Abstract
Background:
Cesarean section (CS) is one of the most important pregnancy concerns in the world. Increased inflammation is associated with increased risk factors for cesarean section. Diet plays a major role in reducing inflammation. This study aimed to investigate the relationship between dietary inflammatory index (DII) and the risk of Cesarean section in Tehranian women.
Methods:
This case-control study included 390 pregnant women in Tehran, Iran between 2020 and 2021 at their initial visit to pregnancy clinics, selected by a cluster sampling method. Dietary intakes were determined using valid reliable questionnaires and DII was calculated. Weight, height, and waist circumference were also measured.
Results:
The mean age of the subjects was 28.5 yr (± 5.02) and weight, body mass index (BMI) and waist circumference (WC) in the case group with a higher DII were higher. Odds ratio (OR) of cesarean section in DII quartiles was statistically significant. Confounding factors including age, BMI and total energy intake were adjusted in the first model and weight, waist circumference, physical activity and supplements in the second model and the relationship remained significant (P<0.001).
Conclusion:
High scores of dietary inflammatory index, possibly through an increase in inflammatory factors, can increase the chances of having a cesarean section.
Keywords: Diet, Inflammation, Cesarean section, Delivery, Obstetric
Introduction
Cesarean section delivery is one of the most critical issues in pregnancy all over the world (1). Recent studies indicate an increasing trend in the prevalence of cesarean section in both developed and developing countries (2). According to the WHO, the average rate of cesarean section was 15%, and with a rate of 48%, it is three times higher than the standard rate (3).
Various factors affect the need for cesarean section delivery, including diabetes, high blood pressure and preeclampsia, reduced uterine contractions, obesity, and breech (4). Social and economic factors also play a great role in increasing the chance of cesarean delivery (5). Obesity as a cesarean risk factor is considered as a chronic inflammation that causes increased CRP and pro-inflammatory cytokines such as IL6 and TNF-α. Thus, an increase in body mass index and obesity in android shape is related to increased inflammation (6).
An unhealthy diet is associated with high levels of inflammatory factors, while a healthy diet containing fruits, vegetables, fish, omega-3 fatty acids and fiber is associated with low levels of inflammatory indices (7). Dietary inflammatory index (DII) is a nutritional index that was developed in 2009 and introduced in 2014 (8), and based on extensive studies its main purpose is to assess the inflammatory and anti-inflammatory potential of the diet (9). A diet with a higher score of DII is associated with hypertension (10), high blood triglyceride and decreased HDL (High-Density Lipoprotein) levels (11), cardiovascular disorders (circulatory disorders, congestive heart failure, coronary heart disease, angina pectoris, heart attack, myocardial infarction) (12) and stroke (13). Also, according to some studies, a diet with a high DII is associated with a higher body mass index (BMI) and waist circumference (WC) (14).
In recent years, several studies have been conducted in Western countries on the correlation between DII and various diseases (15, 16). The diets of Asian countries are different from those of Western countries, and changes in Asian food patterns as a result of the introduction of Western food patterns in recent years have caused many changes, such as increased consumption of foods rich in refined sugar, sodium, saturated fats and trans fats leading to the spread of obesity and inflammation in these countries (17). Some previous studies have examined the effect of healthy eating patterns on birth outcomes (18) or the impact of quality improvement in reducing unnecessary cesarean sections (19). Still, none of them have directly mentioned the relationship between DII and cesarean.
Considering that inflammatory factors can be risk factors for cesarean section (20), and since dietary control is the easiest way to reduce the complications and costs of cesarean delivery, we decided in this study to investigate the relationship between inflammation and the need for cesarean section. We hypothesized that increasing dietary inflammatory index might be associated with increased chances of cesarean section delivery.
Materials and Methods
Study population
This was a case-control study on women referring to pregnancy clinics in Tehran, Iran. Gpower 3.1.9.2 software (Kiel University, Kiel, Germany) was used to calculate the sample size. The required sample size was calculated based on Effect Size = 0.1, α = 0.05, β = 0.1 (power = 0.9) and with seven degrees of freedom, equal to 190 people in each group. Considering the probability of dropping out of 10% of the samples, finally, 210 women in either group (cesarean section and normal delivery) were selected.
The inclusion criteria were a reproductive age of 18 to 45 years, agreeing to participate in the project, completing the informed consent, and being referred to pregnancy clinics in Tehran, Iran, which required either a cesarean section or a normal delivery based on the diagnosis by a gynecologist, not being an immigrant, not having any diseases, not taking certain medications, not being on a diet, no alcohol consumption, and should not be smokers. The exclusion criteria were lack of cooperation and failure to complete the questionnaire.
A written consent was obtained from all participants in the survey, approved by Iran national committee for ethics in biomedical research (Ethical approval number: IR.IAU.SRB.REC.1398.147).
Data collection
Dietary intake: This was assessed using a food frequency questionnaire with 147 items designed according to the Willett method (21). Food items consumed by individuals were converted to grams per day using the home-scale.
Calculating the dietary inflammatory index (DII): DII is based on 45 food parameters using 1943 peer-reviewed articles till 2010; these parameters have pro-inflammatory or anti-inflammatory effects on the inflammatory markers (IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP). The DII scoring system uses a global reference database that includes foods consumed by 11 populations around the world and ranges from −8.87 (anti-inflammatory) to 7.98 (pro-inflammatory) (16).
Anthropometric measurements using standard protocols: Anthropometric measurements, including weight (with least clothing, without shoes, using Seca scale made in Germany), height (without shoes in a standing position, the whole body in one direction, and looking forward, using Seca scales) and waist circumference. The accuracy of height and waist measurements was 0.1 cm and that of weight was 100 g.
Statistical analysis
The software used for data analysis was SPSS 26 (IBM Corp., Armonk, NY, USA). Food intake was analyzed by the Nutritionist 4 software. The range of DII quartiles was calculated and individuals were divided based on quartiles. To determine the existence of a statistically significant relationship between quantitative and qualitative variables with the quartiles of DII, one-way analysis of variance and chi-square test were used, respectively. Linear logistic regression was used to determine the relationship between DII and cesarean section. Except for the raw model, two other models were used for the study. The first model was moderated based on age, energy in-take and BMI, and the second model, in addition to model one, was moderated for physical activity, socioeconomic status, marriage, and taking supplements. Finally, all three models were studied and a P-value less than 0.05 was considered to show statistical significance.
Results
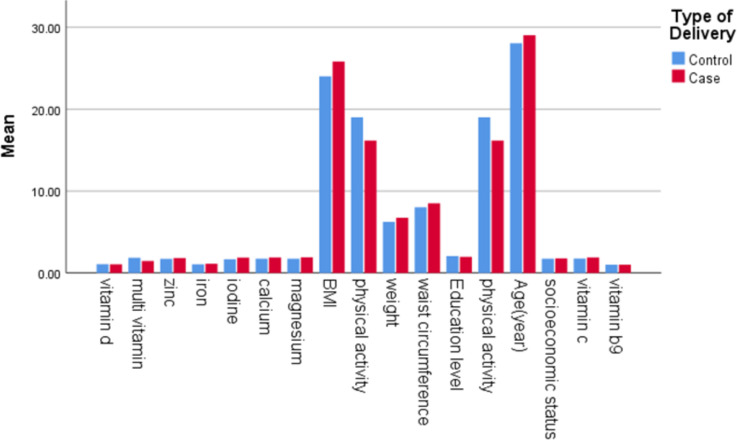
Overall, 390 women between the ages of 18 and 45 years old with a mean age of 28.5 (±5.02) yr were included in this study. The means (±SD) of weight, body mass index, waist circumference, and level of physical activity between case and control groups were significant, shown in Fig. 1. Comparison of demographic and anthropometric factors and lifestyle of participants based on DII score quartiles are indicated in Table 1.
Fig. 1:
Demographic, anthropometric and lifestyle characteristics of participants in case and control groups [mean ± SD]. Case: caesarean section. Control: natural vaginal delivery. Waist circumference and weight with a scale of 0.1 and physical activity with a scale of 0.01 are given in the graph
Table 1:
Comparison of Demographic and Anthropometric Variables and Lifestyle of Participants Based on DII Score Quartiles (Q)
| DII (Dietary Inflammatory Index) | |||||
|---|---|---|---|---|---|
|
| |||||
| Variable | Q1 | Q2 | Q3 | Q4 | P value |
| Age(yr) | 29.05(5.22) | 27.3(5.05) | 29.02(5.32) | 28.63(4.29) | 0.049 |
| Weight(kg) | 63.26(8.77) | 62.82(8.45) | 63.95(9.12) | 69.18(8.45) | <0.001 |
| Waist circumference (cm) | 83.36(6.7) | 81.09(6.84) | 81.84(7.84) | 84.94(9.73) | 0.005 |
| Physical activity( MET-h/wk) | 1690.71(618.17) | 1886.43(690.18) | 1841.14(631.76) | 1649.78(660.78) | 0.03 |
| Educational level | 0.134 | ||||
| Body mass index (BMI) | 0.05 | ||||
| Socio-economic status (SES) | 0.11 | ||||
| Vitamin C supplementation (yes) | 18(18.8) | 22(22.4) | 14(14.3) | 17(17.5) | 0.54 |
| Folate supplementation (yes) | 94(96.6) | 97(99) | 97(99) | 96(99) | 0.56 |
| Vitamin D supplementation (yes) | 91(93.8) | 91(92.9) | 89(90.8) | 92(94.8) | 0.72 |
| Mineral multivitamin supplement (yes) | 30(30.9) | 28(28.6) | 30(30.6) | 37(38.1) | 0.5 |
| zinc supplementation (yes) | 22(22.9) | 26(26.5) | 19(19.4) | 22(22.7) | 0.7 |
| Iron supplementation (yes) | 88(90.7) | 94(95.9) | 85(86.7) | 88(90.7) | 0.16 |
| Iodine supplementation (yes) | 26(27.1) | 28(28.6) | 17(17.3) | 17(17.5) | 0.1 |
| Calcium supplementation (yes) | 18(18.8) | 24(24.5) | 13(13.3) | 16(16.5) | 0.22 |
| Magnesium supplementation (yes) | 22(22.9) | 23(23.5) | 14(14.3) | 11(11.3) | 0.06 |
The obtained values and reported P value were calculated using by ANOVA test (for quantitative data) or chi-square test (for qualitative data) and the numbers are mean (standard deviation) or number (percentage)
Subjects in the fourth quartiles with the highest score of DII consumed less vegetables and grains than those in the first quartile, while the consumption of refined grains was higher. The quartiles also differ in terms of dairy and cereal consumption. According to Table 2 in the raw model, the ratio of the chances of cesarean delivery in the quartiles of the inflammatory index of the diet was statistically significant. After moderating the confounding factors, including age, BMI and total energy intake in the first model and adjusting for weight, waist circumference, physical activity and supplements in the second model, the relationship remained significant (P <0.001).
Table 2:
Odds ratio (OR) of cesarean section delivery and 95% confidence interval (CI) based on quartiles (Q) of Dietary Inflammatory Index (DII) in women with cesarean section delivery
| Variable | Q1 | Q2 | Q3 | Q4 | Ptrend |
|---|---|---|---|---|---|
| The ratio of the number of women in the case group to the total population | 97.34 | 98.37 | 98.47 | 97.64 | |
| Crude model | 1 | 1.39(0.75–2.56) | 2.02(1.11–3.66) | 4.27(2.29–7.96) | <0.001 |
| Model 1† | 1 | 1.76(0.92–3.38) | 2.34(1.25–4.39) | 5.37(2.71–10.64) | <0.001 |
| Modified Model 2 ‡ | 1 | 1.93(0.9–4.13) | 2.06(1–4.26) | 4.52(2.05–9.92) | <0.001 |
The values in the table are equal to the value of the odds obtained (95% confidence interval).
The values obtained for P trend are considered using logistic test and odds ratio for the first quarter.
† Modified model based on age, body mass index and energy.
‡ Modified model based on weight, waistline, physical activity and supplementation with vitamin C, multivitamin mineral, zinc, iron, iodine, calcium and magnesium
After comparing the average food intake in both groups, we found that in the case group, the percentage of fat intake was significantly higher than the control group. The average intake of saturated fatty acids, monounsaturated fatty acids, linolenic acid and cholesterol was higher in the case group. In addition, the average intake of dairy products and vitamin B12 was observed to be higher in the case group. Further analysis of the data showed that the mean DII in the case group (0.95 ± SD) was significantly higher (P<0.001) than that in the control group (0.85± SD).
Discussion
Diets may play a role in the factors involved in cesarean section by altering systemic inflammation and the immune response. High oxidative stress in the placenta and inflammatory response were closely related to cesarean delivery (22).
Kyozuka et al. aimed to investigate the pro-inflammatory diet in pregnant women and its consequences in the pregnancy process and found that the pro-inflammatory diet during pregnancy may create the risk of intrapartum fetal Asphyxia, which is one of the indications for emergency cesarean section (23). On the other hand, inflammation before delivery affects the manner of delivery to cesarean section and increases bleeding afterward (20). Diet as an environmental factor can increase or decrease inflammation (24). Casas et al. examined the diets of 1028 pregnant women between 19 and 23 weeks of gestation and found a positive correlation between DII score and maternal BMI (25). DII is associated with inflammatory diseases such as multiple sclerosis, ulcerative colitis, and metabolic syndrome (26, 27). Natércia Paula Alves de Freitas et al. used DII as a tool to predict pregnancy outcomes in a systematic review in 2023, and the results indicated a direct correlation between DII and preeclampsia and premature delivery (28). An inflammatory diet with high DII scores is associated with an increased risk of GDM in pregnant women (29, 30).
Healthy diets are high in fruits and vegetables, which are high in antioxidants and fiber. Antioxidants play an important role as part of the defense mechanism against tissue damage caused by oxidants (31). Some components of the diet have antioxidant properties (32). Soluble fibers can be fermented in the gut to produce short-chain fatty acids that activate the GPR43 receptor, thereby stimulating the production of anti-inflammatory mediators (33).
High-quality diets during pregnancy were associated with lower diastolic blood pressure (34). Pregnancy hypertension or preeclampsia is one of the main risk factors for cesarean delivery (35). In a study including 75,432 pregnant women from Jan 1998 to Dec 2009, adverse pregnancy outcomes were associated with maternal obesity.
One of the adverse complications of the mother and fetus includes neonate death related to maternal BMI (20). In a cohort study on 3,772 pregnant women between 2010–2009 and 2012–2013, Jenny Bjorklund and colleagues investigated the effect of obesity on cesarean delivery after labor induction and concluded that higher BMI is directly related to increased risk of cesarean delivery after labor induction (36). Weight, BMI and waist circumference are significantly (P<0.001) higher in women who had a cesarean delivery compared to the control group.
A higher quality diet during pregnancy was associated with lower diastolic blood pressure (34). Consumption of vitamin C supplements in a group of 384 pregnant women reduces the hospitalisation time even if there is no access to fruit and vegetables (37). Changamir et al. conducted a study on 8468 pregnant women in 2015 and found that women who took multivitamins during pregnancy had better gestational weights, which is a significant predictor of birth weight (38). One of the strengths of our study was adjusting confounders such as age, total energy in-take, level of physical activity, social-economic status, marital status, and consumption of supplements. In addition, validated tools and questionnaires were used for gathering data.
Conclusion
Increased DII may increase the need for cesarean delivery. Further studies will help to examine the related mechanisms and effects in more detail.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The authors are grateful to the participants for their enthusiastic cooperation.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Boerma T, Ronsmans C, Melesse DY, et al. (2018). Global epidemiology of use of and disparities in caesarean sections. Lancet, 392 (10155):1341–1348. [DOI] [PubMed] [Google Scholar]
- 2.Betran AP, Ye J, Moller AB, et al. (2021). Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health, 6 (6): e005671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rafiei M, Saei Ghare M, Akbari M, et al. (2018). Prevalence, causes, and complications of cesarean delivery in Iran: A systematic review and meta-analysis. Int J Reprod Biomed, 16 (4):221–234. [PMC free article] [PubMed] [Google Scholar]
- 4.Mylonas I, Friese K. (2015). Indications for and Risks of Elective Cesarean Section. Dtsch Arztebl Int, 112 (29–30):489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Latifnejad Roudsari R, Zakerihamidi M, Merghati Khoei E. (2015). Socio-Cultural Beliefs, Values and Traditions Regarding Women’s Preferred Mode of Birth in the North of Iran. Int J Community Based Nurs Midwifery, 3 (3):165–76. [PMC free article] [PubMed] [Google Scholar]
- 6.Bernhardt GV, Shivappa P, Bernhardt K, et al. (2022). Markers of inflammation in obese pregnant women: Adenosine deaminase and high sensitive C - reactive protein. Eur J Obstet Gynecol Reprod Biol X, 16:100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stromsnes K, Correas AG, Lehmann J, et al. (2021). Anti-Inflammatory Properties of Diet: Role in Healthy Aging. Biomedicines, 9 (8):922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hébert JR, Shivappa N, Wirth MD, et al. (2019). Perspective: The Dietary Inflammatory Index (DII)-Lessons Learned, Improvements Made, and Future Directions. Adv Nutr, 10 (2):185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duggan MR, Butler L, Peng Z, et al. (2023). Plasma proteins related to inflammatory diet predict future cognitive impairment. Mol Psychiatry, 28 (4):1599–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou N, Xie ZP, Liu Q, et al. (2023). The dietary inflammatory index and its association with the prevalence of hypertension: A cross-sectional study. Front Immunol, 13:1097228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yarizadeh H, Mirzababaei A, Ghodoosi N, et al. (2021). The interaction between the dietary inflammatory index and MC4R gene variants on cardiovascular risk factors. Clin Nutr, 40 (2):488–495. [DOI] [PubMed] [Google Scholar]
- 12.Zuercher MD, Harvey DJ, Santiago-Torres M, et al. (2023). Dietary inflammatory index and cardiovascular disease risk in Hispanic women from the Women’s Health Initiative. Nutr J, 22 (1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi Y, Zhou W. (2023). Interactive Effects of Dietary Inflammatory Index with BMI for the Risk of Stroke among Adults in the United States: Insight from NHANES 2011–2018. J Nutr Health Aging, 27 (4):277–284. [DOI] [PubMed] [Google Scholar]
- 14.Aslani Z, Qorbani M, Hébert JR, et al. (2019). Association of Dietary Inflammatory Index with anthropometric indices in children and adolescents: the weight disorder survey of the Childhood and Adolescence Surveillance and Prevention of Adult Non-communicable Disease (CASPIAN)-IV study. Br J Nutr, 121 (3):340–350. [DOI] [PubMed] [Google Scholar]
- 15.Shivappa N, Wang R, Hébert JR, et al. (2019). Association between inflammatory potential of diet and risk of lung cancer among smokers in a prospective study in Singapore. Eur J Nutr, 58 (7):2755–2766. [DOI] [PubMed] [Google Scholar]
- 16.Zhao Q, Tan X, Su Z, et al. (2023). The Relationship between the Dietary Inflammatory Index (DII) and Metabolic Syndrome (MetS) in Middle-Aged and Elderly Individuals in the United States. Nutrients, 15 (8):1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Therdtatha P, Shinoda A, Nakayama J. (2022). Crisis of the Asian gut: associations among diet, microbiota, and metabolic diseases. Biosci Microbiota Food Health, 41 (3):83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chia AR, Chen LW, Lai JS, et al. (2019). Maternal Dietary Patterns and Birth Outcomes: A Systematic Review and Meta-Analysis. Adv Nutr, 10 (4):685–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borem P, de Cássia Sanchez R, Torres J, et al. (2020). A Quality Improvement Initiative to Increase the Frequency of Vaginal Delivery in Brazilian Hospitals. Obstet Gynecol, 135 (2):415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cierny JT, Unal ER, Flood P, et al. (2014). Maternal inflammatory markers and term labor performance. Am J Obstet Gynecol, 210 (5): 447.e1–6. [DOI] [PubMed] [Google Scholar]
- 21.Asghari G, Rezazadeh A Fau - Hosseini-Esfahani F, et al. (2012). Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr, 108 (6): 1109–17. [DOI] [PubMed] [Google Scholar]
- 22.Hu Y, Huang K, Sun Y, et al. (2017). Placenta response of inflammation and oxidative stress in low-risk term childbirth: the implication of delivery mode. BMC Pregnancy Childbirth, 17 (1):407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kyozuka H, Murata T, Fukuda T, et al. (2020). Dietary Inflammatory Index during Pregnancy and the Risk of Intrapartum Fetal Asphyxia: The Japan Environment and Children’s Study. Nutrients, 12 (11):3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Philippou E, Nikiphorou E. (2018). Are we really what we eat? Nutrition and its role in the onset of rheumatoid arthritis. Autoimmun Rev, 17 (11): 1074–1077. [DOI] [PubMed] [Google Scholar]
- 25.Casas R, Castro-Barquero S, Crovetto F, et al. (2022). Maternal Dietary Inflammatory Index during Pregnancy Is Associated with Perinatal Outcomes: Results from the IMPACT BCN Trial. Nutrients, 14 (11):2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Namazi N, Larijani B, Azadbakht L. (2018). Dietary Inflammatory Index and its Association with the Risk of Cardiovascular Diseases, Metabolic Syndrome, and Mortality: A Systematic Review and Meta-Analysis. Horm Metab Res, 50 (5): 345–358. [DOI] [PubMed] [Google Scholar]
- 27.Shivappa N, Hébert JR, Rashvand S, et al. (2016). Inflammatory Potential of Diet and Risk of Ulcerative Colitis in a Case-Control Study from Iran. Nutr Cancer, 68 (3): 404–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Freitas NPA, Carvalho TR, Gonçalves CCRA, et al. (2022). The Dietary Inflammatory Index as a predictor of pregnancy outcomes: Systematic review and meta-analysis. J Reprod Immunol, 152:103651. [DOI] [PubMed] [Google Scholar]
- 29.Denova-Gutiérrez EA-O, Muñoz-Aguirre P, Shivappa N, et al. (2018). Dietary Inflammatory Index and Type 2 Diabetes Mellitus in Adults: The Diabetes Mellitus Survey of Mexico City. Nutrients, 10 (4):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shivappa N, Wang R, Hébert JR, et al. (2019). Association between inflammatory potential of diet and risk of lung cancer among smokers in a prospective study in Singapore. Eur J Nutr, 58 (7):2755–2766. [DOI] [PubMed] [Google Scholar]
- 31.Demirci-Çekiç S, Özkan G, Avan AN, et al. (2022). Biomarkers of Oxidative Stress and Antioxidant Defense. J Pharm Biomed Anal, 209:114477. [DOI] [PubMed] [Google Scholar]
- 32.Huang D. (2018). Dietary Antioxidants and Health Promotion. Antioxidants (Basel), 7 (1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood LG, Shivappa N Fau, Berthon BS, et al. (2015). Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy, 45 (1): 177–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siregar DAS, Rianda D, Irwinda R, et al. (2020). Associations between diet quality, blood pressure, and glucose levels among pregnant women in the Asian megacity of Jakarta. PLoS One, 15 (11): e0242150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sukmawati S, Sunarno I, Arsyad MA, Idris I. (2020). Vaginal and cesarean section delivery with severe preeclampsia and preeclampsia with complications. Enfermería Clínica, 30:537–540. [Google Scholar]
- 36.Bjorklund J, Wiberg-Itzel E, Wallstrom T. (2022). Is there an increased risk of cesarean section in obese women after induction of labor? A retrospective cohort study. PLoS One, 17 (2):e0263685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hans U, Edward B. (2010). Regular vitamin C supplementation during pregnancy reduces hospitalization: outcomes of a Ugandan rural cohort study. Pan Afr Med J, 5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Changamire FT, Mwiru RS, Peterson KE, et al. (2015). Effect of multivitamin supplements on weight gain during pregnancy among HIV-negative women in Tanzania. Matern Child Nutr, 11 (3):297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]