Abstract
BACKGROUND
The impact of frailty on postoperative outcomes in patients undergoing hepatectomy is still unclear.
AIM
To study the influence of frailty on postoperative outcomes, such as mortality, rate of complications, and length of hospitalization, following hepatectomy.
METHODS
PubMed, EMBASE, and Scopus databases were searched for observational studies with adult (≥ 18 years) patients after planned/elective hepatectomy. A random-effects model was used for all analyses, and the results are expressed as weighted mean difference (WMD), relative risk (RR), or hazards ratio (HR) with 95% confidence interval (CI).
RESULTS
Analysis of the 13 included studies showed a significant association of frailty with elevated risk of in-hospital mortality (RR = 2.76, 95%CI: 2.10-3.64), mortality at 30 d (RR = 4.60, 95%CI: 1.85-11.40), and mortality at 90 d (RR = 2.52, 95%CI: 1.70-3.75) in the postoperative period. Frail patients had a poorer long-term survival (HR = 2.89, 95%CI: 1.84-4.53) and higher incidence of “any” complications (RR = 1.69, 95%CI: 1.40-2.03) and major (grade III or higher on the Clavien-Dindo scale) complications (RR = 2.69, 95%CI: 1.85-3.92). Frailty was correlated with markedly lengthier hospital stay (WMD = 3.65, 95%CI: 1.45-5.85).
CONCLUSION
Frailty correlates with elevated risks of mortality, complications, and prolonged hospitalization, which need to be considered in surgical management. Further research is essential to formulate strategies for improved outcomes in this vulnerable cohort.
Keywords: Frailty, Frail adults, Hepatic resection, Hepatectomy, Complications, Mortality, Survival, Clinical outcomes, Meta-analysis
Core Tip: This meta-analysis examined how frailty affects people undergoing liver surgery (hepatectomy). Findings from published studies were utilized to compare frail individuals to non-frail ones in terms of outcomes after hepatectomy. The findings show that frail individuals had higher mortality rates while in the hospital and within 30 d and 90 d after surgery, compared to non-frail individuals. Frail people also had lower long-term survival rates, experienced more complications, and had to stay in the hospital longer. These findings suggest that it is important to consider frailty when planning hepatectomy.
INTRODUCTION
Frailty, often characterized as a diminished physiological reserve and increased susceptibility to external stressors, is considered a significant determinant of postoperative outcomes[1-3]. Characteristic manifestations of frailty include diminished muscle mass, decreased physical activity, cognitive impairment, and nutritional deficits[4-6]. Frailty, therefore, was recognized as a significant risk factor for postoperative complications, prolonged hospitalization, increased readmission, and poorer functional outcomes following general surgical procedures[3,7,8]. With the gradual aging of the population, an increasing number of frail patients with comorbidities are being considered for major surgeries, including hepatectomy that emerged as a potentially curative treatment for primary and secondary hepatic malignancies[8-11].
The incidence of frailty among hepatectomy patients ranges from 15% to 30%[12,13]. However, a definitive connection between frailty and poorer postoperative outcomes in the context of hepatectomy is still not established.
This analysis aimed to investigate the relationship between frailty and postoperative outcomes following hepatectomy. The primary outcomes for the study included postoperative complications, length of hospital stay, and mortality/overall survival (OS) rates.
The findings of this review may be used to inform clinical practice and decision-making, such as risk stratification, and development of targeted pre- and postoperative interventions for this vulnerable group of patients undergoing hepatectomy.
MATERIALS AND METHODS
Search strategy
A comprehensive systematic search was done in PubMed, EMBASE, and Scopus databases up to August 15, 2023 using the following combination of terms: (Frailty OR muscle weakness OR sarcopenia OR frail elderly OR impaired muscle function OR frail older adults) AND (hepatectomy OR liver resection OR liver surgery OR hepatic surgery OR hepatic segmental resection) AND (clinical outcomes OR postoperative outcomes OR mortality OR survival OR complications). To ensure transparency and accountability, our protocol was registered with PROSPERO under registration number CRD42023456351, and PRISMA guidelines were followed[14].
Selection of studies
The inclusion criteria were as follows: (1) Observational (prospective and retrospective cohort and case-control) studies; (2) Studies with adult participants (18 years or older) undergoing planned/elective hepatectomy (either partial or complete); (3) Recognized tools used for frailty assessment; (4) Definition and categorization of frailty according to established criteria; (5) Studies with a comparator group of non-frail participants undergoing elective hepatectomy; (6) Studies with at least one of the following outcomes: Mortality, OS, postoperative complications, and length of hospital stay; and (7) Data sufficient for effect size calculation.
The exclusion criteria were as follows: (1) Case reports, case series, editorials, reviews, and conference abstracts; (2) Studies with participants aged < 18 years; (3) Studies that involved patients undergoing emergency hepatectomy; (4) Studies focusing exclusively on patients undergoing liver transplantation, as opposed to hepatectomy; and (5) Studies without a comparison group.
In cases of studies that resulted in more than one publication, data were taken from the most complete and recent publication.
Screening and selection
After executing the search strategy across three databases and assembling the initial pool of studies, duplicate entries were eliminated. Subsequently, two researchers examined the titles and abstracts of studies for their relevance to the research question(s), followed by the full-text examination of the shortlisted studies for eligibility. All differences were resolved by consensus or a consultation with the third author.
Quality assessment, data extraction, and analysis
The Newcastle-Ottawa Scale (NOS) was employed for study quality assessment[15], and two independent reviewers used a standardized data extraction form to systematically extract relevant data such as author's name, publication year, study location, number and characteristics of the participants, duration of follow-up, the operational definition of "frailty" employed, and the outcomes of interest. All differences were resolved by consensus or a consultation with the third author.
All statistical analyses were performed with STATA version 15.0. Data are reported as relative risk (RR) when the outcome is categorical and as weighted mean difference (WMD) when it is continuous. Survival outcomes after a long-term follow-up are expressed as hazards ratio (HR). All estimates included 95% confidence interval (CI). A random-effects model was used for all analyses. To evaluate potential publication bias, we utilized both Egger's test and funnel plots[16]. P < 0.05 was considered significant.
RESULTS
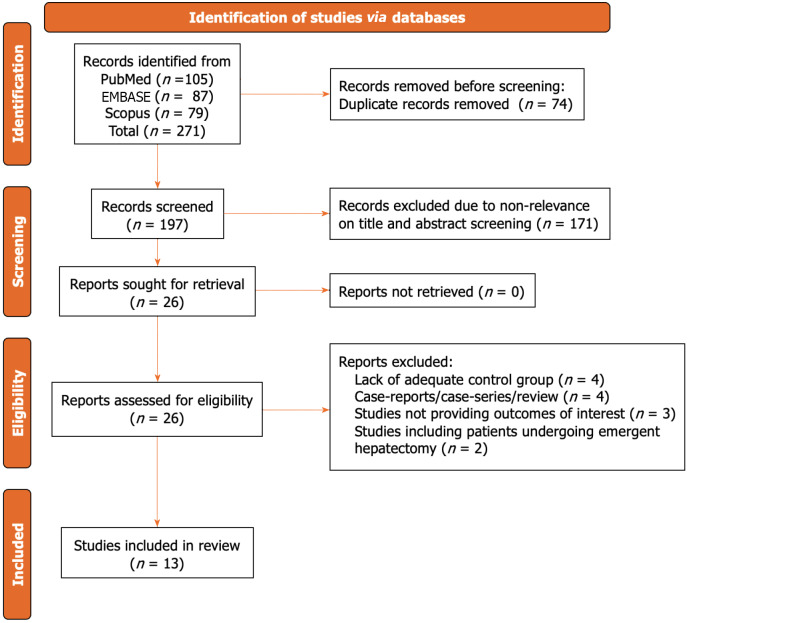
Our search strategy yielded a total of 271 studies. Of them, 74 duplicate papers were removed. Title and abstract screening eliminated 171 studies as not meeting the predetermined criteria, leaving 26 studies. After full-text examination, 13 studies were included in the final analysis[17-29]. The selection process is summarized in Figure 1.
Figure 1.
Selection process of studies included in the review.
As shown in Table 1, all studies, except two, were retrospective cohort ones. The remaining two studies were prospective. The majority of the studies were performed in the United States (n = 6) and Japan (n = 5). One study each was done in Canada and the United Kingdom. Male gender was prevalent in all studies, and the average age of patients was between 58 and 80 years. The indication for hepatectomy in the included studies was either primary hepatic malignancy or liver metastasis. Laparoscopic resection was done in two studies and open resection in five (Table 1). Other studies did not report on the mode of surgical intervention. We detected a substantial variability in the criteria used for the assessment of frailty. Even when similar assessment tools were used, the cut-offs considered for frailty differed. The tools to assess frailty included the Modified Frailty Index (mFI), the Clinical Frailty Scale (CFS), the Johns Hopkins Adjusted Clinical Groups (JHACG) frailty assessment, and the Kihon Checklist (KCL) tool[30-36]. mFI was used in six studies, CFS was used in four studies, JHACG was used in two studies, and one study used the KCL tool.
Table 1.
Summary of included studies
|
Ref.
|
Study design
|
Country
|
Subject characteristics
|
Definitions used for frailty
|
Sample size
|
Newcastle Ottawa quality score
|
| Okada et al[17], 2024 | Prospective cohort | Japan | Median age of 73 years; males (74%); indication for surgery - HCC; the majority with laparoscopic surgery (60.0%; proportion with laparoscopic surgery higher in non-frail subjects); extent of resection similar in two groups; no differences in age, sex, underlying hepatic diseases, or proportion of patients with comorbidities in two groups | Assessed using KCL tool (phenotypic frailty index; self-administered questionnaire comprising 25 items); score of ≥ 8 points - frail; score of < 7 points - non-frail | Frailty: 25; no frailty: 56 | 7 |
| Shahrestani et al[18], 2023 | Retrospective cohort | United States | Mean age of 62 years; males (51%); indication for surgery - liver metastasis; type of surgery not specified | JHACG frailty-defining diagnosis indicator was used. It uses 10 categories of ICD-10 codes to predict a patient’s frailty status | Frailty: 766; no frailty: 749 | 7 |
| Osei-Bordom et al[19], 2022 | Retrospective cohort | United Kingdom | Median age of 65.3 years; males (57%); most common indication for surgery - colorectal liver metastases followed by HCC; the majority undergoing open surgery (86.0%; proportion similar in two groups); extent of resection similar in two groups (P = 0.20); those classified as frail had increased BMI and prevalence of hypertension, diabetes, and COPD | MFI used: Patients stratified based on an mFI cut-off - frail (mFI ≥ 1) and robust (mFI = 0) | Frailty: 634; no frailty: 1192 | 8 |
| Hosoda et al[20], 2022 | Prospective cohort | Japan | Median age of 71 years; males (65%); indication for surgery - perihilar cholangiocarcinoma; type of surgery not specified; extent of resection similar in two groups; those with frailty had higher ASA classification; no differences in proportion of patients with comorbidities (hypertension and DM) in two groups | Assessed using CFS. Score of 3 to 9 points - frail; score of 1 to 2 points - non-frail | Frailty: 44; no frailty: 35 | 7 |
| Madrigal et al[21], 2022 | Retrospective cohort | United States | Mean age of 72 years; males (52%); most frail patients were male and had malignant liver disease as the indication for resection; compared with their non-frail counterparts, frail patients were older and had higher burden of comorbidities | JHACG frailty-defining diagnosis indicator | Frailty: 3655; no frailty: 37080 | 7 |
| Maegawa et al[22], 2022 | Retrospective cohort | United States | Patients underwent hepatectomy due to primary hepatobiliary cancer or secondary liver metastasis; open surgery in the majority (> 80%); mean age of 59 years; males (51%) | mFI-5: MFI = 0 indicated no frailty; mFI ≥ 1 indicated frailty | Frailty: 11687; no frailty: 12463 | 8 |
| Dauch et al[23], 2022 | Retrospective cohort | United States | Patients underwent minor hepatectomy; open surgery (82%); mean age of 58 years; males (58%); patients with frailty had higher ASA classification | mFI-5: MFI = 0 indicated no frailty; mFI ≥ 2 indicated frailty | Frailty: 654; no frailty: 2737 | 8 |
| Yamada et al[24], 2021 | Retrospective cohort | Japan | Mean age of 80 years; males (62%); similar burden of comorbidities (diabetes and hypertension) in two groups; primary indication for surgery - HCC; similar tumour characteristics in two groups; mean follow-up of 2.6 years | Assessed using CFS; score of ≥ 4 points - frail | Frailty: 21; no frailty: 71 | 7 |
| McKechnie et al[25], 2021 | Retrospective cohort | Canada | Patients with liver resection mainly due to HCC and colorectal cancer liver metastasis; median age of 64 years; females (45%); mean BMI of 28 kg/m2; laparoscopic resection (57%); median number of liver segments resected similar in two groups; patients with low mFI were younger, had lower ASA class, and were more likely to have > 4 METS on exercise tolerance testing, and less likely to be smokers | MFI used: Patients stratified based on an mFI cut-off - frail (mFI ≥ 0.27) and robust (mFI < 0.27) | Frailty: 58; no frailty: 351 | 7 |
| Tokuda et al[26], 2021 | Retrospective cohort | Japan | Mean age of 70 years; males (63%); burden of comorbidities (diabetes and hypertension) higher in frail group; primary indication for surgery - colorectal liver metastasis; mean follow-up of 46 mo | Assessed using CFS. Score of ≥ 4 points - frail | Frailty: 29; no frailty: 58 | 7 |
| Okabe et al[27], 2019 | Retrospective cohort | Japan | Mean age of 75 years; males (74%); indication for surgery - liver metastasis from colorectal cancer; mean BMI of subjects 23 kg/m2; type of surgery not specified; extent of resection similar in two groups | Assessed using CFS; score of ≥ 4 points - frail | Frailty: 16; no frailty: 127 | 6 |
| Chen et al[28], 2018 | Retrospective cohort | United States | Patients underwent liver and colorectal resection (for colorectal cancer with liver metastasis); open surgery (86%); mean age of 59 years; males (55%); patients with frailty were older, and had higher ASA classification, higher BMI, and greater number of comorbidities (hypertension, COPD, and DM) | 5-item mFI; mFI = 0 indicated no frailty; mFI ≥ 2 indicated frailty | Frailty: 225; no frailty: 1063 | 8 |
| Louwers et al[29], 2016 | Retrospective cohort | United States | Mean age of 58 years; males (49%); indication for surgery - primary hepatic malignancy and liver metastasis; open hepatectomy in the majority | MFI used: Patients stratified based on an mFI cut-off- frail (mFI ≥ 1) and robust (mFI = 0) | Frailty: 6150; no frailty: 4150 | 6 |
mFI: Modified frailty index; COPD: Chronic obstructive pulmonary disease; DM: Diabetes mellitus; ASA: American Society of Anaesthesia; BMI: Body mass index; CFS: Clinical Frailty Scale; METS: Metabolic equivalents; HCC: Hepatocellular cancer; mFI-5: 5-point Modified Frailty Index; JHACG: Johns Hopkins Adjusted Clinical Groups; ICD-10: International Classification of diseases-10; KCL: Kihon Checklist.
In most studies, the tumour characteristics and the extent of resection were similar in the two groups (frail and non-frail). However, frail patients had a higher baseline American Society of Anaesthesiology score, were older, and had a higher burden of comorbidities. The total number of patients included was 84096. Of them, 23964 were frail and 60132 were non-frail. Average NOS score of the studies was 7.2, with a maximal score of 9, indicating good quality (Table 1).
Mortality and OS
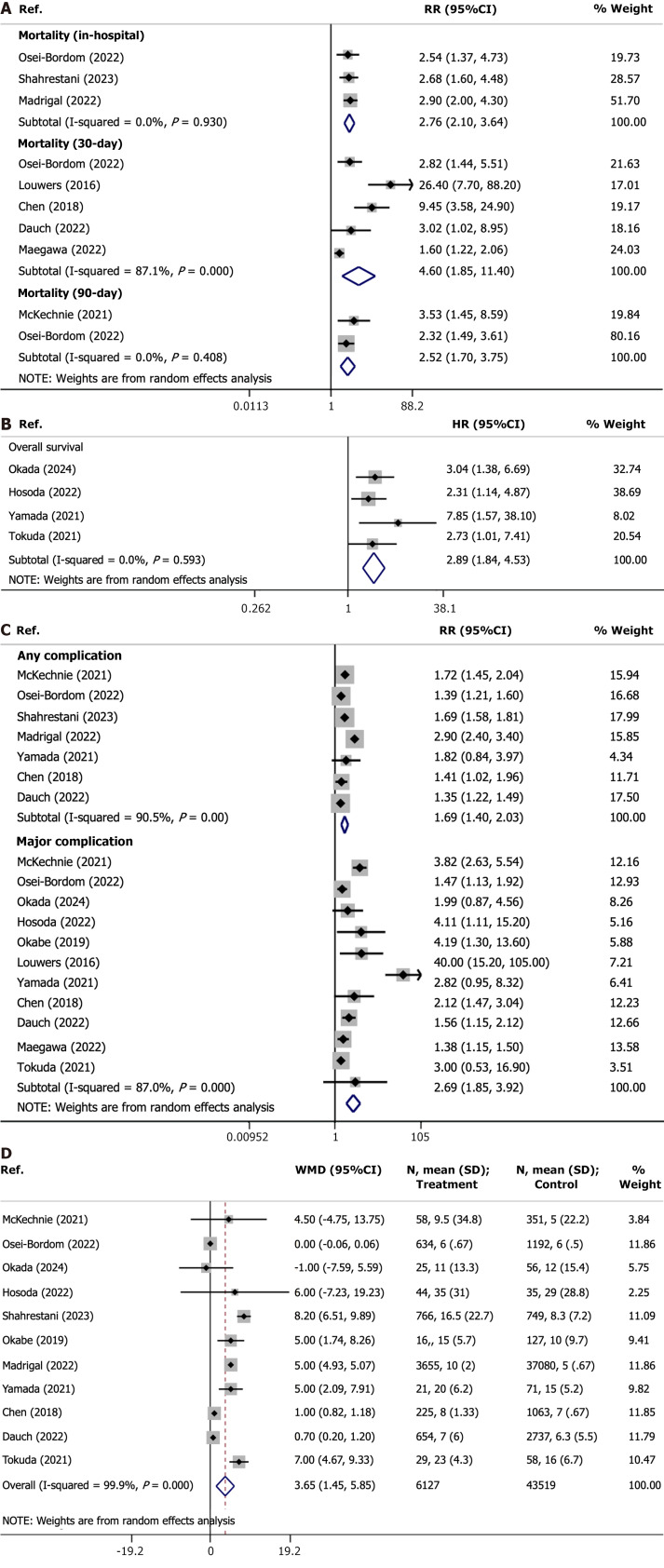
Frailty correlated with an increased incidence of in-hospital mortality (RR = 2.76, 95%CI: 2.10-3.64; n = 3, I2 = 0.0%), with some evidence of publication bias on Egger’s test (P = 0.036). Frail patients had a higher mortality at 30 d (RR = 4.60, 95%CI: 1.85-11.40; n = 5, I2 = 87.1%) and 90 d (RR = 2.52, 95%CI: 1.70-3.75; n = 2, I2 = 0.0%) in the postoperative period (Figure 2A). No evidence of bias was detected for mortality at 30 d (P = 0.164). Since only a small number of studies reported the risk of mortality at 90 d, Egger’s test could not be done. The funnel plots for mortality outcomes (in-hospital and 30-d) are shown in Supplementary Figures 1 and 2.
Figure 2.
Frail patients compared with non-frail subjects for mortality, survival, complications, and length of hospital stay. A: Risk of mortality; B: Overall survival (5-year); C: Risk of complications; D: Length of hospital stay (in days).
Frailty was associated with worse long-term survival (5-year OS) (HR = 2.89, 95%CI: 1.84-4.53; n = 4, I2 = 0.0%) in patients undergoing hepatectomy (Figure 2B), with no evidence of publication bias (P = 0.08; Supplementary Figure 3).
Complications and length of hospital stay
Frailty correlated with a higher rate of “any” complications (RR = 1.69, 95%CI: 1.40-2.03; n = 7, I2 = 90.5%) as well as major complications (as indicated by the Clavien-Dindo scale classification of grade III or higher) (RR = 2.69, 95%CI: 1.85-3.92; n = 11, I2 = 87.0%) (Figure 2C), with no publication bias detected for both outcomes (Supplementary Figures 4 and 5). Most common complications reported in the included studies were organ/space surgical site infection, post-hepatectomy hepatic failure, pneumonia, shock/sepsis, respiratory and renal complications, cardiac and cerebrovascular complications, bleeding requiring transfusion, and bile leak. Frail patients had significantly higher length (in days) of hospital stay (WMD = 3.65, 95%CI: 1.45-5.85; n = 11, I2 = 99.9%; Figure 2D).
DISCUSSION
This meta-analysis systematically evaluated the influence of frailty on postoperative outcomes following hepatectomy and showed that it was significantly associated with elevated risks of mortality, overall higher incidence of complications, and prolonged hospitalization. Our results further emphasize the significance of frailty assessment for optimizing patient care. A consistent association between frailty and adverse postoperative outcomes, elevated risks of short-term mortality, and poor long-term survival along with increased risk of complications underscore the consequences of reduced physiological reserves and increased susceptibility to operative stress.
Frail individuals often present with compromised cardiovascular, respiratory, and immune functions, which lowers their ability to endure the physiological strain of surgery and its aftermath[1,37,38]. This vulnerability might translate into increased susceptibility to postoperative complications, such as adverse cardiac events, respiratory failure, and infections, which may contribute to elevated mortality rates. The additional impact of frailty is linked to the disruption of the stress response that could lead to changed inflammatory status, impaired wound healing, and compromised tissue repair[39,40], which would may make frail subjects more prone to complications. Furthermore, the altered pharmacokinetics and drug metabolism, commonly associated with frailty due to changes in liver and kidney function, as well as changes in body composition, can compromise the effectiveness and safety of medications that are used during and after the surgery[41-43]. Subsequently, it may lead to adverse drug reactions, organ dysfunction, and ultimately poorer postoperative outcomes. Frail patients are also highly susceptible to infections that are associated with surgical procedures[40,44]. Compromised immune response in these patients predisposes them to developing postoperative infections, and increases the risk of mortality and long-term complications.
Notably, malnutrition and muscle wasting that accompanies frailty can impede wound healing, compromise immune function, and delay recovery[45,46]. Moreover, the diminished functional capacity, a characteristic of frailty, often results in a slower recuperation following surgical stress: Effective postoperative rehabilitation requires physical and functional recovery which is challenging for frail patients[47,48]. The resulting prolonged immobility ultimately leads to more complications and increased mortality rates observed in this vulnerable population. Lastly, underlying chronic comorbidities such as cardiovascular disease, diabetes, and respiratory disorders can further complicate surgical procedures and lead to more postoperative complications in frail patients[49-51].
Our study demonstrated that frail patients undergoing hepatectomy require longer hospital stays. Longer hospitalization puts a substantial burden on the healthcare system and the well being of patients and their families. Our results further underscore the importance of the integration of frailty assessment into the preoperative evaluation process for these patients. Collaborative approach and timely identification of frail patients will allow to develop tailored interventions that may optimize care, minimize associated adverse effects, and improve survival of frail patients undergoing hepatectomy.
Our study has limitations. First, the included studies had some variability in patient populations, operational techniques, and classifications of outcomes, which may have led to variability in the reported data. Variations in frailty assessment methods may have contributed to variability in the classification of frailty, which may have in turn influenced the strength of our analysis. Additionally, most included studies were retrospective, which increases the risk of selection bias in including frail patients for hepatectomy. Moreover, we could not account for such confounding factors as accompanying diseases of socioeconomic variables that might have certain impact on the outcomes. Only a few studies reported long-term follow-up data for survival outcomes, which prevented us from the comprehensive assessment of the interplay between frailty and long-term survival. Nevertheless, our study provided an important synthesis of the existing literature and highlights the need for standardized approaches to frailty assessment and further investigation into interventions aimed at improving outcomes for frail individuals undergoing hepatectomy.
CONCLUSION
Our results further underscore the predictive value of frailty in assessing the risk of poor postoperative outcomes following hepatectomy. We show that frailty is linked to increased risks of mortality, complications, and prolonged hospital stays. Our results further emphasize the need for comprehensive strategies for the unique needs of such patients. Assessment of frailty needs to be incorporated into clinical practice to enhance the quality of care, guide clinical decision-making, and improve overall surgical outcomes in frail patients undergoing hepatectomy.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Ghannam WM, Egypt S-Editor: Li L L-Editor: Wang TQ P-Editor: Zhang XD
Contributor Information
Yao-Jia Lv, Day Surgery Ward, Huzhou Central Hospital, The Affiliated Central Hospital of Huzhou University, Huzhou 313000, Zhejiang Province, China.
Guang-Xing Xu, School of Basic Medical Sciences, Zhejiang Chinese Medical University, Hangzhou 310053, Zhejiang Province, China.
Jia-Rong Lan, Department of Medicine, Huzhou Traditional Chinese Medicine Hospital Affiliated to Zhejiang Chinese Medical University, Huzhou 313000, Zhejiang Province, China. sdwaters@126.com.
References
- 1.Doody P, Lord JM, Greig CA, Whittaker AC. Frailty: Pathophysiology, Theoretical and Operational Definition(s), Impact, Prevalence, Management and Prevention, in an Increasingly Economically Developed and Ageing World. Gerontology. 2023;69:927–945. doi: 10.1159/000528561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ko FC. Preoperative Frailty Evaluation: A Promising Risk-stratification Tool in Older Adults Undergoing General Surgery. Clin Ther. 2019;41:387–399. doi: 10.1016/j.clinthera.2019.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panayi AC, Orkaby AR, Sakthivel D, Endo Y, Varon D, Roh D, Orgill DP, Neppl RL, Javedan H, Bhasin S, Sinha I. Impact of frailty on outcomes in surgical patients: A systematic review and meta-analysis. Am J Surg. 2019;218:393–400. doi: 10.1016/j.amjsurg.2018.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27:1–15. doi: 10.1016/j.cger.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bortz WM 2nd. A conceptual framework of frailty: a review. J Gerontol A Biol Sci Med Sci. 2002;57:M283–M288. doi: 10.1093/gerona/57.5.m283. [DOI] [PubMed] [Google Scholar]
- 6.Aubertin-Leheudre M, Woods AJ, Anton S, Cohen R, Pahor M. Frailty Clinical Phenotype: A Physical and Cognitive Point of View. Nestle Nutr Inst Workshop Ser. 2015;83:55–63. doi: 10.1159/000382061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beggs T, Sepehri A, Szwajcer A, Tangri N, Arora RC. Frailty and perioperative outcomes: a narrative review. Can J Anaesth. 2015;62:143–157. doi: 10.1007/s12630-014-0273-z. [DOI] [PubMed] [Google Scholar]
- 8.Mima K, Nakagawa S, Miyata T, Yamashita YI, Baba H. Frailty and surgical outcomes in gastrointestinal cancer: Integration of geriatric assessment and prehabilitation into surgical practice for vulnerable patients. Ann Gastroenterol Surg. 2023;7:27–41. doi: 10.1002/ags3.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang R, Wolfson M, Lewis MC. Unique Aspects of the Elderly Surgical Population: An Anesthesiologist's Perspective. Geriatr Orthop Surg Rehabil. 2011;2:56–64. doi: 10.1177/2151458510394606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becher RD, Vander Wyk B, Leo-Summers L, Desai MM, Gill TM. The Incidence and Cumulative Risk of Major Surgery in Older Persons in the United States. Ann Surg. 2023;277:87–92. doi: 10.1097/SLA.0000000000005077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papis D, Vagliasindi A, Maida P. Hepatobiliary and pancreatic surgery in the elderly: Current status. Ann Hepatobiliary Pancreat Surg. 2020;24:1–5. doi: 10.14701/ahbps.2020.24.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Komici K, Cappuccio M, Scacchi A, Vaschetti R, Delli Carpini G, Picerno V, Avella P, Brunese MC, Rengo G, Guerra G, Bencivenga L. The Prevalence and the Impact of Frailty in Hepato-Biliary Pancreatic Cancers: A Systematic Review and Meta-Analysis. J Clin Med. 2022;11 doi: 10.3390/jcm11041116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner D, DeMarco MM, Amini N, Buttner S, Segev D, Gani F, Pawlik TM. Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg. 2016;8:27–40. doi: 10.4240/wjgs.v8.i1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [cited 13 May 2024]. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okada T, Tanaka S, Shinkawa H, Ohira G, Kinoshita M, Amano R, Kimura K, Nishio K, Tauchi J, Uchida-Kobayashi S, Fujii H, Ishizawa T. Impact of frailty on long-term outcomes after liver resection for hepatocellular carcinoma in elderly patients: A prospective study. Asian J Surg. 2024;47:147–153. doi: 10.1016/j.asjsur.2023.05.139. [DOI] [PubMed] [Google Scholar]
- 18.Shahrestani S, Silverstein M, Nasrollahi T, Nasrollahi T, Maas M, Ugarte C, Kulkarni S, Lenz HJ, Genyk Y. The influence of frailty on perioperative outcomes in patients undergoing surgical resection of liver metastases: a nationwide readmissions database study. Ann Gastroenterol. 2023;36:333–339. doi: 10.20524/aog.2023.0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osei-Bordom D, Hall L, Hodson J, Joshi K, Austen L, Bartlett D, Isaac J, Mirza DF, Marudanayagam R, Roberts K, Dasari BV, Chatzizacharias N, Sutcliffe RP. Impact of Frailty on Short-Term Outcomes After Laparoscopic and Open Hepatectomy. World J Surg. 2022;46:2444–2453. doi: 10.1007/s00268-022-06648-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hosoda K, Shimizu A, Kubota K, Notake T, Masuo H, Yoshizawa T, Sakai H, Hayashi H, Yasukawa K, Soejima Y. Usefulness of frailty to predict short- and long-term outcomes in patients who have undergone major hepatectomy for perihilar cholangiocarcinoma. Ann Gastroenterol Surg. 2022;6:833–841. doi: 10.1002/ags3.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Madrigal J, Hadaya J, Lee C, Tran Z, Benharash P. Association of Frailty with Perioperative Outcomes Following Hepatic Resection: A National Study. J Am Med Dir Assoc. 2022;23:684–689.e1. doi: 10.1016/j.jamda.2022.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Maegawa FB, Ahmad M, Aguirre K, Elhanafi S, Chiba S, Philipovskiy A, Tyroch AH, Konstantinidis IT. The impact of minimally invasive surgery and frailty on post-hepatectomy outcomes. HPB (Oxford) 2022;24:1577–1584. doi: 10.1016/j.hpb.2022.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Dauch J, Hamidi M, Arrington AK, O'Grady CL, Hsu CH, Joseph B, Riall TS, Khreiss M. The Impact of Frailty on Patients Undergoing Liver Resection for Colorectal Liver Metastasis. J Gastrointest Surg. 2022;26:608–614. doi: 10.1007/s11605-021-05149-0. [DOI] [PubMed] [Google Scholar]
- 24.Yamada S, Shimada M, Morine Y, Imura S, Ikemoto T, Arakawa Y, Saito Y, Yoshikawa M, Miyazaki K. Significance of Frailty in Prognosis After Hepatectomy for Elderly Patients with Hepatocellular Carcinoma. Ann Surg Oncol. 2021;28:439–446. doi: 10.1245/s10434-020-08742-w. [DOI] [PubMed] [Google Scholar]
- 25.McKechnie T, Bao T, Fabbro M, Ruo L, Serrano PE. Frailty as a Predictor of Postoperative Morbidity and Mortality Following Liver Resection. Am Surg. 2021;87:648–654. doi: 10.1177/0003134820949511. [DOI] [PubMed] [Google Scholar]
- 26.Tokuda K, Morine Y, Miyazaki K, Yamada S, Saito YU, Nishi M, Ikemoto T, Shimada M. Frailty Can Predict Prognosis After Hepatectomy in Patients With Colorectal Liver Metastasis. Anticancer Res. 2021;41:4637–4644. doi: 10.21873/anticanres.15277. [DOI] [PubMed] [Google Scholar]
- 27.Okabe H, Hayashi H, Higashi T, Nitta H, Ikuta Y, Yusa T, Takeyama H, Ogawa K, Ozaki N, Akahoshi S, Ogata K, Osaki T, Baba H, Takamori H. Frailty Predicts Severe Postoperative Complication after Elective Hepatic Resection. Gastrointest Tumors. 2019;6:28–35. doi: 10.1159/000500086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen SY, Stem M, Cerullo M, Gearhart SL, Safar B, Fang SH, Weiss MJ, He J, Efron JE. The Effect of Frailty Index on Early Outcomes after Combined Colorectal and Liver Resections. J Gastrointest Surg. 2018;22:640–649. doi: 10.1007/s11605-017-3641-5. [DOI] [PubMed] [Google Scholar]
- 29.Louwers L, Schnickel G, Rubinfeld I. Use of a simplified frailty index to predict Clavien 4 complications and mortality after hepatectomy: analysis of the National Surgical Quality Improvement Project database. Am J Surg. 2016;211:1071–1076. doi: 10.1016/j.amjsurg.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 30.Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res. 2013;183:104–110. doi: 10.1016/j.jss.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 31.Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J Am Coll Surg. 2018;226:173–181.e8. doi: 10.1016/j.jamcollsurg.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Chimukangara M, Helm MC, Frelich MJ, Bosler ME, Rein LE, Szabo A, Gould JC. A 5-item frailty index based on NSQIP data correlates with outcomes following paraesophageal hernia repair. Surg Endosc. 2017;31:2509–2519. doi: 10.1007/s00464-016-5253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The Johns Hopkins ACG® System. Excerpt from technical reference guide. Nov, 2024. [cited 13 May 2024]. Available from: https://www2.gov.bc.ca/assets/gov/health/conducting-health-research/data-access/johns-hopkins-acg-system-technical-reference-guide.pdf .
- 35.Abrams C, Lieberman R, Weiner J. Development and evaluation of the Johns Hopkins University risk adjustment models for Medicare + Choice plan payment. Jun 6, 2003. [cited 13 May 2024]. Available from: https://www.hopkinsacg.org/document/development-and-evaluation-of-the-johns-hopkins-university-risk-adjustment-models-for-medicarechoice-plan-payment/
- 36.Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15:518–519. doi: 10.1111/ggi.12397. [DOI] [PubMed] [Google Scholar]
- 37.Clegg A, Young J. The frailty syndrome. Clin Med (Lond) 2011;11:72–75. doi: 10.7861/clinmedicine.11-1-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fried LP, Cohen AA, Xue QL, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1:36–46. doi: 10.1038/s43587-020-00017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng TP, Lu Y, Choo RWM, Tan CTY, Nyunt MSZ, Gao Q, Mok EWH, Larbi A. Dysregulated homeostatic pathways in sarcopenia among frail older adults. Aging Cell. 2018;17:e12842. doi: 10.1111/acel.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pansarasa O, Pistono C, Davin A, Bordoni M, Mimmi MC, Guaita A, Cereda C. Altered immune system in frailty: Genetics and diet may influence inflammation. Ageing Res Rev. 2019;54:100935. doi: 10.1016/j.arr.2019.100935. [DOI] [PubMed] [Google Scholar]
- 41.Cusack BJ. Pharmacokinetics in older persons. Am J Geriatr Pharmacother. 2004;2:274–302. doi: 10.1016/j.amjopharm.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Waring RH, Harris RM, Mitchell SC. Drug metabolism in the elderly: A multifactorial problem? Maturitas. 2017;100:27–32. doi: 10.1016/j.maturitas.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Hilmer SN, Kirkpatrick CMJ. New Horizons in the impact of frailty on pharmacokinetics: latest developments. Age Ageing. 2021;50:1054–1063. doi: 10.1093/ageing/afab003. [DOI] [PubMed] [Google Scholar]
- 44.Li H, Manwani B, Leng SX. Frailty, inflammation, and immunity. Aging Dis. 2011;2:466–473. [PMC free article] [PubMed] [Google Scholar]
- 45.Moradell A, Fernández-García ÁI, Navarrete-Villanueva D, Sagarra-Romero L, Gesteiro E, Pérez-Gómez J, Rodríguez-Gómez I, Ara I, Casajús JA, Vicente-Rodríguez G, Gómez-Cabello A. Functional Frailty, Dietary Intake, and Risk of Malnutrition. Are Nutrients Involved in Muscle Synthesis the Key for Frailty Prevention? Nutrients. 2021;13 doi: 10.3390/nu13041231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pourhassan M, Rommersbach N, Lueg G, Klimek C, Schnatmann M, Liermann D, Janssen G, Wirth R. The Impact of Malnutrition on Acute Muscle Wasting in Frail Older Hospitalized Patients. Nutrients. 2020;12 doi: 10.3390/nu12051387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, von Haehling S, Vandewoude MF, Walston J. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–397. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tornero-Quiñones I, Sáez-Padilla J, Espina Díaz A, Abad Robles MT, Sierra Robles Á. Functional Ability, Frailty and Risk of Falls in the Elderly: Relations with Autonomy in Daily Living. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17031006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weiss CO. Frailty and chronic diseases in older adults. Clin Geriatr Med. 2011;27:39–52. doi: 10.1016/j.cger.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 50.Pandey A, Kitzman D, Reeves G. Frailty Is Intertwined With Heart Failure: Mechanisms, Prevalence, Prognosis, Assessment, and Management. JACC Heart Fail. 2019;7:1001–1011. doi: 10.1016/j.jchf.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sinclair AJ, Abdelhafiz AH. Unravelling the frailty syndrome in diabetes. Lancet Healthy Longev. 2021;2:e683–e684. doi: 10.1016/S2666-7568(21)00256-7. [DOI] [PubMed] [Google Scholar]