Abstract
ABSTRACT
Objectives
Our aims were (a) to describe the prevalence and incidence of self-reported injuries and illnesses of amateur golfers over a 5-month period and (b) to investigate potential risk factors for injury.
Methods
We recruited 910 amateur golfers (733 males [81%] and 177 females [19%]) from golf clubs in the USA and Switzerland. The median age was 60 (IQR: 47–67) and the median golfing handicap was 12 (IQR: 6–18). Participants’ health was monitored weekly for 5 months using the Oslo Sports Trauma Research Centre Questionnaire on Health Problems. Players also completed a baseline questionnaire on personal and golf-specific characteristics and their medical history.
Results
We distributed 19 406 questionnaires and received 11 180 responses (57.6%). The prevalence of injuries was 11.3% (95% CI: 9.8 to 12.8) and of illnesses was 2% (95% CI 1.7 to 2.2). The incidence of injuries and illnesses was 3.79 (95% CI 3.54 to 4.06) and 0.94 (95% CI 0.81 to 1.07) per golfer per year, respectively. The injury regions with the highest burden of injury (time-loss days per player per year) were lumbosacral spine (5.93), shoulder (3.47) and knee (2.08). Injury risk was higher with increased age, osteoarthritis and previous injury.
Conclusion
The prevalence and incidence of injury and illness in amateur golf were low compared with many other sports. To further reduce the burden of injury, future research attention should be directed towards the lumbosacral spine, knee and shoulder.
Keywords: Golf, Epidemiology, Injuries, Illness, Risk factor
WHAT IS ALREADY KNOWN ON THIS TOPIC
The International Olympic Committee’s Consensus on Injuries and Illnesses in Sport was adapted for golf and published in 2020.
Large prospective descriptive studies identifying risk factors for injury in golf are lacking.
The prevalence and severity of musculoskeletal complaints in amateur golf are similar to the general population.
Golf participation has a low to moderate risk of injury per hour played compared with other sports.
WHAT THIS STUDY ADDS
This prospective study demonstrates the incidence of musculoskeletal complaints in a large cohort of amateur golfers.
Injury burden from golf injuries was highest in lumbosacral spine, shoulder and knee regions.
Previous injury, increasing age and self-reported osteoarthritis were associated with a higher likelihood of self-reported injury.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Injury burden was highest in the lumbosacral spine, knee and shoulder region and clinicians should target prevention interventions to address this injury pattern in golfers.
Treatment optimisation and injury prevention should be targeted across golfers of all ability levels.
Introduction
Golf is a sport that allows players of all ages and abilities to participate together. It is played in over two-thirds of countries, by more than 66 million people and there are now more women and men playing the game than ever before.1,3 Golf has seen a surge in participation following the COVID-19 pandemic, likely because it can be played outside safely.1 4 5 Playing golf provides mental well-being, social and physical benefits to a player’s health and playing for at least 150 min per week enables players to meet key WHO’s recommendations on weekly physical activity.6 A study reported that, after controlling for socioeconomic factors, golfers live on average 5 years longer than non-golfers.7
Although golf is associated with health benefits, there are injuries that can occur secondary to playing. A scoping review by Murray et al described epidemiological studies (both prospective and retrospective) reporting the incidence of injuries in amateur golfers to be between 16% and 41% annually.6 Prospective longitudinal studies analysing golfing-related injuries have reported low injury rates per hour played compared with other sports, at 0.28 to 0.60 injuries per 1000 hours in amateur players.8,10 A more recent study of injury incidence at the Rio 2016 Olympics found golf to have a relatively lower injury rate in comparison to other Olympic sports.11 Injury rates in professional players are higher than in amateurs, perhaps reflecting an increased volume of training and play12,14 and typically affect the spine (lumbar spine followed by cervical spine followed by thoracic spine) and the hand and wrist.12
Most epidemiological studies in golf are over 20 years old. Such studies vary considerably regarding the reporting of the definition of injury, nature of the injury, injury mechanism, time to return to sport and potential causative factors. Consensus statements, injury forms, diagnostic coding and protocols for data collection have since been developed by key stakeholders in other sports including cricket,15 football,16 rugby union,17 rugby league,18 aquatic sports,19 tennis,20 athletics21 and horse racing22 to ensure data from studies is comparable.23 In 2020, the International Olympic Committee (IOC) consensus statement on recording and reporting of illness and injury in sport was published.24 Shortly after, experts in the field of golf medicine and epidemiology published the International Golf Federation (IGF) consensus statement adapted specifically for golf.25 There are currently no large prospective studies analysing the incidence and burden of injuries in non-professional nor professional golfers using the golf-specific consensus framework. Our author group have previously applied the IGF framework in a cross-sectional study reporting injuries among 1170 male golfers, finding that more than a third of the golfers reported low back complaints in the preceding 7 days, while other frequently affected body parts were the shoulder and knee.26 Given this study used a baseline questionnaire at the start of the season, a prospectively conducted study to analyse the injuries and illnesses affecting golfers during the season, and furthermore, the risk factors for injuries and injury burden was warranted.
The main aim of the present study was to assess the prevalence, incidence and burden of injuries and illnesses among amateur golfers over a 5-month period using the IOC and IGF consensus statements methods. Our secondary aim was to investigate potential risk factors by analysing the associations of injury during the season with personal and golfing characteristics obtained at the start of the season.
Methods
Study design and participants
This was a prospective cohort study of 910 amateur golfers over a 5-month period, 767 from the USA and 143 from Switzerland. The breakdown of demographics by country can be seen in online supplemental appendix 1. The mean age of the cohort was 56 years (range 18–80, SD=14) and it included 733 males (81%) and 177 females (19%). The methods applied to this study were consistent with the IGF statement of reporting injuries and illnesses in golf. Ethical approval was granted by the Ethical Committee of Canton Zurich on 14 May 2020 (BASEC Nr.; 2020–00477) and by Belmont University Institutional Review Board, protocol 1112 from 26 April 2021. All golfers provided written informed consent to participate in the study.
Recruitment and inclusion criteria
The inclusion criteria were amateur players (defined as recreational, subelite or elite who do not play on professional tours for money) aged 18 years or older who had played at least one competition in the last 12 months and who are currently playing golf on a course or driving range. Exclusion criteria were those with a golfing handicap over 40, those playing golf where a full swing is not taken (for example those that only putt, or play crazy/mini golf), those with a current injury/illness limiting golf training or competition, significant systemic disease (for example cancer or unstable cardiovascular disease) or professional golfers (defined as those who play on professional tours for money).
The participants received information about the objectives, methodology, inclusion criteria, data protection of the study, and were requested to fill in the informed consent form and an online questionnaire on personal and golf-specific characteristics as well as on their medical history and current complaints at the start of the season, and a weekly questionnaire on injuries and illnesses during the season. The IOC Consensus on Injuries and Illnesses in Sport adapted by the International Golf Federation for the recording and reporting of epidemiological data on injuries and illnesses in golf was used for this study.25 The specific data gathering forms from the consensus guidelines included (1) Baseline Questionnaire, and (2) Weekly Self-Report of Health Complaints and Exposure to Golf. All questionnaires were written in English. Those who completed the entirety of the questionnaires were included.
Injury data collection
Data were collected using a web application and short messaging service (AthleteMonitoring, FITSTATS, Moncton, Canada), with the study questionnaires integrated into the software. Each participant received a username and created an individual password. Once the baseline questionnaire was completed, weekly follow-up reminders were sent to the designated e-mail address of the golfer.
Weekly self-report of health complaints and exposure to golf
This questionnaire was created as part of the IGF consensus on injuries and illnesses reporting in golf.25 It was designed to collect data from players without the need for researchers/medical staff to be available to conduct weekly monitoring. The report form was filled in by the athlete regarding health complaints that affect them but might or might not receive medical attention. These include current injuries or other health problems occurring in the preceding 7 days. It also included questions covering the participants’ golf exposure (hours or balls hit). The questionnaire included the four questions of the Oslo Sports Trauma Research Centre questionnaire on health problems (OSTRC-H2) which recorded the consequences of health problems on golf participation, training and performance, as well as the degree of symptoms the player had experienced in the preceding 7 days. Based on the player’s responses to these questions, a severity score ranging from 0 to 100 was calculated each week for each health problem.27 28
Definition and classification of health problems
Golfers were asked to record all health problems, irrespective of whether they sought medical attention or whether the problem affected their golf participation (ie, we applied in ‘all complaints’ definition).25 Consistent with the IOC and IGF consensus recommendations, health problems were classified as injuries or illnesses, and injuries were classified as gradual-onset or sudden-onset injuries. Health problems were considered ‘substantial’ if they lead to moderate or severe modifications to training, moderate or severe reductions in performance, or cause the participant to be unable to participate in golf. Burden was a combined measure of the overall effect of a health problem and was expressed as time-loss days per player-year.29
Prevalence calculation
We calculated weekly prevalence by dividing the number of participants reporting health complaints by the number of questionnaire respondents. The average weekly prevalence with 95% CI was calculated for all health problems, substantial health problems, all injuries, substantial injuries, all illnesses and substantial illnesses.
Injury incidence and burden
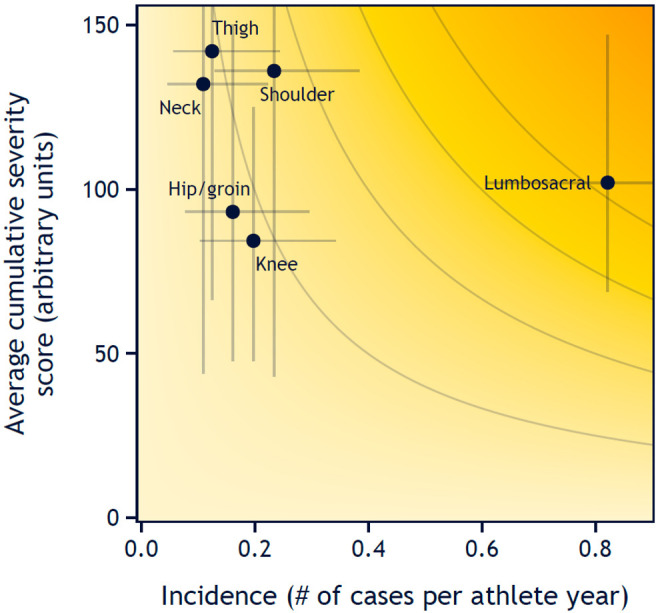
The injury incidence was calculated as the number of new injuries per golfer per year (365 days). Injury and illness burden was calculated factoring in both injury incidence and severity. For each injury type, severity was shown as the median number of days lost. To reflect the relative burden of sudden-onset injuries, gradual-onset injuries, and illnesses as a proportion of the total health burden, we summarised the severity scores for each health problem type and divided the result by the cumulative severity score for all health problems.30 We created risk matrices to illustrate the severity and incidence of injuries in the most affected anatomic regions. This was performed for both sudden-onset and gradual-onset injuries, as well as illnesses, using two measures of severity: the average number of time-loss days per case and the average severity score per case.
Risk factor analyses
Information on the following potential risk factors was obtained from the baseline questionnaire: age, sex, previous injury, osteoarthritis, golfing handicap (dichotomised as ‘less than 6’ or ‘6 or higher’ as per the International Golf Federation consensus statement definition of subelite golfers),25 average number of days playing golf per week, whether the player performed a warm-up prior to playing golf and whether the player performed specific injury prevention training. Associations between these variables and injury were analysed in R using the Ime4 package.31 Potential risk factors were entered into univariate generalised linear mixed-effects models with injury as the dependent variable and time as a fixed effect. All factors that were found to have a significant association with injury in univariate analyses were included in a multivariable model. The results are reported as OR with a 95% CI.
Results
Response rate to weekly questionnaires
We distributed 19 406 questionnaires and received 11 180 responses (57.6%). The average weekly response rate for the USA was 50.7% and Switzerland was 91.9% during the 5-month study period.
Participant characteristics
The median age was 60 (IQR: 47–67) and the median age to start playing golf was 20 years (IQR: 12–35) with the majority being right-handed (n=831; 92.7%). The median golfing handicap was 12 (IQR: 6–18). Most golfers (n=730; 81.5%) classified themselves as recreational players, 155 (17.3%) as subelite (PGA teaching professionals, amateurs competing in regional/county/state tournaments or with handicap 5 or less), and 11 (1.2%) as elite (amateurs competing in international/national amateur championships).
Prior to the study, participants reported the mean number of rounds of golfing per week was 2.3 (SD=1.3) and the median number of holes played was 36 (IQR: 18–54). The median number of balls hit on the driving range per week was 100 (IQR: 65–200) while the median number of hours per week used for golf-related fitness was 3 (IQR: 2–5). Injury prevention was performed in 44.5% (n=335) of the study population and 91.5% (n=689) performed a golf warm-up prior to playing.
Prevalence of injuries, illnesses and health problems
The overall prevalence of health problems during the study period was 13% (95% CI 11.4 to 14.6). Prevalence of injuries was 11.3% (95% CI 9.8 to 12.8). The prevalence of illnesses was 2% (95% CI 1.7 to 2.2). The onset of injuries and illnesses and their substantiality can be seen in table 1.
Table 1. Prevalence of health problems.
| Females (95% CI) | Males (95% CI) | Both sexes (95% CI) | |
| All health problems | 14.1 (12.1 to 16.1) | 12.7 (11.2 to 14.3) | 13 (11.4 to 14.6) |
| All injuries | 10.7 (9.1 to 12.3) | 11.5 (10.0 to 13.0) | 11.3 (9.8 to 12.8) |
| All sudden-onset injuries | 4.1 (3.0 to 5.3) | 5.0 (4.2 to 5.7) | 4.8 (4.0 to 5.6) |
| All gradual-onset injuries | 7.0 (6.3 to 7.8) | 6.7 (5.9 to 7.5) | 6.8 (6.0 to 7.5) |
| All illness | 4.5 (3.5 to 5.4) | 1.3 (1.1 to 1.6) | 2.0 (1.7 to 2.2) |
| Substantial health problems | 5.7 (4.8 to 6.6) | 5.8 (5.2 to 6.4) | 5.8 (5.1 to 6.4) |
| Substantial injuries | 3.3 (2.7 to 4) | 4.9 (4.3 to 5.4) | 4.6 (4.0 to 5.1) |
| Substantial sudden-onset injuries | 1.6 (1.1 to 2) | 2.7 (2.2 to 3.1) | 2.4 (2.0 to 2.9) |
| Substantial gradual-onset injuries | 1.8 (1.3 to 2.2) | 2.3 (2.0 to 2.5) | 2.2 (1.9 to 2.4) |
| Substantial illness | 2.6 (2.0 to 3.2) | 1 (0.8 to 1.2) | 1.3 (1.1 to 1.5) |
Incidence and severity of injuries, illnesses and health problems
There were 4.73 (95% CI 4.44 to 5.02) health problems per golfer per year. The incidence of injuries and illnesses was 3.79 (95% CI 3.54 to 4.06) and 0.94 (95% CI 0.81 to 1.07) per golfer per year, respectively. The number of injuries by body parts and the related median severity of complaints is presented in table 2. The injury burden by anatomical location can be seen in figure 1.
Table 2. Injury incidence, severity and burden.
| Sex | Cases (n) | Incidence (95% CI) | Median time loss (25th–75th percentile) | Burden | |
| All health problems | Both sexes | 996 | 4.73 (4.44 to 5.02) | 2 (0–5) | 24.15 |
| Male | 760 | 4.64 (4.32 to 4.98) | 2 (0–6) | 23.73 | |
| Female | 236 | 5.01 (4.4 to 5.68) | 1.5 (0–4) | 25.62 | |
| Sudden-onset injury | Both sexes | 345 | 1.64 (1.47 to 1.81) | 2 (0–6) | 10.40 |
| Gradual-onset injury | Both sexes | 454 | 2.15 (1.96 to 2.36) | 1 (0–3) | 7.88 |
| Illness | Both sexes | 197 | 0.94 (0.81 to 1.07) | 3 (1–7) | 5.90 |
| Head | Both sexes | 4 | 0.02 (0.01 to 0.05) | 3.5 (0–8.75) | 0.11 |
| Neck | Both sexes | 39 | 0.19 (0.14 to 0.25) | 0 (0–2.5) | 0.40 |
| Shoulder | Both sexes | 69 | 0.33 (0.25 to 0.41) | 1 (0–6) | 3.47 |
| Upper arm | Both sexes | 6 | 0.03 (0.01 to 0.06) | 1.5 (0.25–2) | 0.05 |
| Elbow | Both sexes | 50 | 0.24 (0.18 to 0.31) | 0 (0–2) | 0.95 |
| Forearm | Both sexes | 17 | 0.08 (0.05 to 0.12) | 1 (0–3) | 0.58 |
| Wrist | Both sexes | 26 | 0.12 (0.08 to 0.18) | 0 (0–1.75) | 0.27 |
| Hand | Both sexes | 32 | 0.15 (0.1 to 0.21) | 0 (0–3.5) | 0.61 |
| Thoracic spine | Both sexes | 47 | 0.22 (0.17 to 0.3) | 1 (0–5) | 0.68 |
| Lumbosacral spine | Both sexes | 265 | 1.26 (1.11 to 1.41) | 2 (0–5) | 5.93 |
| Abdomen | Both sexes | 11 | 0.05 (0.03 to 0.09) | 1 (0–2.5) | 0.13 |
| Hip/groin | Both sexes | 53 | 0.25 (0.19 to 0.33) | 1 (0–3) | 0.77 |
| Thigh | Both sexes | 17 | 0.08 (0.05 to 0.12) | 2 (0–10) | 0.41 |
| Knee | Both sexes | 82 | 0.39 (0.31 to 0.48) | 1 (0–4) | 2.08 |
| Lower leg | Both sexes | 10 | 0.05 (0.03 to 0.08) | 2.5 (0–4) | 0.13 |
| Ankle | Both sexes | 16 | 0.08 (0.05 to 0.12) | 3 (0–8.25) | 0.50 |
| Foot | Both sexes | 46 | 0.22 (0.16 to 0.29) | 2 (0–4) | 0.97 |
| Region unspecified | Both sexes | 9 | 0.04 (0.02 to 0.08) | 3 (1–5) | 0.28 |
Figure 1. Risk matrix depicting the relationship between incidence (number of injuries per athlete per year) and severity (average cumulative severity score) of the six anatomical locations with the highest overall burden. Darker shades of background indicate a higher injury burden error bars represent 95% CIs.
Risk factors associated with injury
Univariate regression analysis revealed that injury was associated with increasing age, osteoarthritis, previous injury and undertaking injury prevention exercises. Sex, golfing frequency, warm-up and handicap were not associated with injury (table 3). Following multivariate analysis (age, osteoarthritis, previous injury and injury prevention exercises), all associations remained significant (table 4).
Table 3. Univariate logistic regression analysis of factors associated with injury.
| Independent variable | OR | 95% CI | P value |
| Age (per 10 years) | 1.02 | 1.01 to 1.03 | <0.001 |
| Male sex | 1.13 | 0.67 to 1.89 | 0.646 |
| Golf days per week | 1.05 | 0.85 to 1.29 | 0.654 |
| Osteoarthritis | 3.30 | 1.94 to 5.61 | <0.001 |
| Warm-up | 1.29 | 0.58 to 2.87 | 0.529 |
| Previous injury | 3.29 | 2.05 to 5.28 | <0.001 |
| Injury prevention | 3.97 | 2.57 to 6.14 | <0.001 |
| Handicap <6 | 1.00 | 1.00 to 1.00 | 0.549 |
Table 4. Multivariate regression analysis including significant independent variables.
| Independent variable | OR | 95% CI | P value |
| Age | 1.03 | 1.01 to 1.04 | 0.002 |
| Osteoarthritis | 1.97 | 1.16 to 3.35 | 0.013 |
| Previous injury | 2.32 | 1.46 to 3.68 | <0.001 |
| Injury prevention | 3.13 | 2.05 to 4.78 | <0.001 |
Discussion
This study is the first to prospectively analyse health complaints during the season using the IGF guidelines for reporting of injuries and illnesses in the amateur golfing population. We found injury and illness rates to be similar or lower compared with those reported in many other sports. Injuries located at the lumbosacral spine, knee and shoulder had both the highest incidence and burden. Injuries were associated with increasing age, previous injury and osteoarthritis. We found no association between the self-reported number of days playing golf per week in the previous season and injury.
Since the publication of the IGF guidelines on reporting of injuries and illnesses in golf, this is the first study to apply the methodology in a prospective way on a large cohort. As golfing participation continues to grow, it is important that well-performed research into the sport is undertaken using comparable processes. Furthermore, golf’s contribution to population-level physical activity increases with age32 and as we have shown age to be a correlating factor with injury, therefore, clear understanding of golf injuries may lead to improved playing longevity and subsequently physical activity. A recent retrospective study showed musculoskeletal complaints in recreational male players to be comparable to injury complaints in the general population.26 It is possible that this reflects participants reporting the musculoskeletal complaints that occurred taking part in daily life and other activities in addition to those sustained playing golf. When comparing the prevalence of injuries to other non-contact recreational sports using comparable methods, the results of this study suggest injury rates are substantially lower.33,35 In regard to the incidence of injuries in other non-contact, recreational sports such as running and tennis, rates of injury appear to be lower compared in our study.36 37
The findings of our study do not pertain to touring professional golfers. A previous study of the incidence of injury and illness of professional athletes at the Tokyo 2020 Olympics found golfers to have a surprisingly high rate of health problems.38 Golf had the highest rate of health problems of any non-contact sports over the 17-day period with an injury prevalence of 15% and illness prevalence of 6%. The relatability of these findings to the current study is limited by their professional athlete population and short study period.
This study is the first to report injury burden among golfers. Previous expert opinion has described the benefits of reporting injury burden in addition to incidence and time loss.30 39 The two concepts can be combined in a risk matrix as seen in figure 1 to give the relative importance of each injury. This has previously been used a number of times in a variety of sports including rugby, athletics, ice hockey and para-sports.3540,42 In this current study, we found the lumbosacral spine injuries to have both the highest incidence and burden. Knee and shoulder injuries were the next two most burdensome injuries. However, despite a higher incidence compared with shoulder injuries, knee injuries had a lower burden. Furthermore, sudden-onset injuries, despite being much less common, had a higher burden compared with gradual-onset injuries. Using the risk matrix demonstrated, researchers and clinicians involved in golf can focus their attention on reducing the most burdensome musculoskeletal complaints, identify when injury risk is at its highest and assess the impact of sudden-onset vs gradual-onset injuries.
The lumbosacral spine was the most common location of injury in recreational golfers in our study. This aligns with previous research, where lumbosacral pain has been found to contribute to 35% of all golf-related injuries9 30 and this is likely related to the high forces subjected to the back during the swing, as well as low back pain being a frequent complaint in daily life.43 Knee and shoulder injuries were found to be the second and third most prevalent locations of injuries in golfers in previous cross-sectional research published.26 The golf literature has previously shown that elbow injuries are the second most common injuries in amateur golfers.44 45 However, we found this to be only the fourth most common injury in this current study.
Most studies identify the volume of repetitive practice and suboptimal swing biomechanics as potential underlying causes of injuries in amateur players.45 46 We did not explore swing biomechanics in this study; however, we found no correlation between days per week playing golf and injury incidence. To fully elucidate the relationship between golf playing load and injury, studies specifically targeting this research question are necessary. We found that performing injury prevention exercises to be an independent risk factor for sustaining an injury. This association is surprising but may be at least partially related to the possibility that those who perform injury prevention exercises have sustained a previous injury and therefore, are more likely to sustain a subsequent injury.
The methods used in this study should have value if explored in elite golfers. Such methods including injury burden have been successfully applied in other fields of elite sport41 47 and if applied to golf, would add a great deal of understanding to the injury patterns as well as health problems sustained in this cohort of players.
Limitations
The study population contained a relatively high-level skill with a mean handicap lower than the world average. Furthermore, the average amount of golf played (both holes and driving range activity) is perhaps higher than what would be typical of the wider population of golfers. In addition, there was a high percentage of participants performing injury prevention exercises compared with previous studies.26 Therefore, this may suggest the current study population’s volume of golf and preparation is not typical of the overall golfing population. This study was performed over a 5-month period, a typical playing season, and therefore, extrapolations have been made as to the injury incidence over the course of an entire year. In addition, the study size was not powered to a particular outcome measure. The response rate of our study was 57.6% and therefore, non-response bias is possible. However, research has reported the reliability and validity of prevalence data being unsubstantially affected with response rates as low as 18%.48
The risk factors used in this study were self-reported, including playing load (ie, the number of days playing golf per week in the previous season). Previous studies have reported challenges in measuring load. We used self-reported injuries and illnesses in this study and recorded self-reported playing load. A previous study on elite cricketers showed poor validity between self-reported and independently observed throwing volume. There were 78% of players who had a level of error >10%.49 Furthermore, golfing handicap was not significant as a risk factor for injury, despite previous studies reporting increased injuries with elite players compared with amateurs.44 We did not record the nature of practice surfaces in this study. Some clinicians believe the nature of playing surfaces is associated with golfing-related injuries. This was not captured in the present study but may be worthwhile capturing in future work. Further, only two countries were included and future work may benefit from wider international data collection to analyse the spectrum of playing surfaces.
Using time loss as a measure of severity has some shortcomings. For example, long-term consequences beyond those directly related to golfing participation are not captured that is, later disability. In addition, it does not account for injuries where there is no time loss, but that may still limit athlete performance significantly, which is often the case for overuse injuries. This is particularly important in the case of high-level amateur golfers who may be keen to compete despite having ongoing injuries. This was mitigated in our study by using severity score from OSTRC which allowed us to quantify non-time-loss-related consequences. Finally, the side of injury was not recorded in this study. With differences in incidence of injuries in the lead and trail side of injuries, it would be helpful for future studies to record this.
Lower back pain is known to be a common complaint of the general population. We did not use a non-golfing control cohort to compare rates of lower back pain to the general population. This limits our confidence of the association between lower back injuries and its relationship to golf. However, previous studies have shown lower back pain to be higher in athletes50 and previous biomechanical data has shown compressive forces in the back during the golf swing to be eight times body weight.43 Mental health was not covered in the golf-specific statement and therefore, not reported in this study. However, we know the burden is high in professional golf51 and this has also been reported in elite amateur golf with 32.5% of players reporting mental health problems in the 4 weeks preceding a world championship.52 Further research should consider including guidance from the recent consensus statement on surveillance of mental health symptoms and disorders in athletes.53
Conclusions
This is the first large prospective study to use the IGF reporting guidelines on injuries and illnesses in amateur golfers. The prevalence and incidence of injuries in amateur golf were lower compared with other similar sports. The lumbosacral spine, knee and shoulder were the anatomical locations with the highest incidence and burden of injury. Given the growing popularity of golf and the large number of players globally, researchers and clinicians should focus their attention on investigating the areas creating the greatest burden for players to further prevent injuries.
supplementary material
Acknowledgements
The group acknowledge assistance in data collection from the Titleist Performance Institute and the use of FITStats technology.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Consent obtained directly from patient(s).
Ethics approval: This study involves human participants and ethical approval was granted by the Ethical Committee of Canton Zurich on 14 May 2020 (BASEC Nr.; 2020-00477) and by Belmont University Institutional Review Board, protocol 1112 from 26 April 2021. Participants gave informed consent to participate in the study before taking part.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Author note: Equity, diversity and inclusion statement: Our authorship represents a multi-national group with researchers ranging from early stage to senior. We have both male and female genders represented. Our study population covers diversity through age, gender, demographics and comorbidities. We hope this study of the sport of golf demonstrates the efforts made to present golf as an inclusive and accessible sport to all interested players.
Contributor Information
Patrick Gordon Robinson, Email: patrick.robinson321@gmail.com.
Benjamin Clarsen, Email: ben.clarsen@nih.no.
Andrew Murray, Email: docandrewmurray@gmail.com.
Astrid Junge, Email: astrid.junge@medicalschool-hamburg.de.
Margo Lynn Mountjoy, Email: mountjm@mcmaster.ca.
Tomas Drobny, Email: tomas.drobny@kws.ch.
Lance Gill, Email: lance@lgperformance.com.
Francois Gazzano, Email: francois@athletemonitoring.com.
Mike Voight, Email: mike.voight@belmont.edu.
Jiri Dvorak, Email: Jiri@dvorakmedical.com.
Data availability statement
Data are available upon reasonable request.
References
- 1.The R&A Record numbers now playing golf worldwide. 2021. [01-May-2022]. https://www.randa.org/en/news/2021/12/record-numbers-now-playing-golf-worldwide Available. Accessed.
- 2.The R&A Golf around the world. The Royal and Ancient. 2019. [12-Jun-2023]. https://www.randa.org/News/2019/02/New-Golf-Around-the-World-Report-Published Available. Accessed.
- 3.National Golf Federation Participation and engagement rise again. 2022. [04-Jan-2023]. https://www.ngf.org/participation-and-engagement-rise-again/ Available. Accessed.
- 4.Robinson PG, Foster C, Murray A. Public health considerations regarding golf during the COVID-19 pandemic: a narrative review. BMJ Open Sport Exerc Med. 2021;7:e001089. doi: 10.1136/bmjsem-2021-001089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson PG, Murray A, Close G, et al. Assessing the risk of SARS-CoV-2 transmission in international professional golf. BMJ Open Sport Exerc Med. 2021;7:e001109. doi: 10.1136/bmjsem-2021-001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray AD, Daines L, Archibald D, et al. The relationships between golf and health: a scoping review. Br J Sports Med. 2017;51:12–9. doi: 10.1136/bjsports-2016-096625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farahmand B, Broman G, de Faire U, et al. Golf: a game of life and death--reduced mortality in Swedish golf players. Scand J Med Sci Sports. 2009;19:419–24. doi: 10.1111/j.1600-0838.2008.00814.x. [DOI] [PubMed] [Google Scholar]
- 8.Parkkari J, Natri A, Kannus P, et al. A controlled trial of the health benefits of regular walking on a golf course. Am J Med. 2000;109:102–8. doi: 10.1016/s0002-9343(00)00455-1. [DOI] [PubMed] [Google Scholar]
- 9.Parkkari J, Kannus P, Natri A, et al. Active living and injury risk. Int J Sports Med. 2004;25:209–16. doi: 10.1055/s-2004-819935. [DOI] [PubMed] [Google Scholar]
- 10.McHardy A, Pollard H, Luo K. One-year follow-up study on golf injuries in Australian amateur golfers. Am J Sports Med. 2007;35:1354–60. doi: 10.1177/0363546507300188. [DOI] [PubMed] [Google Scholar]
- 11.Soligard T, Steffen K, Palmer D, et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic summer games: a prospective study of 11274 athletes from 207 countries. Br J Sports Med. 2017;51:1265–71. doi: 10.1136/bjsports-2017-097956. [DOI] [PubMed] [Google Scholar]
- 12.Robinson PG, Murray IR, Duckworth AD, et al. Systematic review of musculoskeletal injuries in professional golfers. Br J Sports Med. 2019;53:13–8. doi: 10.1136/bjsports-2018-099572. [DOI] [PubMed] [Google Scholar]
- 13.Thériault G, Lachance P. Golf injuries. Sports Med . 1998;26:43–57. doi: 10.2165/00007256-199826010-00004. [DOI] [PubMed] [Google Scholar]
- 14.Barclay C, West S, Shoaib Q, et al. Injuries patterns among professional golfers: an international survey. Br J Sports Med. 2011;45:e1. doi: 10.1136/bjsm.2010.081554.12. [DOI] [Google Scholar]
- 15.Orchard JW, Ranson C, Olivier B, et al. International consensus statement on injury surveillance in cricket: a 2016 update. Br J Sports Med. 2016;50:1245–51. doi: 10.1136/bjsports-2016-096125. [DOI] [PubMed] [Google Scholar]
- 16.Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med. 2006;16:97–106. doi: 10.1097/00042752-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Fuller CW, Molloy MG, Bagate C, et al. Consensus statement on injury definitions and data collection procedures for studies of injuries in rugby union. Clin J Sport Med. 2007;17:177–81. doi: 10.1097/JSM.0b013e31803220b3. [DOI] [PubMed] [Google Scholar]
- 18.King DA, Gabbett TJ, Gissane C, et al. Epidemiological studies of injuries in rugby league: suggestions for definitions, data collection and reporting methods. J Sci Med Sport. 2009;12:12–9. doi: 10.1016/j.jsams.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Mountjoy M, Junge A, Alonso JM, et al. Consensus statement on the methodology of injury and illness surveillance in FINA (aquatic sports) Br J Sports Med. 2016;50:590–6. doi: 10.1136/bjsports-2015-095686. [DOI] [PubMed] [Google Scholar]
- 20.Pluim BM, Fuller CW, Batt ME, et al. Consensus statement on epidemiological studies of medical conditions in tennis, April 2009. Br J Sports Med. 2009;43:893–7. doi: 10.1136/bjsm.2009.064915. [DOI] [PubMed] [Google Scholar]
- 21.Timpka T, Alonso J-M, Jacobsson J, et al. Injury and illness definitions and data collection procedures for use in epidemiological studies in athletics (track and field): consensus statement. Br J Sports Med. 2014;48:483–90. doi: 10.1136/bjsports-2013-093241. [DOI] [PubMed] [Google Scholar]
- 22.Turner M, Fuller CW, Egan D, et al. European consensus on epidemiological studies of injuries in the thoroughbred horse racing industry. Br J Sports Med. 2012;46:704–8. doi: 10.1136/bjsports-2011-090312. [DOI] [PubMed] [Google Scholar]
- 23.Dvorak J, Pluim BM. Injury and illness surveillance in sports: how golf, tennis, cycling and parasport extended the IOC consensus statement to tailor injury and illness surveillance to specific sports. Br J Sports Med. 2021;55:6–7. doi: 10.1136/bjsports-2020-102616. [DOI] [PubMed] [Google Scholar]
- 24.Bahr R, Clarsen B, Derman W, et al. International Olympic committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE extension for sport injury and illness surveillance (STROBE-SIIS)) Br J Sports Med. 2020;54:372–89. doi: 10.1136/bjsports-2019-101969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray A, Junge A, Robinson PG, et al. International consensus statement: methods for recording and reporting of epidemiological data on injuries and illnesses in golf. Br J Sports Med. 2020;54:1136–41. doi: 10.1136/bjsports-2020-102380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray A, Junge A, Robinson PG, et al. Cross-sectional study of characteristics and prevalence of musculoskeletal complaints in 1170 male golfers. BMJ Open Sport Exerc Med . 2023;9:e001504. doi: 10.1136/bmjsem-2022-001504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clarsen B, Rønsen O, Myklebust G, et al. The Oslo Sports Trauma Research Center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. 2014;48:754–60. doi: 10.1136/bjsports-2012-092087. [DOI] [PubMed] [Google Scholar]
- 28.Clarsen B, Bahr R, Myklebust G, et al. Improved reporting of overuse injuries and health problems in sport: an update of the Oslo Sport Trauma Research Center questionnaires. Br J Sports Med. 2020;54:390–6. doi: 10.1136/bjsports-2019-101337. [DOI] [PubMed] [Google Scholar]
- 29.Bahr R, Clarsen B, Derman W, et al. International Olympic committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 (including the STROBE extension for sports injury and illness surveillance (STROBE-SIIS)) Orthop J Sports Med. 2020;8:2325967120902908. doi: 10.1177/2325967120902908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. 2018;52:1018–21. doi: 10.1136/bjsports-2017-098160. [DOI] [PubMed] [Google Scholar]
- 31.Bates D, Mächler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Stats Software. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 32.Strain T, Fitzsimons C, Foster C, et al. Age-related comparisons by sex in the domains of aerobic physical activity for adults in Scotland. Prev Med Rep. 2016;3:90–7. doi: 10.1016/j.pmedr.2015.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aasheim C, Stavenes H, Andersson SH, et al. Prevalence and burden of overuse injuries in elite junior handball. BMJ Open Sport Exerc Med . 2018;4:e000391. doi: 10.1136/bmjsem-2018-000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson A, Clarsen B, Verhagen EALM, et al. High prevalence of self-reported injuries and illnesses in talented female athletes. BMJ Open Sport Exerc Med. 2017;3:e000199. doi: 10.1136/bmjsem-2016-000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mann RH, Clarsen BM, McKay CD, et al. Prevalence and burden of health problems in competitive adolescent distance runners: a 6-month prospective cohort study. J Sports Sci. 2021;39:1366–75. doi: 10.1080/02640414.2021.1874160. [DOI] [PubMed] [Google Scholar]
- 36.Pluim BM, Clarsen B, Verhagen E. Injury rates in recreational tennis players do not differ between different playing surfaces. Br J Sports Med. 2018;52:611–5. doi: 10.1136/bjsports-2016-097050. [DOI] [PubMed] [Google Scholar]
- 37.Buist I, Bredeweg SW, Bessem B, et al. Incidence and risk factors of running-related injuries during preparation for a 4-mile recreational running event. Br J Sports Med. 2010;44:598–604. doi: 10.1136/bjsm.2007.044677. [DOI] [PubMed] [Google Scholar]
- 38.Soligard T, Palmer D, Steffen K, et al. New sports, COVID-19 and the heat: sports injuries and illnesses in the Tokyo 2020 summer Olympics. Br J Sports Med. 2022 doi: 10.1136/bjsports-2022-106155. [DOI] [PubMed] [Google Scholar]
- 39.Fuller CW. Injury risk (burden), risk matrices and risk contours in team sports: a review of principles, practices and problems. Sports Med. 2018;48:1597–606. doi: 10.1007/s40279-018-0913-5. [DOI] [PubMed] [Google Scholar]
- 40.Brooks JHM, Fuller CW, Kemp SPT, et al. Epidemiology of injuries in english professional rugby union: part 1 match injuries. Br J Sports Med. 2005;39:757–66. doi: 10.1136/bjsm.2005.018135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nordstrøm A, Bahr R, Clarsen B, et al. Prevalence and burden of self-reported health problems in junior male elite ice hockey players: a 44-week prospective cohort study. Am J Sports Med. 2021;49:3379–85. doi: 10.1177/03635465211032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clarsen B, Steffen K, Berge HM, et al. Methods, challenges and benefits of a health monitoring programme for Norwegian Olympic and paralympic athletes: the road from London 2012 to Tokyo 2020. Br J Sports Med. 2021;55:1342–9. doi: 10.1136/bjsports-2020-103717. [DOI] [PubMed] [Google Scholar]
- 43.Cole MH, Grimshaw PN. The biomechanics of the modern golf swing: implications for lower back injuries. Sports Med. 2016;46:339–51. doi: 10.1007/s40279-015-0429-1. [DOI] [PubMed] [Google Scholar]
- 44.Gosheger G, Liem D, Ludwig K, et al. Injuries and overuse syndromes in golf. Am J Sports Med. 2003;31:438–43. doi: 10.1177/03635465030310031901. [DOI] [PubMed] [Google Scholar]
- 45.McCarroll JR, Rettig AC, Shelbourne KD. Injuries in the amateur golfer. Phys Sportsmed. 1990;18:122–6. doi: 10.1080/00913847.1990.11709999. [DOI] [PubMed] [Google Scholar]
- 46.McCarroll JR. The frequency of golf injuries. Clin Sports Med. 1996;15:1–7. [PubMed] [Google Scholar]
- 47.Kelly S, Pollock N, Polglass G, et al. Injury and illness in elite athletics: a prospective cohort study over three seasons. Int J Sports Phys Ther. 2022;17:420–33. doi: 10.26603/001c.32589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mealing NM, Banks E, Jorm LR, et al. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med Res Methodol. 2010;10:26. doi: 10.1186/1471-2288-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoyne ZG, Cripps AJ, Mosler AB, et al. Self-reported throwing volumes are not a valid tool for monitoring throwing loads in elite Australian cricket players: an observational cohort study. J Sci Med Sport. 2022;25:845–9. doi: 10.1016/j.jsams.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 50.Trompeter K, Fett D, Platen P. Prevalence of back pain in sports: a systematic review of the literature. Sports Med. 2017;47:1183–207. doi: 10.1007/s40279-016-0645-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hopley G, Murray A, MacPherson AC. The prevalence of symptoms of common mental disorders among professional golfers. Int J Golf Sci. 2022:1–14. [Google Scholar]
- 52.Mountjoy M, Schamasch P, Murray A, et al. Inequities in the training environment and health of female golfers participating in the 2022 International golf federation world amateur team championships. Clin J Sport Med. 2024;34:127–34. doi: 10.1097/JSM.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 53.Mountjoy M, Junge A, Bindra A, et al. Surveillance of athlete mental health symptoms and disorders: a supplement to the International Olympic committee’s consensus statement on injury and illness surveillance. Br J Sports Med. 2023;57:1351–60. doi: 10.1136/bjsports-2022-106687. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.


