Abstract
We describe a case of globe rupture due to a forklift accident. A 64-year-old man presented to the ophthalmology hospital shortly after the jaws of a forklift struck his left eye. The left eye was shrunken with a full-thickness scleral laceration. B-scan ultrasonography revealed a hypotonic eyeball with antero-posterior shrinkage. We promptly performed scleral suturing to maintain the ocular shape. The patient's intraocular pressure improved to 7.1 mmHg, and visual acuity was limited to light perception. Despite this, intraocular hemorrhage in the anterior chamber persisted, and an electroretinogram demonstrated poor response to light. Subsequently, the patient underwent a vitrectomy with silicone oil tamponade to address the vitreous hemorrhage, proliferative membranes, and retinal detachment. However, proliferative vitreoretinopathy with tractional retinal detachment progressed postoperatively, resulting in the loss of light perception. Ocular trauma caused by forklifts accident is rare; however, the strong external forces they exert can cause severe and irreversible visual impairment. Therefore, it is necessary for forklift operators and other concerned individuals to exercise caution to prevent forklift-related ocular trauma. Moreover, ophthalmologists should be aware of the dangers of forklift-related ocular trauma and treatment and management of the same.
Keywords: Ocular trauma, Vehicle, Industrial injury, Open globe injury, Proliferative vitreoretinopathy
Introduction
Forklifts are load-handling vehicles equipped with hydraulically powered cargo jaws and are used in industrial or agricultural settings. Owing to their large size and strong jaws, mishandling or contact with the surroundings can easily lead to accidents. Forklift-related accidents are mainly orthopedic, involving mechanical stress fractures [1,2], and can be fatal [3,4]. Such accidents reportedly cause injuries of varying severity to the legs and back [5,6].
However, there are no reports on forklift accidents resulting in eye injuries. Herein, we describe a case of eyeball rupture caused by a forklift accident, which resulted in blindness.
Case report
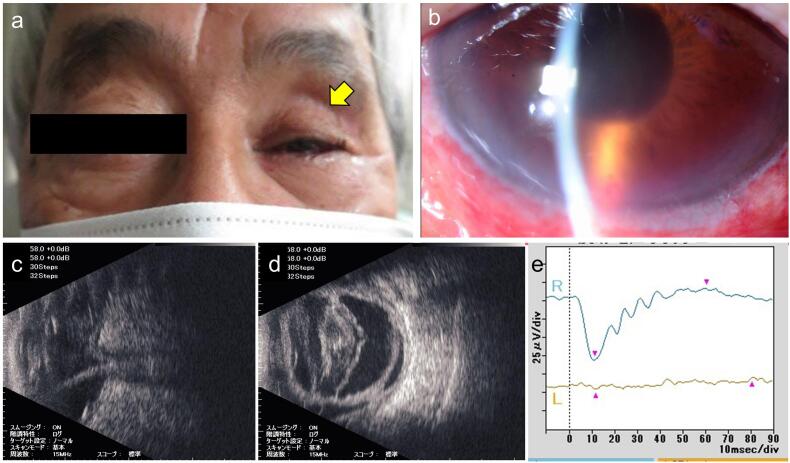
A 64-year-old male pig farmer presented to our hospital an hour after the jaws of a farm forklift hit his face, including his left eye. His chief complaint was loss of vision in the left eye. He had been regularly followed up at our hospital for fundus examination for diabetes mellitus, hypertension, and dyslipidemia after cataract surgery. On admission, the patient was conscious, afebrile, and in a stable condition. His blood pressure was 164/98 mmHg, heart rate was 68 beats/min, and oxygen saturation was 98 %. On initial examination, an open globe injury was noted, and the left eye was shrunken with a scleral laceration (Fig. 1a). The intraocular pressure was unmeasurable. A slit-lamp examination revealed that the anterior chamber was deep; however, cells and blood were observed (Fig. 1b). The intraocular lens was lost. Fundus examination was difficult because of the edematous cornea and blood in the anterior chamber. B-scan ultrasonography revealed a hypotonic, antero-posteriorly shrunken eyeball (Fig. 1c). The Ocular Trauma Score raw point was calculated to be 26, based on a previous report [7]. The right eye was intact, with a best-corrected visual acuity of 20/20 and an intraocular pressure of 13 mmHg.
Fig. 1.
Ocular manifestation of a 64-year-old man with a forklift injury.
(a) Face of the patient at the initial presentation. The eyeball was depressed, and the eyelid fissure was narrowing (arrow). (b) Photograph of the anterior segment of the left eye on slit-lamp examination. Intraocular cells and blood were observed through the edematous cornea. (c) B-mode echography image at the initial presentation. The eyeball was shrunk, and the axial length was abnormally short. Retinal detachment was also observed. (d) B-mode echography image after scleral suturing. Strong opacified vitreous hemorrhage was observed, although the ocular round structure was maintained. (e) Results of electroretinogram after scleral suturing. Response to light stimulation was scarce in the left eye.
On the same day, we performed scleral suturing with irrigation of the anterior chamber with vancomycin and ceftazidime to prevent endophthalmitis under local anesthesia. The ruptured sclera on the superior temporal side was accessed after temporary disinsertion of the lateral rectus muscle. Postoperatively, meropenem (3 g/day) was administered intravenously, along with topical instillation of 1.5 % levofloxacin six times daily, 0.1 % betamethasone six times daily, and tropicamide/phenylephrine once daily. Computed tomography of the head revealed no bone fractures around the eyes. Postoperatively, the ocular shape was maintained; however, bleeding in the anterior chamber continued, and prominent vitreous hemorrhage was observed on B-scan ultrasonography (Fig. 1d). Prominent folds in the Descemet's membrane were also observed. Two days later, there was no leakage from the sutured wound, and the intraocular pressure improved to 7.1 mmHg; however, the fundus could not be observed. An electroretinogram obtained 10 days postoperatively showed poor response to light in the left eye (Fig. 1e). Visual acuity was limited to light perception. Subsequently, intravenous antibiotics were discontinued, and the patient was discharged.
Although vitreous surgery was planned to remove vitreous hemorrhage and observe the fundus, the patient was undecided on undergoing further surgery because the visual prognosis was uncertain. However, he requested surgery 3 weeks later, and vitrectomy of the left eye was performed under topical anesthesia. Owing to severe corneal edema and poor visibility, the surgery was performed with the 25-gauge Constellation Vision System (Alcon) after debriding the corneal epithelium. The proliferative membranes were treated, the retina was reinstated with perfluorocarbon, and retinal photocoagulation was performed (200 mW, 0.2 s, 400 shots). The surgery was completed with intraocular silicone oil replacement and suturing of the sclera and conjunctiva with 8–0 Vicryl, followed by ofloxacin eye ointment application. Postoperatively, the patient was treated with 1.5 % levofloxacin four times daily, 0.1 % betamethasone four times daily, and 0.1 % bromfenac twice daily.
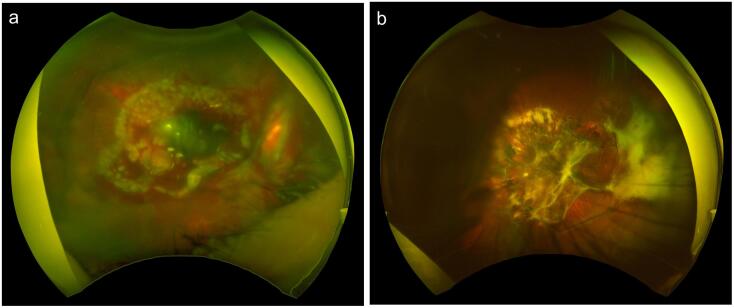
One month after vitrectomy, postoperative inflammation gradually subsided, and only light perception was noted. A wide-field fundus camera revealed retinal hemorrhage (Fig. 2a). The intraocular pressure was 3 mmHg. Levofloxacin and betamethasone were discontinued; however, bromfenac was continued. Two months after vitrectomy, inflammation in the anterior chamber stabilized, and there was no intraocular bleeding. However, proliferative vitreoretinopathy recurred, and tractional retinal detachment progressed. As visual function could not be maintained, the patient chose to avoid additional surgery, and a follow-up plan was decided. Topical 0.1 % bromfenac was discontinued 5 months postoperatively. Two years postoperatively, the left eye showed no light perception, and the intraocular pressure was 4.7 mmHg with severe proliferative vitreoretinopathy (Fig. 2b). No sympathetic ophthalmitis was observed in the right eye for 2.5 years postoperatively without additional immunosuppressant use.
Fig. 2.
Wide-field fundus images in a 64-year-old man with forklift injury.
(a) Fundus image 1 month after vitreous surgery. Retinal hemorrhage and photocoagulation scar were observed through silicone oil. (b) Fundus image 2 years after vitreous surgery. Proliferative vitreoretinopathy progressed, and tractional retinal detachment was observed.
Discussion
Ocular trauma is typically classified into two main categories: open-globe and closed-globe injuries [8]. Open-globe injuries are generally more severe, prone to ocular infection, and associated with a poorer prognosis than closed-globe injuries [9]. The present case involved an open-globe injury with ocular rupture, specifically affecting the posterior sclera of the superior temporal side. Although the sclera was sutured to preserve the ocular structure, vitrectomy was subsequently performed to address retinal detachment, vitreous hemorrhage, and proliferative vitreoretinopathy. However, visual impairment persisted. The prognosis was influenced by the following factors: 1) severely hypotonic eye and loss of ocular structure; 2) significant hemorrhage; and 3) retinal detachment. Based on these presentations on initial examination, the ocular trauma score was calculated as “1”, at which 73 % of patients have no light perception [7]. The patient was initially hesitant to undergo vitrectomy after scleral suture, and the delay may have affected proliferative vitreoretinopathy progression. Ultimately, the patient declined further surgery; on follow-up, there was no improvement in visual acuity, with persistent lack of light perception.
One characteristic of ocular trauma caused by forklifts accidents is significant tissue damage resulting from the strong external forces. Forklifts are highly maneuverable, small-turning vehicles that often operate at high speeds. The strong structure of their jaws inflicts considerable damage upon striking human tissues, such as the eyes. Typical injuries include lower limb fractures and renal and spinal injuries, and ocular injuries have not been frequently reported [5,10,11]. However, when forklift truck jaws strike the eye, the resulting injury is significant, requiring immediate diagnosis and treatment at a specialized institution.
Forklift trauma is one of the common types of industrial injuries, highlighting the importance of preventive measures. From an ophthalmological viewpoint, it is important that during forklift operations in warehouses and agricultural settings, people in the vicinity wear facial protective gear, including sturdy safety glasses. Furthermore, workers should avoid putting their faces close to forklifts and other moving vehicles, and drivers should check their surroundings and be aware of pedestrians before operating such equipment.
Conclusion
Ocular trauma resulting from forklift accidents is rare; however, the strong external forces forklifts exert can cause severe visual impairment, requiring prompt specialized medical intervention. Forklift operators and other concerned people should exercise caution to prevent forklift-related ocular trauma. Further, ophthalmologists should be aware of the dangers of forklift-related ocular trauma and its management.
Ethics approval/consent to participate
Written informed consent was obtained from the patient before drafting the case report. This study was conducted in accordance with the principles of the Declaration of Helsinki (2013). The authors contacted the Institutional Review Board of Miyata Eye Hospital, which confirmed that ethical approval was not required for this case report, in accordance with the ethical guidelines for medical and health research involving human subjects established by the Ministry of Education, Culture, Sports, Science and Technology, the Ministry of Economy, Trade and Industry, and the Ministry of Health, Labor and Welfare.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Patient consent statement
Written informed consent was obtained from the patient before drafting the case report. This study was conducted in accordance with the principles of the Declaration of Helsinki (2013).
Data statement
The data supporting the findings of this study are available from the corresponding author upon request. However, the data are not publicly available because they contain information that may compromise the privacy of the research participants.
CRediT authorship contribution statement
Takashi Ono: Writing – original draft, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Takuya Iwasaki: Writing – review & editing, Validation, Supervision, Data curation, Conceptualization. Michiyo Kato: Validation, Resources, Methodology, Investigation, Data curation. Toshihiro Sakisaka: Visualization, Validation, Resources, Project administration, Investigation, Formal analysis, Data curation. Yosai Mori: Writing – original draft, Visualization, Validation, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ryohei Nejima: Writing – review & editing, Visualization, Validation, Software, Resources, Project administration, Methodology, Investigation, Data curation. Fumiki Okamoto: Writing – review & editing, Visualization, Validation, Supervision, Resources, Project administration, Methodology, Data curation. Kazunori Miyata: Writing – review & editing, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors report there are no competing interests to declare.
References
- 1.Born C.T., Ross S.E., Aron B., DeLong W.G., Jr., Iannacone W.M. Patterns of injury and disability caused by forklift trucks. J. Trauma. 1996;40:636–639. doi: 10.1097/00005373-199604000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Darcy C.M., Lovell M.E., Metcalfe J.W. Injuries from forklift trucks. Injury. 1995;26:285. doi: 10.1016/0020-1383(95)90019-t. [DOI] [PubMed] [Google Scholar]
- 3.Lifschultz B.D., Donoghue E.R. Deaths due to forklift truck accidents. Forensic Sci. Int. 1994;65:121–134. doi: 10.1016/0379-0738(94)90267-4. [DOI] [PubMed] [Google Scholar]
- 4.Collins J.W., Landen D.D., Kisner S.M., Johnston J.J., Chin S.F., Kennedy R.D. Fatal occupational injuries associated with forklifts. United States, 1980–1994. Am. J. Ind. Med. 1999;36:504–512. doi: 10.1002/(sici)1097-0274(199911)36:5<504::aid-ajim2>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 5.Bage T., Ibrahim M., Baden J., Filobbos G. Forklift-related lower limb injuries: a retrospective case series study with patient-reported outcome measures (PROMs) Ann. R. Coll. Surg. Engl. 2021;103:730–733. doi: 10.1308/rcsann.2020.7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong C.C., Nashi N., Kuan W.S., Teh J.W., Tan K.J. Forklift-related crush injuries of the foot and ankle. Foot Ankle Int. 2015;36:806–811. doi: 10.1177/1071100715576486. [DOI] [PubMed] [Google Scholar]
- 7.Kuhn F., Maisiak R., Mann L., Mester V., Morris R., Witherspoon C.D. The ocular trauma score (OTS) Ophthalmol. Clin. N. Am. 2002;15:163–165. doi: 10.1016/s0896-1549(02)00007-x. [DOI] [PubMed] [Google Scholar]
- 8.Pieramici D.J., Sternberg P., Jr., Aaberg T.M., Sr., et al. A system for classifying mechanical injuries of the eye (globe). The ocular trauma classification group. Am. J. Ophthalmol. 1997;123:820–831. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 9.Onakpoya O.H., Adeoye A., Adeoti C.O., Ajite K. Epidemiology of ocular trauma among the elderly in a developing country. Ophthalmic Epidemiol. 2010;17:315–320. doi: 10.3109/09286586.2010.508352. [DOI] [PubMed] [Google Scholar]
- 10.Maruhashi T., Kashimi F., Yamaya T., Takeuchi I., Kataoka Y., Asari Y. A case of renal vein branch injury identified by multidetector computed tomography. Trauma Case Rep. 2017;7:19–22. doi: 10.1016/j.tcr.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang T., Liu Y., Cao J., et al. Case report: traumatic lumbosacral spondyloptosis with locked L5 inferior articular process. Front. Surg. 2023;10:1174169. doi: 10.3389/fsurg.2023.1174169. [DOI] [PMC free article] [PubMed] [Google Scholar]