Abstract
Background
Prostate cancer in younger men is rare but not exceptional. Radiotherapy is a cornerstone of prostate cancer treatment and yet, its impact on fertility is scarcely reported in literature. Given the radiosensitivity of testicular tissue, this study aimed to determine the testicular dose using modern radiotherapy techniques for definitive prostate irradiation.
Methods
One hundred radiotherapy plans were reviewed. Testicles were contoured retrospectively without dosimetric optimization on testicles.
Results
The median testicular dose was 0.58 Gy: 0.18 Gy in stereotactic plans, 0.62 Gy in Volumetric Modulated Arc Therapy plans and 1.50 Gy in Tomotherapy plans (p < 0.001). Pelvic nodal irradiation increased the median testicular dose to 1.18 Gy versus 0.26 Gy without nodal irradiation (p < 0.001). Weight and BMI were inversely associated with testicular dose (p < 0.005). 65% of patients reached the theoretical dose threshold for transient azoospermia, and 10% received more than 2 Gy, likely causing definitive azoospermia.
Conclusion
Despite being probably lower than doses from older techniques, the testicular dose delivered with modern prostate radiotherapy is not negligible and is often underestimated because the contribution of daily repositioning imaging is not taken into account and most Treatment Planning Systems underestimate the out of field dose. Radiation oncologists should consider the impact on fertility and gonadal endocrine function, counseling men on sperm preservation if they wish to maintain fertility.
Trial registration: retrospectively registered.
Keywords: Fertility, Prostate cancer, Radiotherapy, Testicles, Dose
Background
Prostate cancer is the most common cancer among men globally, with over 1.4 million cases annually, including 415,000 cases in men under 64 years old (Globocan 2020 data) [1]. Fertility issues post-oncologic treatment are frequently addressed in pediatric or gynecological cancers treatments but are often overlooked in prostate neoplasms due to the older age of typical patients [2]. However, younger men are increasingly being diagnosed due to prostate-specific antigen screening, coupled with a societal trend of fathering children later in life [3–7]. Testicular tissue is highly radiosensitive, with doses as low as 0.15–0.3 Gy impacting function [8, 9].
Modern prostate radiotherapy includes dose escalation (above 74 Gy) and intensity modulated techniques (IMRT), which scatter low doses potentially affecting nearby radiosensitive tissues like the testicles. On-board imaging required for these techniques further contributes to dose exposure.
To our knowledge, no studies have reported on testicular dose from modern prostate radiotherapy techniques. This study aimed to report testicular doses from modern prostate irradiation and to assess the need for patient counseling regarding fertility preservation.
Methods
We reviewed one hundred radiotherapy plans of patients treated for the first time for a prostate cancer with curative intent, with an Equivalent Dose in 2 Gy fractions (EQD2) ≥ 74 Gy, between 2018 and 2020. All localized prostate cancer cases treated with EBRT in our department were included consecutively, irrespective of age, in order to have a sufficient sample of patients. We made the assumption that the genital anatomy of a 40–50 year-old man is superimposable on that of the older men in our cohort, and that the dosimetric results would therefore be comparable to younger men. The aim here was a dosimetric study to provide a proof of concept. The patients were not provided fertility counseling based on collected data.
For normofractionated treatments, prostate and pelvic nodes (when indicated) were contoured per international recommendations, in particular European SocieTy for Radiotherapy and Oncology (ESTRO) and Radiation Therapy Oncology Group (RTOG) guidelines [10, 11]. The pelvis, when treated, received 50 Gy with a 7 mm isotropic margin around the nodal Clinical Target Volume (CTV) to define nodal Planning Target Volume (PTV). A 5 mm isotropic margin around the prostate was used to define the high dose PTV, prescribed 74 to 80 Gy. For stereotactic radiotherapy, 40 Gy were prescribed in 5 fractions, pelvic nodes were never treated and PTV consisted in the prostate with an isotropic margin of 4 mm [12, 13]. At our institution, for prostate radiotherapy, Volumetric Modulated Arc-Therapy (VMAT) normofractionated plans were treated on a VersaHD ® (Elekta). Normofractionated tomotherapy plans were treated with a Tomotherapy ® (Accuray) using the TomoEdge™ technology from December 2018. Hypofractionated plans (stereotactic) were treated on Novalis Tx ™ (Varian Medical Systems and BrainLab) using only coplanar beams and a VMAT technique, with at least three gold fiducials and the ExacTrac system (Brainlab) for daily repositioning.
Testicles were contoured a posteriori and dose was estimated with a collapsed cone algorithm, on the Raystation (Raysearch Laboratories) treatment planning system (TPS) for VMAT and hypofractionated plans and on TomoTherapy or Precision TPS for tomotherapy plans. The plans were optimized neither a priori nor a posteriori to protect testicles. Average dose, D50 (dose received by half of the testicular volume) and D1% (minimum dose received by the most exposed 1% of testicular volume, which is an estimated of the maximum testicular dose) were recorded. Factors that may potentially influence the dose received to the testicles were also recorded, such as Body Mass Index (BMI), prescribed dose, age or pelvic nodes irradiation. Clinical data collection was based on medical consultations, histological and radiological reports. Biologically Equivalent Dose (BED) and EQD2 calculations were made according to formulas published by Vienna university [14], using a linear-quadratic model with an α/β = 1.5 Gy for prostate [15–17].
Ethics
This retrospective study was institutional review-board–approved and complied with the MR-004 French Reference Methodology according to 2016-41 law. A specific information note was sent to patients.
Statistical analysis
Analyzes were performed using GraphPad Prism software version 8.4.2 and R statistical software version 3.5.2. Categorical variables were compared using Fisher’s exact test and continuous variables were compared using Mann–Whitney or Student’s t test. The association with mean testicular dose was assessed using an ANOVA multiple comparisons test for categorical variables and Pearson correlation test for continuous ones. Statistical significance was defined as a p value < 0.05. Multivariate regression models included significant prognostic factors from univariate analysis.
The present study was conducted in accordance with the ethical principles of the Declaration of Helsinki and did not require further ethics committee approval.
Results
A total of 100 patients were included. Patients’ characteristics and technical data are reported in Table 1. Fifty-four patients were treated with a normofractionated VMAT technique, twenty were treated with a normofractionated tomotherapy technique and twenty-six plans were extremely fractionated “stereotactic” radiotherapy. The average testicular dose ranged from 0.01 to 7.85 Gy (median = 0.58 Gy). Testicle D50 ranged from 0.01 to 2.61 Gy (median = 0.54 Gy). Testicle D1% ranged from 0.08 to 20.4 Gy (median = 1.27 Gy).
Table 1.
Patients’ characteristics and technical data
| Median [IQR] | N | |
|---|---|---|
| Age | 74 [70–77] | 100 |
| Weight (kg) | 78 [70–88.5] | 60 |
| BMI (kg/m2) | 25.5 [23–28.8] | 56 |
| Technique (n (%)) | 100 | |
| VMAT | 54 | |
| Tomotherapy | 20 | |
| Stereotactic radiotherapy | 26 | |
| Total physical dose to prostate (Gy) | 78 [40–80] | 100 |
| Number of fractions | 39 [5-39] | 100 |
| EQD21.5 to prostate (Gy) | 80 [78–108.6] | 100 |
| Pelvic nodes irradiation | 100 | |
| Yes | 54 | |
| No | 46 | |
| Testicular volume (cc) | 54.8 [43–70] | 100 |
| Distance between inferior contour of CTV and testicle (mm) | 51 [41–60] | 100 |
IQR interquartile range, BMI body mass index, VMAT volumetric modulated arc-therapy, EQD21.5 equivalent dose in 2Gy fractions considering an α/β ratio of 1.5Gy, CTV clinical target volume
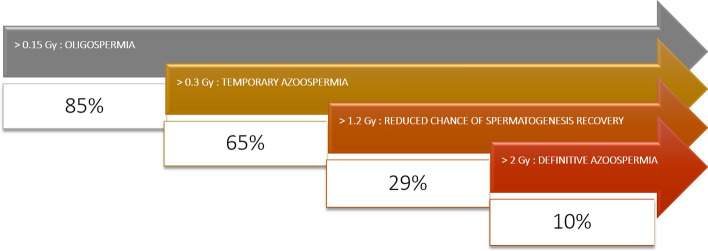
84% of patients had an average testicular dose above 0.15 Gy, and 65% exceeded 0.3 Gy. 29% received an average dose above 1.2 Gy, and 10% exceeded 2 Gy.
Factors significantly associated with an increased dose to the testicles are reported in Table 2 and Fig. 1. Median distance between the inferior border of the prostate and the upper border of the testicle, measured in a median sagittal plane was 51 mm with large variability between patients. This variability explains for a large part the testicular dose (Fig. 2).
Table 2.
Factors associated with testicular dose in univariate and multivariate analyses
| Continuous variables | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Coefficient [CI 95%] | p value | Coefficient [CI 95%] | p value | |
| Age | − 0.12 [− 0.31; 0.08] | 0.2 | ||
| Weight (kg) | − 0.45 [− 0.63; − 0.22] | < 0.001 | 0.002 [− 0.02; 0.02] | 0.915 |
| BMI (kg/m2) | − 0.37 [− 0.58; − 0.12] | 0.004 | − 0.04 [− 0.10; 0.02] | 0.213 |
| Physical dose to prostate (Gy) | − 0.40 [− 0.53; − 0.19] | < 0.001 | − 0.01 [− 0.07; 0.06] | 0.857 |
| Testicular volume (cc) | − 0.08 [− 0.27; 0.12] | 0.4 | ||
| Distance between inferior contour of CTV and testicle (mm) | − 0.62 [− 0.73; − 0.49] | < 0.001 | − 0.02 [− 0.02; − 0.01] | < 0.001 |
| Categorical variables | Mean physical dose to testicles (Gy) [CI 95%] | p value | OR [CI 95%] | p value |
|---|---|---|---|---|
| Technique | < 0.001 | 0.017 | ||
| Stereotactic radiotherapy (ref) | 0.18 [0.13; 0.23] | Ref | ||
| VMAT | 0.96 [0.64; 1.29] | 0.18 [− 1.87; 2.24] | ||
| Tomotherapy | 1.67 [1.24; 2.09] | 0.65 [− 1.46; 2.76] | ||
| Pelvic nodes irradiation | < 0.001 | 0.003 | ||
| No (ref) | 0.58 [0.27; 0.89] | Ref | ||
| Yes | 1.27 [1.01; 1.54] | 0.49 [0.18; 0.79] |
Bold indicates p value < 0.05 considered significant
CTV clinical target volume, VMAT volumetric modulated arc-therapy
Fig. 1.
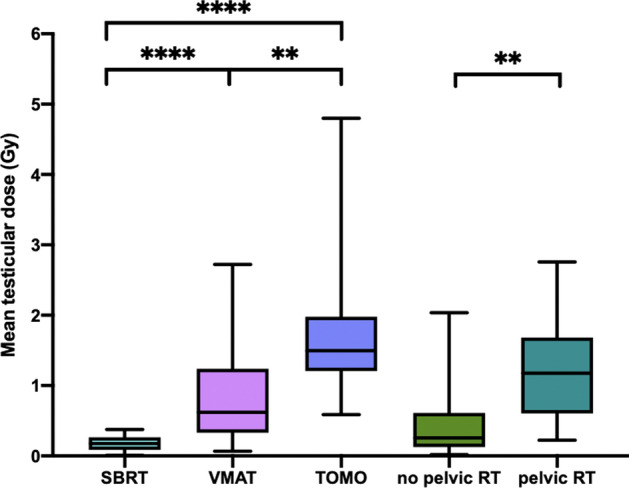
Technique and pelvic radiotherapy are associated with testicular dose. **p value < 0.01 and ****p value < 0.0001
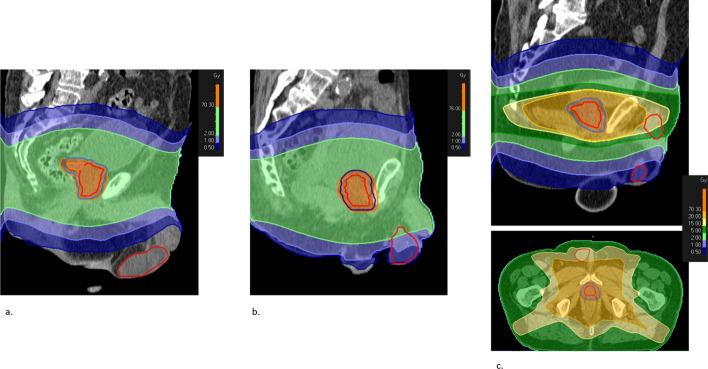
Fig. 2.
differences in anatomy explain the large variability of testicular dose: illustration with three sole-prostate Volumetric Modulated Arc-Therapy (VMAT) plans (no pelvic node irradiation). a Normal anatomy, testicle relatively low. Distance testicle – prostate 80 mm. Testicular dose: 0.06 Gy. b Normal anatomy, testicle relatively high. Distance testicle – prostate 18 mm. Testicular dose: 1.88 Gy. c Testicle inside the inguinal canal, that receives high dose from prostate irradiation (average testicular dose 7.85 Gy, max dose over 20 Gy)
Pelvic nodal irradiation significantly increased testicular dose (median 1.18 Gy vs. 0.26 Gy, p < 0.001). One patient with positive inguinal nodes required nodal external beam radiotherapy (EBRT) boost up to 60 Gy and in consequence an increased testicular dose, with an average dose of 2.04 Gy.
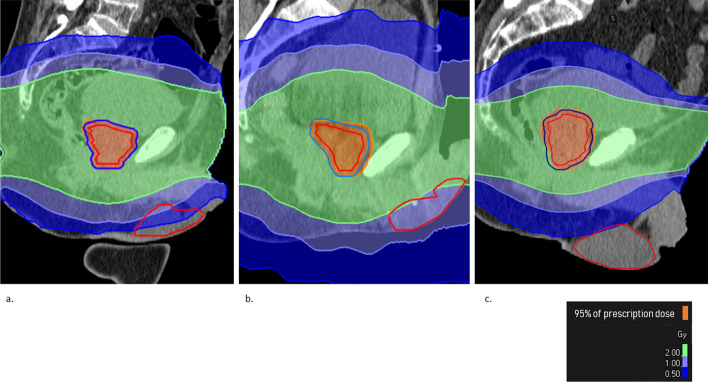
Median testicular dose in stereotactic radiotherapy plans was 0.18 Gy versus 0.62 Gy in VMAT plans and 1.50 Gy in tomotherapy plans (p < 0.001) (Fig. 1). One can notice on Fig. 3 the differences in dose repartition depending on radiotherapy techniques. Tomotherapy has a tendency to deliver low doses away from the target volume while stereotactic radiotherapy has a narrow dose gradient that explains the significantly lower dose delivered to testicles.
Fig. 3.
Testicular dose distribution depending on radiotherapy technique: illustration in 3 plans without pelvic irradiation. a Volumetric Modulated Arc-Therapy (VMAT). b Tomotherapy. c Stereotactic radiotherapy
Weight and Body Mass Index (BMI) were inversely correlated with testicular dose (p < 0.005) but not age (p = 0.2) on univariate analysis.
On multivariate analysis, radiotherapy technique, pelvic irradiation and the distance between the inferior border of the CTV and the testicles remained significantly associated with testicular dose (p < 0.001, 0.003 and < 0.001 respectively) (Table 2).
Discussion
Our study showed that testicular dose delivered by modern radiotherapy techniques during a standard prostate irradiation is not negligible, with a median dose of 0.58 Gy. Tomotherapy, pelvic nodal irradiation and lower BMI were significantly associated with increased median testicular dose.
Testis is one of the most radiosensitive tissues in humans and especially spermatogonia stem cells. Numerous studies have reported the impact on sperm count of incidental irradiation for testicular seminoma, Hodgkin disease, thyroid cancer (131I ablation) or rectal cancer. Doses as low as 0.15 Gy have been described to produce reduction in sperm count and temporary azoospermia occurs for doses over 0.3 Gy [8, 9]. The doses of irradiation required to kill spermocytes and spermatids are higher than spermatogonia (2–3 Gy and 4–6 Gy respectively). After low dose testis irradiation, spermatogonia, spermatocytes, and, ultimately, spermatids disappear from the testis. Since the combined life span of spermatocytes and spermatids is about 46 days and transport through the epididymis and vas deferens takes 4–12 days, sperm production is maintained during the first 50–60 days and then drops dramatically with resultant temporary oligo- or azoospermia [18, 19]. The nadir of sperm count occurs 4–6 months after the end of treatment, and complete recovery requires 10–18 months after less than 1 Gy, 30 months for 2–3 Gy, and 5–10 or more years after 4–6 Gy since germinal epithelium seems to been damaged at this dose range [9, 18, 20–22]. Doses above 1.2 Gy have been associated with a reduced risk of recovery of spermatogenesis [23]. Cumulative doses of fractionated radiotherapy more than 2–2.5 Gy generally result in prolonged and likely permanent azoospermia [9, 24–26].
Our cohort indicated that many patients could face fertility impairment post-EBRT, despite using modern techniques. Notably, 84% of patients reached the oligospermia theoretical dose threshold, and 65% reached the azoospermia dose threshold. 29% received an average testicular dose above 1.2 Gy (dose associated with reduced chance of spermatogenesis recovery in literature) and 10% exceeded 2 Gy (associated with a risk ofpermanent azoospermia) (Fig. 4).
Fig. 4.
proportion of patients in the cohort meeting the testicular dose threshold for oligospermia, temporary azoospermia, and definitive azoospermia with a modern prostate cancer radiotherapy plan
Beyond the impact on spermatozoid production, some studies reported a long-term impact of prostate cancer EBRT on hormone levels [27–29]. Leydig cells are reputed less radiosensitive then spermatogonial stem cells but negative effects have been reported after 2 Gy [9, 23, 30]. In a study on 33 men, serologic evaluation for hypogonadism was undertaken three to eight years after primary EBRT treatment for localized prostate carcinoma and was compared with 55 similar men who had received radical prostatectomy (none had undergone hormonal treatment since primary therapy). In the EBRT group, total testosterone levels averaged 27.3% less, luteinizing hormone (LH) levels 52.7% greater, and follicle-stimulating hormone (FSH) levels 100% greater [28]. However, in Tomić, Grigsby and Daniell studies [27–29], radiation technique were ancient and estimated dose to testicle was high (from 1 to 10 Gy for instance in Tomić’s study) so one can suppose that the hormonal impact of modern radiotherapy may be lower. So far, there is no evidence about the precise dose range in which hormonal impairment remains as a permanent side effect of irradiation [30].
Our study is, to the best of our knowledge, the only one reporting testicular dose with modern radiotherapy techniques. One can see that the dose reported in our study seems lower than what used to be delivered with 2D or 3D techniques. For instance, a prediction of a four-field treatment 3D radiotherapy on an anthropomorphic phantom in 17 patients indicates that testicular doses may be estimated with 1–2% of the tumor dose (range 0.4–2.2%), being about 1 Gy for a 80 Gy prescription [31]. In Boehmer et al.’s study, the calculated projected doses received by the unshielded testicles during a course of 20-MV conventional external-beam radiotherapy on a standard series of 40 fractions of external-beam radiotherapy for patients with localized prostate cancer were 1.96 Gy (± 1.45 Gy) [30]. Indeed, during the 2D/3D era, the clinical volumes were larger than what we can define nowadays with prostate magnetic resonance imaging (MRI) and the setup margins were also larger because of greater repositioning uncertainties with 2D imaging compared with Cone Beam Computed Tomography (CBCT).
Although it has not been proven in humans, some studies showed in animals that fractionated irradiation of the testes is more harmful than single treatments, at least up to total doses of about 6 Gy [20, 24]. Extremely hypofractioned treatments such as the ones allowed by stereotactic radiotherapy may reduce the fertility impact, all the more since their steep dose gradient deliver significantly lower dose to testicles compared with VMAT and Tomotherapy (median 0.18 Gy in our study). However, one should be careful when using stereotactic radiotherapy with non-coplanar beams such as Cyberknife for instance, since the entrance of the beams can be directly through the testicles and the radiation oncologist should take this in consideration when checking dosimetry. Moreover, our study showed that tomotherapy should be avoided in younger prostate cancer patients with a parenthood desire, since one fourth of the patients in our cohort received more than 2 Gy in average to testicles with this technique, despite the use of TomoEdge. The TomoEdge technology enables the superior and inferior jaw to open and close independently at the start and end of a target in order to reduce the longitudinal penumbra [32]. Without this feature, the dose to testicles might be far greater. Certainly, the radiation dose may be even more reduced by using even more advanced radiotherapy techniques such as proton therapy. Indeed, in one study on 16 men with low- or intermediate-risk prostate cancer treated with proton therapy, only one was found to have oligospermia indicating minimal scatter radiation to the testis during treatment. There was however a statistically significant reduction in semen volume and increase in pH [33].
Moreover, lead shields are not routinely used in prostate radiotherapy and yet they have been proven to reduce testicular dose in 3D techniques [27]. The gonadal shield allows a two to tenfold reduction in dose to the testes depending primarily on the distance from the field edge to the gonads [34]. In a study reporting the testicular dose using in vivo measurements in 16 men with testicular seminoma receiving abdominopelvic radiation therapy (modified dog-leg field) with anteroposterior/posteroanterior parallel-opposed photon beams with and without gonadal shielding, the mean measured dose to the testis in the patients with gonadal shielding was 0.03 Gy compared with 0.3 Gy in the unshielded group for a 25 Gy treatment [35]. However, testicular dose results from both leakage from the primary source as well as internal scatter and testicular shielding reduces only the dose from the primary source but not the internal scatter part.
The best technique to reduce testicular dose in a radical primary treatment for localized prostate cancer remains surely brachytherapy given its incomparable dose gradient. In a study following four young prostate cancer patients after brachytherapy with a total estimated dose to testis of 0.2 Gy, no significant change in semen parameters were found post-therapy and three of them were able to father a child subsequently without any deleterious side‐effects [36]. Huyghe’s team has one of the most important experiences in fertility after prostate brachytherapy. Among the 122 men under 65 years old treated by brachytherapy, four men manifested a fatherhood desire. One year after brachytherapy, their spermogram showed a low ejaculatory volume and a moderate asthenospermia but had a rich sperm count, compatible with a spontaneous pregnancy [37]. However, due to the prolonged half-life of the isotopes used, attempts at conception have to be delayed for up to 3 to 12 months after treatment [36, 38].
The issue of fertility preservation in prostate cancer patients is sometimes overlooked because of misconceptions from medical staff of a “limit” age to be a father. However, in a survey in 115 men treated for prostate cancer, all patients stated that they were informed of the incontinence and impotence side effects of the treatments, but only 8.7% stated that they were informed of the effect on their future fertility while 3.7% listed fertility as their major concern [39].
As reminded in the recent European Society for Medical Oncology (ESMO) recommendations on fertility preservation, sperm cryopreservation before initiation of anticancer treatments (chemotherapy, radiotherapy or surgery) is standard of care and should be discussed with any male cancer patient at risk of infertility [40]. If azoospermia is discovered after radiation therapy in a patient that has a paternity desire, the only possibility to harvest spermatozoa is through in invasive procedure (deferential, epididymal or testicular sperm extraction) and IntraCytoplasmic Sperm Injection (ICSI) [9, 41]. Pretreatment semen cryopreservation is safer, cheaper and generally results in more sperm for future use than postoperative surgical retrieval. Moreover, our results showed that patients requiting pelvic irradiation were the ones receiving the highest dose to testicles and those patients usually requires hormone deprivation therapy, from 6 months up to 3 years, with a testosterone recuperation that may take months or even years [42]. This will likely push these patients into an age range where testis recovery is rather moot and spermatogenesis naturally declines after 40 years old [43]. Ideally, the situation should be anticipated and discussed before any specific treatment, to favor pretreatment semen cryopreservation. An appropriate pre-treatment counseling in a center specialized in fertility issues is advisable.
The limitations of our study are of course its retrospective nature, its relatively low numbers and the lack of correlation with post-treatment fertility data such as hormonal and semen analyses or ulterior successful pregnancies. However, given the relatively low incidence of cancer prostate in young patients in each radiotherapy center, the feasibility of such a prospective study with sperm counts is unrealistic. The mean age of the patients included in this dosimetric study was also much higher than patients usually concerned with fertility issues but there is no reason why the dose to testicles would be different. Indeed, the dose to the testicles in our study was not significantly associated with age. The radiation doses threshold data and their semenanalysis outcomes used in this study were primarily in younger patients. It is not known if radiation therapy is more or less of a risk to the younger, developing testis or the older testis. Furthermore, emerging data suggests that spermatogenesis declines slowly after age 40 [43], so it is unclear if at these advanced paternal ages radiotherapy really will impact the testis that may have already declined.
Neither of the plans was optimized to deliver the lowest dose possible to testicle since it is not performed in routine care. Yet, modern radiotherapy techniques allow for inverse planning and optimization, providing the organ at risk is contoured and a constraint is set on it. However, clinically meaningful doses to testicles being very low, it is probable that a mere optimization won’t decrease testicular dose in a significant way. Also, modern commercial TPS allow for a testicular dose estimation although they tend to underestimate the out-of-field dose, up to 60% in mean dose to organs located beyond the 2% isodose [44–47]. A Monte Carlo simulation or direct measurements are precise but are so time-consuming that they are impractical for routine clinical use [44]. Modern radiotherapy also includes Image Guided RadioTherapy (IGRT). The dose delivered with imaging has historically been discarded because of its negligible contribution compared with therapeutic dose, in the era of 2D imaging. However, modern prostate radiotherapy requires a simulation CT scan for dosimetry and usually a CBCT at each fraction for an accurate repositioning since it was proven to improve outcomes in prostate cancer [48]. The limit of our study is that the dose delivered by daily positioning images was not recorded, and yet it is not negligible with daily CBCTs, especially when considering organs with very low dose tolerance [49]: about 0.8 Gy to testicles for 40 fractions for a pelvic treatment [50] and the typical imaging dose is approximately 1.5 cGy per image in Tomotherapy (0.6 Gy for a whole 40-fractions treatment considering one CBCT per fraction) [51]. A solution could be to reduce CBCT frequency, notably with moderate or ultra-hypofractionation. MR-guided radiotherapy is also a way to avoid the low doses delivered with repositioning imaging. The variability of techniques, equipment and field sizes used in our study also introduce a degree of heterogeneity in the cohort that cannot be accounted for. The latter limitations show that the testicular dose we estimated in our cohort and more generally in clinical practice is underestimated and the rate of clinically meaningful impact on fertility is probably higher than we could expect.
Our study shows that even with modern techniques, the dose delivered to testicles during a prostate radiotherapy is far from negligible, especially when pelvic nodes are treated or when a Tomotherapy technique is used. This dose could probably be reduced with optimized patient positioning to increase the distance between testicles and radiotherapy fields. Above all, SBRT and brachytherapy should be favored in younger patients in this consideration when suitable. Patients are often ill-informed and yet concerned with the potential impacts that the cancer treatments may have on their fertility. Given the difficulties that one can foresee to retrieve spermatozoa after a prostate radiotherapy, the ideal situation is to offer fertility counseling and sperm cryopreservation before any treatment to the fraction of patients who may still have a paternity desire.
Acknowledgements
Not applicable.
Abbreviations
- IMRT
Intensity modulated radiotherapy
- EQD2
Equivalent dose in 2 Gy fractions
- ESTRO
European society for radiotherapy and oncology
- RTOG
Radiation therapy oncology group
- CTV
Clinical target volume
- PTV
Planning target volume
- VMAT
Volumetric modulated arc-therapy
- TPS
Treatment planning system
- D50
Dose received by half of the volume
- D1%
Minimum dose received by the most exposed 1% of the volume
- BMI
Body mass index
- BED
Biologically equivalent dose
- IQR
Interquartile range
- EBRT
External beam radiotherapy
- LH
Luteinizing hormone
- CBCT
Cone beam computed tomography
- ESMO
European society for medical oncology
- ICSI
Intracytoplasmic sperm injection
- IGRT
Image guided radiotherapy
- MRI
Magnetic resonance imaging
Author contributions
MK: conception; design of the work; acquisition and interpretation of data; drafted the work. MT, NG and PB: design of the work; analysis of the data; substantively revised the manuscript. AA, MC, JV: acquisition of data; substantively revised the manuscript. PB; PM; AB: substantively revised the manuscript; supervision. All authors read and approved the final manuscript.
Funding
This study received neither grant nor funding.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This retrospective study was institutional review-board–approved and complied with the MR-004 French Reference Methodology according to 2016-41 law. A specific information note was sent to patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Le Guevelou J, Zilli T. Prostate cancer radiotherapy and incidental testicular irradiation: Impact on gonadal function. Clin Transl Radiat Oncol. 2023;40:100611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobsen SJ, Katusic SK, Bergstralh EJ, Oesterling JE, Ohrt D, Klee GG, et al. Incidence of prostate cancer diagnosis in the eras before and after serum prostate-specific antigen testing. JAMA. 1995;274(18):1445–9. 10.1001/jama.1995.03530180039027 [DOI] [PubMed] [Google Scholar]
- 4.Hamilton BE. Births: Provisional Data for 2022. 2021;
- 5.Laopaiboon M, Lumbiganon P, Intarut N, Mori R, Ganchimeg T, Vogel JP, et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG Int J Obstet Gynaecol. 2014;121(Suppl 1):49–56. 10.1111/1471-0528.12659 [DOI] [PubMed] [Google Scholar]
- 6.Mathews TJ, Hamilton BE. Mean age of mother, 1970–2000. Natl Vital Stat Rep Cent Dis Control Prev Natl Cent Health Stat Natl Vital Stat Syst. 2002;51(1):1–13. [PubMed] [Google Scholar]
- 7.Osterman M, Hamilton B, Martin J, Driscoll A, Valenzuela C. Births: Final Data for 2020. National Center for Health Statistics (U.S.); 2021 Feb [cited 2023 Mar 26]. Available from: https://stacks.cdc.gov/view/cdc/112078 [PubMed]
- 8.Rowley MJ, Leach DR, Warner GA, Heller CG. Effect of graded doses of ionizing radiation on the human testis. Radiat Res. 1974;59(3):665–78. 10.2307/3574084 [DOI] [PubMed] [Google Scholar]
- 9.Trottmann M, Becker AJ, Stadler T, Straub J, Soljanik I, Schlenker B, et al. Semen quality in men with malignant diseases before and after therapy and the role of cryopreservation. Eur Urol. 2007;52(2):355–67. 10.1016/j.eururo.2007.03.085 [DOI] [PubMed] [Google Scholar]
- 10.Harris VA, Staffurth J, Naismith O, Esmail A, Gulliford S, Khoo V, et al. Consensus guidelines and contouring atlas for pelvic node delineation in prostate and pelvic node intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2015;92(4):874–83. 10.1016/j.ijrobp.2015.03.021 [DOI] [PubMed] [Google Scholar]
- 11.Salembier C, Villeirs G, De Bari B, Hoskin P, Pieters BR, Van Vulpen M, et al. ESTRO ACROP consensus guideline on CT- and MRI-based target volume delineation for primary radiation therapy of localized prostate cancer. Radiother Oncol. 2018;127(1):49–61. 10.1016/j.radonc.2018.01.014 [DOI] [PubMed] [Google Scholar]
- 12.Zelefsky MJ, Kollmeier M, McBride S, Varghese M, Mychalczak B, Gewanter R, et al. Five-year outcomes of a phase 1 dose-escalation study using stereotactic body radiosurgery for patients with low-risk and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2019;104(1):42–9. 10.1016/j.ijrobp.2018.12.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Musunuru HB, Davidson M, Cheung P, Vesprini D, Liu S, Chung H, et al. Predictive parameters of symptomatic hematochezia following 5-fraction gantry-based SABR in prostate cancer. Int J Radiat Oncol Biol Phys. 2016;94(5):1043–51. 10.1016/j.ijrobp.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 14.Kirisits C, Schmid MP, Nesvacil N, Pötter R. Medical University of Vienna, Vienna, Austria. In: Song WY, Tanderup K, Pieters BR, editors. Series in medical physics and biomedical engineering. CRC Press: Boca Raton; 2017. p. 275–84. 10.1201/9781315120966-20. [Google Scholar]
- 15.Proust-Lima C, Taylor JMG, Sécher S, Sandler H, Kestin L, Pickles T, et al. Confirmation of a low α/β ratio for prostate cancer treated by external beam radiation therapy alone using a post-treatment repeated-measures model for PSA dynamics. Int J Radiat Oncol Biol Phys. 2011;79(1):195–201. 10.1016/j.ijrobp.2009.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miralbell R, Roberts SA, Zubizarreta E, Hendry JH. Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: α/β = 1.4 (0.9–2.2) Gy. Int J Radiat Oncol Biol Phys. 2012;82(1):e17-24. 10.1016/j.ijrobp.2010.10.075 [DOI] [PubMed] [Google Scholar]
- 17.Dasu A, Toma-Dasu I. Prostate alpha/beta revisited—an analysis of clinical results from 14 168 patients. Acta Oncol Stockh Swed. 2012;51(8):963–74. 10.3109/0284186X.2012.719635 [DOI] [PubMed] [Google Scholar]
- 18.Ogilvy-Stuart AL, Shalet SM. Effect of radiation on the human reproductive system. Environ Health Perspect. 1993;101(Suppl 2):109–16. 10.1289/ehp.93101s2109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clermont Y. Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and spermatogonial renewal. Physiol Rev. 1972;52(1):198–236. 10.1152/physrev.1972.52.1.198 [DOI] [PubMed] [Google Scholar]
- 20.Okada K, Fujisawa M. Recovery of spermatogenesis following cancer treatment with cytotoxic chemotherapy and radiotherapy. World J Mens Health. 2019;37(2):166–74. 10.5534/wjmh.180043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hahn EW, Feingold SM, Nisce L. Aspermia and recovery of spermatogenesis in cancer patients following incidental gonadal irradiation during treatment: a progress report. Radiology. 1976;119(1):223–5. 10.1148/119.1.223 [DOI] [PubMed] [Google Scholar]
- 22.Hahn EW, Feingold SM, Simpson L, Batata M. Recovery from aspermia induced by low-dose radiation in seminoma patients. Cancer. 1982;50(2):337–40. [DOI] [PubMed] [Google Scholar]
- 23.Howell SJ, Shalet SM. Spermatogenesis after cancer treatment: damage and recovery. J Natl Cancer Inst Monogr. 2005;34:12–7. 10.1093/jncimonographs/lgi003 [DOI] [PubMed] [Google Scholar]
- 24.Ash P. The influence of radiation on fertility in man. Br J Radiol. 1980;53(628):271–8. 10.1259/0007-1285-53-628-271 [DOI] [PubMed] [Google Scholar]
- 25.Sandeman TF. The effects of x irradiation on male human fertility. Br J Radiol. 1966;39(468):901–7. 10.1259/0007-1285-39-468-901 [DOI] [PubMed] [Google Scholar]
- 26.Centola GM, Keller JW, Henzler M, Rubin P. Effect of low-dose testicular irradiation on sperm count and fertility in patients with testicular seminoma. J Androl. 1994;15(6):608–13. 10.1002/j.1939-4640.1994.tb00507.x [DOI] [PubMed] [Google Scholar]
- 27.Tomić R, Bergman B, Damber JE, Littbrand B, Löfroth PO. Effects of external radiation therapy for cancer of the prostate on the serum concentrations of testosterone, follicle-stimulating hormone, luteinizing hormone and prolactin. J Urol. 1983;130(2):287–9. 10.1016/S0022-5347(17)51110-6 [DOI] [PubMed] [Google Scholar]
- 28.Daniell HW, Clark JC, Pereira SE, Niazi ZA, Ferguson DW, Dunn SR, et al. Hypogonadism following prostate-bed radiation therapy for prostate carcinoma. Cancer. 2001;91(10):1889–95. [DOI] [PubMed] [Google Scholar]
- 29.Grigsby PW, Perez CA. The effects of external beam radiotherapy on endocrine function in patients with carcinoma of the prostate. J Urol. 1986;135(4):726–7. 10.1016/S0022-5347(17)45831-9 [DOI] [PubMed] [Google Scholar]
- 30.Boehmer D, Badakhshi H, Kuschke W, Bohsung J, Budach V. Testicular dose in prostate cancer radiotherapy: impact on impairment of fertility and hormonal function. Strahlenther Onkol Organ Dtsch Rontgengesellschaft Al. 2005;181(3):179–84. 10.1007/s00066-005-1282-1 [DOI] [PubMed] [Google Scholar]
- 31.Budgell GJ, Cowan RA, Hounsell AR. Prediction of scattered dose to the testes in abdominopelvic radiotherapy. Clin Oncol R Coll Radiol G B. 2001;13(2):120–5. [DOI] [PubMed] [Google Scholar]
- 32.Katayama S, Haefner MF, Mohr A, Schubert K, Oetzel D, Debus J, et al. Accelerated tomotherapy delivery with TomoEdge technique. J Appl Clin Med Phys. 2015;16(2):33–42. 10.1120/jacmp.v16i2.4964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoppe BS, Harris S, Rhoton-Vlasak A, Bryant C, Morris CG, Dagan R, et al. Sperm preservation and neutron contamination following proton therapy for prostate cancer study. Acta Oncol Stockh Swed. 2017;56(1):17–20. 10.1080/0284186X.2016.1205219 [DOI] [PubMed] [Google Scholar]
- 34.Fraass BA, Kinsella TJ, Harrington FS, Glatstein E. Peripheral dose to the testes: the design and clinical use of a practical and effective gonadal shield. Int J Radiat Oncol Biol Phys. 1985;11(3):609–15. 10.1016/0360-3016(85)90196-8 [DOI] [PubMed] [Google Scholar]
- 35.Lieng H, Chung P, Lam T, Warde P, Craig T. Testicular seminoma: Scattered radiation dose to the contralateral testis in the modern era. Pract Radiat Oncol. 2018;8(2):e57-62. 10.1016/j.prro.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 36.Mydlo JH, Lebed B. Does brachytherapy of the prostate affect sperm quality and/or fertility in younger men? Scand J Urol Nephrol. 2004;38(3):221–4. 10.1080/00365590410025451 [DOI] [PubMed] [Google Scholar]
- 37.Delaunay B, Delannes M, Bachaud JM, Bouaziz M, Salloum A, Thoulouzan M, et al. Fertility after prostate brachytherapy with Iode 125 permanent implants for localized prostate cancer. Progres En Urol J Assoc Francaise Urol Soc Francaise Urol. 2012;22(1):53–7. [DOI] [PubMed] [Google Scholar]
- 38.Khaksar SJ, Laing RW, Langley SEM. Fertility after prostate brachytherapy. BJU Int. 2005;96(6):915. 10.1111/j.1464-410X.2005.05841_1.x [DOI] [PubMed] [Google Scholar]
- 39.Boyd BG, McCallum SW, Lewis RW, Terris MK. Assessment of patient concern and adequacy of informed consent regarding infertility resulting from prostate cancer treatment. Urology. 2006;68(4):840–4. 10.1016/j.urology.2006.04.009 [DOI] [PubMed] [Google Scholar]
- 40.Lambertini M, Peccatori FA, Demeestere I, Amant F, Wyns C, Stukenborg JB, et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2020;S0923753420424482. [DOI] [PubMed]
- 41.Knoester PA, Leonard M, Wood DP, Schuster TG. Fertility issues for men with newly diagnosed prostate cancer. Urology. 2007;69(1):123–5. 10.1016/j.urology.2006.09.036 [DOI] [PubMed] [Google Scholar]
- 42.Hall MC, Fritzsch RJ, Sagalowsky AI, Ahrens A, Petty B, Roehrborn CG. Prospective determination of the hormonal response after cessation of luteinizing hormone-releasing hormone agonist treatment in patients with prostate cancer. Urology. 1999;53(5):898–902. 10.1016/S0090-4295(99)00061-8 [DOI] [PubMed] [Google Scholar]
- 43.da Silva SM, Anderson RA. Reproductive axis ageing and fertility in men. Rev Endocr Metab Disord. 2022;23(6):1109–21. 10.1007/s11154-022-09759-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson LJ, Newhauser WD, Schneider CW, Kamp F, Reiner M, Martins JC, et al. Method to quickly and accurately calculate absorbed dose from therapeutic and stray photon exposures throughout the entire body in individual patients. Med Phys. 2020;47(5):2254–66. 10.1002/mp.14018 [DOI] [PubMed] [Google Scholar]
- 45.Sánchez-Nieto B, Medina-Ascanio KN, Rodríguez-Mongua JL, Doerner E, Espinoza I. Study of out-of-field dose in photon radiotherapy: a commercial treatment planning system versus measurements and Monte Carlo simulations. Med Phys. 2020 [DOI] [PMC free article] [PubMed]
- 46.Joosten A, Matzinger O, Jeanneret-Sozzi W, Bochud F, Moeckli R. Evaluation of organ-specific peripheral doses after 2-dimensional, 3-dimensional and hybrid intensity modulated radiation therapy for breast cancer based on Monte Carlo and convolution/superposition algorithms: implications for secondary cancer risk assessment. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2013;106(1):33–41. 10.1016/j.radonc.2012.11.012 [DOI] [PubMed] [Google Scholar]
- 47.Schneider U, Hälg RA, Hartmann M, Mack A, Storelli F, Joosten A, et al. Accuracy of out-of-field dose calculation of tomotherapy and cyberknife treatment planning systems: a dosimetric study. Z Med Phys. 2014;24(3):211–5. 10.1016/j.zemedi.2013.10.008 [DOI] [PubMed] [Google Scholar]
- 48.Zelefsky MJ, Kollmeier M, Cox B, Fidaleo A, Sperling D, Pei X, et al. Improved clinical outcomes with high-dose image guided radiotherapy compared with non-IGRT for the treatment of clinically localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012;84(1):125–9. 10.1016/j.ijrobp.2011.11.047 [DOI] [PubMed] [Google Scholar]
- 49.Alaei P, Spezi E. Imaging dose from cone beam computed tomography in radiation therapy. Phys Med PM Int J Devoted Appl Phys Med Biol Off J Ital Assoc Biomed Phys AIFB. 2015;31(7):647–58. [DOI] [PubMed] [Google Scholar]
- 50.Alaei P, Spezi E, Reynolds M. Dose calculation and treatment plan optimization including imaging dose from kilovoltage cone beam computed tomography. Acta Oncol Stockh Swed. 2014;53(6):839–44. 10.3109/0284186X.2013.875626 [DOI] [PubMed] [Google Scholar]
- 51.Shah AP, Langen KM, Ruchala KJ, Cox A, Kupelian PA, Meeks SL. Patient dose from megavoltage computed tomography imaging. Int J Radiat Oncol Biol Phys. 2008;70(5):1579–87. 10.1016/j.ijrobp.2007.11.048 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.