Abstract
Background and Aims:
Artificial intelligence (AI) chatbots like Conversational Generative Pre-trained Transformer (ChatGPT) have recently created much buzz, especially regarding patient education. Such informed patients understand and adhere to the management and get involved in shared decision making. The accuracy and understandability of the generated educational material are prime concerns. Thus, we compared ChatGPT with traditional patient information leaflets (PILs) about chronic pain medications.
Methods:
Patients' frequently asked questions were generated from PILs available on the official websites of the British Pain Society (BPS) and the Faculty of Pain Medicine. Eight blinded annexures were prepared for evaluation, consisting of traditional PILs from the BPS and AI-generated patient information materials structured similar to PILs by ChatGPT. The authors performed a comparative analysis to assess materials’ readability, emotional tone, accuracy, actionability, and understandability. Readability was measured using Flesch Reading Ease (FRE), Gunning Fog Index (GFI), and Flesch-Kincaid Grade Level (FKGL). Sentiment analysis determined emotional tone. An expert panel evaluated accuracy and completeness. Actionability and understandability were assessed with the Patient Education Materials Assessment Tool.
Results:
Traditional PILs generally exhibited higher readability (P values < 0.05), with [mean (standard deviation)] FRE [62.25 (1.6) versus 48 (3.7)], GFI [11.85 (0.9) versus 13.65 (0.7)], and FKGL [8.33 (0.5) versus 10.23 (0.5)] but varied emotional tones, often negative, compared to more positive sentiments in ChatGPT-generated texts. Accuracy and completeness did not significantly differ between the two. Actionability and understandability scores were comparable.
Conclusion:
While AI chatbots offer efficient information delivery, ensuring accuracy and readability, patient-centeredness remains crucial. It is imperative to balance innovation with evidence-based practice.
Keywords: AI, artificial intelligence, analgesia, ChatGPT, chronic pain, medication adherence, patient education, readability
INTRODUCTION
The rise of artificial intelligence (AI) chatbots in medical literature has sparked interest in their potential for patient education. These chatbots, powered by large language models (LLMs) like Conversational Generative Pre-trained Transformer (ChatGPT), hold promise in delivering medical information to patients. However, despite their potential benefits, concerns exist regarding the accuracy and reliability of AI-generated content due to inherent limitations in language models.[1]
Traditionally, patient information leaflets (PILs) have been crafted by subject experts to educate patients and the general population about various medical conditions and treatments. These PILs are meticulously curated to ensure accuracy, reliability, and relevance, thereby minimising the risk of misinformation and its potential consequences.[2]
The implications of inaccuracies in patient education materials are profound, potentially leading to misunderstandings, treatment errors, and harmful consequences.[3] While AI chatbots offer streamlined information delivery, their reliability and accuracy require scrutiny to ensure patient safety. Moreover, in a landscape where search engines and online encyclopaedias often provide overwhelming and jargon-heavy information, the appeal of AI chatbots lies in offering clear and user-friendly explanations to patients seeking clarity.[4]
In this study, we compared patient information materials from ChatGPT and reputable sources such as the British Pain Society (BPS) and the Faculty of Pain Medicine (FPM). We focussed specifically on common pain medications prescribed for conditions such as neuropathic pain and depression, including amitriptyline, duloxetine, non-steroidal anti-inflammatory drugs (NSAIDs), and pregabalin.[5] Thus, the study’s primary objective was to compare the accuracy and completeness of the patient education materials generated by ChatGPT with those from established sources like the BPS. The other objectives were to assess the readability, emotional tone, actionability, and understandability of ChatGPT-generated information compared to BPS standards.
METHODS
This study employed a comparative design to evaluate patient information materials generated by ChatGPT against traditional materials sourced from reputable organisations such as the Faculty of Pain Medicine and BPS, which are available in the public domain for healthcare workers and patients. The comparison focussed on multiple dimensions: readability, emotional tone, accuracy, completeness, actionability, and understandability.
This study adhered to ethical guidelines, ensuring the confidentiality and anonymity of materials and participants. Patient education materials were sourced ethically from reputable organisations. The study did not involve direct human interaction, so institutional review board approval was not sought. The methodology was designed to maintain integrity and impartiality, with any conflicts of interest disclosed. The authors take full responsibility for the study’s content and findings. Appropriate permissions were sought and granted by the FPM to utilise their patient information leaflets in this study. While preparing this work, the authors used an AI chatbot, ChatGPT, to generate the response to the Frequently Asked Questions (FAQs) for further analysis, comparing them to the traditional PILs. After using this tool, the authors reviewed and edited the content as needed.
Patient FAQs concerning pain medications—specifically amitriptyline, duloxetine, NSAIDs, and pregabalin—were collected from the official websites of the FPM of the Royal College of Anaesthetists and the BPS. These FAQs covered diverse aspects of medication use, including indications, mechanisms of action, dosing instructions, side effects, and discontinuation, as endorsed by various organisations.[5]
Eight blinded annexures were prepared for evaluation purposes. Annexures A to D contained traditional PILs obtained from the BPS, each focused on one of the four medications—amitriptyline, duloxetine, NSAIDs, and pregabalin, respectively. Annexures E to H comprised patient information materials generated by ChatGPT for the same medications, structured similar to PILs.
A panel of five experts was assembled to assess the accuracy and completeness of each annexure. The panel comprised one anaesthesiology expert, three pain medicine specialists, and one individual with an educational background. These experts were selected based on their proficiency in evaluating patient education materials. Readability was evaluated using three commonly used metrics—Flesch Reading Ease (FRE), Gunning Fog Index (GFI), and Flesch-Kincaid Grade Level (FKGL)—to measure the ease of comprehension. Sentiment analysis was conducted to gauge the emotional tone of the materials, while accuracy and completeness were rated on a Likert scale ranging from 1 to 5. Additionally, the Patient Education Materials Assessment Tool (PEMAT) was utilised to assess the actionability and understandability of the materials.[6,7,8]
Blinding process and sequential labelling of the annexures: Annexures A, F, H, and C were relabelled 1, 2, 3, and 4, respectively. They were then enclosed in envelopes and handed over to the experts for their independent scoring on accuracy and completeness on the first day. Conversely, the remaining Annexures, E, D, G, and B, were designated as 5, 6, 7, and 8 and handed over on the fourth day. All Annexures were collected back on the seventh day for further analysis.
The data were collected and recorded in Microsoft® Excel® 2021 MSO (Version 2403 Build 16.0.17425.20124), and results were evaluated using the statistical tests calculator online (https://www.socscistatistics.com/tests/) and using Microsoft® Excel®. The data’s normality was checked using the Kolmogorov–Smirnov test of normality. Normally distributed variables (accuracy-completeness scores, readability scores, and the PEMAT scores) were described as mean [standard deviation (SD)] [95% confidence interval (CI)] and compared using the t-test (unpaired for values across groups). A P value of <0.05 was considered significant. Microsoft® Excel® was used to generate graphical representations of various data sets.
RESULTS
Readability Assessment: The readability of annexures A to H was compared, encompassing materials from the BPS and ChatGPT-generated texts. BPS annexures consistently showed higher readability levels, with a mean FRE score of 62.25 compared to 48 for ChatGPT-generated texts (P value <0.001). Similarly, BPS materials had lower GFI scores (mean of 11.85) than ChatGPT-generated texts (mean of 13.65, P = 0.008). FKGL scores reflected these findings, with BPS annexures averaging 8.33 compared to 10.23 for ChatGPT-generated texts (P = 0.004). These results suggest that BPS materials are more readable, potentially facilitating easier comprehension [Table 1 and Figure 1].
Table 1.
Readability Scores
| Readability Scores | Flesch Reading Ease | Gunning Fog Index | Flesch-Kincaid Grade Level | |||
|---|---|---|---|---|---|---|
| Annexures | ||||||
| A (BPS- Amitriptyline) | 61 | 11.1 | 7.87 | |||
| B (BPS- Duloxetine) | 61 | 12.9 | 9.07 | |||
| C (BPS- NSAIDs.) | 65 | 10.8 | 7.83 | |||
| D (BPS- Pregabalin) | 62 | 12.6 | 8.53 | |||
| A to D: Mean (SD) (95% CI) | 62.25 (1.64) (60.6,63.9) | 11.85 (0.91) (11.0,12.7) | 8.33 (0.51) (7.83,8.83) | |||
| E (GPT- Amitriptyline) | 45 | 13.9 | 10.62 | |||
| F (GPT- Duloxetine) | 44 | 14.4 | 10.75 | |||
| G (GPT- NSAIDs.) | 53 | 12.6 | 9.54 | |||
| H (GPT- Pregabalin) | 50 | 13.7 | 10 | |||
| E to H: Mean (SD) (95% CI) | 48 (3.67) (44.4, 51.6) | 13.65 (0.66)(13.0,14.3) | 10.23 (0.49)(9.8, 10.8) | |||
| P | <0.001 | 0.008 | 0.004 |
Data expressed as scores, mean (standard deviation) (95% confidence interval). NSAIDs=non-steroidal anti-inflammatory drugs, BPS=Patient information leaflet by British Pain Society, GPT=patient education material generated by ChatGPT version 3.5. (SD) = Standard deviation, 95% CI=95 percent confidence interval
Figure 1.
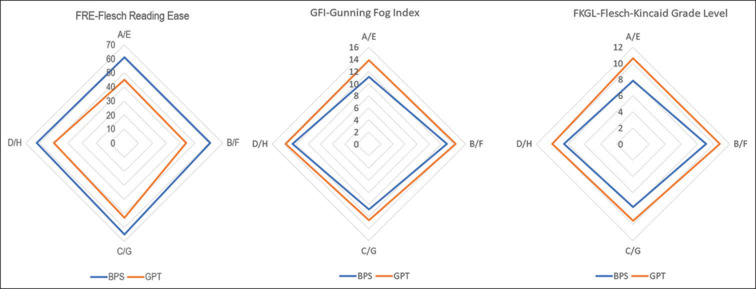
Readability Scores: Flesch Reading Ease (FRE), Gunning Fog Index (GFI), Flesch-Kincaid Grade Level (FKGL). A/E-Annexure A versus Annexure E ‘Amitriptyline’, B/F- Annexure B versus Annexure F ‘Duloxetine’, C/G-Annexure C versus Annexure G ‘NSAIDs’, D/H-Annexure D versus Annexure H ‘Pregabalin’, BPS- British Pain Society, GPT- Response generated by ChatGPT version 3.5
Sentiment analysis: Diverse emotional tones were observed across the materials. Traditional PILs exhibited somewhat negative sentiments (annexures A, B, D: -32.1, -30.3, -31.9), characterised by a serious tone. Conversely, traditional PILs (annexure C: 53.2) and ChatGPT-generated texts (annexures E, G, H: 12.9, 10.1, 12.3) displayed more positive sentiments. Annexure F was neutral (sentiment score: 9.9). These findings suggest varying emotional expressions within the materials, potentially impacting reader engagement [Figure 2].
Figure 2.
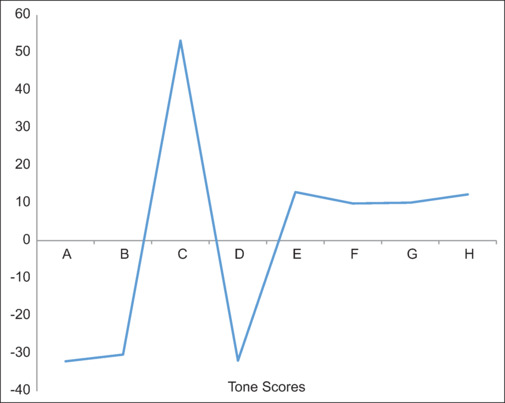
Sentiment Tone Analysis for Each Annexure [A to H]. X-axis: Sentiment analysis scores, Y-axis: Annexures A to H. A and E (Amitriptyline); B and F (Duloxetine); C and G (NSAIDs- non-steroidal anti-inflammatory drugs.); D and H (Pregabalin). Annexures A to E- British Pain Society patient information leaflets, Annexure F to G- Patient education material generated by ChatGPT version 3.5
Patient Education Materials Assessment Tool (PEMAT) Analysis: Materials from BPS generally exhibited comparable scores to ChatGPT-generated texts in understandability and actionability. BPS materials had mean understandability scores of 83.75 compared to 80 for ChatGPT-generated texts (P = 0.222). Actionability scores for BPS materials (81.25) were slightly lower than ChatGPT-generated texts (85), although not statistically significant (P = 0.108). These findings indicate similar levels of understandability and actionability between both sets of materials, suggesting their potential effectiveness in facilitating patient comprehension and engagement [Table 2].
Table 2.
Patient Education Materials Assessment Tool (PEMAT) Scores Analysing Understandability and Actionability of Each Annexure
| Patient Education Materials Assessment Tool (PEMAT) | Understandability | Actionability | ||
|---|---|---|---|---|
| ANNEXURES | [Scores out of 100] | [Scores out of 100] | ||
| A (BPS- Amitriptyline) | 85 | 85 | ||
| B (BPS- Duloxetine) | 80 | 85 | ||
| C (BPS- NSAIDs) | 80 | 75 | ||
| D (BPS- Pregabalin) | 90 | 80 | ||
| A to D: Mean (SD) (95% CI) | 83.75 (4.15) (79.7, 87.8) | 81.25 (4.15)(77.2,85.3) | ||
| E (GPT- Amitriptyline) | 80 | 85 | ||
| F (GPT- Duloxetine) | 80 | 90 | ||
| G (GPT- NSAIDs) | 85 | 85 | ||
| H (GPT- Pregabalin) | 75 | 80 | ||
| E to H: Mean (SD) (95% CI) | 80 (3.54) (76.5,83.5) | 85 (3.54) (81.5, 88.5) | ||
| P | 0.222 | 0.108 |
Data expressed as scores, mean (standard deviation) (95% confidence interval). NSAIDs=non-steroidal anti-inflammatory drugs, P<0.05 Significant, BPS=Patient information leaflet by British Pain Society, GPT=patient education material generated by ChatGPT version 3.5. (SD)=Standard deviation, 95% CI=95 percent confidence interval
Accuracy and Completeness Evaluation: Both BPS materials and ChatGPT-generated texts received high ratings for accuracy and completeness from the expert panel. Across all annexures, mean accuracy and completeness scores were comparable. BPS materials demonstrated mean accuracy scores [expressed as mean (SD) (95% CI)] 4.45 (0.26) (95% CI: 4.2, 4.71) and completeness scores 4.6 (0.14) (95% CI: 4.6, 4.74). Similarly, ChatGPT-generated texts showed comparable mean accuracy and completeness 4.4 (0.2) (95% CI: 4.2, 4.6) and 4.55 (0.17) (95% CI: 4.38, 4.72). While slight differences were noted, they were not statistically significant (P value 0.39 for accuracy and 0.36 for completeness). These findings suggest that the experts perceived both sets of materials as accurate and comprehensive, indicating their potential utility in patient education [Figures 3 and 4].
Figure 3.
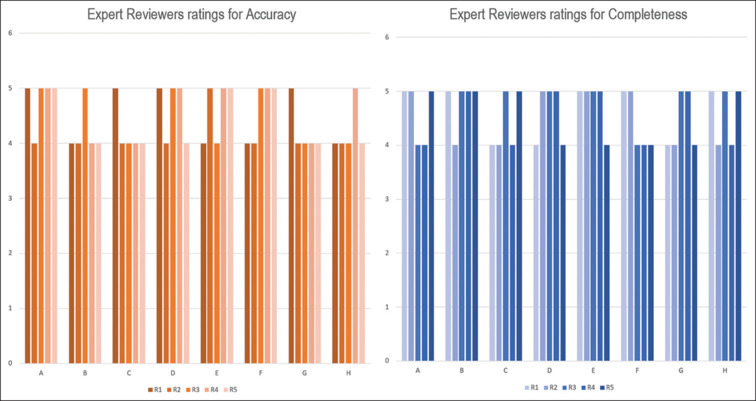
Expert ratings [Likert scale range1-5] for each Annexure for Accuracy and Completeness. Accuracy and Completeness scoring by each Expert/reviewer ‘R’ (1 to 5). Annexure A and Annexure E ‘Amitriptyline’, Annexure B and Annexure F ‘Duloxetine’, Annexure C and Annexure G’ Non-steroidal Anti-inflammatory drugs, Annexure D and Annexure H ‘Pregabalin’. Scoring range- 5 pointer Likert scale
Figure 4.
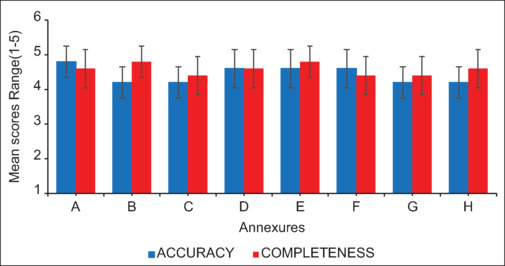
Expert ratings Mean (SD) Scoring for each Annexure for Accuracy and Completeness. Annexures A to E- British Pain Society patient information leaflets, Annexures F to G- Patient education material generated by ChatGPT version 3.5. A and E (Amitriptyline); B and F (Duloxetine); C and G (NSAIDs- non-steroidal anti-inflammatory drugs.); D and H (Pregabalin)
DISCUSSION
The study results consistently showed that BPS materials were easier to understand than ChatGPT-generated texts. This indicates that traditional PILs may be more accessible to a wider audience based on established readability metrics. The significant differences in readability metrics highlight the importance of considering readability in designing patient education materials for optimal comprehension and engagement.
Chronic pain medications, encompassing opioids, NSAIDs, antidepressants, anticonvulsants, and muscle relaxants, are essential for managing persistent pain conditions. Individual responses to these medications vary, making it challenging to balance pain relief with adverse effects.[9] Proper patient education is crucial to help patients understand treatment options, make informed decisions, adhere to prescribed regimens, and communicate effectively with healthcare providers, thus promoting safe medication use and enhancing overall quality of life.[10,11] Chatbots, like those powered by large language models such as ChatGPT, may inadvertently provide false or misleading information due to the complexity of natural language processing, evolving training data, and potential biases. To mitigate these risks, ongoing monitoring, robust validation mechanisms, and human oversight are necessary to ensure the delivery of accurate responses while acknowledging the potential of chatbots to offer accessible and timely information.[12] Thia and Saluja[13] found ChatGPT comparable to traditional materials in readability but suggested using specific prompts to improve ease of use for certain audiences.[13]
While traditional PILs tend towards negative sentiments and ChatGPT-generated texts convey more positive tones, caution is warranted in interpreting emotional tone’s impact on patient engagement and understanding. Further research is necessary to elucidate these effects on patient outcomes.
The PEMAT scores indicated comparable levels of understandability and actionability between BPS materials and ChatGPT-generated texts. Both sets of materials received high ratings, suggesting that they are perceived as effective in facilitating patient comprehension and guiding actions based on the information provided. These findings are encouraging as they indicate that AI-generated patient education materials can be as effective as traditional PILs in conveying information to patients in a clear and actionable manner. Ayoub et al.[14] found that ChatGPT scored significantly higher than a Google search for patient education questions.
While expert ratings show no significant differences in accuracy and completeness between BPS materials and ChatGPT-generated texts, we suggest additional validation through empirical studies or patient feedback is warranted.
While insightful, this study has limitations. This study’s narrow focus on pain medications might miss other crucial patient education materials for chronic pain management. Standardised metrics may not fully capture patient understanding or emotions. Expert ratings are subjective and may be influenced by biases. Future research could use qualitative methods for better insights. However, cultural and healthcare differences may limit the findings’ applicability beyond the specific context. When extrapolating the results to other populations or medical domains, caution should be exercised.
CONCLUSION
While AI chatbots offer efficient information delivery, ensuring accuracy, readability, and patient-centeredness remains crucial. While they show promise as supplements, they may not fully substitute traditional methods of information dissemination. Balancing innovation with evidence-based practice is vital for delivering high-quality healthcare information.
Study data availability
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared after approval as per the authors’ Institution policy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
PATIENT INFORMATION
Adult patient prescribed drugs for the treatment of pain.
Pregabalin
Why have I been prescribed pregabalin?
How does pregabalin work?
When should I take it?
How is pregabalin taken?
How long will it take to work?
What are the possible side effects?
Can I take this medication long-term?
Can I drink alcohol?
Can I drive?
What should I tell the doctor?
What if I forget or miss a dose?
What if I want to stop taking pregabalin?
Nonsteroidal anti-inflammatory drugs (NSAIDS)
What are anti inflammatory medicines?
Why have I been prescribed a NSAID?
How does NSAID work?
When should I take it?
How is NSAID taken?
How long will it take to work?
What are the possible side effects?
Can I take this medication long-term?
Can I drink alcohol?
Can I drive?
What should I tell the doctor?
What if I forget or miss a dose?
What if I want to stop taking pregabalin?
Amitriptyline
Why have I been prescribed Amitriptyline?
How does Amitriptyline work?
When should I take it?
How is Amitriptyline taken?
How long will it take to work?
What are the possible side effects?
Can I take this medication long-term?
Can I drink alcohol?
Can I drive?
What should I tell the doctor?
What if I forget or miss a dose?
What if I want to stop taking Amitriptyline?
Duloxetine
Why have I been prescribed Duloxetine?
How does Duloxetine work?
When should I take it?
How is Duloxetine taken?
How long will it take to work?
What are the possible side effects?
Can I take this medication long-term?
Can I drink alcohol?
Can I drive?
What should I tell the doctor?
What if I forget or miss a dose?
What if I want to stop taking pregabalin?
| Annexure | BPS | Annexure | ChatGPT | |||
|---|---|---|---|---|---|---|
| A | BPS- Amitryptiline | E | GPT- Amitryptiline | |||
| B | BPS- Duloxetine | F | GPT- Duloxetine | |||
| C | BPS- NSAIDS | G | GPT- NSAIDS | |||
| D | BPS- Pregabalin | H | GPT- Pregabalin |
FOR THE EXPERTS/ REVIEWERS.
RATE EACH ANNEXURE [LIKERT SCALE 1-5] BOTH FOR ACCURACY AND COMPLETENESS.
ANNEXURE A
Information for adult patients prescribed for the Treatment of Pain
-
Why have I been prescribed amitriptyline?
Amitriptyline is used to treat many types of persistent pain. Amitriptyline is commonly prescribed for nerve pain, such as burning, shooting or stabbing pain, and for pain that keeps you awake at night. Amitriptyline belongs to the group of medicines called tricyclic antidepressants that are also used to treat depression. The dose of amitriptyline needed for pain relief is usually much lower than that prescribed for depression. Amitriptyline has been used to treat pain for many years.
-
How does amitriptyline work?
Amitriptyline works by changing the amount of specific nerve transmitters in the nervous system, reducing pain messages arriving in the brain.
-
When should I take it?
It is best to take amitriptyline in the evening. Start by taking it 1-3 hours before going to bed, if you find that you feel drowsy the next morning, try taking it earlier in the evening.
-
How is amitriptyline taken?
The tablets should be swallowed whole, with a glass of water. Amitriptyline may be taken on an empty or full stomach. You will be told how much to start taking and when to increase the dose. The table at the end of the leaflet will help you remember when to increase the dose. Do not take more than prescribed.
-
How long will it take to work?
Every patient is different. You may notice some initial benefit within 2 weeks. Your doctor may advise you to gradually increase the dose to get the maximum effect.
Amitriptyline does not work for everyone. If you do not feel any improvement in your pain, do not suddenly stop taking the tablets but speak to your doctor who may advise you to reduce it gradually.
-
What are the possible side effects?
Most side effects are mild and it is expected that they reduce after a few doses.
Common side effects include; drowsiness, dizziness, dry mouth, constipation and sweating. If you have these side effects and they are of concern contact your doctor or pharmacist for advice.
Less common side effects include fainting, trembling, irregular heartbeat, blurred vision or problems passing water. If any of these side effects occur contact your doctor or pharmacist for advice.
If amitriptyline is taken along with antidepressants (e.g. citalopram, fluoxetine, sertraline, etc) some patients may develop “serotonin syndrome” (sweating, shivering, tremors, agitation, restlessness, confusion, muscle spasms, raise in body temperature, increased heart rate, diarrhoea, etc). If you get any such symptoms contact your doctor immediately for advice.
-
Can I take this medication long-term?
Yes, if it helps. You may wish to reduce treatment every so often, to check if your pain is still a problem. This should be done with the advice of your prescriber gradually reducing your medication over a period of time.
-
Can I drink alcohol
Effects of alcohol are enhanced (e.g. sedative effects) when taking amitriptyline. It is best not to drink alcohol when you start taking it. Be aware that alcohol taken in combination with some medications can substantially increase the risk of accidents. Please also look at the section “Can I drive?”.
-
Can I drive?
Amitriptyline may affect your ability to drive (e.g. drowsiness). The risk is increased if you take it along with other medications that have drowsiness as a side effect.
If you feel any impairment, do not drive.
-
What to discuss with your prescriber?
If you are allergic to any drug
If you are taking any other medicines or herbal medicines
If you are pregnant or breastfeeding, or if you are planning to become pregnant in the future
If you have had a heart attack recently or have any heart problems
If you have a history of epilepsy or fits
If you have glaucoma
If you have difficulty in passing water
If you have thyroid disease
If you have or have had a mental health problem
If you are taking an antidepressant medicine, especially one called a monoamine oxidase inhibitor (MAOI)
If you have or have had a history of excessive alcohol use, recreational drug use or addiction to prescribed or over-the-counter medication
If you are regularly taking strong opioid medicines (e.g. tramadol, tapentadol, morphine, oxycodone, fentanyl).
-
What if I forgot or miss a dose?
If you forget a dose then you can consider taking it when you remember that night but this may result in sleepiness the following day and affect your concentration, work or driving ability. The alternative is to wait until the next dose is scheduled.
If you only take one dose at bedtime and you miss the dose, do not take the medicine in the morning. Wait until the next night and skip the missed dose.
Do not take two doses together.
-
What if I want to stop taking amitriptyline?
If you stop taking amitriptyline suddenly, you might experience withdrawal symptoms. Speak to your prescriber who will be able to supervise a gradual reduction.
ANNEXURE B:
Why have I been prescribed duloxetine?
Duloxetine is used to treat some types of persistent pain.
Duloxetine is commonly prescribed for nerve pain, such as burning, shooting or stabbing pain.
Duloxetine belongs to the group of medicines called Serotonin Norepinephrine Reuptake Inhibitors (SNRI) that are also used to treat depression.
You may notice that information from the manufacturer may not mention your type of pain.
How does duloxetine work?
Duloxetine works by changing the amount of specific nerve transmitters in the nervous system, reducing pain messages arriving in the brain.
When should I take it?
It is best to take duloxetine at the same time each day. Most people take it in the morning. If you find that you feel drowsy after taking it in the morning, try taking it in the evening. Some patients may be advised to take duloxetine twice a day. Information for adult patients prescribed duloxetine for the treatment of pain endorsed by fpm.ac.uk/patients.
How is duloxetine taken?
The capsules should be swallowed whole, with a glass of water.
Duloxetine may be taken on an empty or full stomach.
You will be told how much to start taking and when to increase the dose. The table at the end of the leaflet will help you remember when to increase the dose.
Do not take more than prescribed.
How long will it take to work?
Every patient is different. You may notice some initial benefit within 1 week. Your doctor may advise you to increase the dose gradually to get the maximum effect.
Duloxetine does not work for everyone. If you do not feel any improvement in your pain, do not suddenly stop taking the tablets but speak to your doctor who may advise you to reduce it gradually.
What are the possible side effects?
Most side effects are mild and can be expected to reduce after a few doses.
Common side effects include; headache, drowsiness, sickness (nausea), dizziness, blurred vision and dry mouth. If you have these side effects and they are of concern, contact your doctor or pharmacist for advice.
Less common side effects include loss of appetite, flushes, raised blood pressure, difficulty sleeping, feeling anxious, shaky and increased sweating. If any of these side effects occur contact your doctor or pharmacist for advice.
If duloxetine is used along with antidepressants (e.g. citalopram, fluoxetine, sertraline, etc) this can in some patients lead to “serotonin syndrome” (sweating, shivering, tremors, agitation, restlessness, confusion, muscle spasms, raise in body temperature, increased heart rate, diarrhoea, etc). If you get any such symptoms contact your doctor immediately for advice.
Can I take this medication long-term?
Yes, if it helps. You may wish to reduce treatment every so often, to check if your pain is still a problem. This should be done with the advice of your prescriber, gradually reducing your medication over a period of time.
Can I drink alcohol
Effects of alcohol are enhanced (e.g. sedative effects) when taken while on duloxetine. It is best not to drink alcohol when you start taking it.
Can I drive?
Duloxetine may affect your ability to drive (e.g. drowsiness). The risk is increased if you take it along with other medications that have drowsiness as a side effect. If you feel any impairment, do not drive.
You may need to tell the DVLA about your medical condition. Check https://www.gov.uk/driving-medical-conditions You can find more information in our Driving and Pain leaflet: https://fpm.ac.uk/media/846
What to discuss with your prescriber?
If you are allergic to any drugs
If you are taking any other medicines or herbal medicines
If you have epilepsy or a glaucoma
If you are taking any medicine that causes sleepiness (e.g. strong painkillers such as morphine) or increases the level of serotonin (e.g. tramadol, medicines taken for depression)
If you are pregnant or breastfeeding, or if you are planning to become pregnant in the future
If you take any anticoagulants, antiplatelet agents or other drugs to thin the blood.
If you have or have had a mental health problem
If you have kidney or liver problems
If you are taking any antidepressant
If you are taking ciprofloxacin, an antibiotic used to treat infections
If you have or have had a history of excessive alcohol use, recreational drug use or addiction to prescribed or over-the-counter medication
If you are regularly taking strong opioid medications (e.g. tramadol, tapentadol, morphine, oxycodone, fentanyl). What if I forgot or miss a dose?
If you take duloxetine at night only and forget a dose then you can consider taking it when you remember that night but this may result in sleepiness the following day and affect your concentration, work or driving ability. The alternative is to wait until the next dose is scheduled.
If you only take one dose in the morning and you miss the dose, do not take the medicine in the evening. Wait until the next morning and skip the missed dose.
If you are taking duloxetine twice a day take the missed dose as soon as you remember, unless it is less than 4 hours until your next dose, in which case skip the missed dose
Do not take two doses together.
What if I want to stop taking duloxetine?
If you stop taking duloxetine suddenly, you might experience withdrawal symptoms. Speak to your prescriber who will be able to supervise a gradual reduction.
ANNEXURE C
What are anti-inflammatory medicines?
These can be called Non-steroidal anti-inflammatory drugs (NSAIDS). They include ibuprofen, naproxen, diclofenac, meloxicam, indomethacin, piroxicam, etoricoxib.
The NSAID your prescriber has chosen for you will have a leaflet with detailed information about the specific medicine and its side effects.
You can also ask your pharmacist or prescriber if you have any questions.
Why have I been prescribed a NSAID?
NSAIDs are used to treat pain from an injury or surgery.
NSAIDs can also be used in long term painful conditions, such as osteoarthritis, back pain, rheumatoid arthritis.
Taking NSAIDs may mean that you can reduce stronger pain medicines, which leads to fewer side effects. This leaflet has been developed in conjunction with the British Pain Society, Pain UK and the Royal College of Nursing, and has been endorsed by The Royal Pharmaceutical Society.
How do NSAIDs work?
When you feel pain and stiffness, your body is making chemicals (prostaglandins) which ‘tell’ you it hurts.
NSAIDs reduce the amount of these prostaglandins and therefore reduces your pain but they may not alter the progress of the disease.
When should I take it?
NSAIDs can be taken regularly or as needed if the pain is not constant.
NSAIDs should ideally be taken with or shortly after food. How are NSAIDs taken?
NSAIDs come in many different forms including tablets, capsules, or a liquid.
Some come as a gel or cream to rub into the painful area.
Some people prefer to take it by suppository.
Do not take more than prescribed.
Do not take more than one NSAID at a time as their effects can add up causing more side effects.
How long will it take to work?
Everyone is different. The average time for pain to reduce is an hour after taking a tablet or suppository, however it may take longer for the full effect.
NSAIDs as a gel or cream can vary in the time it takes to give pain relief.
NSAIDs do not work for everyone. If there is no improvement in your pain you should consult your prescriber.
What are the possible side effects? Most side effects are mild.
Common side effects include heartburn, indigestion or pains in your stomach, and feeling sick (nausea) or being sick (vomiting). If these side effects are frequent and severe, you should stop taking the medicine and consult your prescriber or pharmacist.
If you vomit any blood or dark particles that look like coffee grounds or have blood stained faeces (stools/motions): You should stop taking the medicine immediately and seek medical advice.
Less common side effects include headache, dizziness, swollen feet or legs, and weight gain. Again if these side effects are constant and severe discuss with your prescriber or pharmacist. Other less common side effects include a rash or itching, or unexplained wheezing or shortness of breath. If you have any of these side effects you should discuss them with your prescriber or pharmacist.
Recent evidence suggests that even short term NSAID use may be linked to a very small increased risk of having a stroke or heart attack. However your risk of having a stroke or a heart attack whilst taking NSAIDs is thought to remain very low. The risk of this increases with dose and duration of treatment and the risk is greater for those who already have heart disease.
Before taking a NSAID, your prescriber should discuss the risk of heart attack or stroke with you.
If you experience chest pain, shortness of breath, or sudden weakness or difficulty speaking while taking a NSAID, seek medical help immediately.
Use of NSAIDs, even for a short period of time, can harm the kidneys. This is especially true in people with underlying kidney disease.
Side effects are usually related to the dose of medicine you take, but some people are more sensitive than others. They are less likely if you can take the smallest dose that you find reduces your pain.
Can I take this medicine long-term?
NSAIDs can be taken for long term conditions. You should first discuss it with your prescriber to make sure it is safe. The benefit of long term NSAID use should be regularly reviewed with your prescriber.
Can I drink alcohol? Once you are settled on a stable dose, you may drink alcohol in moderation.
Can I drive? Yes, it is usually safe to drive whilst taking a NSAID.
Although not common, NSAIDs may make you dizzy or drowsy. If you experience any of these symptoms do not drive, operate machinery or do anything, including driving that requires you to be alert. NSAID use is associated with a very small increased risk of motor vehicle accidents. It is not clear if this increased risk is a result of medicine related side effects, or the underlying pain condition, however NSAID information leaflets produced by manufacturers warn of caution when driving or using heavy machinery.
What should I tell my prescriber?
If you are allergic to any medicines.
If you are taking any other prescribed medicines, bought from the pharmacy or herbal medicines.
If you are pregnant or breastfeeding, or if you are planning to become pregnant in the future.
If you have: - a stomach ulcer or have had one in the past - a kidney problem - asthma or any other breathing disorder - any problem with bleeding or blood clots - a liver problem - Crohn’s Disease or ulcerative colitis - high-blood pressure - had a heart attack, suffer with angina or have recurrent chest pains - shortness of breath, fatigue, swelling in legs, ankles or feet, or other symptoms of heart failure - had a stroke - dementia or Parkinson’s disease
What if I forget or miss a dose?
Take it as soon as you remember, unless it is almost time for your next dose. If it is, skip the missed dose and take your next dose as normal. Do not take two doses together. Ensure that you do not take more than the maximum prescribed daily dose. What if I want to stop taking NSAIDs? Over time your pain may change. It is important to regularly review whether you still need to use your NSAID medicine. If your pain improves, you should consider stopping your medicine or reducing the dose as any medicine can have unwanted side effects. Although you can safely stop taking your NSAID whenever you want to. It is best to discuss it with your prescriber if you have been taking them for a long time.
ANNEXURE D
Why have I been prescribed pregabalin?
Pregabalin is used to treat some types of persistent pain. Pregabalin is commonly prescribed for nerve pain, such as burning, shooting or stabbing pain. Pregabalin belongs to a group of medicines called anticonvulsants which are also used to treat epilepsy. You may notice that information from the manufacturer may not mention your type of pain.
How does pregabalin work? Pregabalin works by changing the way that nerves send messages to your brain. If the messages are reduced, then the pain will be reduced.
When should I take it? Normally, the starting dose is small and may be taken one to two times a day, but the dose will be gradually increased. You will be told how much to start taking and how to increase or decrease the dose based on pain relief and side effects. The table at the end of the leaflet will help you remember when to increase the dose. If you are taking antacid medication, it is best to wait for two hours after taking it before taking pregabalin.
How is Pregabalin taken? The capsules should be swallowed whole, with a glass of water. Pregabalin may be taken on an empty or full stomach. Do not take more than prescribed.
How long will it take to work? Every patient is different. You may notice some initial benefit within a few days, however it may take a little longer for a full effect. Your prescriber may need to increase the dose for Pregabalin to be effective. Do not increase the dose without consulting with your prescriber Pregabalin does not work for everyone. If you do not feel any improvement in your pain after 4-6 weeks, do not suddenly stop taking the tablets but speak to your prescriber or pharmacist to discuss reducing and stopping the medication.
What are the possible side effects? Most side effects are mild and it is expected that they will reduce after several days. Generally side effects are more troublesome just after starting pregabalin or increasing the dose. It is important to persist in taking pregabalin as these side effects usually wear off. Common side effects include; drowsiness, dizziness, fatigue, weight gain and muscle tremor. If you have these side effects and they are of concern contact your presciber or pharmacist for advice. Less common side effects include vision disturbances, indigestion, leg swelling, memory loss, euphoria, mood changes, hallucinations or rash. If any of these side effects occur, contact your prescriber or pharmacist for advice. Some people develop severe anxiety if they miss a dose and some take more than prescribed to help their symptoms. If you are worried this is happening to you, discuss it with your prescriber.
Can I take this medication long-term? Yes, if it helps. You may wish to reduce treatment every so often, to check if your pain is still a problem. This should be done with the advice of your GP or pain specialist, gradually reducing your medication over a period of time. Do not stop taking pregabalin suddenly, you might experience withdrawal symptoms. Speak to your prescriber who will be able to supervise a gradual reduction.
Can I drink alcohol? Alcohol increases the sedative effects of pregabalin, it is best not to drink alcohol when taking it.
Can I drive? Pregabalin may affect your ability to drive (e.g. drowsiness). The risk is increased if you take it along with other medications that have drowsiness as a side effect. If you feel any impairment, do not drive You may need to tell the DVLA about your medical condition. Check https://www.gov.uk/driving-medical-conditions You can find out more information in our Driving and Pain leaflet: https://fpm.ac.uk/media/846
What should I tell the doctor/prescriber? If you are allergic to any drugs If you are taking any other medicines or herbal medicines If you are pregnant or breast feeding, or if you are planning to become pregnant in the future If you have a kidney problem If you have or have had a history of excessive alcohol use, recreational drug use or addiction to prescribed or over-the-counter medication. If you are regularly taking strong opioid medications (e.g. tramadol, tapentadol, morphine, oxycodone, fentanyl) What if I forget or miss a dose? If you forget a dose, consider taking it when you remember. However, this may result in some increased sleepiness and may affect your concentration, work or driving ability. Alternatively, you could wait until the next dose is scheduled and take your medication as normal. Do not take two doses together.
What if I want to stop taking pregabalin? Do not stop taking pregabalin suddenly, you might experience withdrawal symptoms. Speak to your prescribing healthcare professional who will be able to supervise a gradual reduction
ANNEXURE G
Patient Information Leaflet: NSAIDs (Nonsteroidal Anti-Inflammatory Drugs)
1. Why have I been prescribed NSAIDs?
NSAIDs are prescribed to help manage pain, inflammation, and fever associated with various conditions, such as arthritis, musculoskeletal injuries, menstrual cramps, and headaches.
2. How do NSAIDs work?
NSAIDs work by inhibiting the production of prostaglandins, which are substances in the body that contribute to inflammation, pain, and fever. By reducing prostaglandin levels, NSAIDs help alleviate pain and inflammation.
3. When should I take them?
NSAIDs are usually taken as needed to relieve pain or inflammation. However, your doctor may recommend a specific dosing schedule based on your condition and individual needs. Follow your doctor’s instructions carefully.
4. How are NSAIDs taken?
NSAIDs are typically taken orally in the form of tablets, capsules, or liquids. Some NSAIDs are also available as topical formulations, such as creams or gels, which can be applied directly to the affected area. Take NSAIDs with a full glass of water and with food or milk to help reduce the risk of stomach upset.
5. How long will it take to work?
The effectiveness of NSAIDs may vary depending on the type and severity of pain or inflammation. Some individuals may experience relief within a short time after taking NSAIDs, while others may require more time. It is essential to use NSAIDs as directed and to consult your doctor if you do not experience adequate pain relief.
6. What are the possible side effects?
Common side effects of NSAIDs may include stomach upset, heartburn, nausea, diarrhea, headache, dizziness, and fluid retention. More serious side effects may include gastrointestinal ulcers or bleeding, kidney problems, high blood pressure, and allergic reactions. Contact your doctor immediately if you experience any severe or concerning side effects.
7. Can I take NSAIDs long-term?
NSAIDs can be taken on a short-term or long-term basis, depending on the underlying condition being treated and your doctor’s recommendations. However, long-term use of NSAIDs may increase the risk of certain side effects, such as gastrointestinal bleeding or kidney damage. Your doctor will monitor your response to NSAIDs and adjust your treatment as needed.
8. Can I drink alcohol?
It is advisable to avoid or limit alcohol consumption while taking NSAIDs, as it may increase the risk of gastrointestinal side effects, such as stomach irritation or bleeding. Alcohol can also interact with certain NSAIDs and affect their effectiveness.
9. Can I drive?
NSAIDs may cause dizziness, drowsiness, or blurred vision in some individuals. If you experience these side effects, avoid driving or operating machinery until you know how NSAIDs affect you. Use caution when performing tasks that require alertness or coordination.
10. What should I tell the doctor?
Inform your doctor about any medical conditions you have, including a history of stomach ulcers, kidney or liver disease, high blood pressure, or heart problems. Also, tell your doctor about all medications, supplements, or herbal remedies you are currently taking, as they may interact with NSAIDs.
11. What if I forget or miss a dose?
If you miss a dose of NSAIDs, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not double the dose to make up for a missed one.
12. What if I want to stop taking NSAIDs?
If you no longer need NSAIDs or wish to stop taking them, consult your doctor before discontinuing the medication. Your doctor may recommend tapering off NSAIDs gradually to minimize the risk of rebound symptoms or withdrawal effects.
Please remember that this leaflet provides general information about NSAIDs and is not intended to replace advice from your healthcare provider. If you have any questions or concerns about your medication, consult your doctor or pharmacist for further guidance.
ANNEXURE F
Patient Information Leaflet: Duloxetine
1. Why have I been prescribed duloxetine?
Duloxetine is prescribed to help manage various conditions, including depression, generalized anxiety disorder, diabetic neuropathy (nerve pain caused by diabetes), fibromyalgia (chronic widespread pain and tenderness), and certain types of chronic musculoskeletal pain.
2. How does duloxetine work?
Duloxetine belongs to a class of medications called serotonin-norepinephrine reuptake inhibitors (SNRIs). It works by increasing the levels of serotonin and norepinephrine, neurotransmitters in the brain that help regulate mood and pain perception.
3. When should I take it?
Duloxetine is usually taken once daily, with or without food. It is important to take it at the same time each day to maintain steady levels of the medication in your body. If you are prescribed duloxetine for depression or anxiety, it is typically taken in the morning. If you are prescribed duloxetine for pain, it may be taken in the morning or evening, depending on your doctor’s instructions.
4. How is duloxetine taken?
Duloxetine is typically taken orally in the form of capsules. Swallow the capsules whole with a glass of water. Do not crush, chew, or break the capsules unless directed by your healthcare provider.
5. How long will it take to work?
The effectiveness of duloxetine may vary from person to person and depending on the condition being treated. Some individuals may experience improvement in mood or reduction in pain within a few weeks of starting the medication, while others may require more time. It is important to continue taking duloxetine as prescribed, even if you do not notice immediate effects.
6. What are the possible side effects?
Common side effects of duloxetine may include nausea, dry mouth, constipation, dizziness, drowsiness, fatigue, sweating, and decreased appetite. More serious side effects may include suicidal thoughts or behavior, changes in mood or behavior, increased heart rate, and liver problems. Contact your doctor immediately if you experience any severe or concerning side effects.
7. Can I take this medication long-term?
Duloxetine can be taken long-term as prescribed by your healthcare provider. It is important to follow your doctor’s instructions carefully and attend regular follow-up appointments to monitor your response to the medication and any potential side effects.
8. Can I drink alcohol?
It is advisable to avoid or limit alcohol consumption while taking duloxetine, as it may increase the risk of drowsiness, dizziness, and liver problems. Alcohol can also worsen certain side effects of duloxetine and may interact with the medication.
9. Can I drive?
Duloxetine may cause dizziness, drowsiness, or blurred vision in some individuals. If you experience these side effects, avoid driving or operating machinery until you know how duloxetine affects you. Use caution when performing tasks that require alertness or coordination.
10. What should I tell the doctor?
Inform your doctor about any medical conditions you have, including liver or kidney disease, glaucoma, seizures, or a history of substance abuse. Also, tell your doctor about all medications, supplements, or herbal remedies you are currently taking, as they may interact with duloxetine.
11. What if I forget or miss a dose?
If you miss a dose of duloxetine, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not double the dose to make up for a missed one.
12. What if I want to stop taking duloxetine?
Do not stop taking duloxetine suddenly without consulting your doctor, as this may cause withdrawal symptoms or rebound effects. Your doctor will provide guidance on gradually tapering off the medication if necessary.
Please remember that this leaflet provides general information about duloxetine and is not intended to replace advice from your healthcare provider. If you have any questions or concerns about your medication, consult your doctor or pharmacist for further guidance.
ANNEXURE H
Patient Information Leaflet: Pregabalin
1. Why have I been prescribed pregabalin?
Pregabalin is prescribed to help manage certain types of pain, including neuropathic pain, which is caused by damage or dysfunction of nerves. It can also be used to treat seizures in epilepsy and generalized anxiety disorder.
2. How does pregabalin work?
Pregabalin works by reducing the abnormal electrical activity in the brain that can cause seizures and by modifying the activity of certain neurotransmitters involved in pain signaling, which helps to reduce pain sensations.
3. When should I take it?
Pregabalin is usually taken two to three times daily, with or without food. It is important to take it at the same times each day to maintain steady levels of the medication in your body.
4. How is pregabalin taken?
Pregabalin is typically taken orally in the form of capsules or tablets. Swallow the medication whole with a glass of water. Do not crush, chew, or break the capsules or tablets unless directed by your healthcare provider.
5. How long will it take to work?
The effectiveness of pregabalin may vary from person to person. Some individuals may experience relief from pain or other symptoms within a few days to weeks of starting the medication, while others may require more time.
6. What are the possible side effects?
Common side effects of pregabalin may include dizziness, drowsiness, fatigue, blurred vision, dry mouth, weight gain, and swelling of the extremities. Rare but serious side effects may include allergic reactions, suicidal thoughts or behavior, and changes in mood or behavior. Contact your doctor immediately if you experience any severe or concerning side effects.
7. Can I take this medication long-term?
Pregabalin can be taken long-term as prescribed by your healthcare provider. It is important to follow your doctor’s instructions carefully and attend regular follow-up appointments to monitor your response to the medication and any potential side effects.
8. Can I drink alcohol?
It is advisable to avoid or limit alcohol consumption while taking pregabalin, as it may increase the risk of drowsiness, dizziness, and other central nervous system side effects.
9. Can I drive?
Pregabalin may cause dizziness, drowsiness, or blurred vision, which can impair your ability to drive or operate machinery. Avoid driving or engaging in activities that require alertness until you know how pregabalin affects you.
10. What should I tell the doctor?
Inform your doctor about any medical conditions you have, including allergies, kidney problems, or a history of substance abuse. Also, tell your doctor about all medications, supplements, or herbal remedies you are currently taking, as they may interact with pregabalin.
11. What if I forget or miss a dose?
If you miss a dose of pregabalin, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not double the dose to make up for a missed one.
12. What if I want to stop taking pregabalin?
-
Do not stop taking pregabalin suddenly without consulting your doctor, as this may cause withdrawal symptoms or rebound effects. Your doctor will provide guidance on gradually tapering off the medication if necessary.
Please remember that this leaflet provides general information about pregabalin and is not intended to replace advice from your healthcare provider. If you have any questions or concerns about your medication, consult your doctor or pharmacist for further guidance.
ANNEXURE E
Patient Information Leaflet: Amitriptyline
1. Why have I been prescribed amitriptyline?
Amitriptyline is prescribed to help manage various conditions, including depression, certain types of chronic pain, such as neuropathic pain and fibromyalgia, and certain types of headaches, such as migraines.
2. How does amitriptyline work?
Amitriptyline belongs to a class of medications called tricyclic antidepressants (TCAs). It works by increasing the levels of certain neurotransmitters in the brain, such as serotonin and norepinephrine, which help regulate mood and pain perception.
3. When should I take it?
Amitriptyline is usually taken once daily, preferably at bedtime, as it can cause drowsiness. However, your doctor may adjust the dosing schedule based on your individual needs and response to the medication.
4. How is amitriptyline taken?
Amitriptyline is typically taken orally in the form of tablets or capsules. Swallow the medication whole with a glass of water. Do not crush, chew, or break the tablets or capsules unless directed by your healthcare provider.
5. How long will it take to work?
The effectiveness of amitriptyline may vary from person to person. Some individuals may experience improvement in mood or reduction in pain within a few weeks of starting the medication, while others may require more time.
6. What are the possible side effects?
Common side effects of amitriptyline may include drowsiness, dizziness, dry mouth, blurred vision, constipation, weight gain, and difficulty urinating. Rare but serious side effects may include changes in heart rhythm, seizures, and suicidal thoughts or behavior. Contact your doctor immediately if you experience any severe or concerning side effects.
7. Can I take this medication long-term?
Amitriptyline can be taken long-term as prescribed by your healthcare provider. It is important to follow your doctor’s instructions carefully and attend regular follow-up appointments to monitor your response to the medication and any potential side effects.
8. Can I drink alcohol?
It is advisable to avoid or limit alcohol consumption while taking amitriptyline, as it may increase the risk of drowsiness, dizziness, and other central nervous system side effects.
9. Can I drive?
Amitriptyline may cause drowsiness, dizziness, or blurred vision, which can impair your ability to drive or operate machinery. Avoid driving or engaging in activities that require alertness until you know how amitriptyline affects you.
10. What should I tell the doctor?
Inform your doctor about any medical conditions you have, including heart problems, liver or kidney disease, or a history of seizures. Also, tell your doctor about all medications, supplements, or herbal remedies you are currently taking, as they may interact with amitriptyline.
11. What if I forget or miss a dose?
If you miss a dose of amitriptyline, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not double the dose to make up for a missed one.
12. What if I want to stop taking amitriptyline?
-
Do not stop taking amitriptyline suddenly without consulting your doctor, as this may cause withdrawal symptoms or rebound effects. Your doctor will provide guidance on gradually tapering off the medication if necessary.
Please remember that this leaflet provides general information about amitriptyline and is not intended to replace advice from your healthcare provider. If you have any questions or concerns about your medication, consult your doctor or pharmacist for further guidance.
REFERENCES
- 1.Hadi MU, Qureshi R, Shah A, Irfan M, Zafar A, Shaikh MB, et al. Large language models: A comprehensive survey of its applications, challenges, limitations, and future prospects. TechRxiv. 2023 doi: 10.36227/techrxiv.23589741.v4. [Google Scholar]
- 2.Bacher H, Schweyen R, Vordermark D, Leplow B, Hey J. Development and validation of an information leaflet on oral care for irradiated patients. Patient Prefer Adherence. 2020;14:1791–9. doi: 10.2147/PPA.S256990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schulz PJ, Nakamoto K. The perils of misinformation: When health literacy goes awry. Nat Rev Nephrol. 2022;18:135–6. doi: 10.1038/s41581-021-00534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith DA. Situating Wikipedia as a health information resource in various contexts: A scoping review. PLoS One. 2020;15:e0228786. doi: 10.1371/journal.pone.0228786. doi: 10.1371/journal.pone.0228786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.British Pain Society BPS Patient Publication. Available from: https://www.britishpainsociety.org/people-with-pain/patient-publications/#amitriptyline . [Last accessed on 2024 Apr 15] [Google Scholar]
- 6.Baldwin AJ. Readability of Online Patient Education Materials for Congenital Hand Differences. Hand (N Y) 2023 doi: 10.1177/15589447231168907. 15589447231168907. doi: 10.1177/15589447231168907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zunic A, Corcoran P, Spasic I. Sentiment analysis in health and well-being: Systematic review. JMIR Med Inform. 2020;8:e16023. doi: 10.2196/16023. doi: 10.2196/16023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shoemaker SJ, Wolf MS, Brach C. Development of the patient education materials assessment tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns. 2014;96:395–403. doi: 10.1016/j.pec.2014.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Labianca R, Sarzi-Puttini P, Zuccaro SM, Cherubino P, Vellucci R, Fornasari D. Adverse effects associated with non-opioid and opioid treatment in patients with chronic pain. Clin Drug Investig. 2012;32(Suppl 1):53–63. doi: 10.2165/11630080-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Tan CS. The need of patient education to improve medication adherence among hypertensive patients. Malays J Pharm. 2020;6:1–5. [Google Scholar]
- 11.Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12:e0186458. doi: 10.1371/journal.pone.0186458. doi: 10.1371/journal.pone.0186458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ray PP. ChatGPT: A comprehensive review on background, applications, key challenges, bias, ethics, limitations and future scope. Internet Things Cyber Phys Syst. 2023;3:121–54. [Google Scholar]
- 13.Thia I, Saluja M. ChatGPT: Is this patient education tool for urological malignancies readable for the general population? Res Rep Urol. 2024;16:31–7. doi: 10.2147/RRU.S440633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayoub NF, Lee YJ, Grimm D, Divi V. Head-to-head comparison of ChatGPT versus google search for medical knowledge acquisition. Otolaryngol Head Neck Surg. 2023 doi: 10.1002/ohn.465. doi: 10.1002/ohn.465. [DOI] [PubMed] [Google Scholar]


