Abstract
ABSTRACT
Objective
To examine the relationship between schizophrenia, antipsychotic medication adherence and driver responsibility for motor vehicle crash.
Design
Retrospective observational cohort study using 20 years of population-based administrative health and driving data.
Setting
British Columbia, Canada.
Participants
Licensed drivers who were involved in a police-attended motor vehicle crash in British Columbia over a 17-year study interval (2000–16).
Exposures
Incident schizophrenia was identified using hospitalisation and physician services data. Antipsychotic adherence was estimated using prescription fill data to calculate the ‘medication possession ratio’ (MPR) in the 30 days prior to crash.
Primary outcome measures
We deemed drivers ‘responsible’ or ‘non-responsible’ for their crash by applying a validated scoring tool to police-reported crash data. We used logistic regression to evaluate the association between crash responsibility and exposures of interest.
Results
Our cohort included 808 432 drivers involved in a police-attended crash and for whom crash responsibility could be established. In total, 1689 of the 2551 drivers with schizophrenia and 432 430 of the 805 881 drivers without schizophrenia were deemed responsible for their crash, corresponding to a significant association between schizophrenia and crash responsibility (66.2% vs 53.7%; adjusted OR (aOR), 1.67; 95% CI, 1.53 to 1.82; p<0.001). The magnitude of this association was modest relative to established crash risk factors (eg, learner license, age ≥65 years, impairment at time of crash). Among the 1833 drivers with schizophrenia, near-optimal antipsychotic adherence (MPR ≥0.8) in the 30 days prior to crash was not associated with lower crash responsibility (aOR, 1.04; 95% CI, 0.83 to 1.30; p=0.55).
Conclusions
Crash-involved drivers with schizophrenia are more likely to be responsible for their crash, but the magnitude of risk is similar to socially acceptable risk factors such as older age or possession of a learner license. Contemporary driving restrictions for individuals with schizophrenia appear to adequately mitigate road risks, suggesting more stringent driving restrictions are not warranted.
Keywords: Schizophrenia & psychotic disorders, EPIDEMIOLOGY, ACCIDENT & EMERGENCY MEDICINE, Driving Under the Influence, GENERAL MEDICINE (see Internal Medicine), Health policy
Strengths and limitations of this study.
This study examined a population-based cohort of 808 432 crash-involved drivers and used real-world data to establish the diagnosis of schizophrenia, to evaluate adherence to prescribed antipsychotics and to assess driver responsibility for crash.
The use of responsibility analysis is a strength because this study design inherently accounts for road exposure (the hours or miles driven per year) as all individuals were driving at the time of their crash.
Study results apply to the clinically relevant group of individuals with schizophrenia who continue to drive.
Study results do not apply to individuals who never drive (eg, institutionalised, lack access to a vehicle, never licensed, license cancelled due to safety violations, illness severity unquestionably makes driving unsafe).
Investigators had incomplete data on schizophrenia severity and lacked data on the specific driving advice provided to each study subject by clinicians or driver licensing authorities.
Introduction
Schizophrenia is a debilitating chronic mental health disorder that afflicts 19.8 million individuals worldwide.1 Typical features include hallucinations, delusions, disorganised behaviour, and chronic impairments in attention, processing speed, memory and judgement.2 Driving simulator studies suggest that schizophrenia is associated with impaired hazard perception, delayed reaction time, unstable lane position and more variable speeds3,5; severe driving impairment is evident in 32% of individuals with untreated schizophrenia.6 7 Driving restrictions for individuals with schizophrenia have the potential to prevent traffic injury, but unnecessarily severe restrictions are likely to intensify existing social and occupational marginalisation of these individuals.8 Surprisingly few studies tell psychiatrists, general practitioners and policymakers how to navigate this trade-off.
Very few epidemiological studies have examined the association between schizophrenia and crash risk. Landmark studies from the 1960s found that crash risks were twofold higher among drivers with major mental illness.9 10 Another American study from the 1960s found that 97 drivers with schizophrenia had a crash rate no different than controls.11 A Swiss study from the 1970s found that 100 individuals with schizophrenia had a crash rate threefold higher than controls.12 A study from the 1980s found that 70 outpatients with schizophrenia reported a similar annual crash risk but lower annual mileage than age-matched controls.13 These studies are small and several decades out-of-date, so modern crash risks among individuals with schizophrenia remain uncertain.14
A few studies suggest that modern antipsychotic medications have the potential to reduce crash risk among individuals with schizophrenia. One study found that 46 individuals with treated psychoses performed as well as healthy controls on a driving simulator.15 Another driving simulator study found 31 patients with treated schizophrenia performed as well as controls in terms of collisions and defensive driving.3 Periods of suboptimal antipsychotic adherence are exceedingly common among individuals with schizophrenia (up to 72% of time-under-treatment), raising the possibility of a fitness-to-drive policy that makes driver licensing conditional on antipsychotic adherence.15,17 However, the driving simulator studies that indirectly support this approach are small, subject to selection bias and may not reflect real-world crash risk.14
Traffic safety evaluations should account for road exposure (the hours or miles driven per year) because a crash risk of ‘1% per year’ implies a very different level of risk for Driver A (who travels 1000 km/year) and for Driver B (who travels 100 000 km/year). Responsibility analysis is a type of case-control study that inherently accounts for unmeasured differences in road exposure.18 19 This study design only includes drivers who are involved in a crash, thereby ensuring all participants were driving at the instant they were enrolled in the study. Police-reported crash data is used to categorise crash-involved drivers as cases (‘responsible’ for contributing to their crash) or controls (‘non-responsible’ for their crash).20 Responsibility analysis assumes factors that increase crash risk will be more prevalent among ‘responsible’ drivers than among ‘non-responsible’ drivers, as has been demonstrated for well-established crash risk factors including alcohol and drug intoxication,21 distraction22 and sleep deprivation.23 Responsibility analyses have been used to evaluate risk factors for traffic collisions in jurisdictions including the USA, Canada, France, Norway and Australia.1823,26 This design may be particularly suited to assessment of crash risks in schizophrenia because the median annual driving distance among individuals with schizophrenia is less than half that of the general population.8 27
To inform clinical decisions about driver fitness, we performed a responsibility analysis that pragmatically focused on driving safety among individuals with schizophrenia who continue to drive. We examined the association between schizophrenia and crash responsibility among all crash-involved drivers. We also examined the association between antipsychotic medication adherence and crash responsibility among the subset of crash-involved drivers with schizophrenia.
Methods
Study cohort
We set our study in British Columbia (BC), a Canadian province with 4.3 million residents at study midpoint. BC’s publicly funded universal health insurance provides eligible residents with access to subsidised prescription medications and a full array of medical care. Our study cohort included all individuals who were involved as a driver in a police-attended crash that occurred in BC between 1 January 2000 and 31 December 2016. We excluded individuals who did not hold a BC driver license in the study interval and excluded drivers who could not be linked to health data. We focused on incident rather than prevalent cases of schizophrenia by excluding crash-involved drivers who had either of the following during a 3-year washout period (1997–99): (a) a hospitalisation or physician visit for schizophrenia or psychosis or (b) an outpatient prescription fill for an antipsychotic medication. By focusing on incident schizophrenia (ie, newly diagnosed in the study interval) and excluding prevalent schizophrenia (ie, diagnosed prior to the study interval), we improved the homogeneity of the exposure, facilitated assessment of whether ‘time since schizophrenia onset’ influenced the relationship between schizophrenia and crash responsibility (important because the clinical features of schizophrenia change over time in a manner that might influence driving safety) and made more explicit the group to whom our results apply.
Data sources
We obtained de-identified individual-level health data from BC’s population-based administrative databases (online supplemental appendix, items S1-S2).19 28 29 We used hospitalisation data and physician billing data to identify drivers’ chronic medical conditions and recent health service use (online supplemental appendix, items S3- S5); prescription data from all community pharmacies in BC to characterise their medication use; census-derived residential neighbourhood median household income as a proxy for individual socioeconomic status; and vital statistics data to identify driver deaths.
We obtained driving data from the Insurance Corporation of British Columbia, the sole provider of driver licensing services and mandatory basic automobile insurance in BC.26 28 30 Data included license type (learner, novice or full); driver’s license issuance, suspension and expiration dates; crash history; traffic contravention history; and the issuance and cancellation dates of motor vehicle insurance policies. We obtained data on all police-attended crashes from the Traffic Accident System (TAS). Police in BC are required to attend all fatal crashes; they typically attend most serious injury crashes and sometimes attend crashes with property damage only. The attending officer completes a structured TAS crash report that includes detailed information on the circumstances of the crash.
Outcome: driver responsibility for crash
We categorised crash-involved drivers as ‘responsible’ or ‘non-responsible’ for their crash using a validated crash responsibility scoring tool that considers seven external factors that potentially contribute to a crash: road type, driving conditions, vehicle condition, unsafe driving actions, contribution from other parties, type of collision and task involved.20 When many external factors contribute to a collision (score ≥16), the responsibility tool concludes the driver could not have reasonably avoided the crash and the driver is deemed ‘non-responsible’. The relative absence of external contributing factors (score ≤13) suggests the driver should have been able to avoid the crash but did not; the driver is thus deemed ‘responsible’ for the crash. Drivers with ‘indeterminate responsibility’ (score 14–15) were excluded from analyses. The scoring tool assesses crash responsibility independent of any determination of financial responsibility for the crash (as established by the insurance industry), any determination of legal responsibility for the crash (as established by criminal or civil courts) and any determination of criminal responsibility for the crash (as established by experts in forensic psychiatry). We used analytic software to algorithmically calculate responsibility scores for all crash-involved drivers. Drivers involved in multiple police-attended crashes over the study interval could contribute more than one set of crash data to the analysis. We assumed each set of crash data was an independent observation because (a) crashes are rare and the vast majority of crash-involved drivers were only involved in a single police-attended crash during the study interval; (b) police complete crash reports for involved drivers without any input from prior crash reports (making crash responsibility independent of the driver’s responsibility for prior crashes); and (c) each driver involved in a crash is scored independently, with no requirement that one driver to be deemed responsible and the others to be deemed non-responsible for the crash.26 28 The term ‘crash-involved drivers’ will hereafter refer to unique driver-crash combinations, each treated as an independent observation.
Exposure for analysis 1: Prior diagnosis of schizophrenia
We identified individuals diagnosed with schizophrenia by applying a validated administrative health data case definition: ≥1 hospital admission or ≥3 physician visits for schizophrenia within 36 months (online supplemental appendix, items S3-S4).31 32 Among individuals meeting this exposure criteria, the date of first hospitalisation or clinic visit for schizophrenia was deemed the diagnosis date. We only considered a crash-involved driver to be exposed if the schizophrenia diagnosis date preceded the crash date.
Analysis 1 used logistic regression to examine the association between crash responsibility (outcome) and a prior diagnosis of schizophrenia (exposure), as for a conventional case-control study. We forced our regression model to include variables with known strong effects on crash risk: driver age and sex; license type; history of crashes and traffic contraventions in a 3-year lookback; and documented impairment by alcohol or drugs at time of crash. We used backward elimination to evaluate other potential confounders: rurality, region and median household income of the driver’s residential neighbourhood; hospitalisations or physician visits for alcohol and other drug use in a 3-year lookback; Charlson Comorbidity Index ≥1; number of years with a full license; crash location; nighttime crash; crash severity; season and calendar year of crash (online supplemental appendix, item S1 and S5). We assessed stability of variable selection over 200 bootstrap resamples using inclusion frequencies and the variance of coefficient estimates.
Exposure for analysis 2: near-optimal antipsychotic adherence
Analysis 2 used the subset of the main study cohort who had (a) a diagnosis of schizophrenia, with a diagnosis date ≥30 days prior to the crash; (b) ≥1 antipsychotic prescription fill after the diagnosis date; and (c) ≥1 antipsychotic prescription fill in the year prior to crash (hereafter termed the ‘adherence cohort’). These criteria sought to exclude individuals whose physician intentionally avoided prescribing antipsychotics because the diagnosis of schizophrenia remained uncertain.
Analysis 2 focused on drivers with schizophrenia and used logistic regression to examine the association between crash responsibility (outcome) and antipsychotic adherence in the 30-day interval leading up to the crash (exposure). We quantified antipsychotic adherence for each individual using the ‘medication possession ratio’ (MPR), a validated measure of medication adherence defined as the number of days of antipsychotic dispensed within a given interval divided by the number of days in that interval.33 We used standard techniques to calculate MPR for the 30-day exposure interval ending on the crash date (online supplemental appendix, item S6).34 We focused on ‘near-optimal’ adherence to antipsychotics, defined as MPR ≥0.8 (suggesting consumption of prescribed antipsychotics on ≥80% of days in the month prior to crash); the referent was ‘suboptimal’ adherence, defined as MPR <0.8.35 Analysis 2 used the same model building process described above for analysis 1.
Additional analyses
We performed exploratory subgroup and sensitivity analyses for both exposures. We also calculated the ‘absolute annual crash rate’ (crashes divided by driver-years) and the ‘responsible crash rate’ (proportion of drivers responsible for crash) for crash-involved drivers with and without a prior diagnosis of schizophrenia.
Research process
Data were deidentified before release to investigators. Data analysis occurred between June and December 2022 using R V.4.0.5. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines. All inferences, opinions and conclusions drawn are those of the authors and do not reflect the opinions or policies of the Data Stewards.
Patient and public involvement
We did not involve patients or the public in the design, conduct, reporting or dissemination of our research.
Results
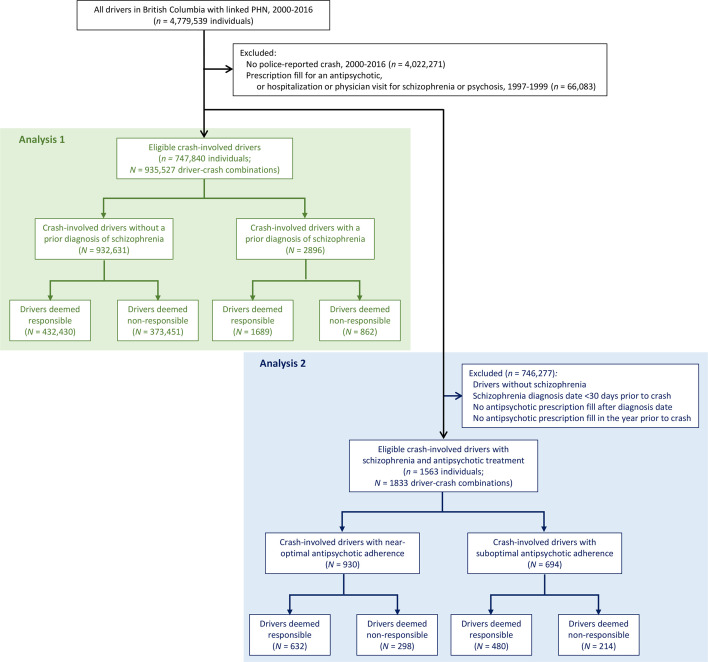
Our final study cohort included 747 840 unique drivers, 612 304 unique crashes and 935 527 unique driver-crash combinations (figure 1; online supplemental appendix, items S7-S8). Crash-involved drivers were predominantly male and had a median age of 39 years; 10% had a police-attended crash and 47% had a traffic contravention in the 3 years prior to index crash (table 1). As expected, the actions of the index driver and the actions of other drivers involved in the crash were the primary determinants of crash responsibility (online supplemental appendix, items S9-S11). Established risk factors for crash that do not directly contribute to the responsibility score were more common among crash-responsible drivers (eg, male sex, younger age, learner or novice license, a history of prior crashes and contraventions, recent medical visits for alcohol or drug use, distracted/inattentive or impaired at the time of crash), supporting the face validity of responsibility analysis (table 1; online supplemental appendix, item S10).
Figure 1. Flow diagram. We focused on individuals with incident schizophrenia by excluding individuals with prevalent schizophrenia, defined as either of the following in a 3-year baseline washout period (1997–99): ≥1 hospitalisation or physician visit for schizophrenia or psychosis, or ≥1 antipsychotic prescription fill. We did so to render our cohort more homogeneous, to clarify the group to whom our results might apply, and to allow estimation of ‘time since schizophrenia onset’ to understand if the relationship between schizophrenia and crash responsibility changes over the course of the disease. Analysis 1 evaluated crash responsibility among all eligible crash-involved drivers (green-shaded region). Analysis 2 used a subset of the analysis 1 cohort and evaluated crash responsibility among all eligible crash-involved drivers with schizophrenia and prior antipsychotic treatment (blue-shaded region). Among all drivers with a linked PHN, there were 21 280 drivers with a diagnosis of schizophrenia and at least one antipsychotic prescription fill in the study interval. Exclusion criteria were not mutually exclusive. Drivers with indeterminate crash responsibility were excluded between rows 4 and 5 in analysis 1 and between rows 7 and 8 in analysis 2 (not shown). PHN=Provincial Healthcare Number; n indicates unique individuals; N indicates unique driver-crash combinations.
Table 1. Driver characteristics at the time of crash.
| Characteristic | Drivers deemed responsible for crash, count (%)n=434 119 | Drivers deemed non-responsible for crash, count (%)n=374 313 | Drivers with indeterminate responsibility, count (%)n=127 095 | P values, responsible vs non-responsible |
| Median age (Q1, Q3) (years) | 37 (23, 52) | 40 (28, 52) | 40 (27, 53) | <0.001 |
| Age categories | <0.001 | |||
| ≤20 years | 73 042 (16.8%) | 35 696 (9.5%) | 12 792 (10.1%) | |
| 21 to 44 years | 202 189 (46.6%) | 185 292 (49.5%) | 62 776 (49.4%) | |
| 45 to 64 years | 107 132 (24.7%) | 120 604 (32.2%) | 39 026 (30.7%) | |
| ≥65 years | 51 756 (11.9%) | 32 721 (8.7%) | 12 501 (9.8%) | |
| Male sex | 283 487 (65.3%) | 233 001 (62.2%) | 80 882 (63.6%) | <0.001 |
| Residential neighbourhood household income quintile | <0.001 | |||
| 1 (lowest income) | 82 859 (19.1%) | 67 265 (18%) | 23 573 (18.5%) | |
| 2 | 86 632 (20%) | 73 955 (19.8%) | 25 944 (20.4%) | |
| 3 | 85 237 (19.6%) | 74 453 (19.9%) | 25 207 (19.8%) | |
| 4 | 84 086 (19.4%) | 75 530 (20.2%) | 25 161 (19.8%) | |
| 5 (highest income) | 76 160 (17.5%) | 68 408 (18.3%) | 22 325 (17.6%) | |
| Missing | 19 145 (4.4%) | 14 702 (3.9%) | 4885 (3.8%) | |
| Rural residence | 210 543 (48.5%) | 178 512 (47.7%) | 51 953 (40.9%) | <0.001 |
| ≥1 hospitalisation in prior year | 49 490 (11.4%) | 39 527 (10.6%) | 13 416 (10.6%) | <0.001 |
| ≥7 physician visits in prior year | 20 649 (4.8%) | 14 320 (3.8%) | 5233 (4.1%) | <0.001 |
| Comorbidities | ||||
| Any psychiatric disorder | 25 516 (5.9%) | 17 747 (4.7%) | 6378 (5%) | <0.001 |
| Hypertension | 19 876 (4.6%) | 15 669 (4.2%) | 5515 (4.3%) | <0.001 |
| Alcohol use | 5065 (1.2%) | 2036 (0.5%) | 852 (0.7%) | <0.001 |
| Other drug use | 8117 (1.9%) | 3464 (0.9%) | 1512 (1.2%) | <0.001 |
| Diabetes | 7860 (1.8%) | 5438 (1.5%) | 2038 (1.6%) | <0.001 |
| Active prescriptions at baseline | <0.001 | |||
| 0 or 1 | 351 528 (81.0%) | 307 211 (82.1%) | 103 684 (81.6%) | |
| ≥2 | 82 591 (19.0%) | 67 102 (17.9%) | 23 411 (18.4%) | |
| Medications filled in prior 90 days | ||||
| Quetiapine | 3360 (0.8%) | 1759 (0.5%) | 733 (0.6%) | <0.001 |
| Risperidone | 1127 (0.3%) | 619 (0.2%) | 211 (0.2%) | <0.001 |
| Olanzapine | 660 (0.2%) | 278 (0.1%) | 128 (0.1%) | <0.001 |
| Aripiprazole | 233 (0.1%) | 168 (<0.1%) | 58 (<0.1%) | 0.086 |
| Clozapine | 36 (<0.1%) | 24 (<0.1%) | 5 (<0.1%) | 0.396 |
| Other antipsychotics | 904 (0.2%) | 455 (0.1%) | 189 (0.1%) | <0.001 |
| Benzodiazepines | 28 330 (6.5%) | 18 676 (5.0%) | 6925 (5.4%) | <0.001 |
| Opioids | 34 990 (8.1%) | 26 432 (7.1%) | 9268 (7.3%) | <0.001 |
| Driver licence type | <0.001 | |||
| Learner | 8047 (1.9%) | 2484 (0.7%) | 1213 (1.0%) | |
| Novice | 80 621 (18.6%) | 42 973 (11.5%) | 15 464 (12.2%) | |
| Full | 342 706 (78.9%) | 328 157 (87.7%) | 110 041 (86.6%) | |
| No license | 2745 (0.6%) | 699 (0.2%) | 377 (0.3%) | |
| Active license in prior 3 years | 429 365 (98.9%) | 372 921 (99.6%) | 126 374 (99.4%) | <0.001 |
| Median years with full license | 10.4 | 13.9 | 13.5 | <0.001 |
| Police-attended crash in prior 3 years | 48 207 (11.1%) | 34 783 (9.3%) | 12 340 (9.7%) | <0.001 |
| Any contravention in prior 3 years | 214 693 (49.5%) | 164 796 (44.0%) | 57 685 (45.4%) | <0.001 |
| Alcohol contravention | 34 356 (7.9%) | 16 415 (4.4%) | 6664 (5.2%) | <0.001 |
| Speed contravention | 133 427 (30.7%) | 105 679 (28.2%) | 36 151 (28.4%) | <0.001 |
| Distraction contravention | 6508 (1.5%) | 6165 (1.6%) | 2365 (1.9%) | <0.001 |
Our sample included 935 527 driver-crash combinations, of which 46% were deemed responsible for the crash and 2896 (0.31%) had a diagnosis of schizophrenia prior to the crash. Drivers with indeterminate responsibility were not included in analyses and are presented here for descriptive purposes only. Relative to non-responsible drivers, crash -responsible drivers were younger and more likely to have a novice driver’s license, recent medical visits for alcohol and other drug use, recent police-attended crashes, and recent traffic contraventions. The displayed p- values compare responsible drivers to non-responsible drivers. We note that the large sample size may produce p values <0.001 even in the absence of a clinically meaningful difference between groups.
Results for analysis 1: Prior diagnosis of schizophrenia
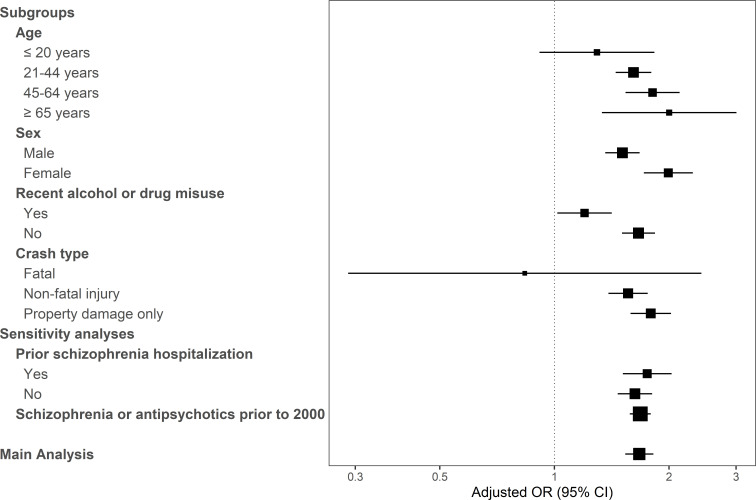
Overall, 434 119 drivers were deemed responsible and 374 313 drivers were deemed non-responsible for their crash; 127 095 had indeterminate crash responsibility and were excluded from further analysis. In total, 1689 of the remaining 2551 drivers with schizophrenia and 432 430 of the remaining 805 881 drivers without schizophrenia were deemed responsible for their crash, corresponding to a modest but significant association between schizophrenia and crash responsibility (66.2% vs 53.7% deemed responsible for their crash, respectively; adjusted odds ratio (aOR), 1.67; 95% CI, 1.53 to 1.82; p≤0.001). Notably, age ≥65 years (aOR 2.04), possession of a learner license (aOR 2.39) and impairment with alcohol or drugs (aOR 5.37) were all stronger predictors of crash responsibility than a diagnosis of schizophrenia (online supplemental appendix, item S12). Subgroup and sensitivity analyses generally supported the conclusions of analysis 1 (figure 2; online supplemental appendix, item S13). Among the 2551 crash-involved drivers with schizophrenia and determinate crash responsibility, the odds of crash responsibility diminished by about 5% per year after schizophrenia onset.
Figure 2. Forest plot of results for key subgroup and sensitivity analyses evaluating the association between schizophrenia and crash responsibility. X-axis depicts the adjusted OR; squares, the point estimate, with size reflecting the inverse of the SE; horizontal lines, the 95% CI. ‘Prior schizophrenia hospitalisation’ indicates the patient had ≥1 hospitalisation for schizophrenia prior to the crash; individuals in our cohort without a prior hospitalisation for schizophrenia met diagnostic criteria prior to crash based on ≥3 physician visits for schizophrenia within 36 months. The sensitivity analysis labelled ‘Schizophrenia or antipsychotics prior to 2000’ indicates that we no longer excluded drivers with a medical visit for schizophrenia or an antipsychotic prescription fill in the washout period (1997–2000), thereby including prevalent schizophrenia and increasing our cohort size to 947 999 crash-involved drivers. The association between schizophrenia and crash responsibility appears to be stronger among female drivers and among drivers without recent visits for drug use but is otherwise reasonably consistent across subgroup and sensitivity analyses.
Results for analysis 2: near-optimal antipsychotic adherence
Over the 17-year study interval, 21 280 drivers with a diagnosis of schizophrenia filled a total of 3.12 million antipsychotic prescriptions (online supplemental appendix, item S14). In the year following the first antipsychotic prescription after schizophrenia diagnosis, 40% of drivers with schizophrenia exhibited near-optimal antipsychotic adherence (online supplemental appendix, item S15).
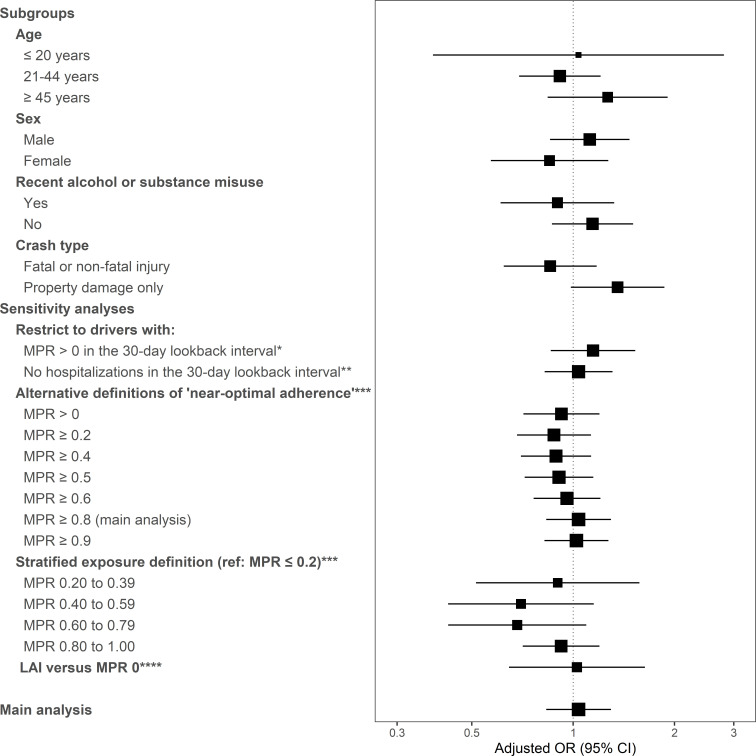
The adherence cohort included 1833 crash-involved drivers with schizophrenia. The median age was 36 years and two thirds were male; in the 3 years prior to crash, one third had a prior visit for non-alcohol drug use, two thirds had a prior traffic contravention and 12% were involved in a prior police-attended crash (table 2). A total of 209 of these drivers were deemed to have indeterminate crash responsibility and were excluded from further analysis. Among the remaining drivers, 632 of 930 drivers with near-optimal antipsychotic adherence and 480 of 694 drivers with suboptimal antipsychotic adherence were deemed responsible for their crash, suggesting no significant relationship between antipsychotic adherence and responsibility for crash among drivers with schizophrenia (68.0% vs 69.2% deemed responsible for their crash, respectively; aOR, 1.04; 95% CI, 0.83 to 1.30; p=0.741; online supplemental appendix, items S16-S18). This null result was consistent among subgroups and robust to changes in the calculation and categorization of MPR (figure 3; online supplemental appendix, item S19).
Table 2. Driver characteristics at the time of crash in the adherence cohort.
| Characteristic | Drivers deemed responsible for crash, count (%)n=1112 | Drivers deemed non-responsible for crash, count (%)n=512 | Drivers with indeterminate responsibility, count (%)n=209 | P values, responsible vs non-responsible |
| Median age (Q1, Q3) (years) | 35 (26, 47) | 36 (28, 46) | 37 (29, 48) | 0.192 |
| Age categories | 0.008 | |||
| ≤20 years | 85 (7.6%) | 33 (6.4%) | 10 (4.8%) | |
| 21 to 44 years | 710 (63.8%) | 332 (64.8%) | 130 (62.2%) | |
| 45 to 64 years | 261 (23.5%) | 138 (27.0%) | 61 (29.2%) | |
| ≥65 years | 56 (5.0%) | 9 (1.8%) | 8 (3.8%) | |
| Male sex | 733 (65.9%) | 362 (70.7%) | 145 (69.4%) | 0.064 |
| Residential neighbourhood household income quintile | 0.132 | |||
| 1 (lowest income) | 327 (29.4%) | 123 (24%) | 55 (26.3%) | |
| 2 | 240 (21.6%) | 106 (20.7%) | 45 (21.5%) | |
| 3 | 185 (16.6%) | 95 (18.6%) | 36 (17.2%) | |
| 4 | 183 (16.5%) | 84 (16.4%) | 32 (15.3%) | |
| 5 (highest income) | 156 (14.0%) | 92 (18.0%) | 37 (17.7%) | |
| Missing | 21 (1.9%) | 12 (2.3%) | <5 | |
| Rural residence | 508 (45.7%) | 223 (43.6%) | 72 (34.4%) | 0.087 |
| ≥1 hospitalisation in prior year | 565 (50.8%) | 184 (35.9%) | 76 (36.4%) | <0.001 |
| ≥7 physician visits in prior year | 237 (21.3%) | 80 (15.6%) | 45 (21.5%) | 0.009 |
| Comorbidities | ||||
| Any psychiatric disorder | 914 (82.2%) | 395 (77.1%) | 154 (73.7%) | 0.020 |
| Hypertension | 46 (4.1%) | 18 (3.5%) | <5 | 0.645 |
| Alcohol use | 138 (12.4%) | 49 (9.6%) | 25 (12%) | 0.114 |
| Other drug use | 369 (33.2%) | 135 (26.4%) | 63 (30.1%) | 0.007 |
| Diabetes | 34 (3.1%) | 18 (3.5%) | 10 (4.8%) | 0.737 |
| Active prescriptions at baseline | 0.417 | |||
| 0 or 1 | 403 (36.2%) | 197 (38.5%) | 82 (39.2%) | |
| ≥2 | 709 (63.8%) | 315 (61.5%) | 127 (60.8%) | |
| Medications filled in prior 90 days | ||||
| Quetiapine | 313 (28.1%) | 118 (23.0%) | 67 (32.1%) | 0.036 |
| Risperidone | 279 (25.1%) | 160 (31.2%) | 51 (24.4%) | 0.011 |
| Olanzapine | 239 (21.5%) | 83 (16.2%) | 45 (21.5%) | 0.016 |
| Aripiprazole | 77 (6.9%) | 35 (6.8%) | 14 (6.7%) | 1.000 |
| Clozapine | 35 (3.1%) | 20 (3.9%) | <5 | 0.524 |
| Other antipsychotics | 162 (14.6%) | 77 (15.0%) | 27 (12.9%) | 0.862 |
| Benzodiazepines | 429 (38.6%) | 156 (30.5%) | 73 (34.9%) | 0.002 |
| Opioids | 163 (14.7%) | 63 (12.3%) | 38 (18.2%) | 0.232 |
| Driver licence type | 0.132 | |||
| Learner | 27 (2.4%) | 10 (2.0%) | <5 | |
| Novice | 203 (18.3%) | 73 (14.3%) | 36 (17.2%) | |
| Full | 876 (78.8%) | 428 (83.6%) | 168 (80.4%) | |
| No license | 6 (0.5%) | <5 | <5 | |
| Active license in prior 3 years | 1092 (98.2%) | 508 (99.2%) | 208 (99.5%) | 0.175 |
| Median years with full license | 11.3 | 12.7 | 11.3 | 0.062 |
| Police-attended crash in prior 3 years | 130 (11.7%) | 70 (13.7%) | 21 (10%) | 0.295 |
| Any contravention in prior 3 years | 661 (59.4%) | 286 (55.9%) | 107 (51.2%) | 0.191 |
| Alcohol contravention | 131 (11.8%) | 45 (8.8%) | 16 (7.7%) | 0.087 |
| Speed contravention | 323 (29.0%) | 124 (24.2%) | 49 (23.4%) | 0.049 |
| Distraction contravention | 32 (2.9%) | 8 (1.6%) | 5 (2.4%) | 0.157 |
Driver characteristics for the 1833 crash-involved drivers in the adherence cohort (schizophrenia diagnosis date ≥30 days prior to the crash; ≥1 antipsychotic prescription fill after the diagnosis date; ≥1 antipsychotic prescription fill in the year prior to crash). The adherence cohort is the subset of the main study cohort that we used to examine the association between antipsychotic adherence and crash responsibility. P- values compare responsible drivers to non-responsible drivers. Drivers with indeterminate responsibility were not included in analyses and are presented here for descriptive purposes only.
Figure 3. Forest plot of results for key subgroup and sensitivity analyses evaluating the association between antipsychotic adherence and crash responsibility among drivers with schizophrenia in the adherence cohort. X-axis depicts the adjusted OR; squares, the point estimate, with size reflecting the inverse of the SE; horizontal lines, the 95% CI. We collapsed some age and crash-type categories because of low sample size and regression model non-convergence. *This sensitivity analysis sought to exclude individuals for whom antipsychotics were intentionally de-prescribed. **Antipsychotics prescribed in hospital do not appear in PharmaNet or any other accessible province-wide data source. This sensitivity analysis sought to evaluate whether this source of bias in calculating medication possession ratio (MPR) influenced our effect estimate. ***These sensitivity analyses suggest there is no ‘threshold MPR’ above which driving safety improves. ****This sensitivity analysis compared drivers who filled a long-acting injectable (LAI) antipsychotic but were not yet due to receive their next dose (implying perfect adherence at the time of crash) to drivers with an MPR of zero. Overall, the lack of association between antipsychotic adherence and crash responsibility appears to be consistent across subgroup and sensitivity analyses.
Additional analyses
As expected, drivers with schizophrenia exhibited a lower absolute annual crash risk but a higher responsible crash rate relative to controls, suggesting drivers with schizophrenia have reduced road exposure relative to controls and highlighting one advantage of responsibility analysis in this population (online supplemental appendix, item S20-S21). Assessment of correlation suggested it was reasonable to treat each driver-crash combination as an independent observation (online supplemental appendix, item S22).
Discussion
Using 20 years of population-based health and driving data for 935 527 drivers involved in police-attended motor vehicle crashes, we found that drivers with schizophrenia were more likely to be responsible for their crash, but that the strength of association was modest relative to conventional traffic safety risk factors such as older age, possession of a learner license, or impairment by alcohol or drugs. Among the subset of 1833 crash-involved drivers with schizophrenia, near-optimal adherence to antipsychotics in the preceding 30 days was not associated with lower crash responsibility.
Taken together, our findings suggest that ‘individuals with schizophrenia who continue to drive’ do not collectively pose a major risk to the driving public. Our findings imply that a 67-year-old male with a recent speeding ticket is, on average, more likely to be responsible for a crash than a 30-year-old female with schizophrenia and a clean driving record. In many jurisdictions, lower but non-zero blood alcohol concentrations that approximately double crash risk (ie, <0.05%) are not subject to any penalty, suggesting societal tolerance of some crash risk factors of the magnitude we observed for schizophrenia.36,38 However, our results should not be misconstrued as a green light for individuals whose mental condition obviously renders them unsafe behind the wheel. Our results apply to individuals with schizophrenia who continue to drive. Our results do not apply to individuals with schizophrenia who never drive (eg, institutionalised, lack access to a vehicle, never licensed, license cancelled due to safety violations, illness severity unquestionably makes driving unsafe). Future research could focus on how to better target driving restrictions, thereby enhancing traffic safety while minimising undue constraints on the mobility of individuals with schizophrenia.
Among individuals with schizophrenia, antipsychotic adherence is associated with gains in employment, improvements in global functioning and reductions in drug use and criminal behaviour.3139,41 It is therefore somewhat surprising that near-optimal antipsychotic adherence was not associated with a lower likelihood of driver responsibility for crash. One explanation posits that somnolence, extrapyramidal symptoms and other adverse drug effects offset the potential driving safety benefits of antipsychotics.19 42 A countervailing explanation argues that the true benefits of antipsychotic adherence are obscured by use of surrogate measures (eg, MPR, crash responsibility) or by misclassification of exposure or outcome.
Our study has many strengths: we focused on road safety in the clinically relevant group of individuals with schizophrenia who continue to drive; we established crash responsibility using objective police crash reports and a validated scoring tool; we used validated case definitions to identify schizophrenia and to estimate antipsychotic adherence; we used multiple sources of health and driving data to control for confounders ignored by many prior studies; we used responsibility analyses to account for road exposure, mitigating a major bias of existing studies; we completed subgroup and sensitivity analyses to examine robustness of results; and we used population-based data to generate findings that can be generalised to many other jurisdictions worldwide. Epidemiological studies of crash risks specific to individuals with schizophrenia appear to include fewer than 257 individuals with schizophrenia in total; the largest study included only 78 drivers with schizophrenia and the most recent was completed in 1989 (online supplemental appendix, item S23).12,14 Our large sample size therefore increases the number of drivers with schizophrenia in the published literature by almost 10-fold.
Our study has several limitations. We included all fatal and most serious injury crashes but were unable to include crashes that were not attended by police. Responsibility scores are calculated using objective crash data, but implicit bias against individuals with schizophrenia might have prejudiced police crash reports. Although prescriptions that are filled may not be consumed and administrative data do not perfectly identify schizophrenia, these forms of exposure misclassification would yield conservative conclusions by biasing ORs toward the null. Confounding by indication might occur if individuals with less symptomatic schizophrenia are prescribed fewer antipsychotics or fewer supports for medication adherence. More adherent individuals might also independently exhibit safer driving habits or less illicit drug use, potentially introducing the healthy user bias. We had incomplete data on schizophrenia severity, alcohol and drug use, and socioeconomic status, but we leveraged multiple linked sources of administrative data to account for prior schizophrenia hospitalisations, prior medical visits for drug use and residential neighbourhood household income. Responsibility analyses include only crash-involved drivers, and our results do not apply to groups of individuals who never drive. The specific driving restrictions and physician driving advice provided to each study subject remain unknown.
Individuals with schizophrenia are subject to widespread stigma and discrimination, resulting in economic marginalisation and social exclusion.43 The modest association we found between schizophrenia and crash responsibility suggests contemporary driving restrictions among individuals with schizophrenia adequately mitigate road risks, and that more stringent driving restrictions are not warranted.
supplementary material
All inferences, opinions and conclusions drawn are those of the authors and do not reflect the opinions or policies of the Data Stewards.
Footnotes
Funding: This study was supported by the Canadian Institutes of Health Research (grant numbers PJT-180343). JS received research salary support from Michael Smith Health Research BC. JB received research salary support from the Michael Smith Health Research BC and the British Columbia Emergency Medicine Network. WH was supported by the Jack Bell Chair in Schizophrenia. Funding organisations were not involved in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review and approval of this manuscript.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-080609).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Data availability free text: Study data provided by the Data Stewards can be requested for other research projects through the Data Stewards or their designated service providers. Access to these data is subject to approval by the Data Stewards. These data are not otherwise publicly available.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics approval: The University of British Columbia Clinical Research Ethics Board approved the study and waived the requirement for individual consent (H12-02678).
Contributor Information
John A Staples, Email: john.staples@ubc.ca.
Daniel Daly-Grafstein, Email: daly-grafstein@stat.ubc.ca.
Mayesha Khan, Email: mayesha.khan@ubc.ca.
Lulu X Pei, Email: lulu.pei@ubc.ca.
Shannon Erdelyi, Email: s.erdelyi@stat.ubc.ca.
Stefanie N Rezansoff, Email: stefanie_rezansoff@sfu.ca.
Herbert Chan, Email: Herbert.chan@ubc.ca.
William G Honer, Email: william.honer@ubc.ca.
Jeffrey R Brubacher, Email: jeff.brubacher@ubc.ca.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marder SR, Cannon TD. Schizophrenia. N Engl J Med. 2019;381:1753–61. doi: 10.1056/NEJMra1808803. [DOI] [PubMed] [Google Scholar]
- 3.Fuermaier ABM, Piersma D, Huntjens RJC, et al. Simulated car driving and its association with cognitive abilities in patients with schizophrenia. Schizophr Res. 2019;204:171–7. doi: 10.1016/j.schres.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 4.St Germain SA, Kurtz MM, Pearlson GD, et al. Driving simulator performance in schizophrenia. Schizophr Res. 2005;74:121–2. doi: 10.1016/j.schres.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Brunnauer A, Laux G, Geiger E, et al. The impact of antipsychotics on psychomotor performance with regards to car driving skills. J Clin Psychopharmacol. 2004;24:155–60. doi: 10.1097/01.jcp.0000116648.91923.82. [DOI] [PubMed] [Google Scholar]
- 6.Segmiller FM, Buschert V, Laux G, et al. Driving skills in unmedicated first- and recurrent-episode schizophrenic patients. Eur Arch Psychiatry Clin Neurosci. 2017;267:83–8. doi: 10.1007/s00406-015-0647-4. [DOI] [PubMed] [Google Scholar]
- 7.Brunnauer A, Laux G, Zwick S. Driving simulator performance and psychomotor functions of schizophrenic patients treated with antipsychotics. Eur Arch Psychiatry Clin Neurosci. 2009;259:483–9. doi: 10.1007/s00406-009-0014-4. [DOI] [PubMed] [Google Scholar]
- 8.Palmer BW, Heaton RK, Gladsjo JA, et al. Heterogeneity in functional status among older outpatients with schizophrenia: employment history, living situation, and driving. Schizophr Res. 2002;55:205–15. doi: 10.1016/s0920-9964(01)00218-3. [DOI] [PubMed] [Google Scholar]
- 9.Waller JA. Chronic medical conditions and traffic safety: review of the California experience. N Engl J Med. 1965;273:1413–20. doi: 10.1056/NEJM196512232732605. [DOI] [PubMed] [Google Scholar]
- 10.Eelkema RC, Brosseau J, Koshnick R, et al. A statistical study on the relationship between mental illness and traffic accidents--a pilot study. Am J Public Health Nations Health. 1970;60:459–69. doi: 10.2105/ajph.60.3.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crancer A, Quiring DL. The mentally ill as motor vehicle operators. Am J Psychiatry. 1969;126:807–13. doi: 10.1176/ajp.126.6.807. [DOI] [PubMed] [Google Scholar]
- 12.Sacher P. [Schizophrenia and the ability to drive] Schweiz Med Wochenschr. 1978;108:373–9. [PubMed] [Google Scholar]
- 13.Edlund MJ, Conrad C, Morris P. Accidents among schizophrenic outpatients. Compr Psychiatry. 1989;30:522–6. doi: 10.1016/0010-440x(89)90082-5. [DOI] [PubMed] [Google Scholar]
- 14.Unsworth CA, Baker AM, So MH, et al. A systematic review of evidence for fitness-to-drive among people with the mental health conditions of schizophrenia, stress/anxiety disorder, depression, personality disorder and obsessive compulsive disorder. BMC Psychiatry. 2017;17:318. doi: 10.1186/s12888-017-1481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bech P. Mental illness and simulated driving: before and during treatment. Pharmacopsychiatry. 1975;8:143–50. doi: 10.1055/s-0028-1094453. [DOI] [PubMed] [Google Scholar]
- 16.Cho SJ, Kim J, Lee JY, et al. Adherence to antipsychotic drugs by medication possession ratio for schizophrenia and similar psychotic disorders in the Republic of Korea: a retrospective cohort study. Clin Psychopharmacol Neurosci. 2022;20:491–7. doi: 10.9758/cpn.2022.20.3.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakonezny PA, Byerly MJ. Electronically monitored adherence in outpatients with schizophrenia or schizoaffective disorder: a comparison of first- vs. second-generation antipsychotics. Schizophr Res. 2006;82:107–14. doi: 10.1016/j.schres.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 18.Orriols L, Avalos-Fernandez M, Moore N, et al. Long-term chronic diseases and crash responsibility: a record linkage study. Accid Anal Prev. 2014;71:137–43. doi: 10.1016/j.aap.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Brubacher JR, Chan H, Erdelyi S, et al. Medications and risk of motor vehicle collision responsibility in British Columbia, Canada: a population-based case-control study. Lancet Public Health. 2021;6:e374–85. doi: 10.1016/S2468-2667(21)00027-X. [DOI] [PubMed] [Google Scholar]
- 20.Brubacher J, Chan H, Asbridge M. Development and validation of a crash culpability scoring tool. Traffic Inj Prev. 2012;13:219–29. doi: 10.1080/15389588.2011.645383. [DOI] [PubMed] [Google Scholar]
- 21.Pitt TM, Aucoin J, Nettel-Aguirre A, et al. Adaptation of a Canadian culpability scoring tool to Alberta police traffic collision report data. Traffic Inj Prev. 2019;20:270–5. doi: 10.1080/15389588.2019.1567916. [DOI] [PubMed] [Google Scholar]
- 22.Asbridge M, Brubacher JR, Chan H. Cell phone use and traffic crash risk: a culpability analysis. Int J Epidemiol. 2013;42:259–67. doi: 10.1093/ije/dys180. [DOI] [PubMed] [Google Scholar]
- 23.Tefft BC. Acute sleep deprivation and culpable motor vehicle crash involvement. Sleep. 2018;41 doi: 10.1093/sleep/zsy144. [DOI] [PubMed] [Google Scholar]
- 24.Longo MC, Hunter CE, Lokan RJ, et al. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: part II: the relationship between drug prevalence and drug concentration, and driver culpability. Accid Anal Prev. 2000;32:623–32. doi: 10.1016/s0001-4575(99)00110-4. [DOI] [PubMed] [Google Scholar]
- 25.Breen JM, Naess PA, Gjerde H, et al. The significance of preexisting medical conditions, alcohol/drug use and suicidal behavior for drivers in fatal motor vehicle crashes: a retrospective autopsy study. Forensic Sci Med Pathol. 2018;14:4–17. doi: 10.1007/s12024-017-9934-x. [DOI] [PubMed] [Google Scholar]
- 26.Staples JA, Erdelyi S, Merchant K, et al. Syncope and subsequent traffic crash: a responsibility analysis. PLoS One. 2023;18:e0279710. doi: 10.1371/journal.pone.0279710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinert T, Veit F, Schmid P, et al. Participating in mobility: people with schizophrenia driving motorized vehicles. Psychiatry Res. 2015;228:719–23. doi: 10.1016/j.psychres.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Staples JA, Erdelyi S, Merchant K, et al. Syncope and the risk of subsequent motor vehicle crash: a population-based retrospective cohort study. JAMA Intern Med. 2022;182:934–42. doi: 10.1001/jamainternmed.2022.2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naik H, Murray TM, Khan M, et al. Population-based trends in complexity of hospital inpatients. JAMA Intern Med. 2024;184:183–92. doi: 10.1001/jamainternmed.2023.7410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Staples JA, Erdelyi S, Merchant K, et al. Syncope While driving and the risk of a subsequent motor vehicle crash. Ann Emerg Med. 2024;83:147–57.:S0196-0644(23)01233-7. doi: 10.1016/j.annemergmed.2023.09.015. [DOI] [PubMed] [Google Scholar]
- 31.Kurdyak P, Lin E, Green D, et al. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry. 2015;60:362–8. doi: 10.1177/070674371506000805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taipale H, Tanskanen A, Mehtälä J, et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20) World Psychiatry. 2020;19:61–8. doi: 10.1002/wps.20699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rezansoff SN, Moniruzzaman A, Fazel S, et al. Adherence to antipsychotic medication and criminal recidivism in a Canadian provincial offender population. Schizophr Bull. 2017;43:1002–10. doi: 10.1093/schbul/sbx084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alsabbagh MW, Eurich D, Lix LM, et al. Does the association between adherence to statin medications and mortality depend on measurement approach? A retrospective cohort study. BMC Med Res Methodol. 2017;17:66. doi: 10.1186/s12874-017-0339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Velligan DI, Maples NJ, Pokorny JJ, et al. Assessment of adherence to oral antipsychotic medications: what has changed over the past decade? Schizophr Res. 2020;215:17–24. doi: 10.1016/j.schres.2019.11.022. [DOI] [PubMed] [Google Scholar]
- 36.Romano E, Torres-Saavedra PA, Calderón Cartagena HI, et al. Alcohol-related risk of driver fatalities in motor vehicle crashes: comparing data from 2007 and 2013-2014. J Stud Alcohol Drugs. 2018;79:547–52. doi: 10.15288/jsad.2018.79.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lenguerrand E, Martin J-L, Moskal A, et al. Limits of the quasi-induced exposure method when compared with the standard case-control design. Application to the estimation of risks associated with driving under the influence of cannabis or alcohol. Accid Anal Prev. 2008;40:861–8. doi: 10.1016/j.aap.2007.09.027. [DOI] [PubMed] [Google Scholar]
- 38.Blais É, Bellavance F, Marcil A, et al. Effects of introducing an administrative.05% blood alcohol concentration limit on law enforcement patterns and alcohol-related collisions in Canada. Accid Anal Prev. 2015;82:101–11. doi: 10.1016/j.aap.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 39.Kozma C, Dirani R, Canuso C, et al. Change in employment status over 52 weeks in patients with schizophrenia: an observational study. Curr Med Res Opin. 2011;27:327–33. doi: 10.1185/03007995.2010.541431. [DOI] [PubMed] [Google Scholar]
- 40.Giraud-Baro E, Dassa D, De Vathaire F, et al. Schizophrenia-spectrum patients treated with long-acting injectable risperidone in real-life clinical settings: functional recovery in remitted versus stable, non-remitted patients (the EveREST prospective observational cohort study) BMC Psychiatry. 2016;16:8. doi: 10.1186/s12888-016-0712-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ascher-Svanum H, Faries DE, Zhu B, et al. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67:453–60. doi: 10.4088/jcp.v67n0317. [DOI] [PubMed] [Google Scholar]
- 42.Said Q, Gutterman EM, Kim MS, et al. Somnolence effects of antipsychotic medications and the risk of unintentional injury. Pharmacoepidemiol Drug Saf. 2008;17:354–64. doi: 10.1002/pds.1559. [DOI] [PubMed] [Google Scholar]
- 43.Thornicroft G, Sunkel C, Alikhon Aliev A, et al. The Lancet Commission on ending stigma and discrimination in mental health. Lancet. 2022;400:1438–80. doi: 10.1016/S0140-6736(22)01470-2. [DOI] [PubMed] [Google Scholar]