Abstract
Introduction
Having good knowledge and a favorable attitude toward human papillomavirus (HPV) and HPV vaccinations is the cornerstone for increasing the use of HPV vaccinations and preventing cervical cancer. The objective of this study was to evaluate the level of knowledge, attitudes, and practices regarding HPV and HPV vaccinations, as well as to identify associated factors among female undergraduate health science students at both the University of Gondar (UoG) and Bahir Dar University (BDU), Amhara, Ethiopia.
Methods
Institutional-based multicenter descriptive cross-sectional study was conducted from June 1, 2023, to July 30, 2023. A multistage sampling technique was used to select 633 female undergraduate health science students, and data were collected using a structured, self-administered questionnaire. The data were coded, entered in Epi-data, and exported to SPSS for analysis. Variables with a P-value < 0.25 in the bivariate analysis were inserted in a multivariate logistic regression model, and those with a P-value of < 0.05 in the multivariate binary logistic regression were considered statistically significant factors for knowledge, attitude, and practice regarding HPV and vaccine against it.
Results
The study included 600 participants with a mean age of 20.8 ± 0.75 years. Using Bloom’s cutoff points for the KAP study, among the participants, 436 (72.7%) had good knowledge about HPV, whereas 315 (52.5%) had good knowledge about HPV vaccinations. More than half of the participants, 359 (59.8%) heard about HPV vaccinations in Ethiopia. More than half of the participants, 342 (57%) had favorable attitudes toward HPV vaccinations. Only 261 (43.5%) participants believed the HPV vaccine was safe and effective. All participants had never been tested for HPV, and 471 (78.5%) refused to have their samples for regular HPV testing. The factors like ages between 21 and 23 years (AOR, 2.12, 95% CI: 1.22–3.09) and favorable attitudes toward HPV vaccinations (AOR: 1.88; 95%, CI: 1.15–3.41) were associated with the participant’s knowledge about HPV vaccinations. Having good knowledge about the virus (AOR: 1.92; 95%, CI: 1.11–5.88) and its vaccine (AOR:1.60; 95%CI: 1.07–2.47) were factors associated with the attitude of the participants about HPV vaccinations. Additionally, HPV vaccination practice was significantly associated with the attitude of the participants toward HPV vaccinations (AOR: 1.85; 95%CI: 1.15–3.45), knowledge about HPV (AOR: 1.18; 95%CI: 0.55–5.50), and HPV vaccinations (AOR: 1.85; 95%CI: 1.08–2.44).
Conclusion
This study revealed that half of the students had good knowledge and a favorable attitude toward HPV vaccinations, but there was poor HPV vaccination practice. There is still a need for continued health education, training, and counseling services for students to strengthen HPV vaccination practices, improve students’ attitudes and knowledge about the benefits of vaccination, and improve counseling abilities against HPV-induced cancer.
Supplementary information
The online version contains supplementary material available at 10.1186/s12905-024-03279-6.
Keywords: Knowledge, Attitude, Practice, Human papillomavirus, Infection, Vaccine, Ethiopia
Introduction
Human papillomavirus (HPV) is a viral infectious disease (IDs) commonly associated with Sexually Transmitted Diseases (STDs) and is a major cause of the global disease burden. It is a common human infection that can cause cervical cancer, other anogenital cancers, genital warts, and recurrent respiratory papillomatosis [1–4].
HPV infection is most common in young and sexually active individuals. It is so prevalent that approximately 75-80% of sexually active individuals become infected in their lifetime [4]. There are more than 100 HPV genotypes. Of these, at least 13 genotypes cause cervical, genital, and pharyngeal cancers. Non-oncogenic HPV types 6 and 11 are responsible for 90% of genital warts, whereas HPV types 16 and 18 are responsible for 70% of cervical malignancies, and most HPV infections are asymptomatic or subclinical, contributing to the rapid transmission and spread of the virus [4, 5].
Persistent infection with high HPV risk has been established as the primary cause of cervical cancer, which is the second most frequent type of cancer among women in Ethiopia, with an incidence rate of approximately 13.0 per 100, 000 women per year [6, 7]. However, anogenital cancers other than cervix are limited in women, but there is an increase in the anus, vulva, and vagina cases, with incidence rates of 0.27, 0.73, and 0.39, respectively, in women, whereas the incidence rates of prostate, anus, and penis cases in men are 4.73, 0.25, and 0.06, respectively [7].
HPV vaccinations have a great potential to prevent HPV-related infections in millions of women and men worldwide. It can prevent more than 90% of cervical cancers [6]. The World Health Organization (WHO) recommends that girls aged 9–14 years be the primary target group for HPV vaccination, with females aged 15 years and older serving as the secondary target population [8]. HPV vaccinations are recommended for everyone up to the age of 26 [9].
Ethiopia also launched the HPV vaccine for the first time with the provision of the Global Alliance for Vaccine and Immunization (GAVI) in 2018. Currently, two doses of the HPV vaccine are administered to females aged 9–14 years at 6-month intervals through a school-based approach [6]. However, the immunization program will not be accepted in Ethiopia because certain members of the community still oppose it for different reasons. Social influence, knowledge and attitude about cervical cancer, HPV, and its vaccine, acceptability of the vaccine, or willingness of an individual to be vaccinated, child age, perceived access to the vaccine, religious background, and perceptions about disease severity can result in vaccine refusal. As a result, the adolescent girls expressed their reluctance to vaccinate. These barriers have been the barriers to successful HPV vaccination programs in Ethiopia [3, 6, 9].
There are limited studies evaluating the knowledge, attitudes, and practices of university students regarding HPV infection and HPV vaccinations in Ethiopia. Therefore, this study aimed to evaluate the level of knowledge, attitudes, and practices of female undergraduate health science students toward HPV infection and HPV vaccinations and to identify associated factors at the University of Gondar (UoG) and Bahir Dar University (BDU). The findings of this study will help identify students’ knowledge, attitudes, and practices about HPV infection and HPV vaccinations to develop strategies to enhance students’ knowledge, attitudes, and practices. Improving students’ knowledge, attitudes, and practices about HPV vaccinations, thus contributing to reducing the incidence of HPV-induced cancer among young adults in the community.
Materials and methods
Study area, design, and period
An institutional-based multicenter cross-sectional study was conducted to evaluate the knowledge, attitudes, and practices of female undergraduate health science students at both UoG and BDU, Amhara, Ethiopia, from June 1, 2023, to July 30, 2023. UOG is located in Gondar city, the capital of the Central Gondar Administrative Zone, which is 747 km from Addis Ababa in the northwest direction. BDU is located in Bahir Dar city, northwest Ethiopia, which is the capital of the Amhara National Regional State (ANRS). This city is located on the southern shore of Lake Tana, a tributary of the Blue Nile. The city is located approximately 565 km north to northwest of Addis Ababa.
Source and study population
The source population was all female undergraduate health science students enrolled at both UoG and BDU for the 2023/2024 academic year, while the study population was those who fulfilled the inclusion criteria at both Universities during the data collection period.
Eligibility criteria
Female undergraduate health science students who attended classes during the data collection period and agreed to participate in the survey were included. Graduate students were excluded from this study.
Independent variables
Sociodemographic characteristics of female health science students (age, religion, residence, department, undergraduate year).
Dependent variables
Knowledge, attitudes, and practices of female health science students toward HPV and HPV vaccinations.
Sample size determination and sampling techniques
The single population proportion formula was used to calculate the sample size based on the assumption that a Proportion (P) of 50% yields a maximum sample size. Furthermore, 1.5% design effect, α value of 0.05, Zα/2 = 1.96, and margin of error (d) = 5% were used. This gives a sample size of 576. Assuming a 10% non-response rate, the final sample size is 633.
A multistage sampling technique was used to select participants. First, out of the 10 departments, four departments (pharmacy, nursing, midwifery, and medical laboratory) were selected randomly. The sample size was distributed proportionally to the two universities, selected departments, and each batch. Finally, the sample was selected from the list of students in all departments and batches using simple random sampling techniques.
 |
Data collection tool and procedures
Closed and open-ended self-administered questionnaires were developed in English and comprised four extensive areas: sociodemographic characteristics, knowledge about HPV infection and HPV vaccinations, attitudes, and practices toward HPV vaccinations. Data were collected by experienced pharmacists after providing training. The researchers closely supervised the data collection process and cross-checked the completeness of the questionnaires. The questionnaire used to collect data in the current study is presented in the Supplementary Information (Supplementary Material 1).
Outcome measurement
Knowledge about HPV infection and HPV vaccination was measured using seven and eight items, respectively. Every correct response received a “score of 1” while every incorrect response received a “score of 0.” The total points to be scored for knowledge about HPV and its vaccine were 7 and 8, respectively, and the minimum was 0. Using Bloom’s cutoff points for the KAP study, a score of 50–100% of correct responses indicated good knowledge and poor knowledge for participants with a score less than 50% of correct.
The attitude toward HPV vaccinations was measured using 15 items. These items were assessed using a five-point Likert scale ranging from 1 “strongly disagree” to 5 “strongly agree.” The highest score was expected to be 75, and the lowest score was 15 for each participant. Those who scored above 50% had a positive attitude, and those who scored below 50% had a negative attitude toward HPV vaccinations.
HPV vaccinations were measured using three items. Each correct response was given a score of 1, and each incorrect response was scored 0. The highest and lowest scores were 3 and 0, respectively. Those who scored above 50% had good HPV vaccination practices, whereas those who scored below 50% had poor HPV vaccination practices.
Data quality assurance
The WHO guidelines were followed when adopting and validating the data collection format. Prior to data collection, informed consent was obtained, and the data collectors were trained on the goals and significance of the study. A pretest was conducted using 5% of the randomly selected samples to ensure data collection feasibility, language clarity, and response accuracy. The internal consistency and validity of the tools were also evaluated using Cronbach’s α, which was 0.84. This proved that the survey was credible and legitimate [10]. The Cronbach’s alpha value of 0.73 indicates an acceptable level of internal consistency. To ensure the completeness and consistency of the collected data, the researchers carried out on-site checks and reviews of all completed questionnaires.
Data processing and analysis
After coding, the data were entered into Epi-Data version 3.1 and then exported to SPSS version 25 for further analysis. Descriptive statistics were used to present mean scores and frequencies of sociodemographic profiles. The Variance Inflation Factor (VIF) was used to determine whether co-linearity existed between independent factors before performing multivariate binary logistic regression analysis. Chi-square statistics were used to check the adequacy of cells for binary logistic regression. Independent predictors of outcome and strength of association between dependent and independent variables were identified using binary logistic regression analysis, and P-values < 0.25 were entered into multiple regression analysis. A two-tailed test with P-values < 0.05 at a 95% confidence interval (Cl) and Adjusted odds ratio (AOR) with 95% CI were considered significant predictors. Finally, tables and charts were used for descriptive analysis.
Results
Sociodemographic characteristics of the participants
Of the 633 participants, 600 were included in this study, with a response rate of 94.8%. The mean age of the participants was 20.8 ± 0.75 (19-23) years. Of the study participants, 448 (74.7%) were aged 21–23 years. Most study participants, 482 (80.3%) were Orthodox religious followers (Table 1).
Table 1.
Sociodemographic characteristics of female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Age | 19–20 | 152 | 25.3 |
| 21–23 | 448 | 74.7 | |
| Mean ± SD | 20.8 ± 0.75 | ||
| Religion | Orthodox | 482 | 80.3 |
| Muslim | 37 | 6.2 | |
| Catholic | 21 | 3.5 | |
| Protestant | 60 | 10.0 | |
| Residence | Urban | 202 | 33.7 |
| Rural | 398 | 66.3 | |
| Department | Pharmacy | 120 | 20.0 |
| Nursing | 190 | 31.7 | |
| Midwifery | 160 | 26.7 | |
| Medical laboratory | 130 | 21.6 | |
| Undergraduate year | Year 1 | 180 | 30.0 |
| Year 2 | 140 | 23.3 | |
| Year 3 | 140 | 23.3 | |
| Year 4 | 100 | 16.7 | |
| Year 5 | 40 | 6.7 | |
| Total | 600 | 100 | |
Sources of HPV infection and vaccine information
All participants heard about HPV infections. However, 359 (59.8%) participants heard about the HPV vaccine (Table 2). The most common source of information about HPV infection and HPV vaccines was health professionals, 180 (30.0%), followed by mass media (radio, television, and newspaper),158 (26.3%) (Fig. 1).
Table 2.
Knowledge of HPV and its vaccination among female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
| Items in the Knowledge Questions | Category | Frequency | Percentage |
|---|---|---|---|
| Ever heard about HPV? | Yes | 600 | 100 |
| No | 0 | 0 | |
| Know the transmission of HPV infection | Yes | 504 | 84.0 |
| No | 96 | 16.0 | |
| Know the signs and symptoms of cervical cancer | Yes | 180 | 30.0 |
| No | 420 | 70.0 | |
| Know the risk factors for HPV | Yes | 498 | 83.0 |
| No | 102 | 17.0 | |
| Know about HPV-associated diseases | Yes | 461 | 76.8 |
| No | 139 | 23.2 | |
| Know the method of prevention of HPV infection | Yes | 560 | 93.3 |
| No | 40 | 6.7 | |
| Can HPV infection be treated? | Yes | 330 | 55.0 |
| No | 270 | 45.0 | |
| Ever heard about HPV vaccines in Ethiopia? | Yes | 359 | 59.8 |
| No | 241 | 40.2 | |
| Know the recipient of the HPV vaccine | Yes | 507 | 84.5 |
| No | 93 | 15.5 | |
| Can the HPV vaccine cause infertility? | Yes | 100 | 16.7 |
| No | 500 | 83.3 | |
| Does the HPV vaccine prevent cervical cancer? | Yes | 459 | 76.5 |
| No | 141 | 23.5 | |
| Is the HPV vaccine used to prevent genital warts? | Yes | 273 | 45.5 |
| No | 327 | 54.5 | |
| What age range is recommended for vaccination against HPV infection? | 10–14 years | 178 | 29.7 |
| I don’t know | 422 | 70.3 | |
| How many doses are recommended for an HPV vaccine? | Two doses | 138 | 23.0 |
| I don’t know | 462 | 77.0 | |
| Did you know the schedule for HPV vaccination? | 6 months–1 year | 152 | 25.3 |
| I don’t know | 448 | 74.7 |
Fig. 1.
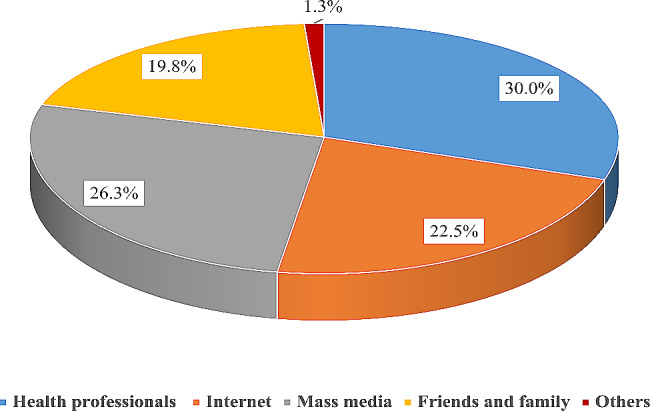
Source of HPV and HPV vaccine information for female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
Knowledge about HPV infection and vaccination
Overall, 436 (72.7%) of the participants had good knowledge about HPV infection, whereas 315 (52.5%) had good knowledge about HPV vaccination (Fig. 2). Among the participants, 504 (84.0%) and 560 (93.3%) knew the transmission and prevention methods of HPV infection, respectively, whereas 420 (70.0%) did not know the signs and symptoms of cervical cancer. More than half of the participants, 359 (59.8%), heard about HPV vaccination in Ethiopia; however, more than two-thirds of the participants, 422 (70.3%), 462 (77.0%), and 448 (74.7%) did not know the recommended age range, dose, and schedule for HPV vaccination, respectively (Table 2).
Fig. 2.
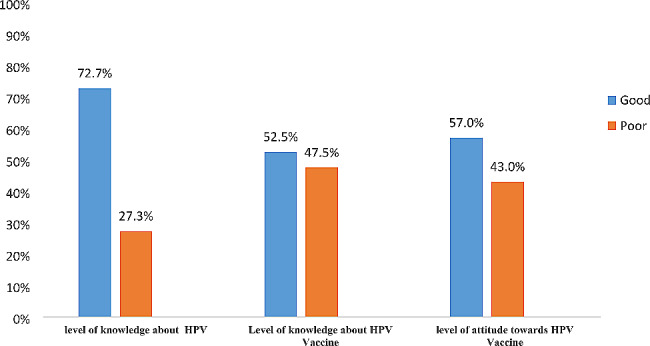
Level of knowledge and attitude toward HPV and its vaccine among female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
Attitude toward the HPV vaccine
More than half of the study participants, 342 (57%) had favorable attitudes toward HPV vaccine (Fig. 2). Most study participants, 547 (91.2%) agreed or strongly agreed that the HPV vaccine is effective in preventing cervical cancer. However, more than two-thirds of the study participants, 483 (80.5%), disagreed or strongly disagreed that they would not take the vaccine because they did not believe they were at risk of getting HPV infection, while 266 (44.3%) believed that the vaccine’s side effects were reasonable and would not prevent them from receiving the vaccine. More than half of the study participants, 338 (56.3%) agreed that the HPV vaccine may not have a long-term negative effect and 261 (43.5%) agreed that the vaccine is safe. Most participants agreed that the vaccine is more useful for women than men (Table 3).
Table 3.
Attitude toward HPV vaccination among female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
| Items in the Attitude Questions | SD | Disagree | Neutral | Agree | SA |
|---|---|---|---|---|---|
| HPV vaccine is effective in preventing cervical cancer | 0 | 0 | 53(8.8) | 284 (47.3) | 263 (43.8) |
| I will take the vaccine because I feel at risk of getting an HPV infection | 66 (11.0) | 417 (69.5) | 94 (15.7) | 23 (3.8) | 0 |
| A person who has only one sexual partner can be protected from HPV infection | 12 (2.0) | 86 (14.3) | 185 (30.8) | 317 (52.8) | 0 |
| It is not necessary to get human papillomavirus vaccination | 123 (20.5) | 183 (30.5) | 111 (18.5) | 183 (30.5) | 0 |
| I believe that the vaccine’s side effects are reasonable and will not prevent me from receiving the vaccine. | 18 (3.0) | 185 (30.8) | 131 (21.8) | 266 (44.3) | 0 |
| I feel that it is better to be vaccinated before becoming sexually active | 0 | 24 (4.0) | 264 (44.0) | 278 (46.3) | 34 (5.7) |
| More information on HPV and its vaccine will be required before I take the vaccine | 0 | 0 | 90 (15.0) | 331 (55.2) | 179 (29.8) |
| The human papillomavirus vaccine may have a long negative effect | 171 (28.5) | 167 (27.8) | 237 (39.5) | 25 (4.2) | 0 |
| I feel that only sexually active ladies should get the vaccine | 16 (2.7) | 360 (60.0) | 110 (18.3) | 114 (19.0) | 0 |
| Do you think your family is allowed to vaccinate? | 0 | 37 (6.2) | 235 (39.2) | 300 (50.0) | 28 (4.7) |
|
Education on the HPV vaccine should be implemented at College |
0 | 25 (4.2) | 77 (12.8) | 327 (54.5) | 171 (28.5) |
| HPV vaccination should be included in the National Program on Immunization | 0 | 13 (2.2) | 247 (41.2) | 340 (56.7) | 0 |
| The vaccine is safe | 0 | 41 (6.8) | 298 (49.7) | 134 (22.3) | 127 (21.2) |
| The vaccine is useful for men | 0 | 102 (17.0) | 223 (37.2) | 275 (45.8) | 0 |
| The vaccine is useful for women | 0 | 0 | 76 (12.7) | 269 (44.8) | 255 (42.5) |
SD: Strongly Disagree, SA: Strongly Agree
HPV vaccination practices
All study participants had never been tested for HPV, and more than two-thirds of the study participants, 471 (78.5%), were unwilling to undergo routine HPV testing by collecting samples by themselves (Table 4).
Table 4.
HPV vaccination practices among female health science students at UoG and BDU, Ethiopia, 2023 (n = 600)
| Items of Practice Questions | Category | Frequency | Percentage |
|---|---|---|---|
| Have you ever been tested for HPV? | Yes | 0 | 0 |
| No | 600 | 100 | |
| I am willing to undergo routine HPV testing if I can collect my samples | Yes | 129 | 21.5 |
| No | 471 | 78.5 | |
| I am willing to undergo routine HPV testing even if I am not allowed to collect my samples | Yes | 204 | 34.0 |
| No | 396 | 66.0 |
Factors associated with participants’ HPV vaccination knowledge
The age, residence, and attitude of female undergraduate health science students were associated with their knowledge of HPV vaccinations in binary logistic regression, with a p-value of < 0.25. However, after multiple logistic regression analysis, age (AOR, 2.12, 95%, CI = 1.22–3.09) and attitude (AOR:1.88; 95%, CI: 1.15–3.41) had a statistically significant association with their knowledge about HPV vaccination at p-value < 0.05 (Table 5).
Table 5.
Factors associated with female health science students’ knowledge about HPV vaccinations at UoG and BDU, Ethiopia, 2023 (n = 600)
| Factors | Category | COR (95% Cl) | AOR (95% Cl) | P value |
|---|---|---|---|---|
| Age |
19–20 21–23 |
1 2.24 (1.34–3.14)* |
2.12 (1.22–3.09)* | 0.04 |
| Residence |
Rural Urban |
1 2.28 (1.47–3.41)* |
2.08 (1.34–2.82) | 0.06 |
| HPV knowledge |
Poor knowledge Good knowledge |
1 2.93 (1.54–5.63)* |
1.12 (1.13–8.34) | 0.07 |
| Attitude toward HPV vaccinations |
Unfavorable Attitude Favorable Attitude |
1 1.67 (1.08–3.18) |
1.88 (1.15–3.41)* | 0.03 |
*Statistically significant at p < 0.05 with COR and AOR
Factors associated with participants’ attitudes toward HPV vaccinations
In the multivariate logistic regression, the study participant’s knowledge about HPV (AOR: 1.90; 95%, CI: 1.11–5.88) and HPV vaccinations (AOR: 1.60; 95%CI: 1.07–2.47) were significantly associated with their attitudes (Table 6).
Table 6.
Factors associated with the attitude of female health science students toward HPV vaccinations at UoG and BDU, Ethiopia, 2023 (n = 600)
| Factors | Category | COR (95% Cl) | AOR (95% Cl) | P value | |
|---|---|---|---|---|---|
| Age |
19–20 21–23 |
1 1.44 (1.01–2.03)* |
1.62 (1.13–2.41) | 0.07 | |
| Residence |
Rural Urban |
1 1.54 (1.1–2.2)* |
1.53 (1.0–2.1) | 0.09 | |
| HPV knowledge |
Poor knowledge Good knowledge |
1 3.21 (1.88–5.21) |
1.92 (1.11–5.88)* | 0.02 | |
| Knowledge about HPV vaccinations |
Poor knowledge Good knowledge |
1 1.83 (1.14–2.53)* |
1.60(1.07–2.47)* | 0.03 | |
*Statistically significant at p < 0.05 with COR and AOR
Factors associated with participants’ HPV vaccination practice
This study found that female undergraduate health science students’ knowledge about HPV (AOR: 1.18; 95%CI: 0.55–5.50), the HPV vaccine (AOR:1.85; 95%CI: 1.08–2.44), and attitudes toward HPV vaccinations (AOR: 1.85; 95%CI:1.15–3.45) were significantly associated with their HPV vaccination practices (Table 7).
Table 7.
Factors associated with the practice of female health science students regarding HPV vaccinations at UoG and BDU, Ethiopia, 2023 (n = 600)
| Factors | Category | COR (95% Cl) | AOR (95% Cl) | P value |
|---|---|---|---|---|
| Age |
19–20 21–23 |
1 1.74 (1.23–3.09)* |
1.63 (1.01–3.15) | 0.06 |
| Residence |
Rural Urban |
1 2.86 (1.41–4.45)* |
2.51 (1.28–4.92) | 0.40 |
| HPV knowledge |
Poor knowledge Good knowledge |
1 1.05(0.79–1.56) |
1.18(0.55–5.50)* | 0.02 |
| Knowledge about HPV vaccinations |
Poor knowledge Good knowledge |
1 1.54(1.21–1.96) |
1.85 (1.08–2.44)* | 0.03 |
| Attitude toward HPV vaccinations |
Unfavorable attitude Favorable attitude |
1 1.22(1.05–2.33) |
1.85(1.15–3.45)* | 0.04 |
*Statistically significant at p < 0.05 with COR and AOR
Discussion
Having good knowledge and a favorable attitude toward HPV and HPV vaccinations are the cornerstones for increasing the use of HPV vaccinations and preventing cervical cancer. This study revealed that the proportion of female undergraduate health sciences students’ knowledge about HPV and HPV vaccinations was 72.7% and 52.5%, respectively, indicating that the participants’ knowledge of HPV vaccinations was greater than their knowledge of HPV vaccinations. This finding was supported by studies conducted at different locations; Malaysia (50.8%) [11] and Jimma (52.7%) [12]. Moreover, the finding was relatively greater than other studies; Uganda (47.7%) [13], Indonesia (44.4%) [14], India (44%) [15], Nigeria (31.2%) [16], Ambo, Ethiopia (24.9%) [17], and South Africa (14.75%) [18], but lower than studies conducted in Romania (85.8%) [19], Ibadan (84%) [20], Thailand (60%) [21], Malaysia (60.9%) [22], Italy (56.3%) [23], UK (54.8%) [24], and other Ethiopian towns like Debre Tabor (59.2%) [25], Bahir Dar (58.1%) [26], Ambo (88.6%) [27], and Arba Minch (71.7%) [28]. This variation may be due to differences in the study setting, study population, study period, and source of information.
All participants heard about HPV infection; however, only 59.8% had heard about HPV vaccinations. This percentage was lower than studies in Debre Tabor, Ethiopia (68.9%) [25] and Italy (80.4%) [27]. In this study, students obtained information about HPV and its vaccine mainly from health professionals (30.0%), followed by mass media (radio, television, and newspaper) (26.3%) and the internet (25.5%). The findings were supported by studies conducted in Malaysia, Ibadan, Thailand, Nigeria, Morocco, and in Addis Ababa, Ethiopia [11, 16, 20, 21, 29, 30]. This indicates that health professionals can play an important role in providing adequate information regarding HPV and its vaccine to female undergraduate health sciences students. There was a minimal role for friends and family (19.8%) as sources of knowledge in this study. On the other hand, in the study conducted in Debre Tabor, Ethiopia [25], Indonesia [14], Nigeria [16], Turkey [31], and Hong Kong [32], the main sources of information for the students were the mass media (radio, television, and newspaper) and the Internet. The possible reasons for this difference could be differences in the study subjects, study locations, and study periods.
In this study, 83.0% of female undergraduate health science students were aware of HPV infection risk factors. The results were similar to those of studies conducted in India (85%) [33], but greater than the study conducted in Uganda (40%) [13]. Approximately 93.3% of the students were aware of cervical cancer prevention methods, which was supported by a study conducted in Addis Ababa, Ethiopia (93.5%) [30], and India (92.5%) [34]. This finding is larger than that of a study conducted in Nigeria (8%) [16], but less than that of a study conducted in Albania (100%) [35].
Approximately 57% of the female undergraduate health science students had a favorable attitude toward HPV vaccinations, whereas the remaining 43% had an unfavorable attitude toward HPV vaccinations, which is consistent with the findings of other studies conducted in Adama, Ethiopia (55.6%) [36], but greater than those studies in Albania (45.9%) [35] and in Jimma, Ethiopia (44.4%) [37]. More than two-thirds of the study participants (80.5%) disagreed or strongly disagreed that they would not take the vaccine because they did not believe they were at risk of HPV infection, while 33.8% believed that the vaccine’s side effects were reasonable and would not prevent them from receiving the vaccine. More than half of the study participants (56.3%) agreed that HPV vaccinations may not have a long-term negative effect, and most students agreed that the vaccinations were more useful to women than men (Table 3).
All female undergraduate health science students had never tested for HPV, and more than two-thirds of the students, 471(78.5%), did not have the willingness to undergo routine HPV testing by collecting samples themselves, which was supported by other studies conducted in Spain (71.5%) [38], Hong Kong (7%) [32], Nigeria (6%) [16], Uganda (19%) [13], and in Addis Ababa, Ethiopia (6.5%) [30]. The main reasons for not being screened were the absence of symptoms; being healthy, lack of awareness, fear of the procedure, and dislike of pelvic examination. The aforementioned reasons follow studies in Nigeria, Uganda, and Adama in Ethiopia [13, 16, 36].
After multiple logistic regression analysis, students who were aged between 21 and 23 were 2 (AOR, 2.12, 95%, CI = 1.22–3.09) times more knowledgeable about HPV vaccinations than students in 19–20 years because, as the age of the students increased, the chance of getting a source of information and hearing about HPV vaccinations increased. The likelihood of being knowledgeable about HPV vaccinations was 1.88 (AOR: 1.88; 95%, CI: 1.15–3.41) times more in students with a favorable attitude than in students with an unfavorable attitude. The participants’ knowledge of HPV and HPV vaccinations was significantly associated with their attitudes. Students who had good knowledge about HPV had a 1.92 (AOR: 1.92; 95%, CI: 1.11–5.88) times more positive attitude, whereas students with good knowledge about HPV vaccinations had a 1.6 (AOR: 1.60; 95%CI: 1.07– 2.47) times more positive attitude toward HPV vaccinations. This finding is consistent with other studies conducted in Ambo, Ethiopia [17]. The findings of this study are greater than those of other studies conducted in the Ethiopian towns; of Jimma, Arba Minch, and Bahir Dar [12, 26, 28]. This can be explained by the fact that individual barriers to HPV vaccination, such as fear of needle injection, side effects, and poor accessibility of information, can negatively affect attitudes toward HPV vaccination.
The study also identified factors associated with HPV vaccinations, female undergraduate health science students’ knowledge about HPV, HPV vaccinations, and their attitudes were significantly associated with HPV vaccination practice. Students who had good knowledge about HPV had 1.18 (AOR: 1.18; 95%CI: 0.55–5.50) times more HPV vaccination practice than students who had poor knowledge, whereas those who had good knowledge on HPV vaccination had 1.85 (AOR: 1.85; 95%CI: 1.08–2.44) times more HPV vaccination practice than those who had poor knowledge on HPV vaccination. Additionally, students who had a favorable attitude had 1.85 times more HPV vaccination practice than those who had an unfavorable attitude (AOR: 1.85; 95%CI: 1.15–3.45).
Strengths and limitations of the study
The results were more representative because of a large sample size and primary sources were used. The main limitation of this study is that it does not involve male students as study participants and relies mainly on a quantitative approach, not a qualitative approach.
Conclusion
This study revealed that half of the students had good knowledge and a favorable attitude toward HPV vaccinations, but they had poor HPV vaccination practices. The age and attitude of the students were associated with their knowledge. Having good knowledge about HPV and its vaccines was significantly associated with an attitude toward HPV vaccinations. HPV vaccination practice was significantly associated with knowledge and attitude toward HPV infection and its vaccines. To strengthen HPV vaccination practices, improve student attitudes and knowledge about the benefits of vaccination, and improve counseling abilities against HPV-induced cancer, health sectors and universities should provide health education, training, and counseling services to their students. Further research is required with large-scale study participants on this issue.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are grateful to both the University of Gondar and Bahir Dar University, College of Medicine and Health Sciences, for providing a written permission letter for conducting this study. We would also like to thank the study participants, supervisors, and data collectors for their active participation.
Author contributions
BAM and MCW were responsible for writing the research proposal, data collection supervision, data entry, analysis, and interpretation. YKA and BAK were responsible for data curation, validation, review, and editing. BAM was also responsible for manuscript writing, revision, and submission approval. All authors have read and approved the final manuscript.
Funding
This study did not receive any specific project funding.
Data availability
All data are included within the article.
Declarations
Ethics approval and consent to participate
A letter of ethical approval was obtained from the Research and Ethical Review Committee, School of Pharmacy, University of Gondar (SOP/247/2023). The participants were informed about the purpose of the study, and they provided verbal consent. The data collection was initiated after obtaining permission and provisions following relevant guidelines. The obtained data from the participants were strictly confidential.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Basri DF, Nor NH. Phytoconstituent screening and antibacterial activity of the leaf extracts from Canarium Odontophyllum Miq. Am J Plant Sci. 2014;5(19):2878–88. 10.4236/ajps.2014.519303 [DOI] [Google Scholar]
- 2.Dash BK, Faruquee HM, Biswas SK, Alam MK, Sisir SM, Prodhan UK. Antibacterial and antifungal activities of several extracts of Centella asiatica L. against some human pathogenic microbes. Life Sci Med Res. 2011;2011:1–5. [Google Scholar]
- 3.Kassa HN, Bilchut AH, Mekuria AD, Lewetie EM. Practice and associated factors of human papillomavirus vaccination among primary school students in Minjar-Shenkora district, North Shoa Zone, Amhara Regional State, Ethiopia, 2020. Cancer Manage Res. 2021:6999–7008. [DOI] [PMC free article] [PubMed]
- 4.Weaver BA. Epidemiology and natural history of genital human papillomavirus infection. J Osteopath Med. 2006;106(s1):2–8. [PubMed] [Google Scholar]
- 5.Trottier H, Franco EL. The epidemiology of genital human papillomavirus infection. Vaccine. 2006;24:S4–15. 10.1016/j.vaccine.2005.09.054 [DOI] [PubMed] [Google Scholar]
- 6.Alene T, Atnafu A, Mekonnen ZA, Minyihun A. Acceptance of human papillomavirus vaccination and associated factors among parents of daughters in Gondar town, Northwest Ethiopia. Cancer Manage Res. 2020:8519–26. [DOI] [PMC free article] [PubMed]
- 7.Piñeros M, Mery L, Soerjomataram I, Bray F, Steliarova-Foucher E. Scaling up the surveillance of childhood cancer: a global roadmap. JNCI: J Natl Cancer Inst. 2021;113(1):9–15. 10.1093/jnci/djaa069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO). Human papillomavirus (HPV) vaccination: from clinical studies to immunization programs. 2018;1317–26. [DOI] [PubMed]
- 9.Megersa BS, Bussmann H, Bärnighausen T, Muche AA, Alemu K, Deckert A. Community cervical cancer screening: barriers to successful home-based HPV self-sampling in Dabat district, North Gondar, Ethiopia. A qualitative study. PLoS ONE. 2020;15(12):e0243036. 10.1371/journal.pone.0243036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48:1273–96. 10.1007/s11165-016-9602-2 [DOI] [Google Scholar]
- 11.Jalani FF, Rani MD, Isahak I, Aris MS, Roslan N. Knowledge, attitude and practice of human papillomavirus (HPV) vaccination among secondary school students in rural areas of Negeri Sembilan, Malaysia. Int J Collaborative Res Intern Med Public Health. 2016;8(6):56. [Google Scholar]
- 12.Biyazin T, Yilma A, Yetwale A, Fenta B, Dagnaw Y. Knowledge and attitude about human papillomavirus vaccine among female high school students at Jimma town, Ethiopia. Hum Vaccines Immunotherapeutics. 2022;18(1):2036522. 10.1080/21645515.2022.2036522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nabirye J, Okwi LA, Nuwematsiko R, Kiwanuka G, Muneza F, Kamya C, Babirye JN. Health system factors influencing uptake of human papilloma virus (HPV) vaccine among adolescent girls 9–15 years in Mbale District, Uganda. BMC Public Health. 2020;20:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Endarti D, Kristina SA, Farida MA, Rahmawanti Y, Andriani T. Knowledge, perception, and acceptance of HPV vaccination and screening for cervical cancer among women in Yogyakarta Province, Indonesia. Asian Pac J cancer Prevention: APJCP. 2018;19(4):1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rashid S, Labani S, Das BC. Knowledge, awareness and attitude on HPV, HPV vaccine and cervical cancer among the college students in India. PLoS ONE. 2016;11(11):e0166713. 10.1371/journal.pone.0166713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Onowhakpor AO, Omuemu VO, Osagie OL, Odili CG. Human papilloma virus vaccination: knowledge, attitude and uptake among female medical and dental students in a tertiary institution in Benin-City. Nigeria J Community Med Prim Health Care. 2016;28(2):101–8. [Google Scholar]
- 17.Yohannes E, Beyen MW, Bulto GA, Chaka EE, Debelo BT, Erena MM, Tasu TL. Knowledge and attitude toward human papillomavirus vaccination and associated factors among adolescent school girls in Ambo town, Ethiopia, 2021: a multicenter cross-sectional study. Health Sci Rep. 2023;6(6):e1305. 10.1002/hsr2.1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eche MT, Vermaak K. Knowledge, attitude and practice of female university students regarding human papillomavirus and self-sampling in KwaZulu-Natal, South Africa: a cross-sectional survey. BMC Womens Health. 2022;22(1):58. 10.1186/s12905-022-01634-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voidăzan S, Tarcea M, Morariu SH, Grigore A, Dobreanu M. Human papillomavirus vaccine-knowledge and attitudes among parents of children aged 10–14 years: a cross-sectional study, Tîrgu mureş, Romania. Cent Eur J Public Health. 2016;24(1):29–38. 10.21101/cejph.a4287 [DOI] [PubMed] [Google Scholar]
- 20.Oluwasola TA, Bello OO, Odukogbe AA. Awareness and attitude of female undergraduates toward human papillomavirus vaccine in Ibadan. Trop J Obstet Gynecol. 2019;36(1):33–8. 10.4103/TJOG.TJOG_7_19 [DOI] [Google Scholar]
- 21.Songthap A, Pitisuttithum P, Kaewkungwal J, Fungladda W, Bussaratid V. Knowledge, attitudes, and acceptability of a human papilloma virus vaccine among students, parents and teachers in Thailand. Southeast Asian J Trop Med Public Health. 2012;43(2):340–53. [PubMed] [Google Scholar]
- 22.Badgujar VB, Ahmad Fadzil FS, Balbir Singh HK, Sami F, Badgujar S, Ansari MT. Knowledge, understanding, attitude, perception, and views on HPV infection and vaccination among health care students and professionals in Malaysia. Hum Vaccines Immunotherapeutics. 2019;15(1):156–62. 10.1080/21645515.2018.1518843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trucchi C, Amicizia D, Tafuri S, Sticchi L, Durando P, Costantino C, Varlese F, Di Silverio B, Bagnasco AM, Ansaldi F, Icardi G. Assessment of knowledge, attitudes, and propensity towards HPV vaccine of young adult students in Italy. Vaccines. 2020;8(1):74. 10.3390/vaccines8010074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sherman SM, Nailer E. Attitudes towards and knowledge about human papillomavirus (HPV) and the HPV vaccination in parents of teenage boys in the UK. PLoS ONE. 2018;13(4):e0195801. 10.1371/journal.pone.0195801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mihretie GN, Liyeh TM, Ayele AD, Belay HG, Yimer TS, Miskr AD, Kassa BG, Tefera AG, Dagnaw E, Belachew YY, Tiruneh GA. Female adolescents’ knowledge and acceptability of human papillomavirus vaccine in Debre Tabor Town, Ethiopia: a cross-sectional study. BMJ open. 2023;13(3):e061813. 10.1136/bmjopen-2022-061813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lakneh EA, Mersha EA, Asresie MB, Belay HG. Knowledge, attitude, and uptake of human papilloma virus vaccine and associated factors among female preparatory school students in Bahir Dar City, Amhara Region, Ethiopia. PLoS ONE. 2022;17(11):e0276465. 10.1371/journal.pone.0276465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Addisu D, Gebeyehu NA, Belachew YY. Knowledge, attitude, and uptake of human papillomavirus vaccine among adolescent schoolgirls in Ethiopia: a systematic review and meta-analysis. BMC Womens Health. 2023;23(1):279. 10.1186/s12905-023-02412-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ukumo EY, Woldehawariat FG, Dessalegn SA, Minamo DM, Ukke GG. Assessment of knowledge about human papillomavirus vaccination among primary school girls in Arba Minch Town, South Ethiopia, 2020 an institution-based cross-sectional study. Cancer Manage Res. 2022:2205–14. [DOI] [PMC free article] [PubMed]
- 29.Yacouti A, Elkhoudri N, El Got A, Benider A, Hadrya F, Baddou R, Forster A, Mouallif M. Awareness, attitudes and acceptability of the HPV vaccine among female university students in Morocco. PLoS ONE. 2022;17(4):e0266081. 10.1371/journal.pone.0266081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Assefa R. Girl’s Preference for Human Papilloma Virus Vaccination in Secondary Schools in Addis Ababa, Ethiopia. Discret Choice Exp. 2017;2017.
- 31.Akpinar CV, Tosun SA. Knowledge and perceptions regarding human papillomavirus (HPV) and willingness to receive HPV vaccination among university students in a north-eastern city in Turkey. BMC Womens Health. 2023;23. [DOI] [PMC free article] [PubMed]
- 32.Leung JT, Law CK. Revisiting knowledge, attitudes and practice (KAP) on human papillomavirus (HPV) vaccination among female university students in Hong Kong. Hum Vaccines Immunotherapeutics. 2018;14(4):924–30. 10.1080/21645515.2017.1415685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sudharshini S, Anantharaman V, Chitra A. A cross-sectional study on knowledge, attitude, and practice on cervical cancer and screening among female health care providers of Chennai corporation, 2013. J Acad Med Sci. 2012;2(4):124. 10.4103/2249-4855.141132 [DOI] [Google Scholar]
- 34.Swarnapriya K, Kavitha D, Reddy GM. Knowledge, attitude and practices regarding HPV vaccination among medical and para medical in students, India a cross sectional study. Asian Pac J Cancer Prev. 2015;16(18):8473–7. 10.7314/APJCP.2015.16.18.8473 [DOI] [PubMed] [Google Scholar]
- 35.Merkuri L, Kamberi F, Qorri E, Shapo L. Assessment of the Albanian University female students’ knowledge, attitudes, and practices on cervical cancer. J Infect Developing Ctries. 2023;17(4):534–41. 10.3855/jidc.18121 [DOI] [PubMed] [Google Scholar]
- 36.Tadesse A, Tafa Segni M, Demissie HF. Knowledge, attitude, and practice (KAP) toward cervical cancer screening among Adama Science and Technology University female students, Ethiopia. Int J Breast Cancer. 2022;2022(1):2490327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dera M, Wondimagegnehu A, Asfaw ZG. Determinants for hesitancy in human papillomavirus (HPV) vaccine uptake among school girls in Jimma Town, Ethiopia. A mixed approach: quantitative and qualitative. Reproductive Health. 2023;20(1):175. 10.1186/s12978-023-01711-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Navarro-Illana P, Diez-Domingo J, Navarro-Illana E, Tuells J, Alemán S, Puig-Barberá J. Knowledge and attitudes of Spanish adolescent girls towards human papillomavirus infection: where to intervene to improve vaccination coverage. BMC Public Health. 2014;14:1–8. 10.1186/1471-2458-14-490 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are included within the article.


