Abstract
Background
An epidemic of Hepatitis E infection occurred in Kitgum district, northern Uganda in 2009. In that epidemic, more than 10,422 people were infected, and over 166 deaths were registered. Kitgum District Health Management Information Systems (HMIS) showed that Hepatitis E cases continued to occur in Mucwini more than in Kitgum Matidi sub-county despite instituting similar epidemic control measures in the two communities. The tenacity of the virus in Mucwini sub-county had remained unclear. This study aimed to assess communities’ views and perspectives on the differential prevalence of Hepatitis E in the two sub-counties of Kitgum Matidi and Mucwini in northern Uganda.
Methods
A mixed study using qualitative and quantitative methods was used. Four Focus group discussions and six key informant interviews were conducted with the village health teams, local council chairpersons, health workers, and community members. These participants were chosen purposively because of their expertise and experience in community health services. Face-to-face interview guides were administered to obtain detailed information on factors associated with the differential occurrence of Hepatitis E in the two sub-counties. This study was approved by a local IRB and the Uganda National Council of Science and Technology (UNCS&T).
Results
The most substantial findings were the differences in prevention and control practices in the two communities. Residents of Mucwini were less compliant with infection, prevention, and control guidelines, and disagreements between local councilors and village health teams in Mucwini over allowances led to poor implementation and non-adherence to guidelines on community control of the epidemic.
Conclusion
A differentially higher prevalence of Hepatitis E in Mucwini than in Kitgum Matidi resulted from poor personal and community hygiene and non-adherence to behavior change communication among residents of Mucwini than their counterparts in Kitgum Matidi. The authors recommend a more proactive approach to managing an epidemic by securing the willingness of the affected community to adopt appropriate infection prevention and control guidelines. In addition, disagreements among stakeholders should be resolved quickly so that all community members adhere to control measures.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13104-024-06869-7.
Keywords: Hepatitis E, Prevalence, Poor personal and community hygiene, Community disagreements
Introduction
Hepatitis E virus (HEV) is one of the five viruses that infect the liver and causes acute viral hepatitis [1]. This non-enveloped, positive-sense, single-stranded RNA (Ribonucleic acid) virus belongs to the herpesvirus genus that resembles calicivirus morphologically and organizationally on its 7.5 kb genome [1]. The “E” was chosen to illustrate its enteric, endemic, and epidemic qualities that captures its epidemiology [1]. “E” also made alphabetical sense because Hepatitis A, B, C, and D viruses had already been identified as causing hepatitis (liver inflammation) in humans [1]. According to the World Health Organization (WHO, 2001), the virus is spread in stools of infected persons and is primarily disseminated through fecal water or food [1, 2]. Hepatitis E is an acute gastrointestinal illness in people and is highly age-specific among persons between 15 and 45 years [3]. It has higher case fatality rates in women during their third trimester of pregnancy, which constitutes almost 30% of this specific group [4].
The risk factors of HEV infection are related to poor sanitation and shedding of the virus in feces [1]. Person-to-person transmissions are usually uncommon [1, 2]; however, predisposing factors include international travelers to different regions of the world where hepatitis E is endemic [1, 5]. In addition, catastrophe, refugees residing in overcrowded temporary camps, persons living with chronic liver diseases, and possibly persons working with non-human primates such as pigs, cows, sheep, donkeys, and goats are potential sources of the virus and significant risk factors [6].
The first documented cases of Hepatitis E in northern Uganda were described in Madi Opei sub-county in Lamwo district in 2007 [7]. The virus spread from Madi Opei to involve all the 19 sub-counties in the neighboring Kitgum district [7, 8]. More than 10,422 people were infected, and over 166 deaths were registered [8]. The case fatality rate in Kitgum district was reportedly 1.59% (Unpublished Hepatitis E surveillance report, 2008) [9]. The Authors suggested that the virus caused more morbidity and mortality in the Acholi sub-region than any other epidemic that occurred in Uganda. In addition, the virus also spread to neighboring districts of Amuru, Gulu, Pader, Kotido, Yumbe, and Kaabong in the north and northeastern Uganda [8].
The Kitgum district epidemic task force instituted interventions to address the identified risk factors for the virus in the community. These interventions included surveying to identify contaminated and unprotected water sources, sinking more boreholes, and initiating water chlorination at water collection points. Meanwhile, at household levels, distribution of jerrycans and soaps, digging more pit latrines, health education, hygiene, and supportive care, especially for pregnant women with severe clinical manifestations of the disease were done [8].
Kitgum Health Management Information Systems (HMIS) showed that Hepatitis E cases continued to occur more in some sub-counties than others despite instituting the same epidemic control measures in the district since the major Hepatitis E epidemic broke out in 2007 [8, 9]. The reasons for the persistence of the virus in some sub-counties had, by the time of this study, remained unclear.
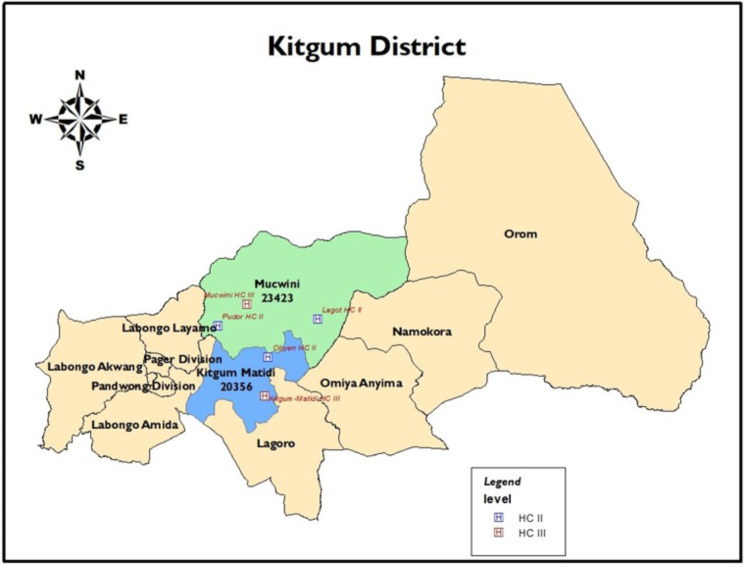
Figure 1 is a map of Kitgum district showing the two sub-counties of Mucwini (colored green) and Kitgum Matidi (colored Blue) where the study was conducted.
Fig. 1.
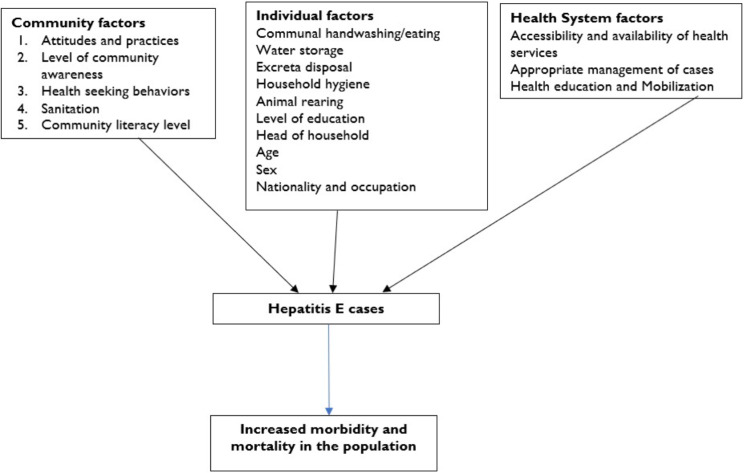
The conceptual framework on factors associated with the occurrence of Hepatitis E
This study aimed to assess communities’ views and perspectives on the differential prevalence of Hepatitis E in the two sub-counties of Kitgum Matidi and Mucwini.
Methodology
Study design
This was mixed study design where quantitative and qualitative data collection methods were used. This qualitative componet was part of a broader survey to determine factors associated with the differential occurrence of Hepatitis E in two sub-counties in Kitgum district.
Study settings
This study was conducted in the Mucwini and Kitgum Matidi sub-counties in Kitgum district. The district is bordered to the north by Lamwo district and South Sudan, east by Kaabong and Kotido districts, south by Pader and Agago districts, and west by Gulu and Amuru districts. The district has an estimated total population of 254,000 people. The district has one county, Chua, with ten sub-counties, 13 parishes, and 112 villages. Mucwini sub-county has a population of 23,423 inhabitants with nine parishes and 65 villages, while Kitgum Matidi has a population of 20,356 inhabitants with four parishes and 47 villages. The district has seven Health Centers II, eight Health Centers III, and two Health Center IV. It has one general hospital and one private and not-for-profit faith-based Hospital (FBH), St. Joseph’s Hospital, Kitgum. The general hospital has a 360-bed capacity, while the private not-for-profit St. Joseph’s hospital, Kitgum is a 250-bed.
The study population
Participants were the District Health Officer (DHO), In-charges of HC III, Chairpersons LC IIIs, Chairperson of LC1s, and the village health teams (VHTs) of the two sub-counties. The persons were selected because they understood and influenced the community’s socio-cultural, and health-related views. They had enormous knowledge on attitudes and practices on Hepatitis E in their communities. They had in-depth knowledge of the community settings and the occurrence of the virus. They were also critical stakeholders in implementing health-related policies and thus were well-placed to give solutions to persisting and emerging diseases.
Sampling
Participants for our study were selected purposively based on their in-depth knowledge and experience relevant to our research topic.
Field procedures. Key informant interviews (KIIs)
Participants of the KIIs were HC III in-charges of Mucwini and Kitgum Matidi, Local LC IIIs, and DHO of Kitgum District. A face-to-face interview guide was administered to these selected participants to obtain information on factors associated with the differential occurrence of Hepatitis E in the two sub-Counties. The interviews consist of a series of open-ended questions designed to draw out responses about the topic on our research. In addition, interviewer ensured that the conversation focussed on the topic while noting down key points and audio recording the conversation. At each step the interviwer ensured that there was a productive exchange of information.
Focus group discussions (FGDs)
Four FGDs were held with VHTs, and LC 1 Chairpersons. These participants were chosen because of their vast experience and expertise in clarifying relationships between the community and health services in addition to their ability to reflect on the general community’s perspectives and views. In Mucwini, FGDs were held at the sub-county headquarter. In contrast, Kitgum Matidi FGDs were held in the waiting room of HC III. The FGDs comprised 11–13 members, six females and seven males aged 25–37 years. All participants had attained at least primary seven education. Discussions were held in Acholi, guided by the principal investigator (PI), whom the two research assistants assisted. The team obtained written informed consent and noted the proceedings and other non-verbal expressions in notebooks. In addition, proceedings were audiotaped and recorded to provide backup information from participants.
Data collection methods and tools
The qualitative data were collected using key informant interviews (KIIs) using KII guides (Additional file A1) and focus group discussions (FGDs) using FGDs guides (Additional file A2). The key informant interview and focus group discussion guides were formulated based on the following criteria: (i) that it helps in establishing the purpose of the interview; (ii) that it helps to explain who is involved in the process (community members and leaders); (iii) to establish credibility for the interviews by the interviewers; (iv) to explain why interviewees’ cooperation is important for establishing the information required for the study. The PI moderated all meetings, and discussions and was assisted by research assistants who noted the meeting proceedings. Interviews and discussions lasted 45–60 min.
Data quality control
To collect quality data, research assistants were trained, were familiar with healthcare systems, had prior experience in data collection, and were identified by the DHO. In two days of training, research assistants were taught interviewing skills, correct recording of responses, and correct identification of respondents. The selection of participants emphasized strict adherence to procedures laid down in the proposal. Additionally, all data collection tools were translated into Acholi, the language most participants spoke. The KII and FGD guides were pre-tested among community members and results were used to moderate the flow and consistency of the instruments. The principal investigator (PI) administered these guides (Additional files A1 and A2) and was assisted by research assistants. In addition, the PI conducted interviews personally, by arranging, and completing data collection herself.
Data analysis
The primary data for this study were recorded (written and audio recorded) and analyzed using thematic narrative analysis [10, 11]. Thematic experience-centered narrative analysis was used to identify themes and sub-themes within the narratives [10, 11]. The researcher analyzed data manually because of the number of participants involved and the volume of information obtained. In the analysis process, the authors became familiar with the data by reading and re-reading all written materials and listening repeatedly to audio recordings from the interviews [10, 11]. The researchers then generated initial codes, searched for themes, reviewed them, and later defined and named the theme before reporting [10, 11]. Inductive coding was created based on the data, and labels were made as they emerged [10, 11]. Consequently, the analysis of experiences on infection, prevention, control (IPC), and differential occurrence of Hepatitis E was maintained inductive throughout the analysis process.
Credibility
The credibility of the study’s findings was ensured by establishing a data trail, acknowledging the researchers’ subjectivity, conducting participant checks and reviews, and ensuring prolonged engagements and follow-up of participants on the subject matter. The purpose of this study was made known to participants before interviews and a suitable venue was agreed before the study’s commencement. In addition, credibility was achieved by traingulating information from key informant interviews and focus group discussions conducted in the two sub-counties. Furthermore, responses from KIIs and FGDs were summarized, and critical quotes on IPC practices in the two sub-counties were included in the results.
Ethical approval
This study was approved by Makerere University School of Public Health Higher Degrees Research and Ethics Committee (MakSPHHRD&EC) and UNCS&T. Administrative approval was obtained from the DHO and Local Council III Chairpersons. Investigators explained the study’s purpose, risks, and benefits to community members before requesting them to participate. Each participant gave informed consent, and the team ensured the confidentiality of their personal information was preserved throughout and after the study. The research team ensured that the data collection tools did not record participants’ names but used unique identifiers.
Results
In this part of the study, four FGDs were conducted with LCs 1 and VHTs while KIIs were conducted with the DHO, In-charge of HC IIIs, and LC III chairpersons.
The prevalence of Hepatitis E in Mucwini and Kitgum Matidi sub-counties
According to the quantitative part of the study, 97(41.99%) participants from Mucwini had cases of Hepatitis E in their households compared to 63(26.47%) in Kitgum Matidi.
Table 1.
Two by two table showing proportion of households with a reported member of the family having Hepatitis E by sub-county
| Suffered from Hepatitis E | |||
|---|---|---|---|
| Sub County | No | Yes | Total |
| Kitgum Matidi | 175(73.53%) | 63(26.47%) | 238(100%) |
| Mucwini | 134(58.01%) | 97(41.99%) | 231(100%) |
| Total | 309(65.88% | 160(34.12%) | 469(100%) |
Table 1 shows a two-by-two table, and the reported prevalence of Hepatitis E which was higher in Mucwini sub-county 97(41.99%) than in Kitgum Matidi 63(26.47%) at 95% Confidence Interval (95% CI): χ2 = 1.61, 95%CI:1.39–1.87;p < 0.001
.
Findings from the qualitative study
This study analysed responses from participants on the differential occurrence of Hepatitis E in the two communities using KIIs and FGDs and structured them according to the themes, i.e. community, individual and health system’s factors.
Community factors
The differential prevalence of Hepatitis E in the two sub-counties was discussed by participants in KIIs and FGDs. The ranking of the most substantial health problems affecting the two sub-counties in 2011 were reviewed.
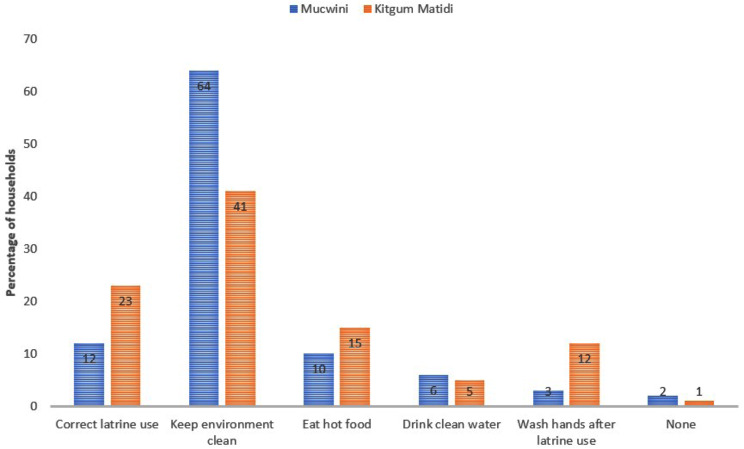
Hepatitis E prevention and practices in homesteads in Kitgum Matidi and Mucwini
The study showed that the number of homesteads that used pit latrine correctly, ate hot food, and washed hands after latrine use during the epidemic were higher in Kitgum Matidi than Mucwini. It was not surprising that a more substantial proportion of participants from Mucwini had not participated in proper Hepatitis E prevention practices than in Kitgum Matidi. In addition, communities from the two sub-counties responded differently to their communities’ infection, prevention, control, and practices to Hepatitis E. The differential occurrence of the virus appeared to be related to the community practices to the epidemic.
A VHT in a FGD from Mucwini said, “……….people in our community do not listen to what is always communicated. Other people up to now do not use pit latrines but go to the bushes for defecation, claiming that they have been recommended not to do hard work, for example, digging pit latrines in their homes.”
Another member in the same group from Mucwini lamented, “……the community is used to getting free items like they were previously in the Internally Displaced Peoples (IDP) camps where things were given free even items for digging, jerrycans and soap.”
The laxity in the use of pit latrines was mentioned as a challenge during the KII with the Mucwini sub-county local council III chairperson who said, “……………. latrine coverage in this sub-county is still low at 45%. Most residents share latrines or use bushes for defecation. Leaders (LC I) of communities are relaxed to enforce some byelaws because VHTs are better paid.”
During one of the FGDs, a VHT from Mucwini said, “we have been advising our community against communal hand washing during funerals and weddings, but the community here are resistant to these messages and continue to do so even during this epidemic.”
On the other hand, a VHT from Kitgum Matidi said, “We have advised the community against the practice of communal hand washings during ceremonies, and we see communities are following our advice during this epidemic. We are informed that communal hand washings only occur in homes among children before and after eating food”.
Figure 2 shows the percentages of homesteads that used pit latrines correctly, keep the environment clean, ate hot food, drank clean water, and washed their hands after latrine use. They were higher in Kitgum Matidi sub-county than Mucwini for most of the variables.
Fig. 2.
A map of Kitgum district showing Mucwini and Kitgum Matidi sub-counties
Individual factors
In one of the FGDs in Mucwini, one LC 1 Chairperson said, “we have advised community members to dig pit latrines, construct standby water stands near the latrines, and encouraged members to use them correctly. We were dismayed to learn that some members have refused to dig pit latrines in many communities and continued to use bushes. In addition, they do not wash their hands after latrine use”.
While in a FGD in Kitgum Matidi, a councilor said, “Ever since the Hepatitis E epidemic broke out here, many families have heeded the health advice and have dug many pit latrines in their homes and used them correctly. In addition, they constructed water points for hand washings after latrine use. The community’s response has been very encouraging, and this collaboration is helping us reduce the number of new cases of the virus”.
Health systems factors
During one of FGDs in the Mucwini, a VHT said, “We, in Mucwini have had problems during the implementation of this epidemic control measures. We should agree to be frank today, especially on issues that affect leaders and health workers. We have been informed that councilors were not supporting our efforts in community health education due to differences in allowances paid to VHTs. This has made us have conflicting messages to the population during this tough time, and community response is feeble.”
On the other hand, a VHT in Kitgum Matidi, in a FGD, said, “We have been having good meetings with the community, local leaders, and VHTs. These meetings have helped us control Hepatitis E virus in our community. The infection prevention and control messages have been taken up well by the community”.
The Chairperson, M1 said, “……………………….Hepatitis E was very serious, followed by malaria, chest infection, and HIV. Many pregnant women had stillbirths and miscarriages due to this yellow disease. Many people in my community resorted to local herbs and traditional healers for the solution.”
Their counterpart M2 said, “Respiratory infection, malaria, and abdominal complaints were major health-related problems affecting the sub-county. Hepatitis E did not affect many of us because the village health team and LC 1 Chairpersons worked hard together to sensitize the community.”
Discussion
This study showed a substantial difference in Hepatitis E control and practices among residents of Kitgum Matidi and Mucwini sub-counties. Residents of Kitgum Matidi were more likely to report better Hepatitis E infection, prevention, control, and practices than their counterparts in Mucwini (Fig. 3). This finding meant there were differences in risks of suffering from Hepatitis E among households in the two sub-counties even though they were in the same district (Fig. 3). The difference in the community prevalence and practices on Hepatitis E in the two communities correlated with reports from Kitgum District Health Management System (Unpublished HMIS report, Kitgum District, 2010) [8, 9] (Fig. 1).
Fig. 3.
Hepatitis E prevention and practices in Kitgum Matidi and Mucwini sub-Counties
Studies elsewhere demonstrated a difference in risk of acquiring Hepatitis E within socio-demographic characteristics, such as age and gender, and not in communities [12, 13]. A study conducted in a displaced population of Darfur found that more women were hospitalized compared to men [12]. This current study found no differences in the demographic characteristics of individuals within the two communities. Instead, it demonstrated a significant difference in the community prevalence and practices on Hepatitis E control and prevention (Fig. 2).
The factors associated with the differential prevalence were poor personal and community hygiene, low community awareness, and inadequate infection prevention, control, and practices on Hepatitis E (Figs. 3, 1 and 2). We found that hand washings after visiting latrines and the frequency of communal hand washings were associated with the differential prevalence of Hepatitis E in the two sub-counties.
In Kitgum Matidi, they were more likely to report hand washings after visiting latrines than Mucwini. This finding highlights the critical aspect of household hygiene in spreading Hepatitis E. This finding was consistent with another study in northern Uganda, where households with two or more cases of Hepatitis E were associated with a family member having attended a funeral, washed hands in communal basins with others during functions, and were likely not to have washed hands after visiting latrine [14]. Also, a study conducted in Lamwo district found that person-to-person transmission was highlighted as one of the factors that propagated the Hepatitis E epidemic secondary to contaminated water sources [14].
However, in this current study, the source of drinking water and storage facilities were not associated with the differential prevalence of Hepatitis E in the two sub-counties. Nevertheless, previous studies demonstrated that outbreaks were linked to contaminated water sources [15]. In addition, there were no associations between domestic animal keeping and the differential prevalence of Hepatitis E in the study population in the two sub-counties, although this contrasted with a study conducted in Chad [13].
The most substantial findings from this study were differences in adherence to infection, prevention, and control practices in the two communities involving improving the hygiene condition and provision of drinking water, as observed in another study [16]. Residents in Kitgum Matidi had better and more effective control prevention practices than Mucwini. Correct use of the latrine, eating hot food, drinking clean water, and washing hands after latrine use were the prevention interventions practiced by residents in Kitgum Matidi.
On the other hand, less than 10% of residents of Mucwini washed their hands after latrine use and drank clean water. These differences in Hepatitis E prevention practices in the two communities may have partly explained the observed differences in the community prevalence of Hepatitis E in the two sub-counties.
Disagreements among implementors of the prevention strategies in the Mucwini
Disturbing reports from the Mucwini showed that disagreements between stakeholders involved in managing the epidemic contributed to the poor response of the community and, therefore, a differentially higher prevalence of Hepatitis E in the Mucwini compared to Kitgum Matidi. This finding drew the authors’ attention, suggesting that indifferent messagings and disagreements between LCs and VHTs on the issue of personal benefits such as allowances significantly led to a higher prevalence of Hepatitis E in Mucwini. The Authors argue that had this problem been identified early by supervisors of epidemic response in the district, an amicable solution would have been achieved, and the unnecessary morbidity and mortality suffered by residents of Mucwini would have been averted or at least minimally experienced in the sub-county. These authors view that, had the district epidemic managers been on the ground, encouraged and practiced the principles of hand washings, and resolved disputes among stakeholders as quickly as possible in managing the epidemic, these higher numbers of cases would have been averted in Mucwini.
Resistance to behavior change communication messages in Mucwini Sub-county
The authors noted that residents of Mucwini were less receptive to behavior change communication messages during the management of the epidemic in their community. This was observed when residents preferred to participate in some selected activities but ignored health workers’ overall infection prevention and control guidelines. For example, residents continued to use bushes for defecation and refused to dig pit latrines in their homesteads. The authors reviewed this information and proposed that managers at the district should have adopted a modified approach to these situations. This occurrence would have involved the use and engagement of change agents, opinion leaders, local leaders, religious, and others who could influence behaviors of communities in Mucwini where there was evident resistance to health massages.
Adherence to traditional practices incompatible with the prevention and control of Hepatitis E
The research team found that traditional practices, such as communal hand washings during congregate functions continued in Mucwini during the epidemic. In addition, correct use of latrines and hand washings after latrine use was not practiced. Instead, residents of Mucwini preferred to defecate in the bushes and not wash their hands after latrine use. The Authors argue that the insistence on the use of traditional practices among residents of Mucwini during the epidemic may have, in part, contributed to a higher prevalence of Hepatitis E in Mucwini compared to Kitgum Matidi. These were confirmed from reports observed from the FGDs and KIIs.
The Authors suggest that in the future, opinion leaders, traditional leaders, and church leaders would be engaged in such undertakings when the need for modification of traditional practices was required. In addition, law enforcement would be necessary to bar residents from participating in actions that lead to persistent negative behaviors. This action was expected to cause the changes required to allow the community to overcome the Hepatitis E epidemic, adversely affecting them.
In summary, these authors argue that for an epidemic to be successfully managed, the community’s willingness to accept unembellished restrictions, forego their ways, and follow infection prevention and control guidelines is critical for successfully managing an epidemic [17, 18]. These became evidenced as residents of Mucwini did not follow IPC guidelines, with resultant persistent and higher prevalence of Hepatitis E in their communities.
Strengths and limitations of this study
This study based its report on qualitative information from DHO, local leaders, and health workers. The qualitative data were triangulated to ensure that the recorded data in the KIIs and FGDS were consistent and followed each other. Because they are qualitative information, their ability for generalizability in a broader context of a community where the study was conducted has limitations.
Conclusion
he differentially higher prevalence of Hepatitis E in Mucwini than Kitgum Matidi sub-county resulted from poor personal and community hygiene, and non-adherence to behavior change communication messages among residents of Mucwini than their counterparts in Kitgum Matidi. The authors recommend a more proactive approach to managing epidemics by securing the willingness of the affected community to adopt appropriate infection prevention and control guidelines. In addition, disagreements among stakeholders involved in epidemic management should be resolved quickly so that all members of the community adhere to the control measures.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the District Health Officer of Kitgum, Dr. Alex Olwedo, and the district health team for logistic field support throughout the data collection period. We thank the research assistants Mr. Ocitti Denis, Ms. Aciro Sarah, Ms. Anena Sunday, and Mr. Richard Amone, for the dedication exhibited during data collection.
Abbreviations
- DHO
District Health Officer
- FGDs
Focus Group Discussions
- HCs
Health Centers
- HEV
Hepatitis E virus
- HMIS
Health Managament Information Systems
- IDP
Internally Displaced Persons
- IPCs
Infection, prevention, and Control
- LCs
Local Councilors; KIIs: Key Informant Interviews
- MOH
Ministry of Health
- RNA
Ribo Nucleic Acid
- WHO
World Health Organization
- UNCST
Uganda National Council of Science and Technology
- VHTs
Village Health Teams
Biographies
Judith Aloyo
is a public health specialist and works as a Deputy Chief of Party at USAID, University Research Council (URC)-Rhites Acholi, Gulu City, Uganda.
Juliet Kiguli
is a lecturer at Makerere University School of Public Health, Kampala, Uganda.
Christopher Garimoi Orach
is a professor of Public health at Makerere University, School of Public Health, Department of Community and Behavioral Sciences, Kampala, Uganda.
David Lagoro Kitara
is a Professor at Gulu University, Faculty of Medicine, Department of Surgery, Gulu City, Uganda and a Takemi Fellow of the Harvard University, T.H. Chan School of Public Health and Populations.
Author contributions
JA, CGO, and JK designed the study. JA and DLK conducted fieldwork supervision. JA, CGO, JK, and DLK conducted data analysis, interpretation, writing, and manuscript revision.
Funding
We are sincerely grateful to PeriPeri for the financial support for this study. We, however, wish to state that Periperi did not participate in the design, collection, analysis, interpretation of data, and writing the manuscript for this study.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval and consent to participate
This study was approved by Makerere University School of Public Health Higher Degrees Research and Ethics Committee and the Uganda National Council of Science and Technology (UNCS&T). We, the authors confirm that all methods and experiments were performed in accordance with relevant institutional guidelines and regulations. In addition, administrative approval was obtained from the office of the District Health Officer of Kitgum District, Local Council III Chairpersons at the two sub-county headquarters. Informed consent was obtained from each participant for this study.
Consent for publication
All participants consented to the publication of this information.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arbeitskreis, Blut. Untergruppe Bewertung Blutassoziierter Krankheitserreger. Hepatitis E Virus. Transfus Med Hemother. 2009;36:40–7.21048820 [Google Scholar]
- 2.World Health Organization (WHO). Hepatitis E. Document WHO/CDSCSR/EDC/2002.12. Geneva, Switzerland. World Health Organization. 2001. Department of communicable disease surveillance and response, 2001.
- 3.San-Shwe. Myint-Myint-Soe. Epidemiological criteria and indication of non-A, non-B hepatitis in a community. Lancet. 1985;2:828. 10.1016/S0140-6736(85)90810-4 [DOI] [PubMed] [Google Scholar]
- 4.Skidmore SJ. Overview in the spread of Hepatitis E. Curr Infect Disease Rep. 2002;4(2):118–23. 10.1007/s11908-002-0051-x [DOI] [PubMed] [Google Scholar]
- 5.Strategic Advisory Group of Experts on Immunization (SAGE), Hepatitis E. Epidemiology and disease burden. 2014. https://www.who.int/immunization/sage/meetings/2014/october/1_HEV_burden_paper_final_03_Oct_14_yellow_book.pdf.
- 6.United Nations. UN and partners are working to control the spread of Hepatitis E in refugee camps in South Sudan. UN News Global Health perspective human stories. 2012. https://news.un.org/en/story/2012/09/419592.
- 7.Teshale EH, Howard CM, Grytdal SP, Epidemic H, et al. Uganda Emerg Infect Dis. 2010;16:126–9. 10.3201/eid1601.090764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Kitgum District Surveillance report on Hepatitis E; Health Management Information System report of Kitgum district. 2010. www.who.int.hac.crises.
- 9.WHO. Update on the Hepatitis E epidemic in Kitgum district. 2008. Kitgum district. Hepatitis E surveillance report. www.who.int/hac/crises/uga/sitreps/uganda_kitgum.
- 10.Riessman Catherine Kohler. Narrative analysis. In: Narrative, Memory & Everyday Life. Univ Hudders Hudders. 2005;1–7. http://eprints.hud.ac.uk/id/eprint/4920/.
- 11.Naderifar M, Goli H, Ghaljaie F. Snowball Sampling: a Purposeful Method of Sampling in qualitative research. Strides Dev Med Educ. 2017;14:e67670. 10.5812/sdme.67670. 10.5812/sdme.67670 [DOI] [Google Scholar]
- 12.Guthmann JP, Hilde K, Boccia D. A large outbreak of Hepatitis E among a displaced population in Darfur, Sudan 2004: the role of water treatment methods. Clin Infect Dis. 2006;42:1685–9. 10.1086/504321 [DOI] [PubMed] [Google Scholar]
- 13.Boccia D, Guthmann JP, Klovstad H, Hamid N. High mortality associated with an outbreak of Hepatitis E among displaced persons in Darfur, Sudan. Clin Infect Dis. 2006;42:1679–84. 10.1086/504322 [DOI] [PubMed] [Google Scholar]
- 14.Christopher MH, Thomas H, Vincent R, Hill SP. Novel risk factors associated with Hepatitis E virus infection in a large outbreak in northern Uganda, results from a case-control study and environmental analysis. Am J Trop Med Hyg. 2010;83(5):1170–3. 10.4269/ajtmh.2010.10-0384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vishwanathan R. Infectious Hepatitis E in New Delhi, 1955–1956 a critical study: Epidemiology. Indian J Med Res. 1957;45(suppl 1):1–29. [Google Scholar]
- 16.Eyasu H, Christopher MA, Scott P, Grytdal SP. Evidence of person-to-person transmission of Hepatitis E during a large outbreak in northern Uganda. Clin Infect Disease. 2010;50(7):1006–10. 10.1086/651077 [DOI] [PubMed] [Google Scholar]
- 17.Eyasu H, Teshale DJ, Hu, Scott D, Holmberg JM, Hughes, Mary E, Wilson. The two faces of the Hepatitis E virus. Clin Infect Disease. 2011;51:328–34. [DOI] [PubMed] [Google Scholar]
- 18.David Lagoro Kitara. Eric Nzirakaindi Ikoona. A proposed framework to limit post-lockdown community transmission of COVID-19 in Africa. Pan Afr Med J. 2021;38:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.