Abstract
Objectives:
To compare patients' self-administered responses to the Fecal Incontinence Severity Index (FISI) questionnaire (A1) with their responses to physician's oral interview (A3).
Methods:
Patients (n=100: mean age: 72 years; 66 women) with FI completed the FISI and the modified FISI (with written explanations) questionnaires, followed by a physician interview. To identify a threshold for the rating gap between A1 and A3, we calculated each patient's mean difference in the FISI scores.
Results:
There was no significant difference in the FISI scores between A1 and A3. A rating gap existed in the FISI scores (mean difference=8.9). It occurred in 37% of the patients, making its threshold 9. Multivariate analysis revealed that older age and no history of pelvic floor surgery were independently associated with the presence of a rating gap in the FISI scores. The in-coincidence of ticked boxes to all types of leakage between the self-administered responses and those by physician's oral history was 49% (197/400). Older age was associated with the in-coincidence of a ticked box between the assessment results of gas or solid stool leakage.
Conclusions:
Some non-negligible discrepancy existed between patients' self-administered responses and their responses to physician's oral interview, especially in older patients.
Keywords: fecal incontinence, patient's self-administered responses, responses of patients by physician's oral interview
Introduction
Fecal incontinence (FI), the inability to control stool loss, affects 2%-5% of the general population and up to 15% of older adults living in the community[1,2]. Assessing the severity of FI is important for researchers and clinicians evaluating FI to determine the appropriate management strategies and to judge the degree of effectiveness of interventions. Multiple instruments are available to measure the severity of FI. The Fecal Incontinence Severity Index (FISI)[3] is a psychometrically robust instruments used for assessing symptom severity. The Cleveland Clinic Florida Fecal Incontinence Score[4] and Vaizey incontinence score[5] are used to determine not only the frequency of FI symptoms but also the frequency of “lifestyle alterations”; thus, they do not solely assess the symptom severity.
Despite progress in the assessment of FI severity, the use of these validated instruments is limited without an understanding of whether patients' self-administered responses to the instruments are identical to the responses of patients by physician's oral interview. However, previous published articles have not compared the FI severity based on self-administered responses with that based on the responses of patients by physician's oral interview, where the latter seems more accurate.
To address this issue, we compared each patient's self-administered responses to the FISI questionnaire with the responses of patients by physician's oral interview. Additionally, the patients' self-administered responses to the FISI questionnaire were compared with their responses to the modified FISI questionnaire, where symptoms are documented in writing.
Methods
This study was conducted at a proctology clinic in Kameda Medical Center. Between August 2022 and October 2023, consecutive patients whose primary complaint was FI were screened for eligibility. Patients aged at least 18 years, who planned to undergo FI treatment, with no severe cognitive impairment, and who were not blind or deaf were analyzed. This study was approved by the regional Ethics Committee (approved number 22-048). Written informed consent was obtained from all study participants.
Incontinence severity was evaluated using the FISI[4]. The FISI is based on a type × frequency matrix. The matrix includes four types of leakage commonly found in the FI population (gas, mucus, liquid stool, and solid stool) and five frequencies (one to three times per month, once per week, twice or more per week, once per day, and twice or more per day) (Table 1). To understand the four types of leakage more clearly, these were expressed in writing (Table 2, modified FISI which is the authors' original). “Gas” was changed to “Break wind unexpectedly”, “Mucus” to “Mucus adheres to underwear or pads or leak out,” “Liquid stool” to “Liquid stool adheres to underwear or pads or leak out,” and “Solid stool” to “Solid stool adheres to underwear or pads or leak out.” The four types of leakage were sorted in reverse order to avoid replicating the patients' original FISI responses (Table 2). Patients were asked to tick only one box per row. Each of the four items (types of leakage) is awarded various points, depending on the frequency at which that type of incontinence is experienced. The maximum number of points that can be awarded for liquid stool incontinence with frequency of two or more times per week per individual is 19. A total score is the sum of all points and varies from 0 to 61, where the higher the score, the higher the perceived severity of the FI.
Table 1.
Fecal Incontinence Severity Index.
For each of the following, please indicate on average how often in the past month you experienced any amount of accidental bowel leakage: (Check only one box per row).
| 1 to 3 Times | Once a | 2 or More | Once a | 2 or More | ||
|---|---|---|---|---|---|---|
| Never | a Month | Week | Times a Week | Day | Times a day | |
| Gas | □ | □ | □ | □ | □ | □ |
| Mucus | □ | □ | □ | □ | □ | □ |
| Liquid stool | □ | □ | □ | □ | □ | □ |
| Solid stool | □ | □ | □ | □ | □ | □ |
Table 2.
Modified Fecal Incontinence Severity Index.
For each of the following, please indicate on average how often in the past month you experienced any amount of accidental bowel leakage: (Check only one box per row).
| 1 to 3 Times | Once a | 2 or More | Once a | 2 or More | ||
|---|---|---|---|---|---|---|
| Never | a Month | Week | Times a Week | Day | Times a day | |
| Solid stool adheres to underwear or pads or leak out. | □ | □ | □ | □ | □ | □ |
| Liquid stool adheres to underwear or pads or leak out. | □ | □ | □ | □ | □ | □ |
| Mucus adheres to underwear or pads or leak out. | □ | □ | □ | □ | □ | □ |
| Break wind unexpectedly. | □ | □ | □ | □ | □ | □ |
FI was defined based on the patient's responses to the FISI questionnaire; the leakage of solid or liquid stool with or without the use of pads was defined as FI. Because the initial two FISI questionnaires were used to assess gas or mucus incontinence, patients who only completed these questionnaires were excluded from the study.
A physician explained the study to patients for 5 min. Patients who presented with FI completed the FISI questionnaire as an initial assessment (A1). After 2-3 min, they were asked to respond to the modified FISI questionnaire as a second assessment (A2). Again, after 2-3 min, the patients were interviewed by a Japanese physician (A.T.) to determine the FISI score as a third assessment (A3). Data on age, sex, duration of FI, type of FI (passive, urge, and mixed), disease or condition which may cause FI, history of surgery in the pelvic floor, and use of electric bidet before and/or after defecation were collected.
The primary outcome was to explore the rating gap between the FISI scores assessed based on self-administration (A1) and the FISI scores assessed based on oral interview by a physician (A3) and to determine the factors associated with the rating gap. This was a prospective experimental study.
Statistical analysis
Statistical analysis was performed using SPSS v26 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as the mean with the corresponding 95% confidence interval (CI) and analyzed using the Wilcoxon signed rank test for paired data and the Mann-Whitney U test for unpaired data. Qualitative data were analyzed using the chi-square test. A P-value of <0.05 was considered significant.
Analysis 1
The mean difference between the FISI scores of each patient on A1 and A3 was computed. When the difference between the patient's responses to the two questionnaires exceeded the computed score, the patient was considered positive for a rating gap in the FISI score. We used the receiver operating characteristic curve analysis for changes in age that differentiated between patients with and without a rating gap in the FISI score. The cut-off value was assessed using Youden's index. A stepwise multiple regression analysis was used to determine the characteristics independently associated with the presence of a substantial rating gap in the FISI scores.
Analysis 2
The in-coincidence of ticked boxes related to each type of leakage between the FISI responses on A1 and those on A2, between the FISI responses on A1 and those on A3, or between the FISI responses on A2 and those on A3 were computed and compared between the groups. A stepwise multiple analysis was used to determine the characteristics independently associated with the presence of in-coincidence of ticked boxes related to each type of leakage between the FISI responses on A1 and those on A3.
Results
During the study period, 113 patients with FI symptoms were examined at a proctology clinic. Of these patients, eight who had been diagnosed with severe cognitive impairment and five patients with extremely hard of hearing or who were deaf were excluded. The remaining patients were included in this study. Table 3 shows the characteristics of 100 patients. Their mean age was 72 years (CI 69-75 years); approximately 66% of the study patients were women. FI types, duration of FI symptoms, previous pelvic surgery, and bidet use before or after defecation were not significantly different between sex groups. Women had more previous experience of a physician-led oral interview assessment of FISI than men (20/66 vs. 3/34, P = 0.02).
Table 3.
Characteristics of Patients (n= 100).
| Age, years | Mean (95% CI) 72 (69-75) | |
| Sex | Men | 34 |
| Women | 66 | |
| FI type | Passive | 74 |
| Urge | 16 | |
| Mixed | 10 | |
| Duration of FI, months | Mean (95% CI) 39.6 (23.4-55.8) | |
| Disease or condition which may cause FI | ERP | 13 |
| RAI | 13 | |
| Mucosal prolapse | 2 | |
| Rectocele | 5 | |
| Sphincter injury | 5 | |
| Prolapsed hemorrhoids | 5 | |
| Neurological disorder | 7 | |
| Irritable bowel syndrome | 8 | |
| Radiation-induced proctitis | 2 | |
| Low anal pressure | 17 | |
| Others | 23 | |
| Previous surgery of pelvic floor | No | 56 |
| Yes | 44 | |
| Surgery for anal disease | 12 | |
| Sphincter repair | 2 | |
| LVR for ERP | 8 | |
| Delorme’ procedure for ERP | 3 | |
| LVR for RAI | 4 | |
| Sphincter saving rectal cancer surgery | 2 | |
| Rectocele repair | 2 | |
| POP surgery | 2 | |
| Hysterectomy | 4 | |
| Others | 5 | |
| Bidet use | No | 51 |
| Yes | 49 | |
| Previous experience of a physician-led | No | 77 |
| oral interview assessment | Yes | 23 |
Values are presented as n, unless otherwise indicated.
CI, confidence interval; FI, fecal incontinence; ERP, external rectal prolapse; RAI, rectoanal intussusception; LVR, laparoscopic ventral rectopexy; POP, pelvic organ prolapse
Table 4 shows the comparison of the FISI scores or scores for each of the FISI components in the three assessments. There was no significant difference in the FISI scores between A1 (self-administered responses on the original FISI questionnaire) and A3 (the responses of patients from physician's oral interview). The mean FISI scores on A2 (self-administered responses on the modified FISI questionnaire) were significantly greater than those on A1 and A3. The scores for solid stool leakage on A3 were significantly smaller than those on A1 and A2. The scores for gas leakage on A2 were significantly greater than those on A1 and A3. When dividing the patients into Groups 1 (with previous experience of a physician-led oral interview assessment of FISI) and 2 (without previous experience of a physician-led oral interview assessment of FISI), the mean FISI scores in either group were not significantly different among the three assessments. There were significant differences in the scores for some of the FISI components between the assessments (the scores for gas in Group 2, the scores for mucus in Group 1, and the scores for solid stool in both groups).
Table 4.
Comparison of the Total FISI Scores or Scores of Each FISI Component among Three Assessments.
| Assessment | Self-administration to the FISI questionnaire (A1) |
Self-administration to the modified FISI questionnaire (A2) |
Physician-led oral interview assessment of the FISI questionnaire (A3) |
|
|---|---|---|---|---|
| FISI scores | 22.9 (20.1-25.6) | 25.9 (23.2-28.5) * | 23.5 (21.3-25.7) | |
| Group 1 (n = 23) | 25.1 (20.8-29.4) | 27.0 (22.4-31.5) | 22.9 (19.3-26.5) | |
| Group 2 (n=77) | 22.2 (18.9-25.5) | 25.5 (22.3-28.7) | 23.7 (21.0-26.4) | |
| Gas | 5.2 (4.3-6.2) | 6.6 (5.6-7.5) * | 5.8 (4.9-6.8) | |
| Group 1 (n = 23) | 7.3 (5.4 -9.3) | 7.5 (5.5-9.5) | 6.8 (4.8-8.8) | |
| Group 2 (n=77) | 4.6 (3.5-5.7) ‡ | 6.3 (5.5-9.5) | 5.5 (4.4-6.6) | |
| Mucus | 4.0 (3.1-4.9) | 4.1 (3.2-4.9) | 3.9 (3.0-4.7) | |
| Group 1 (n = 23) | 3.7 (1.9-5.7) # | 2.7 (1.0-4.4) | 1.6 (0.3-2.8) | |
| Group 2 (n=77) | 4.1 (3.1-5.1) | 4.5 (3.5-5.5) | 4.5 (3.5-5.6) | |
| Liquid stool | 7.4 (6.2-8.6) | 8.1 (6.9-9.3) | 8.7 (7.5-9.9) | |
| Group 1 (n = 23) | 7.3 (5.3-9.4) | 8.3 (5.8-10.7) | 7.8 (5.5-10.0) | |
| Group 2 (n=77) | 7.5 (6.0-8.9) | 8.0 (6.6-9.5) | 9.0 (7.6-10.4) | |
| Solid stool | 6.2 (5.0-7.5) | 7.2 (5.9-8.4) | 5.1 (7.5-9.9) † | |
| Group 1 (n = 23) | 6.7 (4.2-9.1) | 8.5 (5.9-11.1) * | 6.8 (4.5-9.1) | |
| Group 2 (n=77) | 6.1 (4.6-7.5) | 6.8 (5.3-8.2) | 4.6 (3.3-6.0) † | |
FISI, Fecal Incontinence Severity Index; Group 1, Patients with previous experience of a physician-led oral interview assessment of FISI; Group 2, Patients without previous experience of a physician-led oral interview assessment of FISI.
*P < 0.05 vs. A1 and A3; †P < 0.05 vs. A1 and A2; #P < 0.05 vs. A3; ‡P <0.05 vs. A2.
The mean difference between the FISI scores assessed in each patient on A1 and A3 was 8.9 (standard error 0.94) (Figure 1). Then, when the difference was 9 or more in each patient, the patient was considered positive for rating gap in the FISI scores. Figure 2 shows the number of patients based on the difference between the FISI scores assessed on A1 and A3. Consequently, 37 (37%) patients were positive for a rating gap in the FISI score. The cut-off value of age using Youden's index was 66 years. A multivariate analysis revealed that older age (66 years and more) and no history of pelvic floor surgery were independently associated with the presence of rating gap in the FISI scores (Table 5). Although no significance was observed, a rating gap in the FISI scores was found in 41% (15/37) of patients aged ≥80 years and 60% (3/5) of those aged ≥90 years. In Group 2, the mean difference between the FISI scores assessed in each patient on A1 and A3 was 9.9. When the difference was 10 or more in each patient, the patient was considered positive for rating gap in the FISI scores. Ther cut-off value of age using Youden's index in Group 2 was 65 years. A multivariate analysis revealed that older age (65 years and more) was independently associated with the presence of rating gap in the FISI scores (Table 6). No variables were selected in equation in Group 1 patients using a multivariate analysis.
Figure 1.

Mean difference between the FISI scores based on self-administration by patients and based on oral interview by a physician.
FISI, Fecal Incontinence Severity Index; bar, standard error.
Mean value is 8.9 (standard error 0.94).
Figure 2.
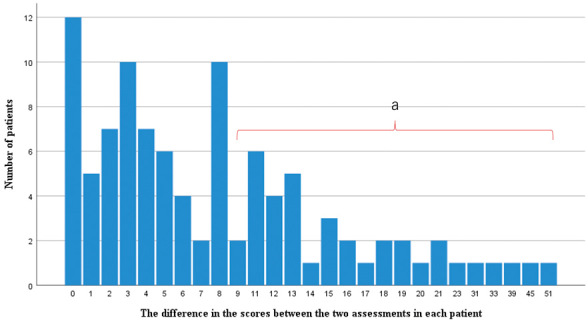
Number of patients based on the difference between the FISI scores obtained by self-administration by patients and the responses of patients by physician’s oral interview.
FISI, Fecal Incontinence Severity Index; a, A total of 37 patients who showed a rating gap (≥9) in the FISI scores.
Table 5.
Multiple Regression Showing the Characteristics Independently Associated with the Presence of Rating Gap in the FISI Scores* in All Subjects (n = 100).
| Variables included in equation | Unstandardized regression weight |
t value | P value | Variance explained |
|---|---|---|---|---|
| Age, 66 years and more | 0.35 | 3.35 | 0.001 | 13% |
| No previous history of pelvic surgery | 0.23 | 2.13 | 0.04 |
*defined as positive when the difference between the FISI scores on self-administration and those on physician-led oral interview assessment in each patient was 9 or more; FISI, Fecal Incontinence Severity Index
Table 6.
Multiple Regression Showing the Characteristics Independently Associated with the Presence of Rating Gap in the FISI Scores* in Patients without Previous Experience of a Physician-Led Oral Interview Assessment (n = 77).
| Variables included in equation | Unstandardized regression weight |
t value | P value | Variance explained |
|---|---|---|---|---|
| Age, 65 years and more | 0.40 | 3.20 | 0.002 | 12% |
*defined as positive when the difference between the FISI scores on self-administration and those on physician-led oral interview assessment in each patient was 10 or more; FISI, Fecal Incontinence Severity Index
Table 7 shows the in-coincidence rates of ticked boxes related to all types of leakage or for each type of leakage between the assessments on A1 and A2, between the assessments on A1 and A3, and between the assessments on A2 and A3. When dividing the patients into Groups 1 and 2, there was no significant difference between Group 1 (51%) and Group 2 (49%) in the in-coincidence rates of the ticked box for all types of leakage between the assessments on A1 and A3 (P=0.69).
Table 7.
In-Coincidence Rates of Ticked Boxes Related to All Types of Leakage or Each Type of Leakage between the Assessments.
| Between A1 and A3 | Between A2 and A3 | Between A1 and A2 | ||
|---|---|---|---|---|
| FISI scores | 49% (197/400) | 41% (163/400) | 39% (155/400) | |
| Group 1 (n = 23) | 51% (47/92) | 37% (34/92) | 48% (44/92) | |
| Group 2 (n=77) | 49% (150/308) * | 42% (129/308) | 40% (123/308) | |
| Gas | 54% (54/100) | 39% (39/100) | 44% (44/100) | |
| Group 1 (n = 23) | 61% (14/23) | 30% (7/23) | 57% (13/23) | |
| Group 2 (n=77) | 52% (40/77) | 42% (32/77) | 56% (43/77) | |
| Mucus | 49% (49/100) | 41% (41/100) | 33% (33/100) | |
| Group 1 (n = 23) | 52% (12/23) | 35% (8/23) | 48% (11/23) | |
| Group 2 (n=77) | 48% (37/77) | 43% (33/77) | 29% (22/77) | |
| Liquid stool | 54% (54/100) | 42% (42/100) | 46% (46/100) | |
| Group 1 (n = 23) | 52% (12/23) | 48% (11/23) | 52% (12/23) | |
| Group 2 (n=77) | 55% (42/77) | 40% (31/77) | 44% (34/77) | |
| Solid stool | 40% (40/100) | 41% (41/100) | 32% (32/100) | |
| Group 1 (n = 23) | 39% (9/23) | 35% (8/23) | 35% (8/23) | |
| Group 2 (n=77) | 40% (31/77) | 43% (33/77) | 31% (24/77) | |
FISI, Fecal Incontinence Severity Index; A1, Self-administration to the FISI; A2, Self-administration to the modified FISI; A3, Physician-led oral interview assessment of the FISI.
Group 1, Patients with previous experience of a physician-led oral interview assessment of FISI; Group 2, Patients without previous experience of a physician-led oral interview assessment of FISI.
*P = 0.69 vs. Group 1.
Multivariate analysis revealed that older age (66 years and more) was independently associated with the in-coincidence of ticked boxes corresponding to gas or solid stool leakage between the assessments on A1 and A3. Similarly, no bidet use and no history of pelvic surgery were associated with the in-coincidence of ticked boxes related to mucus leakage and liquid stool leakage between the assessments on A1 and A3, respectively. This finding indicates that bidet use was predictive of the coincidence of the ticked box related to mucus leakage, and previous history of pelvic surgery was associated with the coincidence of the ticked box for liquid stool leakage (Table 8). Group 2 patients also similar results. Multivariate analysis in Group 2 also showed the similar results, except the age included in the equation (65 years and more) (Table 9).
Table 8.
Multiple Regression Showing the Characteristics Independently Associated with the Presence of In-Coincidence for Ticked Boxes to Each Type of Leakage between the FISI Assessments on A1 and A3 in All Subjects (n = 100).
| Variables included in equation | Unstandardized regression weight |
t value | P value | Variance explained |
|---|---|---|---|---|
| Gas | ||||
| Age, 66 years and more | 0.24 | 2.11 | 0.037 | 4.3% |
| Mucus | ||||
| No bidet use | 0.32 | 3.35 | 0.001 | 10.3% |
| Liquid stool | ||||
| No previous history of pelvic surgery | 0.23 | 2.37 | 0.02 | 5.4% |
| Solid stool | ||||
| Age, 66 years and more (no, yes) | 0.27 | 2.40 | 0.018 | 5.6% |
FISI, Fecal Incontinence Severity Index; A1, Self-administration to the FISI; A3, Physician-led oral interview assessment of the FISI.
Table 9.
Multiple Regression Showing the Characteristics Independently Associated with the Presence of In-Coincidence for Ticked Boxes to Each Type of Leakage between the FISI Assessments on A1 and A3 in Patients without Previous Experience of a Physician-Led Oral Interview Assessment (n = 77).
| Variables included in equation | Unstandardized regression weight |
t value | P value | Variance explained |
|---|---|---|---|---|
| Gas | ||||
| Age, 65 years and more (no, yes) | 0.27 | 2.08 | 0.041 | 5.4% |
| Mucus | ||||
| No bidet use | 0.38 | 3.51 | 0.001 | 14.1% |
| Liquid stool | ||||
| No previous history of pelvic surgery | 0.36 | 2.92 | 0.005 | 10.2% |
| Solid stool | ||||
| Age, 65 years and more (no, yes) | 0.33 | 2.58 | 0.012 | 8.2% |
FISI, Fecal Incontinence Severity Index; A1, Self-administration to the FISI; A3, Physician-led oral interview assessment of the FISI
Discussion
To the best of our knowledge, this is the first to compare patients' self-administered responses to the FISI questionnaire with the responses of patients by physician's oral interview. This study demonstrated that the mean difference between the FISI scores assigned by each patient and those provided during the oral history taking was 8.9. There is no consensus on how many points make the difference clinically significant. However, this figure seems significant as a previous study reported that the minimum important difference value for FISI was 4[6]. Older age was predictive of either the rating gap in the FISI scores (≥9.0) or the in-coincidence of the ticked box for solid stool or gas leakage.
The standard method for measuring FI and its severity is self-report. In most of the previous studies examining patients with FI, patients were asked to complete the self-administered questionnaire[7-9]. Clinicians should evaluate the severity of FI correctly to determine the appropriate treatment. Additionally, when the effectiveness of interventions for the treatment of FI is investigated, the FI severity at baseline should be correctly assessed to determine the effectiveness of interventions. Even if the severity of FI improved significantly after an intervention compared with that at baseline, the assessment results of the treatment efficacy could be misleading, if the FI severity was not accurately assessed at baseline.
The results of this study suggested that there is some non-negligible discrepancy between patients' self-administered responses and their responses from physician's oral interview, especially in older patients. This allows for continuous interviews with the physician until accurate results are obtained. A practical manual on the utilization of self-administered questionnaires in clinical practice elucidates that elderly patients might encounter challenges or may find it infeasible to independently fill out the questionnaires. In such cases, the questionnaire can be completed with the assistance of family members or medical staff[10]. In line with the authors' view[10], patients typically appreciate the active engagement of health professionals in addressing critical issues such as the symptoms of FI, which are not comprehensively explored using a self-report questionnaire. On the other hand, if physicians are conducting research using the FISI questionnaire, there is a concern that bias among physicians may occur, which affects the uniformity of the results when the questionnaire is scored by physicians after an oral interview.
We anticipated that the FISI scores obtained using a self-administered questionnaire should be significantly different from those obtained by a physician-led oral interview assessment. Additionally, we predicted that the scores obtained during oral interview assessment should be close to the scores obtained using a modified FISI self-administered questionnaire. This expectation was based on the assumption that a questionnaire with an explanatory text may facilitate patients' comprehension of their incontinence status. However, our predictions were proven incorrect. These results suggest that it is desirable to create a Japanese version of the FISI which is based on the validation study. When the scores for each FISI component were compared with those obtained in all three assessments, the scores for solid stool leakage obtained based on oral interview assessment were significantly smaller than those obtained using either the baseline self-administered FISI questionnaire or the modified self-administered FISI questionnaire. The patients possibly misunderstood the questions on the baseline FISI or modified FISI questionnaire, causing them to provide affirmative written responses. However, during direct physician interviews, they demonstrated a better understanding of the questions and did not report frequent solid stool leakage. The scores for gas leakage obtained based on oral interview assessment were significantly smaller than those obtained using the modified self-administered FISI questionnaire with a written explanation. This may be partly due to the fact that patients' tended to misunderstand the phrase “break wind unexpectedly” for “feel free and relaxed about breaking wind at home”.
There was no significant difference between Group 1 (51%) and Group 2 (49%) in the in-coincidence rates of the ticked box for all types of leakage between the assessments on A1 and A3, which suggests that the previous experience of a physician-led oral interview assessment did not have a significant influence on FISI scores. Meanwhile, when the characteristics independently associated with the presence of in-coincidence for ticked boxes to each type of leakage between the FISI assessments on A1 and A3 were selected, no history of pelvic surgery was predictive of either a rating gap in the FISI scores or the in-coincidence of the ticked box for liquid stool leakage in this study. These findings could be attributed to the fact that 23 of 44 patients (52%) with a history of pelvic surgery had previously undergone an oral interview assessment of the FISI and were accustomed to this assessment process. By contrast, the FISI assessment was conducted for the first time in the remaining 77 patients.
No bidet use was predictive of the in-coincidence of ticked boxes related to mucus leakage. Mucus leakage is one of the characteristic symptoms of bidet users[11]. Naturally, they might focus on the symptom frequency and independently assess their condition, potentially leading to a higher likelihood of checking the boxes related to mucus leakage properly.
This study had certain limitations. First, the patients possibly gained a better understanding of their incontinence condition over time. As they were administered with both the FISI and modified FISI questionnaires and subsequently interviewed by a physician, they may have developed a more accurate response pattern. Second, the extent of cognitive impairment in the patients was not assessed; consequently, the effect of cognitive function on the results remained unknown. Third, 23 patients with a previous history of pelvic surgery had not filled out the baseline or modified FISI self-administered questionnaire but underwent oral history assessment of the FISI prior to this study. This prior experience may introduce bias into the study's results. Fourth, the explanation of “Break wind unexpectedly” for modified FISI might have caused a misunderstanding of “gas incontinence” to patients, because it sometimes could be expected by them before it happens. Fifth, the FI data recalled from a specific period were not accurate. Although the patient is the best source of data on FI severity[4], such data can be manipulated by the patient or it may not be an accurate representation of the patient's actual status. Conversely, the oral interview assessment gathered by the physician may not closely reflect the patient's actual FI status. Further studies are required comparing FI severity on daily stool diaries with recall data.
In conclusion, there was no significant difference in the FISI scores between self-administered responses on the original FISI questionnaire and the responses of patients by physician's oral interview. Patients totaling to 37% showed a rating gap in the FISI score. Older age was predictive of either the rating gap or the in-coincidence of ticked boxes related to solid stool or gas leakage based on the self-administered FISI score and FISI score obtained through oral interview assessment. This finding suggests that there is some non-negligible discrepancy between patients' self-administered responses and their responses from physician's oral interview, especially in older patients.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
Akira Tsunoda: acquisition of data, analysis and interpretation of data; drafting the article; and final approval of the version to be published.
Hiroshi Kusanagi: acquisition of data, analysis and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published.
Approval by Institutional Review Board (IRB)
Institutional review board: Ethical Committee of Kameda Medical Center
Review board approval number: 22-048
References
- 1.Bliss DZ, Fischer LR, Savik K, et al. Severity of fecal incontinence in community-living elderly in a health maintenance organization. Res Nurs Health. 2004 Jun; 27(3): 162-73. [DOI] [PubMed] [Google Scholar]
- 2.Nakanishi N, Tatara K, Naramura H, et al. Urinary and fecal incontinence in a community-residing older population in Japan. J Am Geriatr Soc. 1997 Feb; 45(2): 215-9. [DOI] [PubMed] [Google Scholar]
- 3.Rockwood TH, Church JM, Fleshman JW, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum. 1999 Dec; 42(12): 1525-32. [DOI] [PubMed] [Google Scholar]
- 4.Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993 Jan; 36(1): 77-97. [DOI] [PubMed] [Google Scholar]
- 5.Vaizey CJ, Carapeti E, Cahill JA, et al. Prospective comparison of faecal incontinence grading systems. Gut. 1999 Jan; 44(1): 77-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jelovsek JE, Chen Z, Markland AD, et al. Minimum important differences for scales assessing symptom severity and quality of life in patients with fecal incontinence. Female Pelvic Med Reconstr Surg. 2014 Nov-Dec; 20(6): 342-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hosmer AE, Saini SD, Menees SB. Prevalence and Severity of Fecal Incontinence in Veterans. J Neurogastroenterol Motil. 2019 Oct; 25(4): 576-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olopade FA, Norman A, Blake P, et al. A modified Inflammatory Bowel Disease questionnaire and the Vaizey Incontinence questionnaire are simple ways to identify patients with significant gastrointestinal symptoms after pelvic radiotherapy. Br J Cancer. 2005 May; 92(9): 1663-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuismanen K, Nieminen K, Karjalainen K, et al. Outcomes of primary anal sphincter repair after obstetric injury and evaluation of a novel three-choice assessment. Tech Coloproctol. 2018 Mar; 22(3): 209-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolfe F, Pincus T. Listening to the patient: a practical guide to self-report questionnaires in clinical care. Arthritis Rheum. 1999 Sep; 42(9): 1797-808. [DOI] [PubMed] [Google Scholar]
- 11.Tsunoda A, Kusanagi H. A Retrospective Investigation on Electric Bidet Use as a Possible Cause of Anal Incontinence. J Anus Rectum Colon. 2021 Jul; 5(3): 268-73. [DOI] [PMC free article] [PubMed] [Google Scholar]


