Abstract
Aims/Introduction
To estimate the prevalence, awareness, treatment, control rate, and influence factors of type 2 diabetes in Fujian province and provide the scientific basic for prevention.
Materials and Methods
A population‐based study with the analysis of binary logistic regression was carried out to estimate the odds ratios of the influencing factor on type 2 diabetes. Data of the Patient‐Centered Evaluative Assessment of Cardiac Events (PEACE) in southeast China were used. The study sample originated from 12 counties in Fujian province and included 135,352 permanent residents aged 35–75 years in 2021.
Results
The prevalence of type 2 diabetes was 18.32% (24,801/135,352). Among them, 13,921 (56.13%) were aware of their condition, 11,894 (47.96%) were receiving treatment, and 4,537 (18.29%) had achieved control of blood glucose. Multivariate logistic regression analysis showed that older age, men, low‐family income, low‐education level, urban locality, no medical insurance, and histories of myocardial infarction, stroke, dyslipidemia, hypertension, alcohol consumption, and obesity were associated with a higher prevalence of type 2 diabetes.
Conclusions
The prevalence of type 2 diabetes among residents aged 35–75 years in southeast China is high, whereas the status of its low awareness, treatment and control is severe, warranting a broad‐based global strategy, including greater efforts in earlier screening, and more effective and affordable treatment is essential.
Keywords: Diabetes, Influence factors, Treatment, Type 2
The prevalence of type 2 diabetes among residents aged 35–75 years in southeast China is high, whereas the status of its low awareness, treatment and control is severe, warranting a broad‐based global strategy, including greater efforts in earlier screening, and more effective and affordable treatment is essential.
INTRODUCTION
Diabetes is a common noncommunicable disease (NCD) with multiple complications that contribute to the global healthcare burden 1 . According to the 2016 World Health Organization report, approximately 8.5% of the adult population (8.4% women and 9.1% men aged 20–79 years) suffer from type 2 diabetes worldwide 2 , with the largest number of patients in China, India and the USA 3 , 4 , 5 . The World Health Organization, the American Diabetes Association, the World Diabetes Foundation, and other authoritative institutions believe that only by actively carrying out prevention and intervention can we slow down and gradually curb the incidence and progress of diabetes 6 . The World Health Organization estimated that between 2000 and 2030, the number of patients with diabetes would increase by 114% worldwide 7 . Asia is the major site of a rapidly emerging diabetes epidemic. Conservative estimates based on population growth and aging, and the rate of urbanization in Asia showed that India and China would remain the two countries with the highest rates of diabetes by 2030 8 .
Diabetes prevalence in China increased from <1% in the 1980s to 9.7% in 2013 9 . China has the largest number of patients with diabetes, and spends the second highest amount on diabetes and its complications worldwide. At the same time, the population with prediabetes represents a large reservoir of patients at risk of diabetes. Previous research showed low rates of awareness, treatment and control of diabetes in China 10 . Fujian province, in southeast China, is a high‐prevalence area of cerebrovascular disease.
Epidemiological studies of diabetes are abundant, whereas comprehensive community‐based studies of a specific large population are rare. In the present study, the population aged 35–75 years in Fujian townships was recruited, and type 2 diabetes prevalence, awareness, treatment and control rates were investigated to provide a theoretical basis for prevention, as well as treatment and the future development of cardiovascular disease prevention strategies.
MATERIALS AND METHODS
Design and population
In the present study, a unified program, unified training, unified quality control, unified blood glucose monitoring and measurement method were used. The convenient sampling method was carried out, and possible eligible participants were recognized in each village or community through government residential records, and then informed by local community staff through extensive advertising in the newspapers, on television and through the mobile phone app, WeChat. All participants were required to bring their identity cards to the community plaza or community healthcare center to verify that they met both of the inclusion criteria: (1) aged 35–75 years; and (2) permanent residents (living in the county for >6 months). The study design has been previously published. The project protocol was approved by the central ethics committee at Fuwai Hospital, Beijing, China (Approval No. 2014‐574). All enrolled participants provided written informed consent.
Subgroups were divided according to 13 variables including sex, age, residence, education, income, insurance, marriage, occupation, smoking, drinking, hypertension, dyslipidemia and body mass index (BMI). Each subgroup was stratified with at least one variable, and at most variables. The participants in each subgroup were not mutually exclusive, of which >250 people were retained, 536,443 subgroups for prevalence, and 171,555 for awareness, and treatment and control rates, and the result was calculated. After verification of residency, participants who had signed the informed consent agreement were then enrolled. After the inclusion of respondents, face‐to‐face interviews were carried out to collect general information (educational level, annual family income, marital status and medical insurance), lifestyle (smoking and alcohol consumption) and medical history (hypertension, dyslipidemia, myocardial infarction and stroke). Blood pressure, height and weight were measured by standard methods, and BMI was calculated, BMI = weight (kg) / height (m2).
We recruited and trained nurses or doctors from the local district hospitals or community health service centers to carry out investigations. The training covered blood pressure, waist circumference, height, blood lipid and glucose measurements, and questionnaire surveys. The National Center for Cardiovascular Disease, Fujian Provincial Center for Disease Control and Prevention, and Fujian Provincial Hospital provided operation training. All investigators passed an examination before participating in the investigation to ensure reliable results. The right upper arm was measured twice by HEM‐7430 electronic sphygmomanometer (Omron, Tokyo, Japan) for blood pressure, with an interval of 5 min. When the difference in systolic blood pressure was >10 mm Hg, a third measurement was carried out, and the last two measurements were taken as the mean value.
Nurses from the local district hospitals or community health service center were in charge of fasting plasma glucose testing. The fingertip blood of the participants was collected, and fasting plasma glucose (FPG) was detected by an electrochemical biosensor using the Baijie PD‐G001 blood glucose meter (China Qinli Company, Taiwan). The following methods were used for blood sample collection: (1) prepare the inspection instrument, and check whether it is complete and the function is normal; (2) the participant is seated, and 75% alcohol is used to wipe the lateral and the finger pad of the left fingertip, and wait to dry; (3) open the blood glucose meter, take a piece of test paper, tense the skin, press the blood collection needle close to the skin and squeeze from the root of the palm to the fingertip to express a drop of blood; (4) blood squeezed from the fingertip drips to the prescribed range of the test paper, then use the cotton swab to press the puncture until there is no bleeding; and (5) set up the blood glucose meter and needle, take readings and register. Informed consent including precautions is issued to the participants the afternoon before FPG measurement to ensure accuracy. The participants are given the following instructions: (1) no high‐sugar and high‐fat food, meanwhile no fasting at dinner the night before the measurement of FPG to ensure accurate values, alcohol consumption should be avoided; (2) ensure no food (including water) for at least 8 h and sufficient sleep (6–8 h) before measuring; (3) calm down and avoid strenuous exercise; and (4) avoid the influence of medications: try to discontinue medications that affect blood glucose, such as hydrochlorothiazide and dexamethasone, 1 week before. There is no need to stop insulin or other glucose‐lowering drugs in the case of diabetes patients.
A total of 12 counties in nine cities from Fujian province, including Taijiang Fuzhou, Wuping and Zhangping Longyan, Yanping Nanping, Shouning and Zherong Ningde, Hanjiang Putian, Jinjiang Quanzhou, Datian Sanming, Longhai Zhangzhou, Siming and Haicang Xiamen, were selected as the survey sites. The regions were selected on the basis of the geographic location, quality of demographic registries and local capacity to support the study. In each region, three to five urban communities or rural villages were chosen according to their size, population stability (e.g., no significant change in the resident number), and commitment and ability of the local government to carry out the project. Investigation stations were set up in each community plaza or community healthcare center. The central ethics committee at the China National Center for Cardiovascular Disease and the Fuwai Hospital approved this project (No. 2014‐547). Written informed consent was obtained from all participants on entry into the study.
Data collection was completed through the electronic information system, key data, such as blood pressure and blood sugar, were entered twice, logic errors and abnormal questionnaires were monitored through the real‐time monitoring platform. All personal information from the physical measurements and laboratory tests was confidential and stored in an encrypted database. The local community health service center assigned special personnel to collect, organize, double computer backup, preserve and report all of the data, including questionnaires, physical examinations, laboratory tests and training. Fujian Provincial Center for Disease Control and Prevention was responsible for the management, cleaning, summarizing, statistical analysis and double computer backup of the database from each project site.
Definitions
Type 2 diabetes mellitus was defined as FPG ≥7.0 mmol/L or self‐reported to have been diagnosed with type 2 diabetes by grade ≥2 hospitals. The prevalence of type 2 diabetes was defined as the proportion of all participants who met the diagnostic criteria for type 2 diabetes or had been diagnosed by grade ≥2 hospitals grade 11 . The awareness rate of type 2 diabetes was defined as the proportion of all patients with type 2 diabetes who knew they were suffering from diabetes. The treatment rate of type 2 diabetes was defined as the proportion of all patients with type 2 diabetes who took measures, such as lifestyle intervention or drug therapy, to control and treat diabetes. The control rate of type 2 diabetes was defined as the proportion of all patients with type 2 diabetes whose FPG was controlled at ≤7.0 mmol/L. Obesity was defined as BMI ≥28.0 kg/m2. Hypertension was defined as systolic blood pressure ≥140 mmHg (1 mmHg = 0.133 kPa) and/or diastolic blood pressure ≥90 mmHg measured more than three times on a different day 12 . Dyslipidemia was defined as any one of these four types, including high total cholesterol, high low‐density lipoprotein cholesterol, high triglyceride and low high‐density lipoprotein cholesterol (Table 1). The prevalence of drinking was defined as the proportion of all participants who drank alcohol (no matter how much and no matter what type of alcohol including beer, liquor, fruit wine, rice wine, glutinous rice wine, highland barley wine weekly or daily) in the past 12 months.
Table 1.
Clinical diagnostic criteria for dyslipidemia of adults in China
| Clinical classification | Standard of diagnosis (mmol/L) |
|---|---|
| High TC | TC ≥6.2 and TG <2.3 |
| High TG | TG ≥2.3 and TC <6.2 |
| Mixed hyperlipidemia | TG ≥2.3 and TC ≥6.2 |
| Low HDL‐C | HDL‐C <1.0 |
HDL‐C, high‐density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation, and were compared using the Student's t‐test, The enumeration data are expressed as the frequency and percentage, and the comparison between groups was carried out using the χ2‐test, changing the trend of age by the trend χ2‐test. Multivariate non‐conditional logistic regression was used to analyze the influencing factors of the prevalence, awareness, treatment and control of type 2 diabetes. All analyses were carried out using SAS statistical software (release 9.3; SAS Institute Inc., Cary, NC, USA), and a P‐value <0.05 was considered statistically significant.
RESULTS
Demographic characteristics
A total of 135,352 participants aged 35–75 years were included in the present study, and 54,794 of the participants (40.50%) were men; the mean age was 56.70 ± 9.87 years. Participants had a higher representation of people aged 40–70 years (63.39%). The vast majority of participants (124,078; 91.67%) were married. A great proportion had low education (76.98%) compared with high school or above (23.02%). A higher proportion of participants from rural (70.72%) than urban (29.28%) localities responded to our survey. Participants whose family income was ≥50,000 RMB (30.17%) were lower than those with household incomes <50,000 RMB (69.83%). Most respondents (97.11%) had medical insurance. Smokers counted for 25,849 (19.10%), and obesity 14,942 (11.04%). A low prevalence of history of myocardial infarction (416; 0.31%) and stroke (731; 0.54%) was reported in this population aged 30–75 years, which was significantly higher among men than women (0.43 vs 0.22%, P < 0.001; 0.85 vs 0.33%, P < 0.001). The majority of participants (121,862, 90.03%) reported that they had never drunk alcohol. A significant difference in the prevalence of regular alcohol drinkers was observed between men and women (21.16 vs 2.35%, P < 0.001; Table 2).
Table 2.
Characteristics of respondents, and prevalence, awareness, treatment and control of type 2 diabetes
| Characteristics | n † | Prevalence ‡ (%) | Awareness § (%) | Treatment ¶ (%) | Control †† (%) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 54,794 (40.48) | 10,645 (19.43) | 5,832 (54.79) | 4,911 (46.13) | 1,903 (17.88) |
| Female | 80,558 (59.52) | 14,156 (17.58) | 8,089 (57.14) | 6,983 (49.33) | 2,634 (18.61) |
| χ2 | 75.34* | 13.69* | 24.84* | 2.93 | |
| Age (years) | |||||
| ≥35 | 5,903 (4.36) | 255 (4.32) | 67 (26.27) | 45 (17.65) | 19 (7.45) |
| ≥40 | 29,533 (21.82) | 2,560 (8.67) | 960 (37.50) | 755 (29.49) | 309 (12.07) |
| ≥50 | 42,288 (31.24) | 7,392 (17.48) | 3,972 (53.73) | 3,302 (44.67) | 1,260 (17.05) |
| ≥60 | 43,509 (32.15) | 10,691 (24.57) | 6,501 (60.81) | 5,628 (52.64) | 2,159 (20.19) |
| ≥70~75 | 14,119 (10.43) | 3,903 (27.64) | 2,421 (62.03) | 2,164 (55.44) | 790 (20.24) |
| trendχ2 | 4,590.49* | 620.55* | 657.29* | 131.21* | |
| Urban and rural | |||||
| Urban | 39,629 (29.28) | 8,444 (21.31) | 5,504 (65.18) | 4,735 (56.08) | 2,098 (24.85) |
| Rural | 95,723 (70.72) | 16,357 (17.09) | 8,417 (51.46) | 7,159 (43.77) | 2,439 (14.91) |
| χ2 | 334.38* | 425.99* | 338.03* | 368.2* | |
| High school or above | |||||
| Yes | 31,157 (23.02) | 5,064 (16.25) | 3,045 (60.13) | 2,510 (49.57) | 1,163 (22.97) |
| No | 104,195 (76.98) | 19,737 (18.94) | 10,876 (55.10) | 9,384 (47.55) | 3,374 (17.09) |
| χ2 | 117.47* | 41.34* | 23.14* | 93.17* | |
| Annual family income ≥50,000 RMB | |||||
| Yes | 40,829 (30.17) | 6,886 (16.87) | 4,120 (59.83) | 3,531 (51.28) | 1,422 (20.65) |
| No | 94,523 (69.83) | 17,915 (18.95) | 9,801 (54.71) | 8,363 (46.68) | 3,115 (17.39) |
| χ2 | 83.74* | 53.02* | 42.11* | 35.79* | |
| Married | |||||
| Yes | 124,078 (91.67) | 22,461 (18.10) | 12,545 (55.85) | 10,690 (47.59) | 4,093 (18.22) |
| No | 11,274 (8.33) | 2,340 (20.76) | 1,376 (58.80) | 1,204 (51.45) | 444 (18.98) |
| χ2 | 50.12* | 7.5* | 12.65* | 0.90 | |
| Medical insurance | |||||
| Yes | 131,440 (97.11) | 23,915 (18.19) | 13,399 (56.03) | 11,424 (47.77) | 4,369 (18.27) |
| No | 3,912 (2.89) | 886 (22.65) | 522 (58.92) | 470 (53.05) | 168 (18.96) |
| χ2 | 50.46* | 2.90 | 9.54* | 0.31 | |
| History of myocardial infarction | |||||
| Yes | 416 (0.31) | 136 (32.69) | 106 (77.94) | 99 (72.79) | 43 (31.62) |
| No | 134,936 (99.69) | 24,665 (18.28) | 13,815 (56.01) | 11,795 (47.82) | 4,494 (18.22) |
| χ2 | 57.58* | 21.71* | 33.8* | 16.25* | |
| History of stroke | |||||
| Yes | 731 (0.54) | 221 (30.23) | 175 (79.19) | 154 (69.68) | 73 (33.03) |
| No | 134,621 (99.46) | 24,580 (18.26) | 13,746 (55.92) | 11,740 (47.76) | 4,464 (18.16) |
| χ2 | 69.67* | 48.13* | 42.17* | 32.41* | |
| History of hypertension | |||||
| Yes | 35,991 (26.59) | 11,428 (31.75) | 7,732 (67.66) | 6,725 (58.85) | 2,776 (24.29) |
| No | 99,361 (73.41) | 13,373 (13.46) | 6,189 (46.28) | 5,169 (38.65) | 1,761 (13.17) |
| χ2 | 5,908.88* | 1,143.74* | 1,006.86* | 511.37* | |
| Smoking | |||||
| Yes | 34,593 (25.56) | 6,626 (18.04) | 3,590 (54.18) | 3,021 (45.59) | 1,189 (17.94) |
| No | 100,759 (74.44) | 18,175 (19.15) | 10,331 (56.84) | 8,873 (48.82) | 3,348 (18.42) |
| χ2 | 22.72* | 13.97* | 20.26* | 1.11 | |
| Drinking | |||||
| Yes | 13,490 (9.97) | 2,666 (19.76) | 1,232 (46.21) | 1,001 (37.55) | 358 (13.43) |
| No | 121,862 (90.03) | 22,135 (18.16) | 12,689 (57.33) | 10,893 (49.21) | 4,179 (18.88) |
| χ2 | 21.17* | 119.36* | 129.72* | 47.44* | |
| Obesity | |||||
| Yes | 14,942 (11.04) | 4,063 (27.19) | 2,287 (56.29) | 1,967 (48.41) | 718 (17.67) |
| No | 120,410 (88.96) | 20,738 (17.22) | 11,634 (56.10) | 9,927 (47.87) | 3,819 (18.42) |
| χ2 | 883.08* | 0.05 | 0.40 | 6.35* | |
| Total | 135,352 (100) | 24,801 (18.32) | 13,921 (56.13) | 11,894 (47.96) | 4,537 (18.29) |
P‐values < 0.05.
The data outside the brackets are the number of participants, and inside the brackets are the composition ratios (%).
The data outside the brackets are the number of patients, and inside the brackets are the prevalence rates (%).
The data outside the brackets are the number of those who know they are patients of type 2 diabetes, and inside the brackets are the awareness rates (%).
The data outside the brackets are the number of those who take measures, such as lifestyle intervention or drug therapy among type 2 diabetes patients, and inside the brackets are the treatment rates (%).
The data outside the brackets are the number of those whose fasting plasma glucose were controlled at ≤7.0 mmol/L among type 2 diabetes patients, and inside the brackets are the control rates (%).
Prevalence, awareness, treatment and control of type 2 diabetes
A total of 24,801 patients with type 2 diabetes were screened in this study, with a prevalence rate of 18.32%. The prevalence of type 2 diabetes in men (10,645; 19.43%) was higher than that in women (14,156; 17.58%), and it was lower in rural areas (16,357; 17.09%) than in urban areas (8,444; 21.31%), the difference was statistically significant (P < 0.05). The prevalence of type 2 diabetes increased with age (P < 0.05). The awareness, treatment and control rates of type 2 diabetes were 56.13% (13,921/24,801), 47.96% (11,894/24,801) and 18.29% (4,537/24,801), respectively. The awareness, treatment and control rates of type 2 diabetes in rural areas were lower than those in urban areas, and the difference was statistically significant (P < 0.05; Table 2).
Multivariate logistic regression analysis of influencing factors for prevalence, awareness, treatment and control of type 2 diabetes
Multivariate logistic regression analysis was carried out with the statistical variables of univariate analysis as independent variables, and the prevalence, awareness, treatment and control of type 2 diabetes as dependent variables. Multivariate logistic regression analysis showed that older age (≥40 years odds ratio [OR] 1.68, ≥50 years OR 3.73, ≥60 years OR 5.14, 70–75 years OR 5.62), men (OR 1.13), low family income (OR 1.15), low education level (OR 1.20), urban (OR 1.18), no medical insurance (OR 1.32), and histories of myocardial infarction (OR 1.41), stroke (OR 1.14), dyslipidemia (OR 2.18) and hypertension (OR 2.25), alcohol consumption (OR 1.11) and obesity (OR 1.56) were associated with a higher prevalence of type 2 diabetes. Among those who were suffering from type 2 diabetes, older age (≥≤40 years OR 1.61, ≥50 years OR 2.70, ≥60 years OR 3.27, 70–75 years OR 3.16), women (OR 1.10), high school or above (OR 1.12), household income >50,000 yuan (OR 1.25), urban (OR 1.48), and histories of myocardial infarction (OR 1.73), stroke (OR 1.92), dyslipidemia (OR 2.91) and hypertension (OR 2.04) were associated with higher awareness of type 2 diabetes. older age (≥40 years OR 1.85, ≥50 years OR 3.10, ≥60 years OR 3.87, 70–75 years OR 4.02), women (OR 1.14), high school or above (OR 1.01), household income >50,000 yuan (OR 1.23), urban (OR 1.40), and histories of myocardial infarction (OR 1.94), stroke (OR 1.67), dyslipidemia (OR 2.10) and hypertension (OR 1.90) were associated with higher treatment of type 2 diabetes. Those who were smoking (OR 0.81) and drinking (OR 0.65) had lower treatment; older age (≥40 years OR 1.71, ≥50 years OR 2.06, ≥60 years OR 2.32, 70–75 years OR 2.15), high school or above (OR 1.27), household income >50,000 yuan (OR 1.13), urban (OR 1.58), and histories of myocardial infarction (OR 2.08), stroke (OR 1.57), dyslipidemia (OR 1.87) and hypertension (OR 1.85) were associated with higher control of type 2 diabetes. Those who were smoking (OR 0.87) and drinking (OR 0.66) had lower control (Table 3, Figure 1).
Table 3.
Multivariate logistic regression analysis of the prevalence, awareness, treatment and control of type 2 diabetes
| Variables † | Group | Prevalence | Awareness | Treatment | Control |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Age (years) | ≥40 | 1.91 (1.68–2.18)* | 1.61 (1.20–2.16)* | 1.85 (1.32–2.59)* | 1.71 (1.05–2.78)* |
| ≥50 | 3.73 (3.28–4.24)* | 2.70 (2.02–3.60)* | 3.10 (2.23–4.31)* | 2.06 (1.28–3.31)* | |
| ≥60 | 5.14 (4.51–5.84)* | 3.27 (2.45–4.36)* | 3.87 (2.78–5.38)* | 2.32 (1.44–3.72)* | |
| ≥70 | 5.62 (4.92–6.42)* | 3.16 (2.35–4.24)* | 4.02 (2.88–5.61)* | 2.15 (1.33–3.48)* | |
| Sex | Female | 0.92 (0.89–0.96)* | 1.10 (1.05–1.16)* | 1.14 (1.08–1.20)* | 1.03 (0.95–1.12) |
| Married | Yes | 0.84 (0.81–0.89)* | 0.89 (0.81–0.97)* | 0.86 (0.79–0.93)* | 1.01 (0.90–1.13) |
| Annual family income ≥50,000 RMB | Yes | 0.87 (0.84–0.89)* | 1.25 (1.18–1.32)* | 1.23 (1.16–1.31)* | 1.13 (1.05–1.22)* |
| High school or above | Yes | 0.83 (0.80–0.86)* | 1.12 (1.04–1.21)* | 1.01 (0.94–1.08) | 1.27 (1.16–1.38)* |
| Urban | Yes | 1.18 (1.14–1.22)* | 1.48 (1.40–1.57)* | 1.40 (1.33–1.49)* | 1.58 (1.47–1.69)* |
| Medical insurance | Yes | 0.84 (0.77–0.91)* | 0.89 (0.77–1.02) | 0.81 (0.71–0.93)* | 0.96 (0.81–1.13) |
| Myocardial infarction | Yes | 1.41 (1.14–1.74)* | 1.73 (1.13–2.65)* | 1.94 (1.31–2.88)* | 2.08 (1.44–2.98)* |
| Stroke | Yes | 1.14 (0.97–1.34)* | 1.92 (1.37–2.69)* | 1.67 (1.24–2.25)* | 1.57 (1.17–2.10)* |
| Dyslipidemia | Yes | 2.18 (2.05–2.30)* | 2.91 (2.57–3.29)* | 2.10 (1.89–2.33)* | 1.87 (1.68–2.08)* |
| Hypertension | Yes | 2.25 (2.18–2.32)* | 2.04 (1.93–2.16)* | 1.90 (1.80–2.01)* | 1.85 (1.73–1.99)* |
| Smoking | Yes | 0.99 (0.95–1.02) | 0.84 (0.78–0.91)* | 0.81 (0.76–0.86)* | 0.87 (0.80–0.95)* |
| Drinking | Yes | 1.11 (1.06–1.16)* | 0.65 (0.59–0.71)* | 0.65 (0.59–0.71)* | 0.66 (0.59–0.75)* |
| Obesity | Yes | 1.56 (1.49–1.62)* | 1.01 (0.94–1.08) | 1.02 (0.96–1.09) | 0.95 (0.87–1.04) |
P‐values < 0.05.
Variable assignments: age, 1 = 35 to <40, 2 = 40 to <50, 3 = 50 to <60, 4 = 60 to <70, 5 = 70–75; sex, 1 = male, 2 = female; married, 0 = no, 1 = yes; annual family income ≥50,000 RMB, 0 = no, 1 = yes; high school or above, 0 = no, 1 = yes; urban, 0 = no, 1 = yes; medical insurance, 0 = no, 1 = yes; myocardial infarction, 0 = no, 1 = yes; stroke, 0 = no, 1 = yes; dyslipidemia, 0 = no, 1 = yes; hypertension, 0 = no, 1 = yes; smoking, 0 = no, 1 = yes; drinking, 0 = no, 1 = yes; obesity, 0 = no, 1 = yes.
CI, confidence interval; OR, odds ratio.
Figure 1.
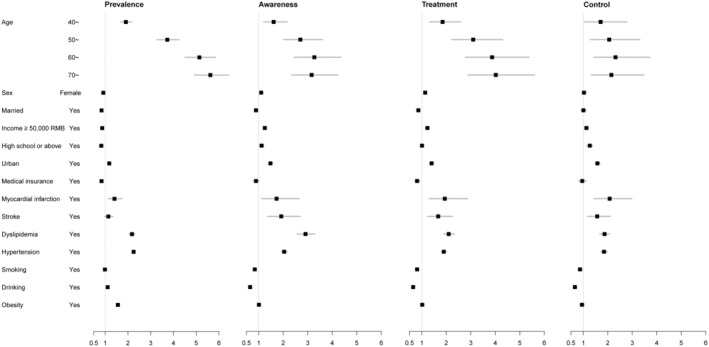
Forest plots for multivariate logistic regression analysis of the prevalence, awareness, treatment and control of type 2 diabetes.
DISCUSSION
In the present study, specialized epidemiological investigations for the prevalence, awareness, treatment, control rates and influencing factors on type 2 diabetes in individuals aged 35–75 years from 12 counties of southeast China were explored in 2021. A total of 135,352 community residents were enrolled, detecting 24,801 patients, with an overall prevalence rate of 18.32%, lower than that in the Inner Mongolia Autonomous Region in north China (19.9%) 13 . As a large country with many type 2 diabetes patients, the prevalence had obvious regional differences, generally showing the characterized distribution of “high in the north and low in the south”. The reasons might be related to diet, exercise and climate 14 . Residents in the northern region mainly eat meat from livestock, and prefer frying and grilling, whereas residents in the southeast coastal region mainly eat seafood, fruits and vegetables, and prefer lighter cooking methods, such as stewing, soup, steaming and boiling. The residents in the north area rarely play outdoor sports, mostly because of the cold climate in the long winter, whereas suitable temperatures all year round in the southeast provide residents with good climatic conditions for physical exercise outdoors.
A study in Iran showed that the prevalence, awareness, treatment and control of type 2 diabetes among the adult residents aged ≥35 years of Tehran were 16.7, 82.8, 71.9 and 31.7%, respectively 15 . In the present investigation, the prevalence of diabetes (18.32%) was higher than in Iran, whereas its awareness (56.13%), treatment (47.96%) and control (18.29%) were obviously lower than that of Tehran. It can be seen that the type 2 diabetes control task in China, including Fujian, province remains challenging, and more attention should be paid to raising the control rate and lowering prevalence, meanwhile further increasing awareness and treatment. The fact that the living standard has been continuously improved and the average life expectancy has constantly increased might be related to the increase in type 2 diabetes prevalence 16 .
The study showed that type 2 diabetes prevalence was higher in urban areas (21.31%) compared with rural areas (17.09%), and in men (19.43%) higher than in women (17.58%). The possible reason was that residents living in urban areas had more daily entertainment, ate more fatty and sugary meals, and engaged in less physical activity, especially men. In addition, residents living in urban areas had superior conditions, such as medical treatment, medical insurance, physical examination, health‐supporting environment, self‐care and life expectancy was longer 17 . This project suggested that during the process of urbanization in China, coordinating the relationship between urbanization and the comprehensive prevention of chronic diseases was of great significance, especially for type 2 diabetes. Meanwhile, it was necessary to strengthen urban men's diabetes screening for those aged 35–75 years. In recent years, China's network of primary medical and health institutions has improved. By the end of 2021, nearly 980,000 medical and health institutions had been built nationwide, with >4.4 million health personnel, achieving full coverage of streets, communities, townships and villages, and 90% of families can reach the nearest medical point within 15 min.
Multivariate logistic regression analysis showed that older individuals with a history of myocardial infarction, stroke, dyslipidemia and hypertension had a higher prevalence, awareness, treatment and control of type 2 diabetes. The main reason was that the metabolic function and immunity in the body had declined, resulting in the glucose metabolism function weakening, leading to hyperglycemia and diabetes 18 . At the same time, there were increased opportunities to receive diabetes‐related knowledge with increasing age. A study showed that increasing age, and risks of developing hypertension and dyslipidemia would correspondingly increase the opportunity of receiving medical education, improving awareness and treatment of type 2 diabetes 19 .
The relationship between drinking and type 2 diabetes remains controversial. According to a meta‐analysis, moderate alcohol consumption leads to a lower risk of type 2 diabetes, whereas heavy alcohol consumption raises the risk 20 . In the present study, those who were addicted to alcohol had a high prevalence of type 2 diabetes, whereas they had low awareness, treatment and control. The reason might be that people who often drink alcohol do not usually pay attention to their health, and they do not know when they develop diabetes if they do not see a doctor or improve their lifestyle, let alone their blood sugar control. Previous studies have shown that smoking is a risk factor for diabetes, and the larger the cumulative smoking amount, the higher the risk 21 .
Previous studies have shown that obesity is associated with an increased risk of type 2 diabetes 22 , 23 , 24 . The present study confirmed this. Research showed that obesity, particularly abdominal intraabdominal fat, intrahepatic and intramuscular triglyceride, was a major risk factor for prediabetes and type 2 diabetes because of insulin resistance and β‐cell dysfunction. Accordingly, the worldwide increase in the prevalence of obesity led to the concomitant increase in the prevalence of type 2 diabetes 25 . These results emphasized the importance of weight loss for obese people. It would be necessary to establish appropriate policies, such as providing weight meters in pharmacies, restaurants and other public places, as well as building convenient and accessible sports facilities 26 .
Integrating NCDs, including type 2 diabetes, programs within the current primary medical and health institutions, along with the effective implementation of such programs, are essential to achieving health and well‐being, and ensuring universal access to health services by 2030. There is also a need for developing and implementing effective, context‐specific, and cost‐effective interventions in China. The “Health China 2030” planning outline emphasizes the implementation of a comprehensive prevention and control strategy for NCDs, strengthening the construction of national demonstration areas for comprehensive prevention and control of NCDs, Basically achieving full coverage of management interventions for hypertension and diabetes.
The prevalence of type 2 diabetes among residents aged 35–75 years in Fujian province, in southeast China, is higher, whereas awareness, treatment and control are still lower. Given this, it is necessary to strengthen health education and information, and regular screening. At the same time, it is necessary to strengthen the treatment, intervention and management of detected patients, and improve patient compliance, ultimately increasing the control of type 2 diabetes.
DISCLOSURE
The authors declare no conflict of interest.
Approval of the research protocol: The studies involving human participants were reviewed and approved by the ethics committee of Fuwai Hospital, Chinese Academy of Medical Sciences (No. 2014‐547).
Informed consent: The patients/participants provided their written informed consent to participate in this study.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
ACKNOWLEDGMENTS
We express our sincere gratitude to the 12 counties (Taijiang Fuzhou, Wuping and Zhangping Longyan, Yanping Nanping, Shouning and Zherong Ningde, Hanjiang Putian, Jinjiang Quanzhou, Datian Sanming, Longhai Zhangzhou, Siming and Haicang Xiamen) in Fujian province for providing the site and organization for the research. This study was sponsored by the Fujian Provincial Health Technology Project (2020GGA023).
REFERENCES
- 1. Ko YM, Ko SH, Han K, et al. Importance of awareness and treatment for diabetes in influenza vaccination coverage of diabetic patients under 65 years: A population‐based study. Diabetes Metab J 2021; 45: 55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Diabetes 2018. Available from: https://www.who.int/news‐room/fact‐sheets/detail/diabetes/ Accessed May 22, 2020.
- 3. Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018; 138: 271–281. [DOI] [PubMed] [Google Scholar]
- 4. Thankappan KR, Daivadanam M, Mini GK, et al. Editorial: Awareness, treatment, and control of hypertension or diabetes in India: The impact of public health promotion. Front Public Health 2022; 10: 906862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thakur JS, Nangia R. Prevalence, awareness, treatment, and control of hypertension and diabetes: Results from two state‐wide STEPS survey in Punjab and Haryana, India. Front Public Health 2022; 10: 768471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dalfrà MG, Burlina S, Del Vescovo GG, et al. Adherence to a follow‐up program after gestational diabetes. Acta Diabetol 2020; 57: 1473–1480. [DOI] [PubMed] [Google Scholar]
- 7. Uthman OA, Ayorinde A, Oyebode O, et al. Global prevalence and trends in hypertension and type 2 diabetes mellitus among slum residents: A systematic review and meta‐analysis. BMJ Open 2022; 12: e052393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dahal PK, Rawal LB, Mahumud RA, et al. Economic evaluation of health behavior interventions to prevent and manage type 2 diabetes mellitus in Asia: A systematic review of randomized controlled trials. Int J Environ Res Public Health 2022; 19: 10799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang L, Peng W, Zhao Z, et al. Prevalence and treatment of diabetes in China, 2013‐2018. JAMA 2021; 326: 2498–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liu C, Li X, Lin M, et al. A cross‐sectional study on diabetes epidemiology among people aged 40 years and above in Shenyang, China. Sci Rep 2020; 10: 17742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ninomiya H, Katakami N, Matsuoka TA, et al. Association between poor psychosocial conditions and diabetic nephropathy in Japanese type 2 diabetes patients: A cross‐sectional study. J Diabetes Investig 2018; 9: 162–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dorobantu M, Tautu OF, Dimulescu D, et al. Perspectives on hypertension's prevalence, treatment and control in a high cardiovascular risk East European country: Data from the SEPHAR III survey. J Hypertens 2018; 36: 690–700. [DOI] [PubMed] [Google Scholar]
- 13. Xi Y, Cao N, Niu L, et al. Prevalence and treatment of high cardiovascular disease risk in Inner Mongolia, China. Rev Cardiovasc Med 2021; 22: 521–529. [DOI] [PubMed] [Google Scholar]
- 14. Kim YJ, Jeong IK, Kim SG, et al. Changes in the quality of life in patients with type 2 diabetes mellitus according to physician and patient behaviors. Diabetes Metab J 2020; 44: 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oraii A, Shafiee A, Jalali A, et al. Prevalence, awareness, treatment, and control of type 2 diabetes mellitus among the adult residents of tehran: Tehran Cohort Study. BMC Endocr Disord 2022; 22: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu X, Wang L, Wang P, et al. The dynamics of type 2 diabetes mellitus prevalence and management rates among rural population in Henan Province, China. J Diabetes Res 2017; 2017: 9092759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Avilés‐Santa ML, Monroig‐Rivera A, Soto‐Soto A, et al. Current state of diabetes mellitus prevalence, awareness, treatment, and control in Latin America: Challenges and innovative solutions to improve health outcomes across the continent. Curr Diab Rep 2020; 20: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. den Braver NR, de Vet E, Duijzer G, et al. Determinants of lifestyle behavior change to prevent type 2 diabetes in high‐risk individuals. Int J Behav Nutr Phys Act 2017; 14: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hu M, Wan Y, Yu L, et al. Prevalence, awareness and associated risk factors of diabetes among adults in Xi'an, China. Sci Rep 2017; 7: 10472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bhattarai M, Salih M, Regmi M, et al. Association of sodium‐glucose cotransporter 2 inhibitors with cardiovascular outcomes in patients with type 2 diabetes and other risk factors for cardiovascular disease: A meta‐analysis. JAMA Netw Open 2022; 5: e2142078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yang Y, Peng N, Chen G, et al. Interaction between smoking and diabetes in relation to subsequent risk of cardiovascular events. Cardiovasc Diabetol 2022; 21: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jiang C, Cifu AS, Sam S. Obesity and weight management for prevention and treatment of type 2 diabetes. JAMA 2022; 328: 389–390. [DOI] [PubMed] [Google Scholar]
- 23. Klein S, Gastaldelli A, Yki‐Järvinen H, et al. Why does obesity cause diabetes? Cell Metab 2022; 34: 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Da Porto A, Cavarape A, Colussi G, et al. Polyphenols rich diets and risk of type 2 diabetes. Nutrients 2021; 13: 1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. SantaCruz‐Calvo S, Bharath L, Pugh G, et al. Adaptive immune cells shape obesity‐associated type 2 diabetes mellitus and less prominent comorbidities. Nat Rev Endocrinol 2022; 18: 23–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shrestha R, Yadav UN, Shrestha A, et al. Analyzing the implementation of policies and guidelines for the prevention and management of type 2 diabetes at primary health care level in Nepal. Front Public Health 2022; 10: 763784. [DOI] [PMC free article] [PubMed] [Google Scholar]


