Abstract
Background:
Quadricepsplasty has been used for over half a century to improve range of motion (ROM) in knees with severe arthrofibrosis. Various surgical techniques for quadricepsplasty exist, including Judet and Thompson, as well as novel minimally invasive approaches. The goal of this review was to compare outcomes between quadricepsplasty techniques for knee contractures.
Methods:
A systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Available databases were queried for all articles on quadricepsplasty. Outcomes included postoperative ROM, outcome scores, and complication rates. Secondarily, we summarized rehabilitation protocols and descriptions of all modified and novel techniques.
Results:
Thirty-three articles comprising 797 patients were included in final analysis. Thirty-five percent of patients underwent Thompson quadricepsplasty, 36% underwent Judet, and 29% underwent other techniques. After Judet and Thompson quadricepsplasty, patients achieved a mean postoperative active flexion of 92.7° and 106.4°, respectively (p < 0.01). Complication rates after Judet and Thompson were 17% and 24%, respectively. Wound infection was the most frequently recorded complication after Judet, whereas extension lag predominated for Thompson.
Conclusion:
Both the Thompson and Judet quadricepsplasty techniques offer successful treatment options to restore functional knee ROM. Although the Thompson technique resulted in greater postoperative knee flexion compared with the Judet, the difference may be attributable to differences in preoperative flexion and time from injury to quadricepsplasty. Overall, the difference in flexion gained between the 2 techniques is comparable and clinically negligible.
Level of Evidence:
Level IV. See Instructions for Authors for a complete description of levels of evidence.
Background
Arthrofibrosis of the knee involves joint stiffness because of intra-articular and extra-articular adhesions and fibrous scar tissue that retracts the quadriceps muscle and joint capsule1,2. It often presents as a postoperative complication of surgical fixation of traumatic distal femur and periarticular knee fractures3. Because of the lack of widely accepted diagnostic criteria, diagnosis is primarily based on clinical assessment and knee range of motion (ROM) deficits.4,5 Gait analysis has shown that >65° of knee flexion is required for activities of daily living (ADLs)6. Severe knee arthrofibrosis, defined as knee flexion <65° or knee ROM <70°, can cause marked disability and interfere with ADLs2,4,5. In severe extension contractures, conservative treatment is often inadequate to restore functional knee ROM and thus requires surgical intervention with the quadricepsplasty procedure1,2.
Thompson (1944) and Judet (1959) quadricepsplasty techniques and their modifications have remained the most common surgeries to treat these contractures7-10. Although both techniques are effective in increasing knee ROM, they are associated with a high rate of complications such as significant extension lag and wound infection/necrosis4,10-16. Newer techniques have been introduced to reduce morbidity of this procedure such as V-Y, quadriceps snip, arthroscopic, mini-incision, and pie-crusting quadricepsplasty; however, the outcomes and efficacy of these techniques have not been extensively explored17-25.
The purpose of this systematic review and meta-analysis was to (1) compare Thompson and Judet quadricepsplasty for post-traumatic severe knee arthrofibrosis; (2) present outcomes and complications of the techniques; (3) determine whether there is an ideal surgical approach; and (4) summarize clinical outcome data on newer quadricepsplasty techniques.
Methods
A systematic review of reported clinical outcomes for quadricepsplasty was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines26. We queried PubMed/MEDLINE, Embase, Web of Science, and Cochrane databases to identify all articles on quadricepsplasty from inception to February 5, 2023. Terms used for the title search included “quadricepsplasty,” “Thompson,” and “Judet.” Specific search terms used across databases are detailed in the Supplementary Appendix
Inclusion and Exclusion Criteria
All studies reporting on any quadricepsplasty technique, written in the English language, and reporting on ≥5 patients were included for further review. See Fig. 1 for details on exclusion criteria.
Fig. 1.
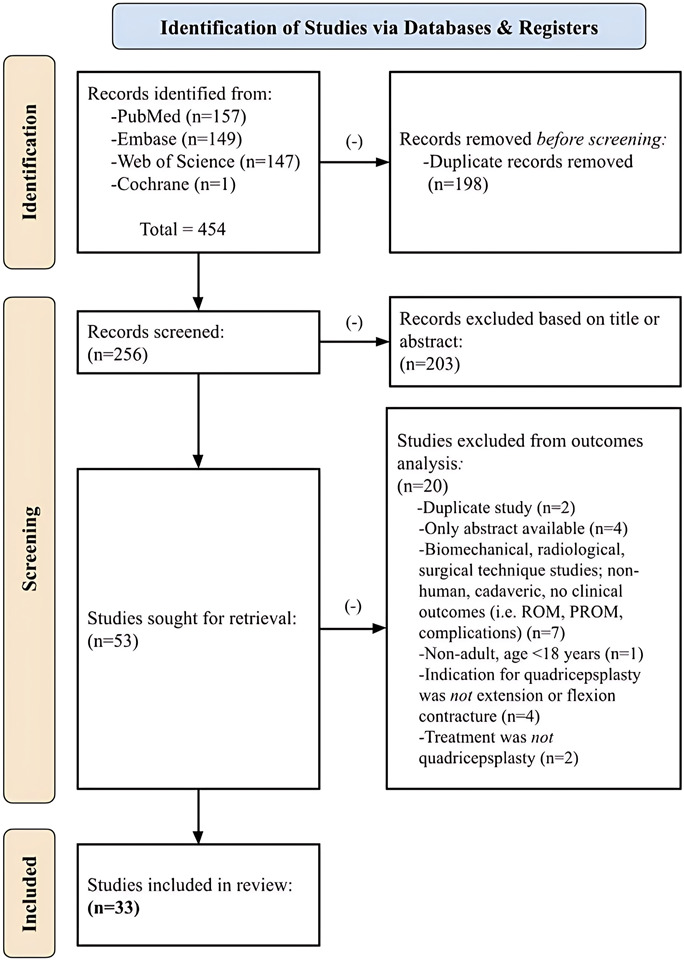
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram depicting article identification, subsequent exclusion, and analysis for clinical outcomes and complications of quadricepsplasty techniques. ROM = range of motion.
All studies identified by search results were incorporated into screening software with duplicates removed. Articles were initially screened for inclusion by 2 authors (C.G. and K.H.) by title or abstract. The same 2 authors then performed a full-text review of the remaining articles for inclusion or exclusion. Any discrepancies were resolved by the senior author.
Data Extraction
Studies that matched inclusion criteria underwent data extraction using a standardized data-collection form by 2 authors (C.G. and K.H.). During full-text review of the included articles, demographic and surgical characteristics were collected. Descriptions of modified Judet and Thompson techniques and the “other” novel quadricepsplasty techniques were also recorded including torniquet use and rectus femoris lengthening (Appendix Table I). We collected postoperative rehabilitation protocol when provided (Appendix Table II). Primary outcome was postoperative active knee flexion (POAF). Additional clinical outcomes included preoperative and intraoperative knee ROM; extension lag; outcome scores (Judet criteria and Hospital for Special Surgery [HSS] knee score); and complications.
Patients were stratified by quadricepsplasty technique into 3 groups: Judet (included modified Judet techniques), Thompson (included modified Thompson techniques), and other (included various novel quadricepsplasty techniques). To allow for further subgroup comparison, we also stratified patients into 5 categories: Judet, modified Judet, Thompson, modified Thompson, and others.
Data Synthesis and Analysis
Study characteristics were summarized as weighted means for continuous variables and count (percent) for categorical variables while accounting for the number of knees in each study. When studies stratified outcomes by treatment modality, we recorded the data as separate cohorts to enable meta-analysis where possible. Because of the heterogeneity of the data, we recorded postoperative outcome scores and complications descriptively.
The weighted mean of POAF was calculated by meta-analysis to compare the functional outcome between Judet, Thompson, and other novel techniques. Studies were included for meta-analysis if they reported one or more of the POAF and provided study-specific (Judet vs. Thompson vs. other) data required adequate for meta-analysis (number of patients, mean, and SD or minimum and maximum). Meta-analyses were performed using the meta-mean function from the R package meta43,44. For each study considered, measures of effect were represented as raw mean (MRAW) and its corresponding 95% confidence intervals (CIs). Aggregated means for each treatment type were quantified by pooling the MRAWs provided by the original studies using random effect models, and the results were represented as forest plots. Statistical heterogeneity and true effect size in 95% of the study population were assessed using the I2 and Tau2 statistics, respectively. All statistical analyses were performed using R software (version 4.2.2; R Core Team) with an α of 0.05.
Results
Search Results
A total of 33 articles on quadricepsplasty were included for data extraction and analysis. Bias assessment was performed using the Methodological Index for Nonrandomized Studies (MINORS) criteria45. Noncomparative studies had an average score of 10.8 ± 0.9, whereas comparative studies averaged 20 ± 1, indicating moderate quality of evidence. See Appendix Table III for included studies and their corresponding MINORS scores.
Study Characteristics
Of the 33 articles included for analysis, most studies were conducted in China (21%), United States (12%), and England (12%). Study designs included retrospective case series (82%), retrospective cohort (3%), prospective case series (12%), and prospective cohort (3%). The levels of evidence reported were III (6%) and IV (94%). Postoperative rehabilitation protocols varied with each individual study, ranging from cast immobilization to immediate continuous passive motion on postoperative day 0. Individual study rehabilitation protocols are summarized in Appendix Table II.
Patient Characteristics
A total of 797 patients were included in the final analysis. The overall mean age was 36.2 years, and the mean follow-up was 30.2 months. A total of 175 (22%) of the patients included were female. Most patients underwent quadricepsplasty for a preoperative diagnosis of extension contracture (96%), whereas 35 (4%) had a diagnosis of flexion contracture. Femoral shaft fractures represented the most common initial fracture injury. The most common nonfracture initial injury was secondary to limb-lengthening interventions. Patient demographic and clinical characteristics for the Judet, Thompson, and other techniques are further summarized in Table I.
Table I.
| Outcome Measure | Total (n = 797) | Judet (n = 288) | Thompson (n = 278) | Others (n = 231) |
|---|---|---|---|---|
| Age at surgery (yr) | 36.2 | 36.2 | 33.9 | 39.4 |
| Females | 175 (22) | 79 (26) | 30 (11) | 66 (29) |
| Average follow-up (mo) | 30.2 | 30.4 | 39.3 | 18.5 |
| Minimum follow-up (mo) | 13.7 | 16.9 | 14.1 | 8.7 |
| Average time from injury to quadricepsplasty (mo) | 24.2 | 31.9 | 22.5 | 15.9 |
| Preoperative diagnosis of extension contracture | 761 (96) | 277 (97) | 253 (92) | 231 (100) |
| Preoperative diagnosis of flexion contracture | 35 (4) | 10 (3) | 25 (9) | |
| Initial injury | ||||
| Fractures | ||||
| Femoral shaft fracture | 319 (40) | 152 (53) | 101 (37) | 66 (29) |
| Femoral supracondylar fracture | 156 (20) | 51 (18) | 61 (22) | 44 (19) |
| Proxima tibial fracture | 23 (3) | 15 (5) | 8 (3) | |
| Tibial plateau fracture | 69 (9) | 7 (2) | 6 (2) | 56 (24) |
| Floating knee injury | 3 (0) | 3 (1) | ||
| Fracture-dislocation of knee | 3 (0) | 1 (0) | 2 (0) | |
| Patella fracture | 45 (6) | 6 (2) | 27 (10) | 12 (5) |
| Multiple periarticular fractures of the knee* | 59 (21) | 32 (14) | ||
| Nonfractures | ||||
| Postsurgical scarring | 8 (1) | 8 (3) | ||
| Post-TKA | 1 (0) | 1 (0) | ||
| Open meniscectomy | 1 (0) | 1 (0) | ||
| Femoral osteomyelitis | 17 (2) | 17 (6) | ||
| Limb lengthening | 21 (3) | 19 (7) | 2 (0) | |
| Nonunion | 13 (2) | 13 (5) | ||
| Angular deformity | 3 (0) | 3 (1) | ||
| Rotational deformity | 1 (0) | 1 (0) | ||
| Hip conditions | 2 (0) | 2 (0) | ||
| Infection | 9 (1) | 7 (2) | 1 (0) | 1 (0) |
| Gunshot wound | 11 (1) | 11 (4) | ||
| Failed nonsurgical treatment | 9 (1) | 9 (2) | ||
| Intramuscular injection | 3 (0) | 3 (1) | ||
| Laceration to thigh | 1 (0) | 1 (0) | ||
| Degloving or burn/contracture | 3 (0) | 3 (1) | ||
| Initial treatment | ||||
| External fixation | 118 (15) | 69 (24) | 28 (10) | 21 (9) |
| Internal fixation | 242 (31) | 73 (25) | 65 (24) | 104 (45) |
| Casting | 22 (3) | 13 (5) | 8 (2) | 1 (0) |
| Patellectomy | 3 (0) | 3 (1) | ||
| Ilizarov frame | 21 (3) | 18 (6) | 2 (0) | 1 (0) |
| Traction with splint | 11 (1) | 1 (0) | 10 (4) |
≥2 fracture sites = femoral shaft, distal femur, proximal tibia, tibial plateau, patella.
Values presented as n (%), unless otherwise noted.
Clinical Outcomes
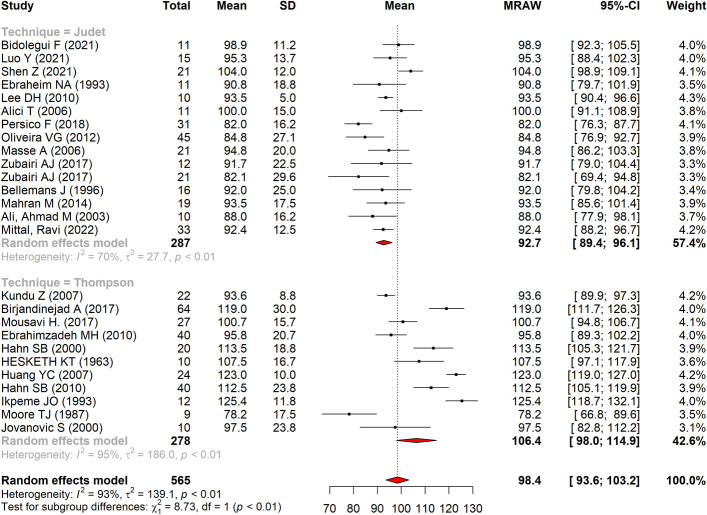
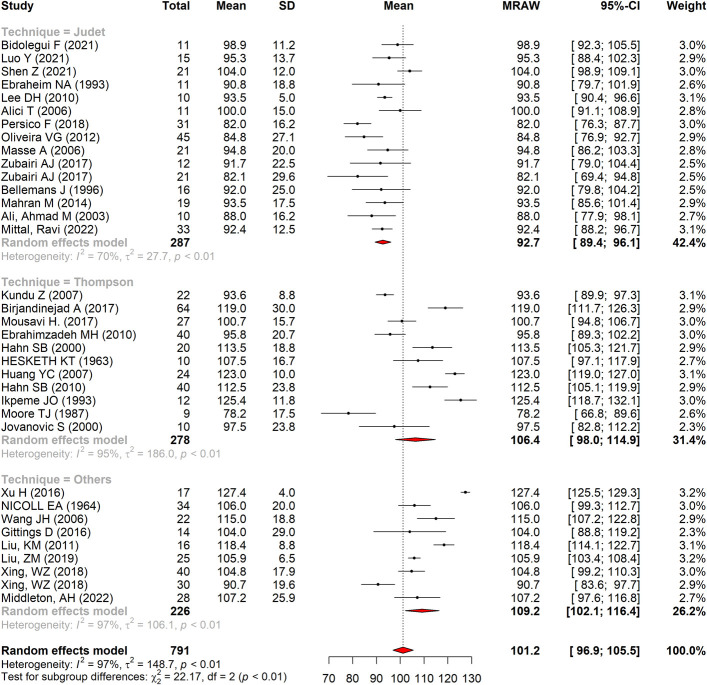
Patients who underwent Judet vs. Thompson quadricepsplasty achieved a mean POAF of 92.7° (95% CI: 89.4-96.1°) vs. 106.4° (95% CI: 98.0-114.9°), p < 0.01 (Fig. 2). Preoperative active flexion for Judet and Thompson was 27.5° and 38.5°, respectively. Postoperative flexion gained for Judet was 63.9° and 67.3° for Thompson. Postoperative extension lag was 10.8° and 9.1° for Judet and Thompson, respectively (Table II). Mean POAF between Judet, Thompson, and other techniques was 92.7° (95% CI: 89.4-96.1°), 106.4° (95% CI: 98.0-114.9°), and 109.2 (CI 102.1-116.3°), respectively (p < 0.01, Fig. 3).
Fig. 2.
Postoperative active flexion stratified by quadricepsplasty technique (Judet vs. Thompson). CI = confidence interval and MRAW = raw mean.
Fig. 3.
Postoperative active flexion stratified by quadricepsplasty technique (Judet vs. Thompson vs. others). CI = confidence interval and MRAW = raw mean.
Table II.
Outcomes and Complications for Judet vs. Thompson*
| Outcome Measure | Total (n = 566) | Judet (n = 288) | Thompson (n = 278) |
|---|---|---|---|
| Range of motion | |||
| Preoperative active flexion (°) | 32.9 | 27.5 | 38.5 |
| Intraoperative flexion (°) | 115.4 | 109.5 | 122.3 |
| Postoperative active flexion (°) | 99.6 | 90.9 | 108.7 |
| Postoperative flexion gain (°) | 65.7 | 63.9 | 67.3 |
| Postoperative extension lag (°) | 9.4 | 10.8 | 9.1 |
| Outcome scores | |||
| Judet criteria | |||
| Excellent | 239 (49) | 106 (39) | 133 (60) |
| Good | 193 (39) | 127 (47) | 66 (30) |
| Fair | 38 (8) | 25 (9) | 13 (6) |
| Poor | 21 (4) | 13 (5) | 8 (4) |
| Complications | |||
| Total complications | 117 (21) | 49 (17) | 68 (24) |
| Extension lag | 56 (10) | 11 (4) | 45 (16) |
| Wound infection | 17 (3) | 13 (5) | 4 (1) |
| Septic infection | 4 (1) | 3 (1) | 1 (0) |
| Wound complication | 14 (2) | 6 (2) | 8 (3) |
| Compartment syndrome | 1 (0) | 1 (0) | |
| Quadriceps tendon rupture | 2 (0) | 1 (0) | 1 (0) |
| Hematoma | 5 (1) | 4 (1) | 1 (0) |
| Fracture of lateral femoral condyle | 1 (0) | 1 (0) | |
| Avulsion fracture of tibial tuberosity | 3 (0) | 1 (0) | 2 (1) |
| Patella fracture | 4 (1) | 4 (1) | |
| Patella dislocation | 1 (0) | 1 (0) | |
| Rapid recurrence of contracture | 1(0) | 1 (0) | |
| Reflex sympathetic dystrophy | 1 (0) | 1 (0) | |
| Anemia requiring blood transfusion | 5 (1) | 5 (1) | |
| Anemia | 1 (0) | 1 (0) | |
| Reoperation | 1 (0) | 0 (0) | 1 (0) |
Values presented as n (%), unless otherwise noted.
Between the 5 subgroups of quadricepsplasty techniques, the average POAF was 89.5°, 93.4°, 103.7°, 110.3°, and 107.3° for Judet, modified Judet, Thompson, modified Thompson, and other techniques. Flexion gained between preoperative and postoperative measurements was comparable between the 5 subgroups. Postoperative extension lag was 10.8°, 6.5°, 9.7°, and 25.3° for Judet, Thompson, modified Thompson, and others, respectively (Table III). Average postoperative extension lag was not recorded by any of the articles published on the Modified Judet technique.
Table III.
Outcomes and Complications for Judet, Modified Judet, Thompson, Modified Thompson, and Others*
| Outcome Measure | Total (n = 797) | Judet (n = 185) | Modified Judet (n = 103) | Thompson (n = 71) | Modified Thompson (n = 207) | Others (n = 231) |
|---|---|---|---|---|---|---|
| Range of motion | ||||||
| Preoperative active flexion (°) | 35.6 | 28.3 | 26.1 | 26.0 | 42.8 | 42.2 |
| Intraoperative flexion (°) | 116.4 | 108.9 | 110.7 | 113.3 | 125.2 | 120.0 |
| Postoperative active flexion (°) | 101.9 | 89.5 | 93.4 | 103.7 | 110.3 | 107.3 |
| Postop flexion gain (°) | 65.0 | 62.2 | 68.2 | 77.6 | 63.8 | 63.5 |
| Postop extension lag (°) | 12.8 | 10.8 | 6.5 | 9.7 | 25.3 | |
| Outcome scores | ||||||
| Judet criteria | ||||||
| Excellent | 312 (52) | 64 (38) | 42 (41) | 13 (41) | 120 (58) | 73 (67) |
| Good | 218 (36) | 79 (47) | 48 (46) | 15 (47) | 51 (25) | 25 (23) |
| Fair | 47 (8) | 16 (10) | 9 (9) | 2 (6) | 11 (5) | 9 (8) |
| Poor | 23 (4) | 9 (5) | 4 (4) | 2 (6) | 6 (3) | 2 (2) |
| Complications | ||||||
| Total complications | 128 (16) | 30 (16) | 19 (18) | 14 (20) | 54 (26) | 11 (5) |
| Extension lag | 61 (8) | 8 (4) | 3 (3) | 7 (10) | 38 (18) | 5 (2) |
| Wound infection | 18 (2) | 6 (3) | 7 (7) | 0 (0) | 4 (2) | 1 (0) |
| Septic infection | 4 (0) | 3 (2) | 1 (1) | |||
| Wound complication | 14 (2) | 6 (3) | 0 (0) | 1 (1) | 7 (3) | 0 (0) |
| Compartment syndrome | 1 (0) | 1 (0) | ||||
| Quadriceps tendon rupture | 2 (0) | 1 (0) | 1 (0) | 0 (0) | ||
| Hematoma | 5 (1) | 1 (0) | 3 (3) | 1 (1) | ||
| Fracture of lateral femoral condyle | 1 (0) | 1 (0) | 0 (0) | |||
| Avulsion fracture of tibial tuberosity | 3 (0) | 1 (0) | 1 (1) | 1 (0) | ||
| Patella fracture | 4 (0) | 2 (3) | 2 (1) | 0 (0) | ||
| Patella dislocation | 2 (0) | 1 (0) | 1 (0) | |||
| Rapid recurrence of contracture | 1 (0) | 1 (0) | ||||
| Reflex sympathetic dystrophy | 1 (0) | 1 (0) | ||||
| Anemia requiring blood transfusion | 5 (1) | 5 (5) | ||||
| Anemia | 1 (0) | 1 (1) | ||||
| Reoperation | 5 (1) | 0 | 1 (1) | 4 (2) |
Values presented as n (%), unless otherwise noted.
Outcome scores according to Judet criteria were included in the analysis when available. Judet quadricepsplasty resulted in knee flexion that was considered excellent in 39% (106/271) of cases. Comparatively, the Thompson quadricepsplasty resulted in 60% (133/220) excellent cases (Table II). Excellent results between the 5 subgroups were 38% (64/168) for Judet, 41% (42/103) for modified Judet, 41% (13/32) for Thompson, 58% (120/188) for modified Thompson, and 67% (73/109) for others (Table III). The HSS Knee score was not included in the final analysis because it was not consistently recorded in all studies across cohorts.
Complications
A total of 49 complications were reported in patients who underwent Judet quadricepsplasty (17%), whereas 68 complications were reported in the Thompson cohort (24%). The most frequent outcome in the Judet cohort was wound infection, followed by extension lag. In the Thompson cohort, the most common complication was extension lag, followed by wound complication. Between these 2 techniques, only one reoperation was reported, and it was in the Thompson cohort (Table II).
When comparing the 5 quadricepsplasty subgroups, modified Thompson had the highest complication rate, and others had the lowest complication rate. The most frequently recorded complication was extension lag for Judet, Thompson, modified Thompson, and others. Wound infection was the most common complication for modified Judet. There were 4 reported reoperations in the others cohort (Table III).
Discussion
Despite the long history of quadricepsplasty, there lacks a clear consensus on the superior technique for the treatment of knee contractures. The original technique described by Thompson involves isolating the rectus femoris and then releasing the vastus lateralis and medialis from either side of the patella using a longitudinal midline10. Judet developed an alternative technique involving a stepwise release of the knee based on intraoperative flexion, without disrupting the vastus medialis oblique, vastus lateralis, or rectus femoris using lateral and medial longitudinal incisions7,46. Although literature demonstrates continued use of both quadricepsplasty techniques, much of the data are limited to small studies and lack direct comparison of the 2 techniques. This systematic review summarized the current data on various quadricepsplasty techniques including the Thompson and Judet techniques and their modifications, as well as novel techniques.
Meta-analysis yielded greater POAF in those treated with the Thompson quadricepsplasty when compared with the Judet technique; however, both techniques achieved knee flexion to a functional ROM to accomplish ADLs6. This difference in POAF may be attributed to the differences in preoperative knee flexion (38.5° for Thompson vs. 27.5° for Judet) as well as interval from injury to quadricepsplasty (22.5 months for Thompson vs. 31.9 months for Judet). Ebrahimzadeh et al.39 demonstrated quadricepsplasty within 6 months of the patient's last trauma surgery resulted in improved functional outcomes and flexion gained was greater in patients with worse preoperative flexion. It is also important to consider variability in goniometric measurement, especially given the wide range in publication dates of the included studies47-50. Overall, the flexion gained between the 2 techniques was found to be less than the minimal clinically important difference (MCID); thus, both techniques offer successful treatment options to restore knee flexion to a functional ROM48,51.
It is important to note that baseline patient characteristics, such as the initial injury and index surgery, may influence the outcome of the quadricepsplasty. Severity of arthrofibrosis may vary with the degree of articular involvement, such as intra-articular (isolated patella fractures), extra-articular injury (midshaft femur fractures), or a combination of both2. Haller et al.52 found that the use of a provisional external fixator to treat tibial plateau fractures was associated with the development of arthrofibrosis and each additional day in external fixation was associated with a 10% increased risk of developing arthrofibrosis. In this review, most patients who underwent Thompson quadricepsplasty were initially treated with internal fixation, whereas equal portions of the Judet cohort underwent either internal or external fixation. Initial injury mechanism and treatment before quadricepsplasty were variably recorded in the literature; thus, it was difficult to delineate whether the contracture was secondary to the initial injury vs. initial treatment.
Although both techniques were associated with notable excellent (final flexion ≥100°) and good (final flexion between 80° and 99°) outcomes according to Judet criteria (Tables II and III), they equally demonstrated considerable complication rates. In this review, complication rates were found to be 17% and 24% for the Judet and Thompson cohorts, respectively. Complications include quadriceps tendon rupture, wound complications, and, most notably, extension lag3,8,14,27-30,32-39,41. Permanent extension lag is an associated risk of quadricepsplasty, especially with the Thompson technique, where the rectus femoris is isolated from the rest of the quadriceps and may undergo lengthening11,31,35,40,41. Our study found a 16% rate extension lag rate in the Thompson cohort compared with only 4% in the Judet. Lower rates may be secondary to the stepwise Judet approach, which preserves the rectus femoris and reduces the potential for iatrogenic quadriceps rupture8,38,42. However, the classically described long lateral and medial incisions involved in the Judet technique are still associated with wound complications and dehiscence, as reflected in the 5% wound infection and 2% wound complication rates3,8,37,38. Modifications of the traditional techniques (Appendix Table II) sought to decrease these associated complications; however, complication rates among the modified Judet and Thompson techniques were comparable with the original Judet and Thompson techniques (Table III).
Since the advent of the Thompson and Judet techniques, several newer techniques have been described (Appendix Table II) and were included in this review to create a comprehensive landscape of the quadricepsplasty. As denoted by the others cohort in Table III, techniques explored such as the quadriceps snip, and arthroscopic lysis of adhesions effectively restored knee flexion. It is also worth noting that these techniques were used to treat a substantial number of contractures secondary to tibial plateau fractures when compared with Judet and Thompson (Table III). The total number of reported extension lag complications in the other group was low (2%); however, the degree of extension lag (25.3°) was notably high. Given the small incidence of this complication, this high average may be due to outliers in the data. It is also important to note that the “other” category encompasses a heterogenous group of techniques that did not fit the traditional Judet or Thompson techniques and their modifications, which may contribute to wider variations in the data. The study by Nicoll et al.15 reported a high average extension lag of 32° in 4 cases, which positively skewed this data point, given the small number of reported extension lag cases within this subgroup. Thus, interpretation of extension lag in this subgroup should be interpreted with caution. The main objective of this study was to evaluate the Thompson and Judet techniques; however, the comparable clinical outcomes and relatively low complication profile show promise for these newer procedures.
Although not within the scope of this meta-analysis, postoperative protocols are perhaps as important as surgical technique. Aggressive postoperative ROM therapy coupled with adequate pain control and patient compliance is necessary to maintain the ROM improvements achieved in the operating room without losing active extension. Other factors previously associated with improved outcomes include younger age and earlier time to surgery11,12,31. Future studies could be directed at evaluating these variables.
This study has limitations inherent to any systematic review and meta-analysis. Studies were primarily retrospective and, thus, subjected to reporting bias. Although the MINORS scores45 suggested moderate quality, the quality of evidence ultimately depends on individual study methodology. The body of evidence primarily consisted of level IV evidence, as we did not set a minimum level of evidence for inclusion. Limiting inclusion to articles with full text published in the English language may have resulted in a loss of literature and a potential bias. Publication bias also impacts available and included data. Statistical comparison of some clinical characteristics was not feasible, given the heterogeneity of the data, thus limiting portions of the data to descriptive statistics. Systematic review methodology limits data interpretation to the reporting methods of the individual articles, and thus, we were unable to stratify differences in quadricepsplasty outcomes by initial injury or index surgery. We were also unable to statistically analyze postoperative rehabilitation regiments, which remains an important limitation in comparison of these techniques. Despite these limitations, this study provided a comprehensive review and meta-analysis that compares current quadricepsplasty techniques for the treatment of severe knee contractures about the knee joint. Future cohort studies should further investigate the role of novel, minimally invasive quadricepsplasty techniques within these patient populations.
Conclusion
Both Judet and Thompson quadricepsplasty techniques are reliable options to restore ROM in patients with knee contractures. Although the Thompson technique yielded significantly greater postoperative knee flexion compared with Judet, the overall difference in preoperative to postoperative flexion gained between these 2 techniques was within the MCID and thus clinically insignificant. Compared with the Judet, the Thompson approach was associated with an overall higher complication rate and particularly greater risk of postoperative extension lag. Modifications to the traditional Judet and Thompson techniques yielded similar clinical outcomes and complication rates. Newer minimally invasive quadricepsplasty techniques demonstrate promise with similar outcome profiles, and future comparative studies should be directed at discerning their role in the treatment of knee arthrofibrosis.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A650). This content was not copyedited or verified by JBJS.
Footnotes
Investigation performed at Cooper University Hospital, Camden, New Jersey
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A649).
Contributor Information
Caroline T Gutowski, Email: gutows24@rowan.edu.
Kathryn Hedden, Email: hedden-katie@cooperhealth.edu.
Parker Johnsen, Email: johnsen-parker@cooperhealth.edu.
John E Dibato, Email: dibato-john@cooperhealth.edu.
Christopher Rivera-Pintado, Email: Rivera-Pintado-Christopher@CooperHealth.edu.
References
- 1.Paley D, Pfeil J. Principles of deformity correction around the knee [in German]. Der Orthopäde. 2000;29(1):18-38. [DOI] [PubMed] [Google Scholar]
- 2.Pujol N, Boisrenoult P, Beaufils P. Post-traumatic knee stiffness: surgical techniques. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S179-86. [DOI] [PubMed] [Google Scholar]
- 3.Luo Y, Li H, Mei L, Mao X. Effects of Judet quadricepsplasty in the treatment of post-traumatic extension contracture of the knee. Orthop Surg. 2021;13(4):1284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen Z, Deng Y, Peng A, Zhang Y. Modified Judet's quadricepsplasty plus patellar traction for knee stiffness after femoral fracture surgery. Int Orthop. 2021;45(5):1137-45. [DOI] [PubMed] [Google Scholar]
- 5.Thompson R, Novikov D, Cizmic Z, Feng JE, Fideler K, Sayeed Z, Meftah M, Anoushiravani AA, Schwarzkopf R. Arthrofibrosis after total knee arthroplasty: pathophysiology, diagnosis, and management. Orthop Clin North Am. 2019;50(3):269-79. [DOI] [PubMed] [Google Scholar]
- 6.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52(1):34-43. [DOI] [PubMed] [Google Scholar]
- 7.Judet J, Judet R, Lagrange J. Technic of liberation of the extensor apparatus in knee stiffness [in French]. Mem Acad Chir (Paris). 1956;82(29-30):944-7. [PubMed] [Google Scholar]
- 8.Mittal R, Digge V, Jain S. Judet's quadricepsplasty technique offers excellent functional outcome without an extension lag for extension contracture of the knee: a retrospective cohort of 33 patients. Indian J Orthop. 2022;56(11):1913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mousavi H, Mir B, Safaei A. Evaluation of Thompson's quadricepsplasty results in patients with knee stiffness resulted from femoral fracture. J Res Med Sci. 2017;22:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson TC. Quadricepsplasty. Ann Surg. 1945;121(5):751-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birjandinejad A, Ebrahimzadeh MH, Sayyed-Hosseinian SH, Tabesh S, Ghanbarifard M. Prognostic factors affecting the results of modified Thompson quadricepsplasty for the treatment of extension contracture of the knee. Arch Bone Joint Surg. 2017;5(2):109-13. [PMC free article] [PubMed] [Google Scholar]
- 12.Kundu Z, Sangwan S, Guliani G, Siwach R, Kamboj P, Singh R. Thompson's quadricepsplasty for stiff knee. Indian J Orthop. 2007;41(4):390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee DH, Kim TH, Jung SJ, Cha EJ, Bin SI. Modified Judet quadricepsplasty and Ilizarov frame application for stiff knee after femur fractures. J Orthop Trauma. 2010;24(11):709-15. [DOI] [PubMed] [Google Scholar]
- 14.Masse A, Biasibetti A, Demangos J, Dutto E, Pazzano S, Gallinaro P. The Judet quadricepsplasty: long-term outcome of 21 cases. J Trauma. 2006;61(2):358-62. [DOI] [PubMed] [Google Scholar]
- 15.Nicoll EA. Quadricepsplasty: the treatment of stiff knee following trauma. Postgrad Med J. 1964;40(467):521-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zubairi AJ, Rashid H, Rashid RH, Ali M, Hashmi PM. Outcome of Judet's quadricepsplasty for knee contractures and the effect of local infiltration of epinephrine on reducing blood loss. Chin J Traumatol. 2017;20(3):147-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gittings D, Hesketh P, Dattilo J, Zgonis M, Kelly J, Mehta S. Arthroscopic lysis of adhesions improves knee range of motion after fixation of intra-articular fractures about the knee. Arch Orthop Trauma Surg. 2016;136(12):1631-5. [DOI] [PubMed] [Google Scholar]
- 18.Liu KM, Liu S, Cui Z, Han X, Tang T, Wang A. A less invasive procedure for posttraumatic knee stiffness. Arch Orthop Trauma Surg. 2011;131(6):797-802. [DOI] [PubMed] [Google Scholar]
- 19.Liu Z, Li Y, Sun P, Sang P, Zhang C, Ren Y, Yang J, Zhu X, Huang W, Liu Y. All-arthroscopic release for treating severe knee extension contractures could improve the knee range of motion and the mid-term functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):724-30. [DOI] [PubMed] [Google Scholar]
- 20.Middleton AH, Perlewitz MA, Edelstein AI, Vetter CS. Knee arthrofibrosis following tibial plateau fracture treated with arthroscopic lysis of adhesions with manipulation. J Knee Surg. 2022;35(7):816-20. [DOI] [PubMed] [Google Scholar]
- 21.Trousdale RT, Hanssen AD, Rand JA, Cahalan TD. V-Y quadricepsplasty in total knee arthroplasty. Clin Orthop Relat Res. 1993;286:48-55. [PubMed] [Google Scholar]
- 22.Wang JH, Zhao JZ, He YH. A new treatment strategy for severe arthrofibrosis of the knee. Surgical technique. J Bone Joint Surg Am. 2007;89(suppl 2 Pt.1):93-102. [DOI] [PubMed] [Google Scholar]
- 23.Xing W, Sun L, Sun L, Liu C, Kong Z, Cui J, Zhang Z. Comparison of minimally invasive arthrolysis vs. conventional arthrolysis for post-traumatic knee stiffness. J Orthop Sci. 2018;23(1):112-6. [DOI] [PubMed] [Google Scholar]
- 24.Xu H, Ying J. A mini-invasive procedure for treating arthrofibrosis of the knee. Acta Orthop Traumatol Turc. 2016;50(4):424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhamilov V, Karatosun V, Kalkan S, Unver B, Gunal I. Evaluation of extensor mechanism in revision knee arthroplasty. J Arthroplasty. 2017;32(8):2484-6. [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bidolegui F, Pereira SP, Pires RE. Safety and efficacy of the modified Judet quadricepsplasty in patients with post-traumatic knee stiffness. Eur J Orthop Surg Traumatol. 2021;31(3):549-55. [DOI] [PubMed] [Google Scholar]
- 28.Alici T, Buluc L, Tosun B, Sarlak AY. Modified Judet's quadricepsplasty for loss of knee flexion. Knee. 2006;13(4):280-3. [DOI] [PubMed] [Google Scholar]
- 29.Persico F, Vargas O, Fletscher G, Zuluaga M. Treatment of extraarticular knee extension contracture secondary to prolonged external fixation by a modified Judet quadricepsplasty technique. Strateg Trauma Limb Reconstr. 2018;13(1):19-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahran M, El Batrawy Y, Sala F, Al Kersh M. Quadricepsplasty: a sustained functional achievement in front of a deteriorated flexion gain. Injury. 2014;45(10):1643-7. [DOI] [PubMed] [Google Scholar]
- 31.Ebrahimzadeh MH, Birjandi-Nejad A, Ghorbani S, Khorasani MR. A modified Thompson quadricepsplasty for extension contracture resulting from femoral and periarticular knee fractures. J Trauma. 2010;68(6):1471-5. [DOI] [PubMed] [Google Scholar]
- 32.Hahn SB, Lee WS, Han DY. A modified Thompson quadricepsplasty for the stiff knee. J Bone Joint Surg Br. 2000;82(7):992-5. [DOI] [PubMed] [Google Scholar]
- 33.Huang YC, Wu CC. Modified Thompson quadricepsplasty to treat extension contracture of the knee after surgical treatment of patellar fractures. Chang Gung Med J. 2007;30(3):263-9. [PubMed] [Google Scholar]
- 34.Hahn SB, Choi YR, Kang HJ, Lee SH. Prognostic factors and long-term outcomes following a modified Thompson's quadricepsplasty for severely stiff knees. J Bone Joint Surg Br. 2010;92(2):217-21. [DOI] [PubMed] [Google Scholar]
- 35.Moore TJ, Harwin C, Green SA, Garland DE, Chandler RW. The results of quadricepsplasty on knee motion following femoral fractures. J Trauma. 1987;27(1):49-51. [DOI] [PubMed] [Google Scholar]
- 36.Jovanovic S, Orlic D, Wertheimer B, Zelic Z, Has B. Quadricepsplasty after war fractures. Mil Med. 2000;165(4):263-7. [PubMed] [Google Scholar]
- 37.Ali AM, Villafuerte J, Hashmi M, Saleh M. Judet's quadricepsplasty, surgical technique, and results in limb reconstruction. Clin Orthop Relat Res. 2003;415:214-20. [DOI] [PubMed] [Google Scholar]
- 38.Bellemans J, Steenwerckx A, Brabants K, Victor J, Lammens J, Fabry G. The Judet quadricepsplasty: a retrospective analysis of 16 cases. Acta Orthop Belg. 1996;62(2):79-82. [PubMed] [Google Scholar]
- 39.Ebraheim NA, DeTroye RJ, Saddemi SR. Results of Judet quadricepsplasty. J Orthop Trauma. 1993;7(4):327-30. [DOI] [PubMed] [Google Scholar]
- 40.Hesketh KT. Experiences with the Thompson quadricepsplasty. J Bone Joint Surg Br. 1963;45:491-5. [PubMed] [Google Scholar]
- 41.Ikpeme JO. Quadricepsplasty following femoral shaft fractures. Injury. 1993;24(2):104-8. [DOI] [PubMed] [Google Scholar]
- 42.Oliveira VG, D'Elia LF, Tirico LE, Gobbi RG, Pecora JR, Camanho GL, Angelini FJ, Demange MK. Judet quadricepsplasty in the treatment of posttraumatic knee rigidity: long-term outcomes of 45 cases. J Trauma Acute Care Surg. 2012;72(2):E77-80. [DOI] [PubMed] [Google Scholar]
- 43.Cooper H, Hedges LV, Valentine JC. Research synthesis as a scientific enterprise. In: The Handbook of Research Synthesis and Meta-Analysis. New York, NY: Russell Sage Foundation; 1994:3-16. [Google Scholar]
- 44.Paule RC, Mandel J. Consensus values and weighting factors. J Res Natl Bur Stand. 1977;87(5):377-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-6. [DOI] [PubMed] [Google Scholar]
- 46.Pataru R, Gutowski CT, Martinez-Casaneda D, Patel D, Rivera-Pintado C, Graf K. Quadricepsplasty for Extension Contracture. Camden, NJ: American Academy of Orthopaedic Surgeons Orthopaedic Video Theater; 2023. [Google Scholar]
- 47.Bennett D, Hanratty B, Thompson N, Beverland D. Measurement of knee joint motion using digital imaging. Int Orthop. 2009;33(6):1627-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cleffken B, van Breukelen G, Brink P, van Mameren H, Olde Damink S. Digital goniometric measurement of knee joint motion. Evaluation of usefulness for research settings and clinical practice. Knee. 2007;14(5):385-9. [DOI] [PubMed] [Google Scholar]
- 49.Jakobsen TL, Christensen M, Christensen SS, Olsen M, Bandholm T. Reliability of knee joint range of motion and circumference measurements after total knee arthroplasty: does tester experience matter? Physiother Res Int. 2010;15(3):126-34. [DOI] [PubMed] [Google Scholar]
- 50.Naylor JM, Ko V, Adie S, Gaskin C, Walker R, Harris IA, Mittal R. Validity and reliability of using photography for measuring knee range of motion: a methodological study. BMC Musculoskelet Disord. 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guzik A, Drużbicki M, Wolan-Nieroda A, Turolla A, Kiper P. Estimating minimal clinically important differences for knee range of motion after stroke. J Clin Med. 2020;9(10):3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haller JM, Holt DC, McFadden ML, Higgins TF, Kubiak EN. Arthrofibrosis of the knee following a fracture of the tibial plateau. Bone Joint J. 2015;97-b(1):109-14. [DOI] [PubMed] [Google Scholar]