ABSTRACT:
Objective
The incidence of acute kidney injury (AKI) in pediatric patients has been increasing over the years, and AKI significantly impacts children’s health and quality of life. This article reviews the current epidemiological research on pediatric AKI.
Methods
The clinical data of hospitalized children aged 0 to 14 years from 20 different hospitals in Hunan Province, China, collected from December 2017 to February 2018, were analyzed. The incidence rate, misdiagnosis rate, main causes, and medical costs of AKI in hospitalized children were examined.
Results
A total of 29,639 patients were included, with an AKI incidence rate of 4.34% (1286/29,639). Among the 1286 AKI patients, 863 (67.11%) were classified as AKI stage 1324 (25.19%) as AKI stage 2, and 99 (7.7%) as AKI stage 3. AKI patients had significantly longer hospital stays [6.0 (4.0, 10) days vs. 6.0 (4.0, 8.0) days, p < 0.001] and higher hospitalization costs [3375.22 (1600, 6083.83) yuan vs. 2729.4 (1659.45, 8216.65) yuan, p = 0.003] than non-AKI patients. The mortality rate (1.2% vs. 0.1%, p < 0.001), intensive care unit (ICU) transfer rate (8.7% vs. 5.97%, p < 0.001), and use of invasive mechanical ventilation (3.6% vs. 1%, p < 0.001) were significantly greater in patients with AKI than in those without AKI patients. The etiology of AKI varied among different age groups, and dehydration, diarrhea, and shock were the main causes of pre-renal AKI.
Conclusion
The incidence and missed diagnosis rates of AKI in hospitalized children were high. AKI prolongs hospital stays, increases hospitalization costs, and increases the risk of mortality in children.
Keywords: Children, acute kidney injury, multicenter study, epidemiology
1. Introduction
Acute kidney injury (AKI) is one of the most common and serious complications in hospitalized patients. According to previous studies, the incidence of AKI has been increasing over the years [1], with approximately 13 million hospitalized patients worldwide developing AKI annually, resulting in approximately 1.7 million deaths [2]. The occurrence rate of AKI varies from 0.5% to 78% owing to differences in the definition, timeframe, and study population [3]. AKI not only has a high incidence and risk of death [2] but can also progress to chronic kidney disease and end-stage renal disease, leading to increased hospitalization time and costs for patients [3–5]. Additionally, it reduces the quality of life of the patients [6].
The incidence of AKI was reported to be 6.0% in Kaiser Permanente Northern California 2008 and increased to 8.8% in 2016[7]. Despite the relatively high incidence of AKI, there is still insufficient awareness and attention, resulting in a high rate of missed AKI diagnoses. Early diagnosis and timely intervention for AKI are particularly important for improving kidney damage. However, in clinical practice, there is relatively little focus on pediatric AKI, and relevant clinical research data are limited. Therefore, we conducted a multicenter cross-sectional study to understand the incidence, missed diagnosis rate, and main etiology of AKI in children.
2. Materials and methods
2.1. Study population
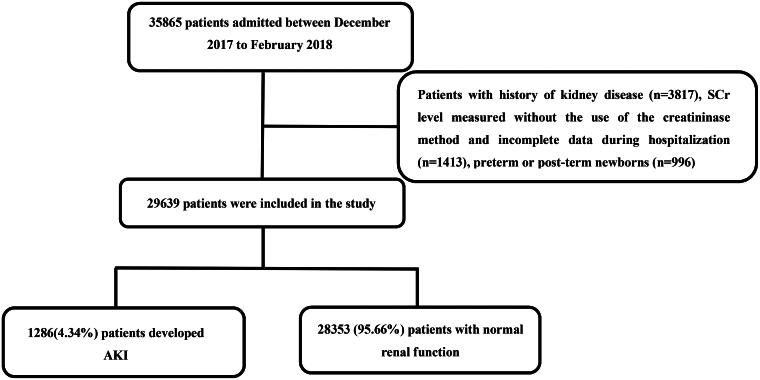
Our study was conducted in Hunan Province (Hunan, China), which was divided into five different regions (east, south, west, north, and central) according to the geographical location. Depending on the population of the region, 3-5 hospitals were randomly selected in different regions, and finally a total of 20 hospitals participated in the study. The study population consisted of all hospitalized patients from the 20 hospitals, including patients in internal medicine, surgery and intensive care units. Eligible patients were aged between 0 and 14 years. We identified all inpatients who were in the 20 hospitals during the study period (n = 35,865). We excluded patients with a history of kidney disease, including nephrotic syndrome, acute or chronic nephritis, patients with a history of kidney tumors, patients who previously underwent kidney surgery (n = 3817), patients with a serum creatinine (SCr) measurement for which the creatininase method was not used, patients with incomplete data during hospitalization (n = 1413), and patients who were preterm or post-term newborns (n = 996). The final analytical cohort included 29,639 patients of hospitalized children (Figure 1). This clinical trial had been registered in the Chinese Clinical Trial Registry (http://www.chictr.org.cn; Identifier: ChiCTR-EOC-17013597).
Figure 1.
Study flowchart. AKI: acute kidney injury; SCr: serum creatinine.
2.2. Definition
Acute kidney injury (AKI) was defined as a serum creatinine level ≥ 26.5 μmol/L (0.3 mg/dl) within 48 h, or increased more than 50% from the baseline within 7 days, or urine output of less than 0.5 mL/kg/h and continued for more than 6 h[8]. The baseline value was defined as the serum creatinine value within 7 days before onset, or the average serum creatinine value available from 7 to 365 days before onset, and the AKI staging criteria are shown in Table 1.
Table 1.
AKI staging criteria.
| Stage | Creatinine (SCr) | Urine Output |
|---|---|---|
| 1 | Increase in SCr ≥ 0.3 mg/dl (26.5 μmol/L) within 48 h; or increase in SCr 1.5–1.9 times baseline within 7 days | < 0.5 ml/kg/h for ≥ 6 h |
| 2 | serum creatinine 2–2.9 times baseline | < 0.5 ml/kg/h for ≥ 12 h |
| 3 | Increase in SCr ≥ 3.0 times baseline; or SCr ≥ 4.0 mg/dl (353.6 μmol/L); or initiation of renal replacement therapy; or < 18 years old with estimated glomerular filtration rate < 35 ml/min/1.73m2 | < 0.3 ml/kg/h for ≥24 hours or anuria for ≥ 12 h |
Community-acquired AKI (CA-AKI) was defined as when a patient had AKI that could be diagnosed at hospital admission. Hospital-acquired AKI (HA-AKI) was defined as normal kidney function at the hospital, with the development of AKI during hospitalization.
2.3. Data collection
Baseline demographic and clinical data, including age, gender, age, intensive care unit (ICU) transfer status, total hospitalization duration, hospitalization expenses, mortality, mechanical ventilation usage, and laboratory investigations (hemoglobin, proteinuria, blood in the urine, albumin, serum creatinine), were recorded.
2.4. Statistical analysis
Statistical analyses were performed using SPSS version 22.0, and analyses. Categorical data were presented as n (%). Continuous variables were reported as medians with interquartile ranges (IQR) due to a skewed distribution. The chi-square test or Fisher’s exact test was used for categorical variables, whereas the Mann-Whitney U test or Kruskal-Wallis H test was used for continuous variables. Statistical significance was set at p < 0.05.
3. Results
3.1. Demographic characteristics
A total of 29,639 pediatric patients were included in this study, including 18,762 males (63.3%) and 10,877 females (36.69%). The average age was 2.83 ± 3.11 years, and the average length of hospital stay was 6.0 (4.0, 8.0) days. The average hospitalization cost was 3346 (1602, 6132) yuan. Among them, 11,361 patients (39.2%) were less than 1 year old, 7501 patients (25.1%) were between 1 and 3 years old, 7089 patients (23.6%) were between 3 and 7 years old, and 3688 patients (12.1%) were between 7 and 14 years old (Table 2).
Table 2.
Comparison of clinical data between AKI group and non-AKI group.
| AKI group | non-AKI group | p | |
|---|---|---|---|
| patients (n) | 1286 | 28353 | |
| Age group (n [%]) | 0.000 | ||
| 0– 28 d | 115(8.94%) | 2721(9.59%) | |
| 29 d − 1 yr | 323(25.12%) | 8202(28.93%) | |
| 1–3 yr | 485(37.71%) | 7016(24.75%) | |
| 3–7 yr | 292(22.71%) | 6797(23.97%) | |
| 7–14 yr | 71(5.52%) | 3617(12.76%) | |
| Gender (n, male/female) | 833/453 | 17929/10424 | 0.274 |
| Age (years) | 2.29 ± 2.44 | 2.85 ± 3.14 | 0.000 |
| Transfer to ICU (n, %) | 112(8.7) | 1694(5.97) | 0.000 |
| Surgery (n, %) | 167(13) | 4213(14.9) | 0.066 |
| put on ventilator (n, %) | 46(3.6) | 281(1) | 0.000 |
| Hospitalization expenses (yuan) | 2729.4(1659.45,8216.65) | 3375.22(1600,6083.83) | 0.003 |
| Length of stay in hospital (days) | 6(4.10) | 6(4.8) | 0.000 |
| mortality (n, %) | 16(1.2) | 28(0.1) | 0.000 |
AKI: acute kidney injury.
Among the 29,639 pediatric patients included in the study, 1286 (4.34%) developed acute kidney injury (AKI). Of these, 863 patients (67.11%) were classified as AKI stage 1, 324 (25.19%) as AKI stage 2, and 99 (7.7%) as AKI stage 3 (Table 3). Interestingly, only 38 patients (2.95%) were diagnosed with AKI during hospitalization, indicating a high misdiagnosis rate of 97.05%.
Table 3.
Comparison of clinical data according to AKI stage.
| AKI stage 1 | AKI stage 2 | AKI stage 3 | p | |
|---|---|---|---|---|
| patients (n,%) | 863(67.11) | 324(25.19) | 99(7.7) | |
| Gender (n, male/female) | 533/330 | 235/89 | 65/34 | 0.002 |
| Age (years) | 1.81 ± 1.94 | 3.20 ± 2.53 | 3.46 ± 4.25 | 0.525 |
| Transfer to ICU (n, %) | 40(4.63)* | 30(9.26)* | 42(42.42) | 0.000 |
| Surgery (n, %) | 100(11.59) | 53(16.36) | 14(14.14) | 0.088 |
| put on ventilator (n, %) | 13(1.51)* | 13(4.01)* | 20(20.2) | 0.000 |
| Hospitalization expenses (yuan) | 2413.07 (1581,6534.28)* |
2618.35 (1657.25,9369.77)* |
13885.36 (6631,30663.24) |
0.000 |
| Length of stay in hospital (days) | 6(4.8)* | 6(4,9.75)* | 12(7.19) | 0.000 |
| mortality, (n, %) | 4(0.46)* | 4(1.23)* | 8(8.08) | 0.000 |
| hemoglobin (g/L) | 0.000 | |||
| ≥120, n(%) | 278(32.21) | 155(47.84) | 35(35.35) | |
| 90–120, n(%) | 558(64.66) | 158(48.77) | 52(52.53) | |
| <90, n(%) | 27(3.13)* | 11(3.39)* | 12(12.12) | |
| Proteinuria, n(%) | 13(1.51)* | 16(4.94)* | 15(15.15) | 0.000 |
| Blood in the urine, n(%) | 20(2.32)* | 23(7.1)* | 37(37.37) | 0.000 |
| Albumin < 30 g/L, n(%) | 6(0.7)* | 9(2.78)* | 14(14.14) | 0.000 |
*p < 0.001 vs AKI stage 3.
3.2. Incidence rates of AKI in different age groups
Among the 1286 pediatric patients who developed AKI, the highest incidence rate of AKI was observed in children aged 1–3 years, with a rate of 6.47% (485/7016). Children aged ≥ 7 years had the lowest incidence rate of AKI, with only 1.93% (71/3688) affected. The incidence rates of AKI in children aged < 1 month, 1 month to 1 year, and 3 to 7 years were 4.06% (115/2836), 3.79% (323/8525), and 4.12% (292/7089), respectively. There were statistically significant differences in the incidence rates of AKI among the different age groups (p < 0.001) (Table 2).
3.3. Clinical data of AKI and non-AKI patients
Patients were divided into AKI and non-AKI groups based on the diagnostic criteria for AKI. There was no significant difference in male composition between the AKI and non-AKI groups (64.8% vs. 63.2%, p > 0.05). However, there were significant differences in the total length of hospital stay between the AKI and non-AKI groups, with 6.0 (4.0, 10.0) days and 6.0 (4.0, 8.0) days, respectively (p < 0.001). The average total hospitalization cost per person in the AKI group was significantly higher than that in the non-AKI group, with costs of 3375.22 (1600, 6083.83) yuan vs. 2729.4 (1659.45, 8216.65) yuan (p = 0.003). Compared to the non-AKI group, the AKI group had a greater mortality rate (1.2% vs. 0.1%, p < 0.001), higher rate of invasive mechanical ventilation use (3.6% vs 1%, p < 0.001), and a higher rate of ICU transfer (8.72% vs. 6%, p < 0.001) (Table 2).
3.4. Comparative analysis of clinical data among the different AKI stage groups
By analyzing the clinical data of pediatric patients at different stages of AKI, it was found that the rates of ICU transfer, mechanical ventilation use, and mortality increased gradually with increasing AKI severity. The progression of AKI resulted in prolonged hospitalization and increased hospitalization costs (Table 3). The rates of mechanical ventilation use and ICU transfer in stage 3 AKI patients were significantly greater than those in stage 1 AKI patients and stage 2 AKI patients (p < 0.001). Hospitalization duration and costs were significantly greater for stage 3 AKI patients than for stage 1 AKI patients and stage 2 AKI patients (p < 0.001). The mortality rate of AKI stage 3 patients was significantly greater than that of stage 1 AKI patients and stage 2 AKI patients. Additionally, stage 3 AKI patients had a significantly greater incidence of a hemoglobin level < 90 g/L, proteinuria, hematuria, and hypoalbuminemia than stage 1 AKI patients and stage 2 AKI patients (Table 3).
3.5. Etiological analysis of AKI in children of different ages
The etiology of AKI varied among children of different ages. Among the newborns, the top three causes of AKI were dehydration, diarrhea, and shock, accounting for 19 patients (16.5%), kidney injury due to respiratory system diseases in 18 patients (15.6%), and neonatal asphyxia in 13 patients (11.3%). Neonatal hyperbilirubinemia and sepsis were also common causes of AKI, accounting for 12 patients each. In infants under 1 year old, the top three causes of AKI are drug-induced kidney injury with 159 patients (54.5%), diarrhea, vomiting, and dehydration with 37 patients (12.7%), and respiratory system diseases with 15 patients (5.1%). For children aged 1 to 3 years, the top three causes of AKI were drug-induced kidney injury (218 patients, 56.5%), diarrhea, vomiting, and dehydration (29 patients, 7.5%), and sepsis (14 patients, 3.6%). In children aged 3–7 years, the top three causes of AKI were drug-induced kidney injury (99 patients, 41.6%), diarrhea, vomiting, dehydration, and bleeding (20 patients, 8.4%), and respiratory system diseases (19 patients, 8.0%). For children aged > 7 years, the top three causes of AKI were drug-induced kidney injury (15 patients, 23.4%), primary renal diseases (acute nephritis, nephrotic syndrome, and IgA nephropathy) (12 patients, 18.8%), and kidney injury due to conditions such as diarrhea, dehydration, shock, and bleeding (6 patients, 9.4%).
3.6. Comparison of the general conditions of children with hospital-acquired AKI and those with community-acquired AKI
Among the 1286 children with AKI, 107 (8.3%) had hospital-acquired AKI (HA-AKI), 1179 (91.7%) had community-acquired AKI (CA-AKI), and the missed diagnosis rates of HA-AKI of the two groups were 1148 (97.4%) and 98 (91.6%), respectively, which were significantly different (p = 0.003). The rates of ICU transfer, invasive ventilator use, and mortality in patients with HA-AKI were significantly greater than those in patients with CA-AKI (p < 0.001) (Table 4).
Table 4.
Comparison of clinical data between the HA-AKI and non-AKI groups.
| n | rate of missed diagnosis (%) | put on a ventilator (n, %) | mortality (n, %) | Transfer to ICU (n, %) | Hospitalization expenses (yuan) | Length of stay in hospital (days) | |
|---|---|---|---|---|---|---|---|
| HA-AKI | 107 | 91.6% | 23(21.5%) | 6(5.61%) | 45(42.1%) | 24991.9(11138.2, 56945.3) | 15.0(10.0, 27.0) |
| CA-AKI | 1179 | 97.4% | 41(3.5%) | 10(0.85%) | 112(9.5%) | 4655.0(1932.0, 9656.1) | 5.0(4.0, 8.0) |
| P | – | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
HA-AKI: hospital-acquired AKI; CA-AKI: community-acquired AKI.
3.7. Renal function at discharge in patients with AKI
The serum creatinine levels of 853 children returned to normal before discharge, those of 98 children did not return to normal before discharge, and 335 children were not rechecked their serum creatinine level due to missed diagnosis or temporary discharge.
4. Discussion
The incidence of acute kidney injury (AKI) has gradually increased over the years and has become a global public health issue. Studies have shown that the incidence of AKI among hospitalized patients is approximately 15%, but it significantly increases to > 60% in critically ill patients in the intensive care unit (ICU) [9]. Epidemiological studies have shown that AKI is an independent risk factor for mortality in hospitalized patients [10]. Therefore, early diagnosis and timely intervention are important to improve kidney damage. However, pediatric AKI has received less clinical attention, and limited clinical research data are available.
In 2013, a survey conducted in China reported a misdiagnosis rate of 74.2% among adult inpatients with AKI and a nephrology consultation rate of only 21.4% [11]. In this study, the incidence of AKI was 4.34% (1286/29,639). However, the diagnostic rate of AKI during hospitalization was only 2.95% (38/1286), indicating a high rate of missed AKI diagnoses (97.05%). The misdiagnosis rate of AKI was high, indicating a severe lack of awareness regarding AKI among healthcare professionals.
Of the 29,639 pediatric patients enrolled, 1286 (4.34%) were diagnosed with AKI. Among the 1286 AKI patients, 863 (67.11%) were classified as AKI stage 1, which was significantly higher than AKI stage 2 or AKI stage 3. Research has shown that even mild AKI or a slight increase in the SCr level can lead to significant adverse outcomes. Even a small increase in SCr levels can significantly increase the risk of death [12]. Therefore, early intervention is necessary. Regardless of severity, patients who experience AKI should be followed up to improve their long-term prognosis and monitor the development of chronic kidney disease (CKD) and its subsequent complications [6]. Studies have shown that, in most developing countries, blood volume depletion remains one of the main causes of AKI, which is similar to the etiology of AKI found in this study [9].
In this study, 44 deaths occurred at the time of discharge, with 16 deaths among AKI patients (1.2%) and 28 deaths among non-AKI patients (0.1%). The in-hospital mortality and AKI mortality rates were lower than those reported in the literature [13]. This may be related to the fact that our study included not only ICU inpatients, but also other hospitalized patients. This may also be related to the decrease in mortality rate during hospitalization for AKI patients due to improvements in medical care. However, the risk of death in AKI patients was significantly higher than that in non-AKI patients, which is consistent with the literature [14, 15].
The results of this survey showed that the occurrence of AKI during hospitalization prolonged the length of hospital stay and increased the cost of hospitalization. The average length of stay and hospitalization costs gradually increased with increasing AKI stage. These results are similar to those reported in the literature [16, 17]. Early identification of patients with risk factors for AKI and intervention can prevent some patients of AKI. Renal function can be reversed in some patients even after the occurrence of AKI [18]. Therefore, it is necessary to strengthen the early recognition and intervention of AKI.
In summary, this study demonstrated that AKI is not uncommon in hospitalized children, with a misdiagnosis rate as high as 96.9%. AKI increases the length of hospital stay, hospitalization costs, the use of invasive mechanical ventilation, and the risk of death in pediatric patients. Therefore, it is crucial for pediatric healthcare professionals to gain a better understanding of and pay attention to AKI. However, our study has several limitations. The level of SCr as the main diagnostic index of AKI, we were unable to ascertain the timing of the peak SCr level, and the patient’s urine volume may not be accurately recorded, the true prevalence of AKI and the severity of kidney injury may be underestimated. In addition, this study was a cross-sectional survey with a relatively short observation period and lacking a long-term follow-up. Owing to the wide scope of the study and the large sample size, conducting follow-up investigations posed challenges. Therefore, further research is required to explore the long-term prognosis of AKI in pediatric patients.
Acknowledgments
Pediatric Department at Children’s Hospital of Chenzhou City (Xingyuan Xie); Pediatric Department at the First Affiliated Hospital of South China University (Yunhua Yang); Pediatric Department at People’s Hospital of Xiangxi Autonomous Prefecture (Min Shi); Pediatric Department at People’s Hospital of Zhangjiajie City (Guihua Yang); Liuyang Maternal and Child Health Hospital (Chunxiang Liu); Pediatric Department at Qiyang County People’s Hospital (Jianjun Jiang); Pediatric Department at Yueyang City Second People’s Hospital (Dijun Liu); Pediatric Department at Linwu County Traditional Chinese Medicine Hospital (Hui Su); Third People’s Hospital of Huaihua City (Fanmao Zeng); Pediatric Department at Loudi Central Hospital (Xinping Jiang); Pediatric Department at Anxiang County Maternal and Child Health Hospital (Mingmai Wang); Pediatric Department at Ziyang District Maternal and Child Health Hospital (Yuhui Huang); Pediatric Department at People’s Hospital of Lianyuan City (Meifen Song); People’s Hospital of Longshan County(Dejun Wu); Longhui County Maternal and Child Health Hospital(Xuexia Tan); Maternal and Child Health Hospital of Xiangtan City(Qingru Xiao); Maternal and Child Health Hospital of Lei Yang City(Hui Li); Taohuajiang Central Hospital(Bicheng Wang); People’s Hospital of Xintian County(Qionghui Zheng)
Funding Statement
This work was supported by the Key Research and Development Program of Hunan Province (No.2018SK2139) and the Key Research Funding Project of the Health Commission of Hunan Province (No. 202106012359)
Ethics approval
This study was approved by the Scientific Research and Ethics Board of Hunan Children’s Hospital and 19 other hospitals in accordance with the Declaration of Helsinki. Written informed parental consent was obtained from all patients or their parents.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The raw data supporting the conclusions of this manuscript will be made available by the authors, The datasets during the current study are available on the website of http://www.chictr.org.cn/login.aspx?referurl=/addproject2.aspx
References
- 1.Negi S, Koreeda D, Kobayashi S, et al. Acute kidney injury: epidemiology, outcomes, complications, and therapeutic strategies. Semin Dial. 2018;31(5):519–527. doi: 10.1111/sdi.12705. [DOI] [PubMed] [Google Scholar]
- 2.Yang Z, Wang C, Wang H, et al. Cross-sectional survey on adult acute kidney injury in Chinese ICU: the study protocol (CARE-AKI.)BMJ Open. 2018;8(6):e020766. doi: 10.1136/bmjopen-2017-020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melo FAF, Macedo E, Fonseca Bezerra AC, et al. A systematic review and meta-analysis of acute kidney injury in the intensive care units of developed and developing countries. PLOS One. 2020; 15(1):e0226325. doi: 10.1371/journal.pone.0226325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uber AM, Sutherland SM.. Acute kidney injury in hospitalized children: consequences and outcomes. Pediatr Nephrol. 2020;35(2):213–220. doi: 10.1007/s00467-018-4128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alobaidi R, Morgan C, Goldstein SL, et al. Population-based epidemiology and outcomes of acute kidney injury in critically ill children. Pediatr Crit Care Med. 2020;21(1):82–91. doi: 10.1097/PCC.0000000000002128. [DOI] [PubMed] [Google Scholar]
- 6.Medina KRP, Jeong JC, Ryu JW, et al. Comparison of outcomes of mild and severe community- and hospital-acquired acute kidney injury. Yonsei Med J. 2022; 63(10):902–907. doi: 10.3349/ymj.2021.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parikh RV, Tan TC, Salyer AS, et al. Community-based epidemiology of hospitalized acute kidney injury. Pediatrics. 2020; 146(3):e20192821. doi: 10.1542/peds.2019-2821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kellum J, Lameire N, Aspelin P, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO Clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1):19–36. doi: 10.1038/kisup.2012.1. [DOI] [Google Scholar]
- 9.Khan FG, Awan S, Namran S, et al. Community acquired versus hospital-acquired acute kidney injury; causes and outcome. J Pak Med Assoc. 2022; 72(6):1128–1132. doi: 10.47391/JPMA.3385. [DOI] [PubMed] [Google Scholar]
- 10.Zeng J, Miao H, Jiang Z, et al. Pediatric reference change value optimized for acute kidney injury: multicenter retrospective study in China. Pediatr Crit Care Med. 2022; 23(12):e574–e582. Epub 2022 Oct 10. doi: 10.1097/PCC.0000000000003085. [DOI] [PubMed] [Google Scholar]
- 11.Yang L, Xing G, Wang L, et al. Acute kidney injury in China: a cross-sectional survey. Lancet. 2015;386(10002):1465–1471. doi: 10.1016/S0140-6736(15)00344-X. [DOI] [PubMed] [Google Scholar]
- 12.Gameiro J, Agapito Fonseca J, Jorge S, et al. Acute kidney injury definition and diagnosis: a narrative review. J Clin Med. 2018; 7(10):307. doi: 10.3390/jcm7100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaddourah A, Basu RK, Bagshaw SM, , et al. Epidemiology of Acute kidney injury in critically ill children and young adults. N Engl J Med. 2017; 376(1):11–20. doi: 10.1056/NEJMoa1611391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soto K, Campos P, Pinto I, et al. The risk of chronic kidney disease and mortality are increased after community-acquired acute kidney injury. Kidney Int. 2016; 90(5):1090–1099. doi: 10.1016/j.kint.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flaatten H, Darmon M.. A nephrologist should be consulted in all patients of acute kidney injury in the ICU: yes. Intensive Care Med. 2017; 43(6):874–876. doi: 10.1007/s00134-017-4790-4. [DOI] [PubMed] [Google Scholar]
- 16.Sigurjonsdottir VK, Chaturvedi S, Mammen C, et al. Pediatric acute kidney injury and the subsequent risk for chronic kidney disease: is there cause for alarm? Pediatr Nephrol. 2018; 33(11):2047–2055. doi: 10.1007/s00467-017-3870-6. [DOI] [PubMed] [Google Scholar]
- 17.Khadzhynov D, Schmidt D, Hardt J, et al. The incidence of acute kidney injury and associated hospital mortality. Dtsch Arztebl Int. 2019; 116(22):397–404. doi: 10.3238/arztebl.2019.0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kerr M, Bedford M, Matthews B, et al. The economic impact of acute kidney injury in England. Nephrol Dial Transplant. 2014;29(7):1362–1368. Epub 2014 Apr 21. doi: 10.1093/ndt/gfu016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this manuscript will be made available by the authors, The datasets during the current study are available on the website of http://www.chictr.org.cn/login.aspx?referurl=/addproject2.aspx