Abstract
Background:
Increased HIV testing efforts have resulted in retesting previously diagnosed persons. This study examined Centers for Disease Control and Prevention (CDC)–funded HIV testing programs to evaluate how the needs of previously diagnosed persons are being addressed.
Methods:
The following were examined by demographic and test setting among previously diagnosed HIV-positive persons in 2015: CDC-funded HIV testing, previously diagnosed HIV positivity, current care status, and linkage to care. In addition, trends of HIV positivity and previously diagnosed HIV-positivity were examined from 2011 to 2015.
Results:
In 2015, CDC funded 3,026,074 HIV tests, and 27,729 were HIV-positive tests. Of those, 13,528 (48.8%) were previously diagnosed persons. Only 11.6% of previously diagnosed persons reported already being in HIV care; after excluding them, 62.1% of previously diagnosed persons were linked within 90 days. In addition, the percentage of previously diagnosed persons steadily increased from 2011 (25.9%) to 2015 (34.1%; P < 0.001).
Conclusions:
Almost half of all HIV-positive tests were among previously diagnosed persons, but only 11.6% were already in HIV care. Linkage is necessary among persons who already know their HIV status because they either were never linked or need to be reengaged into care. Barriers in linkage and retention among this group also need to be addressed.
Approximately 1.1 million persons are living with HIV in the United States, including 15.0% of persons who did not know their status at the end of 2014.1 Each year, 30% of new HIV infections are transmitted by persons who are living with undiagnosed HIV.2 HIV testing efforts have been expanded to help identify HIV-positive persons who are unaware of their HIV-positive status. The Centers for Disease Control and Prevention (CDC) recommends routine HIV screening in health care settings where prevalence is greater than 0.01% for persons aged 13 to 64 years. Those who are at higher risk are encouraged to get tested more frequently.3 However, in addition to identifying new cases, increased testing efforts often result in retesting previously diagnosed HIV-positive persons. This indicates a potential gap in HIV testing and prevention programs because if previously diagnosed persons are being retested, they likely were never linked to HIV medical care, never engaged in medical care, or fell out of care and have not been reengaged.
Early diagnoses, linkage to HIV medical care, and retention in care are important for decreasing viral load and reducing morbidity and mortality among persons living with HIV.4,5 Once patients are linked and retained in care and on antiretroviral treatment, this leads to a decrease in viral load, decrease in HIV transmission to others, and ultimately a decrease in HIV incidence.4,6 However, despite the importance of engagement in HIV medical care, it has been estimated that only 40% of HIV-positive persons are engaged in care.7
Identifying potential gaps in CDC-funded testing programs is important, and this includes a better understanding of persons who have been previously diagnosed as having HIV but are retesting for HIV. The current analyses examined characteristics of previously diagnosed HIV-positive persons, current care and treatment status, and linkage to HIV medical care among CDC-funded HIV testing events (i.e., a single HIV testing event could include multiple tests to make a final determination of the test result; hereafter referred to as tests) in 2015.
MATERIALS AND METHODS
Data Source
The CDC funds 61 health department jurisdictions, which include the 50 states, District of Columbia, Puerto Rico, US Virgin Islands, and 8 directly funded city or county health departments, to provide HIV testing and other HIV prevention activities. Data for each CDC-funded HIV test are collected by local service providers and submitted without personal identifiers to CDC biannually via a secure, online CDC-supported system. The CDC uses these National HIV Prevention Program Monitoring & Evaluation data to monitor HIV testing and other HIV-related service delivery. Data for the testing period January 1 through December 31, 2015, that were submitted to CDC by March 17, 2016, were included in the current analyses. This data collection effort is considered a nonresearch, program evaluation activity by the CDC; therefore, approval from the institutional review board was not required.
Measures
Demographics and HIV Test Setting.
Measures are age, sex, race/ethnicity, and test setting. Only data on white, black/African American, and Hispanic/Latino persons are presented; other racial/ethnic groups were not examined because of a small sample size. The CDC requires the collection of risk behavior data to define target populations (e.g., gay, bisexual, and other men who have sex with men; i.e., MSM, persons who inject drugs) for all HIV tests in non–health care settings and for HIV-positive tests in health care settings. Therefore, data for target populations are only available for persons tested in non–health care settings. Data were stratified by HIV test setting (i.e., health care or non–health care). A health care setting is defined as one that provides both medical diagnostic and treatment services (e.g., inpatient facilities, outpatient facilities, and emergency departments). A non–health care setting is defined as one that does not provide both medical diagnostic and treatment services (e.g., HIV counseling and testing sites and community settings).
HIV Tests.
HIV tests included all National HIV Prevention Program Monitoring & Evaluation HIV testing records for which a test result (positive or negative) was reported. A single HIV testing event could include multiple tests that were administered to the same person to make a final determination of the test result.
Previously Diagnosed HIV Positivity.
Previously diagnosed HIV positivity included those who tested HIV positive during the current testing event and were found to be previously reported in the health department’s HIV surveillance system. In 2015, 37 health department jurisdictions checked more than 80% of their records against surveillance data. Self-report data for prior HIV-positive test result were used to determine prior HIV positive status for health department jurisdictions that did not or were unable to verify prior test results within their surveillance system because of specific policies within their state and/or health department. In that case, previously diagnosed persons were those who tested HIV positive during the current test event and also self-reported having a previous HIV-positive test result.
HIV Medical Care Status and Linkage to HIV Medical Care.
The percentage of persons who reported already being in HIV medical care was estimated. If not referred to HIV medical care, the reason for not being referred was assessed, which included the response that the person was already in HIV medical care. The percentage of persons with values other than already in HIV medical care was considered not in HIV medical care. In addition, linkage to HIV medical care within 90 days was examined for all previously diagnosed persons who did not report already being in care. Linkage was defined as attendance at first medical appointment. Grantees collect these data in various ways, including client self-report, provider report, medical records, surveillance data, or local program data.
Data Analysis Plan
Descriptive statistics were used to examine HIV testing, previously diagnosed HIV positivity, current HIV medical care status, and linkage among previously diagnosed persons by age, sex, race/ethnicity, target populations, and test setting in 2015. Log binominal regression analysis was used to assess differences across demographic characteristics for HIV positivity, previously diagnosed HIV positivity, current HIV medical care status, and linkage among previously diagnosed persons. Finally, estimated annual percent change analyses examined trends in previously diagnosed HIV positivity from 2011 to 2015. Analyses were conducted in SAS, version 9.3 (SAS, Inc, Cary, NC).
RESULTS
Previously Diagnosed HIV-Positive Persons
In 2015, 3,026,074 CDC-funded HIV tests were conducted. Of those, 27,729 were HIV positive and 13,528 were previously diagnosed HIV-positive persons (0.4% of all CDC-funded tests and 48.8% of all HIV-positive tests). Among all previously diagnosed persons, the following groups accounted for the highest percentage of previously diagnosed persons: male individuals (76.4%), persons tested in health care facilities (74.4%), blacks/African Americans (60.0%), MSM (41.4%), and persons aged 20 to 29 years (29.6%). When examining previously diagnosed HIV positivity by demographic characteristics and test setting, the highest positivity was among MSM (0.9%), persons aged 40 to 49 years (0.7%), persons 50 years and older (0.7%), and male individuals (0.7%; Table 1).
TABLE 1.
HIV Tests, Previously Diagnosed HIV-Positive Persons, and Linkage to HIV Medical Care Among Previously Diagnosed HIV-Positive Persons, 61 Health Department Jurisdictions in the United States, Puerto Rico and the US Virgin Islands, 2015
| Client Characteristics and Test Setting | HIV Tests | Previous Diagnosed HIV-Positive Persons* | Not in HIV Medical Care* | Linkage to HIV Medical Care in 90 d* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Col % | n | Col % | Row % | PR (95% CI) | n | Row % | PR (95% CI) | n | Row % | PR (95% CI) | |
| Age, y | ||||||||||||
| 13–19 | 221,338 | (7.3) | 216 | (1.6) | (0.1) | 0.29 (0.26–0.34) | 197 | (91.2) | 1.00 (0.96–1.05) | 134 | (68.0) | 1.09 (0.99–1.20) |
| 20–29 | 1,200,078 | (39.7) | 4005 | (29.6) | (0.3) | Referent | 3639 | (90.9) | Referent | 2276 | (62.5) | Referent |
| 30–39 | 721,244 | (23.8) | 3379 | (25.0) | (0.5) | 1.40 (1.34–1.47) | 3073 | (90.9) | 1.00 (0.99–1.02) | 1987 | (64.7) | 1.03 (1.00–1.07) |
| 40–49 | 409,127 | (13.5) | 2807 | (20.7) | (0.7) | 2.06 (1.96–2.16) | 2427 | (86.5) | 0.95 (0.93–0.97) | 1484 | (61.1) | 0.98 (0.94–1.02) |
| 50+ | 457,285 | (15.1) | 3098 | (22.9) | (0.7) | 2.03 (1.94–2.13) | 2602 | (84.0) | 0.92 (0.91–0.94) | 1528 | (58.7) | 0.94 (0.90–0.98) |
| Sex | ||||||||||||
| Male | 1,535,214 | (50.7) | 10,342 | (76.4) | (0.7) | 3.32 (3.19–3.46) | 9187 | (88.8) | 1.03 (1.01–1.04) | 5815 | (63.3) | 1.10 (1.06–1.14) |
| Female | 1,457,341 | (48.2) | 2953 | (21.8) | (0.2) | Referent | 2556 | (86.6) | Referent | 1475 | (57.7) | Referent |
| Race/Ethnicity | ||||||||||||
| White | 785,623 | (26.0) | 2347 | (17.3) | (0.3) | 0.48 (0.46–0.50) | 2156 | (91.9) | 1.07 (1.05–1.08) | 1444 | (67.0) | 1.12 (1.09–1.17) |
| Black/African American | 1,304,956 | (43.1) | 8115 | (60.0) | (0.6) | Referent | 6995 | (86.2) | Referent | 4166 | (59.6) | Referent |
| Hispanic/Latino | 647,773 | (21.4) | 2282 | (16.9) | (0.4) | 0.57 (0.54–0.59) | 2072 | (90.8) | 1.05 (1.04–1.07) | 1439 | (69.4) | 1.17 (1.13–1.21) |
| Target population in non-health care settings† | ||||||||||||
| MSM | 153,842 | (21.9) | 1422 | (41.4) | (0.9) | Referent | 1302 | (91.6) | Referent | 895 | (68.7) | Referent |
| Heterosexual men | 159,948 | (22.7) | 427 | (12.4) | (0.3) | 0.29 (0.26–0.32) | 401 | (93.9) | 1.03 (1.00–1.06) | 261 | (65.1) | 0.95 (0.87–1.03) |
| Heterosexual women | 154,598 | (22.0) | 330 | (9.6) | (0.2) | 0.23 (0.20–0.26) | 312 | (94.5) | 1.03 (1.00–1.06) | 224 | (71.8) | 1.04 (0.97–1.13) |
| Persons who | 42,152 | (6.0) | 232 | (6.8) | (0.6) | 0.60 (0.52–0.68) | 203 | (87.5) | 0.96 (0.91–1.01) | 115 | (56.7) | 0.82 (0.73–0.93) |
| inject drugs‡ | ||||||||||||
| Setting | ||||||||||||
| Health care facilities | 2,313,742 | (76.5) | 10,066 | (74.4) | (0.4) | Referent | 8772 | (87.1) | Referent | 5352 | (61.0) | Referent |
| Non-health care facilities | 703,890 | (23.3) | 3434 | (25.4) | (0.5) | 1.12 (1.08–1.17) | 3160 | (92.0) | 1.06 (1.04–1.07) | 2056 | (65.1) | 1.07 (1.03–1.10) |
| Total | 3,026,074 | (100.0) | 13,528 | (100.0) | (0.4) | 11,959 | (88.4) | 7421 | (62.1) | |||
The denominator for previously diagnosed HIV-positive persons is HIV tests. The denominator for not in HIV medical care is previously diagnosed HIV-positive persons. The denominators for the linkage variables are previously diagnosed HIV-positive persons, excluding those who are already in HIV medical care.
Data to identify target populations are required for all tests conducted in non–health care settings but are only required for HIV-positive persons from health care settings.
Includes all injection drug users in non–health care settings, including those who identified as MSM, heterosexual men, or heterosexual women.
If not referred to HIV medical care, the reason for not being referred was assessed, which included the response that the person was already in HIV medical care. The percentage of persons with values other than already in HIV medical care was considered not in HIV medical care.
Significant findings from log binomial regression analyses indicated that persons aged 20 to 29 years (0.3%) were more likely to have a higher percentage of previous diagnoses than persons aged 13 to 17 years (0.1%), but less likely than persons aged 30 to 39 years (0.5%) and those 40 years and older (0.7%). Male individuals (0.7%) were more likely to have a higher percentage of previous diagnoses than female individuals (0.2%). In addition, blacks/African Americans (0.6%) were more likely to have a higher percentage of previous diagnoses than whites (0.3%) and Hispanics/Latinos (0.4%). Men who have sex with men (0.9%) were more likely to have a higher percentage of previous diagnoses than heterosexual men (0.3%), heterosexual women (0.2%), and persons who inject drugs (0.6%). Finally, although health care facilities tested 74% of persons with a previous diagnoses, when examining the percentages in each health care facility, non–health care facilities (0.5%) were more likely to identify persons with a previous diagnosis than health care facilities (0.4%; Table 1).
HIV Medical Care
With regard to HIV medical care, 88.4% of previously diagnosed HIV-positive persons reported that they were not already in HIV medical care. By client characteristics and test setting, the percentages of previously diagnosed persons who were not already in care ranged from 84.0% to 94.5%. The highest percentages for those not in HIV care were among heterosexual women (94.5%), heterosexual men (93.9%), and persons tested in non–health care settings (92.0%). In other groups, percentages were also still very high and included the following groups: persons 50 years and older (84.0%), blacks/African Americans (86.2%), and persons aged 40 to 49 years (86.5%; Table 1).
Significant findings from log binomial regression analyses indicated that previously diagnosed persons aged 20 to 29 years (90.9%) were more likely not to be in HIV medical care than previously diagnosed persons aged 40 to 49 years (86.5%) and persons 50 years and older (84.0%). In addition, previously diagnosed whites (91.9%) and Hispanics/Latinos (90.8%) were more likely not to be in HIV medical care than blacks/African Americans (86.2%). However, it was noteworthy that the number of previously diagnosed blacks/African Americans who were not in HIV medical care (6995) was much higher than whites (2156) and Hispanics/Latinos (2072). Finally, previously diagnosed persons who were tested in non–health care facilities (92.0%) were more likely to report that they were not in HIV medical care than those tested in health care facilities (87.1%). There were no significant differences among the target population groups (Table 1).
Linkage to HIV Medical Care
After excluding those who reported being in HIV medical care (1569; 11.6%), 62.1% were linked within 90 days after the current testing event (Table 1). Significant findings from log binomial regression analyses indicated that previously diagnosed persons aged 20 to 29 years (62.5%) were more likely to be linked within 90 days than persons 50 years and older (58.7%). Previously diagnosed male individuals (63.3%) were more likely to be linked than female individuals (57.7%). In addition, blacks/African Americans (59.6%) were less likely to be linked than whites (67.0%) and Hispanics/Latinos (69.4%). Men who have sex with men (68.7%) were more likely to be linked than persons who inject drugs (56.7%). Finally, previously diagnosed persons tested in health care facilities (61.0%) were less likely to be linked than those who tested in non–health care facilities (65.1%; Table 1).
Previously Diagnosed HIV-Positive Persons, 2011 to 2015
From 2011 to 2015, the percentage of previously diagnosed HIV-positive persons significantly increased by an estimated annual percent change of 7.15% from 2011 (25.9%) to 2015 (34.1%; P < 0.001). In addition, the number of previously diagnosed has steadily increased from 2011 to 2015 (Fig. 1).
Figure 1.
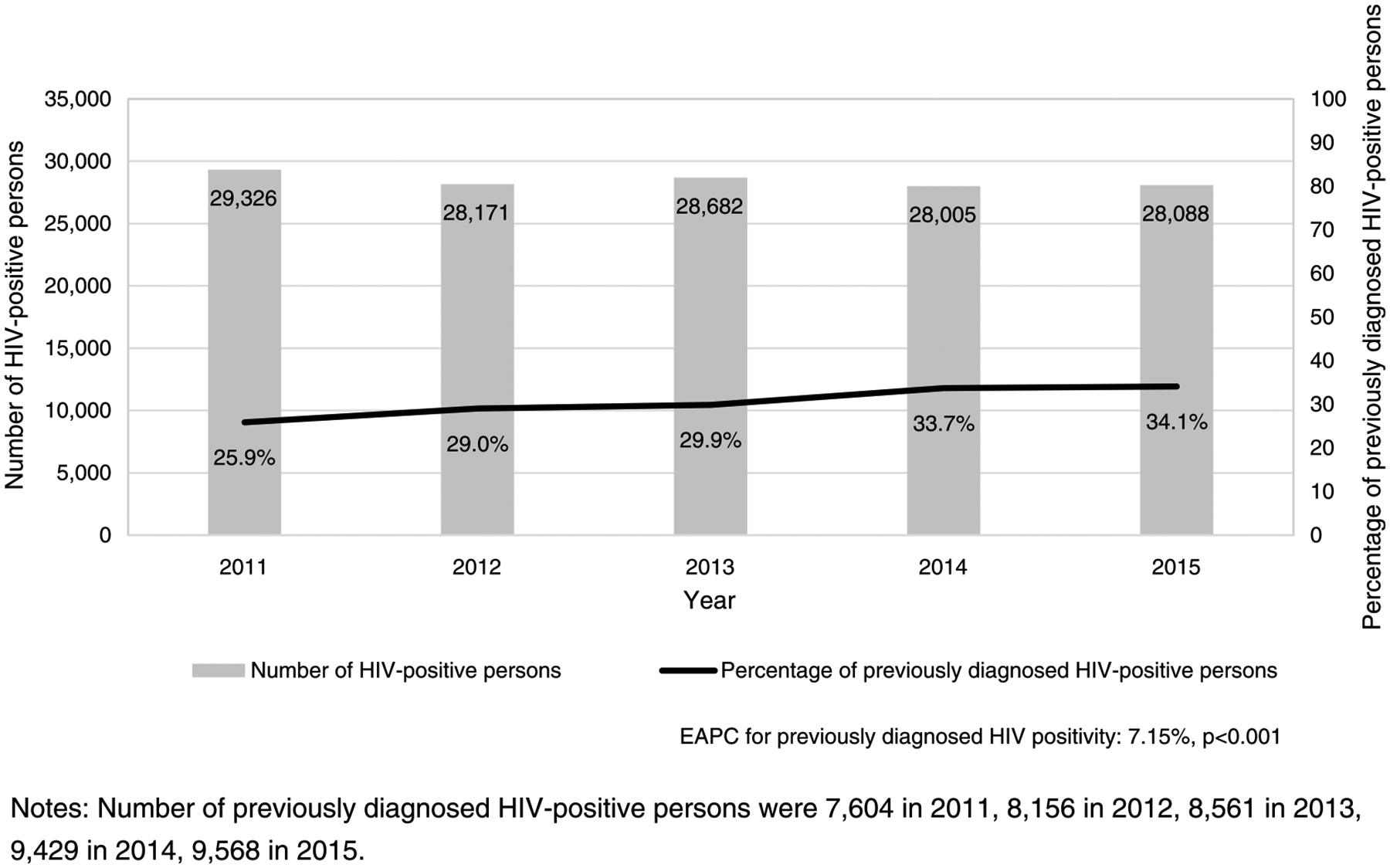
Number of HIV-positive persons and percentage of previously diagnosed HIV-positive persons in the United States, Puerto Rico, and US Virgin Islands, 2011 to 2015.
DISCUSSION
In 2015, nearly half of CDC-funded HIV-positive tests were among persons who were previously diagnosed, and of those, almost 90% were not in HIV medical care. After excluding those who were already in care, less than two thirds of previously diagnosed HIV-positive persons were linked within 90 days of the current testing event. Although blacks accounted for less than half of all HIV tests, they accounted for almost two thirds of persons who were identified as previously diagnosed. One possible reason that HIV-positive persons are testing a second time is doing so as a means to get engaged or reengaged in care. Linkage to HIV medical care is crucial for those previously diagnosed persons who were either never linked to care or need to be reengaged into care in order for them to reduce viral load and achieve better health outcomes. HIV prevention programs should offer previously diagnosed persons dedicated behavioral and health services to address the barriers that may be impacting linkage and engagement in care. Although likely available through surveillance data, it is unknown when these persons may have been first diagnosed or first infected with HIV through the programmatic data used for analyses. However, a very small percentage of previously diagnosed HIV-positive persons reported already being in HIV medical care at the time of the current test. This is of primary concerns because this decreases the likelihood of viral suppression and improved health outcomes among this group and increases the likelihood of HIV transmission to partners.8
The primary goals of CDC-funded HIV testing programs are to increase persons’ awareness of their HIV status and to immediately link those with a positive test result to HIV care. Although HIV testing programs have historically been designed to provide services to those who were unaware of their HIV status, data from CDC-funded HIV testing programs indicate that many clients who access testing services are already aware of their HIV-positive status. In addition, trends indicated that the number of previously diagnosed HIV-positive persons has been steadily increasing since 2011. It is important to gain more understanding about the reasons for retesting among persons with a prior HIV diagnosis, but perhaps more important is to recognize this pattern as an opportunity for intervention. Findings indicate that very few persons who were previously diagnosed as having HIV and accessed CDC-funded HIV testing services were in care at the time they were tested. Because they are not in care, these persons may be in need of immediate and perhaps more intensive linkage services than those receiving a new diagnosis, given that they have some history of not accessing HIV care at initial diagnosis or having fallen out of care. Similar to Data to Care strategies,9 HIV testing programs may serve as unexpected but important and efficient gateways for identifying persons living with HIV and linking or reengaging them into care.
The current findings are subject to limitations. The percentage of persons reported as currently not being in HIV medical care may be overestimated because of methodological limitations, because this question was assessed in response to not being referred to HIV medical care during that testing appointment. When assessing whether persons were “not in HIV medical care,” HIV medical care was not explicitly defined. Therefore, there may have been varying interpretations of what was meant by “out of care.” If the person was ever engaged in care, it is not clear how long she/he may have been out of care. It is possible that although out of care, certain persons may have been virally suppressed (e.g., if out of care for 3 months). A more refined measure to measure current HIV medical care status is needed.
In addition, data are limited to CDC-funded HIV tests, and reliable estimates are not available to determine what proportion of all HIV tests in the United States are CDC funded. Similarly, risk data to define target populations are only required to be collected from HIV-positive persons tested in health care settings but are required for all persons tested in non–health care settings. Therefore, the true number of CDC-funded tests and the HIV positivity cannot be determined for risk groups. As a result, findings on risk groups are only presented for persons tested in non–health care setting. Thus, findings are not generalizable to the US population.
Moreover, because of missing data, linkage data represent the minimum percentage achieved and are likely an underestimate of the true linkage values achieved. Because of client protections associated with the Health Insurance Portability and Accountability Act, non–health care settings are not always able to determine if an HIV-positive client was linked into HIV medical care, resulting in missing data. However, significant improvements in the quality and completeness of program data have been seen each year.10–13
Finally, previous diagnoses were based on self-report data for health departments that are unable to verify prior HIV status from their HIV surveillance system. Therefore, the percentage of previous diagnoses may be an underestimate because of self-report bias and because some HIV testing programs may offer incentives for getting tested.
CONCLUSIONS
Barriers to linkage and retention efforts for persons living with HIV need to be addressed, and programmatic efforts may need to be scaled up to ensure that HIV-positive persons are engaged and retained in care and treatment. The CDC has recommended that surveillance data be used to identify persons who need to be reengaged into care (i.e., data to care).9,14 However, a gap in best practices remains, which contributes to the challenges that many programs may face. A recent systematic review on linkage, retention, and reengagement in care did not identify any evidence-based interventions that focused on reengagement.14 However, HIV testing programs allow for the identification of newly diagnosed HIV-positive persons as well as previously diagnosed persons who may have fallen out of care. This provides another opportunity to link HIV-positive persons in HIV care. Regardless of CD4 count, it is recommended that HIV-positive persons initiate treatment soon after learning of their HIV status not only for their own benefit but also to prevent transmission to HIV-negative partners.15 The needs and challenges with linking newly diagnosed and previously diagnosed persons may differ, requiring programs to be strategic in their program planning.
Acknowledgments:
The authors thank Samuel Dooley, MD, and the Prevention Program Branch at the Centers for Disease Control and Prevention for monitoring the HIV testing programs.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest and Sources of Funding: None declared.
REFERENCES
- 1.Singh S, Song R, Satcher Johnson A, et al. HIV incidence, prevalence, and undiagnosed injections in men who have sex with men. Paper presented at: Conference on Retroviruses and opportunities infections 2017; Seattle, WA. Available at: http://www.hivdent.org/_CROI2017/HIV%20Incidence.pdf. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Testing 2016. Available at: https://www.cdc.gov/hiv/testing/index.html. Accessed April 9, 2017.
- 3.Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55:1–17. [PubMed] [Google Scholar]
- 4.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365: 493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Insight Start Study Group, Lundgren JD, Babiker AG, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 2015; 373:795–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gardner EM, McLees MP, Steiner JF, et al. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011; 52:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley H, Hall HI, Wolitski RJ, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR 2014; 63:1–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen MS, Muessig KE, Smith MK, et al. Antiviral agents and HIV prevention: Controversies, conflicts, and consensus. AIDS 2012; 26: 1585–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Data to care: Improving health and prevention. 2017. Available at: https://effectiveinterventions.cdc.gov/en/HighImpactPrevention/PublicHealthStrategies/DatatoCare.aspx. Accessed April 9, 2017.
- 10.Centers for Disease Control and Prevention. HIV Testing at CDC Funded Sites, United States, Puerto Rico and the U.S. Virgin Islands, 2011. 2013. Available at: http://www.cdc.gov/hiv/library/reports/index.html. Accessed March 2, 2016.
- 11.Centers for Disease Control and Prevention. CDC-Funded HIV Testing: United States, Puerto Rico, and the U.S. Virgin Islands, 2012. 2014. Available at: http://www.cdc.gov/hiv/pdf/2012_HIV_Testing_Report_01-29-15.pdf. Accessed March 2, 2016.
- 12.Centers for Disease Control and Prevention. CDC-Funded HIV Testing: United States, Puerto Rico and the U.S. Virgin Islands, 2013. 2015. Available at: http://www.cdc.gov/hiv/pdf/library/reports/cdc-hiv-CDCFunded_HIV_Testing_UnitedStates_Puerto_Rico_USVI_2013.pdf Accessed March 2, 2016.
- 13.Centers for Disease Control and Prevention. CDC-Funded HIV Testing: United States, Puerto Rico and the U.S. Virgin Islands, 2014. 2016. Available at: http://www.cdc.gov/hiv/library/reports/index.html. Accessed June 25, 2016.
- 14.Higa DH, Crepaz N, Mullins MM, et al. Identifying best practices for increasing linkage to, retention, and re-engagement in HIV medical care: Findings from a systematic review, 1996–2014. AIDS Behav 2016; 20:951–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eholié SP, Badje A, Kouame GM, et al. Antiretroviral treatment regardless of CD4 count: The universal answer to a contextual question. AIDS Res Ther 2016; 13:27. [DOI] [PMC free article] [PubMed] [Google Scholar]


