (cold hands or feet). |
| Liv 3 (Taichong) | Location: on the dorsum of the foot in a depression distal to the junctions of the 1st and 2nd metatarsal bones. Point associations: Shu Stream point Earth point Yuan source point Actions and effects: Generally, resolves stagnation and tonifies Yin ‐ balancing for all LV pathologies. LV Qi Stagnation, LV Yang Rising ‐ headaches, dizziness, canker sores. Eye issues ‐ blurred vision, red, swollen, painful eyes. Menstrual issues from deficient blood, Yin, Qi, LV Qi stagnation ‐ dysmenorrhea, amenorrhoea, PMS, breast tenderness. Genital issues ‐ pain and swelling, hernia, impotence, seminal emission. Stagnation in the middle warmer ‐ subcostal tension, chest or flank pain, swellings in the axillary region. Digestive issues from LV attacking ST/SP ‐ nausea, vomiting, constipation, diarrhoea with undigested food. Calming point ‐ anger, irritability, insomnia, anxiety. With LI 4, four gates treatment ‐ powerfully effects the flow of Qi and blood in the body. Location: On the dorsum of the foot in a depression distal to the junctions of the 1st and 2nd metatarsal bones. Point associations: Shu Stream point Earth point Yuan source point Actions and effects: Generally, resolves stagnation and tonifies Yin ‐ balancing for all LV pathologies. LV Qi Stagnation / LV Yang Rising ‐ headaches, dizziness, canker sores. Eye issues ‐ blurred vision, red, swollen, painful eyes. Menstrual issues from deficient blood, Yin, Qi a/or LV Qi stagnation ‐ dysmenorrhea, amenorrhoea, PMS, breast tenderness. Genital issues ‐ pain and swelling, hernia, impotence, seminal emission. Stagnation in the middle warmer ‐ subcostal tension, chest/flank pain, swellings in the axillary region. Digestive issues from LV attacking ST/SP ‐ nausea, vomiting, constipation, diarrhoea with undigested food. Calming point ‐ anger, irritability, insomnia, anxiety. With LI 4, four gates treatment ‐ powerfully effects the flow of Qi and blood in the body. |
| LI 4 (Hegu) | Location: in the middle of the 2nd metacarpal bone on the radial side. Precautions: no moxa, no needle in pregnancy. Point associations: Yuan source point Entry point Command point for face, nose, mouth and jaw Actions and effects: Releases the exterior for wind‐cold or wind‐heat syndromes. Strengthens the wei qi, improves immunity. Regulates the sweat glands, for excessive sweating tonify LI 4 then disperse KD 7 and vice versa. Any problem on the face ‐ sense organs, mouth, teeth, jaw, toothache, allergies, rhinitis, hay fever, acne, eye problems, etc. Toothache use both LI 4 & ST 44 ‐ LI for the lower jaw & ST for the upper jaw. Headache, especially frontal, sinus (yangming area). Chronic pain. Influence the circulation of Qi and blood ‐ use the four gates, LI 4 & LV 3 to strongly move the Qi and blood in the body clearing stagnation and alleviating pain. Promote labor or for retained placenta. |
| LI 10 (Shoushanli) | Location: 2 cm below LI 11 on the LI 5 to LI 11 line.
Actions and effects:
The following relationships exist between the ST and the LI and can be used to treat ST, LI and SI organ problems.
SI: LI 8 & ST 39.
LI: LI 9 & ST 37.
ST: LI 10 & ST 36.
Shoulder, elbow and wrist pain issues, general aches in these areas.
Less dispersive and more tonifying than other LI points.
Epigastric and abdominal pain, ulcers, vomiting. Location: 2 cm below LI 11 on the LI 5 to LI 11 line. |
| SP 6 (Sanyinjiao) | Location: 3 cm directly above the tip of the medial malleolus on the posterior border of the tibia. Precautions: no needle in pregnancy Point associations: Intersection point of the SP, LV and KD (3 leg yin meridians) Actions and effects: Tonify Yin and blood, all spleen disorders. Digestive disorders, sinking or prolapse. Gynecological issues, male sexual issues, difficult labor (expel fetus). Bleeding disorders, cool blood in hot skin diseases. Insomnia and other anxiety related emotions. |
| SP 8 (Diji) | Location: 3 cm below SP 9 on line connecting SP 9 and the tip of the medial malleolus. Point associations: Xi Cleft point. Actions and effects: Xi Cleft point ‐ acute and painful menstrual issues due to blood stagnation ‐ clotting, fibroids, dysmenorrhoea. Male infertility. |
| SP 10 (Xuehai) | Location: with knee flexed, 2 cm above the superior medial border of the patella on the bulge of the medial portion of quadriceps femoris (vastus medialis). Actions and effects: Any gynaecological issues originating from blood, heat, stasis and/or deficiency ‐ irregular menstruation, cramping, PMS. Skin problems from damp‐heat or hot blood. |
| ST29 (Guilai) | Location: 2 cm lateral to the AML level with CV 3. Actions and effects: Excess or cold/deficient disorders of the lower warmer ‐ amenorrhoea, irregular menstruation, qi stagnation/masses. Running Piglet disorder. |
| ST36 (Zushanli) | Location: 3 cm below ST 35, one finger width lateral from the anterior border of the tibia. Point associations: He Sea point Lower Lower He Sea point of the ST Earth point Sea of Water and Grain point Command point of the abdomen Actions and effects: Tonify deficient Qi or blood. Tonify Wei Qi. All issues involving the stomach or the spleen. Clear disorders along the course of the channel ‐ breast problems, lower leg pain. Earth as the mother of Metal ‐ will support lung function in cases of asthma, wheezing, dyspnoea. Psychological/Emotional disorders ‐ PMS, depression, nervousness. |
| PC6 (Neiguan) | Location: 2 cm above the wrist crease between the tendons of palmaris longus and flexor carpi radialis. Point associations: Luo Connecting point Yin Wei Master point coupled with SP 4 Actions and effects: Similar to PC 3 but more for chronic heart symptoms from Qi stagnation. Opens and relaxes the chest, chest tightness, asthma, angina, palpitations. Insomnia, other spirit disorders of an excess or deficient nature, mania, nervousness, stress, poor memory. Nausea, seasickness, motion sickness, vomiting, epigastric pain. Carpal tunnel syndrome. |
| Ren 3 (Zhongji) | Location (zhongji): 1 cm superior to qugu. Regulates LR, warms KI, irregular menses. |
| RN 4 (Guanyuan) | Location: 1.5 cm lateral to the Du meridian, at the level of the lower border of the spinous process of the 5th lumbar vertebra. Indications Low back pain, abdominal distension, diarrhoea, enuresis, sciatica, frequent urination. Traditional action Strengthens the lower back, removes obstructions from the channel. |
| RN6 (Qihai) | Location: 1.5 cm lateral to the Du meridian, at the level of the lower border of the spinous process of the third lumbar vertebra. Indications Low back pain, irregular menstruation, dysmenorrhoea, asthma. Traditional action Strengthens lower back, removes obstructions fro mchannel, regulates Qi and blood. |
| KI 3 (Taixi) | Location: in the depression between the medial malleolus and tendo calcaneus, at the level with the tip of the medial malleolus. Indications Sore throat, toothache, deafness, tinnitus, dizziness, spitting of blood, asthma, thirst, irregular menstruation, insomnia, nocturnal emission, impotence, frequency of micturition, pain in the lower back. Traditional action Tonifies the kidneys, benefits essence, strengthens the lower back and knees, regulates the uterus. |
| KI 11 (Henggu) | Location: 1.5 cm posterior to Wuchu (UB 5), 1.5 cm lateral to the Du meridian. Indications Headache, blurring of vision, nasal obstruction. Traditional action Clears heat and eliminates vexation, brightens the eyes and opens the portals. |
| TE 5 (Weiguan) | Location: 1.5 cm lateral to the lower border of the spinous process of the eighth thoracic vertebra. Indications Diabetes, vomiting, abdominal pain, pain in the chest and hypochorondriac region. Traditional action Relieves stagnation of blood. |
1. Acupuncture around the time of oocyte retrieval
None of the studies with the intervention performed around the time of oocyte retrieval had controls using sham or needling acupuncture.
1.1 Live birth rate (LBR)
Two studies (Humaidan 2004; Stener‐Victorin 2003) reported on the LBR. There was no evidence of a difference in the LBR between the treatment group (75/229) and the control group (84/235) (OR 0.87, 95% CI 0.59 to 1.29, I2 = 0%) (Analysis 1.1; Figure 4).
1.1. Analysis.
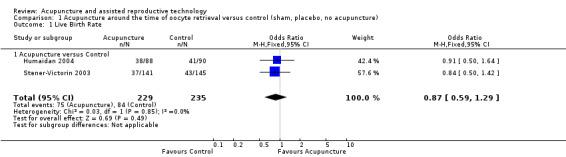
Comparison 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), Outcome 1 Live Birth Rate.
4.
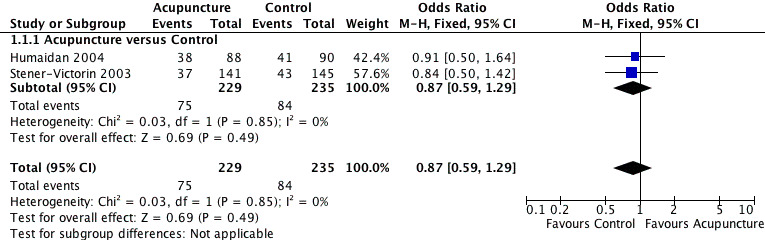
Forest plot of comparison: 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), outcome: 1.1 Live Birth Rate.
1.2 Ongoing pregnancy rate
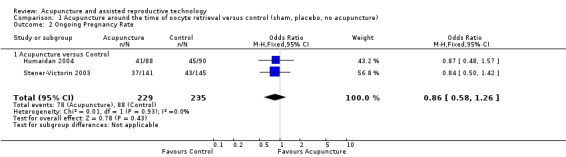
Two trials (Humaidan 2004; Stener‐Victorin 2003) reported an ongoing pregnancy rate of 78/229 in the treatment group versus 88/235 in the control group (OR 0.86, 95% CI 0.58 to 1.26, I2 = 0%) (Analysis 1.2).
1.2. Analysis.
Comparison 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), Outcome 2 Ongoing Pregnancy Rate.
1.3 Clinical pregnancy rate
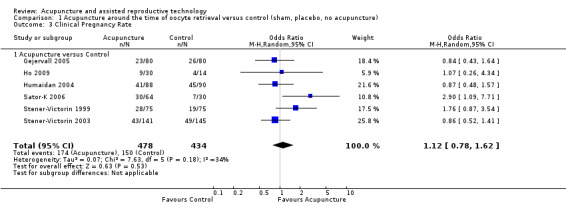
In the pooled results of six trials (Gejervall 2005; Ho 2009; Humaidan 2004; Sator‐K 2006; Stener‐Victorin 1999; Stener‐Victorin 2003), there was no evidence of a difference in the clinical pregnancy rate between the treatment group (174/478) and the control group 150/434 (OR 1.12, 95% CI 0.78 to 1.62, P = 0.53, I2 = 34%) (Analysis 1.3).
1.3. Analysis.
Comparison 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), Outcome 3 Clinical Pregnancy Rate.
1.4 Miscarriage rate
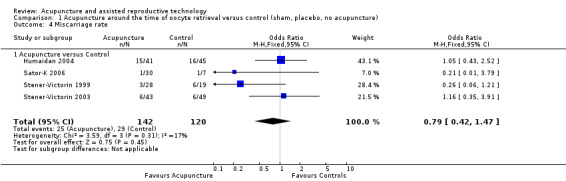
The pooled results from four trials (Humaidan 2004; Sator‐K 2006; Stener‐Victorin 1999; Stener‐Victorin 2003) showed no significant difference in miscarriage rates between the treatment group and control: 25/142 versus 29/120 (OR 0.79, 95% CI 0.42 to 1.47, I2 = 17%) (Analysis 1.4; Figure 5).
1.4. Analysis.
Comparison 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), Outcome 4 Miscarriage rate.
5.
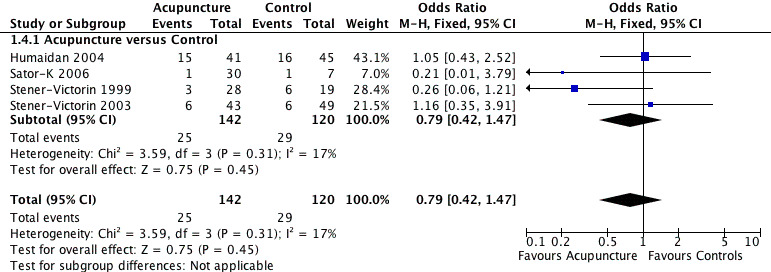
Forest plot of comparison: 1 Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture), outcome: 1.4 Miscarriage rate.
1.5 Multiple pregnancy
No trials reported multiple pregnancy.
1.6 Ovarian hyperstimulation syndrome (OHSS)
No trials reported OHSS.
2. Acupuncture on or around the day of embryo transfer
2.1 Live birth rate (LBR)
In women who had acupuncture on the day of and around ET (Andersen 2010; Dieterle 2006; Madaschi 2010; Paulus 2002; Paulus 2003; So 2009; So 2010; Westergaard 2006) (N = 2505), the overall LBR was 389/1302 compared to the controls 338/1203 (OR 1.22, 95% CI 0.87 to 1.70, P = 0.30, I2 = 69%) (Analysis 2.1; Figure 6). This was not statistically significant.
2.1. Analysis.
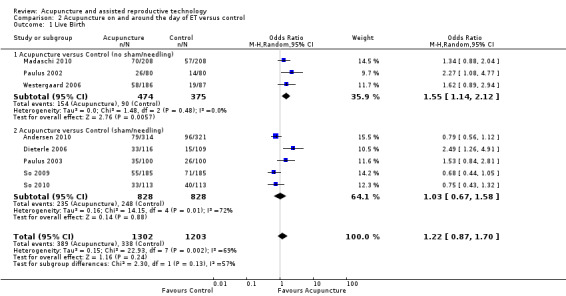
Comparison 2 Acupuncture on and around the day of ET versus control, Outcome 1 Live Birth.
6.
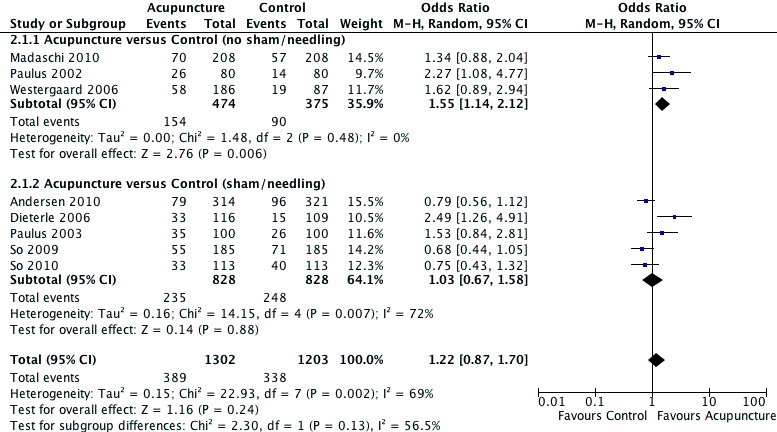
Forest plot of comparison: 2 Acupuncture on and around the day of ET versus control, outcome: 2.1 Live Birth.
In studies that had controls without sham acupuncture or needling (Madaschi 2010; Paulus 2002; Westergaard 2006), the LBR in the acupuncture group was significantly higher at 154/474 compared to 90/375 (OR 1.55, 95% CI 1.14 to 2.12, I2 = 0%) in the controls. In the studies that had controls with sham acupuncture (Andersen 2010; Dieterle 2006; Paulus 2003; So 2009; So 2010) the results were 235/828 in the acupuncture group compared to 248/828 (OR 1.03, 95% CI 0.67 to 1.58, P = 0.88, I2 = 72%) in the controls. This was not statistically significant.
2.2 Ongoing pregnancy rate
In the pooled results of 10 trials (Andersen 2010; Craig 2007; Dieterle 2006; Fraterelli 2008; Paulus 2002; Paulus 2003; Smith 2006; So 2009; So 2010; Westergaard 2006) (N = 2807), the overall ongoing pregnancy rate was 460/1451 in the acupuncture group compared to 427/1356 for all controls (OR 1.10, 95% CI 0.80 to 1.52, P = 0.56, I2 = 72%) (Analysis 2.2).
2.2. Analysis.
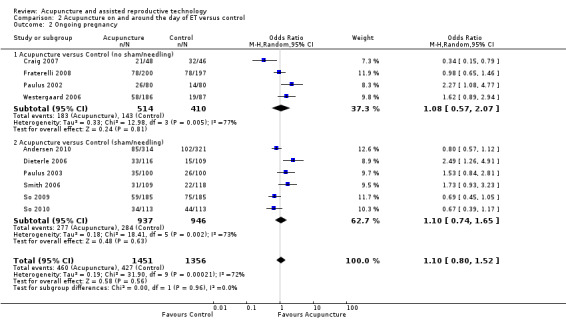
Comparison 2 Acupuncture on and around the day of ET versus control, Outcome 2 Ongoing pregnancy.
In studies that had controls without sham acupuncture or needling (Craig 2007; Fraterelli 2008; Paulus 2002; Westergaard 2006), the ongoing pregnancy rate in the acupuncture group was 183/514 compared to 143/410 in the controls (OR 1.08, 95% CI 0.57 to 2.07, P = 0.81, I2 = 77%). In the studies that had controls with sham acupuncture (Andersen 2010; Dieterle 2006; Paulus 2003; Smith 2006; So 2009; So 2010) the results were 277/937 in the acupuncture group compared to 284/946 in the controls (OR 1.10, 95% CI 0.74 to 1.65, P = 0.63, I2 = 73%). This was not statistically significant .
2.3 Clinical pregnancy rate
In the pooled results of 14 trials (Andersen 2010; Benson 2006; Craig 2007; Dieterle 2006; Domar 2009; Fraterelli 2008; Madaschi 2010; Moy 2011; Paulus 2002; Paulus 2003; Smith 2006; So 2009; So 2010; Westergaard 2006) (N = 3632) the clinical pregnancy rate was 734/1876 in the acupuncture group compared to 658/1756 for all controls (OR 1.11, 95% CI 0.87 to 1.42, P = 0.39, I2 = 66%). This was not statistically significant (Analysis 2.3).
2.3. Analysis.
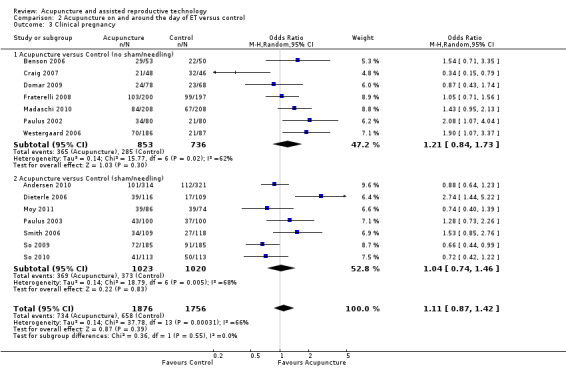
Comparison 2 Acupuncture on and around the day of ET versus control, Outcome 3 Clinical pregnancy.
In studies that had controls without sham acupuncture or needling (Benson 2006; Craig 2007; Domar 2009; Fraterelli 2008; Madaschi 2010; Paulus 2002; Westergaard 2006) the clinical pregnancy rate in the acupuncture group was 365/853 compared to 285/736 (OR 1.21, 95% CI 0.84 to 1.73, P = 0.30, I2 = 62%). In the studies that had controls with sham acupuncture (Andersen 2010; Dieterle 2006; Moy 2011; Paulus 2003; Smith 2006; So 2009; So 2010) the results were 369/1023 compared to 373/1020 (OR 1.04, 95% CI 0.74 to 1.46, P = 0.83, I2 = 68%). This was not statistically significant.
2.4 Miscarriage rate
Six trials evaluated the possible impact of acupuncture on miscarriage (Dieterle 2006; Madaschi 2010; Smith 2006; So 2009; So 2010; Westergaard 2006). The miscarriage rate was 71/340 in the acupuncture group compared to 57/276 in the overall controls (OR 1.10, 95% CI 0.73 to 1.67, I2 = 0%) (Analysis 2.4; Figure 7). There was no significant difference found between the two groups in the subgroup analysis.
2.4. Analysis.
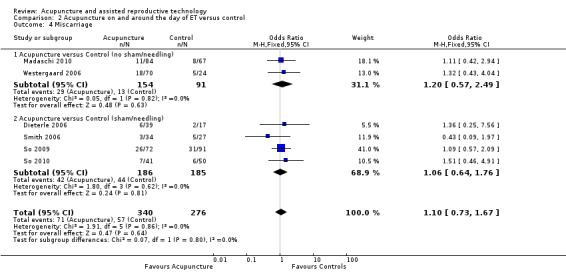
Comparison 2 Acupuncture on and around the day of ET versus control, Outcome 4 Miscarriage.
7.
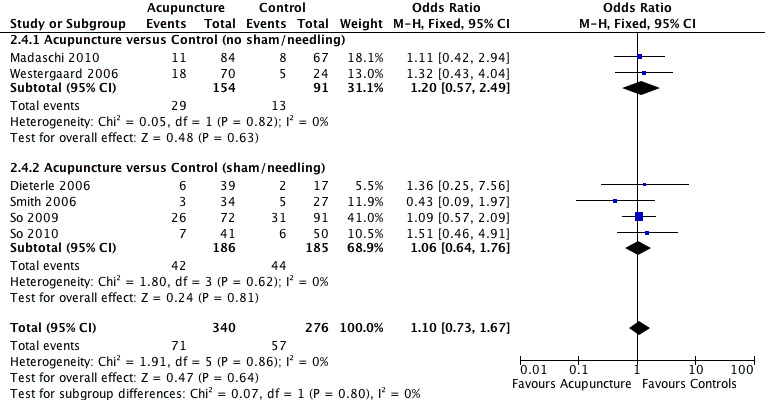
Forest plot of comparison: 2 Acupuncture on and around the day of ET versus control, outcome: 2.4 Miscarriage.
2.5 Multiple gestations
Two trials reported on multiple pregnancy rates (Andersen 2010; Moy 2011); both had control groups which used sham acupuncture. There was no significant difference detected between the acupuncture (30/400) and control groups (25/395) (OR 1.32, 95% CI 0.74 to 2.35, I2 = 0%) (Analysis 2.5).
2.5. Analysis.
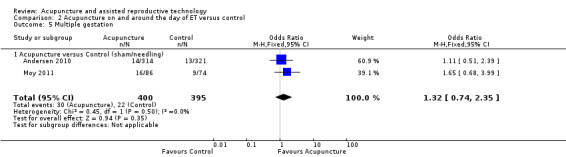
Comparison 2 Acupuncture on and around the day of ET versus control, Outcome 5 Multiple gestation.
2. 6 Ovarian hyperstimulation syndrome (OHSS)
None of the 14 trials reported ovarian hyperstimulation.
2.7 Any side effects
So 2009 and So 2010 did not report any statistically significant difference between side effects in the 'real' and 'placebo' acupuncture groups; side effects included nausea, dizziness, fainting, tiredness, headache, chest pain and puncture site itching. However, Moy 2011 suggest a difference between the two groups in the main categories of the McGill pain score. Women in the true arm reported greater affective perception of being tired and fearful as well as more achiness.
Assessment of heterogeneity
Heterogeneity was generally absent or low when studies of acupuncture around the time of oocyte retrieval were pooled
However when analyses of studies of acupuncture on or around the day of embryo transfer were pooled there was high heterogeneity (I‐squared >50%) for several outcomes, and we considered clinical and methodological differences between the studies that might account for this. The increased heterogeneity may be a result of the large variation in the definition of controls and acupuncture points used in the included studies (see below).
Discussion
Summary of main results
This updated review reports no evidence of overall benefit of acupuncture in improving live birth rate (LBR) when acupuncture was performed around the time of oocyte retrieval or on and around the day of ET.
The subgroup analysis showed that in studies with controls without sham or needling, women who had acupuncture on and around the day of ET had a higher LBR than the controls (OR 1.55, 95% CI 1.14 to 2.12); however this evidence of benefit was not present in studies where the control group had sham acupuncture (acupuncture compared to sham controls (OR 0.93, 95% CI 0.75 to 1.15). The difference in findings between the two subgroups could possibly be due to study quality: only two RCTs, both in the sham acupuncture group, reported satisfactory methods of allocation concealment.
There was no evidence that acupuncture had an effect on miscarriage rates or other treatment side effects.
Most authors in the field assume that acupuncture has little detrimental effect. Our review reports no evidence of effect on the miscarriage rate between acupuncture groups and all controls, regardless of the timing of the intervention. This data does not prove that acupuncture is free of harm in early pregnancy and one should apply caution when giving advice to women about undergoing acupuncture in early pregnancy.
Overall completeness and applicability of evidence
It is generally accepted that acupuncture is relatively painless and has few side effects, although recent studies have shown that serious adverse events can occur (He et al, 2012). Before routine treatment can be accepted into mainstream medicine, acupuncture needs to have proven efficacy. In other words, acupuncture has to be demonstrably more effective than placebo. However, the use of an appropriate placebo in this context is variable. The variety of controls used for the RCTs included in this review ranged across no intervention, placebo needling, and sham acupuncture needles. Although sham needles are regarded as an acceptable control, true patient blinding has been shown to be a challenge (Tan 2011). It is possible that acupuncture needling could elicit a placebo or true biological effect over a wide area of the body not specific to 'points'. It has been suggested that a placebo effect may positively influence reproductive outcomes through mechanisms related to stress relief (Domar 2011; Meissner 2007), although postulating the biological impact of placebo is very much outside the context of this review.
Studies included in this review also had a large variation in pregnancy rates, but most studies did not report their centre's normal pregnancy rate for comparison.
Although all 20 trials in this review examined the use of acupuncture for improving the pregnancy rate with IVF, different acupuncture points were selected to achieve the same objective and it is unclear why this is the case. In Western medicine, where the standardisation of methodology is of key importance in medical research, the absence of complete concordance of the acupuncture points in these studies is an unfamiliar concept. There is no consensus amongst practicing acupuncturists as to what constitutes a reasonable variation of the acupuncture treatment protocol. There is also no consensus as to how much experience or training an acupuncturist needs to provide effective acupuncture treatment, although courses are available that provide a license to practice the art.
At the time of writing this review, the authors knew of four further studies in the area that are ongoing (ACTRN12611000226909; IRCT201011275181N4; NCT00317317; NCT01449396).
Quality of the evidence
The overall quality of evidence for live birth outcomes was rated as low, using GRADE methods (seeTable 1 and Table 2). The quality of individual studies was generally low, with over 75% failing to describe an adequate method of allocation concealment (see Figure 2 and Figure 3).
Potential biases in the review process
We made every effort to identify all potentially eligible studies, and sought additional data from study authors as necessary. However, it is possible that there are unpublished studies that were not retrieved.
Agreements and disagreements with other studies or reviews
Several meta‐analyses have been published in the last six years in this area (Anderson 2007; Cheong 2010; El‐Toukhy 2010; Manheimer 2008; Zheng 2012). Depending on the data included and when the reviews were published, researchers have reached different conclusions about the beneficial effects on acupuncture on women undergoing IVF. Such discrepancies will continue to exist unless agreed standard scientific principles and research methodologies are incorporated into future studies (MacPherson 2010).
Authors' conclusions
Implications for practice.
We found no evidence that acupuncture improves live birth rate, ongoing pregnancy rate or clinical pregnancy rate. We also found no evidence that acupuncture increases the rate of miscarriage.
Implications for research.
Future research into the value of acupuncture in improving the pregnancy rate of women undergoing IVF treatment should incorporate basic scientific principles and methodologies. Within the realm of RCTs, studies in this area should focus on the use of 'standardised' acupuncture methods so that reasonable comparisons can be made; live birth rate should be used as the primary outcome.The use of 'sham needles' may enhance the quality of the studies performed, though further research into the biological effect of sham acupuncture is needed. Ideally, studies in this area should carefully consider how they determine the necessary treatment points, gather qualitative as well as quantitative data in parallel with a three arm study design, acupuncture, no intervention and placebo needling. They should also provide their centre's pregnancy rates during the time course of the study for comparison. It is with this comprehensive study design that any clinical benefit of acupuncture can be delineated.
What's new
| Date | Event | Description |
|---|---|---|
| 23 July 2013 | New citation required but conclusions have not changed | Seven new studies included in this update (Andersen 2010; Fraterelli 2008; Ho 2009; Madaschi 2010; Moy 2011; So 2009; So 2010) |
| 23 July 2013 | New search has been performed | Updated review |
History
Protocol first published: Issue 1, 2008 Review first published: Issue 4, 2008
| Date | Event | Description |
|---|---|---|
| 13 June 2008 | Amended | Converted to new review format. |
| 13 October 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We thank the Cochrane Menstrual Disorders and Subfertility Group for providing us with the search strategy and for proof reading the review.
Appendices
Appendix 1. MDSG search string
Menstrual Disorders and Subfertility Database Search strategy for IRS911
All reports which described randomised controlled trials of acupuncture in assisted conception were identified using the following search strategy.
Keywords CONTAINS "ART" or "assisted reproduction" or "assisted reproduction techniques" or "IVF" or "ICSI" or "in vitro fertilisation" or "in‐vitro fertilisation techniques" or "in vitro fertilization" or "in vitro maturation" or "intracytoplasmic sperm injection" or "subfertility" or "Infertility" or "IUI" or "Intrauterine Insemination" or "*Embryo Transfer" or "ET" or Title CONTAINS "ART" or "assisted reproduction" or "assisted reproduction techniques" or "IVF" or "ICSI" or "in vitro fertilisation" or "in‐vitro fertilisation techniques" or "in vitro fertilization" or "in vitro maturation" or "intracytoplasmic sperm injection" or "subfertility" or "Infertility" or "IUI" or "Intrauterine Insemination" or "*Embryo Transfer" or "ET"
AND
Keywords CONTAINS "acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "Tui Na" or "ear electroacupuncture" or "ear point pressing" or Title CONTAINS"acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "Tui Na" or "ear electroacupuncture" or "ear point pressing"
Appendix 2. MEDLINE
Database: Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) <1950 to Present> 1 exp reproduction techniques/ (101304) 2 exp fertility agents/ (24722) 3 (in vitro adj5 fertili$).tw. (16577) 4 ivf.tw. (12990) 5 icsi.tw. (4184) 6 (intracytoplas$ adj5 sperm$).tw. (4102) 7 subfertil$.tw. (2853) 8 (sperm$ adj5 inject$).tw. (5040) 9 suzi.tw. (101) 10 (subzon$ adj5 sperm$).tw. (110) 11 (zona adj5 dissect$).tw. (111) 12 pzd.tw. (61) 13 (ovar$ adj5 hyperstim$).tw. (3208) 14 ohss.tw. (899) 15 (oocyt$ adj5 retriev$).tw. (3100) 16 (oocyt$ adj5 pickup).tw. (48) 17 (sperm$ adj5 prepa$).tw. (1589) 18 (acrosom$ adj5 sperm$).tw. (4519) 19 (sperm$ adj5 stimul$).tw. (2014) 20 (sperm$ adj5 pentox$).tw. (114) 21 (sperm$ adj5 caff$).tw. (143) 22 (sperm$ adj5 kalli$).tw. (59) 23 (sperm$ adj5 swimup$).tw. (4) 24 (sperm adj5 percol$).tw. (239) 25 (embry$ adj5 biops$).tw. (563) 26 (cocult$ adj5 embry$).tw. (401) 27 (cocult$ adj5 trophobl$).tw. (33) 28 (luteal phase adj5 support).tw. (210) 29 (sperm$ adj5 cryopreserv$).tw. (1809) 30 (frozen adj5 embry$).tw. (1648) 31 (antisperm$ adj5 antibod$).tw. (1061) 32 (sperm$ adj5 antibod$).tw. (2406) 33 (artific$ adj5 inseminat$).tw. (4842) 34 (cervi$ adj5 inseminat$).tw. (201) 35 (fallopian tub$ adj5 perfus$).tw. (30) 36 (luteal adj5 defect$).tw. (375) 37 (luteal adj5 dysfunct$).tw. (82) 38 (ovulat$ adj5 induc$).tw. (6757) 39 (intraut$ adj5 inseminat$).tw. (1569) 40 (ectop$ adj5 preg$).tw. (7399) 41 (tub$ adj5 preg$).tw. (4499) 42 inseminat$.tw. (12887) 43 varicoc$.tw. (3433) 44 fertility/ (28979) 45 fertilization/ (11655) 46 insemination/ (630) 47 ovum implantation/ (8013) 48 Ovarian Hyperstimulation Syndrome/ (1424) 49 (embry$ adj5 transf$).tw. (16430) 50 or/1‐49 (198724) 51 acupuncture/ (944) 52 exp acupuncture therapy/ (14092) 53 electroacupuncture/ (1949) 54 meridians/ (341) 55 acupuncture points/ (2977) 56 acupunctur$.tw. (12149) 57 (electroacupunctur$ or electro‐acupunctur$).tw. (2370) 58 acupoint$.tw. (1825) 59 ((meridian or non‐meridian or trigger) adj10 point$).tw. (1359) 60 exp Moxibustion/ (887) 61 (moxabustion or moxibustion or moxa$).tw. (2215) 62 or/51‐61 (19443) 63 randomised controlled trial.pt. (307764) 64 controlled clinical trial.pt. (83549) 65 randomized.ab. (220349) 66 placebo.tw. (132278) 67 clinical trials as topic.sh. (153325) 68 randomly.ab. (163109) 69 trial.ti. (95112) 70 (crossover or cross‐over or cross over).tw. (50660) 71 or/63‐70 (747590) 72 exp animals/ not humans.sh. (3606997) 73 71 not 72 (691399) 74 50 and 62 and 73 (54) 75 (200710$ or 200711$ or 200712$).ed. (201896) 76 (2008$ or 2009$ or 2010$).ed. (2609966) 77 75 or 76 (2811862) 78 74 and 77 (23)
Appendix 3. CENTRAL
Database: EBM Reviews ‐ Cochrane Central Register of Controlled Trials 1 exp reproduction techniques/ (2310) 2 exp fertility agents/ (1423) 3 (in vitro adj5 fertili$).tw. (1280) 4 ivf.tw. (1749) 5 icsi.tw. (600) 6 (intracytoplas$ adj5 sperm$).tw. (385) 7 subfertil$.tw. (124) 8 (sperm$ adj5 inject$).tw. (431) 9 suzi.tw. (13) 10 (subzon$ adj5 sperm$).tw. (19) 11 (zona adj5 dissect$).tw. (23) 12 pzd.tw. (6) 13 (ovar$ adj5 hyperstim$).tw. (506) 14 ohss.tw. (138) 15 (oocyt$ adj5 retriev$).tw. (547) 16 (oocyt$ adj5 pickup).tw. (7) 17 (sperm$ adj5 prepa$).tw. (98) 18 (acrosom$ adj5 sperm$).tw. (54) 19 (sperm$ adj5 stimul$).tw. (113) 20 (sperm$ adj5 pentox$).tw. (45) 21 (sperm$ adj5 caff$).tw. (7) 22 (sperm$ adj5 kalli$).tw. (16) 23 (sperm$ adj5 swimup$).tw. (0) 24 (sperm adj5 percol$).tw. (38) 25 (embry$ adj5 biops$).tw. (26) 26 (cocult$ adj5 embry$).tw. (20) 27 (cocult$ adj5 trophobl$).tw. (0) 28 (luteal phase adj5 support).tw. (122) 29 (sperm$ adj5 cryopreserv$).tw. (59) 30 (frozen adj5 embry$).tw. (114) 31 (antisperm$ adj5 antibod$).tw. (48) 32 (sperm$ adj5 antibod$).tw. (49) 33 (artific$ adj5 inseminat$).tw. (54) 34 (cervi$ adj5 inseminat$).tw. (19) 35 (fallopian tub$ adj5 perfus$).tw. (23) 36 (luteal adj5 defect$).tw. (34) 37 (luteal adj5 dysfunct$).tw. (10) 38 (ovulat$ adj5 induc$).tw. (535) 39 (intraut$ adj5 inseminat$).tw. (368) 40 (ectop$ adj5 preg$).tw. (170) 41 (tub$ adj5 preg$).tw. (139) 42 inseminat$.tw. (599) 43 varicoc$.tw. (106) 44 fertility/ (101) 45 fertilization/ (127) 46 insemination/ (3) 47 ovum implantation/ (313) 48 Ovarian Hyperstimulation Syndrome/ (121) 49 (embry$ adj5 transf$).tw. (1050) 50 or/1‐49 (5752) 51 acupuncture/ (100) 52 exp acupuncture therapy/ (1824) 53 electroacupuncture/ (299) 54 meridians/ (25) 55 acupuncture points/ (662) 56 acupunctur$.tw. (3825) 57 (electroacupunctur$ or electro‐acupunctur$).tw. (559) 58 acupoint$.tw. (687) 59 ((meridian or non‐meridian or trigger) adj10 point$).tw. (256) 60 exp Moxibustion/ (117) 61 (moxabustion or moxibustion or moxa$).tw. (513) 62 or/51‐61 (5069) 63 50 and 62 (34) 64 limit 63 to yr="2007 ‐Current" (13)
Appendix 4. EMBASE
Database: EBM Reviews ‐ Cochrane Central Register of Controlled Trials 1 exp reproduction techniques/ (2310) 2 exp fertility agents/ (1423) 3 (in vitro adj5 fertili$).tw. (1280) 4 ivf.tw. (1749) 5 icsi.tw. (600) 6 (intracytoplas$ adj5 sperm$).tw. (385) 7 subfertil$.tw. (124) 8 (sperm$ adj5 inject$).tw. (431) 9 suzi.tw. (13) 10 (subzon$ adj5 sperm$).tw. (19) 11 (zona adj5 dissect$).tw. (23) 12 pzd.tw. (6) 13 (ovar$ adj5 hyperstim$).tw. (506) 14 ohss.tw. (138) 15 (oocyt$ adj5 retriev$).tw. (547) 16 (oocyt$ adj5 pickup).tw. (7) 17 (sperm$ adj5 prepa$).tw. (98) 18 (acrosom$ adj5 sperm$).tw. (54) 19 (sperm$ adj5 stimul$).tw. (113) 20 (sperm$ adj5 pentox$).tw. (45) 21 (sperm$ adj5 caff$).tw. (7) 22 (sperm$ adj5 kalli$).tw. (16) 23 (sperm$ adj5 swimup$).tw. (0) 24 (sperm adj5 percol$).tw. (38) 25 (embry$ adj5 biops$).tw. (26) 26 (cocult$ adj5 embry$).tw. (20) 27 (cocult$ adj5 trophobl$).tw. (0) 28 (luteal phase adj5 support).tw. (122) 29 (sperm$ adj5 cryopreserv$).tw. (59) 30 (frozen adj5 embry$).tw. (114) 31 (antisperm$ adj5 antibod$).tw. (48) 32 (sperm$ adj5 antibod$).tw. (49) 33 (artific$ adj5 inseminat$).tw. (54) 34 (cervi$ adj5 inseminat$).tw. (19) 35 (fallopian tub$ adj5 perfus$).tw. (23) 36 (luteal adj5 defect$).tw. (34) 37 (luteal adj5 dysfunct$).tw. (10) 38 (ovulat$ adj5 induc$).tw. (535) 39 (intraut$ adj5 inseminat$).tw. (368) 40 (ectop$ adj5 preg$).tw. (170) 41 (tub$ adj5 preg$).tw. (139) 42 inseminat$.tw. (599) 43 varicoc$.tw. (106) 44 fertility/ (101) 45 fertilization/ (127) 46 insemination/ (3) 47 ovum implantation/ (313) 48 Ovarian Hyperstimulation Syndrome/ (121) 49 (embry$ adj5 transf$).tw. (1050) 50 or/1‐49 (5752) 51 acupuncture/ (100) 52 exp acupuncture therapy/ (1824) 53 electroacupuncture/ (299) 54 meridians/ (25) 55 acupuncture points/ (662) 56 acupunctur$.tw. (3825) 57 (electroacupunctur$ or electro‐acupunctur$).tw. (559) 58 acupoint$.tw. (687) 59 ((meridian or non‐meridian or trigger) adj10 point$).tw. (256) 60 exp Moxibustion/ (117) 61 (moxabustion or moxibustion or moxa$).tw. (513) 62 or/51‐61 (5069) 63 50 and 62 (34) 64 limit 63 to yr="2007 ‐Current" (13)
Appendix 5. AMED
Database: AMED (Allied and Complementary Medicine) 1 (IVF or ICSI or IUI).tw. (29) 2 "embryo transfer".tw. (3) 3 ("in vitro fertilisation" or "in vitro fertilization").tw. (22) 4 ("intrauterine insemination" or "intracytoplasmic sperm injection").tw. (10) 5 exp Infertility female/ (122) 6 exp acupuncture therapy/ (5986) 7 acupuncture.tw. (8055) 8 exp Moxibustion/ (419) 9 (moxibustion or moxabustion or moxa$).tw. (498) 10 or/6‐9 (8837) 11 or/1‐5 (149) 12 10 and 11 (31) 13 limit 12 to yr="2007 ‐Current" (13)
Appendix 6. CINHAL
1 Controlled study/ or randomised controlled trial/ 2 (drug$ adj5 compar$).ti,ab,hw,tn,mf. 3 placebo/ 4 random$.ti,ab,hw,tn,mf. 5 latin square.ti,ab,hw,tn,mf. 6 crossover.ti,ab,hw,tn,mf. 7 cross‐over.ti,ab,hw,tn,mf. 8 placebo$.ti,ab,hw,tn,mf. 9 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf. 10 (comparative adj5 trial$).ti,ab,hw,tn,mf. 11 (clinical adj5 trial$).ti,ab,hw,tn,mf. 12 or/1‐11 13 animal/ not (human/ and animal/) 14 12 not 13 15 exp reproduction techniques/ 16 exp fertility agents/ 17 (in vitro adj5 fertili$).tw. 18 ivf.tw. 19 icsi.tw. 20 (intracytoplas$ adj5 sperm$).tw. 21 subfertil$.tw. 22 (sperm$ adj5 inject$).tw. 23 suzi.tw. 24 (subzon$ adj5 sperm$).tw. 25 (zona adj5 sperm$).tw. 26 (zona adj5 dissect$).tw. 27 pzd.tw. 28 (ovar$ adj5 hyperstim$).tw. 29 ohss.tw. 30 (oocyt$ adj5 retriev$).tw. 31 (oocyt$ adj5 pickup).tw. 32 (sperm$ adj5 prepa$).tw. 33 (acrosom$ adj5 sperm$).tw. 34 (sperm$ adj5 stimul$).tw. 35 (sperm$ adj5 pentox$).tw. 36 (sperm$ adj caff$).tw. 37 (sperm$ adj5 kalli$).tw. 38 (sperm$ adj5 swimup$).tw. 39 (sperm adj5 percol$).tw. 40 (embry$ adj5 biops$).tw. 41 (cocult$ adj5 embry$).tw. 42 (cocult$ adj5 trophobl$).tw. 43 (luteal phase adj5 support).tw. 44 (sperm$ adj5 cryopreserv$).tw. 45 (frozen adj5 embry$).tw. 46 (antisperm$ adj5 antibod$).tw. 47 (sperm$ adj5 antibod$).tw. 48 (artific$ adj5 inseminat$).tw. 49 (cervi$ adj5 inseminat$).tw. 50 (fallopian tub$ adj5 perfus$).tw. 51 (luteal adj5 defect$).tw. 52 (luteal adj5 dysfunct$).tw. 53 (ovulat$ adj5 induc$).tw. 54 (intraut$ adj5 inseminat$).tw. 55 (ectop$ adj5 preg$).tw. 56 (tub$ adj5 preg$).tw. 57 inseminat$.tw. 58 varicoc$.tw. 59 fertility/ 60 fertilization/ 61 insemination/ 62 ovum implantation/ 63 Ovarian Hyperstimulation Syndrome/ 64 (embry$ adj5 transf$).tw. 65 or/15‐64 66 65 and 14 67 acupuncture/ or electroacupuncture/ or meridians/ or acupuncture points/ 68 acupunctur$.tw. 69 (electroacupunctur$ or electro‐acupunctur$).tw. 70 acupoint$.tw. 71 ((meridian or non‐meridian or trigger) adj10 point$).tw. 72 exp MOXIBUSTION/ 73 (moxibustion or moxabustion or moxa).tw. 74 or/67‐73 75 66 and 74 76 from 75 keep 1‐8
Appendix 7. PsycINFO
Database: PsycINFO 1 (IVF or ICSI or IUI).tw. (305) 2 "embryo transfer".tw. (74) 3 ("in vitro fertilisation" or "in vitro fertilization").tw. (405) 4 ("intrauterine insemination" or "intracytoplasmic sperm injection").tw. (28) 5 exp Reproductive Technology/ (1025) 6 exp Infertility/ (1378) 7 or/1‐6 (2241) 8 exp Acupuncture/ (850) 9 acupuncture.tw. (1164) 10 Moxibustion.tw. (19) 11 (moxibustion or moxabustion or moxa$).tw. (24) 12 acupressure.tw. (76) 13 electroacupunture.tw. (1) 14 acu$ point$.tw. (97) 15 or/8‐14 (1306) 16 7 and 15 (3)
Data and analyses
Comparison 1. Acupuncture around the time of oocyte retrieval versus control (sham, placebo, no acupuncture).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Live Birth Rate | 2 | 464 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.59, 1.29] |
| 1.1 Acupuncture versus Control | 2 | 464 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.59, 1.29] |
| 2 Ongoing Pregnancy Rate | 2 | 464 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.58, 1.26] |
| 2.1 Acupuncture versus Control | 2 | 464 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.58, 1.26] |
| 3 Clinical Pregnancy Rate | 6 | 912 | Odds Ratio (M‐H, Random, 95% CI) | 1.12 [0.78, 1.62] |
| 3.1 Acupuncture versus Control | 6 | 912 | Odds Ratio (M‐H, Random, 95% CI) | 1.12 [0.78, 1.62] |
| 4 Miscarriage rate | 4 | 262 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.42, 1.47] |
| 4.1 Acupuncture versus Control | 4 | 262 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.42, 1.47] |
Comparison 2. Acupuncture on and around the day of ET versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Live Birth | 8 | 2505 | Odds Ratio (M‐H, Random, 95% CI) | 1.22 [0.87, 1.70] |
| 1.1 Acupuncture versus Control (no sham/needling) | 3 | 849 | Odds Ratio (M‐H, Random, 95% CI) | 1.55 [1.14, 2.12] |
| 1.2 Acupuncture versus Control (sham/needling) | 5 | 1656 | Odds Ratio (M‐H, Random, 95% CI) | 1.03 [0.67, 1.58] |
| 2 Ongoing pregnancy | 10 | 2807 | Odds Ratio (M‐H, Random, 95% CI) | 1.10 [0.80, 1.52] |
| 2.1 Acupuncture versus Control (no sham/needling) | 4 | 924 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.57, 2.07] |
| 2.2 Acupuncture versus Control (sham/needling) | 6 | 1883 | Odds Ratio (M‐H, Random, 95% CI) | 1.10 [0.74, 1.65] |
| 3 Clinical pregnancy | 14 | 3632 | Odds Ratio (M‐H, Random, 95% CI) | 1.11 [0.87, 1.42] |
| 3.1 Acupuncture versus Control (no sham/needling) | 7 | 1589 | Odds Ratio (M‐H, Random, 95% CI) | 1.21 [0.84, 1.73] |
| 3.2 Acupuncture versus Control (sham/needling) | 7 | 2043 | Odds Ratio (M‐H, Random, 95% CI) | 1.04 [0.74, 1.46] |
| 4 Miscarriage | 6 | 616 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.73, 1.67] |
| 4.1 Acupuncture versus Control (no sham/needling) | 2 | 245 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.57, 2.49] |
| 4.2 Acupuncture versus Control (sham/needling) | 4 | 371 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.64, 1.76] |
| 5 Multiple gestation | 2 | 795 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.74, 2.35] |
| 5.1 Acupuncture versus Control (sham/needling) | 2 | 795 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.74, 2.35] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andersen 2010.
| Methods | Randomised controlled trial of fertility patients in Denmark | |
| Participants | Patients (n = 635) scheduled for embryo transfer were randomised into acupuncture according to the principles of Traditional Chinese Medicine (n = 314) or placebo acupuncture (n = 321). The average age of the two groups of women was 31 years and the average body mass index (BMI) was 22.5 for both groups. There were similar numbers of previous IVF/ICSI cycles and similar proportions of causes of infertility between both groups. |
|
| Interventions | Needle acupuncture or placebo acupuncture using Strietberger placebo needle for 25 minutes before and after embryo transfer; performed by nurses who were professional acupuncturists or by nurses who had received instruction and training by the acupuncturists prior to the trial | |
| Outcomes | Ongoing pregnancy rate, implantation and pregnancy rates, live birth rates | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence generation – LOW RISK ‐ ‘the sequence of cluster randomization was based on a computer‐generated list’ |
| Allocation concealment (selection bias) | Unclear risk | ‘nurses did the randomization with the sealed envelope technique’ |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Sequence allocation was performed by nurses and the procedure was performed blinded to patients and the clinician performing ET |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No patients lost to follow up |
| Selective reporting (reporting bias) | Low risk | None known |
| Other bias | Low risk | None known |
Benson 2006.
| Methods | Randomised controlled trial of fertility patients in US; abstract only | |
| Participants | Patients (n = 258) who had been scheduled for ET were randomised into needle acupuncture (n = 53), laser acupuncture (n = 53), sham laser acupuncture (n = 52), relaxation treatment (n = 50) and no treatment (n = 50). For the purpose of this meta‐analysis, only the results from the needle acupuncture and no treatment groups were used. There were no details on the demographics as abstract only available |
|
| Interventions | Needle acupuncture performed for 25 minutes before and after embryo transfer versus no intervention control group. There were no details on the qualifications of the acupuncturists as abstract only available | |
| Outcomes | Clinical pregnancy rate | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Emailed authors for LBR but no reply | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only; sequence generation not stated. |
| Allocation concealment (selection bias) | Unclear risk | Abstract only; allocation concealment not stated. |
| Blinding (performance bias and detection bias) All outcomes | High risk | No sham needle group used, therefore blinding not possible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 258 participants randomized but authors did not state the number of participants that completed the study. |
| Selective reporting (reporting bias) | Unclear risk | Did not report live birth |
| Other bias | Low risk | None known |
Craig 2007.
| Methods | Multicentre randomised control trial undertaken in the US; abstract only | |
| Participants | 107 patients undergoing IVF randomised women into two groups: one with acupuncture treatment (n = 48) and one without (n = 46). There were no details on demographics as this report was presented as an abstract |
|
| Interventions | Acupuncture performed for 25 minutes before and after embryo transfer, against no intervention control group.There were no details on the qualifications of the acupuncturists as abstract only available. | |
| Outcomes | Ongoing and clinical pregnancy rate | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | No information provided by authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only; sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Abstract only; allocation concealment not stated. |
| Blinding (performance bias and detection bias) All outcomes | High risk | No sham acupuncture control used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 107 participants randomized, 94 completed the study. 10 IVF cycles cancelled, 3 patients withdrew. |
| Selective reporting (reporting bias) | Unclear risk | Did not report live birth |
| Other bias | Low risk | None known |
Dieterle 2006.
| Methods | Randomised controlled trial, fertility patients in clinic in Germany | |
| Participants | 225 patients randomised: 116 to treatment and 109 to placebo. Treatment included placing Chinese herbs in patients' ears. No losses to follow up. Placebo treatment at sites that will not affect fertility, but physicians who were performing ET were blinded. The average age (± SD) of the study group (n = 116) was 35.1 years (± 3.8) compared to 34.7 years (± 4) for the placebo group (n = 109). There were no statistical differences in the body mass index (BMI), causes of subfertility, and number of previous cycles between the study and control groups. |
|
| Interventions | Treatment included acupuncture + Chinese herbs in ears versus control group of acupuncture at sites that are not believed to affect fertility. The intervention was performed for 30 minutes after embryo transfer and again 3 days later. All acupuncture was performed by the same practitioner | |
| Outcomes | Live birth rate, clinical pregnancy rates and ongoing clinical pregnancy rates | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | Placebo group did not have drugs placed in ears | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated in the manuscript |
| Allocation concealment (selection bias) | Unclear risk | ‘randomised with sealed randomization envelopes’ but not stated if these envelopes where opaque or sequentially numbered. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Use of placebo treatment in control group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 225 participants randomized; none lost to follow up. |
| Selective reporting (reporting bias) | Unclear risk | Not known whether LBR a prestated outcome |
| Other bias | Low risk | None known |
Domar 2009.
| Methods | Randomised controlled trial of fertility patients in the US | |
| Participants | 150 patients recruited and randomised to either needle acupuncture (n = 78) and no treatment (n=68). The average age of the two groups of women was 36 years, with similar numbers of previous IVF cycles in the two groups. |
|
| Interventions | Acupuncture performed by an acupuncturist 25 minutes before and after embryo transfer versus no treatment control | |
| Outcomes | Clinical pregnancy rate | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘randomisation was accomplished by using a computer‐generated random numbers table’ |
| Allocation concealment (selection bias) | Unclear risk | Not stated in the manuscript |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible to blind as control group had no intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 146 participants randomized but number completed not reported. |
| Selective reporting (reporting bias) | Unclear risk | No LBR outcomes reported. |
| Other bias | Low risk | None known |
Fraterelli 2008.
| Methods | Randomised controlled trial of fertility patients in the US; abstract only | |
| Participants | 1000 patients randomised to five arms: needle acupuncture (n = 200), laser acupuncture (n = 202), sham laser acupuncture (n = 198), relaxation (n = 203) and non‐treatment group (n = 197). No demographics breakdown given but stated no difference between groups |
|
| Interventions | Two treatment arms (laser and needle acupuncture) and three control arms (sham laser acupuncture, relaxation and non‐treatment). For the purpose of this meta‐analysis, only the results from the needle acupuncture and no treatment groups were used | |
| Outcomes | Chemical and clinical pregnancy rate | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Only needle acupuncture versus control are relevant to this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only, no randomisation details given |
| Allocation concealment (selection bias) | Unclear risk | Abstract only, no details given |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group received no treatment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not stated if all participants randomized completed the study |
| Selective reporting (reporting bias) | Unclear risk | No LBR outcomes reported. |
| Other bias | Low risk | None known |
Gejervall 2005.
| Methods | Open, randomised single‐centre trial performed at the IVF unit of Reproductive Medicine at Sahlgrenska University Hospital in Goteborg | |
| Participants | There were 160 women randomised in the study: 80 to the EA (electro‐acupuncture) group and 80 to the CA (conventional acupuncture) group. The average age of the women (± SD) in the control group (n = 80) was 33.9 years (± 3.7) compared to 33.2 years (± 3.6) in the intervention group; the average number of IVF cycles performed was 1.56 (± 0.93) compared to 1.48 (± 0.93). The majority of women had male factor or unexplained subfertility. |
|
| Interventions | The study compared electro‐acupuncture at the time of oocyte retrieval (EA group) with conventional analgesia (intravenous alfentanil). Both groups also had a paracervical block performed. Electro‐acupuncture was performed by midwives who had been trained in the IVF unit. | |
| Outcomes | Wellbeing was evaluated with the State Trait Anxiety Inventory (STAI). Pain and subjective expectations and experiences were recorded on a visual analogue scale (VAS). Time and drug consumption were recorded Pregnancy rate was recorded as secondary outcome |
|
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | Study designed to assess effectiveness of acupuncture as an analgesic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘randomisation was performed by the study coordinator according to a computerized list’ |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) All outcomes | High risk | Conventional analgesia of I.V. alfentanil used as control analgesia. Therefore both participants and personnel not blinded. Not stated if assessor was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 women randomized; 2 lost to follow up. |
| Selective reporting (reporting bias) | Unclear risk | No LBR outcome reported. |
| Other bias | Low risk | None |
Ho 2009.
| Methods | Randomised study performed at the IVF centre of China Medical University Hospital in Taiwan | |
| Participants | A total of 44 women were enrolled in the study: 30 were randomised to acupuncture group and 14 to the control (no‐acupuncture group). The two groups were described as comparable for demographics including age and cause of infertility |
|
| Interventions | The study compared electro‐acupuncture (twice a week for two weeks, from cycle day 2 to the day prior to oocyte retrieval) with no acupuncture around the time of oocyte retrieval | |
| Outcomes | Outcome measures studied were clinical pregnancy and the pulsatility index (PI) of left and right uterine arteries | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | The study was designed to assess the impact of acupuncture on uterine artery blood flow and clinical pregnancy rate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | ‘randomly assigned to one of the two groups by selection of a sealed envelope.’ |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group received no treatment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30 randomised to acupuncture group, and 26 to control group (but 12 in the control group dropped out), leaving 30 in the acupuncture group and only 14 in the control group. |
| Selective reporting (reporting bias) | Unclear risk | No LBR outcome data reported. |
| Other bias | Low risk | None known |
Humaidan 2004.
| Methods | Randomised trial of fertility patients in Denmark | |
| Participants | 200 patients randomised to either electro‐acupuncture (n = 100) or conventional analgesia (n = 100) at the time of oocyte retrieval. Both groups also received a para‐cervical block. | |
| Interventions | Electro‐acupuncture at the time of oocyte retrieval, given by specially trained nurses, versus conventional analgesia control (benzodiazepine, alfentanil) | |
| Outcomes | VAS scale Clinical pregnancy rate | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Study designed to assess effectiveness of acupuncture as an analgesic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not stated |
| Allocation concealment (selection bias) | Low risk | Adequate: randomisation using sealed unlabelled envelopes containing a study number |
| Blinding (performance bias and detection bias) All outcomes | Low risk | ‘doctors and patients are blinded to the arm of treatment’. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 participants randomized; 8 in total withdrew from the study. |
| Selective reporting (reporting bias) | Unclear risk | LBR not a prestated outcome |
| Other bias | Low risk | None known |
Madaschi 2010.
| Methods | Randomised controlled trial of fertility patients in Brazil | |
| Participants | 416 patients stratified according to age and then randomised to either acupuncture group (n = 208) or control with no acupuncture (n = 208) | |
| Interventions | Needle acupuncture 25 minutes before and after embryo transfer versus no acupuncture control. Intervention performed by the same practitioner in all cases There was no statistically significant difference between the two groups for demographic characteristics. The average age (± SD) in the acupuncture group was 35.3 (± 4.7) compared to 34.6 (± 4.6) in the control group (p = 0.103). The average BMI in the acupuncture group was 22.4 (± 3.8) compared to 22.4 (± 2.9) in the control group (P = 0.951) The main causes of subfertility were ovarian disorders and male factor with no statistical significance between both groups for any cause of subfertility |
|
| Outcomes | Pregnancy rate, implantation rate, abortion rate and live birth rate | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘patients were randomized before the beginning of the ovarian stimulation according to computer generated randomized numbers ‘ |
| Allocation concealment (selection bias) | Unclear risk | method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had no treatment. It was not stated if the clinicians or the assessors of the study were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 416 participants were randomized; no drop out noted. |
| Selective reporting (reporting bias) | Unclear risk | LBR not a prestated outcome. |
| Other bias | Low risk | None |
Moy 2011.
| Methods | Randomized controlled trial of fertility patients in US | |
| Participants | 160 patients undergoing IVF ± ICSI were randomised to either true acupuncture (n = 87) or sham acupuncture (n = 74) The average age (± SD) in the true acupuncture group was 33.3 (± 0.307) years compared to 33.16 (± 0.334) years in the sham acupuncture group. There was no statistically significant difference in BMI or infertility diagnosis between the two groups, with the leading causes of infertility being male factor, ovarian dysfunction and unexplained. |
|
| Interventions | True (needle) acupuncture performed by hospital employed licensed acupuncturists versus sham placebo acupuncture. Both interventions performed for 25 minutes before and after embryo transfer | |
| Outcomes | Clinical pregnancy rate and clinical symptoms during embryo transfer | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | patients were randomized using a ‘random number generator’ |
| Allocation concealment (selection bias) | Low risk | Use of 'sealed, sequentially numbered, opaque envelopes’. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Control group was allocated to Sham acupuncture. The physicians and patients were blinded to the randomization until the conclusion of the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 participants were randomized; 1 lost to follow up |
| Selective reporting (reporting bias) | Unclear risk | LBR outcome data not reported. |
| Other bias | Low risk | None |
Paulus 2002.
| Methods | Randomised controlled trial in fertility clinic in Germany | |
| Participants | 160 patients randomised: 80 to treatment and 80 to no intervention control. The age of the women (± SD) in the control group (n = 80) was 32.1 years (± 3.9) compared to 32.8 years (± 4.1) in the acupuncture group (n = 80). In the control group the average number of previous cycles was 2.0 (± 2.0) versus 2.1 (± 2.1) in the treatment group. Most women had tubal disease, followed by male factor infertility then polycystic ovarian disease. These were in equal portions in both the study and control groups. |
|
| Interventions | Acupuncture performed by "well‐trained examiners" 25 min before and after embryo transfer for treatment group; auricular acupuncture also performed on the treatment group | |
| Outcomes | Clinical pregnancy rates | |
| Assisted conception protocols | Protocol breakdown not given | |
| Notes | Same authors as Paulus 2003 but different group of patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not stated how the allocation was carried out. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had no treatment. Not stated if clinicians or assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 randomised; no drop out. |
| Selective reporting (reporting bias) | Unclear risk | Not known whether LBR a prestated outcome |
| Other bias | Low risk | None |
Paulus 2003.
| Methods | Randomised placebo‐controlled trial; abstract only | |
| Participants | Patients were divided into two groups by random selection: embryo transfer with verum acupuncture (n = 100) and embryo transfer with placebo needling (n = 100). No demographic details presented |
|
| Interventions | Acupuncture or sham acupuncture performed for 25 minutes before and after embryo transfer. In the control group (n=100) a placebo needle set was used without penetrating the skin, but at the same acupoints and after the same scheme | |
| Outcomes | Clinical pregnancy rates | |
| Assisted conception protocols | Protocol breakdown not given | |
| Notes | Only included women with good embryos | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Abstract only, not stated |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Control group had placebo needling. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100 participants were randomized. No drop out reported. |
| Selective reporting (reporting bias) | Unclear risk | Not known whether LBR a prestated outcome |
| Other bias | Low risk | None |
Sator‐K 2006.
| Methods | Randomised controlled trial in fertility clinic in Austria | |
| Participants | Patients were randomised in proportions of 1:1:1 to treatment with electro‐acupuncture (n = 32), auricular acupuncture without electrical stimulation (n = 32) or a control group without needles or electrical stimulation (n = 30). The mean ages (± SD) of the women undergoing IVF treatment in the group receiving electro‐acupuncture with remifentanil (EA), acupuncture with remifentanil (A), and remifentanil with placebo (CO) were 33.3 years (± 1.7), 34.2 years (± 1.1) and 33.9 years (± 1.9), respectively. There were no differences in the number of failed cycles or causes of subfertility. |
|
| Interventions | EA, or EA with electrical stimulation or control of conventional analgesia (remifentanil) at the time of oocyte retrieval | |
| Outcomes | Pain intensity and subjective well being were assessed using a visual analogue scale Nausea and tiredness were also assessed using a visual rating scale Analgesic drug requirements during the entire study period | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Study designed to assess effectiveness of acupuncture as an analgesic Each P‐Stim™ was programmed by an independent technician for electrical stimulation or no stimulation before the study. To ensure blinding of the investigator, each P‐Stim™ was packed in a non‐transparent case in which the respective permanent needles or adhesive tapes were also included. The packages were numbered consecutively, according to the randomisation list. Patients and investigators were blinded to the randomisation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer generated sequence randomisaton |
| Allocation concealment (selection bias) | Unclear risk | ‘Randomisation was concealed until at least 30 patients were randomized.’ ‘Patients and investigators were blinded to the randomisation’. Method of allocation concealment not clearly reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had traditional I.V. pain relief. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 94 were randomized. 1 drop out. |
| Selective reporting (reporting bias) | Unclear risk | LBR outcome not reported. |
| Other bias | Low risk | None known |
Smith 2006.
| Methods | Randomised controlled trial in fertility clinic in Australia | |
| Participants | 228 randomised, 36 excluded: 110 in treatment group and 118 in control group. The average age of the control group (± SD) was 35.9 years (± 4.7) versus 36.1 years (± 4.8) in the study group; there were no differences in the number of previous treatment cycles, BMI, duration of subfertility. |
|
| Interventions | All women had 3 sessions: day 9 of stimulation, immediately before ET, and immediately after ET. For the sham acupuncture group a sham needle was used close to but not on the treatment point | |
| Outcomes | Clinical pregnancy rates | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | After 3rd session, 24 in treatment group and 10 in control group guessed their allocation group correctly | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘randomization was in balanced, variable blocks of random size prepared by a researcher not involved in the trial’. |
| Allocation concealment (selection bias) | Unclear risk | Not stated specifically |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Control groups had placebo needles (Streitberger) although after the 3rd session, 24 in the treatment group and 10 in the control group guessed their allocation group correctly. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 228 subjects were randomized. 36 women had to be withdrawn (15%). |
| Selective reporting (reporting bias) | Unclear risk | LBR data not reported. |
| Other bias | Low risk | None known |
So 2009.
| Methods | Randomised controlled trial of fertility patients in Hong Kong | |
| Participants | 370 patients undergoing assisted reproductive treatment randomised to either acupuncture (n = 185) or placebo acupuncture arms (n = 185). The median age (interquartile range) in the acupuncture and placebo groups respectively was 36 (33 ‐ 38) and 36 (34 ‐ 38). Mean BMI (± SD) was similar at 21.6 (± 2.1) and 21.7 (± 2.7) kg/m2 for acupuncture and placebo groups respectively. Both groups were comparable in terms of duration of infertility, cause of infertility, previous experience of acupuncture and smoking habit |
|
| Interventions | Needle acupuncture or placebo needle acupuncture for 25 minutes before and after embryo transfer. Intervention performed by a certified Chinese acupuncturist with a degree in Chinese Medicine and 3 years experience | |
| Outcomes | Pregnancy rate, clinical pregnancy rate, live birth rate, miscarriage rate | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized by a computer generated randomization list |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes from the list used. ‘The sequence of randomization was concealed until interventions were assigned.’ |
| Blinding (performance bias and detection bias) All outcomes | Low risk | ‘patients, clinical staff involved in the care of patients and embryologist were blinded to the treatment group assigned’. The codes were only revealed after the completion of the entire study. Control group also had placebo needles. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 370 participants randomized; all completed the study. |
| Selective reporting (reporting bias) | Low risk | None known. |
| Other bias | Low risk | None known |
So 2010.
| Methods | Randomised controlled trial of fertility patients undergoing frozen embryo transfer in Hong Kong | |
| Participants | 226 patients randomised to either real (n = 113) or placebo acupuncture (n=113). The median age at thawing was 36 (34 ‐ 38) and 36 (34 ‐ 39) years for real and placebo acupuncture respectively. The BMI, duration and cause of infertility and previous experience of acupuncture were also comparable between the two groups. |
|
| Interventions | Needle acupuncture according to TCM principles or placebo acupuncture with Streitberger's sham placebo needles. Intervention performed by a certified Chinese acupuncturist with a degree in Chinese Medicine and 3 years experience | |
| Outcomes | Overall pregnancy rate, clinical pregnancy rate, ongoing pregnancy rate, live birth rate | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | More patients in placebo group correctly guessed their randomisation compared to the true acupuncture group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | participants were randomized by a computer generated randomization list |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes from the list was used. ‘The sequence of randomization was concealed until interventions were assigned.’ |
| Blinding (performance bias and detection bias) All outcomes | Low risk | ‘patients, clinical staff involved in the care of patients and embryologist were blinded to the treatment group assigned’. The codes were only revealed after the completion of the entire study. Control group also had placebo needles. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 226 participants randomized. All completed the study. |
| Selective reporting (reporting bias) | Low risk | LBR available. |
| Other bias | Low risk | None known |
Stener‐Victorin 1999.
| Methods | Randomised controlled trial, conducted in Sweden | |
| Participants | 150 women undergoing IVF and ET were randomised to receive either electro‐acupuncture and a paracervical block or alfentanil analgesia and a paracervical block. The mean ages (range) of the study and control groups were 33.3 years (25 to 42) and 34.4 years (25 to 46). There was no difference in the two groups in terms of the cause of subfertility and the number of previous cycles. |
|
| Interventions | Acupuncture was performed at least 30 min before oocyte aspiration and PCB was placed at the start of the procedure and terminated directly after oocyte aspiration | |
| Outcomes | VAS, level of stress, implantation and pregnancy rates | |
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Study designed to assess effectiveness of acupuncture as an analgesic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each centre randomized its patients using sealed, unlabelled envelopes" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | ‘sealed unlabelled envelope’ |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had traditional analgesia and t (Alfentanil + para cervical block) therefore blinding nor possible for clinicians or participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 150 women were randomized. 1 drop out. |
| Selective reporting (reporting bias) | Unclear risk | LBR data not reported. |
| Other bias | Unclear risk | "There is a possible bias in the study in that some of the women in the EA group were administered additional alfentanil during oocyte aspiration." |
Stener‐Victorin 2003.
| Methods | Randomised, controlled multi‐centre trial in Sweden | |
| Participants | Women were randomised to either electro‐acupuncture and a paracervical block or alfentanil and a paracervical block, as analgesia at the time of oocyte retrieval. The mean age (range) in the study group was 32.9 years (22 to 38) and for the control group it was 32.9 years (25 to 38). The causes of infertility and number of IVF attempts did not differ between the two groups. |
|
| Interventions | Women were given EA and a PCB of lidocaine hydrochloride during oocyte aspiration. Those women randomised to the alfentanil group were given alfentanil and a PCB during oocyte aspiration. The acupuncture stimulation began at least 30 min before oocyte aspiration | |
| Outcomes | VAS were used for pain assessment Other variables recorded included abdominal pain, pain during placement of PCB, time of discomfort, adequacy of analgesia, stress level, nausea. IVF outcomes were pregnancy rate (number of pregnancies per embryo transfer), implantation rate (number of gestational sacs per number of transferred oocytes) and on‐going pregnancies (number of pregnancies per embryo transfer after the 16th week of gestation) |
|
| Assisted conception protocols | Protocol breakdown not provided | |
| Notes | Stopped after interim analysis as results show no difference between two groups. Study designed to assess effectiveness of acupuncture as an analgesic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | ‘sealed unlabeled envelopes’ |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had paracervical block + Alfentanil and therefore blinding nor possible for clinicians or participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 286 randomized; 5 in the acupuncture group and 7 in the control group dropped out. |
| Selective reporting (reporting bias) | Unclear risk | Not known whether LBR a prestated outcome |
| Other bias | Low risk | None |
Westergaard 2006.
| Methods | Randomised controlled trial with patients from private clinic in Denmark | |
| Participants | 273 women randomised: 87 allocated to no acupuncture and 95 to acupuncture on ET day only; 91 to acupuncture on ET and ET+2 days; 27 excluded, The average ages of the three groups of women were: 37 years (27 to 45) in the control (n = 87) group, 37 years (24 to 45) in the group who had acupuncture on the day of ET (n = 95), and 37 years (27 to 45) for those with repeated acupuncture (ET + 2) (n = 91). There was no difference in the BMI between the three groups and about 67% of women had one or more attempts of IVF in the three groups. The main causes of subfertility were described as male factor or unexplained |
|
| Interventions | Acupuncture was performed by specially trained nurses on patients undergoing ET on the day of ET, ET+2 and not on controls | |
| Outcomes | Clinical pregnancy rate on ultrasound | |
| Assisted conception protocols | Standard, long protocol GnRH down‐regulation and the follicle stimulating hormone (FSH) or human menopausal gonadotrophin (hMG) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation procedure handled by nurse not involved in study |
| Allocation concealment (selection bias) | Unclear risk | ‘drawing of sealed envelope’ ‐ no further details reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Control group had paracervical block, so blinding of the participants and personnel not possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 300 participants randomized. 27 dropped out leaving 273 participants for analysis. |
| Selective reporting (reporting bias) | Unclear risk | LBR data not prestated outcome. |
| Other bias | Low risk | none |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Chen 2004 | No reply to written and electronic request; study design, allocation concealment and outcomes unclear |
| Chen 2009 | No reply to electronic request; study design, methods and results not known |
| Chen 2012 | No outcomes of interest |
| Cui 2007 | No reply to electronic request; study design, methods and results not known |
| Cui 2011 | Inadequate randomisation process in study design, based on odd and even numbers |
| Evans 2005 | Lack details on pregnancy outcome, study design, allocation concealment and type of randomisation; no reply to written or electronic letters |
| Feliciani 2011 | No reply to electronic request; study numbers, randomisation process and outcomes unclear |
| Li 2009 | No reply to electronic request; study design, methods and results not known |
| Omodei 2010 | No reply to electronic request; study design, allocation concealment and outcomes unclear |
| Quintero 2004 | Lacks details on allocation concealment and randomisation, no reply to requests for details; crossover design |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12611000226909.
| Trial name or title | Acupuncture compared to sham acupuncture and standard care to improve live birth rates for women undergoing IVF: a randomised controlled trial |
| Methods | Parallel design, randomised controlled trial |
| Participants | Women aged less than 43 years, undergoing a fresh IVF or ICSI cycle, and restricted to women with the potential for a lower live birth rate defined as > 2 previous unsuccessful embryo transfers (fresh or frozen), and unsuccessful clinical pregnancies of quality embryos deemed by the embryologist to have been suitable for freezing by standard criteria |
| Interventions | Needle or sham acupuncture for 1 hr on day 6‐8 of the IVF cycle, plus two treatments on the day of the embryo transfer, 30 minutes before and after embryo transfer. Compared to no treatment control |
| Outcomes | Primary outcome: live birth ‐ defined as the delivery of one or more living infants, greater than 20 weeks gestation or 400 grams or more birth weight. Secondary outcomes: 1. clinical pregnancy defined as demonstration of fetal heart activity on ultrasound scan 2. miscarriage defined as a non viable pregnancy prior to 12 weeks gestation 3. quality of life 4. self efficacy |
| Starting date | Registration: 02/03/2011 |
| Contact information | Caroline Smith Centre for Complementary Medicine Research University of Western Sydney Locked Bag 1797 Penrith South DC NSW 2751, Australia |
| Notes |
IRCT201011275181N4.
| Trial name or title | Effects of acupuncture on outcome of in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) in women with polycystic ovarian ‐ |
| Methods | Parallel design, triple blind, randomised controlled trial |
| Participants | Inclusion criteria: women with the diagnosis of PCO (Rotterdam criteria) admitted to the clinic for IVF or ICSI treatments of infertility |
| Interventions | Intervention group 1: acupuncture based on Traditional Chinese Medicine, 5 sessions of thirty minutes. Intervention 2: Control group: (placebo) the same needles are used in 5 sessions of thirty minutes |
| Outcomes | Primary outcomes: Embryo quality. Timepoint: 2 days after embryo transfer. Method of measurement: diagnosed by Embryologist and with embryological criteria. Oocyte fertilisation rate. Timepoint: first day after embryo transfer. Method of measurement: diagnosed by embryologist and with embryological criteria Oocyte metaphase 2. Timepoint: before and after embryo transfer. Method of measurement: diagnosed by embryologist and with embryological criteria Secondary outcomes: Biochemical pregnancy. Timepoint: 2 weeks after embryo transfer. Method of measurement: B‐hCG Clinical pregnancy. Timepoint: 4 weeks after embryo transfer. Method of measurement: sac observed in vaginal sonography Miscarriage. Timepoint: <12 weeks after embryo transfer. Method of measurement: vaginal sonography Take home baby. Timepoint: 9 months after embryo transfer. Method of measurement: Delivery |
| Starting date | Registration 13/04/2011 |
| Contact information | Rashidi Batool Address: Tehran University of Medical Sciences, Valieasr Hospital and Imam Khomeini Hospital Tehran Islamic Republic of Iran |
| Notes |
NCT00317317.
| Trial name or title | The Effect of Acupuncture on Infertility With In‐Vitro Fertilization (IVF) Patients |
| Methods | Parallel design, single‐blinded randomised controlled trial |
| Participants | Inclusion criteria: ‐ Undergoing in vitro fertilisation protocol (both IVF and intracytoplasmic sperm injection ‐ ICSI) ‐ Acupuncture naive ‐ Basal FSH <10 ‐ Minimum age 21 years |
| Interventions | Acupuncture |
| Outcomes | Primary outcome: Clinical pregnancy rate Secondary outcomes: ‐ B‐endorphin levels ‐ Miscarriage rate ‐ Stress measurement ‐ Take home baby rate |
| Starting date | Registration: 20/06/2006 |
| Contact information | Grant Zhang, Ph.D. Center For Integrative Medicine, University of Maryland |
| Notes |
NCT01449396.
| Trial name or title | Chinese Traditional Medicine Contribution to Improve In‐vitro Fertilization (IVF) Results: Acupuncture in Embryo Transfer |
| Methods | Parallel design, double‐blinded, randomised controlled trial |
| Participants | Inclusion criteria: ‐ 18 to 35 years old ‐ BMI 20‐25 ‐ Medical indication of intracytoplasmic sperm injection (ICSI) treatment to treat sterility ‐ No previous in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI) treatments ‐ No previous experience of acupuncture treatments ‐ Make cause of sterility ‐ At least one high quality embryo on the day of uterine transfer |
| Interventions | Acupuncture versus bed rest |
| Outcomes | Primary outcome: pregnancy rate Secondary outcomes: ‐ Analysis of the results of assisted reproductive cycle ‐ Determination of serum prolactin and 24h urine cortisol ‐ Endometrial vascularisation study ‐ Rating preconceived ideas about acupuncture |
| Starting date | Registered: 04/10/2011 |
| Contact information | Monica Romeu romeu_monvil@gva.es |
| Notes |
NCT01608048.
| Trial name or title | Transcutaneous Electrical Acupoint Stimulation to Improve Pregnancy Rates for Women Undergoing in Vitro Fertilization |
| Methods | Single blind RCT |
| Participants | Women undergoing IVF |
| Interventions | Transcutaneous electrical acupoint stimulation vs no acupuncture |
| Outcomes | Live birth, clinical pregnancy |
| Starting date | May 2012 |
| Contact information | Cui Hong Zheng, Doctor ph: 86‐27‐83663275 email: 635342693@qq.com |
| Notes |
Differences between protocol and review
In the 2013 update the following changes were made.
A third comparison was added ‐ acupuncture versus acupuncture + ART.
Ongoing pregnancy and clinical pregnancy rates were moved from primary to secondary outcomes.
The methodology section was rewritten with subheadings.
Contributions of authors
Ying Cheong developed the selection criteria, wrote the review and performed the analysis. Ernest Ng co‐authored the review. William Ledger acted as a moderator for the meta‐analysis and co‐wrote the review. Sarah Dix performed the analysis, and co‐wrote the review.
Sources of support
Internal sources
None, Not specified.
External sources
-
Cochrane Menstrual and Subfertility Group, New Zealand.
Support of search strategy, advice, refereeing and proof reading
Declarations of interest
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Andersen 2010 {published data only}
- Andersen D, Lossl K, Nyboe Andersen A, Furbringer J, Bach H, Simonsen J, et al. Acupuncture on the day of embryo transfer: a randomized controlled trial of 635 patients. Reproductive Biomedicine Online 2010;21(3):366‐72. [DOI] [PubMed] [Google Scholar]
Benson 2006 {published data only}
- Benson MR, Elkind‐Hirsch KE, Theall A, Fong K, Hogan RB, Scott RT. Impact of acupuncture before and after embryo transfer on the outcome of in vitro fertilization cycles: A prospective single blind randomized study. Fertility and Sterility 2006;86(3 Suppl):135. [Google Scholar]
Craig 2007 {published data only (unpublished sought but not used)}
- Craig LB, Criniti AR, Hansen KR, Marshall LA, Soules MR. Acupuncture lowers pregnancy rates when performed before and after embryo transfer. Fertility and Sterility 2007;88 Suppl 1:40. [Google Scholar]
Dieterle 2006 {published data only}
- Dieterle S, Ying G, Hatzmann W, Neuer A. Effect of acupuncture on the outcome of in vitro fertilisation and intracytoplasmic sperm injection: a randomised, prospective, controlled clinical study. Fertility and Sterility 2006;85:1347‐51. [DOI] [PubMed] [Google Scholar]
Domar 2009 {published data only}
- Domar A, Meshay I, Kelliher J, Alper M, Powers RD. The impact of acupuncture on in vitro fertilization outcome. Fertility and Sterility 2009;91(3):723‐6. [DOI] [PubMed] [Google Scholar]
Fraterelli 2008 {published data only}
- Fratterelli JL, Leondires MR, Fong K, Theall A, Locatelli S, Scott RT. Laser acupuncture before and after embryo transfer improves art delivery rates: results of a prospective randomized double‐blinded placebo controlled five‐armed trial involving 1000 patients. Fertility and Sterility 2008;90 Suppl 1:105. [Google Scholar]
Gejervall 2005 {published data only}
- Gejervall A, Stener‐Victorin E, Moller A, Janson PO, Werner C, Bergh C. Electro‐acupuncture versus conventional analgesia: a comparison of pain levels during oocyte aspiration and patients’ experiences of well‐being after surgery. Human Reproduction 2005;20:728‐35. [DOI] [PubMed] [Google Scholar]
Ho 2009 {published data only}
- Ho M, Huang LC, Chang YY, Chen HY, Chang WC, Yang TC, Tsai HD. Electroacupuncture reduces uterine artery blood flow impedance in infertile women. Taiwanese Journal of Obstetrics and Gynecology 2009;48(2):148‐51. [DOI] [PubMed] [Google Scholar]
Humaidan 2004 {published data only}
- Humaidan P, Stener‐Victorin E. Pain relief during oocyte retrieval with a new short duration electro‐acupuncture technique ‐ an alternative to conventional analgesic methods. Human Reproduction 2004;19:1367‐72. [DOI] [PubMed] [Google Scholar]
Madaschi 2010 {published data only}
- Madaschi C, Braga DP, Figueira Rde C, Iaconelli A Jr, Borges E Jr. Effect of acupuncture on assisted reproduction treatment outcomes. Acupuncture in Medicine 2010;28(4):180‐4. [DOI] [PubMed] [Google Scholar]
Moy 2011 {published data only}
- Moy I, Milad MP, Barnes R, Confino E, Kazer RR, Zhang X. Randomized controlled trial: effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization. Fertility and Sterility 2011;95(2):583‐7. [DOI] [PubMed] [Google Scholar]
Paulus 2002 {published data only}
- Paulus WE, Zhang M, Strehler E, El‐Danasouri I, Sterzik K. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproductive technology. Fertility and Sterility 2002;77:721‐44. [DOI] [PubMed] [Google Scholar]
Paulus 2003 {published data only}
- Paulus WE, Zhang M, Strehler E, Seybold B, Sterzik K. Placebo‐controlled trial acupuncture effects in assisted reproductive therapy. Human Reproduction 2003; Vol. 18 Suppl:18.
Sator‐K 2006 {published data only}
- Sator‐Katzenschlager SM, Wölfler MM, Kozek‐Langenecker SA, Sator K, Sator PG, Li B, et al. Auricular electro‐acupuncture as an additional perioperative analgesic method during oocyte aspiration in IVF treatment. Human Reproduction 2006;21:2114‐20. [DOI] [PubMed] [Google Scholar]
Smith 2006 {published data only}
- Smith C, Coyle M, Norman R. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertility and Sterility 2006;85:1352‐8. [DOI] [PubMed] [Google Scholar]
So 2009 {published data only}
- So EW, Ng EH, Wong YY, Lau EY, Yeung WS, Ho PC. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Human Reproduction 2009;24(2):341‐8. [DOI] [PubMed] [Google Scholar]
So 2010 {published data only}
- So EW, Ng EH, Wong YY, Yeong WS, Ho PC. Acupuncture for frozen‐thawed embryo transfer cycles: a double‐blind randomized controlled trial. Reproductive Biomedicine Online 2010;20(6):814‐21. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 1999 {published data only}
- Stener‐Victorin E, Waldenstrom U, Andersson SA, Wikland M, Janson PO. A prospective randomised study of electro‐acupuncture versus alfentanil as anaesthesia during oocyte aspiration in in‐vitro fertilisation. Human Reproduction 1999;14:2480‐4. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 2003 {published data only}
- Stener‐Victorin E, Waldenstrom U, Wikland M, Nilsson L, Hagglund L, Lundeberg T. Electro‐acupuncture as a preoperative analgesic method and its effects on implantation rate and neuropeptide Y concentrations in follicular fluid. Human Reproduction 2003;18:1454‐60. [DOI] [PubMed] [Google Scholar]
Westergaard 2006 {published data only}
- Westergaard LG, Mao QH, Krogslund M, Sandrini S, Lenz S, Grinsted J. Acupuncture on the day of embryo transfer significantly improves the reproductive outcome in infertile women: a prospective, randomised trial. Fertility and Sterility 2006;85:1341‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Chen 2004 {published data only}
- Chen D, Shi XL, Cai MX. Clinical observation on treatment of functional anovulation by acupunctural prick. Zhongguo Zhong Xi Yi Jie He Za Zhi Zhongxiyi Jiehe Zazhi 2004;27(8):735‐7. [PubMed] [Google Scholar]
Chen 2009 {published data only (unpublished sought but not used)}
- Chen J, Liu L, Cui W, Sun W. Effects of electro‐acupuncture on in vitro fertilization‐embryo transfer (IVF‐ET) of patients with poor ovarian response. Zhongguo Zhen Jiu 2009;29(10):775‐9. [PubMed] [Google Scholar]
Chen 2012 {published data only}
- Chen QQ, Wei QL, Zhang XH. Effects of electroacupuncture on supplementary analgesia and improvement of adverse reactions induced by dolantin in oocyte retrieval. Zhongguo zhen jiu (Chinese acupuncture & moxibustion) 2012;32(12):1113‐6. [PubMed] [Google Scholar]
Cui 2007 {published data only (unpublished sought but not used)}
- Cui W, Sun W, Liu L, Wen J. Study of the effect of electro‐acupuncture treatment on the patients undergoing in vitro‐fertilisation and embryo transfer. Chinese Maternal and Child Health 2007;22:3403‐5. [Google Scholar]
Cui 2011 {published data only}
- Cui W, Li J, Sun W, Wen J. Effect of electroacupuncture on oocyte quality and pregnancy for patients with PCOS undergoing in vitro fertilization and embryo transfer. Chinese Acupuncture & Moxibustion 2011;31(8):687‐91. [PubMed] [Google Scholar]
Evans 2005 {published data only}
- Evans J. A pilot study to explore the effects of acupuncture in women with unexplained infertility. South Bro Tak R&D Consortium 2005.
Feliciani 2011 {published data only}
- Feliciani E, Ferraretti A, Paesano C, Pellizzaro E, Magli M, Gianardi L. The role of acupuncture in ART: preliminary results of an ongoing prospective randomised study. Human Reproduction 2011;26 Suppl 1:281. [Google Scholar]
Li 2009 {published data only}
- Li J, Cui W, Sun W. Effects of electroacupuncture of in vitro fertilisation‐embryo transfer (IVF‐ET) of patients with polycystic ovarian syndrome. Chinese Journal of Human Sexuality 2009;18(8):33‐5. [Google Scholar]
Omodei 2010 {published data only}
- Omodei U, Piccioni G, Tombesi S, Dordoni D, Fallo L, Ghilardi F. Effect of acupuncture on rates of pregnancy among women undergoing in vitro fertilisation. Fertility and Sterility 2010;94:Suppl 1. [Google Scholar]
Quintero 2004 {published data only}
- Quintero R. A randomised controlled, double‐blind, cross‐over study evaluating acupuncture as an adjunct to IVF. Fertility and Sterility 2004;81 Suppl 3:11. [Google Scholar]
References to ongoing studies
ACTRN12611000226909 {published data only}
- Smith C. Acupuncture compared to sham acupuncture and standard care to improve live birth rates for women undergoing IVF: a randomised controlled trial [Acupuncture compared to sham acupuncture and standard care to improve live birth rates for women undergoing IVF: a randomised controlled trial]. http://www.anzctr.org.au/ACTRN12611000226909.aspx Registered 02/03/2011.
- Smith CA, Lacey S, Chapman M, Ratcliffe J, Norman RJ, Johnson N, Sacks G, Lyttleton J, Boothroyd C. Acupuncture to improve live birth rates for women undergoing in vitro fertilization: a protocol for a randomized controlled trial. Trials 2012;13:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT201011275181N4 {published data only}
- Batool R. Effects of acupuncture on outcome of in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) in women with polycystic ovarian. http://www.irct.ir/searchresult.php?id=5181&number=4 Registered 13/04/2011.
NCT00317317 {published data only}
- Zhang G. The Effect of Acupuncture on Infertility With In‐Vitro Fertilization (IVF) Patients. http://clinicaltrials.gov/show/NCT00317317 Registered 20/04/2006.
NCT01449396 {published data only}
- Romeu M. Chinese Traditional Medicine contribution to improve in‐vitro fertilization (IVF) results: acupuncture in embryo transfer. http://clinicaltrials.gov/show/NCT01449396 Registered 04/10/2011.
NCT01608048 {unpublished data only}
- Zheng CH. Transcutaneous Electrical Acupoint Stimulation to Improve Pregnancy Rates for Women Undergoing in Vitro Fertilization. http://www.clinicaltrials.gov/ct2/show/NCT01608048?term=acupuncture&type=Intr&outc=pregnancy&gndr=Female&age=1&rcv_s=10%2F01%2F2011&rcv_e=10%2F01%2F2013&rank=5 2012. [DOI] [PMC free article] [PubMed]
Additional references
Anderson 2007
- Anderson BJ, Haimovici F, Ginsburg ES, Schust DJ, Wayne PM. In vitro fertilization and acupuncture: clinical efficacy and mechanistic basis. Alternative Therapies in Health and Medicine 2007;13(3):38‐48. [PubMed] [Google Scholar]
Boivin 2007
- Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment‐seeking: potential need and demand for infertility medical care. Human Reproduction 2007;22:1506‐12. [DOI] [PubMed] [Google Scholar]
Cheong 2010
- Cheong Y, Nardo LG, Rutherford T, Ledger W. Acupuncture and herbal medicine in in vitro fertilisation: a review of the evidence for clinical practice. Human Fertility 2010;13(1):3‐12. [DOI] [PubMed] [Google Scholar]
Domar 2011
- Domar AD, Rooney KL, Wiegand B, Orav EJ, Alper MM, Berger BM, et al. Impact of a group mind/body intervention on pregnancy rates in IVF patients. Fertility and Sterility 2011;95:2269‐73. [DOI] [PubMed] [Google Scholar]
El‐Toukhy 2010
- El‐Toukhy T, Khalaf Y. A new study of acupuncture in IVF: pointing in the right direction. Reproductive Biomedicine Online 2010;3:278‐9. [DOI] [PubMed] [Google Scholar]
Fisher 1994
- Fisher P, Ward A. Complementary medicine in Europe. BMJ 1994;309:107‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garcia 2013
- Garcia MK, McQuade J, Haddad R, Patel S, Lee R, Yang P, et al. Systematic review of acupuncture in cancer care: a synthesis of the evidence. Journal of Clinical Oncology 2013;31(7):952‐60. doi: 10.1200/JCO.2012.43.5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
He et al, 2012
- Wenju He, Xue Zhao, Yanqi Li, Qiang Xi, Yi Guo. Adverse events following acupuncture: A systematic review of the Chinese literature for the years 1956–2010. The Journal of Alternative and Complementary Medicine 2012;18(10):892‐901. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Holmer 2012
- Holmér Pettersson P, Wengström Y. Acupuncture prior to surgery to minimise postoperative nausea and vomiting: a systematic review. Journal of Clinical Nursing 2012;21(13‐14):1799‐805/ doi: 10.1111/j.1365‐2702.2012.04114.x.. [DOI] [PubMed] [Google Scholar]
Huang 2011
- Huang DM, Huang GY, Lu FE, Stefan D, Andreas N, Robert G. Acupuncture for infertility: is it an effective therapy?. Chinese Journal of Integrative Medicine 2011;17(5):386‐95. [DOI] [PubMed] [Google Scholar]
Klein 2012
- Klein SD, Frei‐Erb M, Wolf U. Usage of complementary medicine across Switzerland: results of the Swiss Health Survey 2007. Swiss Medical Weekly 2012;142:w13666. [DOI] [PubMed] [Google Scholar]
MacPherson 2010
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. Journal of Evidence‐Based Medicine 2010;3(3):140‐55. [DOI] [PubMed] [Google Scholar]
Manheimer 2008
- Manheimer E, Zhang G, Udoff L, Haramati A, Langenberg P, Berman BM. Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta‐analysis. BMJ 2008;336(7643):545‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meissner 2007
- Meissner K, Distel H, Mitzdorf U. Evidence for placebo effects on physical but not on biochemical outcome parameters: a review of clinical trials. BMC Medicine 2007;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meldrum 2013
- Meldrum DR, Fisher AR, Butts SF, Su HI, Sammel MD. Acupuncture‐help, harm, or placebo?. Fertility and Sterility 2013:doi:pii: S0015‐0282(13)00008‐3. 10.1016/j.fertnstert.2012.12.046.. [DOI] [PubMed] [Google Scholar]
NIH Consensus 1998
- NIH Concensus Development Panel of Acupuncture. Acupuncture. JAMA 1998;280:1518‐24. [PubMed] [Google Scholar]
Schmidt 1995
- Schmidt L, Munster K, Helm P. Infertility and the seeking of infertility treatment in a representative population. British Journal of Obstetrics and Gynaecology 1995;102:978‐84. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 1996
- Stener‐Victorin E, Waldenstrom U, Andersson SA, Wikland M. Reduction of blood flow impedence in the uterine arteries of infertile women with electro‐acupuncture. Human Reproduction 1996;11:1314‐7. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 2000
- Stener‐Victorin E, Lundeberg T, Waldenstrom U, Tagnfors U, Lundeberg T, Lindstedt G, Janson P. Effects of electro‐acupuncture on anovulation in women with polycystic ovary syndrome. Acta Obstetricia et Gynecologica Scandinavica 2000;79:180‐8. [PubMed] [Google Scholar]
Stener‐Victorin 2001
- Stener‐Victorin E, Lundeberg T, Waldenstrom U, Bileviciute‐Lindstedt I, Janson P. Effects of acupuncture on corticotropin releasing factor (CRF) in rats with experimentally induced polycystic ovaries. Neuropeptides 2001;6:1‐5. [DOI] [PubMed] [Google Scholar]
Tan 2011
- Tan CW, Sheehan P, Santos D. Discrimination accuracy between real and sham needles using the Park sham device in the upper and lower limbs. Acupuncture in Medicine 2011;29(3):208‐14. [DOI] [PubMed] [Google Scholar]
Thomas 2001
- Thomas KJ, Nicholl JP, Coleman P. Use and expenditure on complimentary medicine in England: a population based survey. Complementary Therapies in Medicine 2001;9:2‐11. [DOI] [PubMed] [Google Scholar]
Vickers 1999
- Vickers A, Zollman C. ABC of complementary medicine: Acupuncture. BMJ 1999;319:973‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zheng 2012
- Zheng CH, Huang GY, Zhang MM, Wang W. Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization: a systematic review and meta‐analysis. Fertility and Sterility 2012;97(3):599‐611. [DOI] [PubMed] [Google Scholar]


