Abstract
Background
Cold homes are associated with an increased risk of adverse health outcomes for older people. To mitigate this risk, homes need to be heated to an appropriate temperature. This review aims to identify interventions designed to improve heating and temperatures within homes and summarize its impact on health, health service utilization and cost effectiveness.
Methods
A rapid review was conducted. Studies assessing the effects of structural, financial, or behavioural interventions designed to improve home temperatures of residents aged 18+ years were eligible. Searches were carried out in four databases. A search for grey literature, and backward and forward citation searching were performed. Data were summarized in a narrative synthesis and mapped using EPPI-Reviewer and EPPI-Mapper software.
Results
Eighteen studies reported across 19 publications were included. Structural interventions were associated with better mental health and quality of life, a reduction in health service utilization, and improvements in satisfaction with internal home temperature, social interactions and financial difficulties. The impact on physical health outcomes varied by age, gender and long-term conditions. Evidence about the impact of behavioural interventions was inconsistent.
Conclusion
Structural improvements to increase home temperatures may offer the potential to improve some aspects of health. However, the impact on physical health, including which groups are most likely to benefit, is unclear. Key gaps include the lack of evidence about the impact of financial interventions, and the impact of all types of interventions, on quality of life, mortality and costs.
Introduction
Cold homes are associated with health inequalities and increased risk of adverse health outcomes for older people.1 The United Kingdom (UK) has the sixth highest long-term rate of excess winter mortality out of 30 European countries, with an estimated 30% of excess deaths in England and Wales associated with living in homes with low temperatures in the winter period of 2021–2022.2,3 It is projected that in 2023, fuel poverty will increase to 14.4% (3.53 million) of households in England.4 Fuel poverty relates to a situation where a household needs to spend more than 10% of their adjusted net income in order to maintain a satisfactory warm indoor environment.5 Older people who are frail, socially isolated, at risk of falls, and/or have underlying health conditions like cardiovascular and respiratory problems, are likely to spend more of their time indoors.6 Therefore, older populations are especially vulnerable to the health consequences of cold homes, such as poor physical and mental health, and increased mortality risk.7
Action is needed to ensure homes are sufficiently heated. Preventable excess winter deaths can be reduced by improving the energy efficiency of homes and making heating systems more affordable.8 Local and national policies are focused on identifying approaches to reduce the health consequences of cold homes.8 Potential interventions include making structural changes to homes and heating systems (e.g. heating systems, insulation and double glazed windows),9,10 supplementing financial resources of older people to increase the affordability of heating (e.g. national fiscal or local funding schemes),4,9 and supporting behavioural changes around heating homes (e.g. using energy more efficiently).11
Although a number of systematic reviews have examined the overall effects of cold homes on health outcomes, mortality and morbidity, and well-being,12,13 only one has focused on identifying the types of interventions associated with health improvements.10 This review,10 published in 2013, found that structural improvements can lead to improved health outcomes especially for people with respiratory conditions. Additional evaluations of interventions to improve home temperatures have been published since this review, warranting an up-to-date and comprehensive synthesis of the evidence base. This study aimed to identify and summarize evidence on the effectiveness of interventions designed to improve heating and temperatures within homes to benefit health outcomes.
Methods
We conducted a rapid review of primary studies to achieve a timely summary of evidence. Rapid reviews use modified systematic review methods to streamline study searches and selection, data extraction and quality assessment.14 The methods are reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Supplementary file S1).15
Search strategy
Searches were carried out on 26th May 2023. The search strategy was developed by an information specialist in Applied Social Sciences Index and Abstracts on ProQuest and translated to other databases: MEDLINE (OVID), PsycINFO (OVID) and CINAHL (EBSCO). The concepts used were [population characteristics: cost of living] AND [population characteristics: housing] AND [interventions] and incorporated subject headings, synonyms, and text word searching. Searches were limited to publications dated from 1st January 2010 (Supplementary file S2). We anticipated that some evidence may be in non-peer reviewed sources; therefore, field experts were contacted to seek advice other non-peer reviewed publications that may be relevant. We also looked into the publication database of He Kainga Oranga Housing & Health. Grey literature was hand-searched based on these to supplement database searches. Backward and forward citation searching were carried out using Google Scholar.
Eligibility criteria
Evaluations of structural, financial or behavioural interventions designed to improve home temperatures for the health benefit of residents aged 18 years or older were eligible (table 1). Eligible outcomes were any measure of physical or mental health, health service utilization, quality of life, mortality and cost effectiveness. Studies that reported non-health outcomes (e.g. mould, damp) were also included if they also reported health outcomes. Due to the changing nature of structural technologies for heating homes (e.g. heating systems, insulation etc.), we prioritized contemporary evidence published from 2010.
Table 1.
Review criteria
| Population |
|
| Intervention |
|
| Comparator | Any comparator or none (i.e. before and after studies). |
| Outcome |
|
| Study design |
|
Study screening and selection
Titles and abstracts were screened independently by two reviewers (E.E.J., N.S.). Disagreements were resolved through discussion or arbitrated by a third reviewer (G.S.). The full texts of selected records were retrieved and assessed independently by two reviewers using a hierarchy of exclusion criteria (K.G., M.T.) (Supplementary file S3). All records were managed in Rayyan,16 an online platform to support systematic review screening.
Data extraction and quality assessment
A data extraction form was developed and piloted. Two reviewers independently performed the data extraction (K.G., M.T.). Fifty percent of extracted data were checked by another researcher (G.S.). Studies were critically appraised using the NIH Quality Assessment Tool for Randomised studies, and Controlled and Before-and-After Studies.17 An overall rating of ‘poor’ was given if two or more of the criteria were unmet; ‘fair’ if one criterion was unmet and ‘good’ if all criteria were met.
Synthesis
Evidence was summarized using a narrative synthesis. We grouped studies by intervention category (i.e. structural, behavioural and financial) and then outcome (i.e. physical health, mental health, quality of life, health service utilization, mortality, cost effectiveness and non-health outcomes). We reported the effectiveness of the interventions by examining the overall direction of effects across studies. Narrative subgroup analysis was conducted on studies that reported outcomes by age (60+ or all adult ages), populations with long-term conditions [e.g. Chronic obstructive pulmonary disease (COPD), heart disease] or socioeconomic status.
An evidence map was produced to visualize the volume and concentration of evidence by intervention type and outcome. A single researcher (E.E.J.) coded records of included studies in EPPI-Reviewer software.18 The coding report was downloaded from EPPI-Reviewer and checked for accuracy against the data extraction by a second researcher (K.G.). The evidence map was then generated using the EPPI-Mapper wizard.
Results
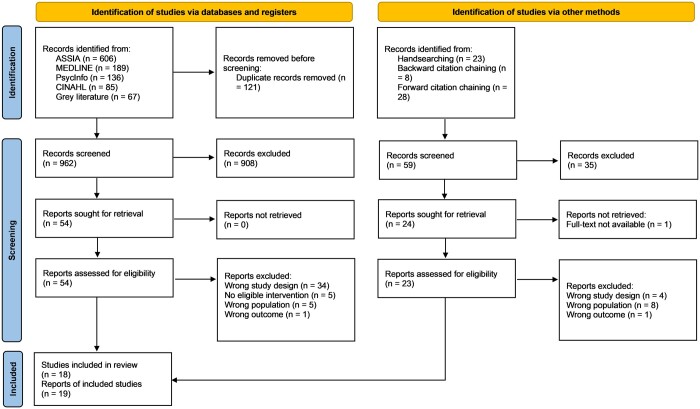
After screening, 18 studies reported across 19 publications met the criteria and were included in this review (figure 1). Three studies were reported across six publications (two publications per study)19–24 and three studies25 were reported in one publication.
Figure 1.
Prisma diagram. Source: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.
Study characteristics
Four studies used randomized designs28–31 and 14 used non-randomized designs,19–25,32–39 including prospective cohort (n = 5), retrospective (n = 6) and before and after (n = 3). Five non-randomized studies reported cost analyses.19,22,24,25,30,32 Overall, half of the included studies specifically reported evidence about older adults aged 60 years and over.20,21,23,24,29–31,34,37–39 Five studies reported evidence for populations aged 18 years and over19,22,28,32,33,34 and a minority of studies reported evidence for all ages (0–60+), where we extracted outcomes for studies of population aged 18 years and over.25,36 Some studies specifically looked at adults living in social or affordable housing,19,21,22,25,36 hard-to-treat homes,25 and/or those experiencing fuel poverty.28,32,35 Eleven studies included populations with long-term health conditions: respiratory (e.g. asthma and COPD) and/or cardiovascular (e.g. high blood pressure) diseases.20,23–25,29,34–39 A summary of all studies included in this review is presented in table 2.
Table 2.
Summary of study characteristics
| Author, year | Study design | Country | Age group | Range or mean (SD) age | Sample size | Target population (Condition) | Type of intervention | Quality rating |
|---|---|---|---|---|---|---|---|---|
| Carrere et. al. 202232 |
|
Spain | 18 and over |
|
|
People who are energy poor, defined as those who are unable to ensure socially and materially required levels of domestic energy services | Behavioural | Poor |
| Pollard et. al. 201935 |
|
UK | 18 and over | The majority of participants completing the questionnaire (73%) were aged over 65 years of age. | n = 22 households | Fuel poor, households that struggle with the costs of keeping their home warm due to the cost of fuel and energy efficiency of the property | Behavioural | Poor |
| Saeki et. al. 201531 | RCT (Prospective) | Japan | 60 and over | 71.6 (6.6) years | n = 359 | Aged 60 and over living at home | Behavioural | Fair |
| Bray et. al. 201719 | Non-RCT (Historical cohort and cost analysis, Prospective) | UK | 25 and over |
|
228 households | Social housing | Structural | Poor |
| Edwards et. al. 201622 |
|
UK | 25 and over |
|
228 households | Families living in social housing in Sunderland. | Structural | Fair |
| Curl and Kearns 201520 |
|
UK | 65 and over |
|
|
Respiratory and circulatory diseases | Structural | Fair |
| Curl et. al. 201521 |
|
UK | 65 and over |
|
|
Social housing | Structural | Fair |
| Fyfe 202123 |
|
New Zealand | All ages, extracted outcomes for 65 and over |
|
|
Residents of owner-occupied and private rental dwellings | Structural | Fair |
| Telfar-Barnard et. al. 201124 | Non-RCT (Cohort study and cost analysis, Retrospective) | New Zealand | All ages, extracted outcome for 65 and over |
|
Total treatment cohort at that time = 107 421 | Structural | Fair | |
| Poortinga et. al. 201825 | Non-RCT (Cohort analysis, Retrospective) | UK | All ages | NA | n = 25 908 individuals living in 4968 intervention | Social housing and COPD, cardiovascular conditions | Structural | Fair |
| Poortinga et. al. 201825,26,27 | Non-RCT (Quasi-experimental before and after study, Prospective) | UK | All ages |
|
|
Hard-to-heat, hard-to-treat Social housing and COPD, cardiovascular conditions | Structural | Poor |
| Poortinga et. al. 201825,26,27 |
|
UK | All ages |
|
NA | Social housing | Structural | Fair |
| Heyman et al. 201128 |
|
UK | 20 and over | NA | 237 households | Households in full or marginal fuel poverty | Structural | Poor |
| Liddell et. al. 201133 |
|
UK | 25 and over |
|
165 686 households | Houses in the private sector | Structural | Poor |
| Osman et. al. 201029 | RCT (Prospective) | UK | 65 and over |
|
n = 178 | Clinician-diagnosed COPD | Structural | Fair |
| Page et. al. 202230 |
|
Australia | 60 and over | 74.8 (11.5) |
|
Most participants had either never smoked (52%) or had given up >12 months ago (39%); only 3% were current smokers | Structural | Poor |
| Peralta et. al. 201734 |
|
Spain | 60 and over |
|
n = 2252 | Deaths of people living in the studied blocks and occurred in the city during the cold periods. | Structural | Poor |
| Poortinga et. al. 201736 |
|
UK | All ages |
|
n = 10 009 | Social housing | Structural | Fair |
| Preval et. al. 201737 | Non-RCT (Quasi-experimental cohort study, Retrospective) | New Zealand | 60 and over |
|
n = 4848 | Cardiovascular and respiratory-related hospitalization | Structural | Fair |
| Rodgers et. al. 201838 |
|
UK | All ages, extracted outcome for 60 and over |
|
|
Tenants aged 60 and over, cardiovascular, respiratory and injuries | Structural | Poor |
| Tonn et. al. 202339 | Non-RCT (Quasi-experimental) | USA | 60 and over |
|
|
Affordable multifamily building offered by property owners that had 5+ units. | Structural | Fair |
COPD, clinician-diagnosed chronic obstructive pulmonary disease; NA, not applicable; RCT, randomized controlled trial; SD, standard deviation; UK, United Kingdom.
Green: RCTs, Orange: non-RCTs; Blue: linked studies.
Fifteen studies assessed structural interventions19–30,33,34,36–39 and three assessed behavioural interventions.31,32,35 No studies assessing the health impact of financial interventions were found. The duration of interventions ranged from 3 months to 20 years. The most common components of structural interventions consisted of the installation of insulation retrofits (n = 12), heating improvements (n = 11) and installation of new double-glazed windows to replace single-glazed windows (n = 8). For the three behavioural interventions, the components were home visits for energy counselling, instructions to change thermostat settings, and the use of wearable telemetry to measure blood pressure. Characteristics of the intervention studies are presented in table 3.
Table 3.
Features of interventions
| Author, year | Study design | Type of intervention | Name of intervention and stakeholder involvement | Funding amount | Components of intervention | Duration of intervention (assessment points) |
|---|---|---|---|---|---|---|
| Carrere et. al. 202232 | Non-RCT | Behavioural | Energia, la Justa (EJUSTA): Partly funded by a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain) co-funded with European Union ERDF funds (European Regional Development Fund) | NA | Energy-counselling home visits to: (i) protect people’s energy via legal action, (ii) promote energy-saving behaviours to achieve savings, (iii) optimization of energy services through change of provide or tariffs, and (iv) installation of micro efficiency measures, that is, plug-in timers, energy saving light bulb, etc. | 5 months, 2016 (Baseline and 1 year after intervention) |
| Pollard et al. 201935 | Non-RCT | Behavioural | Wearable telemetry: Funded by The British Gas Energy Trust Healthy Homes Fund 2015 | NA | Wearable telemetry (i.e. a thermometer with a low-temperature alarm) The loggers were equipped with sensors that triggered a flashing light-emitting diode (LED) if the temperature in the immediate vicinity fell below 18°C or rose above 26°C. This provided participants and their families with an alert for changes in temperature that could exacerbate their LSI. Temperatures were recorded every 15 minutes with the number of readings below 18°C and 15°C noted. | 3 months, winter 2016/2017 (Baseline and after three months) |
| Saeki et al. 201531 | RCT | Behavioural | Instruction in home heating on indoor temperature: Department of Indoor Environmental Medicine, Nara Medical University; JSPS KAKENHI; Mitsui Sumitomo Insurance Welfare Foundation; Meiji Yasuda Life Foundation of Health and Welfare; Osaka Gas Group Welfare Foundation; Japan Diabetes Foundation; Daiwa Securities Health Foundation; and the Japan Science and Technology Agency | NA | Participants were asked to set the heating device in the living room to start 1 hour before the estimated rising time with a target temperature of 24°C, and to stay in the living room until 2 hours after rising as long as possible | 1 year, December–March 2010, September–March 2012 (Baseline and after intervention) |
| Bray et. al. 201719 | Non-RCT | Structural | The Warm Homes for Health: Funded by Gentoo and Nottingham City Homes | Mean total cost of the intervention per household was £3725.26 (SD=£1041.48) | The intervention consisted of the installation of (i) new double-glazed windows to replace single-glazed windows, and (ii) installation of a new energy-efficient combi boiler. | 8 months, April–December 2014 (Baseline and 1 year after intervention) |
| Edwards et. al. 201622 | Non-RCT | Structural | The average cost of improving each house was £3725. This comprised a new combi boiler (£2500 per boiler) and double-glazing (£240 per window) | |||
| Curl and Kearns 201520 | Non-RCT | Structural | GoWell project: Funded by the Scottish government | NA | (i) Central Heating, (ii) Front Doors, (iii) Windows, (iv) Environmental, (v) Fabric Works, (vi) Internal Common Works, (vii) Lift Replacement and (viii) Kitchen, Bathroom & Rewiring. | 2 years, 2006 (Wave 1)–2008 (Wave 2) |
| Curl et. al. 201521 | Non-RCT | Structural | £1.2 billion |
|
||
| Fyfe 202123 | Non-RCT | Structural | Warm Up New Zealand: Funded by the New Zealand government, delivered by Energy Efficiency and Conservation Authority (EECA) | NZ$347 million | Insulation retrofits and clean, efficient heating grants for New Zealand households | 5 years, 2009 to 2014 (2 years) |
| Telfar-Barnard et al 201124 | Non-RCT | Structural | NA | 4 years, 2009–2013 (Baseline and after intervention, 1 January 2008–30 September 2010.) | ||
| Poortinga et al. 201825 | Non-RCT | Structural | Welsh Government Warm Homes programme: Funded by Welsh Government | £68 million | The programme funded retrofit measures such as (i) solid wall insulation, (ii) solar panels, (iii) solar hot water and (iv) heat pumps. Additional options were available such as (v) boiler upgrades and replacements, (vi) window upgrades, (vii) roof extensions, (viii) structural work and (ix) energy saving advice | 1 year, 2010–2011 (Baseline and after intervention) |
| Poortinga et al. 201825 | Non-RCT | Structural | £45 million | 3 years, 2012–2015 (Baseline and 2 years from baseline) | ||
| Poortinga et al. 201825 | Non-RCT | Structural | £68 million | 5 years, 2010–2015 (Phase 1: 2010–2011; Phase 2: 2012–2015) | ||
| Heyman et. al. 201128 | RCT | Structural |
|
Intervention group households received an individually tailored package of improved heating and insulation. Control group households received heating and insulation package. The packages were worth an average of £727 (range £0–3335), and included loft insulation (54%), cavity wall insulation (53%), draught exclusion (29%), heating controls (20%), central heating (13%) and other measures as required | Tailored package of improved (i) heating and (ii) insulation | 4 years, 2000–2004 (End of year 1 and end of year 4) |
| Liddell et. al. 201133 | Non-RCT | Structural | Kirklees Warm Zone Project: Funded by Kirklees council and Scottish Power. Central government contributed through Warm Front scheme. Co-delivered with Kirklees Energy Services, Scottish Power, National Grid, Citizens’ Advice, the Pensions Service, Kirklees Benefits Advice Service and Revenue and Benefits, Warm Zone Ltd., Miller Pattison, West Yorkshire Fire Service, Carers Gateway, Yorkshire Water, Commissioned assessors | £24 million | (i) Free cavity wall insulation, (ii) free low energy light bulbs, (iii) free improvements to heating systems, (iv) competitive prices for replacement boilers and central heating and (v) interest free loans for renewable technologies | 3 years, 2007–2010 (After intervention) |
| Osman et. al. 201029 | RCT | Structural | Affordable Warmth Scheme: Co-delivered with Castlehill Housing Association (Care and Repair) | NA | Improvements included replacement and upgrades to (i) central heating systems, installation of (ii) loft, under-floor and cavity wall insulation and (iii) benefit reassessment. | 18 months, 2004–2007 (Baseline and 1 year after intervention) |
| Page et. al. 202230 | RCT | Structural | Victorian Healthy Homes Program (VHHP): Initial program funding was granted by the Sustainability Fund of the Victorian Government and additional funding was provided by Sustainability Victoria (SV) | The program allowed for an average of $3,500 per home to be spent on labour and materials to improve thermal comfort in an energy-efficient way. This was reduced to a target average of $2600 in the final year of the program |
|
3 years, 2018–2020 (3-month winter period of their study year) |
| Peralta et al. 201734 | Non-RCT | Structural | Energy efficiency facade retrofitting (EEFR): Funded by European Community’s Seventh Framework Programme | NA | Types of EEFR not reported | 20 years, 1982–2012 [Day of death (Lag 0) to 20th day before death (Lag 20)] |
| Poortinga et al. 201736 | Non-RCT | Structural | Carmarthenshire Homes Standard: Funded by Carmathernshire County Council | £200+ million | The programme involved the elements of (i) windows and doors; (ii) boilers; (iii) kitchens; (iv) bathrooms; (v) electrics; (vi) loft insulation; (vii) cavity-wall insulation; (viii) external wall insulation and (ix) safety improvements to external paths. | 7 years, 2009–2016 (2009, 2011, 2012, 2014, 2016) |
| Preval et al 201737 | Non-RCT | Structural | Warm Up New Zealand: Heat Smart Programme: Funded by New Zealand government, delivered by Energy Efficiency and Conservation Authority (EECA) | $347 million | Installation of insulation retrofits and clean, efficient heating grants | 4 years, 2009–2013 (2 years) |
| Rodgers et al 201838 | Non-RCT | Structural | Housing co-interventions: Council | NA | The eight cointerventions were new (i) windows and doors, (ii) kitchens, (iii) bathrooms, (iv) heating systems, (v) wall insulation, (vi) loft insulation, (vii) electrical systems and (viii) garden paths | 10 years dataset, January 2005 and March 2015 (10 years) |
| Tonn et al 202339 | Non-RCT | Structural | Weatherization: One sponsor of this work is based in New York City and the other set of sponsors were utility companies in the Commonwealth of Massachusetts. | NA | Buildings assigned to the Comparison with Treatment or Treatment groups had or were expected to have installed major weatherization measures (i.e. air sealing, insulation, HVAC repair and replacement). Phase 1 and 2 surveys were carried out. | 2 years, 2018–2020 (Baseline and after intervention) |
NZ, New Zealand; RCT, randomized controlled trial; SD, standard deviation.
Green, RCTs, Orange, non-RCTs; Blue, linked studies.
Critical appraisal results
Two of the four randomized controlled trials (RCTs) were rated poor quality,28,30 and two were fair.29,31 The main sources of bias in the RCTs were the large dropout rates and the lack of information to determine blinding of participants and treatment allocation. For the non-randomized studies, seven were rated fair20–22,24,25,36,37 and eight were rated poor quality.19,25,32–35,38,39 The main sources of bias in the non-randomized studies were the lack of blinding of outcome assessors to the participants’ interventions and poor consistency in outcome measures across multiple time points before and after the interventions (Supplementary file S4).
Effectiveness of interventions
Summary data on effectiveness for each intervention are detailed in Supplementary file S5.
Behavioural interventions
Three studies evaluated behavioural interventions.31,32,35 Outcomes evaluated in these studies included: physical health, mental health, quality of life, health service utilization, household temperature and fuel poverty. Two of these studies were rated as poor quality and one study was rated as fair.
Physical health outcomes were assessed in two studies31,32 using self-reported health measures, systolic and diastolic blood pressure surges, and minutes spent in physical activity. These studies produced conflicting evidence. One showed no improvements,32 while the other illustrated positive improvements31 in physical health as a result of the behavioural interventions.
Two studies32,35 reported mental health outcomes using self-reported measures on depression and/or anxiety, the use of antidepressants or sleeping medication, and feeling of vulnerability, cold, or illness during the winter period. Interventions had no significant impact on depression and/or anxiety32 and on self-reported measures of feeling cold or poorly during winter, compared to the previous year.35 However, participants felt less vulnerable after the intervention, all of whom were more aware of the temperature inside their homes after wearing telemetry.35 In contrast, there was a modest but statistically insignificant increase in antidepressant or sleeping medication use in the intervention group.32
One study35 reported changes in quality of life using self-reported well-being measures. The behavioural intervention had no significant effect on the overall well-being of the participants.
In terms of health service utilization, two studies32,35 measured the frequency of primary care visits per year, and the use of other National Health Service (NHS) services, including Accident and Emergency department (A&E) and pharmacy for any respiratory, cardiovascular and/or cold/flu symptoms. The impact of behavioural interventions on primary care visits was inconsistent. One study32 showed a significant decrease in primary care visits as a result of the intervention. The other study35 showed a significant increase in the frequency of primary care service utilization, which was linked to decreased use of A&E and pharmacist services.
Two studies31,32 assessed non-health outcomes, including indoor temperature, self-reported measures of keeping appropriate temperature during winter months, and arrears on utility bills. Both studies31,32 reported significant increase in indoor temperatures, although one study used a subjective measure to assess this (participants’ awareness of ambient temperatures).32 There was also a significant decrease in utility bill arrears in one study,32 although the reduction was larger for the non-intervention group.
Structural interventions
Fifteen studies evaluated structural interventions.19–30,33,34,36–39 Outcomes in these studies included: mortality, physical health, mental health, quality of life, health service utilization, cost effectiveness and a number of non-health outcomes. The quality rating of these studies were poor for eight studies and fair for eight.
Mortality was assessed in three studies23,24,30,34 using all-cause and cold-associated mortality rates. Varied effects were observed across all studies by age groups, gender and types of long-term diseases. In three studies, all-cause mortality for adults aged 60 and over did not improve following a structural intervention.23,30,34 However, only one study adjusted for sociodemographic factors.23 One study, which was rated low in quality, reported that the intervention acted as a risk factor,34 increasing the cold-associated deaths particularly for older men, as well as older adults with respiratory and circulatory diseases. In another study, there was a lower cumulative cold-associated mortality for older adults aged 65 and over who received insulation and heating compared with other types of structural interventions.23 In terms of deaths with an all-cause or cold-associated hospital admission, there was no significant effect for adults aged 65 and over.23,24 In contrast, a significant decrease in mortality was reported for older adults who were hospitalized with circulatory diseases.24
Physical health was assessed in five studies.20,25,28,36,39 One study used objective measures, such as time spent on moderate or vigorous physical activities,39 while the remaining studies recorded self-reported symptoms25,28,36 and association of interventions in preventing or recovering from self-reported respiratory or circulatory symptoms.20 Symptoms for respiratory and cardiovascular diseases were recorded by five studies.20,25,28,36,39
There was inconsistent evidence about the impact of structural interventions on improving these symptoms. One study showed improvement in asthma symptoms (e.g. wheezing) and chronic headaches following structural upgrades.39 Central heating was effective in preventing the development of circulatory and respiratory diseases in the long-term.20 Cavity wall insulation, windows and doors and boilers had no significant impact in improving symptoms of respiratory and circulatory diseases.36 An increase in physical activity was found for households aged 60 and over, albeit this improvement was statistically insignificant.39
Four studies20,25,36,39 assessed mental health outcomes. This was measured using subjective well-being scales, self-reported stress and/or depression scores, and association of interventions in preventing mental health diseases. Two studies20,36 suggested an improvement in mental health conditions, such as long-term stress, anxiety or depression. Installing cavity wall insulation was associated with better mental health for some households living in social housing,36 while central heating was reported to be effective in preventing mental health diseases for adults over the age of 65.20
Six studies19,21,22,25,28–30 recorded health-related quality of life outcomes using a variety of scales. Most of the studies reported improvements.19,21,22,28,30 Housing improvements, such as doors, fabric works and kitchen and bathrooms, as well as central heating, were all associated with a positive change in mental well-being components for older adults aged 65 and over.21
Health service utilization was assessed by nine studies19,22,23,25,28–30,37–39 using measures such as hospital, A&E, and primary care visits, rate of prescriptions dispensed and emergency and routine hospital admission rates. Most of the evidence suggested an overall significant reduction in health service utilization after implementing structural interventions. Results varied per age group and type of long-term condition. Overall general practitioner visits, routine hospital visits, and A&E attendance significantly reduced after structural improvements19,22,25,39 for households with respiratory conditions and those in social/affordable housing. However, one study reported a statistically significant increase in doctor visits for symptoms related to shortness of breath, bronchitis or other COPD, or emphysema flare ups.39 In three studies, hospital admission rates fell only for older adults aged 60 and over who have cardiovascular diseases, such as COPD and/or heart conditions.23,25,37 No significant change in hospital admissions was found for other populations.39 Structural interventions that were associated with fewer hospital admissions were insulation,23,37 heating and electrical systems.38
Five studies19,22,24,25,30,33 reported cost analyses of structural interventions. Evidence across the five studies suggested that the interventions produced overall cost savings and reduced health services expenditure. Estimates of total savings on health services ranged from £2000 to £150 00030,33 and £1.1 to £10 million value on lives saved.25,33 This was primarily associated with a reduction in use of health services and lower mortality rates.
Non-health outcomes, such as room temperatures, home warmth satisfaction and thermal comfort, social interactions, and financial difficulties, were reported by six studies.19,22,25,28–30,36 Structural housing improvements were associated with modest increase in indoor room temperatures in one study.28 This was not the case for households over 65 years and over diagnosed with COPD in another study,29 where no change in temperatures was found. Structural interventions were also associated with satisfaction with internal home temperature,25,28,30,36 increased social interactions,25 and reduced severity of financial difficulties.25 Two studies reported no impact on humidity29 and mould.30
Evidence map
The evidence map (https://eppi.ioe.ac.uk/cms/Portals/35/Maps/NIHRPRU/O1_%20ColdHomeInterventions.html) highlights the concentration of evidence by types of intervention and outcomes, segmented by study design and with a filter for age range (reporting data for people under or over 60 years). The highest concentration of evidence was found for structural interventions investigating physical health, mental health and health service utilization outcomes. Key evidence gaps were observed for mortality and costs outcomes, as well as financial and behavioural interventions.
Discussion
This rapid review found that structural interventions (e.g. heating systems, insulation, double glazed windows) are promising to improve mental health outcomes, quality of life and some aspects of physical health. The impact on mortality and physical health outcomes was inconsistent. Where improvements in physical health were reported for structural interventions, these effects tended to be weaker for older populations, particularly older people with respiratory and cardiovascular conditions.
Structural interventions were linked to health improvements, similar to the findings of previous studies.10 Cavity wall insulation and central heating were associated with better mental health,20,36 central heating was effective in preventing circulatory and respiratory symptoms,20 and electrical systems were associated with reduced hospital admissions.38 Structural interventions may also reduce certain types of health service use, with potential for cost savings. Only one study reported that insulation and heaters were linked to reduced mortality, but only for those aged 65 who had previously been hospitalized with circulatory illness.24 Across some of these studies reporting mortality, there was a lack of information on adjustment for important confounders, warranting caution in the interpretation of the findings.
A very small evidence base about behavioural interventions did not demonstrate consistent health benefits. This may be due to differences in the interventions, study populations and outcome measures across the three evaluations. Notably, two of the behavioural interventions were delivered to populations considered to be ‘energy-poor’32,35. In both studies, the authors suggested that the ability of energy-poor households to heat their home and/or change heating behaviours, largely depend on other factors, such as household income, state of the property (e.g. lack of ventilation etc.) and/or the residents’ health risks.
A key evidence gap identified in this review is around evaluations of financial interventions to improve home temperatures for health benefits. This may reflect the paucity of such interventions, rather than an absence of evaluation. One such intervention does exist in the UK: The Winter Fuel Payment. However, we found no evaluations of the impact of this scheme on health outcomes. A study published in 2019 assessed eligibility for the Winter Fuel Payment: no clear health improvements were observed. This study was ineligible for our review as it considered populations who were eligible for, rather than populations who received, this supplementation.40
A final observation is that the overall quality of the identified evidence was weak, with around half of studies judged to be poor. Thus, while the evidence points to the potential benefits of structural interventions to improve some health outcomes, this finding should be interpreted with caution.
Limitations
Our approach in this review has enabled us to produce a comprehensive synthesis of evidence about approaches to tackling poor health resulting from cold homes. Extensive searches across peer-reviewed and grey literature ensured this synthesis was exhaustive; our inclusion of behavioural, financial and structural interventions guaranteed it was comprehensive. A limitation of our approach is that we excluded evidence published before 2010. This was to ensure our synthesis was not undermined by evidence of outdated structural technologies. Consequently, we may have missed evidence about other types of interventions published before this date. However, we do not believe this to be a major risk as our preliminary scoping did not identify evaluations of non-structural interventions prior to this period.
Implications for practice and future research
Mitigating the health impact of cold homes is a policy priority. Evidence suggests that structural interventions are promising to improve mental health, quality of life and reduce some health care utilization. However, the impact on physical health is less clear, and unlikely to be uniform across populations. Further evidence about the impact of structural (and other) interventions on mortality is also needed.
Conclusions
Structural improvements to homes to increase home temperatures are promising to improve some aspects of health, quality of life and reduce utilization of some types of healthcare. It may also offer cost savings from reduced health service use. Further evidence is needed to understand the impact on mortality. Behavioural interventions did not demonstrate consistent benefits to physical or mental health, or to health service utilization. Key gaps include evaluations of the impact of financial interventions on health, and the impact of all interventions on mortality, quality of life and cost effectiveness outcomes.
Supplementary Material
Glossary
- A&E
Accident and Emergency department
- COPD
Chronic obstructive pulmonary disease
- NHS
National Health Service
- RCT
Randomized controlled trial
- SES
Socioeconomic status
- UK
United Kingdom
Contributor Information
Kimberly Lazo Green, Older People and Frailty Policy Research Unit, National Institute for Health and Care Research, The University of Manchester, Manchester, UK; Healthy Ageing Research Group, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, UK.
Michelle M C Tan, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK.
Eugenie Evelynne Johnson, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK; Evidence Synthesis Group/Innovation Observatory, Population Health Sciences Institute, Newcastle University, Newcastle Upon Tyne, UK.
Nisar Ahmed, Older People and Frailty Policy Research Unit, National Institute for Health and Care Research, The University of Manchester, Manchester, UK; Healthy Ageing Research Group, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, UK.
Claire Eastaugh, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK; Evidence Synthesis Group/Innovation Observatory, Population Health Sciences Institute, Newcastle University, Newcastle Upon Tyne, UK.
Fiona Beyer, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK; Evidence Synthesis Group/Innovation Observatory, Population Health Sciences Institute, Newcastle University, Newcastle Upon Tyne, UK.
Dawn Craig, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK; Evidence Synthesis Group/Innovation Observatory, Population Health Sciences Institute, Newcastle University, Newcastle Upon Tyne, UK.
Gemma F Spiers, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK; Evidence Synthesis Group/Innovation Observatory, Population Health Sciences Institute, Newcastle University, Newcastle Upon Tyne, UK.
Barbara Hanratty, National Institute for Health and Care Research Older People and Frailty Policy Research Unit, Newcastle University, Newcastle upon Tyne, UK.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Policy Research Unit in Older People and Frailty (PR-PRU-1217-21502). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care or its partner organizations.
Conflicts of interest: None declared.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author contributions
Conceptualization and methodology: DC, GS, BH; Data searches: FB, CE; Records screening: KG, MT, EEJ, NA; Data extraction: KG, MT; Analysis: KG, MT, EEJ; Critical appraisal: KG, MT; Interpretation: KG, MT, EEJ, GS; Writing original draft: KG, MT, EEJ, GS; Writing review and editing: KG, MT, EEJ, NA, CE, FB, DC, GS, BH; Supervision: GS, BH.
Key points.
Structural improvements may offer potential to improve some aspects of health.
There is a gap in the evidence on the impact of financial interventions on health, and the impact of all types of interventions on mortality, quality of life and cost effectiveness outcomes.
Identifying the types of interventions to reduce health consequences of cold homes is important to mitigating fuel poverty.
References
- 1. Louise MT, Suzanne M, Eugene MGM, et al. Socioeconomic and behavioural risk factors for adverse winter health and social outcomes in economically developed countries: a systematic review of quantitative observational studies. J Epidemiol Commun Health 2013;67:1061. [DOI] [PubMed] [Google Scholar]
- 2. National Energy Action Group. Fuel Poverty Charity Reveals 45 People Per Day Die from Cold Homes. 2023. Available from: https://www.nea.org.uk/news/fuel-poverty-charity-reveals-45-people-per-day-die-from-cold-homes (8 August 2023, date last accessed).
- 3. Liddell C, Morris C, Thomson H, Guiney C. Excess winter deaths in 30 European countries 1980-2013: a critical review of methods. J Public Health (Oxf) 2016;38:806–14. [DOI] [PubMed] [Google Scholar]
- 4. Statistics of Nation, Department for Energy Security and Net Zero, Department for Business Energy & Industrial Strategy. Annual Fuel Poverty Statistics in England, 2023 (2022 data). London Department for Energy Security and Net Zero, 2023.
- 5. Boardman B. Fuel Poverty: From Cold Homes to Affordable Warmth. London: Belhaven Press, 1991. [Google Scholar]
- 6. Public Health England. Health Matters: Cold Weather and COVID-19. London: Public Health England. 2020. https://www.gov.uk/government/publications/health-matters-cold-weather-and-covid-19/health-matters-cold-weather-and-covid-19.
- 7. Clair A, Baker E. Cold homes and mental health harm: evidence from the UK Household Longitudinal Study. Soc Sci Med 2022;314:115461. [DOI] [PubMed] [Google Scholar]
- 8. (NICE) National Institute for Health and Care Excellence. Excess Winter Deaths and Illness and the Health Risks Associated with Cold Homes. NICE Guideline, London. 2015. [Google Scholar]
- 9. Armstrong B, Bonnington O, Chalabi Z, et al. The impact of home energy efficiency interventions and winter fuel payments on winter- and cold-related mortality and morbidity in England: a natural equipment mixed-methods study. Public Health Res 2018;6:1. [PubMed] [Google Scholar]
- 10. Thomson H, Thomas S, Sellström E, Petticrew M. Housing improvements for health and associated socio-economic outcomes: a systematic review. Campbell Systematic Reviews 2013;9:1–348. [DOI] [PubMed] [Google Scholar]
- 11. The Behaviouralist. Using Behavioural Insights to Encourage Local Residents Save Energy: Final Report. 2023. London.
- 12. Janssen H, Gascoyne B, Ford K, et al. Cold Homes and Their Association With Health and Well-Being: A Systematic Literature Review. 2022. Wrexham, Wales: WHO Collaborating Centre on Investment for Health and Well-being, Public Health Wales NHS Trust. [DOI] [PubMed]
- 13. Jevons R, Carmichael C, Crossley A, Bone A. Minimum indoor temperature threshold recommendations for English homes in winter—a systematic review. Public Health 2016;136:4–12. [DOI] [PubMed] [Google Scholar]
- 14. Irma K, Shannon R, Andrew B, et al. Rapid reviews methods series: guidance on literature search. BMJ Evid-Based Med 2023.28:412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Institutes of Health. Study Quality Assessment Tools, 2013. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (18 August 2023, date last accessed).
- 18. Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: Software for Research Synthesis. EPPI Centre Software. London: Social Science Research Unit, Institute of Education, University of London, 2010. [Google Scholar]
- 19. Bray N, Burns P, Jones A, et al. Costs and outcomes of improving population health through better social housing: a cohort study and economic analysis. Int J Public Health 2017;62:1039–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Curl A, Kearns A. Can housing improvements cure or prevent the onset of health conditions over time in deprived areas? BMC Public Health 2015;15:1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Curl A, Kearns A, Mason P, et al. Physical and mental health outcomes following housing improvements: evidence from the GoWell study. J Epidemiol Community Health 2015;69:12–9. [DOI] [PubMed] [Google Scholar]
- 22. Edwards RT, Bray N, Burns P, Jones A. Warm Homes for Health End of Study Briefing 2016 Warm Homes for Health: Exploring the Costs and Outcomes of Improving Population Health Through Better Housing. Bangor: Centre for Health Economics and Medicines Evaluation, 2016. Report No.: 9780956487.
- 23. Fyfe CS. From Hearth to Health: An Investigation into the Health Impacts of the Warm Up New Zealand Home Insulation Subsidy Programme. 2021. (Thesis, Doctor of Philosophy). University of Otago. Retrieved from http://hdl.handle.net/10523/12255.
- 24. Telfar-Barnard L, Preval N, Howden-Chapman P, et al. The Impact of Retrofitted Insulation and New Heaters on Health Services Utilisation and Costs, Pharmaceutical Costs and Mortality. Evaluation of Warm Up New Zealand: Heat Smart. 2011. University of Otago, New Zealand..
- 25. Poortinga W, Rodgers SE, Lyons RA, et al. The health impacts of energy performance investments in low-income areas: a mixed-methods approach. Public Health Res 2018;6:1–21. [PubMed] [Google Scholar]
- 26. Poortinga W, Rodgers SE, Lyons RA, Anderson P, Tweed C, Grey C, et al. The health impacts of energy performance investments in low-income areas: a mixed-methods approach. Public Health Research. 62018. pp. 23–39. [PubMed] [Google Scholar]
- 27. Poortinga W, Rodgers SE, Lyons RA, Anderson P, Tweed C, Grey C, et al. The health impacts of energy performance investments in low-income areas: a mixed-methodsapproach. Public Health Research. 62018. p. 59–74. [PubMed] [Google Scholar]
- 28. Heyman B, Harrington B, Heyman A, The National Energy Action Research. A randomised controlled trial of an energy efficiency intervention for families living in fuel poverty. Hous Stud 2011;26:117–32. [Google Scholar]
- 29. Osman LM, Ayres JG, Garden C, et al. A randomised trial of home energy efficiency improvement in the homes of elderly COPD patients. Eur Respir J 2010;35:303–9. [DOI] [PubMed] [Google Scholar]
- 30. Page K, Hossain L, Wilmot K, Kim Y, Liu D, Kenny P, editors. The Victorian Healthy Homes Program. Research Findings. Melbourne: Sustainability Victoria, 2022. [Google Scholar]
- 31. Saeki K, Obayashi K, Kurumatani N. Short-term effects of instruction in home heating on indoor temperature and blood pressure in elderly people: a randomized controlled trial. J Hypertens 2015;33:2338–43. [DOI] [PubMed] [Google Scholar]
- 32. Carrere J, Belvis F, Peralta A, et al. Effectiveness of an energy-counseling intervention in reducing energy poverty: evidence from a quasi-experimental study in a Southern European city. J Urban Health 2022;99:549–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liddell C, Morris C, Lagdon S, editors. Kirklees Warm Zone: The Project and its health impacts: A Cost-Benefit Analysis. Ulster: Kirklees Council. 2011. [Google Scholar]
- 34. Peralta A, Camprubí L, Rodríguez-Sanz M, et al. Impact of energy efficiency interventions in public housing buildings on cold-related mortality: a case-crossover analysis. Int J Epidemiol 2017;46:1192–201. [DOI] [PubMed] [Google Scholar]
- 35. Pollard A, Jones T, Sherratt S, Sharpe RA. Use of simple telemetry to reduce the health impacts of fuel poverty and living in cold homes. Int J Environ Res Public Health 2019;16(16): 2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Poortinga W, Jones N, Lannon S, Jenkins H. Social and health outcomes following upgrades to a national housing standard: a multilevel analysis of a five-wave repeated cross-sectional survey. BMC Public Health 2017;17:927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Preval N, Keall M, Telfar-Barnard L, et al. Impact of improved insulation and heating on mortality risk of older cohort members with prior cardiovascular or respiratory hospitalisations. BMJ Open 2017;7:e018079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rodgers SE, Bailey R, Johnson R, et al. Emergency hospital admissions associated with a non-randomised housing intervention meeting national housing quality standards: a longitudinal data linkage study. J Epidemiol Community Health 2018;72:896–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tonn B, Hawkins B, Rose E, et al. Saving lives by saving energy? Examining the health benefits of energy efficiency in multifamily buildings in the United States. Build Environ 2023;228:109716. [Google Scholar]
- 40. Angelini V, Daly M, Moro M, et al. The effect of the Winter Fuel Payment on household temperature and health: a regression discontinuity design study (Public Health Research, No 71). Public Health Res 2019;7:1–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.