Abstract
Background.
Smoking is a risk factor for complications after lung resection. Our primary aim was to ascertain thoracic surgeons’ beliefs and practices on smoking cessation before lung resection.
Methods.
An anonymous survey was emailed to 846 thoracic surgeons who participate in The Society of Thoracic Surgeons General Thoracic Surgery Database.
Results.
The response rate was 23.6% (n = 200). Surgeons were divided when asked whether it is ethical to require that patients quit smoking (yes, n = 96 [48%]) and whether it is fair to have their outcomes affected by patients who do not quit (yes, n = 87 [43.5%]). Most do not require smoking cessation (n = 120 [60%]). Of those who require it, the most common required period of cessation is 2 weeks or more. Most believe that patient factors are the main barrier to quitting (n = 160 [80%]). Risk of disease progression (39% vs 17.5%, p = 0.02) and alienating patients (17.5% vs 8.8%, p = 0.04) were very important considerations of those who do not require smoking cessation versus those who do. Only 19 (9.5%) always refer to a smoking cessation program and prescribe nicotine replacement therapy and even fewer, 9 (4.5%), always refer to a program and prescribe medical therapy.
Conclusions.
Thoracic surgeons are divided on their beliefs and practices regarding smoking cessation before lung resection. Most believe patient factors are the main barrier to quitting and have concerns about disease progression while awaiting cessation. Very few surgeons refer to a smoking cessation program and prescribe nicotine replacement therapy or medical therapy.
In 2018, more than 230,000 patients were diagnosed with lung cancer, approximately 40% of whom underwent surgical resection [1, 2]. Cigarette smoking increases the risk of postoperative complications and mortality by 50% among patients undergoing lung cancer resection [3–5]. Importantly, smoking is a modifiable risk factor, and preoperative cessation reduces postoperative complications [3, 6, 7]. Providing both counseling and medical therapy significantly improves the likelihood of long-term cessation [8, 9]. Training thoracic surgeons on tobacco cessation best practices and implementing cessation programs increases the rate at which patients quit smoking and are important aspects of lung cancer treatment [10, 11].
Scant information has been published on the current practice patterns of thoracic surgeons with regards to assessment of smoking status, assistance with cessation, and whether cessation is required before lung resection. Only one survey of cardiothoracic surgeons has been published that focused solely on practice patterns, and the scope was broad, including lung resection, esophagectomy, and cardiac operations [12]. The primary aim of this study was to ascertain thoracic surgeons’ beliefs and practices on smoking cessation before elective lung resection. A secondary aim was to determine whether surgeon demographic factors are associated with beliefs and practices on smoking cessation.
Material and Methods
An anonymous, online survey was generated using a REDCap (Research Electronic Data Capture, Vanderbilt University, Nashville, TN) application. The survey (Supplemental Table 1) addressed surgeons’ beliefs and practices regarding smoking cessation before elective lung resection. The survey was emailed to 846 United States surgeons who participate in The Society of Thoracic Surgeons General Thoracic Surgery Database. This study was exempt from University of California Davis Institutional Review Board review.
Data Collected
Surgeon characteristics, including age, sex, years in practice, practice type (general thoracic surgery vs cardiothoracic surgery with primarily cardiac cases), and practice setting (academic vs private/health maintenance organization), were collected. Years in practice was categorized as 9 years or less, 10 to 19 years, and 20 years or longer. We emailed nonrespondents every Monday for 4 weeks and after this point, closed the survey. Characteristics for nonrespondents were collected by internet search.
Statistical Analyses
Statistical tests of proportions were conducted to compare two dichotomous variables and ordinal and dichotomous variables. To determine whether demographic factors were associated with certain responses, we used logistic regression analysis for dichotomous outcomes and linear regression analysis for ordinal outcomes, with robust SEs. We included sex, years in practice, practice type, and practice setting in the models. We did not include age to avoid collinearity with years in practice. A p value of less than 0.05 was considered statistically significant. Stata SE 14.2 software (StataCorp, College Station, TX) was used for all analyses.
Results
Demographics
Of 846 surgeons, 200 (23.6%) surveys were completed. Most who responded were males who practice general thoracic surgery at an academic center (Table 1). Respondents were more likely to practice general thoracic surgery at an academic center and to be female and younger in age than nonrespondents (Table 1).
Table 1.
Characteristics of Respondents Versus Nonrespondents
| Respondents | Nonrespondents | ||
|---|---|---|---|
|
|
|
||
| Surgeon Characteristics | (n = 200 [23.6%]) | (n = 646 [76.4%]) | p Value |
|
|
|
||
| n (%) | n (%) | ||
|
| |||
| Practice type | <0.001 | ||
| General thoracic surgery | 167 (83.5) | 349 (54.0) | |
| Cardiothoracic surgery with mostly cardiac cases | 33 (16.5) | 277 (42.9) | |
| Missing | 20 (3.1) | ||
| Practice setting | <0.001 | ||
| University/academic | 137 (68.5) | 305 (47.2) | |
| Private/health maintenance organization | 63 (31.5) | 336 (52.0) | |
| Missing | 5 (0.8) | ||
| Years in practice | 0.09 | ||
| 0–9 | 63 (31.5) | 149 (23.1) | |
| 10–19 | 69 (34.5) | 233 (36.1) | |
| ≥20 | 68 (34.0) | 243 (37.6) | |
| Missing | 21 (3.2) | ||
| Age, years | <0.001 | ||
| 30–39 | 13 (6.5) | 22 (3.4) | |
| 40–49 | 88 (44.0) | 181 (28.0) | |
| 50–59 | 65 (32.5) | 224 (34.7) | |
| 60–69 | 30 (15.0) | 147(22.8) | |
| ≥70 | 4 (2.0) | 30 (4.6) | |
| Missing | 42 (6.5) | ||
| Sex | <0.001 | ||
| Female | 34 (17.0) | 41 (6.4) | |
| Male | 166 (83.0) | 600 (92.9) | |
| Missing | 5 (0.7) | ||
Beliefs Regarding Smoking Cessation
Surgeons were divided when asked whether it is ethical to mandate that patients quit smoking before surgery (yes, n = 96 [48%]) and whether it is fair to have their outcomes affected by patients who refuse or are unable to quit smoking (yes, n = 87 [43.5%]). Of those who responded that it is ethical to require cessation, 67 (69.8%) require it. Of those who responded that it is fair to have outcomes affected by patients who do not quit, 35 (40.2%) require cessation.
Most thoracic surgeons believe that they are responsible for ensuring tobacco cessation before surgery (n = 117 [58.5%]), as opposed to that responsibility being delegated to a tobacco cessation program (n = 22 [11.0%]), primary care physician (n = 10 [5.0%]), or referring physician (n = 4 [2.0%]). The remainder (n = 47 [23.5%]) responded that smoking cessation is unnecessary.
Most surgeons (n = 160 [80.0%]) believe that patient factors (eg, not wanting to quit and lack of willpower) are the main barrier interfering with their ability to help patients quit smoking as opposed to lack of smoking cessation program (n = 23 [11.5%]), not having enough time to counsel them (n = 12 [6.0%]), or lack of familiarity with pharmacotherapy (n = 5 [2.5%]).
When asked how important certain considerations were when mandating smoking cessation, most answered very or moderately important to “risk of disease progression while time elapses after smoking cessation” as an important consideration (Fig 1). The overall highest response was “not important” to “losing patients to other surgeons who do not require them to quit smoking.” Risk of disease progression (Fig 2) and alienating patients (Fig 3) were very important considerations of those who do not require smoking cessation compared with those who do.
Fig 1.
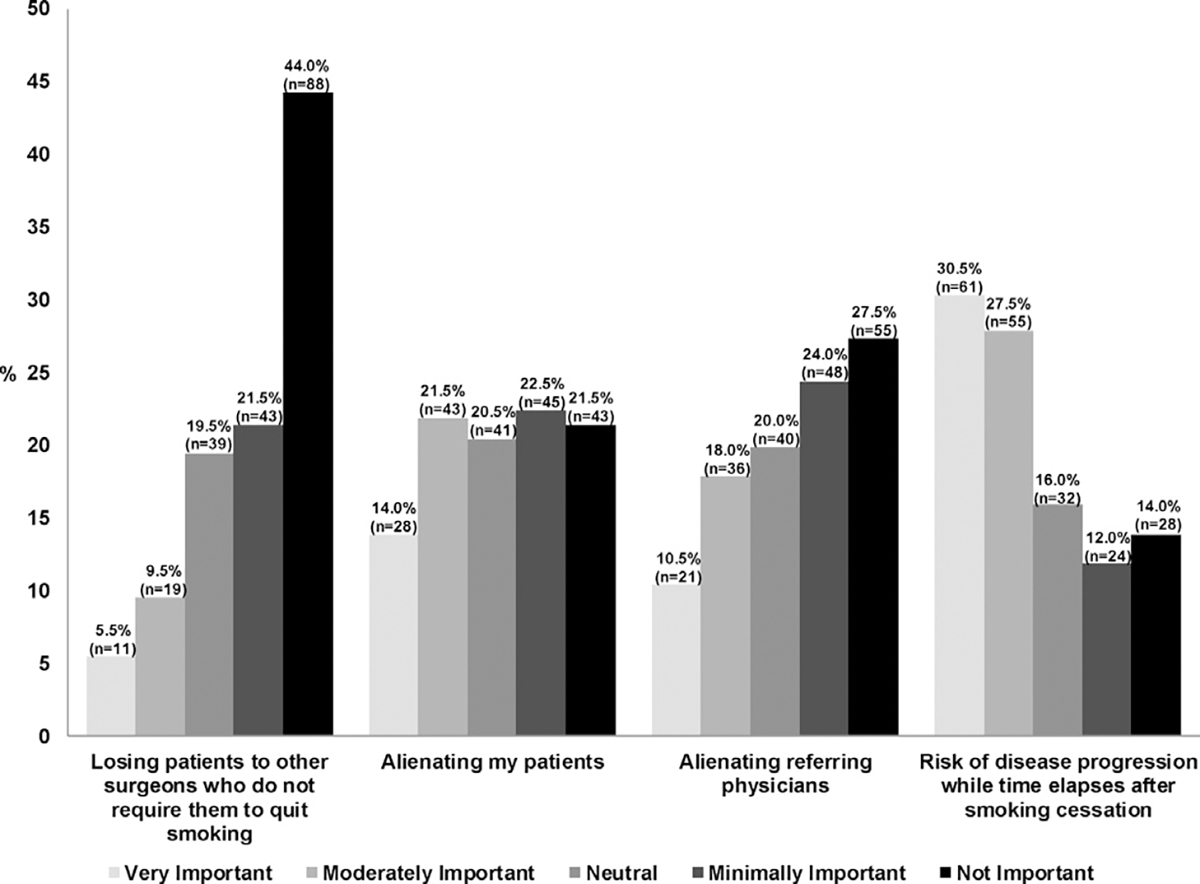
Importance of considerations when mandating smoking cessation before elective lung resection.
Fig 2.
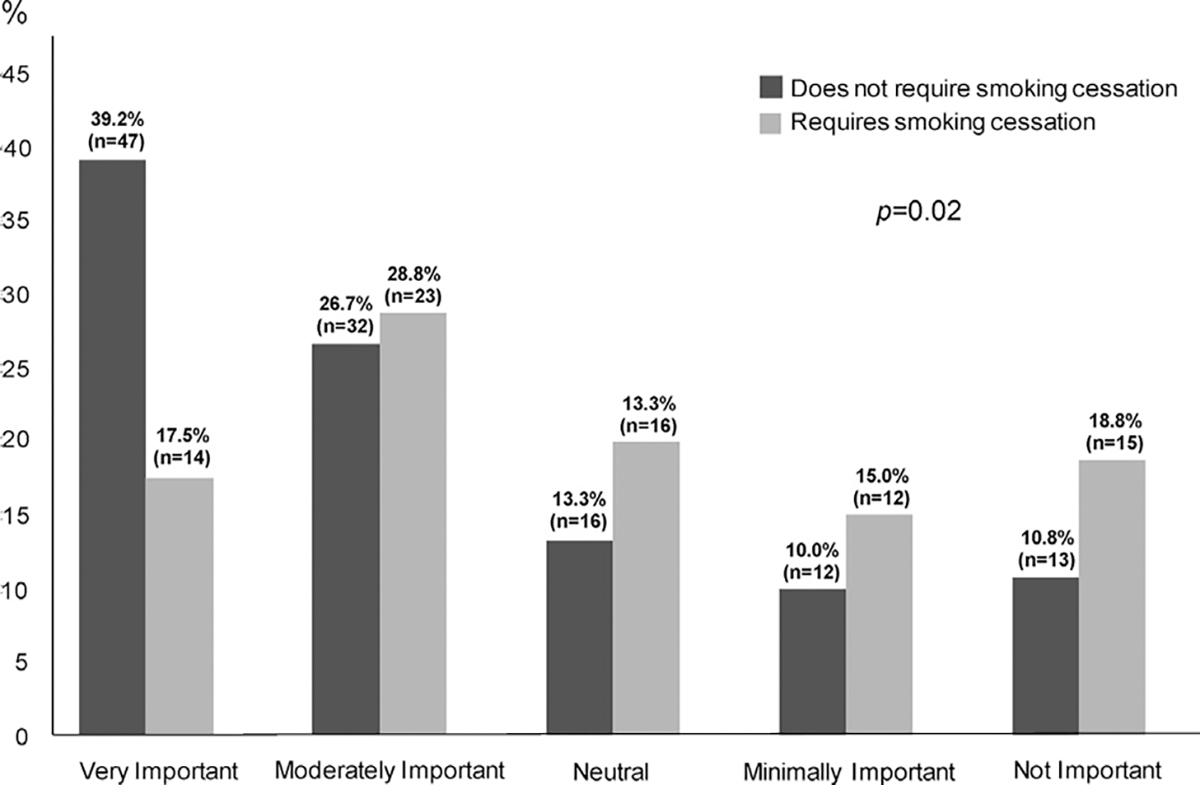
Importance of risk of disease progression according to whether surgeon requires smoking cessation.
Fig 3.
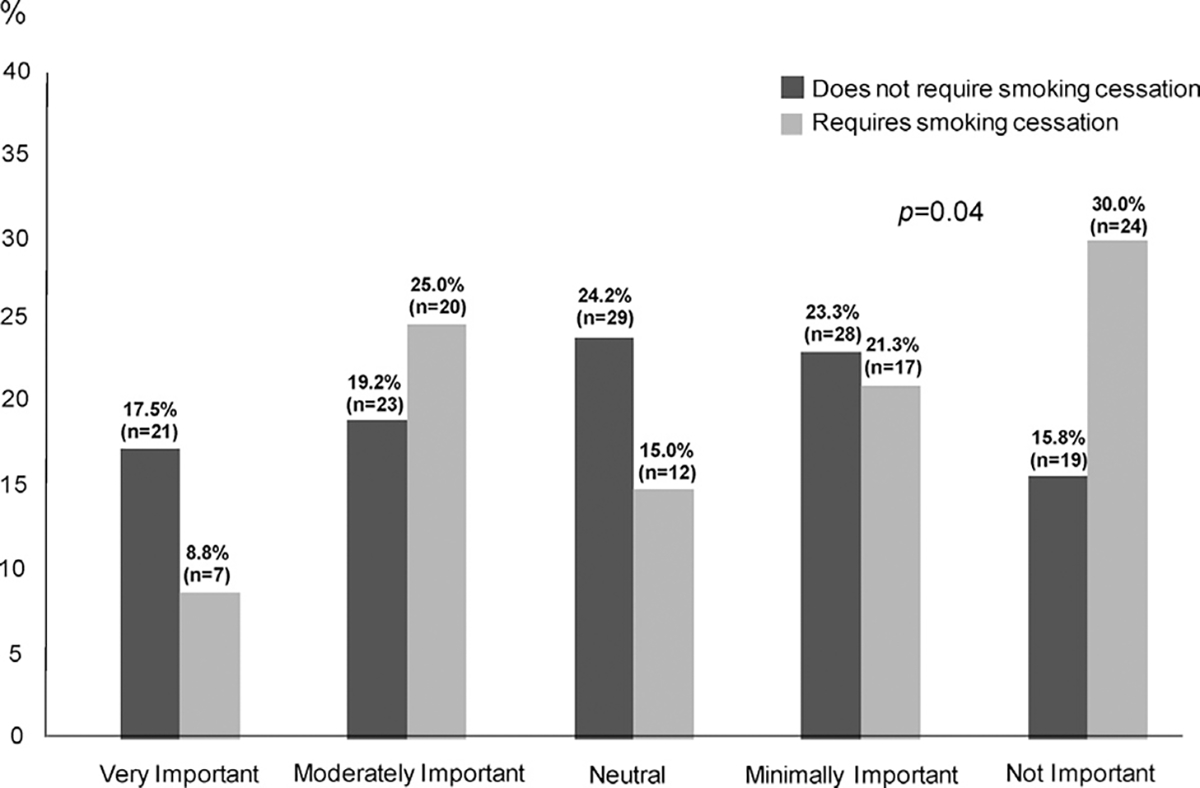
Importance of alienating patients according to whether surgeon requires smoking cessation.
Smoking Cessation Practices
More than half of surgeons (n = 120 [60%]) do not require patients to quit smoking. Surgeons who do and do not require cessation did not differ by demographic factors (Table 2). When asked how long must the period of smoking cessation be, most chose not required (n = 85 [42.5%]) or at least 2 weeks (n = 64 [32.0%]), and others chose at least 3 weeks (n = 26 [13.0%]), 4 weeks (n = 17 [8.5%]), or 1 week (n = 7 [3.5%]).
Table 2.
Characteristics of Thoracic Surgeons Who Require Patients to Quit and Those Who Do Not
| Surgeons Require Patients to Quit Smoking | |||
|---|---|---|---|
|
|
|||
| Yes | No | ||
|
|
|
||
| Surgeon Characteristics | n (%) | n (%) | p Value |
|
| |||
| Practice type | 0.8 | ||
| General thoracic surgery | 66 (82.5) | 101 (84.2) | |
| Cardiothoracic surgery with mostly cardiac cases | 14 (17.5) | 19 (15.8) | |
| Practice setting | 0.4 | ||
| University/academic | 52 (65.0) | 85 (70.8) | |
| Private/health maintenance organization | 28 (35.0) | 35 (29.2) | |
| Years in practice | 0.8 | ||
| 0–9 | 25 (31.3) | 38 (31.7) | |
| 10–19 | 26 (32.5) | 43 (35.8) | |
| ≥20 | 29 (36.3) | 39 (32.5) | |
| Age, years | 0.6 | ||
| 30–39 | 4 (5.0) | 9 (7.5) | |
| 40–49 | 31 (38.8) | 57 (47.5) | |
| 50–59 | 30 (37.5) | 35 (29.2) | |
| 60–69 | 13 (16.3) | 17 (14.2) | |
| ≥70 | 2 (2.5) | 2 (1.7) | |
| Sex | 0.2 | ||
| Female | 17 (14.2) | 17 (21.3) | |
| Male | 63 (78.8) | 103 (85.8) | |
When asked about the “A’s” of smoking cessation—Ask, Advise, Assess, and Assist—199 surgeons (99%) always ask patients whether they smoke,195 (97.5%) advise patients to quit, and 176 (88%) always assess readiness to quit. Fewer always assist with smoking cessation (n = 147 [73.0%]). Most surgeons always counsel their patients on smoking cessation (n = 181 [90.5%]); however, only 19 (9.5%) always refer to a cessation program and prescribe nicotine replacement therapy (NRT) and even fewer (n = 9 [4.5%]) always refer to a program and prescribe medical therapy (Table 3).
Table 3.
Thoracic Surgeons’ Smoking Cessation Practices
| Type of Smoking Cessation Practice | n (%) |
|---|---|
|
| |
| Provide smoking cessation counseling | |
| Always | 181 (90.5) |
| Usually | 10 (5.0) |
| Sometimes | 8 (4.0) |
| Rarely | 0 (0.0) |
| Never | 1 (0.5) |
| Refer patients to a smoking cessation program | |
| Always | 79 (39.5) |
| Usually | 43 (21.5) |
| Sometimes | 45 (22.5) |
| Rarely | 21 (10.5) |
| Never | 12 (6.0) |
| Prescribe nicotine replacement therapy | |
| Always | 27 (13.5) |
| Usually | 50 (25.0) |
| Sometimes | 67 (33.5) |
| Rarely | 33 (16.5) |
| Never | 23 (11.5) |
| Prescribe medical therapya | |
| Always | 11 (5.5) |
| Usually | 27 (13.5) |
| Sometimes | 72 (36.0) |
| Rarely | 49 (24.5) |
| Never | 41 (20.5) |
Varenicline (Chantix; Pfizer Inc, Mission, KS) or bupropion (Wellbutrin; GlaxoSmithKline, Research Triangle Park, NC).
Surgeons’ practices regarding assisting patients with smoking cessation varied according to whether they required smoking cessation (Table 4). Those who require smoking cessation are more likely to prescribe NRT or medical therapy but are similar to those who do not require it with regards to counseling and referral to a program. Almost all surgeons always (n = 145 [72.5%]) or usually (n = 41 [20.5%]) ask patients about relapse after the operation.
Table 4.
Smoking Cessation Practices Among Thoracic Surgeons Who Require Patients to Quit and Those Who Do Not
| Surgeons Require Patients to Quit Smoking | |||
|---|---|---|---|
|
|
|||
| Smoking Cessation Practices | Yes | No | |
|
|
|
||
| n (%) | n (%) | p Value | |
|
| |||
| Provide smoking cessation counseling | 0.3 | ||
| Always | 76 (95.0) | 105 (87.5) | |
| Usually | 2 (2.5) | 8 (6.7) | |
| Sometimes | 2 (2.5) | 6 (5.0) | |
| Rarely | 0 | 0 | |
| Never | 0 | 1 (0.8) | |
| Refer patients to smoking cessation program | 0.9 | ||
| Always | 33 (41.3) | 46 (38.3) | |
| Usually | 17 (21.3) | 26 (21.7) | |
| Sometimes | 19 (23.8) | 26 (21.7) | |
| Rarely | 8 (10.0) | 13 (10.8) | |
| Never | 3 (3.8) | 9 (7.5) | |
| Prescribe nicotine replacement therapy | 0.01 | ||
| Always | 17 (21.3) | 10 (8.3) | |
| Usually | 24 (30.0) | 26 (21.7) | |
| Sometimes | 25 (31.3) | 42 (35.0) | |
| Rarely | 8 (10.0) | 25 (20.8) | |
| Never | 6 (7.5) | 17 (14.2) | |
| Prescribe medical therapya | 0.02 | ||
| Always | 7 (8.8) | 4 (3.3) | |
| Usually | 15 (18.8) | 12 (10.0) | |
| Sometimes | 33 (41.3) | 39 (32.5) | |
| Rarely | 13 (16.3) | 36 (30.0) | |
| Never | 12 (15.0) | 29 (24.2) | |
Varenicline (Chantix; Pfizer Inc, Mission, KS) or bupropion (Wellbutrin; GlaxoSmithKline, Research Triangle Park, NC).
Beliefs and Practices: Regression Analyses
No demographic characteristics were associated with requiring that patients quit smoking. There was only one statistically significant finding in regression analyses of beliefs regarding smoking cessation. Men were more likely to consider it fair to have their outcomes affected by patients who continue to smoke (odds ratio, 2.57; 95% confidence interval [CI], 1.10 to 6.05; p = 0.03).
Several findings in the regression analyses of smoking cessation practices were statistically significant. Men were more likely than women to assist with cessation (adjusted mean difference, 0.29; 95% CI, 0.06 to 0.51; p = 0.01), counsel on smoking cessation (adjusted mean difference, 0.18; 95% CI, 0.05 to 0.31; p = 0.005), and ask about relapse (adjusted mean difference, 0.21; 95% CI, 0.02 to 0.40; p = 0.03). They were also more likely to prescribe NRT (adjusted mean difference, 0.49; 95% CI, 0.08 to 0.90; p = 0.02) and to prescribe medical therapy (adjusted mean difference, 0.44; 95% CI, 0.04 to 0.84; p = 0.03).
Thoracic surgeons were more likely to provide counseling (adjusted mean difference, 0.14; 95% CI, 0.001 to 0.29; p = 0.048) but less likely to refer a patient to a smoking cessation program than a cardiothoracic surgeon (adjusted mean difference, −0.61; 95% CI, −1.17 to −0.06; p = 0.03). Surgeons in practice 10 to 19 years were less likely to ask about relapse (adjusted mean difference, −0.28; 95% CI, −0.55 to −0.02; p = 0.03), and those in practice 20 or more years were less likely to ask (adjusted mean difference, 0.32; 95% CI, −0.58 to −0.06; p = 0.016) than those in practice 9 years or less.
Comment
Beliefs Regarding Smoking Cessation
Thoracic surgeons were divided on whether it is ethical to require that patients quit smoking before surgical resection. Surveys of thoracic oncologists have inquired about beliefs regarding smoking cessation [13, 14], but a prior survey of thoracic surgeons focused only on practice patterns [12]. One study investigated whether physicians and members of the general public support making elective operations conditional upon smoking cessation; a clinical vignette of a patient who was still employed and in need of elective hip replacement was presented [15]. Most agreed that the operation should be conditional upon smoking cessation 4 weeks before and after the operation, and 73.4% stated that the risk of complications was the most compelling argument for mandating cessation before the operation. However, when the qualitative data were analyzed, a common theme emerged indicating that it is right to recommend smoking cessation but wrong to require it [15]. We asked whether it was ethical to mandate that patients quit as a “yes” or “no” question, and perhaps some of the “yes” responses might have softened had we collected qualitative data.
Thoracic surgeons were also divided on whether it is fair to have their outcomes affected by patients who refuse or are unable to quit smoking. In The Society of Thoracic Surgeons General Thoracic Surgery Database model for morbidity and mortality after lung cancer resection, recent cigarette use was associated with a 50% increased risk of the composite end point of hospital mortality or major morbidity [4]. A lobectomy composite score has been developed using these same models [16]. Because smoking is included in the risk adjustment model, surgeons are not penalized for operating on patients who smoke from a quality reporting standpoint.
Most thoracic surgeons responded that it is their responsibility to ensure tobacco cessation. Interestingly, in a similar survey of vascular surgeons, almost 60% responded that primary care providers should be responsible for risk factor modification in vascular surgery patients. This may be because vascular surgical conditions are typically more chronic in nature rather than having most of the smoking cessation effort directed toward quitting before the operation.
Most surgeons responding to this survey believe that patient factors (not wanting to quit and lack of willpower) are the main barrier interfering with their ability to help patients quit smoking. Very few believed that lack of a smoking cessation program, lack of familiarity with pharmacotherapy, or not having enough time to counsel patients were barriers. Of International Association for the Study of Lung Cancer members, more than 50% agreed that patient factors were barriers to smoking cessation [14]. However, nearly 50% of respondents agreed that lack of time for counseling, lack of training or experience in smoking cessation interventions, and lack of available resources or referrals for cessation interventions were barriers [14].
A qualitative study of smokers’ attitudes towards cessation found that although some smokers classified themselves as highly motivated to quit, they had low motivation to quit in the immediate future [17]. The study also revealed that smokers felt they should quit rather than wanting to quit and therefore it is important to find ways to increase smokers’ implicit motivation to quit [17].
Risk of disease progression is an important consideration when delaying the operation for smoking cessation. Although timely definitive treatment for patients with lung cancer is considered important by surgeons, the data supporting this concept are divided [18–21].
Smoking Cessation Practices
Most thoracic surgeons do not require smoking cessation before elective lung resection; however, a large proportion, 40%, do require it. There is only one other survey of thoracic surgeons, by Marino and colleagues [12], and our results regarding requiring smoking cessation before lung resection are similar. That study inquired, “Are there any procedures that you will not perform on patients who are daily smokers?”, and 47% responded “yes” [12].
That study inquired about smoking cessation practice patterns only [12]. Our survey investigated further by inquiring about surgeons’ beliefs regarding smoking cessation before lung resection, including whether it is ethical to require and whether it is fair for surgeons to have their outcomes affected by those who are unable to quit. In addition, we asked questions regarding motivation for or against requiring cessation; for example, alienating patients and referring physicians, losing patients to other surgeons who do not require it, and risk of disease progression. Our study adds to the existing literature by providing more detail regarding surgeons’ practices and views on smoking cessation before lung resection.
Of those who require smoking cessation, most require it for at least 2 weeks before the operation. Studies of patients undergoing lung resection have demonstrated a progressive decrease in the risk of pulmonary complications [3, 6] and hospital death [3] with increasing interval of smoking cessation. However, regardless of the interval of smoking cessation, the risk of hospital death and pulmonary complications never decrease to the level of never smokers [3]. All prior studies have relied on patient-reported smoking history, and future studies using objective data to quantify smoking are needed to better define the dose-response relationship between cessation interval and pulmonary complications.
The “5 A’s” model for treating tobacco use includes (1) Ask about tobacco use at every visit, (2) Advise the patient to quit smoking, (3) Assess whether the patient is ready to quit smoking, (4) Assist those who are ready to quit by offering medication and providing/referring for counseling, and (5) Arrange for follow-up [9]. Almost all surgeons surveyed always ask patients whether they smoke. As the “A’s” progressed, fewer surgeons always consistently provided that “A.” As part the International Association for the Study of Lung Cancer survey, only 70.4% always asked about smoking, 50% always advised to quit, 50% always assessed readiness to quit, and 17.4% always assisted with smoking cessation [14]. Medical oncologists comprised 33.4% of the participants, and the next largest specialty was surgery (24.3%) [14]. Our survey of all surgeons may have reported better adherence to the “A’s” because surgeons see patients preparing for the operation and are aware that smoking is a risk factor for postoperative complications [4].
Smoking cessation counseling and medications are effective when used by themselves; however, the combination of the two is more effective than either alone [9]. Unfortunately, very few respondents practiced a combination of referring their patients to a smoking cessation program and providing NRT or medical therapy. Furthermore, the combination of varenicline with NRT is more effective than varenicline alone at achieving tobacco abstinence [22]. A more recent randomized trial found no significant differences in quit rates after 12 weeks of treatment with nicotine patch, varenicline, or combination NRT (patch and lozenge) [23]. The authors noted that the lack of a difference was caused by a small effect size and that this in turn may have been secondary to low nicotine dependence among the participants or low adherence to the medication, or both. According to the United States Department of Health and Human Services guidelines, clinicians should encourage medication use by all patients who are trying to quit smoking [9]. There are seven first-line medications, including bupropion SR, varenicline, and 5 NRT options.
Limitations
There is significant variability in response rates to internet-based surveys, but it is not uncommon for response rates of health professionals to be less than 20% [24]. Although the response rate was relatively high, the responses are limited to thoracic surgeons who participate in The Society of Thoracic Surgeons General Thoracic Surgery Database and may not be representative of the beliefs and practices of all thoracic surgeons in the United States.
Social desirability bias, which is the tendency of survey respondents to respond to questions in a manner that will be viewed as favorable by others, is likely to play a role in this survey. Thoracic surgeons may have reported practices that they “should be doing” rather than an accurate account of what they are doing; thus, the result could overestimate cessation practices.
Lastly, to permit analyses and comparisons between responders, all responses were binary (yes/no) or on a 5-point Likert scale. Perhaps we might have obtained additional information by including open-ended questions in the survey.
Conclusion
Thoracic surgeons are divided on their beliefs and practices on smoking cessation before elective lung resection. Most agree that it is the responsibility of the surgeon to ensure smoking cessation, believe that patient factors are the main barrier to quitting, and have concerns about disease progression while awaiting cessation. Although almost all surgeons counsel their patients on smoking cessation, very few refer to a smoking cessation program and prescribe NRT or medical therapy.
Supplementary Material
Acknowledgments
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1-TR-001860 and linked award KL2-TR-001859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The Supplemental Table can be viewed in the online version of this article [https://doi.org/10.1016/j.athoracsur.2018.11.055] on http://www.annalsthoracicsurgery.org.
References
- 1.American Cancer Society. Key Statistics for Lung Cancer. Available at https://www.cancer.org/cancer/non-small-cell-lung-cancer/about/key-statistics.html. Accessed November 1, 2018.
- 2.National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Lung and Bronchus Cancer. Available at https://seer.cancer.gov/statfacts/html/lungb.html. Accessed November 1, 2018. [Google Scholar]
- 3.Mason DP, Subramanian S, Nowicki ER, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database Study. Ann Thorac Surg 2009;88:362–71. [DOI] [PubMed] [Google Scholar]
- 4.Kozower BD, Sheng S, O’Brien SM, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg 2010;90:875–81. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez FG, Kosinski AS, Burfeind W, et al. The Society of Thoracic Surgeons Lung Cancer Resection Risk Model: higher quality data and superior outcomes. Ann Thorac Surg 2016;102:370–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrera R, Shi W, Amar D, et al. Smoking and timing of cessation: impact on pulmonary complications after thoracotomy. Chest 2005;127:1977–83. [DOI] [PubMed] [Google Scholar]
- 7.Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg 2011;212:1094–6. [DOI] [PubMed] [Google Scholar]
- 8.Cahill K, Lindson-Hawley N, Thomas K, Fanshawe T, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2016:CD006103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; May 2008. [Google Scholar]
- 10.Kozower BD, Lau CL, Phillips JV, Burks SG, Jones DR, Stukenborg GJ. A thoracic surgeon-directed tobacco cessation intervention. Ann Thorac Surg 2010;89:926–30. [DOI] [PubMed] [Google Scholar]
- 11.Cataldo JK, Dubey S, Prochaska JJ. Smoking cessation: an integral part of lung cancer treatment. Oncology 2010;78:289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marino KA, Little MA, Bursac Z, Sullivan JL, Klesges R, Weksler B. Operating on patients who smoke: a survey of thoracic surgeons in the United States. Ann Thorac Surg 2016;102:911–6. [DOI] [PubMed] [Google Scholar]
- 13.Warren GW, Marshall JR, Cummings KM, et al. Addressing tobacco use in patients with cancer: a survey of American Society of Clinical Oncology members. J Oncol Pract 2013;9:263–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warren GW, Marshall JR, Cummings KM, et al. Practice patterns and perceptions of thoracic oncology providers on tobacco use and cessation in cancer patients. J Thorac Oncol 2013;8:543–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Björk J, Juth N, Lynøe N. “Right To Recommend, Wrong To Require”-an empirical and philosophical study of the views among physicians and the general public on smoking cessation as a condition for surgery. BMC Med Ethics 2018;19:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozower BD, O’Brien SM, Kosinski AS, et al. The Society of Thoracic Surgeons composite score for rating program performance for lobectomy for lung cancer. Ann Thorac Surg 2016;101:1379–86. [DOI] [PubMed] [Google Scholar]
- 17.Uppal N, Shahab L, Britton J, Ratschen E. The forgotten smoker: a qualitative study of attitudes towards smoking, quitting & tobacco control policies among continuing smokers. BMC Public Health 2013;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olsson JK, Schultz EM, Gould MK. Timeliness of care in patients with lung cancer: a systematic review. Thorax 2009;64:749–56. [DOI] [PubMed] [Google Scholar]
- 19.Maiga AW, Deppen SA, Pinkerman R, et al. Timeliness of care and lung cancer tumor-stage progression: how long can we wait? Ann Thorac Surg 2017;104:1791–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang CF, Wang H, Kumar A, et al. Impact of timing of lobectomy on survival for clinical stage IA lung squamous cell carcinoma. Chest 2017;152:1239–50. [DOI] [PubMed] [Google Scholar]
- 21.Gomez DR, Liao KP, Swisher SG, et al. Time to treatment as a quality metric in lung cancer: Staging studies, time to treatment, and patient survival. Radiother Oncol 2015;115:257–63. [DOI] [PubMed] [Google Scholar]
- 22.Koegelenberg CF, Noor F, Bateman ED, et al. Efficacy of varenicline combined with nicotine replacement therapy vs varenicline alone for smoking cessation: a randomized clinical trial. JAMA 2014;312:155–61. [DOI] [PubMed] [Google Scholar]
- 23.Baker TB, Piper ME, Stein JH, et al. Effects of nicotine patch vs varenicline vs combination nicotine replacement therapy on smoking cessation at 26 weeks: a randomized clinical trial. JAMA 2016;315:371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dykema J, Jones NR, Piche T, Stevenson J. Surveying clinicians by web: current issues in design and administration. Eval Heal Prof 2013;36:352–81 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


