Abstract
Introduction and importance
Chronic extra-articular infections of the tibial tunnel are rare, and there are only a few cases reported in the literature, so the diagnosis and management of these infections are still unclear.
Case presentation
We report a 36-year-old patient with chronic infection of the tibial tunnel after ACL reconstruction surgery. The patient was treated with arthroscopic debridement of the tibial tunnel and antibiotic cement filling. Seven months postoperative, there were no signs of infection at the surgical site and the knee joint. The patient has no pain, no joint instability, no limitation of range of motion, and no limitation in daily activities.
Clinical discussion
The definitive diagnosis of chronic infection of the tibial tunnel should be carefully based on clinical signs, blood tests, and imaging to rule out combined intra-articular infections. The arthroscopic technique can be a favorable method to control and debride the inflammatory tissue of the tibial tunnel, limiting the recurrence rate postoperatively.
Conclusion
Arthroscopic debridement and antibiotic-loaded cement can be considered an alternative to traditional surgical methods in the treatment of chronic infection of the tibial bone tunnel after ACL reconstruction.
Level of evidence
A case report.
Keywords: Chronic infected, Tibial bone tunnel, Anterior cruciate ligament reconstruction
Highlights
-
•
The management of chronic infections of the tibial bone tunnel is still unclear.
-
•
The traditional debridement with curette sometimes fails to eradicate the infected bone and non-absorbable suture.
-
•
Arthroscopic debridement and antibiotic-loaded cement overcome the limitations of traditional debridement.
1. Introduction and importance
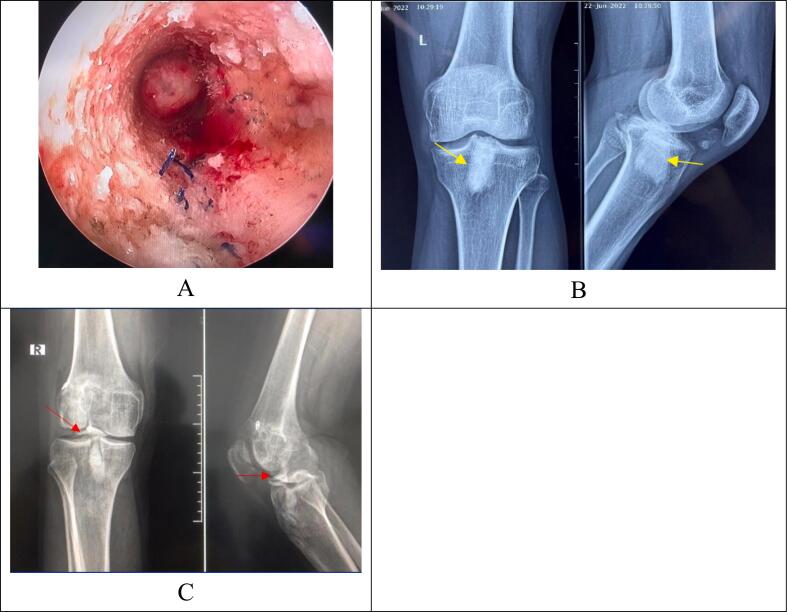
Anterior cruciate ligament (ACL) rupture is one of the most common knee ligament injuries. It is estimated that each year in the United States, there are about 130,000–200,000 cases of arthroscopic ACL reconstruction [1]. Some complications after surgery include joint instability, stiffness, graft rupture, and infection. Septic knee arthritis is a rare complication, accounting for 0.1 %–2.6 % of total surgeries [2,3]. This is considered a catastrophe because it causes serious consequences such as loss of graft function, stiffness, cartilage damage, and possibly the need for graft removal. Apart from intra-articular infections, sole extra-articular chronic disease of the tibial bone tunnel is rarely mentioned, and only a few cases have been reported in the literature. Therefore, the diagnosis and treatment of this disease are still unclear. The definitive diagnosis of sole tibial bone tunnel infection should exclude the combined septic knee arthritis based on clinical signs and blood tests. Otherwise, the treatment will fail. There are some reports in which this disease was treated by removing the implants, curettage of the inflammatory bone, and cementing the tibial bone tunnel. However, recurrence still occurred [4]. The cause of recurrence may be due to the failure to eradicate the infected bone and non-absorbable suture in the wall of the bone tunnel due to the limited observation of the tibial tunnel with the naked eye (Fig. 1A), at the same time, the use of “blind” debridement with curette can cause a significant defect in the tunnel bone (Fig. 1B), cause joint penetration leading to joint infection, or cement is introduced into the joint when cementing the tunnel (Fig. 1C). In the literature, there are no studies that suggest the optimal method to manage the tibial bone tunnel and overcome the disadvantages of the traditional method. Therefore, we report a case of chronic infected tibial tunnel after five months of ACL reconstruction surgery; the patient was successfully treated by arthroscopic debridement and antibiotic-loaded cement.
Fig. 1.
Some pictures of us. A, Image of inflammatory tissue, a Prolene suture in the wall of the tibial tunnel observed by arthroscopy. B. Significant bone defects in the tibial tunnel after “blind” debridement with curette and cement filling on radiographs (yellow arrow). C, Image of cement in the knee joint when cementing the tibial bone tunnel (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2. Case presentation
This case follows 2023 SCARE guidelines for reporting of cases in surgery [5].
A 36-year-old male patient underwent arthroscopic reconstruction of the ACL of the left knee with an autologous hamstring at the age of 35 at a local hospital. The graft was fixed with Transfix on the femoral condyle tunnel and bioabsorbable screws and staples on the tibial plateau tunnel. After eight weeks of surgery, the patient had a surgical incision infection on the anteromedial side of the leg. The surgeons in the local hospital performed debridement surgery to remove the bioabsorbable screw and staples in the 10th week after surgery. The bacterial culture results after surgery were negative, and intravenous antibiotics (levofloxacin 750 mg) were used for 14 days. Postoperatively, the incisions in the anterior knee and anteromedial side of the leg healed well, and the patient could return to rehabilitation and work.
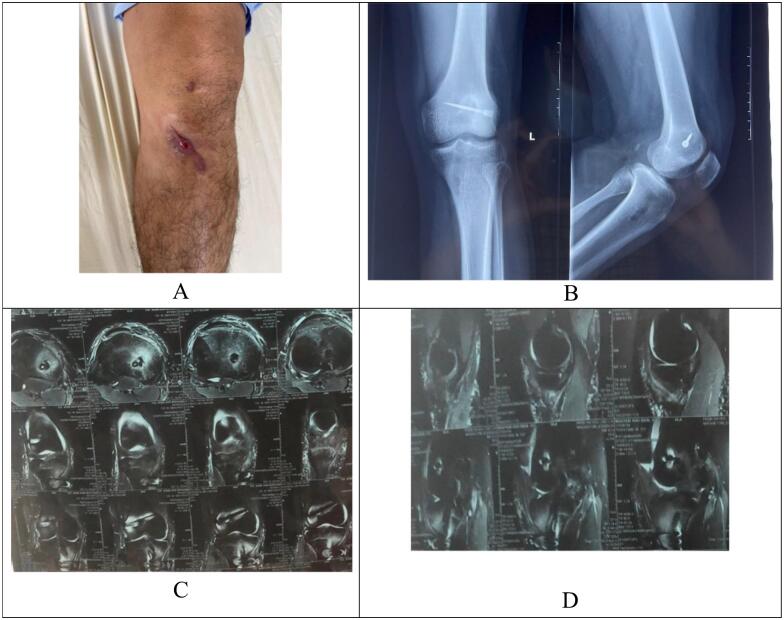
In the 5th month postoperative, the patient suddenly developed pain and swelling of the surgical incision on the anteromedial side of the leg and came to our department for examination. The patient had no fever, pain, or hypersensitivity in the left knee joint and could run lightly. During the examination, there were no signs of arthritis in the left knee, joint effusion, or joint range of motion limitation. The patient did not feel knee instability, Lachman tested positive for grade I, and the anterior drawer tested positive for grade I compared with the healthy leg. The surgical wound in the anteromedial side of the lower leg was about 5 cm long, and there was a fistula in the middle of the incision; pressing on the incision revealed a milky discharge through the fistula (Fig. 2A).
Fig. 2.
Clinical status, radiographs, and MRI before surgery. A preoperative incision. B, Radiographs of the knee joint before surgery. C, D, MRI of the knee joint before surgery.
Blood tests showed 7.76 G/L white blood cells (Normal: 4–10 G/L) with 58 % granulocytes. The erythrocyte sedimentation rate was 7 mm/h (Normal: 0-20 mm/h), and CRP was 2.3 ng/mL (Normal: 0-6 ng/mL). The standard knee joint radiographs showed osteosclerosis around the tibial bone tunnel but were unclear (Fig. 2B). Magnetic resonance imaging of the knee joint indicated an image of inflammation at the anterior aspect of the lower leg and the tibial tunnel; there was no signal of the graft in the tibial tunnel. Only the fluid signal could be seen. In addition, there was the image of bone marrow edema around the tibial plateau tunnel. There is no continuous image between the tibial tunnel and the knee joint and no image of knee arthritis. The signal of the graft in the joint was clear (Fig. 2C, D).
The patient's history revealed no familial genetic disease, neurological disease, or previous knee joint problems. The patient did not drink alcohol or smoke.
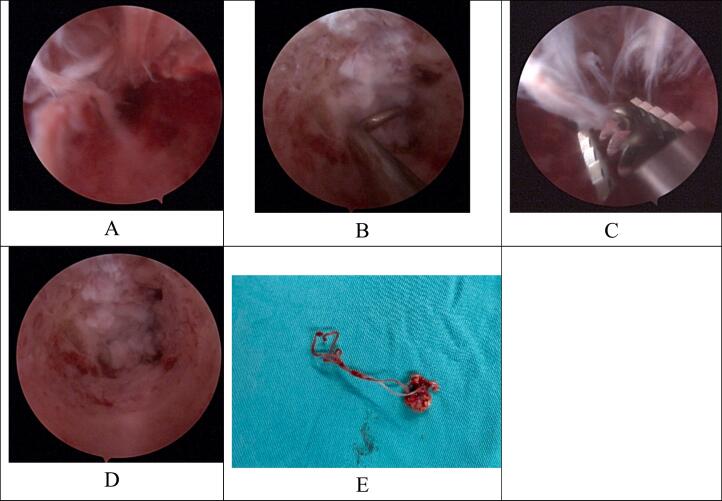
The patient was diagnosed with a sole chronic infection of the tibial tunnel five months after ACL reconstruction surgery. After being explained about the risks and benefits of surgery, the patient agreed with a 2-phased surgical treatment plan. The first phase included fistula enlargement, arthroscopic debridement, and VAC therapy. The second phase included the cementation of the tibial bone tunnel with antibiotic-loaded cement. The authors performed the surgery. During the first surgery, while expanding the wound scar on the front of the leg, a lot of pus was observed, a fistula communicating with the tibial tunnel was also seen, and there was pus in the tunnel. An arthroscope (4.0-mm, 30°) and a small shaver (3.5-mm) were used. An arthroscope observation of the tunnel revealed the inflammatory tissue around the tibial tunnel wall (Fig. 3A), a non-absorbable suture, and the graft covering the bottom of the tunnel. Examination did not show any communication between the tunnel and the joint (Fig. 3B). A pair of Kocher forceps was used to remove the non-absorbable suture in the tunnel. A shaver was used to debride the inflammatory tissue in the tunnel wall (Fig. 3C) until the bone marrow with bleeding was reached (Fig. 3D); all maneuvers were carefully performed to avoid penetrating the knee joint. The inflammatory tissue and the non-absorbable suture were taken to bacterial culture (Fig. 3E).
Fig. 3.
Status of the tibial tunnel before and after arthroscopic debridement. A, An inflammatory tissue in the tibial tunnel before debridement; B, graft covering the tunnel bottom; C, debridement of inflammatory tissue by shaver; D, tibial tunnel after debridement. E, inflammatory tissue and non-absorbable suture taken from the tunnel.
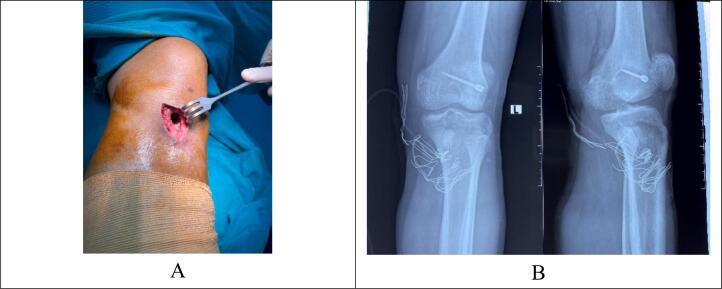
The wound was left open after debridement and was applied to a VAC therapy. The patient was given empiric intravenous antibiotic therapy (oxacillin 8 g/day). On the 3rd day after surgery, the bacterial culture results were Staphylococcus aureus and antibiotic susceptibility tests to levofloxacin, gentamycin, oxacillin, cefoxitin, and vancomycin. We chose oxacillin (8 g/day) and levofloxacin (750 mg/day) for the patient's treatment. After finishing two courses of VAC therapy (Fig. 4A), the patient underwent phase 2 surgery: antibiotic-loaded cement (gentamycin and vancomycin) was introduced in the tibial bone tunnel. Radiographs of the knee joint showed an image of cement filling the tibial tunnel; the cement did not penetrate the joint (Fig. 4B). Intravenous antibiotics are used for 14 days from the date of bacterial culture results. There was no sign of wound infection; the wound healed well after two weeks of cement filling. CRP test was within normal limits. This patient stayed in the hospital for 21 days.
Fig. 4.
A, A surgical site before cementing the tibial tunnel. B, Radiograph of the knee joint after cementing the tibial tunnel.
After discharge, the patient took levofloxacin (750 mg/day) orally for four weeks and was instructed to exercise in the rehabilitation department.
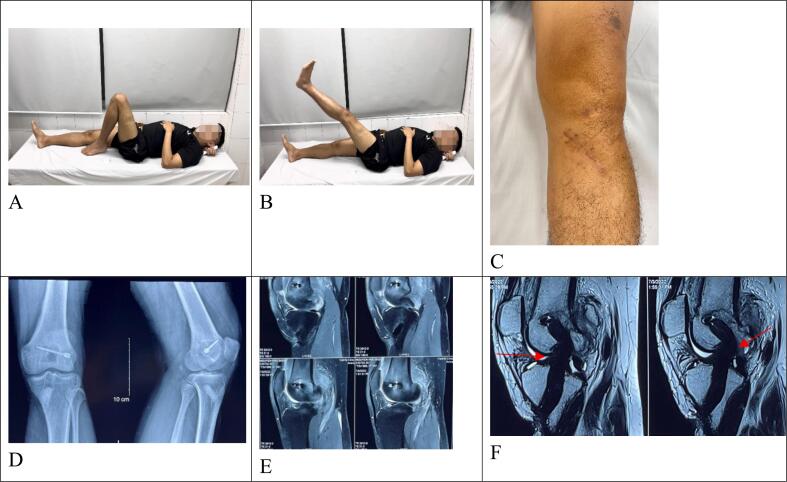
The patient came for a follow-up visit seven months after surgery, with no signs of infection in the knee joint and an anterior incision in the lower leg (Fig. 5C). The patient has no pain, no feeling of joint instability, no limitation of joint range of motion, no limitation in daily activities, IKDC classification was B, Lysholm score was 90 points. Test results for inflammatory markers in the blood were within normal limits (WC: 9.4G/l in which 62 % granulocytes; CRP: 0.58 ng/mL). On the radiograph (Fig. 5D) and magnetic resonance imaging, there was no sign of infection of the tibial tunnel (Fig. 5E), and the ACL graft signal was clear (Fig. 5F). The clinical result was judged satisfactory.
Fig. 5.
Clinical status, radiographs, and MRI 7 months postoperative. A, B, C Seven months postoperative clinical status. D, Radiographs of the left knee joint seven months postoperative. E, F, Left knee MRI seven months postoperative.
3. Discussion
Infection of the knee joint after arthroscopic ACL reconstruction is a rare complication. These complications appeared mainly in the first month after surgery. Extra-articular sole chronic infection of the tibial tunnel is even rarer, and there are only a few case reports in the literature. It is necessary to determine whether the patient has a sole tibial tunnel infection or is a result of septic knee arthritis caused by inflammatory fluid flowing from the joint. The treatment strategies for these conditions are entirely different, so a definitive diagnosis is essential. In the case of tibial tunnel inflammation as a consequence of septic knee arthritis, most patients have typical clinical signs of arthritis such as fever, chills, pain and swelling in the knee, limited joint range of motion [6,7] associated with painful, swelling, and purulent discharge through the anterior medial incision in the lower leg. Inflammatory markers in the blood, such as erythrocyte sedimentation rate and CRP, are often elevated [[7], [8], [9]]. MRI of the knee joint shows a lot of joint fluid, thickening of the synovial membrane, and an image of the inflammatory fluid circulation between the joint and the tibial tunnel [4]. This condition is treated with arthroscopic debridement, continuous irrigation of the joint, and preservation or removal of grafts and implants if the graft is no longer functional [2,3,10]. Therefore, if the lesion in the joint is ignored, the treatment of tibial bone tunnel infection will likely fail and cause severe consequences to the graft and articular cartilage.
Contrary to the above situation, in our case, the patient suddenly noticed the swollen, painful anteromedial incision in the leg while participating in normal daily activities, with a fistula and purulent discharge five months after ACL reconstruction surgery. There was no fever and no clinical symptoms of septic arthritis. Inflammatory markers in the blood were within normal limits. MRI of the knee joint showed diffuse osteitis around the tibial tunnel, but there was no communication with the knee joint and no image of septic arthritis. Our patient's clinical and laboratory characteristics were almost similar to some previous case reports in the literature [3,11,12]. The definitive diagnosis of sole chronic infection of the tibial tunnel requires a detailed history, clinical symptoms combined with inflammatory markers in the blood, and imaging studies to exclude combined septic knee arthritis.
In the literature, there are not many studies regarding chronic infection of the tibial tunnel after ACL reconstruction, so the treatment perspective is still unclear. According to the principle for osteomyelitis surgery, it is necessary to expose the lesion widely to thoroughly remove the inflammatory bone until the healthy bone is reached. Still, for chronic infections of the tibial tunnel, the bone tunnel is often small and deep, making it difficult to observe and evaluate lesions in the tunnel. During the process of “blind” debridement with a curette, it is necessary to be cautious to avoid penetrating the knee joint, so there is a high chance that inflammatory tissue and sutures in the tunnel wall are not eradicated [13]. Some previous reports suggested that the treatment method would be to remove the implant, curettage the inflammatory bone, and cement the tibial tunnel; however, the recurrence rate was still high. Gioi and colleagues performed the abovementioned method but failed and had to use the medial gastrocnemius muscle flap to cover it; the author supposed the leading cause of failure was the remnant of inflammatory bone and non-absorbable suture in the tunnel [4]. To our knowledge, this is the first case report applying an arthroscopic technique to treat chronic infection of the tibial tunnel after ACL reconstruction surgery.
In our case, the patient underwent surgical debridement of the inflammatory tissue using arthroscopic techniques and antibiotic-loaded cement for cementation of the tibial tunnel. We found that the application of the arthroscopic technique has superior advantages over the “blind” curettage: Firstly, the entire inflammatory tissue can be observed in the tibial tunnel wall, and the tunnel bottom can be controlled (the root of the ACL is like a protective barrier between the joint and the tunnel), so it is possible to thoroughly debride the inflammatory bone, remove the foreign body and avoid the injury to the knee joint causes which can cause infection. Secondly, the excessive and uncontrolled debridement, which makes the tibial tunnel defects wider, can be limited, and the overtreatment can make it difficult for patients who require revision surgery later. In this case, the bacteria found after surgery was Staphylococcus aureus. Some studies show the advantages of antibiotic-loaded cement in treating chronic infection of the tibial tunnel after ACL reconstruction [4,11,12]. In addition to filling gaps, antibiotic-loaded cement helps maintain a high concentration of local antibiotics. It diffuses antibiotics into surrounding tissues to improve the effectiveness of local bacteria killing when combined with intravenous antibiotics [14]. Therefore, in this case, besides using antibiotics according to the antibiogram, which were levofloxacin and oxacillin, we used cement mixed with gentamycin and vancomycin to fill the tibial tunnel. Fourteen days after cementing, the incision healed well, and after seven months, there were no signs of infection in the leg and the knee joints. The patient had no pain, no feeling of joint instability, no limitation of joint range of motion, and no limitation in daily activities. Blood tests for inflammatory markers were within normal limits.
4. Conclusion
Sole chronic infection of the tibial tunnel is a rare complication following ACL reconstruction surgery. The definitive diagnosis must be based on clinical symptoms, blood inflammatory markers, and imaging to exclude combined septic knee arthritis. This case report proposes an arthroscopic technique to remove inflammatory tissue and antibiotic-loaded cementation cement in the tibial tunnel. In the future, a study with a larger sample size should be reported to evaluate the effectiveness of this treatment method.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. A copy of the written consent form is available for review by the editor-in-chief of this journal upon request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Funding
No financial support was received to complete this study.
Ethical approval
All procedures were approved by the 108 Central Military Hospital's Institutional Review Board, Hanoi, Vietnam.
Author contribution
Dr. Dung Quoc Nguyen: Conceptualization, Writing - Review & Editing, Supervision.
Dr. Trung Duc Do: Conceptualization, Surgery, Writing - Review & Editing, Supervision.
Dr. Luong Van Nguyen: Conceptualization, Writing - Review & Editing, Supervision.
Dr. Cuong Duc Do: Writing - Review & Editing, Supervision.
Guarantor
Dr. Luong Van Nguyen.
Research registration number
Not applicable.
Conflict of interest statement
The authors declare that they have no conflicts of interest.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
References
- 1.Weng C.J., et al. Outcomes of anterior cruciate ligament reconstruction in patients older than 50 years and younger than 30 years. Orthop. J. Sports Med. 2022;10(5) doi: 10.1177/23259671221094788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waterman B.R., et al. Septic arthritis after anterior cruciate ligament reconstruction: clinical and functional outcomes based on graft retention or removal. Orthop. J. Sports Med. 2018;6(3) doi: 10.1177/2325967118758626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erice A., et al. Septic arthritis following arthroscopic reconstruction of cruciate ligaments of the knee: retrospective case review. Enfermedades Infecciosas y Microbiologia Clinica (English Ed.) 2018;36(6):336–341. doi: 10.1016/j.eimc.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen G.N., Van Nguyen L. Treatment of recurrent infection at the tibial bone tunnel after anterior cruciate ligament reconstruction using a medial gastrocnemius muscle flap - a case report. Int. J. Surg. Case Rep. 2022;94 doi: 10.1016/j.ijscr.2022.107054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cadet E.R., et al. Management of septic arthritis following anterior cruciate ligament reconstruction: a review of current practices and recommendations. J. Am. Acad. Orthop. Surg. 2013;21(11):647–656. doi: 10.5435/JAAOS-21-11-647. [DOI] [PubMed] [Google Scholar]
- 7.Van Tongel A., et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, management and outcome. Am. J. Sports Med. 2007;35(7):1059–1063. doi: 10.1177/0363546507299443. [DOI] [PubMed] [Google Scholar]
- 8.Wang C., et al. C-reactive protein and erythrocyte sedimentation rate changes after arthroscopic anterior cruciate ligament reconstruction: guideline to diagnose and monitor postoperative infection. Arthroscopy. 2014;30(9):1110–1115. doi: 10.1016/j.arthro.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Margheritini F., et al. C-reactive protein and erythrocyte sedimentation rate changes following arthroscopically assisted anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2001;9(6):343–345. doi: 10.1007/s001670100232. [DOI] [PubMed] [Google Scholar]
- 10.Torres-Claramunt R., et al. Managing septic arthritis after knee ligament reconstruction. Int. Orthop. 2016;40(3):607–614. doi: 10.1007/s00264-015-2884-6. [DOI] [PubMed] [Google Scholar]
- 11.Weiss K.S., et al. Delayed tibial osteomyelitis after anterior cruciate ligament reconstruction with hamstrings autograft and bioabsorbable interference screw: a case report and review of the literature. Case Rep. Orthop. 2017;2017 doi: 10.1155/2017/6383526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neill B.J., Molloy A.P., McCarthy T. Osteomyelitis of the tibia following anterior cruciate ligament reconstruction. Int. J. Surg. Case Rep. 2013;4(2):143–145. doi: 10.1016/j.ijscr.2012.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tiemann A.H., Hofmann G.O. Principles of the therapy of bone infections in adult extremities: are there any new developments? Strat. Trauma Limb. Reconstr. 2009;4(2):57–64. doi: 10.1007/s11751-009-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qiu X.S., et al. Coating the plate with antibiotic cement to treat early infection after fracture fixation with retention of the implants: a technical note. BMC Musculoskelet. Disord. 2018;19(1):360. doi: 10.1186/s12891-018-2285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.