Abstract
Aims
The objective of this study was to perform a cost–benefit analysis of the CardioMEMS HF System (Abbott Laboratories, Abbott Park, IL, USA) in a heart failure (HF) clinic in Spain by evaluating the real‐time remote monitoring of pulmonary artery pressures, which has been shown to reduce HF‐related hospitalizations and improve the quality of life for selected HF patients. Particularly, the study aimed to determine the value of CardioMEMS in Southern Europe, where healthcare costs are significantly lower and its effectiveness remains uncertain.
Methods and results
This single‐centre study enrolled all consecutive HF patients (N = 43) who had been implanted with a pulmonary artery pressure sensor (CardioMEMS HF System); 48.8% were females, aged 75.5 ± 7.0 years, with both reduced and preserved left ventricular ejection fraction; 67.4% of them were in New York Heart Association Class III. The number of HF hospitalizations in the year before and the year after the sensor implantation was compared. Quality‐adjusted life years gained based on a literature review of previous studies were calculated. The rate of HF hospitalizations was significantly lower at 1 year compared with the year before CardioMEMS implantation (0.25 vs. 1.10 events/patient‐year, hazard ratio 0.22, P = 0.001). At the end of the first year, the usual management outperformed the CardioMEMS HF System. By the end of the second year, the CardioMEMS system is estimated to reduce costs compared with usual management (net benefits of €346).
Conclusions
Based on the results, we suggest that remote monitoring of pulmonary artery pressure with the CardioMEMS HF System represents a midterm and long‐term efficient strategy in a healthcare setting in Southern Europe.
Keywords: Heart failure, Hospitalizations, Monitoring, Pulmonary pressure sensor, Cost–benefit
Introduction
Heart failure (HF) is a major public health problem and a leading cause of hospitalization in Western countries. The prevalence of HF is ~2% in the adult population in Spain, rising to ≥10% among people >80 years of age. 1 The most common cause of hospitalization in HF patients is HF decompensation, which leads to a progressive deterioration of myocardial function and quality of life and also represents the most important determinant of HF‐associated costs in our country. 2
Despite improvements in HF therapy, the 12 month hospitalization rates remain very high in this population, ranging from 32% to 44% for ambulatory and hospitalized patients, respectively. 3
Remote monitoring emerged as a viable way to overcome the long interval between office visits and to keep patients safe by identifying disease progression in time to prevent hospitalization. 4 The CardioMEMS HF System (Abbott Laboratories, Abbott Park, IL, USA) is the first system to provide real‐time remote monitoring of pulmonary artery pressures (PAPs), with the goal of maintaining this pressure within a therapeutic range by adjusting medications in response to pressure trends. Unlike other implantable devices, the CardioMEMS pressure sensor does not require a battery and therefore continues to function indefinitely.
In a randomized controlled trial of 550 New York Heart Association (NYHA) Class III HF patients with a previous HF hospitalization, those whose treatment was guided by PAP measurements (treatment group) achieved a 33% reduction in HF‐related hospitalizations over an average study duration of 15 months compared with the control arm, who had the device implanted but in whom the data were not used to guide management. The treatment group also had a higher reduction in mean PAP and a greater improvement in quality of life. 5
In 2014, CardioMEMS was approved for use in the United States by the Food and Drug Administration, and in 2016, the Heart Failure Association of the European Society of Cardiology (ESC) included the system in the ESC guidelines for the diagnosis and treatment of acute and chronic HF, indicating that the device may be considered for monitoring symptomatic patients with a previous HF hospitalization in order to reduce the risk of recurrent hospitalization (Class IIb recommendation, Level of Evidence B). 6
A randomized controlled trial conducted in the Netherlands has recently confirmed that haemodynamic monitoring of pulmonary pressures improves quality of life and reduces HF hospitalizations, and a previous cost–utility analysis suggested that the CardioMEMS HF System is also a cost‐effective strategy for HF patients in the United Kingdom. 7 , 8
Southern European countries, such as Spain, Italy, and Greece, maintain healthcare systems predominantly funded by public means, aiming to achieve universal coverage. However, limited resources sometimes slow the uptake of innovative technologies like the CardioMEMS HF System. Economic challenges in this region have historically shaped healthcare budgets, which can, in turn, influence decisions regarding the adoption of advanced medical technologies. The unique cultural characteristics of Southern Europe play a significant role in how patients adhere to treatments. This cultural aspect becomes especially relevant when considering remote monitoring technologies, as the engagement of both patients and their families can directly influence outcomes. Given the economic considerations and the focus on cost‐effectiveness, there has been a cautious approach in Southern Europe towards integrating newer, pricier medical technologies. In light of this context, our study explores the potential of the CardioMEMS HF System to address these challenges and offer an effective solution for HF management in this distinct setting.
Methods
Study population and follow‐up
The study was carried out in an HF clinic of a tertiary hospital in the northern area of Barcelona. This hospital was a pioneer in the use of pulmonary pressure sensors in Southern Europe and currently follows the largest number of patients with the CardioMEMS device implanted in the country.
All consecutive patients implanted with a CardioMEMS from June 2019 to November 2021 were included in the analysis.
The criteria for implementing the CardioMEMS HF System were the presence of symptomatic HF with a high risk of HF hospitalization, regardless of the ejection fraction, in patients already receiving optimal medical treatment. Forty‐three patients meeting the criteria for implementing the CardioMEMS HF System were selected for the procedure.
Because patients initiated follow‐up at the HF clinic, they were followed in regular follow‐up visits, including a minimum of one visit with a nurse every 3 months and one visit with a physician (cardiologist or internist) every 6 months.
During the right heart catheterization at the time of implantation, we measured the pulmonary capillary wedge pressure (PCWP) and right atrial pressure (RAP) to identify the main causes of elevated PAPs. Based on these measurements, we adjusted diuretics when PAP suggested an overload of intravascular volume and recommended vasodilator adjustments in the presence of pronounced vascular resistance.
We also considered potential variances between PCWP and pulmonary artery diastolic (PAD) pressures. While these typically correlate closely, occasional discrepancies can occur. Such differences are crucial when determining PAP threshold ranges for clinical management.
Subsequently, our treatment decisions were centred on PAD pressures. We took action, either increasing or decreasing diuretic therapy, if a change of 3–5 mmHg in PAP was observed over 2–3 days, especially when these values were outside the optimal range.
During the baseline visit, patients provided written consent for the use of their clinical data for research purposes. Demographic, clinical, echocardiographic, and analytical data were recorded in a specific database (Ethical Committee Number PI‐18‐037).
To conduct the cost–benefit analysis, annualized HF hospitalizations in the year before and the year after sensor implantation were taken into account, considering time at risk for each patient. Additional calculations were made in order to assess the accumulated costs over 5 years; for those calculations, a 3% discount rate was considered as per the recommendations for health economics in the Spanish healthcare system. 9
The study was performed in compliance with the laws that protect personal data, in accordance with the international guidelines on clinical investigations from the World Medical Association's Declaration of Helsinki.
Resources and costs
The costs assessed in the study were chosen based on the description of costs from previous studies. To do so, a literature review of CardioMEMS cost‐effectiveness analysis (ranging from 2011 to 2021) was conducted. Out of the 11 results yielded, only six were actual economic evaluations, and only five of them were conducted in the Global North. As shown in Supporting Information, Table S1 , four of the five research papers found were conducted in the United States and one in different countries of the European Union (the United Kingdom, the Netherlands, Belgium, Italy, and Germany). The mean and median incremental cost‐effectiveness ratio (ICER), converting currency and adjusting for inflation, were of €37 536 and €26 398, respectively; as for the quality‐adjusted life years (QALYs) gained after the implant of the CardioMEMS device, the mean and median values were 0.43 and 0.40, respectively. 5 , 8 , 10 , 11 , 12
The perspective of the evaluation was conducted from the hospital centre in order to estimate the costs and impact of the CardioMEMS treatment in comparison with standard treatment. For the benefits, we valuate a QALY monetarily through willingness to pay. 13 As we consider the valuation the patient would make under the public healthcare system, this is a stated preferences approach. 14
Table 1 shows a valuation of the costs and resources. The cost of the device and its pillow, including taxes, totalled €12 650. The implant procedure totalled €1528, counting the use and costs derived from the haemodynamic room (including the salary of the interventional cardiologist), according to public prices. 15 Outpatient costs, including monitoring, regular visits, and possible hospitalizations, were taken into account. Monitoring costs were accounted for as a nurse's 30 min salary, which is the daily time a nurse needs to consult the pulmonary pressures of CardioMEMS patients (this process is repeated 5 days a week). Such cost is accounted as €63 per patient per year, given the fact that all patients are covered under that time.
Table 1.
Cost and resources description
| Parameter | Cost | Source(s) |
|---|---|---|
| CardioMEMS HF device (each) | €11 440 | Own |
| Pillow (each) | €1 210 | Own |
| Implant procedure | €1 528 | 15 |
| Computed tomography of the chest | €110 | 15 |
| Thoracic computed tomography angiography | €235 | 15 |
| Outpatient costs | ||
| Monitoring by the nurse (30 min. daily, 5 days a week) | €16.31 | 16 |
| Regular visits with the nurse (every 4 months) | €80 | 16 |
| Regular visits with the cardiologist (every 6 months) | €80 | 16 |
| Hospitalization (per day) | €674 | 15 |
Regular visits were appointed with both the HF cardiologist (every 6 months) and the nurse (every 3 months). Both regular appointments were accounted for as an outpatient visit under public prices at €80 per visit. 16
The hospitalization per day price is an average of €674. No hospital admission costs were accounted for CardioMEMS implantation as patients were discharged on the same day of implantation. Complication costs were estimated taking into account the additional resources required in the sampled cases. These resources include a chest computed tomography scan (€110), a thoracic computed tomography angiography (€235), and the additional hospitalization days. 15
We valuated the QALY at €25 000. 17 , 18 An effectiveness of 0.3 QALYs was taken as reference as according to the CHAMPION trial. 5
The costs, resources, and benefits of the study and its evaluation were valued in euros (€) as of 2022. The currencies were converted to 2022 euros per the price dates in each study. The reporting of this study follows the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) framework for economic evaluations. 19
Statistical analysis
Categorical variables are expressed as absolute numbers and percentages. Continuous variables are expressed as the mean ± standard deviation for normal distributions, or the median and inter‐quartile range (IQR), for non‐normal distribution. Normal distributions were assessed with normal quantile–quantile plots. Comparisons between groups were performed with paired t‐test for continuous variables.
To compute the HF hospitalization rate for pre‐ and post‐sensor implantation, the risk exposure time (total follow‐up time until death minus days of hospitalization) for each patient was taken into account. For the cost analysis, both the number of hospital admissions and the length of stay were taken into account.
Results
From September 2019 to November 2021, 43 patients from the same HF clinic had a CardioMEMS device implanted, with a balanced representation of both male and female participants, aged 75.5 ± 7.0 years, with both reduced and preserved left ventricular ejection fraction (LVEF) (mean LVEF 49 ± 14%); 67.4% of them were in NYHA Class III and 32.6% in NYHA Class II. Mean creatinine was 1.37 ± 0.49 mg/dL, and median baseline N‐terminal pro‐B‐type natriuretic peptide (NT‐proBNP) was 1919 (IQR 1014–3339) pg/mL.
A total of 79.1% had been previously admitted due to HF decompensation at least once during the year before CardioMEMS implantation (53.5% two or more times). Seven patients died during the first year of follow‐up (two of them due to cardiovascular causes and none of them due to HF); mean follow‐up for those patients was 208.9 ± 91.3 days. The final patient completed 1 year follow‐up in November 2022.
Baseline demographics, clinical characteristics, and treatments of the included patients are shown in Table 2 .
Table 2.
Baseline demographic and clinical characteristics
|
CardioMEMS patients (n = 43) |
|
|---|---|
| Age (years) | 75.5 ± 7.0 |
| Male | 22 (51.2) |
| BMI (kg/m2) | 29.0 ± 5.4 |
| LVEF (%) | 48.7 ± 13.8 |
| NYHA class | |
| II | 14 (32.6) |
| III | 29 (67.4) |
| Ischaemic aetiology | 13 (30.2) |
| Hypertension | 36 (83.7) |
| Dyslipidaemia | 34 (79.0) |
| Diabetes mellitus | 18 (41.9) |
| Atrial fibrillation | 28 (65.1) |
| COPD | 9 (20.9) |
| Anaemia a | 23 (53.5) |
| Serum creatinine (mg/dL) | 1.37 ± 0.49 |
| Baseline HF medication | |
| Loop diuretic | 40 (93.0) |
| ACEI/ARB/ARNI | 30 (69.8) |
| Beta‐blocker | 31 (72.1) |
| SGLT2i | 3 (7.0) |
| Digitalis | 10 (23.3) |
| Hydralazine | 13 (30.2) |
| MRA | 33 (76.7) |
| NT‐proBNP (pg/mL) | 1 919 (1014–3339) |
| ICD | 8 (18.6) |
| CRT | 7 (16.3) |
ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ARNI, angiotensin receptor and neprilysin inhibitor; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CRT, cardiac resynchronization therapy; HF, heart failure; ICD, implantable cardiac defibrillator; IQR, inter‐quartile range; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonist; NT‐proBNP, N‐terminal pro‐B‐type natriuretic peptide; NYHA, New York Heart Association; SGLT2i, sodium–glucose co‐transporter‐2 inhibitor; WHO, World Health Organization.
Data in mean ± SD, median (IQR), or n (%).
According to WHO criteria (<13 g/dL in men and <12 g/dL in women).
The rate of HF hospitalizations was significantly lower at 1 year compared with the year before CardioMEMS implantation [0.25 vs. 1.10 events/patient‐year, hazard ratio (HR) 0.22, P = 0.001], with an absolute reduction of 0.85 events/patient‐year (Figure 1 ).
Figure 1.
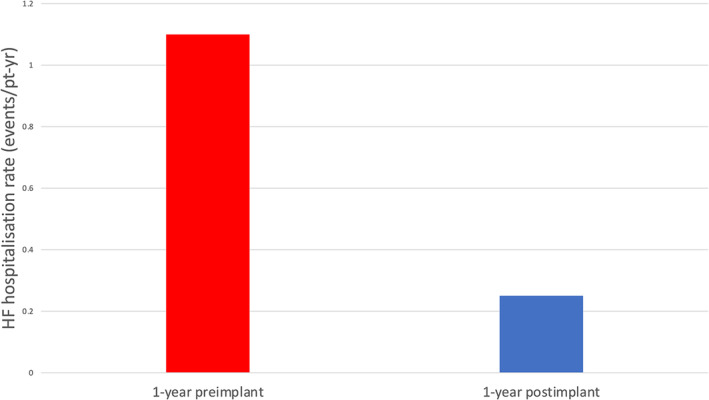
Heart failure (HF) hospitalization rates.
Hospital admissions were considerably longer for the post‐CardioMEMS period (30.5 days) in comparison with the pre‐CardioMEMS period (12.53 days). During the device implementation process, a single complication arose, requiring a chest computed tomography scan, thoracic computed tomography angiography, and an extended 29 day hospitalization. Table 3 shows the comparison between costs and benefits for patients before and after having the CardioMEMS HF System for the first year. For the post‐treatment group, the device and its implant account for the majority of the costs, while in the pre‐treatment group, the hospitalization costs comprised most of the costs. As for the outpatient costs, both groups had regular appointments with nurses and the cardiologist. The benefit–cost ratio was €7500/€20 150 for the post‐treatment group at 1 year.
Table 3.
Cost and benefits for patients before and after CardioMEMS, first year
| Costs and benefits per patient | ||||
|---|---|---|---|---|
| Post‐CM | % | Pre‐CM | % | |
| CardioMEMS | ||||
| Device | €11 440 | 56.8% | €0 | 0% |
| Pillow | €1 210 | 6.0% | €0 | 0% |
| Implant procedure | €1 528 | 7.6% | €0 | 0% |
| Complications | €462 | 2.3% | — | — |
| Total device cost | €14 640 | 72.7% | €0 | 0% |
| Outpatient costs | ||||
| Monitoring | €63 | 0.3% | €0 | 0.00% |
| Nurse | €240 | 1.2% | €240 | 2.5% |
| Cardiologist | €160 | 0.8% | €160 | 1.7% |
| Total outpatient cost | €463 | 2.3% | €400 | 4.1% |
| Hospitalization | €5 047 | 25.0% | €9 248 | 95.9% |
| Total costs | €20 150 | 100.0% | €9 648 | 100.0% |
| Benefits | ||||
| QALYs | €7 500 | — | €0 | — |
| Monetary value | €12 650 | — | €9 648 | — |
CM, CardioMEMS; QALYs, quality‐adjusted life years.
Considering the QALYs gained (applied by the beginning of the first year of the study) as a benefit, a constant cost of hospitalization for all groups, and a 3% discount rate, the initial costs are higher for the post‐CardioMEMS group due to the high costs of the device; however, they are rapidly outgrown by the costs of the pre‐CardioMEMS period, which are mainly driven by higher hospitalization costs, as shown in Figure 2 . By the end of Year 2, the costs of the post‐CardioMEMS and pre‐CardioMEMS groups would be of €18 090 and €18 436 (net benefits of €346 in favour of the post‐CardioMEMS group). By the end of Year 5, the accumulated estimated costs for the post‐CardioMEMS and pre‐CardioMEMS groups would be of €33 956 and €44 066, respectively (net benefits of €10 110 in favour of the post‐CardioMEMS group). Several deterministic sensitivity analyses were performed in order to evaluate how the results could be affected by changes in key assumptions or variables such as QALY benefits (ranging from 0.2 to 0.5), hospitalization costs, and device costs (Supporting Information, Tables S2 and S3 and Figures S1 and S2 ).
Figure 2.
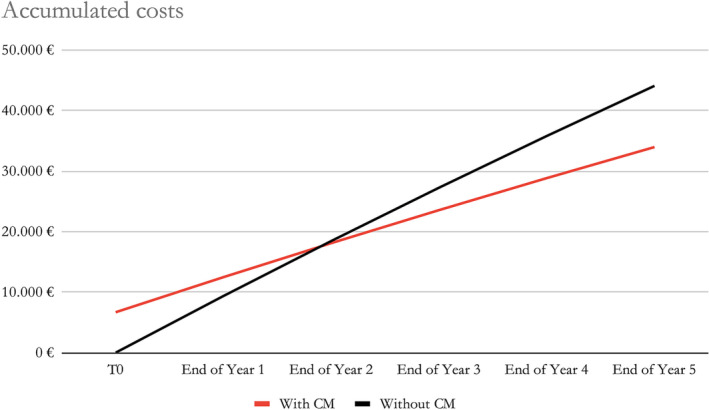
Accumulated estimated costs over 5 years considering the quality‐adjusted life years gained as a benefit, a constant cost of hospitalization for all groups, and a 3% discount rate. CM, CardioMEMS.
Discussion
To our knowledge, this is the first study to perform a cost–benefit analysis of the CardioMEMS system in an HF clinic from Southern Europe. Remote monitoring of PAP with CardioMEMS was associated with a strong reduction in HF hospitalizations at 1 year.
In the context of existing literature, our study presents distinct insights. Unlike prior randomized trials, our cohort came directly from an HF unit and was not confined to a randomized study structure. This approach aligns more with real‐world post‐commercialization studies. Notably, we broadened our patient criteria to include individuals without prior HF admissions but with elevated NT‐proBNP and those classified under NYHA Class II, a strategy similar to the GUIDE‐HF trial approach.
Regarding the evaluation of quality of life benefits, our benchmark was the CHAMPION trial. The absence of blinding in the MONITOR‐HF trial might pose challenges in the clear interpretation of quality of life differentials.
When viewed against studies from other regions of Europe, our findings reveal considerable contrasts, especially in the domain of healthcare economics and the unique cultural attributes of the Southern European demographic. These cultural characteristics can significantly impact patient adherence patterns, which, in turn, can shape outcomes.
Hospitalization costs in Spain are lower in relation to the United Kingdom and the United States. Therefore, one could think that the potential savings by avoiding HF admissions with remote PAP monitoring are also lower. This belief currently leads to an underutilization of this invasive remote monitoring strategy in Southern Europe in comparison with other countries.
In this study, considering the QALYs gained as a benefit, a constant cost of hospitalization for all groups, and a 3% discount rate, the initial costs are higher for the post‐CardioMEMS group due to the high costs of the device; however, they are rapidly outgrown by the costs of the pre‐CardioMEMS period, which are mainly driven by higher hospitalization costs (Figure 2 ). First‐year benefits cover up to 37% of the initial device cost, with further savings in hospitalization costs in subsequent years.
Hospital admissions for the post‐CardioMEMS period were considerably longer than those of the pre‐CardioMEMS group. A possible explanation is that patients who are admitted despite haemodynamic‐guided treatment are more complex and require longer admissions.
The fact that the CardioMEMS system requires no batteries or replacements, along with patients having a lifespan exceeding 2 years, makes invasive remote monitoring a midterm and long‐term cost‐effective strategy.
Table 4 shows the cost structure along with that of the six other studies conducted since the CHAMPION trial. The actual cost shown in this article is similar to the studies by Schmier et al. and Cowie et al., both published after 2017 and all very similar in their cost structure: device, implantation, complications, monitoring, usual cost of HF treatment, and possible hospitalizations. This work has considered all these costs and introduced costs related to regular visits with the nurse and HF cardiologist. Regarding the valuation of costs, ours were most similar to those described in Cowie et al., probably due to a similar context in terms of healthcare.
Table 4.
Cost structure of the studies found in the literature
| Abraham et al. 5 | Sandhu et al. 10 | Martinson et al. 11 | Schmier et al. 12 | Cowie et al. 8 | Present study |
|---|---|---|---|---|---|
| Device | Device | Refers to a market analysis and only presents accumulated costs, not disaggregated | Device | Device | Device |
| Implant | Implant | Implant | Implant | ||
| Complications | Complications | Complications | |||
| Monitoring (nurse wages) | Monitoring (nurse wages) | Monitoring (nurse wages) | Monitoring (nurse wages) | ||
| Regular visits | |||||
| Usual care for HF patients | Usual care for HF patients | Usual care for HF patients | |||
| Hospitalization | Hospitalization | Hospitalization | Hospitalization | Hospitalization | |
| Drugs | |||||
| End‐of‐life support |
The CHAMPION trial found that the CardioMEMS implant had a benefit of 0.3 QALYs for the patient; we used it as an effectiveness benchmark for our study. However, it could be considered a low‐range benefit compared with the mean and median of other published articles, at a benefit of 0.42 and 0.39 QALYs, respectively (Supporting Information, Table S1 ). This could mean that the actual benefit is higher than what we have considered, making the benefit–cost ratio higher.
Study limitations
These results should be interpreted in the context of several potential limitations. First, despite having more implants than any other healthcare centre in Southern Europe and being responsible for over half of the implants performed in Spain, the sample is limited and from a single centre. Of note, a common follow‐up protocol with the HF nurse and doctor was applied to all patients during the study period, limiting possible bias introduced by different management strategies.
Second, the relative reduction in HF hospitalizations in the post‐CardioMEMS period was greater than that observed in the CHAMPION trial but similar to other more recent reports. 20
Third, the choice to utilize a 1 year follow‐up in our study was primarily based on the data we had available at the time. HF patients typically experience an increased frequency of hospitalizations as their condition progresses. Given this trajectory, our 1 year observation could potentially underestimate the benefits of the CardioMEMS system. If we already observe significant benefits within the first year, it stands to reason that these benefits might be even more pronounced as the disease advances.
Fourth, while probabilistic sensitivity analysis has become the gold standard as it permits the joint uncertainty across all parameters in the model to be assessed at the same time, this study employs a simple deterministic sensitivity analysis. Future research should incorporate this type of methodology for a greater understanding of the results.
Fifth, when conducting the literature review, we found that not all studies employed the same perspective, and as such, our healthcare centre perspective does not match all of them. The differences in perspectives could influence economic results.
Finally, a potential limitation lies in the fact that the sensor's effectiveness depends on the quality of the existing HF unit. If an HF unit is already very efficient at preventing HF admissions using other remote non‐invasive strategies, the CardioMEMS system may not be as effective.
Conclusions
The findings from this analysis support the utilization of remote monitoring of PAP with the CardioMEMS HF System as an efficient midterm and long‐term strategy within healthcare centres in Southern Europe. Given the considerable benefits observed in terms of prevention of HF admissions, the CardioMEMS system emerges as a superior alternative to usual management for selected patients at high risk of HF hospitalization.
Conflict of interest
A.B.‐G. and P.C. received speaker fees from Abbott.
Funding
None.
Supporting information
Table S1. Summary from the literature review.
Table S2. Benefit–cost ratio for variations in hospitalisation costs and the QALY benefits.
Table S3. Benefit–cost ratio for variations in hospitalisation and device's costs.
Figure S1. Tornado plot of benefit–cost ratio for variations in hospitalisation costs and the QALY benefits, relative to base.
Figure S2. Tornado plot of benefit–cost ratio for variations in hospitalisation and device's costs, relative to base.
Acknowledgements
We wish to thank the nurses in the heart failure unit for data collection and for their invaluable work in the unit.
Codina, P. , Vicente Gómez, J. Á. , Hernández Guillamet, G. , Ricou Ríos, L. , Carrete, A. , Vilalta, V. , Estrada, O. , Ara, J. , Lupón, J. , Bayés‐Genís, A. , and López Seguí, F. (2024) Assessing the impact of haemodynamic monitoring with CardioMEMS on heart failure patients: a cost–benefit analysis. ESC Heart Failure, 11: 1955–1962. 10.1002/ehf2.14698.
References
- 1. Sicras‐Mainar A, Sicras‐Navarro A, Palacios B, Varela L, Delgado JF. Epidemiology and treatment of heart failure in Spain: The HF‐PATHWAYS study. Rev Esp Cardiol (Engl Ed) 2022;75:31‐38. English, Spanish. doi: 10.1016/j.rec.2020.09.033 [DOI] [PubMed] [Google Scholar]
- 2. Escobar C, Varela L, Palacios B, Capel M, Sicras A, Sicras A, et al. Costs and healthcare utilisation of patients with heart failure in Spain. BMC Health Serv Res 2020;20:964. doi: 10.1186/s12913-020-05828-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, et al. EURObservational Research Programme: Regional differences and 1‐year follow‐up results of the Heart Failure Pilot Survey (ESC‐HF Pilot). Eur J Heart Fail 2013;15:808‐817. doi: 10.1093/eurjhf/hft050 [DOI] [PubMed] [Google Scholar]
- 4. Bayes‐Genis A, Codina P, Abdul‐Jawad Altisent O, Santiago E, Domingo M, Cediel G, et al. Advanced remote care for heart failure in times of COVID‐19 using an implantable pulmonary artery pressure sensor: The new normal. Eur Heart J Suppl 2020;22:P29‐P32. doi: 10.1093/eurheartj/suaa169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: A randomised controlled trial. Lancet 2011;377:658‐666. doi: 10.1016/S0140-6736(11)60101-3 [DOI] [PubMed] [Google Scholar]
- 6. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129‐2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 7. Brugts JJ, Radhoe SP, Clephas PRD, Aydin D, van Gent MWF, Szymanski MK, et al. Remote haemodynamic monitoring of pulmonary artery pressures in patients with chronic heart failure (MONITOR‐HF): A randomised clinical trial. Lancet 2023;401:2113‐2123. doi: 10.1016/S0140-6736(23)00923-6 [DOI] [PubMed] [Google Scholar]
- 8. Cowie MR, Simon M, Klein L, Thokala P. The cost‐effectiveness of real‐time pulmonary artery pressure monitoring in heart failure patients: A European perspective. Eur J Heart Fail 2017;19:661‐669. doi: 10.1002/ejhf.747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abellán Perpiñán JM, Sánchez Martínez FI, Martínez Pérez JE. La medición de la calidad de los estudios de evaluación económica: Una propuesta de “checklist” para la toma de decisiones [Quality assessment of economic evaluations in health care: A checklist and user guide]. Rev Esp Salud Publica 2009;83:71‐84. Spanish. doi: 10.1590/s1135-57272009000100006 [DOI] [PubMed] [Google Scholar]
- 10. Sandhu AT, Goldhaber‐Fiebert JD, Owens DK, Turakhia MP, Kaiser DW, Heidenreich PA. Cost‐effectiveness of implantable pulmonary artery pressure monitoring in chronic heart failure. JACC Heart Fail 2016;4:368‐375. doi: 10.1016/j.jchf.2015.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martinson M, Bharmi R, Dalal N, Abraham WT, Adamson PB. Pulmonary artery pressure‐guided heart failure management: US cost‐effectiveness analyses using the results of the Champion clinical trial. Eur J Heart Fail 2016;19:652‐660. doi: 10.1002/ejhf.642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schmier JK, Ong KL, Fonarow GC. Cost‐effectiveness of remote cardiac monitoring with the CardioMEMS Heart Failure System. Clin Cardiol 2017;40:430‐436. doi: 10.1002/clc.22696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brent RJ. Cost‐benefit analysis versus cost‐effectiveness analysis from a societal perspective in healthcare. Int J Environ Res Public Health 2023;20:4637. doi: 10.3390/ijerph20054637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Robinson R. Cost‐benefit analysis. BMJ 1993;307:924‐926. doi: 10.1136/bmj.307.6909.924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Generalitat de Catalunya . Ordre SLT/71/2020, de 2 de juny, per la qual es regulen els supòsits i conceptes facturables i s'aproven els preus públics corresponents als serveis que presta l'Institut Català de la Salut. 2020. Available at: https://cido.diba.cat/legislacio/10263520/ordre‐slt712020‐de‐2‐de‐juny‐per‐la‐qual‐es‐regulen‐els‐suposits‐i‐conceptes‐facturables‐i‐saproven‐els‐preus‐publics‐corresponents‐als‐serveis‐que‐presta‐linstitut‐catala‐de‐la‐salut‐departament‐de‐salut. Accessed 13 Dec 2022.
- 16. Institut Català de la Salut . Llibre De Retribucions 2022, Personal Estatutari de L'ICS. 2022. Available at: https://administraciopublica.gencat.cat/web/.content/funcio‐publica/empleats‐publics/retribucions/2022/Llibre‐de‐retribucions‐2022.pdf. Accessed 15 Dec 2022.
- 17. Vallejo‐Torres L, García‐Lorenzo B, Serrano‐Aguilar P. Estimating a cost‐effectiveness threshold for the Spanish NHS. Health Econ 2018;27:746‐761. doi: 10.1002/hec.3633 Epub 2017 Dec 28 [DOI] [PubMed] [Google Scholar]
- 18. Vallejo‐Torres L, García‐Lorenzo B, Rivero‐Arias O, Pinto‐Prades JL. The societal monetary value of a QALY associated with EQ‐5D‐3L health gains. Eur J Health Econ 2020;21:363‐379. doi: 10.1007/s10198-019-01140-4 [DOI] [PubMed] [Google Scholar]
- 19. Husereau D, Drummond M, Augustovski F, de Bekker‐Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: Updated reporting guidance for health economic evaluations. Eur J Health Econ 2022;23:1309‐1317. doi: 10.1016/j.jval.2021.11.1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shavelle DM, Desai AS, Abraham WT, Bourge RC, Raval N, Rathman LD, et al. Lower rates of heart failure and all‐cause hospitalizations during pulmonary artery pressure‐guided therapy for ambulatory heart failure: One‐year outcomes from the CardioMEMS Post‐Approval Study. Circ Heart Fail 2020;13:e006863. doi: 10.1161/CIRCHEARTFAILURE.119.006863 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary from the literature review.
Table S2. Benefit–cost ratio for variations in hospitalisation costs and the QALY benefits.
Table S3. Benefit–cost ratio for variations in hospitalisation and device's costs.
Figure S1. Tornado plot of benefit–cost ratio for variations in hospitalisation costs and the QALY benefits, relative to base.
Figure S2. Tornado plot of benefit–cost ratio for variations in hospitalisation and device's costs, relative to base.


