Abstract
Background
Curved varus osteotomy (CVO) is an effective femoral head-preserving surgical procedure for osteonecrosis of the femoral head (ONFH) classified as type B or C1 according to the Japanese Investigation Committee (JIC) classification; it reportedly provides better postoperative outcomes than transtrochanteric rotational osteotomy (TRO). We have developed a new procedure called spherical varus rotational osteotomy (SVRO) in which osteotomy of the femur into a spherical shape is followed by varus and anterior rotation using navigation to increase indications and improve postoperative outcomes.
Methods
Nine joints of eight patients who underwent SVRO and could be followed up for > 1 year were included in the study. Disease types determined preoperatively according to the JIC classification were type C1 for four joints and type C2 for five joints. Preoperative disease JIC classification stages were 3a for eight joints and 1 for one joint. SVRO was performed using OrthoMap® 3D Navigation software, and the following variables were measured: surgery time, intraoperative blood loss, difference between preoperative and postoperative angles of anteversion, postoperative lower limb length discrepancy, and postoperative intact area occupancy. The Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire (JHEQ) was used for clinical evaluation. Visual Analog Scale and JHEQ scores were evaluated preoperatively and at the final follow-up.
Results
The measurement results were as follows: surgery time, 130 min; blood loss, 200 ml; angle of varus, 20°; angle of anterior rotation, 30°; preoperative angle of anteversion, 15°; postoperative angle of anteversion, 22°; lower limb shortening, 11 mm; preoperative intact area occupancy, 0%; and postoperative intact area occupancy, 74.2%. There were no cases of progression in the postoperative stages or re-collapse.
Conclusion
SVRO allows for the repositioning of the exterior and posterior intact areas, providing a broader intact region postoperatively. This technique is particularly beneficial for young patients with ONFH and extensive necrosis and is a less invasive alternative to TRO. This procedure has been shown to be effective in achieving favorable outcomes in patients with extensive necrosis who would have otherwise required rotational osteotomy, depending on the necrosis location. Further longitudinal studies are necessary to validate these findings and establish long-term benefits.
Keywords: Extensive necrosis, CT-based navigation, Curved varus osteotomy osteonecrosis of the femoral head
Background
Curved varus osteotomy (CVO) has been performed as a useful bone-preserving surgical treatment for young patients with osteonecrosis of the femoral head (ONFH) of type B or C1 according to the Japanese Investigation Committee (JIC) classification [1], after it was first introduced by Nishio [2] in 1971 for acetabular dysplasia. The original method involves an osteotomy parallel to the axis of the lower limb with no consideration of femoral anteversion, resulting in errors in the angle of anteversion postoperatively. To perform osteotomies perpendicular to the axis of the femoral neck in patients with different angles of anteversion, we have been using intraoperative images to determine the osteotomy plane with the longest neck length before we perform an osteotomy perpendicular to the axis of the femoral neck to the best of our ability. However, it has been impossible to intraoperatively determine the three-dimensional femoral neck area based on two-dimensional images. Moreover, the postoperative angle of anteversion varies markedly depending on the incident angle of the image used as the angle of anteversion changes substantially depending on the hip flexion angle [3].
Compared with transtrochanteric rotational osteotomy (TRO), which is an intra-articular procedure, CVO is associated with less risk of vascular injury, less intense postoperative pain, less significant lower limb shortening, and better postoperative range of motion and is hence the more preferred bone-preserving surgical treatment [4]. Moreover, as necrosis is often localized anteriorly [5], we have included additional anterior rotation in CVO to obtain greater intact area occupancies. At this step, attempting rotation after linear and cylindrical osteotomies is disadvantageous in terms of osteotomy site stability and bone union because there is an osteotomy surface gap. Attempts to align the posterior wall, which is visible in the operative field, mostly result in retroversion. In fact, poor postoperative ranges of motion were found in some cases in which anterior rotation was added to CVO.
We report here a newly developed surgical procedure in which the transtrochanteric femur is hollowed to form a spherical shape using the Stryker navigation system and a Tagawa chisel before simultaneous varus and rotation without changing the angle of anteversion.
Indications
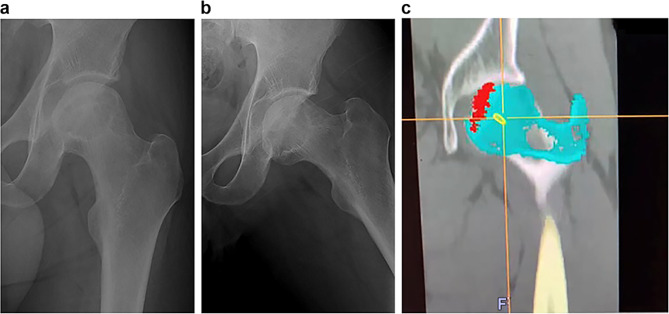
For cases where a greater normal area can be obtained, a simulation was conducted using navigation, comparing the image obtained by rotating the MRI coronal Sect. 30°backward along the cervical axis with the central slice of the femoral head in the MRI Cor images. Those that could acquire more than 40% of the normal area in the central slice of the femoral head were considered suitable (Fig. 1A, B, C) [6].
Fig. 1.
A. JIC classification Type C2 Stage3a. B. Image in an abducted position. Case in which the intact area is sufficient. C. This procedure indicated when simulation shows intact ratio ≥ 40%
Preoperative preparation
Computed tomography (CT) images (2.5-mm slices) from the patient’s iliac crest to the femoral condyle are acquired. The images are imported to the Stryker Orthomap® 3D navigation system. After the necrosis site is identified using the MRI necrosis area as a reference and filled in, the central axis is identified in the coronal, sagittal, and axial sections of the hip. A sphere passing through the greater trochanter apex and near the lesser trochanter is determined so that the center of rotation and the center of the femoral head are as close as possible. After a 30° anterior rotation around the axis of rotation identified earlier, a figure of the 20° varus is constructed.
Surgical technique
In a complete lateral position, a 15-cm lateral longitudinal incision from the greater trochanter top is made to expose the intertrochanteric crest of the posterior wall of the femur. Subsequently, the lesser trochanter is exposed, and the iliopsoas tendon is cut. After registration using the navigation, the surgairtome tip is identified using a calibration tool, and a bone tunnel is made in the posterior wall as per the preoperative plan. The calibration tool is used again to recognize the center of the tip of a Tagawa chisel R60mm and 50 mm and a Hasegawa chisel R45.40.35 mm to form an arc as per the preoperative plan.
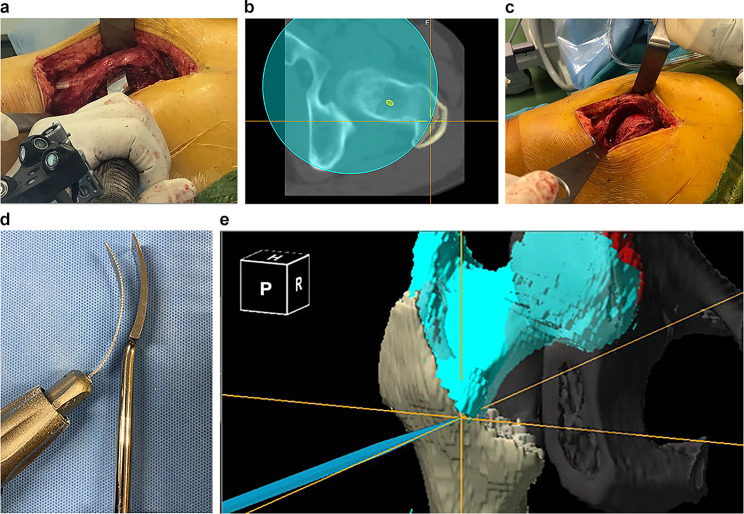
Various chisels are used to perform osteotomy (Fig. 2A and B), and the anterior wall of the femur is cut using a bone saw compatible with the curvature of the chisel used (Fig. 2C and D). After subsequent varus and rotation, the consistency with the imaginary proximal bone fragment simulated is confirmed, and the fragment is fixed using the original CHS (F-system) (Fig. 2E). The greater trochanter is fragile because the concave side is cut. In some early cases, greater trochanteric fractures occurred early after the surgery. Thus, A-I pins have been used since then to fix the greater trochanter (Figs. 3 and 4). In this case, the intact ratio on the central slice of the CT coronal image of the femoral head improved from 0% preoperatively to 76% postoperatively (Fig. 5A and B).
Fig. 2.
A. Tagawa chisel is used for osteotomy. B. The center of the Tagawa chisel is traced with a cross mark. C. As osteotomy surface becomes spherical, increased contact area enhances stability. D. A curved bone saw is used to cut the femur’s anterior wall. E. A pointer confirms and fixes alignment with the imaginary proximal bone fragment
Fig. 3.

The same patient as above after a 20° varus and a 30° anterior rotation
Fig. 4.

Postoperative 3D CT showing that the planned varus and anterior rotation are achieved
Fig. 5.
A. Preoperative CT coronal section shows an intact ratio of 0%. B. Postoperative intact ratio improved to 76%
Subjects: Nine joints of eight patients who underwent spherical varus rotational osteotomy (SVRO) for idiopathic ONFH between February 2021 and May 2023 and could be followed up for > 1 year were included in the study. The average follow-up period was 21 months. Seven patients were men, and one was a woman. Their age at operation was 32 years (30, 44); body mass index was 24.72 (23, 27.18); and preoperative JIC disease types were type C1 for four joints and type C2 for five joints. Preoperative disease stages were 1 for one joint and 3a for eight joints. The etiologies were alcohol-induced in four cases, steroid-induced in three cases, and strictly idiopathic in two cases. One patient with bilateral ONFH (N03.4) underwent SVRO for both sides on the same day. In N07, the contralateral joint was type C2 and stage 3b for which transtrochanteric anterior rotational osteotomy was indicated. Thus, prophylactic SVRO was performed on the affected joint, which was classified as stage 1 and type C2, on the same day as the contralateral side because it was predicted to collapse (Table 1).
Table 1.
Demographic data
| Case no. | Sex | Age at operation | Risk factor | BMI (kg/m2) | Type | Stage | Follow-up period (M) |
|---|---|---|---|---|---|---|---|
| 1 | M | 29 | A | 27.4 | C1 | 3a | 28 |
| 2 | M | 45 | A | 21.1 | C2 | 3a | 30 |
| 3 | M | 44 | A | 27.0 | C1 | 3a | 25 |
| 4 | M | 44 | A | 27.0 | C2 | 3a | 25 |
| 5 | M | 31 | I | 23.0 | C1 | 3a | 24 |
| 6 | F | 19 | S | 24.3 | C2 | 3a | 22 |
| 7 | M | 42 | S | 30.2 | C2 | 1 | 12 |
| 8 | M | 31 | I | 24.7 | C2 | 3a | 12 |
| 9 | M | 32 | S | 23.14 | C1 | 3a | 12 |
Methods
SVRO was performed using the OrthoMap® 3D Navigation software (Stryker), and the following variables were measured: surgery time, intraoperative blood loss, angle of varus, angle of anterior rotation, difference between preoperative and postoperative angles of anteversion, postoperative lower limb length discrepancy (measured at the lower end of the lesser trochanter), postoperative intact area occupancy measured using CT coronal section femoral head central slices [6]. Clinical evaluation was performed to compare preoperative and final follow-up Visual Analog Scale (VAS) and Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire (JHEQ) scores [7]. Statistical analysis was conducted using the Kruskal–Wallis test.
Results
The measurement results were as follows: surgery time, 130 (97.5, 142.5) min; blood loss, 200 (157.5, 305); angle of varus, 20° (20, 20); angle of anterior rotation, 30° (20, 30); preoperative angle of anteversion, 15° (10.5, 22); postoperative angle of anteversion, 22° (12.5, 27); lower limb shortening, 11 (7, 12.5) mm; preoperative intact area occupancy, 0% (0, 18.8); and postoperative intact area occupancy, 74.2% (56.35,76.5) Tables 2 and 3. Clinical evaluation showed an improvement in VAS from 71 mm preoperatively to 12 mm postoperatively and an improvement in JHEQ from 47 points preoperatively to 73 points postoperatively (Table 4). All cases showed bone union on CT images obtained 6 months postoperatively. Although the follow-up period was short, none of the patients showed stage progression or re-collapse at the final follow-up.
Table 2.
Surgery data
| SVRO | |
|---|---|
| Operation time (min) | 130 (97.5, 142.5) |
| Blood loss (ml) | 200 (157.5, 305) |
| Angle of varus (°) | 20° (20, 20) |
| Angle of anterior rotation | 30° (20, 30) |
| LLS (mm) | 11 (7, 12.5) |
Table 3.
Preoperative and postoperative angles of anteversion and intact area occupancies
| Preoperation | Postoperation | p | |
|---|---|---|---|
| Femoral anteversion | 15° (10.5, 22) | 22° (12.5, 27) | 0.33 |
| Intact ratio | 0% (0, 18.8) | 74.2% (56.6, 76.5) | 0.003 |
Table 4.
Clinical results
| Preoperation | Last follow-up | p | |
|---|---|---|---|
| VAS (mm) | 71 (56.6, 93) | 12 (10, 16) | 0.006 |
| JHEQ (points) | 47(31.5, 57) | 73 (66.5, 79.5) | 0.005 |
Postoperative treatment: Patients started weight bearing 2 weeks after the surgery from 1/4 partial weight bearing (PWB), which was increased to 1/3, 1/2, and 2/3 PWB at a 1-week interval. The patients were discharged from the hospital and were asked to use the Lofstrand crutch.
Discussion
In Japan, TRO [8] and CVO [2] have mainly been performed as bone-preserving surgeries for ONFH. Core decompression is performed for osteonecrosis; however, outcomes for extensive necrosis are not favorable. Osteotomy is recommended for extensive necrosis such as JIC types C1 and C2 [9, 10]. Lee et al. [4] compared TRO and CVO and reported that CVO was superior in terms of surgery time, blood loss, rate of recurrent collapse, and osteoarthritis (OA) change;. Compared with TRO that cuts the short external rotators, obturatorius externus muscle, iliopsoas muscle, and the greater trochanter as well as the articular capsule during surgery, CVO is advantageous as only the iliopsoas muscle is cut. There is better postoperative range of motion because CVO is an extracapsular procedure, and above all, there is less risk of vascular injury. Quaranta et al. [11] mentioned in their systematic review of osteotomies for idiopathic osteonecrosis of the femoral head that the mean time from osteotomy to total hip arthroplasty (THA) was 7.6 years, with a conversion rate of 46.2% after TRO compared with that of 13.3% after CVO. Although the indications for each osteotomy type differ, this difference demonstrates the superiority of CVO.
As for the quality of life (QOL), Ōsawa et al. studied patients who underwent CVO or THA at ≤ 50 years of age and reported that survival rates and sports activities 10 years after surgery were similar between the CVO and THA groups, concluding that CVO is effective in younger patients as long as the indications are observed [9]. Meanwhile, the QOL after TRO is reportedly inferior to that after THA [12]. Moreover, because TRO is a technically demanding procedure, surgical outcomes vary substantially between different institutions although good postoperative outcomes have been reported in Asia [13, 14]. In particular, in Western countries, recurrent collapse occurs early after surgery, and TRO is not recommended because of its high complication rates [15–17].
Conventionally, CVO has been indicated for JIC classification [1] type B cases and type C1 cases with less extensive lesions. Based on two-dimensional frontal images of three-dimensional left and right hips in an abducted position, the procedure has been considered suitable when the intact area accounts for at least 40% of the acetabulum to prevent progression of OA [18, 19]. Because the suitability is considered based on two-dimensional images, angles of varus in type B and C1 cases are required to be at least 20° and 30°, respectively [20].
For expansion of the indications of CVO, a study has reported that a greater angle of varus yielded good results [21]; however, as the varus angle determines the amount of lower limb shortening, greater angles reduced patient satisfaction in a postoperative lower limb survey [22]. Furthermore, in the case of Type C2, TRO is applicable.
Ganz et. have stated that nontraumatic ONFH is typically localized anteriorly, superiorly, and exteriorly with a posterior intact part [5], a method to move the posterior part to the acetabulum without increasing or decreasing it and without involving capsulotomy was developed. In other words, the surgical indication of transtrochanteric osteotomy was determined by not only considering it two-dimensionally but also three-dimensionally.
Recently, intraoperative CT-based navigation systems have become available and have been reported to permit highly accurate osteotomies for not only THA on the acetabular side [23] but also femoral osteotomy [24]. We have also introduced a navigation technology in 2021.
To prevent lower limb shortening as much as possible [25], we adopted the navigation technology and performed osteotomies using curved chisels appropriate for each osteotomy line. It was determined using a sphere in which the center of rotation approximated the center of the femoral head as close as possible and the measuring arc of the sphere passed through the greater trochanter top and the lesser trochanter top. The use of the navigation enabled us to trace the tip of curved chisels, such as the Tagawa chisel, and perform osteotomies without the risk of inadvertently allowing the tip of the chisel to enter the anterior joint. We have developed a surgical technique to minimize changes in the angle of anteversion and secure a sufficient intact area with varus and rotation. Retrospective simulation of SVRO with a varus angle of 20° and an anterior rotation angle of 30° in 30 cases in which patients underwent anterior rotational osteotomy at our hospital showed that the intact area acquired postoperatively was ≥ 40% in approximately 80% of the cases.
Clinical evaluation was conducted using PROMs, specifically JHEQ and VAS. Ōsawa et al. [26] reported that the JHEQ score was 50.2 points 10 years after CVO surgery. In this study, despite the shorter mean follow-up period, the score was favorable (73 points). Further long-term follow-up is necessary.
This surgical procedure allows for obtaining sufficient postoperative intact areas using SVRO. This procedure is less invasive and has a past record of good postoperative clinical outcomes in cases of extensive ONFH for which TRO has been indicated conventionally. This method is likely to provide young patients requiring osteotomy with significant benefits.
The limitations of this study include the small sample size, short follow-up period, and lack of comparative data.
Conclusion
SVRO, which is a variant of CVO modified to expand the indications, was effective for patients with extensive necrosis. The use of navigation allowed for accurate spherical osteotomy simultaneously with varus, without increasing or decreasing the anterior rotation. SVRO was also useful for ONFH patients with extensive necrosis who would have previously been treated with anterior rotational osteotomy depending on the location of the necrosis.
Acknowledgements
Not applicable.
Abbreviations
- CT
Computed tomography
- CVO
Curved varus osteotomy
- JHEQ
Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire
- JIC
Japanese Investigation Committee
- LLS
lower limb shortening
- ONFH
Osteonecrosis of the femoral head
- PWB
Partial weight bearing
- QOL
Quality of life
- SVRO
Spherical varus rotational osteotomy
- THA
Total hip arthroplasty
- TRO
Transtrochanteric rotational osteotomy
- VAS
Visual Analog Scale
Author contributions
Conceptualization: Minoru Watanabe. Data curation: Tsubasa Ishikawa. Formal analysis: Satoshi Kagaya. Funding acquisition: Koji Kanzaki. Investigation: Daichi Kuzushima. Methodology: Minoru Watanabe. Project administration: Minoru Watanabe. Resources: Minoru Watanabe. Software: Minoru Watanabe. Supervision: Minoru Watanabe. Validation: Satoe Tanabe. Visualization: Itaru Kachi. Writing—original draft: Minoru Watanabe. Writing—review & editing: Koji Kanzaki.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was approved by Showa University Research Ethics Review Board Committee (approval number: 2023 246 A). The study was carried out in accordance with the World Medical Association Declaration of Helsinki (JBJS 79-A:1089-98,1997). Informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2002;7:601–5. 10.1007/s007760200108 [DOI] [PubMed] [Google Scholar]
- 2.Nishio A, Sugioka Y. A new technique of the varus osteotomy at the upper end of the femur. Orthop Traumatol. 1971;20:381–6. 10.5035/nishiseisai.20.381 [DOI] [Google Scholar]
- 3.Scorcelletti M, Reeves ND, Rittweger J, Ireland A. Femoral anteversion: significance and measurement. J Anat. 2020;237:811–26. 10.1111/joa.13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee YK, Park CH, Ha YC, Kim DY, Lyu SH, Koo KH. Comparison of surgical parameters and results between curved Varus osteotomy and rotational osteotomy for osteonecrosis of the femoral head. Clin Orthop Surg. 2017;9:160–8. 10.4055/cios.2017.9.2.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganz R, Büchler U. Overview of attempts to revitalize the dead head in aseptic necrosis of the femoral head—osteotomy and revascularization. Hip. 1983:296–305. [PubMed]
- 6.Miyanishi K, Noguchi Y, Yamamoto T, Irisa T, Suenaga E, Jingushi S, et al. Prediction of the outcome of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000;82:512–6. 10.1302/0301-620X.82B4.0820512 [DOI] [PubMed] [Google Scholar]
- 7.Matsumoto T, Kaneuji A, Hiejima Y, Sugiyama H, Akiyama H, Atsumi T, et al. Japanese Orthopaedic Association hip disease evaluation questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The Subcommittee on Hip Disease evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. J Orthop Sci. 2012;17:25–38. 10.1007/s00776-011-0166-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978;130:191–201. [PubMed] [Google Scholar]
- 9.Sadile F, Bernasconi A, Russo S, Maffulli N. Core decompression versus other joint preserving ttreatments for osteonecrosis of the femoral head:ameta-analysis. Br Med Bull. 2016;118:33–49. 10.1093/bmb/ldw010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Migliorini F, Maffulli N, Baroncini A, Eschweiler J, Tingart M, Betsch M. Prognostic factors in the management of osteonecrosis of the femoral head: a systematic review. Surgeon. 2023;21:85–98. 10.1016/j.surge.2021.12.004 [DOI] [PubMed] [Google Scholar]
- 11.Quaranta M, Miranda L, Oliva F, Aletto C, Muffulli N. Osteotomy for avascular necrosis of the femoral head. Br Med Bull. 2021;137:98–111. 10.1093/bmb/ldaa044 [DOI] [PubMed] [Google Scholar]
- 12.Osawa Y, Seki T, Okura T, Takegami Y, Ishiguro N, Hasegawa Y. Curved intertrochanteric Varus osteotomy vs total hip arthroplasty for osteonecrosis of the femoral head in patients under 50 years old. J Arthroplasty. 2020;35:1600–5. 10.1016/j.arth.2020.01.026 [DOI] [PubMed] [Google Scholar]
- 13.Koo KH, Song HR, Yang JW, Yang P, Kim JR, Kim YM. Trochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2001;83:83–9. 10.1302/0301-620X.83B1.0830083 [DOI] [PubMed] [Google Scholar]
- 14.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. Indications and long-term results. Clin Orthop Relat Res. 1992;277:111–20. 10.1097/00003086-199204000-00013 [DOI] [PubMed] [Google Scholar]
- 15.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka’s osteotomy for femoral-head necrosis in young caucasians. Int Orthop. 2005;29:140–4. 10.1007/s00264-005-0639-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dean MT, Cabanela ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J Bone Joint Surg Br. 1993;75:597–601. 10.1302/0301-620X.75B4.8331115 [DOI] [PubMed] [Google Scholar]
- 17.Schneider W, Aigner N, Pinggera O, Knahr K. Intertrochanteric osteotomy for avascular necrosis of the head of the femur. Survival probability of two different methods. J Bone Joint Surg Br. 2002;84:817–24. 10.1302/0301-620X.84B6.0840817 [DOI] [PubMed] [Google Scholar]
- 18.Zhao G, Yamamoto T, Ikemura S, Motomura G, Mawatari T, Nakashima Y, et al. Radiological outcome analysis of transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head at a mean follow-up of 12.4 years. J Bone Joint Surg Br. 2010;92:781–6. 10.1302/0301-620X.92B6.23621 [DOI] [PubMed] [Google Scholar]
- 19.Hamanishi M, Yasunaga Y, Yamasaki T, Mori R, Shoji T, Ochi M. The clinical and radiographic results of intertrochanteric curved varus osteotomy for idiopathic osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2014;134:305–10. 10.1007/s00402-013-1919-y [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Yamako G, Okada T, Arakawa H, Nakamura Y, Chosa E. Biomechanical effect of intertrochanteric curved varus osteotomy on stress reduction in femoral head osteonecrosis: a finite element analysis. J Orthop Surg Res. 2021;16:465. 10.1186/s13018-021-02614-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sakano S, Hasegawa Y, Torii Y, Kawasaki M, Ishiguro N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2004;86:359–65. 10.1302/0301-620X.86B3.14383 [DOI] [PubMed] [Google Scholar]
- 22.Ikemura S, Yamamoto T, Jingushi S, Nakashima Y, Mawatari T, Iwamoto Y. Leg-length discrepancy after transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2007;89:725–9. 10.1302/0301-620X.89B6.18499 [DOI] [PubMed] [Google Scholar]
- 23.Xu K, Li YM, Zhang HF, Wang CG, Xu YQ, Li ZJ. Computer navigation in total hip arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg. 2014;12:528–33. 10.1016/j.ijsu.2014.02.014 [DOI] [PubMed] [Google Scholar]
- 24.Takao M, Sakai T, Hamada H, Sugano N. Error range in proximal femoral osteotomy using computer tomography-based navigation. Int J Comput Assist Radiol Surg. 2017;12:2087–96. 10.1007/s11548-017-1577-6 [DOI] [PubMed] [Google Scholar]
- 25.Asano T, Takahashi D, Shimizu T, Irie T, Arai R, Terkawi MA, et al. A mathematical model for predicting postoperative leg shortening after curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. PLoS ONE. 2018;13:e0208818. 10.1371/journal.pone.0208818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osawa Y, Seki T, Okura T, Takegami Y, Ishiguro N, Hasegawa Y. Long-term outcomes of curved intertrochanteric varus osteotomy combined with bone impaction grafting for non-traumatic osteonecrosis of the femoral head. Bone Joint J. 2021;103–B:665–71. 10.1302/0301-620X.103B4.BJJ-2020-1107.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.