Abstract
We evaluated the protective role of passively transferred circulating antibodies in protecting non-human primates against experimental rotavirus infection. Pooled sera with rotavirus-specific IgG titers that were either high (1:10,000), intermediate (1:300), or negative (<1:25) were infused i.v. into naïve pigtailed macaques (ages 3-6 months). Rotavirus-specific IgG could be detected in the sera at 18 h in all animals infused with antibody-containing serum, and fecal IgG titers could be detected only in animals given high-titer pooled sera. When orally challenged with 106 fluorescent-forming units of a simian rotavirus strain, YK-1, at 18 h after serum transfer, control animals shed virus starting 1-3 days after challenge and continued to shed virus at high titers for 6-8 days, whereas passively immunized macaques did not shed virus or had delayed shedding at low titers for only a limited time. The observation that passively transferred antibodies can suppress or delay viral infection in rotavirus-challenged pigtailed macaques has important implications for the design and testing of parenteral candidate rotavirus vaccines.
Keywords: non-human primate, passive immunization
Rotavirus is the leading etiologic agent of severe gastroenteritis in infants and young children worldwide, estimated to cause 440,000 deaths and 140 million episodes of diarrhea each year (1, 2). Studies of the history of rotavirus disease suggest that natural or experimental infection induces immunity that can reduce the incidence and severity of subsequent episodes, indicating that rotavirus disease may be controlled through vaccination (3-6). The mechanisms responsible for immunity to rotavirus infections and illness are not completely understood, especially in humans. For immune protection against rotavirus, some believe that local immunity mediated by IgA and induced by an active infection is necessary, whereas others emphasize circulating antibodies mediated by IgG that, for other enteric infections such as polio and typhoid, can be induced by parenteral immunization.
Live oral vaccines that mimic the protection induced by natural infection have been successful in protecting against rotavirus disease, in part because they seem to induce local immunity in the intestine, which is considered a critical pathway for protection. However, two serious problems associated with live oral vaccines have been identified: the failure to be as immunogenic for children in the developing world and the rare complication of intussusception associated with the first licensed vaccine that may affect other candidate live oral vaccines as well (7-10).
These shortcomings of live oral vaccines have prompted consideration of a second generation of parenteral rotavirus vaccines derived from expressed proteins, virus-like particles, and inactivated rotavirus strains (11-14). The success of a parenteral vaccine might be determined by whether levels of circulating antibodies induced by the vaccine could also induce local protective immunity in the gut. Past studies with a variety of animal models have examined the relative importance of local and systemic antibodies in protection against rotavirus disease and infection (15-24). Some studies using passive immunization strategies have concluded that antibodies in the lumen of the small intestine were the primary determinant of resistance to rotavirus disease and that circulating serum antibodies failed to protect (19, 22-24). Other studies found that systemic rotavirus antibodies were protective when titers were sufficiently high, perhaps because of transcytosis of antibodies into the lumen of the gut (15, 23, 24). Each animal model has advantages and disadvantages for investigating protection against infection and disease, but none could reliably predict the situation in humans. To avoid some of the ambiguity of previous results, we developed a model for rotavirus infection and immunity in non-human primates that most closely resembles the conditions of gastro-intestinal pathophysiology, pharmacokinetics, and immune status found in humans (25).
In this study, we investigated the protective efficacy against rotavirus infection induced by passive transfer of rotavirus-specific IgG immune serum to pigtailed macaques. High- and midtiter immune sera and nonimmune serum were infused in young, rotavirus-seronegative pigtailed macaques, and the animals were subsequently challenged with a simian rotavirus. We hypothesized that if immune sera protected the macaques from rotavirus infection upon challenge, then circulating antibodies would play a critical role in immunity. This would suggest that a parenteral vaccine that elicits a robust response of serum antibodies might also have a protective effect against rotavirus infection and disease in humans.
Materials and Methods
Animals. Colony-bred pigtailed macaques (Macaca nemestrina) 3-6 months old and ≈1 kg in weight were housed in individual cages at the Yerkes National Primate Research Center of Emory University (Atlanta). The animals were maintained in accordance with standards set by the Committee on the Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources (National Research Council). The monkeys were fed daily with commercial monkey chow and fruits and were given water ad libitum. When necessary, animals were anesthetized with 10 mg of ketamine HCl per kg of body weight, injected intramuscularly. Before inclusion in this study, the animals were experimentally naïve and tested serologically negative for rotavirus-specific serum antibodies.
Virus. A cell culture-adapted simian rotavirus strain, YK-1 (VP7 serotype G3, VP4 phenotype P[5]), was obtained from a stool specimen of a pigtailed macaque (25, 26). A viral stock, passage 6, was prepared from YK-1-infected MA104 cells by freeze-thawing three times, centrifuging at 8,500 × g for clarification, and storing at -70°C. The viral titer of the stock was determined to be 5 × 108 fluorescent-forming units (ffu) per ml by a fluorescent focus assay. At the time of challenge, the viral stock was diluted in Dulbecco's modified Eagle's medium (D-MEM, GIBCO/BRL) to 106 ffu per 3 ml, a titer found to be infectious in our previous challenge study.
Passive Immunization and Viral Challenge. High- and midtiter rotavirus-specific IgG sera were obtained from experimentally and naturally infected pigtailed macaques, and nonimmune control sera were obtained from rotavirus-naïve macaques. High- and midtiter sera and nonimmune sera were individually pooled and heat-inactivated for 30 min at 56°C, after which they were passed through a 0.22-mm filter and stored at -70°C until use. The neutralizing titers correlated with rotavirus-specific IgG titers of the pooled sera, and rotavirus-specific IgA or IgM titers were undetectable in any of the three pooled sera (Table 1).
Table 1. Characteristics of pooled pigtailed macaque sera.
| Rotavirus-specific antibody titer
|
||||
|---|---|---|---|---|
| Group | IgG | IgA | IgM | Neut |
| High-titer | 10,000 | <25 | <25 | 15,000 |
| Midtiter | 300 | <25 | <25 | 1,000 |
| Nonimmune | <25 | <25 | <25 | <150 |
Neut, Neutralization titer.
The pigtailed macaques used in this study were divided randomly into three immunization groups (Table 2). The monkeys were infused i.v. with 5 ml of pooled serum per kilogram of animal weight 18 h before virus challenge. The viral inoculum was administered to anesthetized macaques by nasogastric intubation. Stomach acids were first neutralized by administration of 3 ml of a 10% sodium bicarbonate solution in water. After 10 min, the monkeys were inoculated with 106 ffu of YK-1 diluted in 3 ml of D-MEM, and the nasogastric tube was then flushed with 2 ml of D-MEM.
Table 2. Characteristics of pigtailed macaques.
| Macaque | Age, months | Weight, kg |
|---|---|---|
| High-titer group | ||
| H1 | 5 | 1.01 |
| H2 | 4 | 1.05 |
| H3 | 3 | 0.85 |
| Midtiter group | ||
| M1 | 3 | 0.88 |
| M2 | 6 | 1.74 |
| M3 | 6 | 1.16 |
| Nonimmune group | ||
| N1 | 4 | 0.80 |
| N2 | 4 | 1.05 |
| N3 | 4 | 1.18 |
| N4 | 6 | 1.20 |
| N5 | 6 | 1.46 |
Before and after challenge, animals were observed for any departure from normal behavior or appearance, such as inactivity or anorexia, and for abnormal symptoms, including vomiting and loose (unformed or semiliquid) or liquid stools. Serum and stool specimens were collected at appropriated days according to experimental design (Fig. 1). Blood samples were drawn by femoral venipuncture, and individual stool samples were collected from drop pans under each cage.
Fig. 1.
Experimental design: passive immunization of pigtailed macaques with pooled serum with rotavirus-specific IgG of high-titer, midtiter, or non-immune control. Macaques were infused with serum and 18 h later challenged with YK-1.
Sample Processing. For detection of rotavirus antigen, individual stool samples were processed as a 10% (wt/vol) solution with cold PBS (pH 7.4). For detection of fecal antibodies, specimens were initially diluted 50% (wt/vol) with cold PBS/0.1% Tween 20 (PBS-T) including a protease inhibitor mixture [final concentration of 5 mM phenylmethylsulfonyl fluoride, 2 mM iodoacetamide, and 1% aprotinin (all from Sigma)]. The samples were homogenized by vortex mixing and were centrifuged at 1,500 × g for 10 min, and the supernatants were then stored at -70°C until use.
Detection of Rotavirus Antigen in Stools. The presence of rotavirus antigen in fecal samples was determined by use of a commercial immunoassay (Rotaclone, Meridian Diagnostics, Cincinnati). Individual 10% (wt/vol) stool samples were tested, and all positive samples were retested with 10-fold dilutions in cold PBS to determine titers of fecal antigen. Specimens with absorbance (at 450 nm) units >0.100 were considered positive.
Detection of Rotavirus-Specific Antibodies in Serum and Stools. Rotavirus-specific IgA, IgG, and IgM were detected with an immunoassay using the YK-1 strain as the capture antigen. Microtiter plates (Immulon 2, Nalge Nunc) were coated with clarified supernatant (5 × 104 ffu per well) from YK-1-infected MA104 cells or with the clarified supernatant from mock-infected MA104 cells, both diluted in PBS (pH 7.4). The plates were incubated overnight at 4°C, after which the coating solution was discarded. The plates were blocked with 200 ml per well of PBS plus 5% FBS (blocking buffer) and incubated at 37°C for 30 min. The blocking buffer was then discarded. Diluted samples of serum or stool (100 ml per well) were added to the plates and incubated at room temperature for 2 h. Serum samples were diluted 1:25 and then 2-fold with PBS-T and 2% FBS (diluent buffer). Stool samples, initially processed to 50% (wt/vol), were diluted 10-fold and then 2-fold with PBS-T plus a protease inhibitor mixture. After incubation, the plates were washed three times with PBS-T, and then biotin-labeled goat anti-monkey IgA, IgM, or IgG (Research Diagnostics, Flanders, NJ) in diluent buffer was added at 100 ml per well and incubated for 1 h at room temperature. After the plates were washed three times with PBS-T, 100 ml per well of Eu-labeled streptavidin (PerkinElmer) diluted 1:5,000 in DELFIA assay buffer (PerkinElmer) was added, and the plates were incubated for 30 min at room temperature. The plates were washed five times with PBS-T and then incubated for 10 min with 100 ml per well of DELFIA enhancement solution (PerkinElmer). Time-resolved fluorescence was measured at 615 nm, by using a 1232 DELFIA fluorometer (Wallac, Turku, Finland). The titer was defined as the highest dilution that was at least 5 times and 104 counts per second over background (mock wells).
Detection of Serum Rotavirus Neutralization Titers. Neutralization assays were set up to measure the reduction in YK-1 infectivity as previously described (27). YK-1 infectivity was determined by an immunoassay for rotavirus antigen using a polyclonal rabbit anti-serum for rhesus rotavirus (RRV) as the primary antibody and a biotin-conjugated goat anti-rabbit IgG (Southern Biotechnology Associates) as the secondary antibody. Viral infectivity was determined by time-resolved fluorescence, using Eu-labeled streptavidin as described above. The neutralization titer of the serum was defined as the dilution at which there was a 70% reduction of viral antigen as compared with the control wells with no serum.
Statistical Analysis. Fecal viral shedding duration and titers among pigtailed macaques immunized with immune and nonimmune sera were compared by using the Mann-Whitney U test.
Results
Passive Immunization. Eleven pigtailed macaques, ages 3-6 months, were divided into three experimental groups that received serum with either high-titer (1:10,000) rotavirus-specific IgG, midtiter (1:300) rotavirus-specific IgG, or nonimmune control serum (rotavirus-specific IgG titer of <1:25). On the day after i.v. administration of the serum, cumulative titers of serum rotavirus-specific IgG directly reflected the titers of the infused serum (Fig. 2). Macaques infused with high-titer serum had rotavirus-specific IgG titers ranging from 1:800 to 1:1,600, macaques infused with midtiter serum had low rotavirus-specific IgG titers ranging from 1:50 to 1:100, and macaques infused with nonimmune control serum had no increase in detectable rotavirus-specific IgG. No detectable levels of serum rotavirus-specific IgA or IgM were measured in any monkeys immediately after infusion (data not shown).
Fig. 2.
Serum rotavirus-specific IgG titers of pigtailed macaques passively immunized with high-titer rotavirus-specific IgG (a), midtiter rotavirus-specific IgG (b), or nonimmune serum (c).
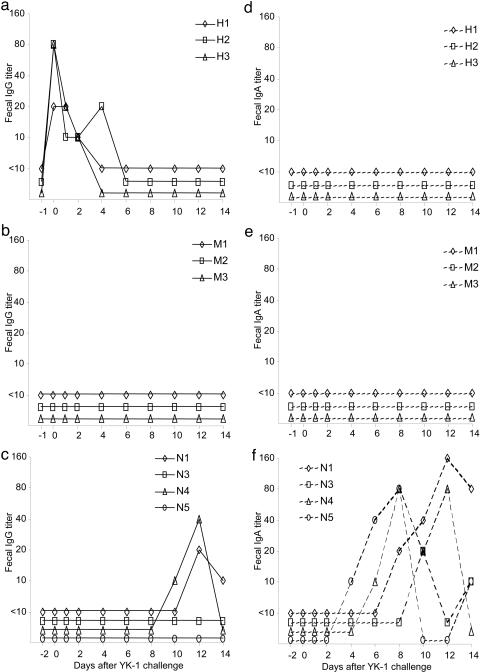
Rotavirus-specific IgG could be detected in the stools 1-3 days after i.v. infusion in macaques that were immunized with high-titer immune serum (Fig. 3a). No detectable rotavirus-specific IgG was observed in stools immediately after immunization of macaques with midtiter or nonimmune control serum (Fig. 3 b and c). Also, no fecal rotavirus-specific IgA was detected in any of the three experimental groups immediately after passive immunization (Fig. 3 d-f). The fact that no rotavirus-specific IgG was detected in the midtiter group may reflect the limits of detection for the assay.
Fig. 3.
Fecal rotavirus-specific IgG titers (a-c) and IgA titer (d-f) of pigtailed macaques passively immunized with high-titer rotavirus-specific IgG (a and d), midtiter rotavirus-specific IgG (b and e), or nonimmune serum (c and f).
Viral Challenge. We previously demonstrated that pigtailed macaques could be productively infected with the simian rotavirus strain YK-1 (25). In that study, viral shedding could be detected in the stools after YK-1 challenge, and the shedding duration and viral titers depended on the immune status of the monkey. Pigtailed macaques that were seropositive for rotavirus, either by natural or experimental infection, were protected from YK-1 challenge as demonstrated by a lack of viral shedding or by a significant reduction in viral titers and duration of viral shedding compared with that of seronegative macaques.
In this study, when pigtailed macaques were challenged with YK-1 after passive immunization with either a high- or a midtiter immune serum, the protective effect from viral infection was evident (Fig. 4 a and b). These animals shed virus in their stools for a short duration, 1-3 days, at low titers and at various time points after challenge. In contrast, macaques immunized with nonimmune serum were productively infected with YK-1 and shed virus at high titers beginning 1-2 days after challenge and for the duration of 6-9 days (Fig. 4c). The duration and peak viral titers of the macaques immunized with nonimmune serum were significantly different than those of macaques immunized with immune sera (P < 0.019 for duration and P < 0.015 for viral titers). One animal in the nonimmune control group, N2, was refractive to YK-1 challenge: detectable viral antigen was not observed in the stools of this animal over the course of the experiment. To determine whether the nonshedding pattern of macaque N2 was due to the inoculum or to procedural error, this macaque was rechallenged 40 days after initial challenge and, again, was refractive to YK-1 challenge and experienced no viral shedding. The shedding pattern of viral antigen from the nonimmune control group, except for macaque N2, resembled the typical pattern observed previously in seronegative pigtailed macaques (25). The shedding pattern from the groups immunized with immune serum closely resembled those from previously YK-1-challenged seropositive (rotavirus-specific serum IgG ≤1:50) pigtailed macaques, although the shedding pattern was somewhat sporadic. We determined that the virus shed from these macaques was YK-1 by RT-PCR with VP4 probes specific for YK-1 (data not shown) (26).
Fig. 4.
Rotavirus antigen shedding curves after YK-1 challenge of pigtailed macaques passively immunized with high-titer rotavirus-specific IgG (a), midtiter rotavirus-specific IgG (b), or nonimmune serum (c).
Immune Responses. In the groups infused with rotavirus-specific IgG (high- and midtiter serum), the initial titers of serum rotavirus-specific IgG waned with time, and titers of rotavirus-specific IgA and IgM did not increase, suggesting the absence of an active immune response to YK-1 challenge (Fig. 2 and data not shown). In contrast, in the group infused with nonimmune control serum, all animals that shed virus had a 4-fold or greater increase in rotavirus-specific serum IgG by 28 days after YK-1 challenge. Three of the four animals that shed virus had detectable rotavirus-specific serum IgM titers of 1:50 or greater at 14 days after challenge, and an IgA titer of >1:25 could be detected in three of these four macaques.
In the control group, active shedding of rotavirus was followed by a robust response of rotavirus-specific fecal IgA that began on days 4-10 after challenge (Fig. 3f). This response appeared at the time of resolution of viral shedding. A rotavirus-specific IgG titer could be detected in the stools of two of four macaques that shed virus (Fig. 3c). In contrast, none of the macaques that received rotavirus-specific IgG had a fecal IgA response (Fig. 3 d and e). Also, similar to the serum IgG titers, fecal IgG titers that were detectable only in the high-titer immunized group waned with time (Fig. 3a).
The one macaque from the control group that was refractive to YK-1 challenge and rechallenge maintained its preinfusion rotavirus specific titers of IgG (≤1:50), IgA (<1:25), and IgM (<1:25) throughout the trial, even after two challenges with YK-1. This was in contrast to previously challenged seropositive macaques that did not shed virus after challenge but demonstrated an anamnestic immune response with 4-fold increases of rotavirus-specific serum and fecal antibody titers.
Discussion
This study demonstrates that protection from rotavirus infection in a non-human primate model can be conferred by passive immunization with serum rotavirus-specific IgG. Both high- and midtiter serum (rotavirus-specific IgG titers of 1:10,000 and 1:300, respectively) prevented infection with simian rotavirus YK-1 in pigtailed macaques as determined not only by the decrease in viral shedding compared with that of controls, but also by the failure to mount a robust immune response to challenge. This protection could not be explained by alternative immunologic mechanisms such as local IgA in the mucosa of the gut or cell-mediated responses that have previously been suggested to be essential for protection (28-32). The role of serum antibodies in preventing rotavirus infections, as demonstrated in this study, could explain how maternal antibodies in infants protect children against severe rotavirus disease in the first few months of life.
Our observation of detectable rotavirus-specific IgG in the feces of macaques immunized with high-titer serum suggests a possible mechanism for this protection. The macaques' serum rotavirus-specific IgG titers after i.v. infusion correlated with the titers of the sera used for immunization. The levels also agreed with the expected titers, which were calculated by estimating that the monkeys have 80 ml of blood per kg of body weight and that they were infused with 5 ml of serum per kg of body weight and by determining that the half-life of macaque serum IgG seems to agree with the estimated half-life of 8.3 days for i.v. injected IgG in rhesus macaques (33). Rotavirus-specific IgG could be detected for 3-4 days in the feces of macaques immediately after infusion with high-titer serum only. The sensitivity of the immunoassay used to titer fecal rotavirus-specific IgG may account for the lack of detectable titers in macaques immunized with midtiter serum. Also, during normal catabolism of IgG, the rate of IgG turnover increases as the amount of serum IgG rises (34, 35). Turnover occurs in endothelial cells when IgG is taken up by fluid-phase endocytosis and transported by FcRn receptors (35). The fate of endocytosed IgG varies depending on the concentration of internalized IgG and is directly proportional to the concentration in serum. With modest IgG levels, transport of IgG may be bidirectional and either recycled or delivered to the intestinal lumen. When IgG levels are high, internalized IgG binding to FcRn becomes limiting, and unbounded IgG is mostly degraded in the lysosomes of endothelial cells found in the arterioles and capillaries of muscle and liver. In intestinal endothelial cells, most of the excess IgG may be transported to the intestinal lumen for clearance of IgG (16, 35, 36). Thus, rotavirus-specific IgG from the infused sera may prevent rotavirus infection by preventing attachment to susceptible cells in the gut and/or by blocking steps of the virus life cycle inside infected intestinal endothelial cells during the transcytosis of IgG. This is similar to mechanisms suggested in studies with rotavirus-challenged immunized mice with impaired mucosal transporters of IgA and IgM (37). It has been documented that both IgG and IgA can be detected in the intestinal lumen (38).
It would have been of interest to rechallenge the passively immunized macaques after serum antibody levels had waned to determine whether the monkeys were still immunologically naïve and susceptible to rotavirus infection. Although viral antigen in fecal specimens could be occasionally detected in macaques that were infused with immune serum, the viral shedding was delayed, short in duration, and at low titers. The delayed shedding patterns could be the result of an abortive infection or reinfection spread within the facility. All immunized and control macaques were housed in separate cages with no physical contact among monkeys, but in previous experiments with infected and naïve animals, a nosocomial infection had occurred (unpublished results). However, the passively immunized macaques still demonstrated protection from the possible nosocomial reinfection, because reduced shedding patterns were similar to the protective effect seen upon rechallenges of previously exposed seropositive monkeys (25).
We have established a rotavirus infection model in non-human primates in which high titers of rotavirus antigen can be detected in the stools 1-10 days after exposure (25). This model has several limitations, the most poignant of which is that it is not a disease model and none of the monkeys developed diarrhea. Although we had hoped to ideally establish a disease model to test for vaccine effectiveness, information about the pathogenesis of symptoms of disease may not be essential. Once an infection is established, the immune responses, achieved by immunization or previous infections, will neither eliminate the pathogen nor treat the symptoms of the disease, although the immune response can diminish the severity of symptoms (6). Also, in our study, one monkey in the control group was refractive to rotavirus infection. This animal did not become infected after YK-1 challenge and rechallenge or mount an immune response to rotavirus. It would have been of interest to determine what host or viral factors contributed to this refractive condition and to investigate whether such conditions occur in humans, because the answer could impact the use of live oral vaccines or protection against disease.
Early studies of passive immunization that tried to establish the importance of circulating antibodies in preventing rotavirus infection yielded conflicting results (15, 19). Besser et al. (15) demonstrated that circulating IgG could appear in the intestines of neonatal calves and could prevent infection and disease, whereas Offit and Clark (19) demonstrated, in suckling mice, that orally administered IgG, but not circulating derived IgG, could protect against infection. Offit and Clark (19) did not, however, look for rotavirus-specific IgG in the intestine of the suckling mice, which may not have mature intestinal endothelial cells for the transcytosis of IgG. Other studies with rabbits and infant mice (6 weeks old) demonstrated that parenteral vaccination prevented rotavirus infection and was associated with the presence of rotavirus-specific IgG in the intestine (11, 39).
The finding that IgG plays a protective role in rotavirus infection has clear implications for rotavirus vaccine development. Although parenteral vaccines for other enteric pathogens, such as polio and cholera, induce good immunity and protection, oral vaccines for enteric pathogens have been preferred, in part because they seem to induce the best local immunity in the intestine, which mimics the immune responses seen after natural infections and is considered more important for protection against disease. However, nonoral vaccines can induce good protective immunity against rotavirus infections when rotavirus-specific IgG levels are amply elevated to reach the gut (11). Parenteral vaccines have also been demonstrated to induce IgM and IgA response, B cell response, and T cell response (both CD4 and CD8 memory cells), which have been shown to localize to the gut (11, 39-43).
Many licensed vaccines confer protective immunity by eliciting serum IgG antibodies that inactivate the pathogen on mucosal surfaces. Although vaccines may induce more than one immune component, vaccines are standardized only by measurement of serum antibodies (44). This implies that serum IgG antibodies, whether passively acquired or actively induced, are a good proxy for determining protection against infection and that an effective vaccine should induce sufficient levels of antibody. A critical level of serum IgG also will inhibit the development of active immunity because these antibodies will prevent the virus from replicating to yield a large immunogenic stimulus, similar to what is seen with maternal antibodies in the prevention of rotavirus infection early in life (23, 24). This may also explain why oral rotavirus vaccines are generally less immunogenic and effective in infants with high rotavirus antibody titers, such as those immunized at an early age or perhaps children in developing countries. Most importantly, if live oral vaccines fail in developing countries or if intussusception occurs with use of another live oral vaccine, a parenteral vaccine that induces robust circulating immune responses could play an important role in the next generation of rotavirus vaccines. Here we provide a sound scientific basis for candidate rotavirus vaccines, such as inactivated viruses, expressed proteins, virus-like particles, and DNA vaccines, that can be administered parenterally and can induce a robust immune response to provide protection against rotavirus without the risk of intussusception and in settings where live oral vaccine may work less well.
Acknowledgments
This work is dedicated to the memory of Dr. Harold M. McClure (1937-2004). We thank Drs. Rafi Ahmed, Aftab Ansari, and Jon Gentsch for helpful discussions; the staff at Yerkes National Primate Research Center for assistance with the monkeys; and Claudia Chesley for editorial assistance. This work was supported by a Cooperative Research and Development Agreement with Aventis Pasteur and in part by Yerkes Base Grant RR00165.
Author contributions: L.E.W., H.M.M., B.J., J.W.A., and R.I.G. designed research; L.E.W. and H.M.M. performed research; L.E.W. and J.W.A. contributed new reagents/analytic tools; L.E.W., H.M.M., B.J., and R.I.G. analyzed data; and L.E.W. and R.I.G. wrote the paper.
Abbreviation: ffu, fluorescent-forming units.
References
- 1.Kapikian, A. Z., Hoshino, Y. & Chanock, R. M. (2001) in Fields Virology, eds. Knipe, D. M. & Howley, P. M. (Lippincott, Philadelphia), Vol. 2, pp. 1787-1833. [Google Scholar]
- 2.Parashar, U. D., Hummelman, E. G., Bresee, J. S., Miller, M. A. & Glass, R. I. (2003) Emerg. Infect. Dis. 9, 565-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernstein, D. I., Sander, D. S., Smith, V. E., Schiff, G. M. & Ward, R. L. (1991) J. Infect. Dis. 164, 277-283. [DOI] [PubMed] [Google Scholar]
- 4.Bishop, R. F., Barnes, G. L., Cipriani, E. & Lund, J. S. (1983) N. Engl. J. Med. 309, 72-76. [DOI] [PubMed] [Google Scholar]
- 5.Ward, R. L. (1996) J. Infect. Dis. 174, Suppl. 1, S51-S58. [DOI] [PubMed] [Google Scholar]
- 6.Velazquez, F. R., Matson, D. O., Calva, J. J., Guerrero, L., Morrow, A. L., Carter-Campbell, S., Glass, R. I., Estes, M. K., Pickering, L. K. & Ruiz-Palacios, G. M. (1996) N. Engl. J. Med. 335, 1022-1028. [DOI] [PubMed] [Google Scholar]
- 7.Clark, H. F., Offit, P. A., Ellis, R. W., Eiden, J. J., Krah, D., Shaw, A. R., Pichichero, M., Treanor, J. J., Borian, F. E., Bell, L. M. & Plotkin, S. A. (1996) J. Infect. Dis. 174, S73-S80. [DOI] [PubMed] [Google Scholar]
- 8.Cunliffe, N. A., Kilgore, P. E., Bresee, J. S., Steele, A. D., Luo, N., Hart, C. A. & Glass, R. I. (1998) Bull. W. H. O. 76, 525-537. [PMC free article] [PubMed] [Google Scholar]
- 9.De Mol, P., Zissis, G., Butzler, J. P., Mutwewingabo, A. & Andre, F. E. (1986) Lancet 328, 108. [DOI] [PubMed] [Google Scholar]
- 10.Murphy, T. V., Gargiullo, P. M., Massoudi, M. S., Nelson, D. B., Jumaan, A. O., Okoro, C. A., Zanardi, L. R., Setia, S., Fair, E., LeBaron, C. W., et al. (2001) N. Engl. J. Med. 344, 564-572, and erratum (2001) 344, 1564. [DOI] [PubMed] [Google Scholar]
- 11.Conner, M. E., Crawford, S. E., Barone, C. & Estes, M. K. (1993) J. Virol. 67, 6633-6641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conner, M. E., Zarley, C. D., Hu, B., Parsons, S., Drabinski, D., Greiner, S., Smith, R., Jiang, B., Corsaro, B., Barniak, V., Madore, H. P., Crawford, S. & Estes, M. K. (1996) J. Infect. Dis. 174, S88-S92. [DOI] [PubMed] [Google Scholar]
- 13.Herrmann, J. E., Chen, S. C., Fynan, E. F., Santoro, J. C., Greenberg, H. B., Wang, S. & Robinson, H. L. (1996) J. Infect. Dis. 174, S93-S97. [DOI] [PubMed] [Google Scholar]
- 14.McNeal, M. M., Rae, M. N. & Ward, R. L. (1999) Vaccine 17, 639-645. [DOI] [PubMed] [Google Scholar]
- 15.Besser, T. E., Gay, C. C., McGuire, T. C. & Evermann, J. F. (1988) J. Virol. 62, 2238-2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Besser, T. E., McGuire, T. C., Gay, C. C. & Pritchett, L. C. (1988) J. Virol. 62, 2234-2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burns, J. W., Krishnaney, A. A., Vo, P. T., Rouse, R. V., Anderson, L. J. & Greenberg, H. B. (1995) Virology 207, 143-153. [DOI] [PubMed] [Google Scholar]
- 18.Conner, M. E., Estes, M. K. & Graham, D. Y. (1988) J. Virol. 62, 1625-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Offit, P. A. & Clark, H. F. (1985) J. Virol. 54, 58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Offit, P. A., Clark, H. F., Kornstein, M. J. & Plotkin, S. A. (1984) J. Virol. 51, 233-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saif, L. J., Ward, L. A., Yuan, L., Rosen, B. I. & To, T. L. (1996) Arch. Virol. Suppl. 12, 153-161. [DOI] [PubMed] [Google Scholar]
- 22.Snodgrass, D. R. & Wells, P. W. (1976) Arch. Virol. 52, 201-205. [DOI] [PubMed] [Google Scholar]
- 23.Barrandeguy, M., Parreno, V., Lagos Marmol, M., Pont Lezica, F., Rivas, C., Valle, C. & Fernandez, F. (1998) Dev. Biol. Stand. 92, 253-257. [PubMed] [Google Scholar]
- 24.Snodgrass, D. R., Campbell, I., Mwenda, J. M., Chege, G., Suleman, M. A., Morein, B. & Hart, C. A. (1995) Vaccine 13, 408-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westerman, L. E., Xu, Y., McClure, H. M., Jiang, B. & Glass, R. (2004) J. Med. Virol. 75, 616-625. [DOI] [PubMed] [Google Scholar]
- 26.Tatti, K. M., Gentsch, J., Shieh, W. J., Ferebee-Harris, T., Lynch, M., Bresee, J., Jiang, B., Zaki, S. R. & Glass, R. (2002) J. Virol. Methods 105, 305-319. [DOI] [PubMed] [Google Scholar]
- 27.Ishida, S., Feng, N., Tang, B., Gilbert, J. M. & Greenberg, H. B. (1996) J. Clin. Microbiol. 34, 1694-1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coulson, B. S., Grimwood, K., Hudson, I. L., Barnes, G. L. & Bishop, R. F. (1992) J. Clin. Microbiol. 30, 1678-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng, N., Burns, J. W., Bracy, L. & Greenberg, H. B. (1994) J. Virol. 68, 7766-7773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franco, M. A. & Greenberg, H. B. (1995) J. Virol. 69, 7800-7806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franco, M. A., Tin, C., Greenberg, H. B., Franco, M. A. & Greenberg, H. B. (1997) J. Virol. 71, 4165-4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Ryan, M. L., Matson, D. O., Estes, M. K. & Pickering, L. K. (1994) J. Infect. Dis. 169, 504-511. [DOI] [PubMed] [Google Scholar]
- 33.Challacombe, S. J. & Russell, M. W. (1979) Immunology 36, 331-338. [PMC free article] [PubMed] [Google Scholar]
- 34.Brambell, F. W., Hemmings, W. A. & Morris, I. G. (1964) Nature 203, 1352-1354. [DOI] [PubMed] [Google Scholar]
- 35.Rojas, R. & Apodaca, G. (2002) Nat. Rev. Mol. Cell Biol. 3, 944-955. [DOI] [PubMed] [Google Scholar]
- 36.Ghetie, V. & Ward, E. S. (2000) Annu. Rev. Immunol. 18, 739-766. [DOI] [PubMed] [Google Scholar]
- 37.Schwartz-Cornil, I., Benureau, Y., Greenberg, H., Hendrickson, B. A. & Cohen, J. (2002) J. Virol. 76, 8110-8117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bull, D. M., Bienenstock, J. & Tomasi, T. B., Jr. (1971) Gastroenterology 60, 370-380. [PubMed] [Google Scholar]
- 39.Johansen, K., Schroder, U. & Svensson, L. (2003) Vaccine 21, 368-375. [DOI] [PubMed] [Google Scholar]
- 40.Coffin, S. E., Clark, S. L., Bos, N. A., Brubaker, J. O. & Offit, P. A. (1999) J. Immunol. 163, 3064-3070. [PubMed] [Google Scholar]
- 41.Coffin, S. E., Klinek, M. & Offit, P. A. (1995) J. Infect. Dis. 172, 874-878. [DOI] [PubMed] [Google Scholar]
- 42.Masopust, D., Vezys, V., Usherwood, E. J., Cauley, L. S., Olson, S., Marzo, A. L., Ward, R. L., Woodland, D. L. & Lefrancois, L. (2004) J. Immunol. 172, 4875-4882. [DOI] [PubMed] [Google Scholar]
- 43.McNeal, M. M., VanCott, J. L., Choi, A. H., Basu, M., Flint, J. A., Stone, S. C., Clements, J. D. & Ward, R. L. (2002) J. Virol. 76, 560-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robbins, J. B., Schneerson, R. & Szu, S. C. (1995) J. Infect. Dis. 171, 1387-1398. [DOI] [PubMed] [Google Scholar]