Abstract
Ebola viruses contain a single glycoprotein (GP) spike, which functions as a receptor binding and membrane fusion protein. It contains a highly conserved hydrophobic region (amino acids 524 to 539) located 24 amino acids downstream of the N terminus of the Ebola virus GP2 subunit. Comparison of this region with the structural features of the transmembrane subunit of avian retroviral GPs suggests that the conserved Ebola virus hydrophobic region may, in fact, serve as the fusion peptide. To test this hypothesis directly, we introduced conservative (alanine) and nonconservative (arginine) amino acid substitutions at eight positions in this region of the GP2 molecule. The effects of these mutations were deduced from the ability of the Ebola virus GP to complement the infectivity of a vesicular stomatitis virus (VSV) lacking the receptor-binding G protein. Some mutations, such as Ile-to-Arg substitutions at positions 532 (I532R), F535R, G536A, and P537R, almost completely abolished the ability of the GP to support VSV infectivity without affecting the transport of GP to the cell surface and its incorporation into virions or the production of virus particles. Other mutations, such as G528R, L529A, L529R, I532A, and F535A, reduced the infectivity of the VSV-Ebola virus pseudotypes by at least one-half. These findings, together with previous reports of liposome association with a peptide corresponding to positions 524 to 539 in the GP molecule, offer compelling support for a fusion peptide role for the conserved hydrophobic region in the Ebola virus GP.
Ebola viruses cause severe hemorrhagic fever in humans and other primates, resulting in high mortality rates (6, 20). The viruses belong to the family Filoviridae, genus Filovirus, which also includes Marburg virus. Ebola viruses are filamentous, enveloped, and nonsegmented negative-stranded RNA viruses (6, 20). The viral genome is approximately 19 kb in length and encodes seven structural proteins: nucleoprotein, VP35, VP40, glycoprotein (GP), VP30, VP24, and large protein. The Ebola virus GP is a highly glycosylated, type-I transmembrane protein containing both N- and O-linked carbohydrates (5–7). Recently, two groups independently demonstrated the cleavage of Ebola virus GP into disulfide-linked GP1 and GP2 subunits (23, 27). The Ebola virus GP is the only transmembrane protein that forms spike projections on the virion surface, and it is responsible for receptor binding and membrane fusion, leading to virus penetration (26).
Recently, we developed a novel vesicular stomatitis virus (VSV) system that can be used to study the function of Ebola virus GPs during the early steps of infection (26). This system relies upon a recombinant form of VSV (VSVΔG*) that contains the green fluorescent protein gene instead of the G protein gene, and thus is not infectious unless a receptor binding and fusion protein is provided in trans. We have shown that Ebola virus GP confers infectivity to the mutant VSV, to the extent that the complemented virus infects primate cells more efficiently than avian, insect, and other mammalian cells, corresponding to the host range tropism of Ebola virus (26). Similar complementation systems have been developed for the Ebola virus GP with the use of retroviruses (33, 34).
Since fusion between the viral envelope and cellular membranes is a critical event in the initiation of virus infection, identification of the fusion domain is essential for understanding the overall process of virus replication. The fusion domain of viral proteins generally consists of a stretch of hydrophobic amino acids (13, 31). For example, with influenza virus hemagglutinin (HA), the hydrophobic amino terminus of HA 2 generated by proteolytic cleavage serves as the fusion domain (12, 25). In contrast, the VSV G protein has an internal hydrophobic region (i.e., no proteolytic processing of the protein) that participates in cell fusion events (8, 36). The Ebola virus GP comprises five hydrophobic regions, one of which (extending from position 524 to 539) is highly conserved among filoviruses and associates with liposomes (21). Gallaher (11) tentatively identified this region as the fusion domain, based on the similarity of its topological position to that of the retroviral transmembrane domain, but this relationship has not been substantiated with direct experimental evidence.
The fusion domains of some viral proteins have been studied by experimental mutagenesis and evaluation of polykaryon formation (8–10, 12, 14, 15, 17, 18, 24, 25, 36). However, because expression of Ebola virus GP on the cell surface does not induce polykaryon formation, regardless of the pH to which the GP is exposed (26), we could not use this or similar assays to identify the fusion domain of the Ebola virus GP. Thus, we introduced amino acid substitutions into the putative fusion domain of the Ebola virus GP and examined the effect of these substitutions on the infectivity of VSVΔG* complemented with a GP mutant. The results suggest that the amino acids at position 524 to 539 do, in fact, constitute the fusion domain of the Ebola virus GP.
Expression of the mutant Ebola GPs.
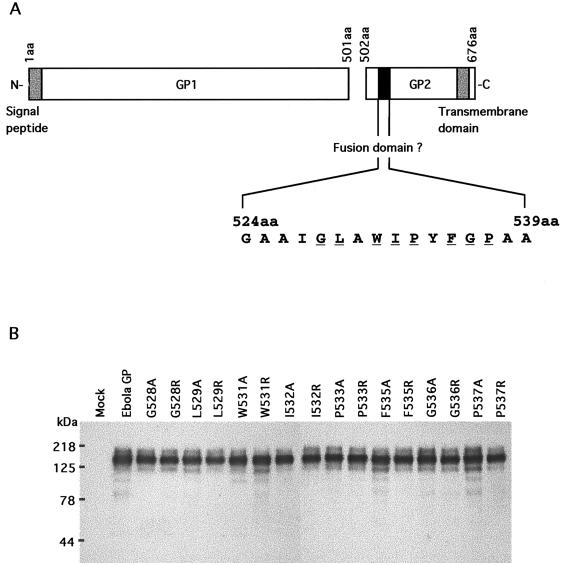
To identify the fusion domain of Ebola virus GP, we introduced conservative (Ala) and nonconservative (Arg) mutations at highly hydrophobic amino acids (positions 528-Gly, 529-Leu, 531-Trp, 532-Ile, 533-Pro, 535-Phe, 536-Gly, and 537-Pro, which are identical in Ebola and Marburg viruses) (Fig. 1A). We first expressed the mutant Ebola virus GPs in 293T cells and analyzed them by Western blotting using anti-Ebola virus GP/secreted GP (SGP) antibody (Fig. 1B). All of the mutant Ebola GPs were expressed in 293T cells, in amounts and with molecular weights that approximated those of the wild-type Ebola GP.
FIG. 1.
(A) Schematic representation of the Ebola virus GP. The Ebola virus GP is cleaved at amino acid position 501 into GP1 and GP2 by furin (23, 27). The signal peptide and the transmembrane domain are represented by shaded boxes. The putative fusion domain is designated by a black box, and its amino acid sequence is indicated underneath in single-letter code. (B) Expression of wild-type Ebola virus GP and its mutants. Human embryonic kidney 293T cells were transfected with a plasmid expressing Ebola virus GP or its mutants and were lysed in a sample buffer. A full-length cDNA encoding the Ebola virus (Zaire subtype) GP (Ebola GP) (22) was cloned into a mammalian expression vector, pCAGGS/MCS (19), with the resulting construct designated pCEboZGP. Proteins in lysates were separated on sodium dodecyl sulfate–8% polyacrylamide gel electrophoresis, transferred to a polyvinylidene difluoride membrane, and detected by anti-Ebola virus GP-SGP rabbit serum. Molecular masses of the proteins are shown on the left. The mutant Ebola virus GPs were designated according to their respective amino acid mutations (e.g., G528A denotes a mutant GP containing a Gly-to-Ala amino acid substitution at position 528).
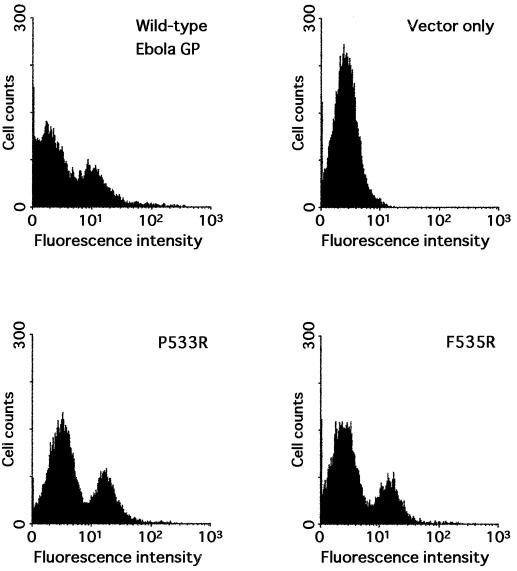
The mutations we introduced had the potential to affect protein processing, including folding and oligomerization, and therefore might have inhibited the transport of GPs to the cell surface, as well as their incorporation into VSV particles (reviewed in reference 3). Therefore, we next examined the cell surface expression of wild-type and mutant Ebola virus GPs by flow cytometry. Figure 2 shows flow cytometric results for the wild-type and a representative sample of mutant Ebola virus GPs. There were no discernible differences in cell surface GP expression between the wild-type and modified Ebola GPs, suggesting that mutations introduced in the putative fusion domain of the Ebola virus GP did not adversely affect the processing, intracellular transport, and overall conformation of the resulting mutants.
FIG. 2.
Flow cytometric analysis of the cell surface expression of wild-type Ebola virus GP and its mutants. Ebola virus GP-expressing 293T cells were incubated with anti-Ebola virus GP-SGP rabbit serum and then stained with fluorescein isothiocyanate-conjugated anti-rabbit immunogloblin.
Incorporation of mutant Ebola virus GPs into recombinant VSV particles.
To investigate the efficiency of incorporation of mutant Ebola virus GPs into VSV particles, we analyzed, by Western blotting, the supernatants of GP-expressing cells that were superinfected with VSVΔG*-G (Fig. 3). With only a few exceptions, the amounts of mutant and wild-type Ebola virus GPs incorporated into VSV particles were approximately equivalent, indicating that manipulation of the hydrophobic region of the Ebola virus GP did not appreciably affect the protein’s incorporation into VSV particles. However, a glycine-to-arginine mutation at position 536 resulted in a lower level of GP incorporation into virions, whereas a glycine-to-alanine substitution had no effect. At positions 531 and 533, both alanine and arginine substitutions reduced the incorporation of mutant Ebola virus GPs into VSV particles.
FIG. 3.
Incorporation of wild-type Ebola virus GP and its mutants into VSV particles. VSVΔG* complemented with Ebola virus GP and its mutants prepared as described previously (26) were partially purified by centrifugation through 25% sucrose and were lysed in a sample buffer. Viral proteins were separated by sodium dodecyl sulfate–8% polyacrylamide gel electrophoresis, transferred to a polyvinylidene difluoride membrane, and detected by anti-VSV M protein monoclonal antibody and anti-Ebola virus GP/SGP serum. Bound antibodies were detected with a VECTASTAIN ABC kit (Vector) and the Western immunoblot ECL system (Amersham). The image on the X-ray film was scanned with a CCD camera. Molecular masses of the proteins are shown on the left.
Effect of amino acid substitutions on the infectivity of VSVΔG*-Ebola virus GPs.
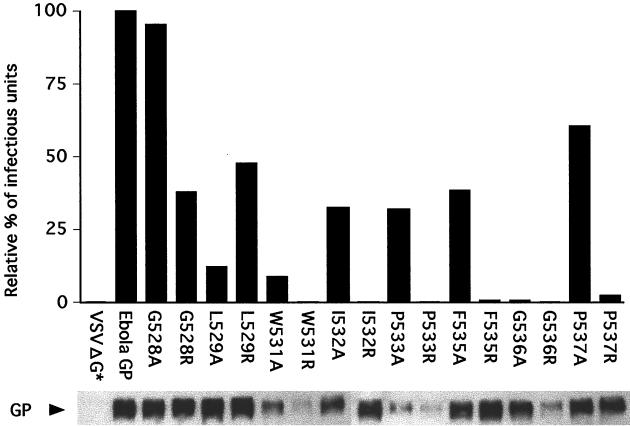
To test the effects of amino acid substitutions on the activity of the putative fusion domain of Ebola virus GP, we examined the infectivity of VSVΔG* complemented with either wild-type or mutant Ebola virus GP in 293 cells (Fig. 4). The wild-type GP control virus had an infectivity titer of 1.2 × 106 infectious units/ml, as judged by the expression of green fluorescent protein. Among the Ebola virus GP mutants we studied, I532R, F535R, G536A, and P537R lost essentially all of their capacity to confer infectivity to VSVΔG*, while G528R, L529A, L529R, I532A, and F535A showed reductions of 12 to 48% (Fig. 4). Four mutant Ebola virus GPs, W531A, W531R, P533R, and G536R, were poorly incorporated into VSV particles, and hence did not efficiently confer infectivity to VSVΔG* (0 to 8.7%); however, P533A was 32% as efficient as wild-type Ebola virus GP in complementing the infectivity of VSVΔG*, even though its incorporation into virions was poor. These results suggest that most of the amino acid residues in the region extending from 524 to 539 are critical for Ebola virus GP function, most likely fusion with the cellular membrane.
FIG. 4.
Infectivity in 293 cells of recombinant VSV complemented with wild-type Ebola virus GP or its mutants. The infectivity of recombinant viruses was determined as described (26) and is reported as the percentage of infectious units, calculated from the number of green-fluorescent-positive cells in 10 microscopic fields. Each result is the average of two independent experiments.
In the model proposed by Gallaher (11), the highly hydrophobic putative fusion domain of Ebola virus lies within a 23- to 38-amino-acid region downstream of the amino terminus of GP2. Here we show that this region is indeed critical for viral entry into cells. With the exception of Ebola virus GPs bearing a substitution at position 531 or 533, at least one of the mutants we constructed for each target position was incorporated into VSV particles as efficiently as the wild-type GP. Importantly, most of these constructs had lost at least 50% of their ability to confer infectivity to a VSV lacking its receptor binding protein, and some showed essentially no activity in this regard (Fig. 4). Experimental mutation of the corresponding region of the transmembrane subunit of avian sarcoma virus (at amino acid positions 21 to 42) likewise produced a striking loss of fusion activity (14). Ruiz-Arguello et al. (21) additionally showed that a synthetic peptide modeled on the putative fusion domain of Ebola virus GP interacts and fuses with lipid vesicles. Taken together, these results strongly promote the fusion domain candidacy of positions 524 to 539 in the Ebola virus GP, although one cannot completely eliminate the possibility that mutations introduced into this domain could have negatively affected GP functions other than fusion.
Several mutant Ebola virus GPs (W531A, W531R, P533A, P533R, and G536R) were poorly incorporated into VSV particles for currently unknown reasons. Amino acid changes in viral glycoproteins can inhibit protein folding and oligomerization, which are prerequisites for the intracellular transport of viral GPs (reviewed in reference 3). Although we did not assess the GP mutants for these characteristics, they were all efficiently transported to the cell surface (Fig. 2), such that folding and oligomerization do not appear to have been affected by the amino acid substitutions tested in the present study. Interestingly, the titers of the recombinant VSV complemented with P533A retained 32% of the infectivity associated with wild-type Ebola virus GP, even though this mutant was poorly incorporated into VSV particles (30% of wild type). Thus, this level of Ebola virus GP incorporated into the recombinant VSV particles may be sufficient to permit binding to the cellular receptor and fusion with the cellular membrane. If so, the results obtained with another GP mutant, W531A, which was both poorly incorporated into VSV particles and incapable of conferring infectivity, would suggest that position 531 affects fusion activity.
The Ebola virus GP mutants with a conservative hydrophobic alanine substitution at Ile-532 or Phe-535 retained the ability to support the infectivity of recombinant VSVs at nearly one-third the wild-type level, whereas those with a nonconservative arginine substitution lost this ability almost entirely. This drastic reduction in infectivity as a result of nonconservative substitutions may reflect an overall reduction in hydrophobicity in this region, leading to a reduction in virus-cell fusion activity. If so, the hydrophobicity of amino acid residues at positions 532 and 535 would be critical for fusion activity. A similar reduction of cell-to-cell fusion activity associated with a change from hydrophobic to hydrophylic residues has been reported for the fusion peptides of human immunodeficiency virus type 1 (9) and simian immunodeficiency virus (1).
In general, fusion peptides are rich in alanine and glycine residues. In this study, we substituted alanine and arginine for the conserved glycines at positions 528 and 536. The mutation at position 536 reduced the infectivity of the VSVΔG*-Ebola virus GP to a near background level, whereas the mutation at 528 had a less pronounced effect. Glycine-to-alanine substitutions have also been introduced into other viral fusion peptides. In the simian immunodeficiency virus (1) and simian virus 5 (15) fusion peptides, such mutations increased cell-to-cell fusion activity, while the same types of mutations negatively affected the fusion of VSV (8, 36) and Semliki Forest virus (SFV) (17) fusion proteins, shifting the pH threshold of fusion to a more acidic range. Although the precise mechanisms of these effects are unknown, glycine-to-alanine substitutions in the latter proteins may have increased the stability of the fusion peptide such that increased acidity was required to destabilize and expose the fusion peptide. The glycine-to-alanine mutation at position 536 in the Ebola virus GP may have exerted the same effect as those in VSV and SFV fusion peptides.
Some viral fusion peptides located in the middle of the polypeptide chain generally contain proline residues (31) (e.g., VSV G [8, 36], SFV E1 [17], and avian leukosis and sarcoma virus TM subunits [14]). The putative fusion peptide of Ebola virus GP also contains two prolines (at positions 533 and 537). A Pro-to-Asp mutation at position 127 in the VSV G fusion peptide shifted the optimal pH toward the acidic range (8), likely blocking the interaction of the peptide with the cellular membrane; a lower pH may have permitted the fusion by neutralizing the charged residue. A Pro-to-Ala substitution at position 533 or 537 reduced the infectivity of VSVΔG*-Ebola virus GP to 32 and 61% of the wild-type level, respectively, whereas a Pro-to-Arg substitution at either of these positions almost completely abolished infectivity. However, because substitutions at position 533 reduced the efficiency of GP incorporation into VSV particles, we could not evaluate the effect of this mutation. Hence, we conclude that the proline residue at position 537 in the Ebola virus GP fusion peptide is important for fusion to the cellular membrane.
Expression of the intact Ebola virus GP does not induce polykaryon formation (cell-to-cell fusion) at any pH, for unknown reasons. Recently, Lavillette et al. (16) showed that the region in the receptor-binding subunit of murine leukemia virus, which is responsible for association with the transmembrane subunit, is critical for cell-to-cell fusogenicity. There must be multiple regions responsible for noncovalent interactions between the Ebola virus GP1 and GP2, even though these subunits are tethered by disulfide bonds (23, 27). We suggest that the nature of GP1-GP2 interaction may be responsible for the lack of cell-to-cell fusion in eukaryotic cells expressing the Ebola virus GP.
In other viral fusion proteins, it is not only the fusion peptide, but also the heptad repeat region, that makes important contributions to fusion activity (2, 4, 24, 30), as demonstrated by studies with synthetic peptides corresponding to this region (32, 35). The predicted structure of Ebola virus GP2 also suggests the presence of a heptad repeat region, probably forming a coiled coil in the trimer of Ebola virus GP (11). Weissenhorn et al. (28) showed that a polypeptide corresponding to the 553- to 650-amino-acid region of Ebola virus GP2 formed a highly α-helical and rod-like trimer when expressed in Escherichia coli; this result was subsequently confirmed by X-ray crystallography (29). This group also demonstrated that the trimeric structure of Ebola virus GP2 consists of a triple-stranded α-helical coiled-coil region corresponding to the heptad repeat region (residues 552 to 595). Thus, the Ebola virus GP2 structure is quite similar to that of the transmembrane subunits of other viral fusion proteins, suggesting that the fusion process during Ebola virus infection may mirror that of influenza virus and human immunodeficiency virus infections.
Acknowledgments
We thank Krisna Wells and Martha McGregor for excellent technical assistance and John Gilbert for editing the manuscript. Automated sequencing was performed at the University of Wisconsin Biotechnology Center.
Support for this work came from NIAID Public Health Service research grants.
REFERENCES
- 1.Bosch M L, Earl P L, Fargnoli K, Picciafuoco S, Giombini F, Wong-Staal F, Franchini G. Identification of the fusion peptide of primate immunodeficiency viruses. Science. 1989;244:694–697. doi: 10.1126/science.2541505. [DOI] [PubMed] [Google Scholar]
- 2.Chen S S, Lee C N, Lee W R, McIntosh K, Lee T H. Mutational analysis of the leucine zipper-like motif of the human immunodeficiency virus type 1 envelope transmembrane glycoprotein. J Virol. 1993;67:3615–3619. doi: 10.1128/jvi.67.6.3615-3619.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doms R W, Lamb R A, Rose J K, Helenius A. Folding and assembly of viral membrane proteins. Virology. 1993;193:545–562. doi: 10.1006/viro.1993.1164. [DOI] [PubMed] [Google Scholar]
- 4.Dubay J W, Roberts S J, Brody B, Hunter E. Mutations in the leucine zipper of the human immunodeficiency virus type 1 transmembrane glycoprotein affect fusion and infectivity. J Virol. 1992;66:4748–4756. doi: 10.1128/jvi.66.8.4748-4756.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feldmann H, Will C, Schikore M, Slenczka W, Klenk H D. Glycosylation and oligomerization of the spike protein of Marburg virus. Virology. 1991;182:353–356. doi: 10.1016/0042-6822(91)90680-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feldmann H, Klenk H D, Sanchez A. Molecular biology and evolution of filoviruses. Arch Virol. 1993;7(Suppl.):81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- 7.Feldmann H, Nichol S T, Klenk H D, Peters C J, Sanchez A. Characterization of filoviruses based on differences in structure and antigenicity of the virion glycoprotein. Virology. 1994;199:469–473. doi: 10.1006/viro.1994.1147. [DOI] [PubMed] [Google Scholar]
- 8.Fredericksen B L, Whitt M A. Vesicular stomatitis virus glycoprotein mutations that affect membrane fusion activity and abolish virus infectivity. J Virol. 1995;69:1435–1443. doi: 10.1128/jvi.69.3.1435-1443.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freed E O, Myers D J, Risser R. Characterization of the fusion domain of the human immunodeficiency virus type 1 envelope glycoprotein gp41. Proc Natl Acad Sci USA. 1990;87:4650–4654. doi: 10.1073/pnas.87.12.4650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freed E O, Myers D J. Identification and characterization of fusion and processing domains of the human immunodeficiency virus type 2 envelope glycoprotein. J Virol. 1992;66:5472–5478. doi: 10.1128/jvi.66.9.5472-5478.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallaher W R. Similar structural models of the transmembrane proteins of Ebola and avian sarcoma viruses. Cell. 1996;85:477–478. doi: 10.1016/s0092-8674(00)81248-9. [DOI] [PubMed] [Google Scholar]
- 12.Gething M J, Doms R W, York D, White J. Studies on the mechanism of membrane fusion: site-specific mutagenesis of the hemagglutinin of influenza virus. J Cell Biol. 1986;102:11–23. doi: 10.1083/jcb.102.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hernandez L D, Hoffman L R, Wolfsberg T G, White J M. Virus-cell and cell-cell fusion. Annu Rev Cell Dev Biol. 1996;12:627–661. doi: 10.1146/annurev.cellbio.12.1.627. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez L D, White J M. Mutational analysis of the candidate internal fusion peptide of the avian leukosis and sarcoma virus subgroup A envelope glycoprotein. J Virol. 1998;72:3259–3267. doi: 10.1128/jvi.72.4.3259-3267.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horvath C M, Lamb R A. Studies on the fusion peptide of a paramyxovirus fusion glycoprotein: roles of conserved residues in cell fusion. J Virol. 1992;66:2443–2455. doi: 10.1128/jvi.66.4.2443-2455.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavillette D, Maurice M, Roche C, Russell S J, Sitbon M, Cosset F L. A proline-rich motif downstream of the receptor binding domain modulates conformation and fusogenicity of murine retroviral envelopes. J Virol. 1998;72:9955–9965. doi: 10.1128/jvi.72.12.9955-9965.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levy-Mintz P, Kielian M. Mutagenesis of the putative fusion domain of the Semliki Forest virus spike protein. J Virol. 1991;65:4292–4300. doi: 10.1128/jvi.65.8.4292-4300.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo Z, Weiss S R. Roles in cell-to-cell fusion of two conserved hydrophobic regions in the murine coronavirus spike protein. Virology. 1998;244:483–494. doi: 10.1006/viro.1998.9121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niwa H, Yamamura K, Miyazaki J. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene. 1991;108:193–199. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- 20.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. Filoviridae: Marburg and Ebola viruses. In: Fields B N, Knipe D M, Howley P M, editors. Virology. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 1161–1176. [Google Scholar]
- 21.Ruiz-Arguello M B, Goni F M, Pereira F B, Nieva J L. Phosphatidylinositol-dependent membrane fusion induced by a putative fusogenic sequence of Ebola virus. J Virol. 1998;72:1775–1781. doi: 10.1128/jvi.72.3.1775-1781.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanchez A, Yang Z Y, Xu L, Nabel G J, Crews T, Peters C J. Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J Virol. 1998;72:6442–6447. doi: 10.1128/jvi.72.8.6442-6447.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sergel-Germano T, McQuain C, Morrison T. Mutations in the fusion peptide and heptad repeat regions of the Newcastle disease virus fusion protein block fusion. J Virol. 1994;68:7654–7658. doi: 10.1128/jvi.68.11.7654-7658.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steinhauer D A, Wharton S A, Skehel J J, Wiley D C. Studies of the membrane fusion activities of fusion peptide mutants of influenza virus hemagglutinin. J Virol. 1995;69:6643–6651. doi: 10.1128/jvi.69.11.6643-6651.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takada A, Robison C, Goto H, Sanchez A, Murti K G, Whitt M A, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volchkov V E, Feldmann H, Volchkova V A, Klenk H D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weissenhorn W, Calder L J, Wharton S A, Skehel J J, Wiley D C. The central structural feature of the membrane fusion protein subunit from the Ebola virus glycoprotein is a long triple-stranded coiled coil. Proc Natl Acad Sci USA. 1998;95:6032–6036. doi: 10.1073/pnas.95.11.6032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weissenhorn W, Carfi A, Lee K H, Skehel J J, Wiley D C. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol Cell. 1998;2:605–616. doi: 10.1016/s1097-2765(00)80159-8. [DOI] [PubMed] [Google Scholar]
- 30.Weng Y, Weiss C D. Mutational analysis of residues in the coiled-coil domain of human immunodeficiency virus type 1 transmembrane protein gp41. J Virol. 1998;72:9676–9682. doi: 10.1128/jvi.72.12.9676-9682.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White J M. Membrane fusion. Science. 1992;258:917–924. doi: 10.1126/science.1439803. [DOI] [PubMed] [Google Scholar]
- 32.Wild C, Oas T, McDanal C, Bolognesi D, Matthews T. A synthetic peptide inhibitor of human immunodeficiency virus replication: correlation between solution structure and viral inhibition. Proc Natl Acad Sci USA. 1992;89:10537–10541. doi: 10.1073/pnas.89.21.10537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wool-Lewis R J, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Z, Delgado R, Xu L, Todd R F, Nabel E G, Sanchez A, Nabel G J. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- 35.Yao Q, Compans R W. Peptides corresponding to the heptad repeat sequence of human parainfluenza virus fusion protein are potent inhibitors of virus infection. Virology. 1996;223:103–112. doi: 10.1006/viro.1996.0459. [DOI] [PubMed] [Google Scholar]
- 36.Zhang L, Ghosh H P. Characterization of the putative fusogenic domain in vesicular stomatitis virus glycoprotein G. J Virol. 1994;68:2186–2193. doi: 10.1128/jvi.68.4.2186-2193.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]