Abstract
Introduction:
Changes in food production and distribution have increased opportunities for foods contaminated early in the supply chain to be distributed widely, increasing the possibility of multistate outbreaks. In recent decades, surveillance systems for foodborne disease have been improved, allowing officials to more effectively identify related cases and to trace and identify an outbreak’s source.
Materials and Methods:
We reviewed multistate foodborne disease outbreaks reported to the Centers for Disease Control and Prevention’s Foodborne Disease Outbreak Surveillance System during 1973–2010. We calculated the percentage of multistate foodborne disease outbreaks relative to all foodborne disease outbreaks and described characteristics of multistate outbreaks, including the etiologic agents and implicated foods.
Results:
Multistate outbreaks accounted for 234 (0.8%) of 27,755 foodborne disease outbreaks, 24,003 (3%) of 700,600 outbreak-associated illnesses, 2839 (10%) of 29,756 outbreak-associated hospitalizations, and 99 (16%) of 628 outbreak-associated deaths. The median annual number of multistate outbreaks increased from 2.5 during 1973–1980 to 13.5 during 2001–2010; the number of multistate outbreak-associated illnesses, hospitalizations, and deaths also increased. Most multistate outbreaks were caused by Salmonella (47%) and Shiga toxin–producing Escherichia coli (26%). Foods most commonly implicated were beef (22%), fruits (13%), and leafy vegetables (13%).
Conclusions:
The number of identified and reported multistate foodborne disease outbreaks has increased. Improvements in detection, investigation, and reporting of foodborne disease outbreaks help explain the increasing number of reported multistate outbreaks and the increasing percentage of outbreaks that were multistate. Knowing the etiologic agents and foods responsible for multistate outbreaks can help to identify sources of food contamination so that the safety of the food supply can be improved.
Introduction
An estimated 9.4 million foodborne illnesses caused by a known pathogen occur every year in the United States (Scallan et al., 2011). Although few of these illnesses are linked to recognized outbreaks (Gould et al., 2013), data gathered during outbreak investigations can be used to identify foods and etiologic agents that cause disease, highlighting vulnerabilities in the food delivery system. Once vulnerabilities are recognized, public health officials and regulatory agencies can design targeted interventions to decrease the risk of food contamination during production and distribution (Lynch et al., 2006; Gould et al., 2013).
Approximately 1000 foodborne disease outbreaks are reported to The Centers for Disease Control and Prevention (CDC) each year (Gould et al., 2013). Of these, only a small percentage is multistate, with cases exposed to the implicated food in more than one state. However, as compared with outbreaks resulting from exposure to a contaminated food at an event or as a result of mishandling at the point of service, multistate outbreaks frequently result from contamination early in the supply chain. Changes in food production and distribution have increased opportunities for foods contaminated early in the supply chain to be distributed widely and, in turn, have increased the possibility of multistate foodborne disease outbreaks. For example, after World War II, lower transportation costs and improved refrigerated transport promoted specialization in farming, mass food production, and wider product distribution (Martinez et al., 2010). Complex distribution networks emerged to transport centrally produced food to distant consumers (McLaughlin et al., 1999). The geographic dispersion of multistate outbreaks presents a unique challenge because of the need for increased coordination among local, state, and federal health officials to identify and investigate them.
In recent decades, the systems that detect and investigate foodborne disease have been improved, allowing officials to more effectively identify related cases and to trace and identify an outbreak’s source. In particular, systems like PulseNet, the national molecular subtyping network started in 1996 to detect outbreaks of foodborne infections caused by Escherichia coli O157 and other Shiga toxin–producing E. coli (STEC), Listeria monocytogenes, and Salmonella species (Swaminathan et al., 2001), have facilitated detection of multistate outbreaks. A better understanding of the etiologic agents and foods implicated in multistate outbreaks can help public health officials to identify important sources of food contamination in the early stages of production and distribution and inform regulatory agencies and the food industry about ways to improve the safety of the food supply. To address these questions and quantify the contribution of multistate outbreaks relative to all foodborne outbreaks, we described multistate foodborne disease outbreaks reported to CDC since reporting began in 1973.
Materials and Methods
A foodborne disease outbreak is defined as the occurrence of two or more similar illnesses resulting from the ingestion of a common food. Outbreaks are classified as multistate if patients were exposed to the implicated food in more than one state. State, local, and territorial health departments have primary responsibility for identifying and investigating foodborne disease outbreaks; however, multistate outbreak investigations are typically coordinated and reported by CDC (http://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/index.html). Results of these outbreak investigations are voluntarily submitted to CDC’s Foodborne Disease Outbreak Surveillance System (FDOSS; www.cdc.gov/foodsafety/fodoss) (Gould et al., 2013). The criteria for reporting a multistate outbreak include at least two of three pieces of information (epidemiologic, laboratory, traceback) indicating a common source. Data reported for each outbreak include the number of illnesses, hospitalizations and deaths, etiologic agent, implicated food, recalled foods, and affected states.
We reviewed foodborne disease outbreaks reported to FDOSS during 1973–2010 and summarized descriptive characteristics by decade: 1973–1980, 1981–1990, 1991–2000, and 2001–2010. We calculated the percentage of multistate foodborne disease outbreaks and outbreak-associated illnesses, hospitalizations, and deaths relative to all foodborne disease outbreaks.
Implicated foods were classified into 18 mutually exclusive single-food categories based on the classification system developed by Painter et al., except for fruits and nuts, which were analyzed separately (Painter et al., 2009). These categories are beef, crustaceans, dairy, eggs, fish, fruits, fungi, game, grains–beans, leafy vegetables, mollusks, nuts, oils–sugars, pork, poultry, root vegetables, sprouts, and vine–stalk vegetables. The food category analysis only included outbreaks with an implicated food(s) or ingredient(s) that could be classified into a single category. We also compared the meat–poultry group (beef, game, pork, poultry) and produce group (fruits, fungi, leafy vegetables, nuts, sprouts, vine–stalk vegetables). We described the median, 25th and 75th percentiles, and minimum and maximum annual number of single-food commodities by decade.
To characterize the geographic distribution of multistate outbreaks, we analyzed the median number of states with reported cases in each outbreak using the Wilcoxon rank sum test and the number of outbreaks involving states in all four U.S. census regions using Fisher’s exact test. For this analysis, data were available for 2001–2010. We compared the geographic distribution of multistate outbreaks for the first half of this period (2001–2005) with the second half (2006–2010). The number of recalls and the most common foods recalled were summarized for outbreaks that occurred in 1998 or later, which was the earliest this information was reported to CDC.
We used the Spearman correlation coefficient to measure the association between the number of foodborne disease outbreaks and the number of human isolates submitted to PulseNet during 1996–2010. Data were managed and analyzed using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA) and SAS version 9.3 (SAS Institute, Cary, NC).
Results
During 1973–2010, a total of 27,755 foodborne disease outbreaks were reported to FDOSS, resulting in 700,600 illnesses, 29,362 hospitalizations, and 628 deaths. Multistate foodborne disease outbreaks accounted for 234 (0.8%) outbreaks, 24,003 (3%) illnesses, 2839 (10%) hospitalizations, and 99 (16%) deaths (Table 1). Across the study period, an average of 12% of outbreak-associated cases were hospitalized and 0.8% died. The median annual number of multistate outbreaks and percentage of multistate outbreaks relative to all foodborne disease outbreaks increased across the study period.
Table 1.
Comparison of Multistate Outbreaks With All Foodborne Disease Outbreaks and Selected Characteristics of Multistate Outbreaks, by Decade, United States, 1973–2010
| 1973–1980 | 1981–1990 | 1991–2000 | 2001–2010 | Total | |
|---|---|---|---|---|---|
| Outbreaks | |||||
| All foodborne outbreaks | 3620 | 5069 | 8188 | 10,878 | 27,755 |
| Multistate outbreaks (percentage of all outbreaks) | 23 (0.6) | 14 (0.3) | 63 (0.8) | 134 (1.2) | 234 (0.8) |
| Median number multistate outbreaks per year | 2.5 | 1 | 6.5 | 13.5 | 4.5 |
| Illnesses | |||||
| All outbreak-associated illnesses | 110,701 | 181,996 | 183,448 | 224,455 | 700,600 |
| Multistate outbreak-associated illnesses (percentage of all) | 3106 (3) | 1314 (1) | 9.163 (5) | 10.420 (5) | 24,003 (3) |
| Median illnesses per multistate outbreak (range) | 27 (2–1500) | 65 (2–295) | 69 (3–755) | 35 (3–1500) | 52 (2–1500) |
| Hospitalizations | |||||
| All outbreak-associated hospitalizations | 5071 | 10,002 | 6321 | 8362 | 29,756 |
| Multistate outbreak-associated hospitalizations (percentage of all) | 144 (3) | 117 (1) | 803 (13) | 1775 (21) | 2839 (10) |
| Percentage of illnesses hospitalized, average | 14% | 10% | 7% | 16% | 12% |
| Deaths | |||||
| All outbreak-associated deaths | 75 | 272 | 120 | 161 | 628 |
| Multistate outbreak-associated deaths (percentage of all) | 0 (0) | 21 (8) | 36 (30) | 42 (26) | 99 (16) |
| Percentage of illnesses died, average | 0% | 3% | 0.3% | 0.5% | 0.8% |
The median number of states involved in multistate outbreaks increased from 4 (interquartile range [IQR] 4–10) during 2001–2005 to 8 (IQR 5–17) during 2006–2010 (p < 0.01). For the same periods, multistate outbreaks involving all four U.S. census regions increased from 8 (16%) outbreaks to 36 (43%) outbreaks (p < 0.01).
The number of multistate foodborne disease outbreaks and human isolates submitted to PulseNet increased from 1996 to 2010 (Fig. 1). There was a significant correlation between the number of pulsed-field gel electrophoresis (PFGE) patterns from human isolates submitted to PulseNet and the number of outbreaks caused by Salmonella, STEC, and Listeria (ρ = 0.87, p < 0.01).
FIG. 1.
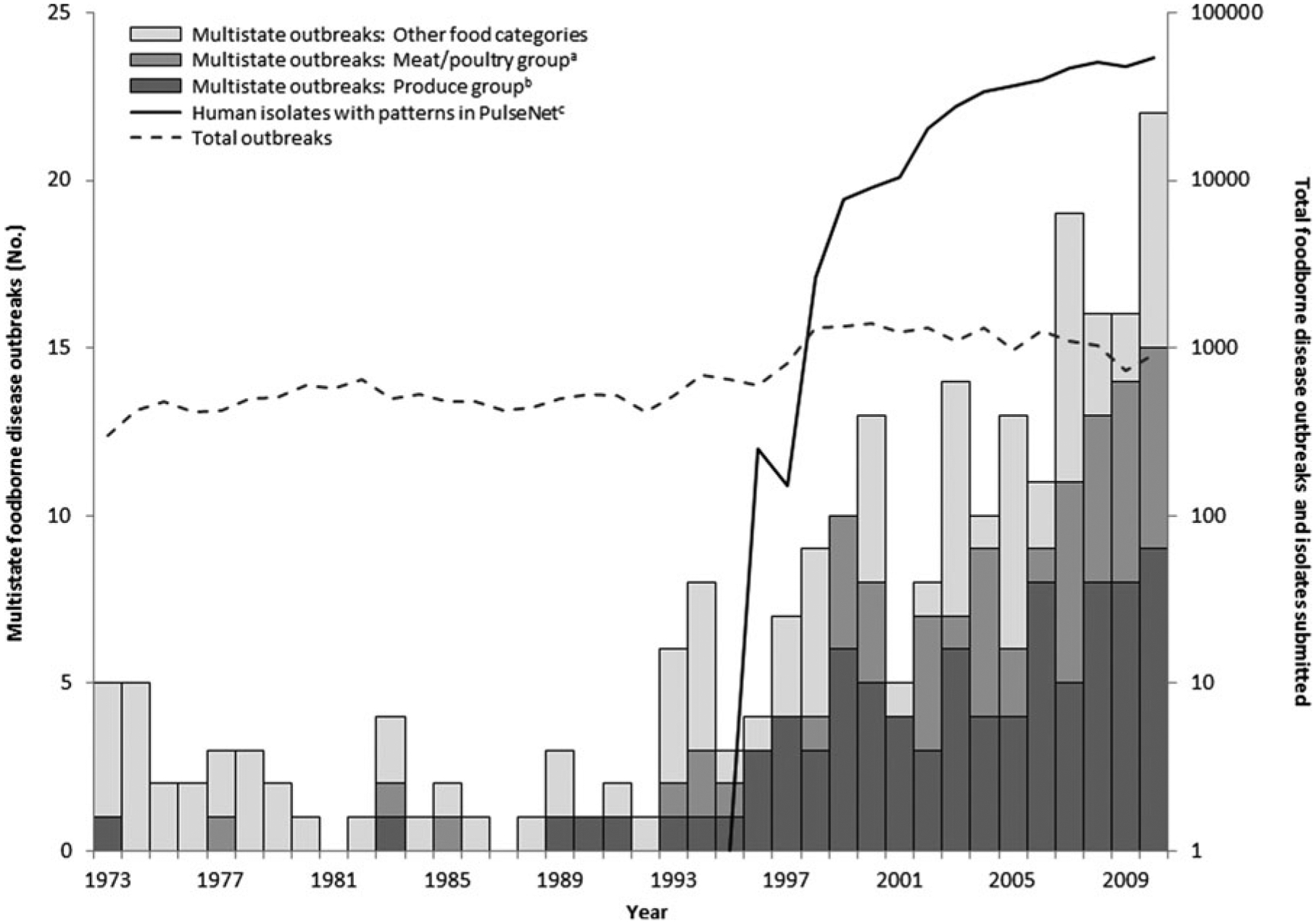
Number of multistate foodborne disease outbreaks, total foodborne disease outbreaks, and number of human isolates with patterns submitted to PulseNet, by year—United States, 1973–2010. aMeat/poultry group consists of beef, game, pork, and poultry food categories. bProduce group consists of fruits, fungi, leafy vegetables, nuts, sprouts, and vine–stalk vegetables food categories. cThe PulseNet laboratory surveillance network began testing isolates in 1996.
Among the 230 (98%) multistate foodborne disease outbreaks with an etiologic agent reported, the most common were Salmonella (47%), STEC (26%), and Listeria (5%) (Table 2). During the most recent decade, 2001–2010, Salmonella and STEC caused 90% of reported multistate outbreaks. Among the 109 multistate Salmonella outbreaks with a reported serotype, the most common were Newport (16; 15%), Typhimurium (14; 13%), and Enteritidis (9; 8%). Among the 60 multistate STEC outbreaks, reported serogroups were O157 (58 outbreaks; 96%), O145 (1; 2%), and O26 (1; 2%).
Table 2.
Etiologic Agents and Food Categories Implicated in Multistate Foodborne Disease Outbreaks—United States, 1973–2010
| Multistate outbreaks | |||||
|---|---|---|---|---|---|
| N (%) | |||||
| Etiologic agent | 1973–1980 N = 23 | 1981–1990 N = 14 | 1991–2000 N = 63 | 2001–2010 N = 134 | Total N = 234 |
| No etiologic agent reported | 2 (9) | 1 (7) | 1 (2) | 0 (0) | 4 (2) |
| Etiologic agent reported | 21 (91) | 13 (93) | 62 (98) | 134 (100) | 230 (98) |
| Salmonella enterica | 9 (43) | 4 (31) | 20 (32) | 76 (57) | 109 (47) |
| Shiga toxin-producing Escherichia coli (STEC) | 0 (0) | 0 (0) | 16 (26) | 44 (33) | 60 (26) |
| Listeria monocytogenes | 0 (0) | 1 (8) | 4 (6) | 6 (4) | 11 (5) |
| Hepatitis A virus | 3 (14) | 2 (15) | 3 (5) | 1 (1) | 9 (4) |
| Norovirus | 0 (0) | 0 (0) | 7 (11) | 1 (1) | 8 (3) |
| Shigella species | 1 (5) | 0 (0) | 4 (6) | 0 (0) | 5 (2) |
| Staphylococcus aureus enterotoxin | 4 (19) | 1 (8) | 0 (0) | 0 (0) | 5 (2) |
| Scombroid toxin | 1 (5) | 1 (8) | 1 (2) | 0 (0) | 3 (1) |
| Other Clostridium species | 1 (5) | 2 (15) | 0 (0) | 0 (0) | 3 (1) |
| Clostridium botulinum | 0 (0) | 0 (0) | 0 (0) | 2 (1) | 2 (1) |
| Clostridium perfringens | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Other etiologic agentsb | 2 (10) | 2 (15) | 7 (11) | 4 (3) | 15 (7) |
| Food category a | N = 23 | N = 14 | N = 63 | N = 134 | N = 234 |
| No food reported | 19 (83) | 2 (14) | 10 (16) | 4 (3) | 35 (15) |
| Food not attributable to one category | 1 (4) | 1 (7) | 6 (10) | 17 (13) | 25 (11) |
| Single category | 3 (13) | 11 (79) | 47 (75) | 113 (84) | 174 (74) |
| Beef | 0 (0) | 2 (18) | 9 (19) | 28 (25) | 39 (22) |
| Fruits | 0 (0) | 1 (9) | 9 (19) | 13 (12) | 23 (13) |
| Leafy vegetables | 0 (0) | 0 (0) | 7 (15) | 15 (13) | 22 (13) |
| Sprouts | 0 (0) | 0 (0) | 6 (13) | 14 (12) | 20 (11) |
| Vine-stalk vegetables | 1 (33) | 0 (0) | 2 (4) | 12 (11) | 15 (9) |
| Dairy | 0 (0) | 3 (27) | 2 (4) | 8 (7) | 13 (7) |
| Mollusks | 1 (33) | 1 (9) | 6 (13) | 3 (3) | 11 (6) |
| Poultry | 0 (0) | 0 (0) | 1 (2) | 7 (6) | 8 (5) |
| Fish | 0 (0) | 1 (9) | 2 (4) | 3 (3) | 6 (3) |
| Nuts | 0 (0) | 0 (0) | 0 (0) | 4 (4) | 4 (2) |
| Eggs | 0 (0) | 0 (0) | 0 (0) | 3 (3) | 3 (2) |
| Pork | 0 (0) | 0 (0) | 1 (2) | 0 (0) | 1 (1) |
| Other categoriesc | 1 (33) | 3 (27) | 2 (4) | 3 (3) | 9 (5) |
The denominator for each etiologic agent is the etiologic agent reported total; the denominator for each food category is the single category total.
Other agents were Campylobacter (2 outbreaks), ciguatoxin (1), Cyclospora (2), paralytic shellfish poison (1), Trichinella (2), Vibrio (3), Yersinia (1), other non-STEC E. coli (1), and other chemicals and toxins (2).
Other categories were grains–beans (3 outbreaks), fungi (2), game (2), root vegetables (2), crustaceans (0), and oils–sugars (0). For single-state outbreaks, other categories were grain–beans (181), fungi (22), game (27), root vegetables (48), crustaceans (93), and oils–sugars (12).
Among the 174 (74%) multistate outbreaks with an implicated food reported that could be classified into a single category, the most common foods were beef (22%), fruits (13%), and leafy vegetables (13%) (Table 2). The number of food categories implicated in multistate outbreaks increased every decade from a median of <1 (IQR 0–0.5) per year during 1973–1980 to 7 (IQR 5–9) during 2001–2010. Multistate outbreaks caused by foods in the meat–poultry and produce groups increased beginning in the mid-1990s (Fig. 1).
An implicated food was reported for all multistate Salmonella and Listeria outbreaks and 57 (95%) STEC O157 outbreaks. Food categories implicated in multistate outbreaks varied by etiologic agent. For Salmonella outbreaks, the most common categories were fruits (18; 17%), sprouts (17; 16%), and vine–stalk vegetables (14; 13%). For STEC O157 outbreaks, the most common categories were beef (30; 53%), leafy vegetables (12; 21%), and unpasteurized dairy products (3; 5%). For Listeria outbreaks, the most common categories were pasteurized dairy products (4; 36%) and poultry (3; 27%).
Among 150 multistate outbreaks caused by Salmonella, STEC, and Listeria from 1998 to 2010, 54 (36%) resulted in food recalls. In 47 (87%) of these outbreaks, the implicated foods could be classified into a single food category. The most common food categories implicated in multistate outbreaks resulting in food recalls were beef (15 outbreaks), sprouts (9), and dairy (5). The 16 multistate outbreaks caused by other etiologic agents resulted in six recalls, including four involving foods that could be classified into single categories: mollusks (3) and root vegetables (1).
Discussion
Multistate outbreaks were only a small percentage of all foodborne disease outbreaks; however, the number of identified and reported multistate foodborne disease outbreaks has increased each decade since the early 1990s. Improvements in detection, investigation, and reporting of foodborne disease outbreaks might help explain the increasing number of reported multistate outbreaks and the increasing percentage of outbreaks that were multistate. After PulseNet was introduced in 1996, clusters of cases with indistinguishable PFGE patterns scattered across multiple states could be more promptly detected and investigated to identify common exposures (Swaminathan et al., 2001). Because PFGE testing is standardized nationally and data are stored centrally, cases can be linked across multiple public health jurisdictions. Conversely, in situations where epidemiologic evidence (e.g., case–control study findings) suggests a link, PFGE patterns can be used to include or exclude cases from an investigation, allowing epidemiologists to focus resources on cases most likely to share an epidemiological association. The strong, positive correlation between the number of isolates submitted to PulseNet and the number of multistate outbreaks demonstrates the important role of improved laboratory surveillance in facilitating multistate outbreak detection and investigation.
Detection and investigation of multistate outbreaks has been strengthened through several improvements to public health surveillance systems. In addition to PulseNet, in 1996, the Foodborne Diseases Active Surveillance Network (FoodNet) was created to perform population-based surveillance for foodborne disease (Scallan et al., 2012). Although FoodNet surveillance does not specifically target outbreaks, it gathers clinical and epidemiologic data on laboratory-confirmed cases of major enteric diseases. In 1998, FDOSS transitioned from a paper to an electronic data collection system, and reports of investigations of both single and multistate foodborne disease outbreaks doubled (Gould et al., 2013). In 2003, the Council to Improve Foodborne Outbreak Response was created to improve how public health officials detect, investigate, control, and prevent foodborne disease outbreaks (CIFOR, 2014). In 2006, the creation of OutbreakNet improved multistate outbreak investigation by coordinating efforts of local, state, territorial, and federal public health officials. Collaboration also improved across disciplines as foodborne disease epidemiologists, laboratory experts, environmental health specialists, and regulatory partners jointly investigated outbreaks (CDC, 2014a). In 2009, CDC created the Foodborne Diseases Centers for Outbreak Response Enhancement (FoodCORE) to develop methods to improve outbreak detection and investigation (CDC, 2014b). Lastly, in 2010, the Council of State and Territorial Epidemiologists made foodborne disease outbreaks a reportable condition.
Despite being only ≈1 percent of all reported outbreaks, multistate outbreaks caused a greater proportion of foodborne outbreak-associated illnesses, hospitalizations, and deaths. PulseNet routinely performs laboratory surveillance for the three pathogens that accounted for most multistate outbreaks, but there are no mechanisms for routine laboratory surveillance and subtyping of pathogens common in foodborne disease outbreaks overall (e.g., norovirus) (Gould et al., 2013). Consequently, our finding that multistate outbreaks accounted for a greater percentage of hospitalizations and deaths might be inflated by the underdetection of outbreaks caused by pathogens that usually present with mild clinical features for which it is less likely a person will seek medical care or have a stool culture performed. Institution of systematic surveillance for norovirus with CaliciNet, the U.S. norovirus outbreak surveillance network of federal, state, and local public health laboratories, might improve detection of multistate norovirus outbreaks (Vega et al., 2011; Hall et al., 2012).
Five food categories accounted for two thirds of multistate outbreaks. Fruits, sprouts, and vine–stalk vegetables were the most common categories among multistate Salmonella outbreaks, whereas beef and leafy vegetables were the most common categories among multistate STEC outbreaks. Over time, outbreaks were attributed to more food categories. This may reflect a change in consumer demand for food variety and consistent availability of seasonal produce year-round (Brooks et al., 2009; Martinez et al., 2010). Compared with 2000–2005, multistate outbreaks from 2006 to 2010 affected more states and U.S. census regions, a possible result of the wider geographic distribution of centrally produced foods, better identification of cases by health officials, or both.
For Salmonella, multistate outbreaks were commonly caused by fruits, sprouts, and vine–stalk vegetables, all of which are produce categories. In contrast, data from FDOSS report that Salmonella outbreaks overall are most commonly caused by protein sources (poultry, eggs, pork, and beef) (Gould et al., 2013). The reasons for this difference are unknown, but one possibility is the difference in multistate and single-state outbreak investigation techniques. Implicating a single produce item during an outbreak investigation can be difficult because multiple produce items are frequently eaten together, for example, in a salad. In a multistate outbreak, individuals are more likely to eat different combinations of each ingredient in different settings (e.g., private homes, restaurants). The variation in exposure histories makes identification of a common ingredient possible and may facilitate traceback investigations to a common source. In contrast, if a salad was implicated in a point source, single-state outbreak, everyone who became ill would have eaten the same salad with the same ingredients, making identification of one contaminated ingredient challenging because of the collinear exposure to all salad ingredients.
Differences in the handling of produce and protein-based foods might also explain the foods most commonly reported in multistate Salmonella outbreaks. Protein-based foods require cooking, a step that should eliminate most pathogens when done properly. A multistate Salmonella outbreak would require that many homes and food service establishments fail to take this step. In contrast, produce is often eaten raw. Without a cooking step, widely distributed contaminated produce could more easily cause illness across multiple states. Although less common, multistate Salmonella outbreaks caused by protein-based foods do occur despite cooking practices that should eliminate contamination, likely because of cross-contamination and consumer preferences for eating certain foods raw or undercooked (e.g., eggs, beef).
This analysis had some limitations. First, these findings likely underestimate the true number of multistate outbreaks. Although PulseNet identifies hundreds of PFGE clusters each year, few multistate cluster investigations collect enough evidence (epidemiologic, laboratory, traceback) to identify a common source and meet the definition of a multistate foodborne disease outbreak. Additional resources to strengthen epidemiologic, laboratory, and traceback investigations will improve the identification of outbreak sources. Second, a lack of information about specific contaminated ingredients for some multistate outbreaks limited the ability to assign foods to 1 of the 18 food categories. Additionally, in 25% of multistate outbreaks, foods were not reported or a specific ingredient was not implicated. Third, most multistate outbreaks were reported during the last two decades of the analysis period, and these conclusions may not be generalizable to earlier decades. Lastly, not all outbreaks are reported to CDC, and changes in reporting practices over time might have affected our findings.
Conclusions
To our knowledge, this analysis provides the most complete summary of multistate foodborne disease outbreaks in the United States. Since 1973, reports of multistate outbreaks have steadily increased, likely driven by improvements in detection, investigation, and reporting, as well as by changes in food distribution patterns. Contamination of food any-where in the production process can result in an outbreak. As foods travel longer distances from farm to table, opportunities for widespread outbreaks will increase (Pirog et al., 2001; Saunders and Hayes, 2007). Coordinated detection and investigation of multistate outbreaks should continue, and new laboratory surveillance techniques must be developed, especially if culture-independent diagnostic techniques become the clinical standard for diagnosing diarrheal diseases. Improved detection, investigation, and reporting of multistate outbreaks allow the public health system to identify weaknesses in the food supply chain, and continued support of these activities will improve the safety of the foods we eat.
Acknowledgments
We thank state and local health departments for reporting foodborne disease outbreaks to CDC.
Footnotes
Disclosure Statement
No competing financial interests exist.
References
- Brooks N, Regmi A, Jerardo A. U.S. Food Import Patterns, 1998–2007. Outlook No. FAU-125. Washington, DC: U.S Department of Agriculture, Economic Research Service, 2009. [Google Scholar]
- [CDC] The Centers for Disease Control and Prevention. Foodborne Outbreaks: CDC’s Role in Outbreak Investigations. 2014a. Available at: http://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/cdc-role.html, accessed March 17, 2014.
- CDC. Foodborne Disease Centers for Outbreak Response Enhancement. 2014b. Available at: http://www.cdc.gov/foodcore/, accessed June 12, 2014.
- [CIFOR] Council to Improve Foodborne Outbreak Response. 2014. Available at: http://www.cifor.us/about.cfm, accessed August 19, 2014.
- Gould LH, Walsh KA, Vieira AR, Herman K, Williams IT, Hall AJ, Cole D. Surveillance for foodborne disease outbreaks—United States, 1998–2008. MMWR Surveill Summ 2013;62: 1–34. [PubMed] [Google Scholar]
- Hall AJ, Eisenbart VG, Etingüe AL, Gould LH, Lopman BA, Parashar UD. Epidemiology of foodborne norovirus outbreaks, United States, 2001–2008. Emerg Infect Dis 2012;18: 1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch M, Painter J, Woodruff R, Braden C. Surveillance for foodborne-disease outbreaks—United States, 1998–2002. MMWR Surveill Summ 2006;55:1–42. [PubMed] [Google Scholar]
- Martinez S, Hand M, Da Pra M, Pollack S, Ralston K, Smith T, Vogel S, Clark S, Lohr L, Low SA, Newman C. Local Food Systems: Concepts, Impacts, and Issues. Report No: 97. Washington, DC: U.S. Department of Agriculture, Economic Research Service, 2010. [Google Scholar]
- McLaughlin EW, Green GM, Park K. Changing Distribution Patterns in the U.S. Fresh Produce Industry: Mid/Late-70s to Mid/Late-90s. Ithaca, NY: Cornell University, College of Agriculture and Life Sciences, Department of Agricultural, Resource, and Managerial Economics, 1999. [Google Scholar]
- Painter JA, Ayers T, Woodruff R, Blanton E, Perez N, Hoekstra RM, Griffin PM, Braden C. Recipes for foodborne outbreaks: A scheme for categorizing and grouping implicated foods. Foodborne Pathog Dis 2009;6:1259–1264. [DOI] [PubMed] [Google Scholar]
- Pirog R, Van Pelt T, Enshayan K. Food, fuel, and freeways: An Iowa perspective on how far food travels, fuel usage, and greenhouse gas emissions. Ames, IA: Leopold Center for Sustainable Agriculture, 2001. Available at: http://www.leopold.iastate.edu/sites/default/files/pubs-and-papers/2011-06-food-fuel-and-freeways-iowa-perspective-how-far-food-travels-fuel-usage-and-greenhouse-gas-emissions.pdf, accessed August 19, 2014. [Google Scholar]
- Saunders C, Hayes P. Airfreight Transport of Fresh Fruits and Vegetables—A Review of the Environmental Impact and Policy Options. Geneva, Switzerland: International Trade Centre, 2007. [Google Scholar]
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM. Foodborne illness acquired in the United States—Major pathogens. Emerg Infect Dis 2011;17:7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scallan E, Mahon BE. Foodborne Diseases Active Surveillance Network (FoodNet) in 2012: A foundation for food safety in the United States. Clin Infect Dis 2012;54(Suppl 5):S381–S384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaminathan B, Barrett TJ, Hunter SB, Tauxe RV; CDC PulseNet Task Force. PulseNet: The molecular subtyping network for foodborne bacterial disease surveillance, United States. Emerg Infect Dis 2001;7:382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega E, Barclay L, Gregoricus N, Williams K, Lee D, Vinjé J. Novel surveillance network for norovirus gastroenteritis outbreaks, United States. Emerg Infect Dis 2011;17:1389–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]


