Abstract
Despite improvements over recent years, morbidity and mortality associated with heart failure (HF) are higher in countries in the Central and Eastern Europe and Baltic region than in Western Europe. With the goal of improving the standard of HF care and patient outcomes in the Central and Eastern Europe and Baltic region, this review aimed to identify the main barriers to optimal HF care and potential areas for improvement. This information was used to suggest methods to improve HF management and decrease the burden of HF in the region that can be implemented at the national and regional levels. We performed a literature search to collect information about HF epidemiology in 11 countries in the region (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). The prevalence of HF in the region was 1.6–4.7%, and incidence was 3.1–6.0 per 1000 person‐years. Owing to the scarcity of published data on HF management in these countries, we also collected insights on local HF care and management practices via two surveys of 11 HF experts representing the 11 countries. Based on the combined results of the literature review and surveys, we created national HF care and management profiles for each country and developed a common patient pathway for HF for the region. We identified five main barriers to optimal HF care: (i) lack of epidemiological data, (ii) low awareness of HF, (iii) lack of national HF strategies, (iv) infrastructure and system gaps, and (v) poor access to novel HF treatments. To overcome these barriers, we propose the following routes to improvement: (i) establish regional and national prospective HF registries for the systematic collection of epidemiological data; (ii) establish education campaigns for the public, patients, caregivers, and healthcare professionals; (iii) establish formal HF strategies to set clear and measurable policy goals and support budget planning; (iv) improve access to quality‐of‐care centres, multidisciplinary care teams, diagnostic tests, and telemedicine/telemonitoring; and (v) establish national treatment monitoring programmes to develop policies that ensure that adequate proportions of healthcare budgets are reserved for novel therapies. These routes to improvement represent a first step towards improving outcomes in patients with HF in the Central and Eastern Europe and Baltic region by decreasing disparities in HF care within the region and between the region and Western Europe.
Keywords: Heart failure management, Central and Eastern Europe and Baltic region, Patient pathway, Multidisciplinary care, Registries, Heart failure nursing
Introduction
Cardiovascular diseases (CVDs), including heart failure (HF), are responsible for nearly one‐third of all deaths in countries in the Central and Eastern Europe and Baltic region. 1 This region includes Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, Slovakia, and Slovenia and has a total population of more than 110 million people. 2 Despite improvements over recent years, CVD mortality remains substantially higher in this region than in Western Europe. For example, the age‐standardized CVD mortalities in Latvia (883 deaths per 100 000 inhabitants) and Romania (951 deaths per 100 000 inhabitants) are more than twice the European Union (EU) average (374 deaths per 100 000 inhabitants). 3
The reasons for this discrepancy in mortality between countries in the Central and Eastern Europe and Baltic region and those in Western Europe are likely to be multifactorial. Heterogeneity in HF burden is considerable according to the Heart Failure Association (HFA) Atlas survey, which was conducted between 2018 and 2019 in 42 European countries. 4 Based on the statistics available for 13 of the participating countries, the median prevalence of HF per 1000 people was 17.2 (inter‐quartile range 14.3–21.0). In the five countries in the Central and Eastern Europe and Baltic region for which data were available, the prevalence of HF per 1000 people was 16.0 in Hungary, 19.7 in Poland, 21.0 in Czechia, 23.0 in Slovakia, and 30.8 in Lithuania.
There are substantial differences in healthcare budgets between the Central and Eastern Europe and Baltic region and the EU5 (France, Germany, Italy, Spain, and the United Kingdom) according to a recent report on healthcare outcomes and expenditure in Central and Eastern Europe. 1 The report, developed by the European Federation of Pharmaceutical Industries and Associations' Central and Eastern Europe Task Force and PricewaterhouseCoopers (PwC), shows that average public spending on healthcare as a proportion of gross domestic product (GDP) is approximately three percentage points lower in countries in Central and Eastern Europe (5.0% of GDP) than the EU5 average (8.0% of GDP) and that this gap in healthcare spending increased between 2010 and 2017. 1 It also showed that patients in these countries have poorer health outcomes than in the EU5. 1 For example, life expectancy is shorter in these countries, and despite a positive trend towards declining CVD mortality across the region, this rate is still about three times higher than in the EU5.
The PwC report also showed that patients in the region had access to fewer novel therapies between 2016 and 2019 than those in the EU5 and waited longer to get access to new drugs (304 days longer on average for a drug to be made available in countries in the Central and Eastern European and Baltic region than in the EU5). 1 Furthermore, it showed that out‐of‐pocket pharmaceutical expenditure was high in many countries in the Central and Eastern European and Baltic region.
The World Heart Federation (WHF) has developed a series of roadmaps to engage stakeholders with patient pathways for HF and the improvement of HF management and to encourage countries to prepare a local ‘call to action’. 5
Published data about HF management in the Central and Eastern Europe and Baltic region are scarce. To build on the WHF Roadmap for Heart Failure, 5 the HFA Atlas survey, 4 and the PwC report, 1 we reviewed the current state of HF epidemiology and management in 11 countries within the Central and Eastern Europe and Baltic region (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). We combined a literature review with original surveys of regional HF experts to supplement the limited literature data available on this subject to create national HF care and management profiles for each country.
The aims of the current analysis are as follows:
to develop national HF profiles for 11 countries in the Central and Eastern Europe and Baltic region by reviewing relevant literature and surveying local HF experts,
to develop a shared patient pathway for HF for the region,
to identify common barriers to optimal HF care and management in the 11 countries, and
to produce a series of short‐ and long‐term actions at the national and regional level to improve HF care and management and decrease the burden of HF in the region.
Data collection
Literature review
Embase, PubMed, and Google Scholar were searched for articles on HF epidemiology, patient pathways for HF, and HF management published between January 2001 and January 2021 (Supporting Information, Table S1 ). Articles written in any language were included. Abstracts were screened for relevance, and articles were sorted according to geographical region (Central and Eastern Europe and Baltic region and the rest of the world). The results of the literature search were combined with relevant publications provided by local HF experts. Epidemiological data (HF prevalence and incidence, mortality due to HF, and hospitalization due to HF) were extracted and recorded in a standard form (Supporting Information, Table S2 ). The literature data were used to develop the national HF profiles, to identify common barriers to optimal HF management and care, and to develop the routes to improvement.
Surveys of regional HF experts
Because published data about HF management in the Central and Eastern Europe and Baltic region are scarce, two original surveys of regional HF experts were designed and performed to supplement the literature search results and provide a more complete picture of the current state of HF epidemiology, care, and management in 11 countries within the Central and Eastern Europe and Baltic region (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia).
National HF status survey
HF experts representing the HF societies of the 11 countries were surveyed to provide a comprehensive picture of HF epidemiology, outcomes, and care in each country. One expert per country completed a qualitative national HF status survey in which they provided free‐text answers to broad questions about HF epidemiology, management, patient pathways, policies, guidelines, initiatives, reimbursement, and key challenges and areas for improvement in their own countries (Supporting Information, Figure S1 ). The experts provided local publications to support their responses to the national HF status survey and to supplement the literature review. The results of this survey were combined with the results of the literature review to develop the national HF profiles, to identify common barriers to optimal HF management and care, and to develop the routes to improvement.
National HF management survey
A semi‐quantitative national HF management survey was used to collect country‐specific information about HF management at the patient, healthcare professional (HCP), and healthcare system levels. A standardized Excel‐based form was completed by the same HF experts representing the 11 countries in the Central and Eastern Europe and Baltic region (Supporting Information, Figure S2 ). For 45 possible HF management/care strategies, the experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country). The results of this survey were used to develop a shared patient pathway for HF for the region, to identify common barriers to optimal HF management and care, and to develop the routes to improvement.
Results
Central and Eastern Europe and Baltic region national HF profiles
Epidemiological data from the national HF status surveys and the literature searches are reported in Figure 1 and Supporting Information, Table S2 . National HF profiles are reported in Supporting Information, National HF profiles and Supporting Information, Table S3 . An overview of these findings across the 11 countries is given here.
Figure 1.
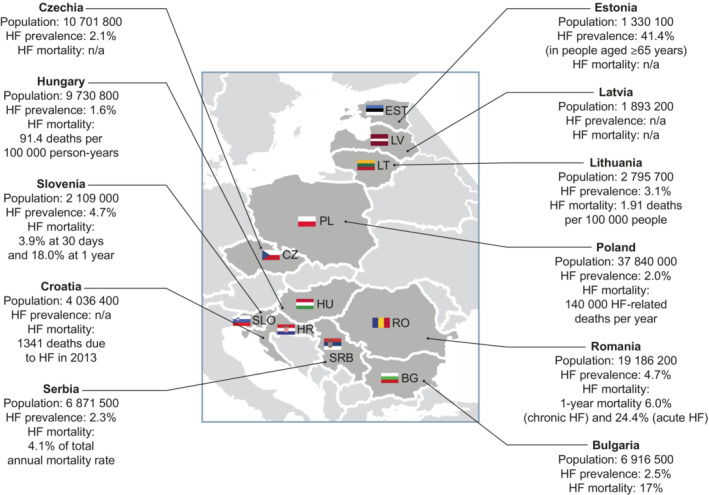
Demographics and HF epidemiology in 11 countries in the Central and Eastern Europe and Baltic region. Population data are for 1 January 2021. 6 HF, heart failure; n/a, not available.
Epidemiology
The prevalence of HF ranged from 1.6% in Hungary to 4.7% in Romania and Slovenia (Figure 1 and Supporting Information, Table S2 ). 4 , 7 For comparison, the median prevalence of HF across the 42 member countries of the European Society of Cardiology (ESC) is 1.7%. 4 For Estonia, prevalence data were available from a cross‐sectional study of 811 patients aged over 65 years with undiagnosed CVDs (41.4%). 8 The incidence of HF ranged from 3.1 per 1000 person‐years in Poland and Serbia to 6.0 per 1000 person‐years in Estonia (Supporting Information, Table S2 ). 4 , 9 , 10 The median incidence of HF across the 42 member countries of the ESC is 3.2 per 1000 person‐years. 4
The number of HF‐related hospital discharges ranged from 1154 per million people annually in Serbia to 6107 per million people annually in Romania (Supporting Information, Table S2 ). The average length of stay ranged from 6 days in Poland to 11 days in Croatia. 4 The median number of HF‐related hospitalizations across the 42 member countries of the ESC is 2671 per million people annually, and the median length of stay is 8.5 days. 4
There was substantial variation in how mortality was measured across the 11 countries, making comparisons difficult (Figure 1 and Supporting Information, Table S2 ). Mortality data were frequently unavailable owing to the lack of HF registries with long‐term follow‐up in the region.
National HF status survey results
According to the results of our national HF status survey, diagnosis of HF in most countries involves both primary care physicians (PCPs) and specialists, including cardiologists, internal medicine specialists, emergency medicine specialists, nephrologists, pulmonologists, and neurologists (Supporting Information, Table S3 ). Access to diagnostics is generally good across the region, particularly where multidisciplinary care (MDC) centres are available, but waiting times for diagnostics vary across the region.
MDC centres of some form are available in most countries (Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Serbia, and Slovenia; there are ongoing attempts to establish them in Romania). However, in many countries, they are located only in university hospitals or in large cities and are therefore not accessible to all patients. Some countries have attempted to implement or have implemented HF care programmes at the national or international level, such as the KONS (in English: Comprehensive care for patients with heart failure) programme in Poland and the OPTIMIZE‐HF Care Programme in Bulgaria, respectively. 11 , 12 Treatment is initiated or intensified in secondary care settings in Bulgaria, Croatia, and Romania and in both primary and secondary care settings in Czechia, Hungary, Latvia, Poland (30% of PCP offices are involved in the coordinated care centre programme and can initiate treatment), 13 and Slovenia (usually depending on disease severity).
In most countries, physicians follow the ESC HF guidelines translated into the local language when making decisions about HF care (Bulgaria, Croatia, Czechia, Hungary, Poland, Romania, and Slovenia). In Latvia, the ESC HF guidelines are not directly translated but are used as a reference for various educational materials, while in Lithuania, they are used as a reference for a recommendation document endorsed by the Ministry of Health. Some countries have also developed local HF care guidelines, including Estonia, where local guidelines are updated in parallel with the ESC guidelines, Latvia, where local guidelines were last updated in 2013, and Serbia, where local guidelines were last updated in 2012. Poland and Estonia provide, or plan to provide, local guidelines specifically for PCPs.
According to the responses to the national HF status survey, of the 11 countries, only Czechia and Hungary have a national HF registry. The experts from both Latvia and Romania identified the creation of a national HF registry as a key area for improvement in their country. The experts from Bulgaria, Hungary, Romania, and Slovenia stated that their countries had participated in the ESC Heart Failure Long‐Term (ESC‐HF‐LT) Registry. Czechia, Estonia, Latvia, Lithuania, Poland, and Serbia also participated in the ESC‐HF‐LT Registry. 14
Reimbursement for novel therapies varies across the region. Reimbursement is full for all therapies in Czechia, Romania and Slovenia, partial or full depending on the therapy in Bulgaria and Estonia, and partial in Hungary, Lithuania, and Serbia. Co‐payments are required for some or all therapies in Croatia and Hungary. Time from approval to reimbursement for newly approved therapies ranges from 6 months in Hungary and Croatia to up to 2 years in Romania and Latvia. Better access to novel therapies for all patients who require them was identified as a key area for improvement for Poland and Serbia. Remote information technology (IT) solutions, such as telemedicine and telemonitoring, are available in Czechia, Hungary, Latvia, Romania, Serbia, and Slovenia but are only reimbursed in some of these countries (Czechia, Hungary, and Latvia).
According to the respondents of the national HF status survey, knowledge about HF among the general population is overall poor across the Central and Eastern Europe and Baltic region, despite many countries running national education programmes. Many countries also hold HF awareness events, such as annual European HF Awareness Days and World Heart Day.
Specialist HF nurse education programmes are already in place in Estonia, Lithuania, Poland, and Slovenia and are planned in Croatia, Czechia, and Hungary.
HF management in the Central and Eastern Europe and Baltic region
Healthcare system level
One of the major healthcare system gaps highlighted by our national HF management survey is that only 4 out of 11 countries in the Central and Eastern Europe and Baltic region (Czechia, Hungary, Lithuania, and Serbia) have a national HF strategy in place (Figure 2 and Supporting Information, Table S4 ). Another significant gap is that most countries lack cross‐specialist patient coordination programmes: only two countries (Hungary and Lithuania) have these programmes in place. According to the national HF management survey, Bulgaria, Czechia, Hungary, and Slovenia have a national HF registry or regional database (Figure 2 and Supporting Information, Table S4 ).
Figure 2.
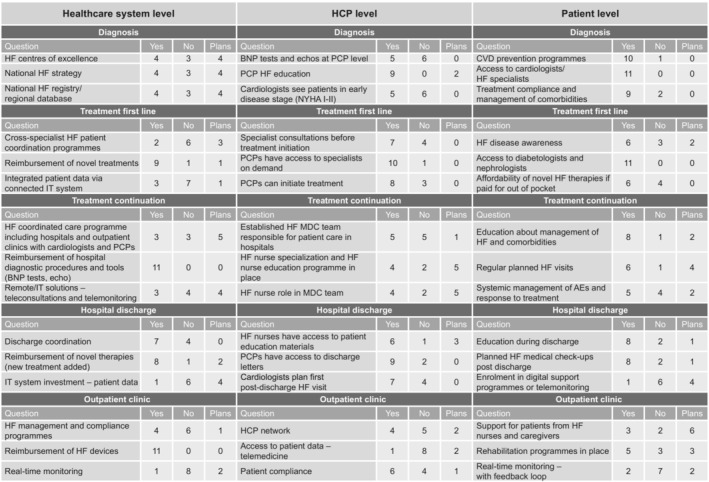
National HF management survey results. A standardized form was used to collect country‐specific information about HF management at the healthcare system level, the HCP level, and the patient level from HF experts representing 11 countries. For 45 possible HF management/care strategies, experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country). AE, adverse event; BNP, B‐type natriuretic peptide; CVD, cardiovascular disease; echo, echocardiography; HCP, healthcare professional; HF, heart failure; IT, information technology; MDC, multidisciplinary care; NYHA, New York Heart Association; PCP, primary care physician.
Only three countries (Czechia, Hungary, and Serbia) use telemonitoring and/or teleconsultation for ongoing HF care, but four countries plan to do so in the future (Croatia, Estonia, Romania, and Slovenia) (Figure 2 and Supporting Information, Table S4 ).
In‐hospital diagnostic procedures and tests are reimbursed in all 11 countries [e.g. echocardiography and B‐type natriuretic peptide (BNP) tests] (Figure 2 and Supporting Information, Table S4 ). Implanted devices for HF are reimbursed in all countries. However, the availability and level of reimbursement of HF therapies differ among countries. First‐line novel HF therapies such as sodium–glucose cotransporter‐2 inhibitors (SGLT‐2is) and/or sacubitril/valsartan are reimbursed in nine countries [Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Poland (SGLT‐2is only, sacubitril/valsartan not reimbursed), Romania, and Slovenia], and there are plans to begin reimbursing these therapies in Serbia. Novel therapies added after hospital discharge are reimbursed in eight countries [Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Poland (SGLT‐2is only, sacubitril/valsartan not reimbursed), and Slovenia]. In Latvia, HF medications are 75% reimbursed regardless of hospitalization.
Hospital discharge coordination involving patient and caregiver education and regular contact with nurses is in place in seven countries (Croatia, Czechia, Estonia, Hungary, Lithuania, Serbia, and Slovenia) (Figure 2 and Supporting Information, Table S4 ). Most countries lack coordinated care programmes involving HF specialists, PCPs, and nurses (in place in three countries: Croatia, Lithuania, and Slovenia). Local HF management and compliance programmes are available in Hungary, Lithuania, Serbia, and Slovenia.
HCP level
The survey also considered the roles of HF specialists, PCPs, and nurses. In most countries in the Central and Eastern Europe and Baltic region, specialist consultations are required before HF treatment initiation [seven countries: Bulgaria, Croatia, Czechia, Hungary, Poland (except PCP coordinated care centres), 13 Romania, and Serbia], and in most countries, PCPs can access specialists on demand (Figure 2 and Supporting Information, Table S4 ).
PCP education on HF is in place or planned in most countries (Figure 2 and Supporting Information, Table S4 ). Nurse HF education programmes are in place in four countries (Estonia, Hungary, Lithuania, and Poland) and are planned in five countries (Croatia, Czechia, Romania, Serbia, and Slovenia). Nurses have access to dedicated HF patient educational materials in six countries (Czechia, Estonia, Hungary, Lithuania, Poland, and Slovenia).
Established MDC teams are responsible for in‐hospital patient care in five countries (Croatia, Estonia, Hungary, Serbia, and Slovenia) (Figure 2 and Supporting Information, Table S4 ). In Lithuania, MDC teams are responsible for patient care in outpatient settings only. Only four countries have a clear role for HF nurses in the MDC team (Estonia, Hungary, Lithuania, and Slovenia). In most countries, cardiologists are responsible for setting the first post‐discharge follow‐up visit (eight countries; all except Latvia, Lithuania, Poland, and Romania; in Poland, post‐discharge follow‐up visits are carried out by cardiologists or PCPs at coordinated care centres) and PCPs have access to discharge letters (nine countries; all except Poland and Romania).
Patient level
Encouragingly, our survey showed that in all 11 countries, patients have access to HF specialists, cardiologists, nephrologists, and diabetologists (Figure 2 and Supporting Information, Table S4 ). Furthermore, patients have access to CVD prevention programmes in 10 countries (all except Poland). When novel HF therapies are paid for out of pocket, these therapies are deemed affordable in six countries (Bulgaria, Estonia, Latvia, Lithuania, Serbia, and Slovenia).
Overall, patient awareness regarding HF is low in most countries in the Central and Eastern Europe and Baltic region, but our survey found that eight countries (Croatia, Czechia, Hungary, Latvia, Lithuania, Poland, Serbia, and Slovenia) provide patient education about the management of HF and its associated comorbidities, and eight countries (Croatia, Czechia, Estonia, Hungary, Lithuania, Poland, Serbia, and Slovenia) provide patient education following hospital discharge (Figure 2 and Supporting Information, Table S4 ).
Optimal long‐term care of chronic HF requires regular planned check‐up visits and the monitoring of treatment responses and adverse events. According to our survey, eight countries carry out post‐discharge check‐ups (Croatia, Czechia, Estonia, Hungary, Lithuania, Poland, Serbia, and Slovenia) and five countries carry out systemic management of adverse events and response to treatment (Croatia, Hungary, Lithuania, Serbia, and Slovenia) (Figure 2 and Supporting Information, Table S4 ).
Following hospital discharge, only one country (Hungary) currently offers enrolment in digital support programmes or telemonitoring (Figure 2 and Supporting Information, Table S4 ). Real‐time outpatient monitoring is available in two countries (Hungary and Serbia). HF rehabilitation programmes for outpatients are available in five countries (Croatia, Hungary, Lithuania, Serbia, and Slovenia), and caregiver education and support programmes are available in three countries (Hungary, Lithuania, and Slovenia).
The results of the above national HF status and national HF management surveys revealed similarities in HF care and management across the Central and Eastern Europe and Baltic region. Using the results of the two surveys, we have developed a shared patient pathway for HF for the region to highlight similarities in the current state of HF care and management across the region (Figure 3 ).
Figure 3.

The Central and Eastern Europe and Baltic region shared patient pathway for HF. BP, blood pressure; BW, body weight; CARD, cardiologist; eGFR, estimated glomerular filtration rate; ENDO, endocrinologist/diabetologist; HF, heart failure; MDC, multidisciplinary care; NEPH, nephrologist; NT‐proBNP, N‐terminal pro‐B‐type natriuretic peptide; PCP, primary care physician; Rx, diagnosis; SoC, standard of care.
Key barriers to optimal HF management and routes to improvement
Based on the results of the literature search and surveys, our expert consensus group identified five key barriers to optimal care for patients with HF and developed routes to improvement to help overcome these barriers by improving knowledge, diagnosis, management, and treatment of HF in the Central and Eastern Europe and Baltic region. Where available, examples from the region and the rest of the world are provided to demonstrate best practice in overcoming each barrier (Figure 4 ).
Figure 4.
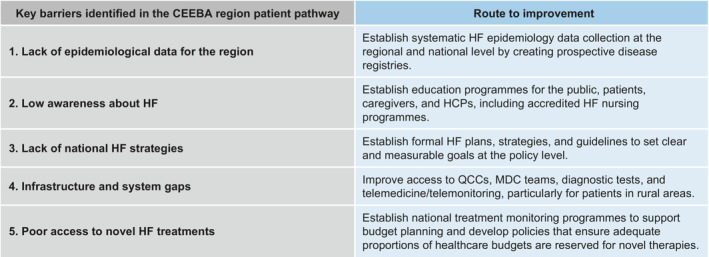
Summary of the key barriers identified along the patient pathway for HF and routes to improvement to improve the diagnosis, management, and treatment of individuals with HF in the CEEBA region to help overcome these barriers. CEEBA, Central and Eastern Europe and Baltic; HCP, healthcare professional; MDC, multidisciplinary care; QCC, quality‐of‐care centre.
1. Lack of epidemiological data for the Central and Eastern Europe and Baltic region
The lack of systematic and actionable epidemiology data on the burden of HF in most countries in the Central and Eastern Europe and Baltic region is obvious. The HFA Atlas survey is the most recent and comprehensive report on HF epidemiology, but this only contains incidence data for four countries (Estonia, Lithuania, Hungary, and Poland), prevalence data for five countries (Czechia, Hungary, Lithuania, Slovakia, and Poland), and HF‐related hospital discharge data for nine countries (Croatia, Czechia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia) in the region. 4 The epidemiological data that are available may also underestimate the true burden of HF in the region. In Poland, for example, an estimated 600 000–750 000 individuals are living with HF, but other estimates suggest that the true number is closer to 1 000 000. 15
Although dedicated HF registries have been established in some countries, our surveys revealed that most countries in the region do not have long‐term national registries in place. The lack of prospective HF registries in the region means that the majority of information collected on HF care and epidemiology comes from administrative databases, short‐term single‐ or multi‐centre studies, and research initiatives, 16 providing only a snapshot of the local burden of HF and quality of care.
Route to improvement
Local HF epidemiology data from prospective disease registries will highlight the gaps in HF care and management to governments, policymakers, and other healthcare system stakeholders and will enable an assessment of the quality of HF care over time. These data may also help guide care decisions, resource allocation, and regional HF management priorities. Clear protocols should be in place to enable HCPs to contribute to such registries. Funding should be a key consideration when setting up a disease registry because cost is a major determinant of its feasibility. In the last 14 years, the ESC has developed several large, well‐designed registries to describe the demographic, clinical, and therapeutic characteristics of patients with HF more accurately, in both acute and chronic settings. 14 , 17 , 18 , 19 , 20 However, these registries have not been fully representative, covering only a limited number of countries or enrolling mainly patients from highly specialized centres. Furthermore, there was a significant time gap between the publication of various pivotal randomized controlled trials and enrolment in these registries, making it difficult to analyse the use of therapies recently recommended by the ESC guidelines and hence adherence to these guidelines. Also, previous long‐term registries have not captured real‐time information about healthcare systems, particularly those relating to HF, in the participating countries.
An alternative to costly long‐term registries with long enrolment periods is repeated cross‐sectional surveys. Such studies can capture the relevant clinical information about patients with HF and would improve our knowledge of real‐world epidemiology and outcomes. During the first survey, each participating country would be asked to provide a country‐specific overview of the national healthcare system, national programmes, and reimbursement. Then, by performing repeated surveys, multiple snapshots can be taken. These snapshots enable the assessment of the implementation of HF guidelines and areas for improvement in the quality of care in each participating country. Finally, from a pooled database of repeated cross‐sectional survey results, single‐country analyses may be performed according to the requirements of the national HF societies in the participating countries.
In general, evidence generation should shift towards shorter, rapid‐cycle studies that enable quicker reporting of results with reduced costs, for example, those using real‐world evidence sources, digital data collection strategies, and artificial intelligence‐based data analysis.
Best practice example
The Hungarian Society of Cardiology initiated the Hungarian Heart Failure Registry in 2015. The aim of this registry is to create a web‐based database containing information about aetiology, comorbidities, diagnosis, treatment, morbidity, and mortality among patients with severe HF in Hungary. 21
2. Low awareness about HF among the public and HCPs
As in many other regions, awareness of HF among the general public is low in the Central and Eastern Europe and Baltic region. 16 , 22 , 23 A survey from Bulgaria revealed that 39% of participants were unable to recognize the symptoms of HF, and in the youngest respondents, this went up to 55%. 24 This echoes findings from a previous global study, which found that more than 50% of participants were unable to identify a description of HF. 23 According to our national HF status survey, many countries in the region have dedicated HF awareness programmes, and educational programmes for individuals with HF are available in some countries. However, there is still room to increase awareness among the public.
There is also a need for dedicated HF education for HCPs, especially nurses, who play an essential role in MDC teams. Despite the publication of a curriculum for HF specialist nurses by the HFA, 25 relatively few countries in the region have an accredited HF nurse training programme in place. 16 Our survey found that only four countries run dedicated HF nurse education programmes (Estonia, Hungary, Lithuania, and Poland). Similar programmes in Western Europe have been shown to decrease the number of hospital re‐admissions for HF. 26 , 27
Route to improvement
Systematic education programmes are required at all levels, with a focus on education for the public, patients, caregivers, PCPs, and nurses. Accredited HF education programmes are suggested for HCPs to ensure continuity of care at the national and regional level. Countries should assess the baseline public HF awareness level and conduct disease awareness campaigns based on this assessment. Increasing public knowledge of the signs and symptoms of HF may lead to improved diagnosis rates, more effective self‐care, and more timely patient reactions to worsening HF symptoms.
By establishing accredited HF nursing programmes, countries will be able to resource MDC teams better and thus reduce the burden on other specialists. To increase the standard of education efficiently across the whole region, shared educational resources could be created centrally before being distributed to the different countries for adaption to local needs.
The implementation of effective cardiovascular rehabilitation programmes led by MDC teams (including cardiologists, psychologists, specialist HF nurses, dieticians, and other HCPs) could also help to raise awareness among patients and their families about HF and CVDs in general, as well as the importance of adherence to therapy and attending regular follow‐up visits.
Availability of funding could be a barrier to the implementation of public educational programmes. Collaborations between national HF societies, academic institutions, and the pharmaceutical industry may be one route for providing funding for such programmes. For example, the Bulgarian Society of Cardiology, in collaboration with the pharmaceutical industry, initiated an information campaign called ‘the heart remembers!’ (‘cърцето помни!’) to improve knowledge about HF. 28
There are also several barriers to the development and accreditation of HF training programmes for HCPs, including delays in governmental approval, a lack of funding, and limited awareness of their benefits. 16 However, the sharing or co‐development of training materials between countries may reduce some of the burden.
Best practice example
In Poland, although there is no nationally accredited programme for specialist HF nurses, nurses can undertake training modules in acute and chronic HF as part of a comprehensive HF nurse education programme led by Wrocław Medical University. 15 The programme provides a unified approach to HF education for nurses through practical and theoretical classes and workshops, supplemented with a dedicated handbook for nurses and a separate patient handbook. 29 , 30 The nurse handbook includes chapters on disease background, HF nursing, patient self‐care, the role of family and caregivers in HF management, patient education, and palliative care. 29 This programme will be cascaded into several other countries in the region by national nurse programme leaders.
3. Lack of national HF strategies
Our national HF management survey revealed that 8 out of 11 countries in the Central and Eastern Europe and Baltic region did not have national HF strategies in place (Figure 2 and Supporting Information, Table S4 ). This may be owing to poor awareness about HF among policymakers and governments, leading to poor prioritization of the disease. A recent survey of 190 policymakers from six countries (Canada, Italy, Germany, Spain, the United Kingdom, and the United States) conducted by the WHF revealed that recognition of HF among government organizations was low, with only 12% of respondents recognizing HF as a leading cause of avoidable hospitalizations. 23 Only 4% of respondents were aware that more than 80% of government spending on HF is associated with hospitalizations. 23 According to the HF policy and practice in Europe report, 7 of the 10 surveyed non‐Central and Eastern European and Baltic countries did not have a national HF plan. 16
Furthermore, our national HF status survey revealed that few countries in the Central and Eastern Europe and Baltic region have developed their own national HF guidelines. Most countries in the region follow the ESC guidelines, which are updated every 5 years and are produced in English and translated into local languages. 31 There is little evidence about how effectively the ESC guidelines are implemented in the region. Good clinical guidelines are key for defining best practice, and guideline‐based care has been shown to improve outcomes in individuals with HF. 31
Route to improvement
Formal HF plans and strategies are required to set clear and measurable goals. Formal strategies may help address HF‐specific challenges including (i) identifying barriers to the reorganization of care; (ii) increasing investment in specialist HF services; (iii) defining the roles of different healthcare system functions along the patient pathway for HF; and (iv) developing methods to collect, analyse, and use HF epidemiology data. National guidelines could be used to formalize strategies for achieving some of these goals.
The implementation of this route to improvement requires awareness among politicians and policymakers about HF and its public health and economic burden.
Best practice example
In England, the 2019 National Health Service (NHS) Long Term Plan includes commitments to improve access to specialist HF nurses and diagnostic tools. 32 In Lithuania, a project dedicated to improving accessibility to specialized multidisciplinary HF care is being carried out by the Ministry of Health. 33
4. Infrastructure and system gaps
Our surveys revealed common infrastructure and system gaps in HF care along the patient pathways across the Central and Eastern Europe and Baltic region. There is insufficient provisioning of HF quality‐of‐care centres (QCCs) in the region. The HFA of the ESC has recommended the development of QCCs to unify and improve the quality of HF care and to promote a common approach to HF education and research. 34 The number of dedicated HF centres varies substantially across the region, from 0.20 per million people in Romania to 4.35 per million people in Slovenia. 4 Limited access to HF specialists may mean that many individuals already have serious cardiac damage by the time they can see a specialist. 16 , 35
There are also gaps in access to diagnostics in the region. The ESC guidelines recommend a multi‐pronged approach to HF diagnosis that involves an electrocardiogram, BNP testing, and an echocardiogram (and a chest X‐ray for acute HF). 16 , 31 Overall, access to diagnostic centres and testing varies substantially both within and among countries in the region. 16 Some tests, particularly echocardiography, are only performed on a 24/7 basis in tertiary care and specialist centres, which are usually located in large cities. This limits access to these tests and may act as a barrier to diagnosis for patients living in rural areas. There are variations in the availability and level of reimbursement for diagnostic tests across the region, which may act as a further barrier to diagnosis. Access to and reimbursement of diagnostic tests also varies among countries in the Central and Eastern Europe and Baltic region and those in Western Europe, potentially owing to a lack of understanding of the value of the tests and/or limited reimbursement. 16 , 36 For example, BNP testing is fully reimbursed in France and Germany but is reimbursed in Slovenia only if the diagnostic request comes from a specialist centre. 16
Within the Central and Eastern Europe and Baltic region, most specialist HF centres are located in large cities and university hospitals, and access to MDC teams varies on a national level. 16 Continuity of care between urban and rural areas is often poor. 16 The ESC guidelines also recommend that individuals with HF are managed by an MDC team made up of PCPs, cardiologists, specialist HF nurses, dieticians, pharmacists, psychologists, and other HCPs. 37 Communication between HCPs is essential for continuity of care between centres and improving clinical outcomes. 31 , 35 , 38 , 39
The COVID‐19 pandemic significantly affected the care of patients with CVDs throughout Europe. It is estimated that changes to routine care due to the pandemic will cause up to 100 000 excess deaths owing to CVDs in the United Kingdom alone. 40 However, the pandemic also acted as a catalyst for the optimization of healthcare delivery and the adoption of innovative approaches to the management of CVD and comorbidities by placing a renewed focus on telemedicine and highlighting the potential benefits of its use in routine clinical practice. 41 Many national HF societies recommended the use of teleconsultation and telemedicine for HF management during local quarantine or ‘lockdown’ measures. 42 However, the feasibility of implementing these recommendations depended on the resilience, efficiency, and sustainability of local healthcare systems, 43 , 44 and the pandemic also served to highlight significant gaps within the Central and Eastern Europe and Baltic region in the development and adoption of digital tools like telemedicine, teleconsultations, telemonitoring, and electronic health records and in the reimbursement of telemedicine. Also, our national HF status survey revealed that telemedicine and telemonitoring have poor availability.
Route to improvement
Access to MDC teams should be improved across the Central and Eastern Europe and Baltic region, particularly for patients living in rural areas. In line with the ESC and HFA proposal, HF QCCs should be established at accredited institutions across the region to enhance MDC in primary, secondary, and tertiary care centres. 34 Investments in diagnostic tools, such as point‐of‐care BNP testing, should be made across the region to facilitate early diagnosis of HF. Steps should also be taken to ensure that such testing is reimbursed for all patients in a timely manner. Telemedicine protocols for patients with HF should be established to facilitate follow‐up care and improve treatment compliance. 45 Wider adoption of telemedicine/telemonitoring could enable access to care for patients living in remote areas and for the vulnerable HF population during the ongoing COVID‐19 pandemic. Moving towards a digitized healthcare system, with strong community‐based care, may help reduce costs without compromising care quality.
The implementation of this route to improvement requires cooperation from policymakers and healthcare budget holders, highlighting the need for better awareness among politicians and policymakers about HF and its substantial public health and economic burden.
Best practice example
Improving Care through Accreditation and Recognition in Heart Failure (ICARe‐HF) has been developed by the HFA of the ESC. 34 , 46 ICARe‐HF evaluates the performance of individual centres, institutions, and clinics against recognized standards of care that have been developed according to the HF Specialist Curriculum, the ESC guidelines, and appropriate publications.
5. Poor access to novel HF treatments
Many innovative, novel HF medicines have been developed and approved in the past decade, including ivabradine, sacubitril/valsartan, SGLT‐2is, and direct oral anticoagulants, supported by data from randomized controlled trials and real‐world studies. 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 A large number of international guidelines have also been issued to help HCPs make decisions in their daily practices, including the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic HF. 37 The ESC has also developed a set of quality indicators for the evaluation of the quality of care of adults with HF. 56 Nevertheless, the delivery of optimal routine HF management is lagging in many countries in the Central and Eastern Europe and Baltic region.
Reimbursement for HF treatments varies substantially across the Central and Eastern Europe and Baltic region, including standard therapies (angiotensin‐converting enzyme inhibitors, angiotensin II receptor blockers, beta‐blockers, diuretics, and mineralocorticoid receptor antagonists) and novel therapies (SGLT‐2is, ivabradine, sacubitril/valsartan, and direct oral anticoagulants), as well as for cardiac devices and transplantation. The level of reimbursement varies from country to country, and some countries require a relatively high co‐payment. Several countries also have gaps in the reimbursement of cardiac devices, with only a limited sum of money available for reimbursement each year.
Time to reimbursement after EU approval of novel therapies also varies widely in the region. Reimbursement negotiations for novel therapies can take 1–2.5 years following European licencing. Owing to these delays in the reimbursement process, it is not possible to implement new evidence‐based treatments and ESC recommendations relating to guideline‐directed medical therapies in a timely manner in many countries in the region.
Route to improvement
Access to novel HF treatments should be improved throughout the Central and Eastern Europe and Baltic region by implementing policies that encourage the use of generic versions of standard HF treatments. This should promote competition and ultimately allow a larger proportion of healthcare budgets to be spent on novel treatments and facilitate the availability of these treatments soon after European regulatory approval. Policymakers should also consider alternative payment schemes for medicines.
Implementing compliance monitoring programmes at the national level could improve adherence to medications, which could reduce resource waste and improve treatment effectiveness. Measuring treatment outcomes at the national level could help identify the most effective treatments and could support local budget planning and resource allocation.
The implementation of this route to improvement also requires cooperation from policymakers and healthcare budget holders.
Limitations of data collection
There were some limitations in the way the two surveys were conducted. First, there may have been differences in how individuals interpreted each question in the qualitative national HF status survey, in which respondents provided free‐text answers to broad questions. There may also have been bias in the interpretation of these free‐text answers by the investigators. For the semi‐quantitative national HF management survey, efforts were made to mitigate these issues by asking the questions and gathering the responses in a systematic and consistent way using a standardized form. Another limitation was that both surveys were provided in English, not in local languages.
Finally, only one expert was surveyed per country, and their experiences may not be representative of all HF specialists across that country. However, care was taken to select very experienced HF specialists who were likely to have a broad understanding of the HF burden and state of HF care and management in their country, and several of the surveyed experts serve/have served as chairs of national cardiac/HF societies.
Conclusions
A literature search and two surveys of HF experts representing 11 countries in the Central and Eastern Europe and Baltic region were conducted to gather country‐specific data about HF epidemiology, management, and policy across the region. This information was used to develop national HF profiles for the 11 countries.
The results of the first survey (national HF status survey) revealed similarities in HF care and management that were used to develop a shared patient pathway for HF for the region. This survey also revealed that, despite the presence of many public education campaigns, public awareness about HF remains low across the region, most countries do not have national HF registries, and reimbursement of HF medications is highly variable across the region.
The results of the second survey (national HF management survey) revealed that, while the region as a whole excelled in certain areas of HF care and management, such as in the reimbursement of diagnostic procedures and HF devices and in access to specialists, it did poorly in other areas, such as in the use of telemedicine and IT solutions for patient monitoring and management and in the provision of coordinated care programmes. Other aspects of effective HF care and management were variable across the region, such as the availability of specialist HF training for HCPs.
The results of the two surveys and the literature search were used to identify five key barriers to optimal HF care and management in the 11 countries and to develop a number of ways to improve HF care and management and decrease the burden of HF in the region, as detailed below.
First, national and regional registries should be established to provide epidemiological data on the impact of HF in the region. Second, education for both patients and HCPs is needed to improve patient outcomes. Third, national strategies are needed to drive the necessary changes to reduce the incidence of HF. Fourth, access to MDC teams, HF QCCs, and telemedicine should be increased, and the reimbursement of diagnostic tests and telemedicine should be improved. Finally, access to novel treatments should be improved by ensuring that these medicines obtain timely and adequate reimbursement.
Overall, implementing these routes to improvement at the national and regional level should improve the consistency of care both within and among countries and help ensure that reductions in HF burden take place in an equitable way across the region.
To our knowledge, and based on our literature search findings, a detailed and multi‐layer summary report on the state of HF care and management such as this one does not exist for the 11 countries investigated here. Our work provides a comprehensive knowledge base for those wishing to drive HF policy and practice changes in this region.
Conflict of interest
.C. reports participation in advisory board for Boehringer Ingelheim. J.B. reports consulting fees from Getinge, Novartis, and Pfizer; lecture fees from Amgen, AstraZeneca, Boehringer Ingelheim, Getinge, Novartis, and Servier Laboratories; advisory board fees from Amgen, Boehringer Ingelheim, Novartis, and Pfizer; research grants from Agentura pro zdravotnický výzkum České republiky; and honoraria for clinical studies from AstraZeneca and Novartis. J.Č. reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Novartis, and Servier Laboratories. G.K. reports advisory board fees from AstraZeneca, Bayer, and Boehringer Ingelheim and speaker fees from AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Recordati, and Servier Laboratories. M.L. reports advisory board fees from AstraZeneca. B.M. reports direct personal payments from Abbott Laboratories, AstraZeneca, Biotronik, Boehringer Ingelheim, and Novartis and institutional grants from Boston Scientific and Medtronic. D.M. reports fees for lecturing, consulting, and participation in advisory boards from Abbott Laboratories, Amgen, AstraZeneca, Berlin‐Chemie Menarini, Boehringer Ingelheim, Krka, Novartis, Novo Nordisk, Pfizer, PLIVA‐Teva, and Servier Laboratories. A.D.R. reports research contracts with Arena Pharmaceuticals, European Commission Horizon 2020, Janssen, Novartis, Novo Nordisk, Pfizer, PhaseBio, and United Therapeutics Corporation and consulting/speaker fees from AstraZeneca, Berlin‐Chemie Menarini, Boehringer Ingelheim, Janssen, Merck Sharp & Dohme, Novartis, Pfizer, and Takeda, all outside of the scope of this publication. L.S. and E.T. are employees of AstraZeneca. P.P. reports personal fees for consultancy and speakers bureau from AstraZeneca, Bayer, Berlin‐Chemie Menarini, Boehringer Ingelheim, Novartis, Radcliffe Group, RenalGuard, and Vifor Pharma; other support for participation in clinical trials from Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, RenalGuard, and Vifor Pharma; and research grants to his institution from Vifor Pharma. J.N., I.U., T.U., and Y.Y. have nothing to disclose.
Funding
This work was supported by AstraZeneca.
Supporting information
Table S1. Search strings used in the literature searches of Embase, PubMed, and Google Scholar to identify local and international publications about HF epidemiology and patient pathways for HF and HF management published between January 2001 and January 2021.
Table S2. Demographics and HF epidemiology in 11 countries in the Central and Eastern Europe and Baltic region (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). Number of inhabitants is population on 1 January 2021.
Table S3. Country‐specific results of the national HF status survey. Country‐specific information about HF epidemiology, outcomes, and care in each country was collected from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). HF epidemiology data are summarized in Table S2.
Table S4. Country‐specific results of the national HF management survey. Country‐specific information about HF management was collected from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). For 45 possible HF management/care strategies, experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country).
Figure S1. National HF status survey. HF experts representing the HF societies of 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia) were surveyed about country‐specific HF epidemiology and HF‐related policies, guidelines, and initiatives.
Figure S2. National HF management survey. A standardized Excel‐based form was used to collect country‐specific information about HF management from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). For 45 possible HF management/care strategies, experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country).
Acknowledgements
Medical writing support was provided by Caitlin Edgell, PhD, of Oxford PharmaGenesis, Oxford, United Kingdom, and was funded by AstraZeneca.
Chioncel, O. , Čelutkienė, J. , Bělohlávek, J. , Kamzola, G. , Lainscak, M. , Merkely, B. , Miličić, D. , Nessler, J. , Ristić, A. D. , Sawiełajc, L. , Uchmanowicz, I. , Uuetoa, T. , Turgonyi, E. , Yotov, Y. , and Ponikowski, P. (2024) Heart failure care in the Central and Eastern Europe and Baltic region: status, barriers, and routes to improvement. ESC Heart Failure, 11: 1861–1874. 10.1002/ehf2.14687.
References
- 1. European Federation of Pharmaceutical Industries and Associations . PwC strategy report: Healthcare outcomes and expenditure in Central and Eastern Europe—A review. https://www.efpia.eu/publications/downloads/health‐outcomes/healthcare‐outcomes‐and‐expenditure‐in‐central‐and‐eastern‐europe‐a‐review/. Accessed 18 October 2021
- 2. United Nations . 2019 revision of world population prospects. https://population.un.org/wpp/. Accessed 18 October 2021
- 3. Movsisyan NK, Vinciguerra M, Medina‐Inojosa JR, Lopez‐Jimenez F. Cardiovascular diseases in Central and Eastern Europe: A call for more surveillance and evidence‐based health promotion. Ann Glob Health 2020;86:21. doi: 10.5334/aogh.2713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Seferović PM, Vardas P, Jankowska EA, Maggioni AP, Timmis A, Milinković I, et al. The Heart Failure Association Atlas: Heart failure epidemiology and management statistics 2019. Eur J Heart Fail 2021;23:906‐914. doi: 10.1002/ejhf.2143 [DOI] [PubMed] [Google Scholar]
- 5. Ferreira JP, Kraus S, Mitchell S, Perel P, Piñeiro D, Chioncel O, et al. World Heart Federation roadmap for heart failure. Glob Heart 2019;14:197‐214. doi: 10.1016/j.gheart.2019.07.004 [DOI] [PubMed] [Google Scholar]
- 6. Eurostat . Population and population change statistics: Population change at national level. https://ec.europa.eu/eurostat/statistics‐explained/index.php?title=Population_and_population_change_statistics#Population_change_at_national_level. Accessed 2 November 2021
- 7. Macarie C, Chioncel O. Studiul romanesc de prevalenta a insuficientei cardiace in populatia arondata medicilor de familie. Prog Cardiol 2007;2:311‐327. [Google Scholar]
- 8. Saks K, Kolk H, Soots A, Takker U, Vask M. Prevalence of cardiovascular disorders among the elderly in primary care in Estonia. Scand J Prim Health Care 2003;21:106‐109. doi: 10.1080/02813430310001716 [DOI] [PubMed] [Google Scholar]
- 9. Ivanuša M, Kralj V. Heart failure in the Republic of Croatia. Cardiol Croat 2014;9:465‐465. doi: 10.15836/ccar.2014.465 [DOI] [Google Scholar]
- 10. Seferović PM, Stoerk S, Filippatos G, Mareev V, Kavoliuniene A, Ristić AD, et al. Organization of heart failure management in European Society of Cardiology member countries: Survey of the Heart Failure Association of the European Society of Cardiology in collaboration with the Heart Failure National Societies/Working Groups. Eur J Heart Fail 2013;15:947‐959. doi: 10.1093/eurjhf/hft092 [DOI] [PubMed] [Google Scholar]
- 11. Nessler J, Kozierkiewicz A, Gackowski A, Ponikowski P, Straburzynska‐Migaj E, Uchmanowicz I, et al. Coordinated heart failure care in Poland: Towards optimal organisation of the health care system. Kardiol Pol 2018;76:479‐487. doi: 10.5603/KP.2018.0050 [DOI] [PubMed] [Google Scholar]
- 12. Cowie MR, Lopatin YM, Saldarriaga C, Fonseca C, Sim D, Magaña JA, et al. The Optimize Heart Failure Care Program: Initial lessons from global implementation. Int J Cardiol 2017;236:340‐344. doi: 10.1016/j.ijcard.2017.02.033 [DOI] [PubMed] [Google Scholar]
- 13. The Ministry of Health and the National Health Fund . Coordinated care in primary health care. https://pacjent.gov.pl/aktualnosc/opieka‐koordynowana‐w‐podstawowej‐opiece‐zdrowotnej. Accessed 27 November 2023
- 14. Crespo‐Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, et al. European Society of Cardiology Heart Failure Long‐Term Registry (ESC‐HF‐LT): 1‐year follow‐up outcomes and differences across regions. Eur J Heart Fail 2016;18:613‐625. doi: 10.1002/ejhf.566 [DOI] [PubMed] [Google Scholar]
- 15. The Heart Failure Policy Network . Heart failure policy and practice in Europe: Poland. 2020. https://www.hfpolicynetwork.org/wp‐content/uploads/Heart‐failure‐policy‐and‐practice‐in‐Europe‐Poland.pdf. Accessed 15 January 2021
- 16. The Heart Failure Policy Network . Heart failure policy and practice in Europe. 2020. https://www.hfpolicynetwork.org/wp‐content/uploads/Heart‐failure‐policy‐and‐practice‐in‐Europe.pdf. Accessed 9 December 2020
- 17. Maggioni AP, Dahlstrom U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, et al. EURObservational Research Programme: The Heart Failure Pilot Survey (ESC‐HF Pilot). Eur J Heart Fail 2010;12:1076‐1084. doi: 10.1093/eurjhf/hfq154 [DOI] [PubMed] [Google Scholar]
- 18. Maggioni AP, Dahlstrom U, Filippatos G, Chioncel O, Crespo Leiro M, Drozdz J, et al. EURObservational Research Programme: Regional differences and 1‐year follow‐up results of the Heart Failure Pilot Survey (ESC‐HF Pilot). Eur J Heart Fail 2013;15:808‐817. doi: 10.1093/eurjhf/hft050 [DOI] [PubMed] [Google Scholar]
- 19. Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo‐Leiro MG, Harjola VP, et al. Epidemiology and one‐year outcomes in patients with chronic heart failure and preserved, mid‐range and reduced ejection fraction: An analysis of the ESC Heart Failure Long‐Term Registry. Eur J Heart Fail 2017;19:1574‐1585. doi: 10.1002/ejhf.813 [DOI] [PubMed] [Google Scholar]
- 20. Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo‐Leiro MG, et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: The ESC Heart Failure Long‐Term Registry. Eur J Heart Fail 2017;19:1242‐1254. doi: 10.1002/ejhf.890 [DOI] [PubMed] [Google Scholar]
- 21. Nyolczas N, Heltai K, Borbély A, Habon T, Járai Z, Sziliczei E, et al. Hungarian Heart Failure Registry 2015–2016. Preliminary results. Orv Hetil 2017;158:94‐100. doi: 10.1007/5584_2017_112 [DOI] [PubMed] [Google Scholar]
- 22. Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: Preventing disease and death worldwide. ESC Heart Fail 2014;1:4‐25. doi: 10.1002/ehf2.12005 [DOI] [PubMed] [Google Scholar]
- 23. World Heart Federation . Accelerate change together: Heart failure gap review. 2020. https://www.world‐heart‐federation.org/wp‐content/uploads/HF‐Gap‐Review‐Final.pdf. Accessed 14 October 2020
- 24. Zdrave.net . 55% of young people in our country do not recognize the symptoms of heart failure. https://www.zdrave.net/Новини/55‐‐от‐младите‐хора‐у‐нас‐не‐разпознават‐симптомите‐на‐сърдечната‐недостатъчност/n13047. Accessed 21 March 2022
- 25. Riley JP, Astin F, Crespo‐Leiro MG, Deaton CM, Kienhorst J, Lambrinou E, et al. Heart Failure Association of the European Society of Cardiology heart failure nurse curriculum. Eur J Heart Fail 2016;18:736‐743. doi: 10.1002/ejhf.568 [DOI] [PubMed] [Google Scholar]
- 26. McDonagh TA, Blue L, Clark AL, Dahlström U, Ekman I, Lainscak M, et al. European Society of Cardiology Heart Failure Association standards for delivering heart failure care. Eur J Heart Fail 2011;13:235‐241. doi: 10.1093/eurjhf/hfq221 [DOI] [PubMed] [Google Scholar]
- 27. Oyanguren J, Garcia‐Garrido L, Nebot‐Margalef M, Latorre‐García P, Torcal‐Laguna J, Comín‐Colet J, et al. Noninferiority of heart failure nurse titration versus heart failure cardiologist titration. ETIFIC multicenter randomized trial. Rev Esp Cardiol 2021;74:533‐543. doi: 10.1016/j.recesp.2020.04.032 [DOI] [PubMed] [Google Scholar]
- 28. Bulgarian Society of Cardiology . The heart remembers! Information campaign on the risk of recurrent cardiovascular events in patients with acute coronary syndrome. https://bgcardio.org/bg/news/srceto‐pomni‐informacionna‐kampaniya‐za‐riska‐ot‐povtorni‐srdechnosdovi‐incidenti‐pri‐pacienti‐prezhiveli‐ostr‐koronaren‐sindrom. Accessed 11 November 2021
- 29. Institute of Heart Diseases, Wrocław Medical University . Heart failure nursing: From theory to practice. https://educardio.umw.edu.pl/nurses/docs/NURSE_handbook_pl.pdf. Accessed 5 January 2022
- 30. Institute of Heart Diseases, Wrocław Medical University . A guide to heart failure for patients and their families. https://educardio.umw.edu.pl/nurses/docs/PATIENT_handbook_PL.pdf. Accessed 5 January 2022
- 31. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129‐2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 32. NHS . Cardiovascular disease. https://www.longtermplan.nhs.uk/online‐version/chapter‐3‐further‐progress‐on‐care‐quality‐and‐outcomes/better‐care‐for‐major‐health‐conditions/cardiovascular‐disease/. Accessed 12 November 2021
- 33. Ministry of Health of the Republic of Lithuania . Improving access to services for cardiologists and nurses for people with heart failure. https://sam.lrv.lt/lt/veiklos‐sritys/programos‐ir‐projektai/gydytojo‐kardiologo‐ir‐slaugytojo‐konsultacijos‐asmenims‐sergantiems‐sirdies‐nepakankamumu‐paslaugu‐prieinamumo‐gerinimas. Accessed 21 March 2022
- 34. Seferović PM, Piepoli MF, Lopatin Y, Jankowska E, Polovina M, Anguita‐Sanchez M, et al. Heart Failure Association of the European Society of Cardiology Quality of Care Centres Programme: Design and accreditation document. Eur J Heart Fail 2020;22:763‐774. doi: 10.1002/ejhf.1784 [DOI] [PubMed] [Google Scholar]
- 35. Morton G, Masters J, Cowburn PJ. Multidisciplinary team approach to heart failure management. Heart 2018;104:1376‐1382. doi: 10.1136/heartjnl-2016-310598 [DOI] [PubMed] [Google Scholar]
- 36. The Heart Failure Policy Network . Heart failure policy and practice in Europe: Belgium. 2020. https://www.hfpolicynetwork.org/wp‐content/uploads/Heart‐failure‐policy‐and‐practice‐in‐Europe‐Belgium.pdf. Accessed 14 December 2020
- 37. Authors/Task Force Members , McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2022;24:4‐131. doi: 10.1002/ejhf.2333 [DOI] [PubMed] [Google Scholar]
- 38. Smeets M, Van Roy S, Aertgeerts B, Vermandere M, Vaes B. Improving care for heart failure patients in primary care, GPs' perceptions: A qualitative evidence synthesis. BMJ Open 2016;6:e013459. doi: 10.1136/bmjopen-2016-013459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taylor CJ, Rutten FH, Brouwer JR, Hobbs FDR. Practical guidance on heart failure diagnosis and management in primary care: Recent EPCCS recommendations. Br J Gen Pract 2017;67:326‐327. doi: 10.3399/bjgp17X691553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M, Denaxas S, et al. Excess deaths in people with cardiovascular diseases during the COVID‐19 pandemic. Eur J Prev Cardiol 2021;28:1599‐1609. doi: 10.1093/eurjpc/zwaa155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Salzano A, D'Assante R, Stagnaro FM, Valente V, Crisci G, Giardino F, et al. Heart failure management during the COVID‐19 outbreak in Italy: A telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail 2020;22:1048‐1050. doi: 10.1002/ejhf.1911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kaluzna‐Oleksy M, Gackowski A, Jankowska EA, Kukulski T, Lelonek M, Nessler J, et al. The patient with heart failure in the face of the coronavirus disease 2019 pandemic: An expert opinion of the Heart Failure Working Group of the Polish Cardiac Society. Kardiol Pol 2020;78:618‐631. doi: 10.33963/KP.15359 [DOI] [PubMed] [Google Scholar]
- 43. British Society of Echocardiography . Clinical guidance regarding provision of echocardiography during the COVID‐19 pandemic. https://bsecho.org/covid19. Accessed 24 July 2020
- 44. Cheung JC, Lam KN. POCUS in COVID‐19: Pearls and pitfalls. Lancet Respir Med 2020;8:e34. doi: 10.1016/S2213-2600(20)30166-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Eurlings CGMJ, Boyne JJ, de Boer RA, Brunner‐La Rocca HP. Telemedicine in heart failure—More than nice to have? Neth Heart J 2019;27:5‐15. doi: 10.1007/s12471-018-1202-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. European Society of Cardiology . ICARe‐HF—Recognising excellence in heart failure care. https://www.escardio.org/Education/Career‐Development/Accreditation/icare‐hf‐recognising‐excellence‐in‐heart‐failure‐care. Accessed 8 November 2023
- 47. Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost‐Brama A, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): A randomised placebo‐controlled study. Lancet 2010;376:875‐885. doi: 10.1016/S0140-6736(10)61198-1 [DOI] [PubMed] [Google Scholar]
- 48. McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014;371:993‐1004. doi: 10.1056/NEJMoa1409077 [DOI] [PubMed] [Google Scholar]
- 49. McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995‐2008. doi: 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 50. Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, et al. Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: Rationale and design of the DELIVER trial. Eur J Heart Fail 2021;23:1217‐1225. doi: 10.1002/ejhf.2249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 2021;385:1451‐1461. doi: 10.1056/NEJMoa2107038 [DOI] [PubMed] [Google Scholar]
- 52. Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 2020;383:1413‐1424. doi: 10.1056/NEJMoa2022190 [DOI] [PubMed] [Google Scholar]
- 53. Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med 2021;384:117‐128. doi: 10.1056/NEJMoa2030183 [DOI] [PubMed] [Google Scholar]
- 54. Vaduganathan M, Docherty KF, Claggett BL, Jhund PS, de Boer RA, Hernandez AF, et al. SGLT‐2 inhibitors in patients with heart failure: A comprehensive meta‐analysis of five randomised controlled trials. Lancet 2022;400:757‐767. doi: 10.1016/S0140-6736(22)01429-5 [DOI] [PubMed] [Google Scholar]
- 55. Roberti R, Iannone LF, Palleria C, Curcio A, Rossi M, Sciacqua A, et al. Direct oral anticoagulants: From randomized clinical trials to real‐world clinical practice. Front Pharmacol 2021;12:684638. doi: 10.3389/fphar.2021.684638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Aktaa S, Polovina M, Rosano G, Abdin A, Anguita M, Lainscak M, et al. European Society of Cardiology quality indicators for the care and outcomes of adults with heart failure. Developed by the Working Group for Heart Failure Quality Indicators in collaboration with the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2022;24:132‐142. doi: 10.1002/ejhf.2371 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search strings used in the literature searches of Embase, PubMed, and Google Scholar to identify local and international publications about HF epidemiology and patient pathways for HF and HF management published between January 2001 and January 2021.
Table S2. Demographics and HF epidemiology in 11 countries in the Central and Eastern Europe and Baltic region (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). Number of inhabitants is population on 1 January 2021.
Table S3. Country‐specific results of the national HF status survey. Country‐specific information about HF epidemiology, outcomes, and care in each country was collected from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). HF epidemiology data are summarized in Table S2.
Table S4. Country‐specific results of the national HF management survey. Country‐specific information about HF management was collected from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). For 45 possible HF management/care strategies, experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country).
Figure S1. National HF status survey. HF experts representing the HF societies of 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia) were surveyed about country‐specific HF epidemiology and HF‐related policies, guidelines, and initiatives.
Figure S2. National HF management survey. A standardized Excel‐based form was used to collect country‐specific information about HF management from HF experts representing 11 countries (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Serbia, and Slovenia). For 45 possible HF management/care strategies, experts answered ‘Yes’ (this strategy is in place in their country), ‘No’ (this strategy is not in place in their country), or ‘Plans’ (plans exist to implement this strategy in their country).


