Abstract
Aims
Reducing sodium intake is necessary for patients with chronic heart failure (CHF). Salt substitutes (saltSubs) have become increasingly popular as recommendations by healthcare professionals (HCPs) as well as options for patients and their caregivers. However, their consumption is generally potassium based and remains poorly evaluated in CHF management. Their impact on guideline‐directed medical therapies (GDMTs) also remains unknown. The primary objective of this study was to provide a description and estimate of HCP recommendations and reported use of saltSubs in France. Secondary objectives were to identify if there was an association between these recommendations by HCPs and the use of GDMTs.
Methods and results
A nationwide, questionnaire‐based, cross‐sectional, epidemiological study was conducted from September 2020 to July 2021. Data collection included baseline characteristics, the use and recommendations of saltSubs, and the use of GDMTs, which included (i) angiotensin‐converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs) or angiotensin receptor–neprilysin inhibitors (ARNis), (ii) mineralocorticoid receptor antagonists (MRAs), and/or (iii) beta‐blockers (BBs). In total, 13% of HCPs advised saltSubs and 17% of patients and 22% of caregivers reported their consumption. CHF patients advised to take saltSubs did not differ in terms of left ventricular ejection fraction (EF) <40%, ischaemic origin, and New York Heart Association III–IV class, but were more recently hospitalized for acute HF (P = 0.004). HCPs who recommended saltSubs to patients were more likely to advise an anti‐diabetic diet (P < 0.001), cholesterol‐lowering diet (P < 0.001), and exercise (P = 0.018). In the overall population, ACEi/ARB/ARNi use was less frequent in case of saltSub recommendations (74% vs. 82%, P = 0.012). The concomitant prescription of none, one, two, or three GDMTs was less favourable in case of saltSub recommendations (P = 0.046). There was no significant difference for the presence of MRA (56% vs. 58%) and/or BB (78% vs. 82%). The under‐prescription of ACEi/ARB/ARNi was found when patients had EF < 40% (P = 0.029) and/or EF ≥ 40% (P = 0.043). In the subgroup with left ventricular EF ≥ 40%, we found a higher thiazide use (P = 0.014) and a less frequent use of low EF GDMTs (P = 0.044) in case of being recommended saltSubs.
Conclusions
Beyond the well‐established risk for hyperkalaemia, our preliminary results suggest a potentially negative impact of saltSubs on GDMT use, especially for ACEis/ARBs/ARNis in CHF management. saltSub recommendations and their availability from open sale outlets should be considered to avoid possible misuse or deference from GDMTs in the future. Informed advice to consumers should also be considered from HCPs or pharmacists.
Keywords: Salt substitutes, Sodium intake, Heart failure, Guideline‐directed medical therapy
Introduction
Chronic heart failure (CHF) is a cardiac syndrome that carries a major burden on healthcare systems. 1 According to the 2021 European Society of Cardiology guidelines, sodium intake of 6 g/day is recommended for CHF patients. 2 Concurrently, the food industry offers a wide range of salt substitutes (saltSubs) to reduce sodium consumption, which are generally potassium based. 3 , 4 The potential risk of hyperkalaemia, death, and underuse of guideline‐directed medical therapies (GDMTs) are also concerns for CHF patients consuming saltSubs. 5 Literature on their use exists in populations with hypertension, high‐sodium consumption, poor access to care, and low hyperkalaemia risk. 6 , 7 , 8 However, studies on the risk–benefit balance of saltSubs and on populations in Europe and North America are limited. 9 , 10 The primary objectives of this study were to describe and estimate healthcare professional (HCP) recommendations and the preliminary reported use of saltSubs by patients in France. Secondary objectives were to assess whether these recommendations by HCPs influence the use of GDMTs.
Methods
A nationwide, questionnaire‐based, cross‐sectional, epidemiological study was conducted by the Heart Failure and Cardiomyopathy Group (GICC) within the French Society of Cardiology (SFC) from September 2020 to July 2021. This research was encouraged by the SFC with the support of cardiology professional groups and heart failure (HF) patient associations. Three different questionnaires were sent to be completed by HCPs, patients, and caregivers across more than 100 centres. Patients were recruited from specialized consultations or from already known local cohorts (remote monitoring or rehabilitation programmes).
The questionnaires were validated by the SFC and are available upon request or via the website http://www.sfcardio.fr/. The HCP questionnaire consisted of 11 questions with seven multiple choice questions (MCQs), three binary (and two optional for pharmacists or nurses), and one 10‐point Likert scale (Supporting Information, Table S1 ). Items covered HF type according to the ejection fraction (EF) and characteristics, provided GDMTs and other treatments, and saltSub recommendations.
The caregiver questionnaire was composed of 11 items with question types varying from binary, 4‐point, 5‐point, and 10‐point Likert scale, free‐form, and MCQs (Supporting Information, Table S2 ). The items covered a variety of subjects including the caregivers: (i) personal situation, (ii) professional and social situation, (iii) professional activities regarding HF, (iv) evaluation of the care pathway since the patients' diagnosis, (v) patients' symptoms and experience of care, (vi) evaluation regarding treatments, (vii) support given to patients, (viii) psychological impact, daily life and on health, and (ix) training and information (Supporting Information, Table S2 ). In the patient's questionnaire, participants had 12 sections to complete and included items such as recommendations given by their HCPs, monitoring of a low‐sodium diet, and saltSub consumption.
Data collection included baseline characteristics, the use and recommendations of saltSubs, and the use of GDMTs involving: (i) angiotensin‐converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs) or angiotensin receptor–neprilysin inhibitors (ARNis), (ii) mineralocorticoid receptor antagonists (MRAs), and/or (iii) beta‐blockers (BBs).
Continuous variables were described by median [Q1–Q3]. Interferential analysis was performed using the χ 2 test for related items; otherwise, Fisher's exact test was used. Categorical variables were described by numbers and percentages (%). The comparison of these variables was tested using Student's t‐test if they were considered normal and if homoscedasticity was respected; otherwise, the Kruskal–Wallis test was applied. The risk significance was set at 0.05. Statistical analysis was performed using SAS Version 9.4 (SAS Institute, NC, USA).
Results
In total, 1398 HCPs, 1049 patients, and 594 caregivers were included. Most HCPs were cardiologists (71%) followed by nurses (23%) and other (6%) (Table 1 ). Patients were mostly male (70%), with a median age of 70 [59–77] years. The main comorbidities declared were diabetes (32%), renal disease (24%), and pulmonary disease (25%). Caregivers were mostly female (78%), with a median age of 66 [55–74] years, and were mostly spouses (80%) or family members (20%).
Table 1.
Baseline characteristics
| Characteristics | |
|---|---|
| Healthcare professionals, n (%) | |
| Cardiologist | 992 (71) |
| Nurse | 321 (23) |
| Other | 85 (6) |
| Patients, n (%) | |
| Male | 734 (70) |
| Female | 315 (30) |
| Median age (years) [Q1–Q3] | 70 [59–77] |
| Comorbidities, n (%) | |
| Diabetes | 336 (32) |
| Renal disease | 252 (24) |
| Pulmonary disease | 262 (25) |
| Caregivers, n (%) | |
| Male | 130 (22) |
| Female | 464 (78) |
| Median age (years) [Q1–Q3] | 66 [55–74] |
| Relation to patient | |
| Spouse | 475 (80) |
| Family member | 118 (20) |
Recommendations and the use of saltSubs were reported by 13% of HCPs (n = 1288), 17% of patients (n = 932), and 22% of caregivers (n = 512). Sixteen per cent of patients and 21% of caregivers reported using saltSubs without being recommended by an HCP. Patients with CHF who were advised to consider taking saltSubs did not differ in terms of left ventricular EF (LVEF) <40% (57%), ischaemic origin (41%), or New York Heart Association (NYHA) III–IV class (36%) and were more recently hospitalized for acute HF (P = 0.004).
HCPs who recommended saltSubs to their patients were more likely to advise an anti‐diabetic diet (57% vs. 34%, P < 0.001), cholesterol‐lowering diet (63% vs. 42%, P < 0.001), vitamin K‐lowering diet (37% vs. 13%, P < 0.001), and physical activity (86% vs. 77%, P = 0.018) without a difference in terms of sodium consumption recommendations (91% vs. 89%) nor the need for an educational programme (61% vs. 57%). ACEis/ARBs/ARNis were less frequently recommended in case of saltSub recommendations (74% vs. 82%, P = 0.012). Thiazide use was more frequent (11% vs. 6%, P = 0.04) and had a similar trend for loop diuretics (80% vs. 73%, P = 0.078).
We did not find a significant difference for BBs (78% vs. 82%) nor MRAs (56% vs. 58%). The concomitant prescription of none, 1, 2, or 3 of three GDMTs was less favourable in case of saltSub recommendations (Figure 1 and Table 2 ).
Figure 1.
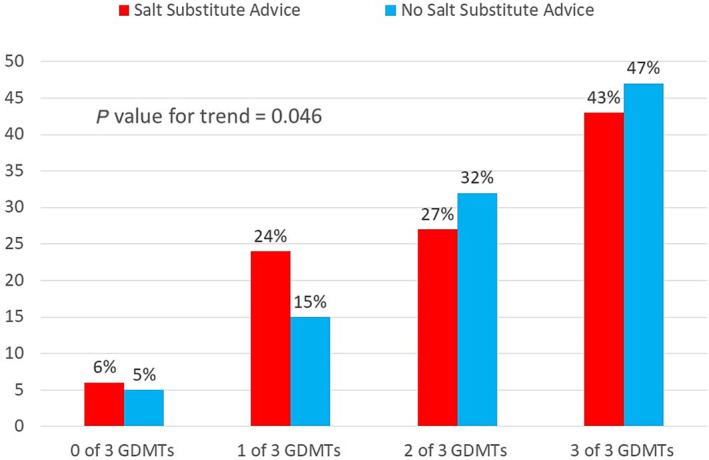
Prescription rate of guideline‐directed medical therapies (GDMTs) including (i) angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers or angiotensin receptor–neprilysin inhibitors, (ii) mineralocorticoid receptor antagonists, and/or (iii) beta‐blockers, according to whether salt substitute recommendations were provided by healthcare professionals in France.
Table 2.
Prescription rate of GDMTs according to whether saltSub recommendations were provided by HCPs in France
| Number of prescriptions, n (%) | |||
|---|---|---|---|
| saltSub recommended by HCPs, n = 157 | saltSub not recommended by HCPs, n = 1105 | HCPs overall, n = 1262 | |
| No GDMTs a | 10 (6) | 58 (5) | 68 (5) |
| One GDMT | 37 (24) | 168 (15) | 168 (13) |
| Two GDMTs | 42 (27) | 355 (32) | 397 (31) |
| All three GDMTs | 68 (43) | 524 (47) | 592 (47) |
GDMTs, guideline‐directed medical therapies; HCPs, healthcare professionals; saltSub, salt substitute.
GDMTs included (i) angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers or angiotensin receptor–neprilysin inhibitors, (ii) mineralocorticoid receptor antagonists, and/or (iii) beta‐blockers.
The same under‐prescription of ACEis/ARBs/ARNis was found when patients had an EF < 40% (P = 0.029) or EF ≥ 40% (P = 0.043). In the patient population with LVEF ≥ 40%, we found a higher thiazide use (P = 0.014) and a less frequent use of the low EF GDMTs (P = 0.044) when saltSubs were recommended.
Discussion
In this study, we showed that saltSub recommendations were associated with the under‐prescribing of ACEis/ARBs/ARNis for patients with CHF and that this may influence the titration of GDMTs. A higher use of diuretics (mainly thiazides) was also found. Recommendations of saltSubs by HCPs may not relate to the severity of HF in terms of EF or NYHA class; however, they could reflect a poor control of CHF due to the low use of GDMTs by patients. Similar to our findings, a pilot study by Bistola et al. reported that baseline characteristics did not differ among patients using saltSubs vs. regular salt; however, increased exercise capacity was present for those consuming saltSubs. 11
On the other hand, these recommendations could be interpreted as a corrective measure especially due to the higher rate of thiazides being used. As reported by Chang et al. and Greer et al., patients with CHF have most risk factors for hyperkalaemia, which may be amplified by uncontrolled or even unknown doses of saltSub recommended. 12 , 13
Our preliminary findings may indicate that HCPs, patients, and caregivers should be informed of the risks associated with the use and recommendations of potassium‐rich saltSubs, particularly when such substitutes are not considered as drugs and are difficult to observe. Although literature on the risk of hyperkalaemia based on up‐titration of GDMTs and associated doses of ACEis/ARBs/ARNis is well established, optimization of drugs improving outcomes in CHF may have other consequences. 14 Patients consuming saltSubs based on the recommendation of HCPs, caregivers or on their own choice, may indicate that they could be undertreated, since doses would not be maximal and, consequently, there could be a dose‐dependent effect to the maximum tolerated dose.
Regarding limitations, because this study was questionnaire based, it may have incurred sampling and response bias. In France, market authorization for the use of sodium–glucose cotransporter‐2 (SGLT2) inhibitors in HF was not available at the time of conducting the questionnaire (decree of 3 November 2021); therefore, information on SGLT2 inhibitors was not detailed and may be worth exploring in the future. The presence and use of potassium‐binding agents were also not provided.
Conclusions
saltSub recommendations and their availability from open sale outlets to patients with CHF should be considered to avoid any misuse or deference from GDMTs in the future. Informed advice to consumers should also be considered from HCPs or pharmacists. Future studies and randomized clinical trials on salt supplements in HF could be explored.
Conflict of interest
None declared.
Funding
This work was funded by the Heart Failure and Cardiomyopathy Group (GICC) within the French Society of Cardiology; Société Française de Cardiologie (SFC).
Supporting information
Table S1. Healthcare professional questionnaire.
Table S2. Caregiver questionnaire.
Acknowledgements
The authors would like to thank the Collège National des Cardiologues Français, the Fédération Française de Cardiologie, and the Collège Nationale des Cardiologues Hospitaliers, as well as the general practitioners (SFMG), pharmacists of Ile de France (URPS), and the heart failure patient associations for their voluntary and essential contribution to this study. The authors would also like to thank Marty Brucato and Sarina Yaghobian from AcaciaTools for their reviewing and proofreading services.
Tartière, J.‐M. , Roubille, F. , Salvat, M. , Damy, T. , Beauvais, F. , Berthelot, E. , Lamblin, N. , and Kesri‐Tartière, L. (2024) Salt substitute recommendations for heart failure patients may influence guideline‐directed medical therapies titration. ESC Heart Failure, 11: 2455–2459. 10.1002/ehf2.14706.
References
- 1. Patel Y, Joseph J. Sodium intake and heart failure. Int J Mol Sci 2020;21:9474. doi: 10.3390/ijms21249474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2022;24:4‐131. doi: 10.1002/ejhf.2333 [DOI] [PubMed] [Google Scholar]
- 3. McLean R. Low sodium salt substitutes: A tool for sodium reduction and cardiovascular health. Cochrane Database Syst Rev 2022;2022:ED000158. doi: 10.1002/14651858.ED000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kong B, Yang S, Long J, Tang Y, Liu Y, Ge Z, et al. National initiatives on salt substitutes: Scoping review. JMIR Public Health Surveill 2023;9:e45266. doi: 10.2196/45266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Te Dorsthorst RPM, Hendrikse J, Vervoorn MT, van Weperen VYH, van der Heyden MAG. Review of case reports on hyperkalemia induced by dietary intake: Not restricted to chronic kidney disease patients. Eur J Clin Nutr 2019;73:38‐45. doi: 10.1038/s41430-018-0154-6 [DOI] [PubMed] [Google Scholar]
- 6. Tsai Y‐C, Tsao Y‐P, Huang C‐J, Tai Y‐H, Su Y‐C, Chiang C‐E, et al. Effectiveness of salt substitute on cardiovascular outcomes: A systematic review and meta‐analysis. J Clin Hypertens Greenwich Conn 2022;24:1147‐1160. doi: 10.1111/jch.14562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brand A, Visser ME, Schoonees A, Naude CE. Replacing salt with low‐sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev 2022;8:CD015207. doi: 10.1002/14651858.CD015207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farrand C, MacGregor G, Campbell NRC, Webster J. Potential use of salt substitutes to reduce blood pressure. J Clin Hypertens 2019;21:350‐354. doi: 10.1111/jch.13482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marklund M, Tullu F, Raj Thout S, Yu J, Brady TM, Appel LJ, et al. Estimated benefits and risks of using a reduced‐sodium, potassium‐enriched salt substitute in India: A modeling study. Hypertens Dallas Tex 1979;2022:2188‐2198. doi: 10.1161/HYPERTENSIONAHA.122.19072 [DOI] [PubMed] [Google Scholar]
- 10. Marklund M, Singh G, Greer R, Cudhea F, Matsushita K, Micha R, et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: Modelling study. BMJ 2020;369:m824. doi: 10.1136/bmj.m824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bistola V, Arfaras‐Melainis A, Trogkanis E, Bakosis G, Polyzogopoulou E, Karavidas I‐N, et al. Safety and efficacy of salt substitution with a low sodium‐potassium enriched dietary salt in patients with heart failure with reduced ejection fraction: A pilot study. Clin Nutr ESPEN 2020;35:90‐94. doi: 10.1016/j.clnesp.2019.11.004 [DOI] [PubMed] [Google Scholar]
- 12. Chang AR, Sang Y, Leddy J, Yahya T, Kirchner HL, Inker LA, et al. Antihypertensive medications and the prevalence of hyperkalemia in a large health system. Hypertens Dallas Tex 1979;2016:1181‐1188. doi: 10.1161/HYPERTENSIONAHA.116.07363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Greer RC, Marklund M, Anderson CAM, Cobb LK, Dalcin AT, Henry M, et al. Potassium‐enriched salt substitutes as a means to lower blood pressure: Benefits and risks. Hypertens Dallas Tex 1979;2020:266‐274. doi: 10.1161/HYPERTENSIONAHA.119.13241 [DOI] [PubMed] [Google Scholar]
- 14. Henrysson J, Thunström E, Chen X, Fu M, Basic C. Hyperkalaemia as a cause of undertreatment with mineralocorticoid receptor antagonists in heart failure. ESC Heart Fail 2023;10:66‐79. doi: 10.1002/ehf2.14137 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Healthcare professional questionnaire.
Table S2. Caregiver questionnaire.


