Abstract
Progesterone is a natural steroid hormone, while progestins are synthetic molecules. In the female reproductive system, progesterone contributes to the control of luteinizing hormone and follicle-stimulating hormone secretion and their pulsatility, via its receptors on the kisspeptin, neurokinin B, and dynorphin neurons in the hypothalamus. Progesterone together with estradiol controls the cyclic changes of proliferation and decidualization of the endometrium; exerts anti-mitogenic actions on endometrial epithelial cells; regulates normal menstrual bleeding; contributes to fertilization and pregnancy maintenance; participates in the onset of labor. In addition, it exerts numerous effects on other endocrine systems. Micronized progesterone (MP) is natural progesterone with increased bioavailability, due to its pharmacotechnical micronized structure, which makes it an attractive diagnostic and therapeutic tool. This critical literature review aims to summarize and put forward the potential diagnostic and therapeutic uses of MP in the field of endocrinology. During reproductive life, MP is used for diagnostic purposes in the evaluation of primary or secondary amenorrhea as a challenge test. Moreover, it can be prescribed to women presenting with amenorrhea or oligomenorrhea for induction of withdrawal bleeding, in order to time blood-sampling for diagnostic purposes in early follicular phase. Therapeutically, MP, alone or combined with estrogens, is a useful tool in various endocrine disorders including primary amenorrhea, abnormal uterine bleeding due to disordered ovulation, luteal phase deficiency, premenstrual syndrome, polycystic ovary syndrome, secondary amenorrhea [functional hypothalamic amenorrhea, premature ovarian insufficiency], perimenopause and menopause. When administrated per os, acting as a neurosteroid directly or through its metabolites, it exerts beneficial effects on brain function such as alleviation of symptoms of anxiety and depression, asw well as of sleep problems, while it improves working memory in peri- and menopausal women. Micronized progesterone preserves full potential of progesterone activity, without presenting many of the side-effects of progestins. Although it has been associated with more frequent drowsiness and dizziness, it can be well tolerated with nocturnal administration. Because of its better safety profile, especially with regard to metabolic ailments, breast cancer risk and veno-thromboembolism risk, MP is the preferred option for individuals with an increased risk of cardiovascular and metabolic diseases and of all-cause mortality.
Keywords: Micronized progesterone, Amenorrhea, Oligomenorrhea, Menopause, Perimenopause, Hormone therapy
Introduction
Progesterone is a natural steroid hormone, while progestins are synthetic molecules. In 1929, crystalline progesterone was isolated from the corpus luteum of sow. In 1934, its chemical structure was determined by Adolf Butenandt (Nobel Prize 1935). Progestins appeared in the late 30s and were initially used for birth control in the 50s. They were a more effective treatment than per os administrated natural progesterone which presented poor absorption and rapid metabolic decay. In 1984, micronized progesterone (MP), natural progesterone with increased bioavailability was synthesized. Its pharmacotechnical micronized structure preserves its potential of activity without presenting many of the side-effects of progestins [1]. Micronization, first employed in France, is currently employed in other European countries and in USA as well.
Because MP appears as an attractive diagnostic tool and a therapeutic alternative to progestins, this critical literature review aims to summarize and to put forward the potential diagnostic and therapeutic uses of MP in the field of endocrinology. To identify publications regarding the role of MP in endocrinology and its advantages, a systematic literature search for human studies was conducted in three electronic databases (PubMed, Cochrane and Medline) until september 2023 using combinations of the key terms “micronized progesterone”, “bioavailability” and “advantages in endocrinology”. In addition, a manual search of key journals and abstracts from the major annual meetings in the fields of endocrinology and reproductive gynecology was conducted.
Biochemistry and physiology of progesterone
Biochemistry of progesterone
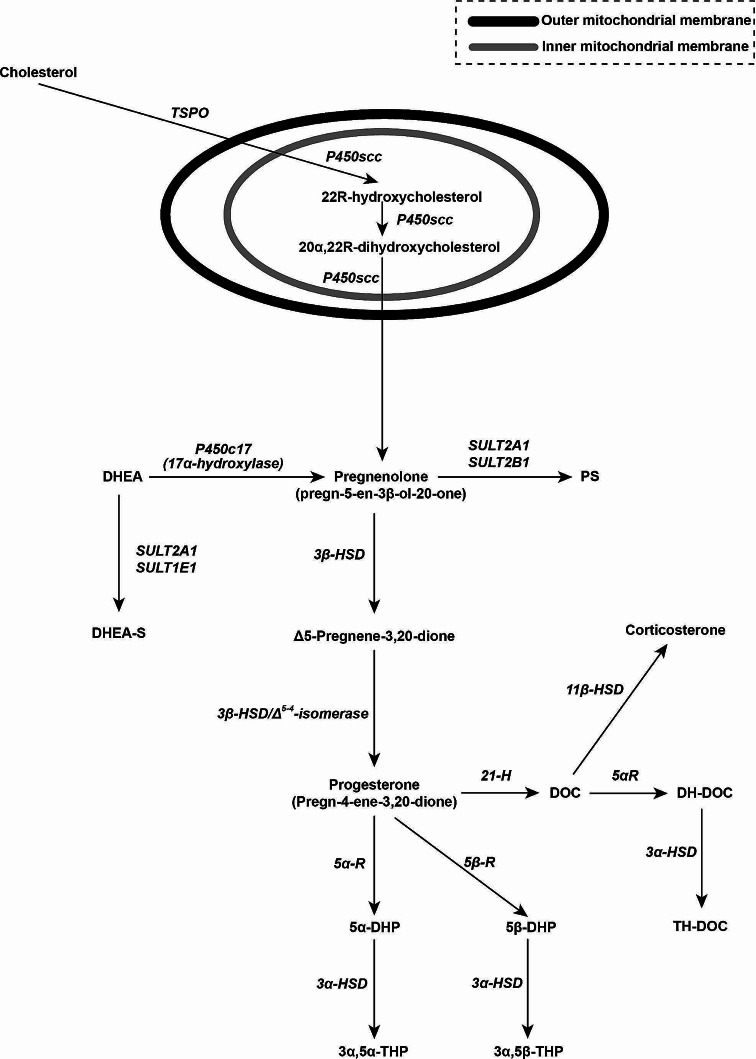
Progesterone is a C21-steroid hormone (pregn-4-ene-3,20-dione) [Fig. 1] which binds to plasma proteins such as albumin (over 80%, with low affinity; 42 min half-life) and corticosteroid binding globulin or transcortin (approximately 15–20%, with high affinity; 6 min half-life) [2]. The biological half-life of unbound progesterone in circulation is very short (approximately 5 min) [3]. Following intravenous injection, its half-life ranges widely from 3 to 90 min. Thus, although many authors suggest a single daily administation of MP per os, it is wiser to administrate it in two daily doses separated by 12 h. This way of administration might represent an inconvenience. Its metabolism is almost completed in first-pass through the liver and other organs (i.e. adrenal gland, ovary, gastrointestinal mucosa, brain, skin) [2]. Progesterone is synthesized by cholesterol (in two main steps) in the adrenal gland, the ovaries, the testis, the placenta and the central nervous system (CNS). Cholesterol undergoes double oxidation to two intermediate-diols (22R-hydroxycholesterol, 20α,22R-dihydroxycholesterol) [Fig. 1]. The latter is further oxidized [via cholesterol side-chain cleavage enzyme at the inner mitochondrial membrane] to pregnenolone, which is further converted to progesterone [4] [Fig. 1]. Progesterone is metabolized to 17α-hydroxyprogesterone. In the liver, progesterone can be hydroxylated by not steroid-specific cytochrome P450 enzymes. Of note, environmental chemicals and some drugs increase progesterone hydroxylation, resulting in a decrease in the concentration of progesterone in the body [5].
Fig. 1.
Biosynthesis of progesterone in the intra- and extra- mitochondrial cellular compartment and pathways of its metabolism to steroid hormones. translocator protein (TSPO), cholesterol side-chain cleavage enzyme (P450scc), 3β-hydroxysteroid dehydrogenase/Δ5−4-isomerase (3β-HSD)
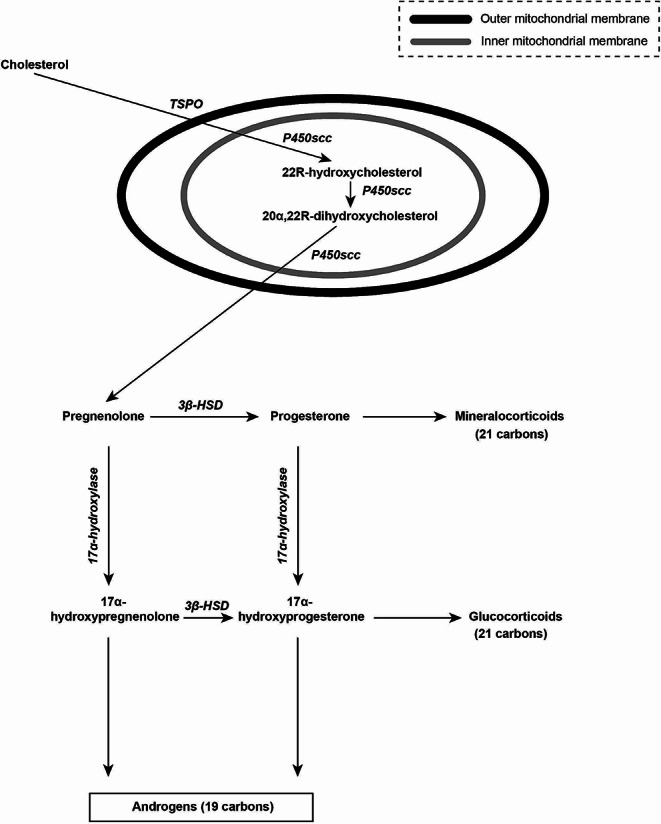
Neurosteroids (neuroactive steroids) are synthesized either in the brain or in an endocrine gland and then they reach the brain [6]. They are classified in prοneurosteroids [pregnenolone, Δ5-pregnene-3,20-dione, progesterone, pregnenolone sulfate, deoxycorticosterone (DOC), corticosterone], pregnane neurosteroids [5α-dihydroprogesterone, 3α,5α-tetrahydroprogesterone, 5β- dihydroprogesterone, 3α-5β-tetrahydroprogesterone, 5α-dihydrodeoxycorticosterone, tetrahydrodeoxycorticosterone], and androstane neurosteroids [(dehydroepiandrosterone (DHEA), dehydroepiandrosterone- sulfate (DHEA-S)] [Fig. 2]. Progesterone, a neurosteroid itself, is synthesized in the central (glia, neurons) and peripheral nervous system [7]. The crucial cholesterol side-chain cleavage enzyme is expressed in several brain areas (glia, neurons) in humans, with its greatest concentrations found in the olfactory bulb, caudate nucleus, thalamus, corpus collosum, amygdala, hippocampus, cerebral cortex and cerebellum [8]. In the brain, pregnenolone can be converted: to pregnenolone sulfate; to DHEA in neurons and astrocytes and then DHEA can be transformed to DHEA-S (via sulfotransferases, a conversion not yet clearly demonstrated in the human brain) [9]; to progesterone in two steps (via 3β-hydroxysteroid dehydrogenase and 3β-hydroxysteroid dehydrogenase/Δ5−4-isomerase activities, expressed in human oligodendroglial, astrocytes and neuronal cell lines) either in the cytoplasm or in the mitochondria [Fig. 2] [8]. Progesterone, in its turn, can be sequentially converted to neuroactive metabolites, such as 5α-dihydroprogesterone [via 5α-reductase (type 1, the most abundant isoform expressed in the brain of humans and other species)] and then to tetrahydroprogesterone or allopregnanolone synthesized de novo in the brain (via 3α- hydroxysteroid dehydrogenase), or 5β-dihydroprogesterone [via 5β-reductase (the expression of this enzyme in the human brain is debated)] and subsequently to 3α,5β- tetrahydroprogesterone or pregnanolone. Progesterone may also be converted to DOC [via 21-hydroxylase, the expression of this enzyme in the human brain is debated)] [10]. Subsequently, DOC is reduced in the neurosteroids dihydrodeoxycorticosterone and tetrahydrodeoxycorticosterone. Moreover, DOC may alternatively be converted to corticosterone [11]. Other neurosteroids which also have clinical and therapeutic importance, such as dihydrotestosterone and androstenedione (A4), result via the activity of enzymes investigated for their neural activity [9]. Other reductions of progesterone, by 5α- and 5β- reductase and 3β-hydroxysteroid dehydrogenase, result in the formation of other neurosteroids such as iso- and epi- pregnanolone, which, in CNS, are reduced to pregnanediols by 20α- and 20β- hydroxysteroid dehydrogenase.
Fig. 2.
Biosynthesis of progesterone in the intra- and extra- mitochondrial cellular compartment and pathways of its metabolism to neurosteroids. Prοneurosteroids [pregnenolone, Δ5-Pregnene-3,20-dione, progesterone, pregnenolone sulfate (PS), deoxycorticosterone (DOC), corticosterone], pregnane neurosteroids [5α- dihydroprogesterone (5α-DHP), 3α-5α-tetrahydroprogesterone (3α-5α-THP), 5β- dihydroprogesterone (5β-DHP), 3α-5β-tetrahydroprogesterone (3α-5β-THP), dihydrodeoxycorticosterone (DH-DOC), tetrahydrodeoxycorticosterone (TH-DOC)], androstane neurosteroids [dehydroepiandrosterone (DHEA), dehydroepiandrosterone-sulfate (DHEA-S)], translocator protein (TSPO), cholesterol side-chain cleavage enzyme (P450scc), DHEA, 17α-hydroxylase (P450c17), sulfotransferase 2 A1 (SULT2A1), sulfotranferase 2 B1 (SULT2B1), PS, sulfotranferase 1 E1 (SULT1E1), DHEA-S, 3β-hydroxysteroid dehydrogonase (3β-HSD), 11β-hydroxysteroid dehydrogonase (11β-HSD), 21 hydroxylase (21 H), deoxycorticosterone or 11-deoxycorticosterone or 21-hydroxyprogesterone (DOC), 5α-reductase (5α-R), 5α-dihydrodeoxycorticosterone (DH-DOC), 5β-reductase (5β-R), 3α-hydroxysteroid dehydrogonase (3α-HSD), 5α-dihydroprogesterone or allopregnanedione (5α-DHP), 5β-dihydroprogesterone or pregnanedione (5β-DHP), tetrahydrodeoxycorticosterone (TH-DOC), 3α-5α-tetrahydroprogesterone or allopregnanolone (3α-5α-THP), 3α-5β-tetrahydroprogesterone or pregnanolone (3α-5β-THP)
Physiology of progesterone
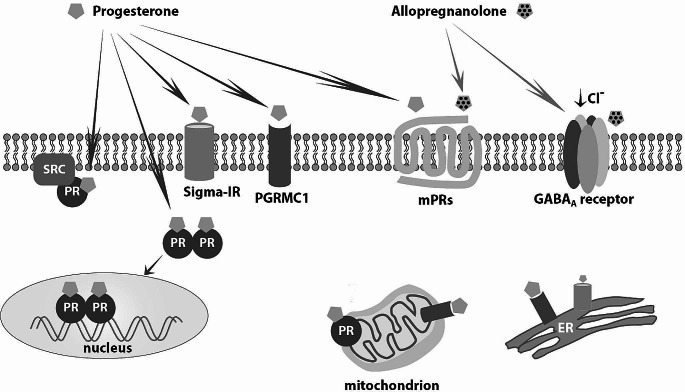
Actions of progesterone through classic progesterone and other receptors
Progesterone, secreted from the corpus luteum, dominates the luteal phase of menstrual cycle. Progesterone and progestins bind to progesterone receptors (PRs), while they can interfere with the receptors of other steroid hormones as well [Fig. 3]. Progesterone receptors are encoded by a single gene (11q22), are found in the cytoplasm and the nucleus, and are located throughout the body (i.e. in uterus, ovary, vagina, testes, breast, brain, vascular endothelium, thymus, pancreatic islets, osteoblast-like cells, lungs). Their main isoforms are PR-A (the commonest) and PR-B. The latter seems to act as a positive regulator of progesterone on progesterone response element (PRE). Progesterone receptor A (as well as PR-C) acts as a transcriptional repressor on PREs suppressing the transcriptional activity of PR-B as well as those of estrogen receptors (ER), glucocorticoid, androgen and mineralocorticoid receptors [12]. Increased concentrations of progesterone during luteal phase as well as progestins suppress the expression of ERα and ERβ in the endometrial epithelium [13]. Progesterone and progestins inactivate (via paracrine mechanisms)estradiol (E2) through 17β-hydroxysteroid dehydrogenase type 2 [converts E2 to estrone (E1)] and E1-sulfotransferase (conjugates E1 to sulphates) activities [2]. In addition, E2 induces the expression of PRs mainly via its activity on ER-α [14]. Estrogens differentially regulate PR-A and PR-B expression in the female hypothalamus, while in the endometrium they increase PR synthesis, preparing thus, the endometrium for the secretory phase [15]. Interestingly, in a mouse model, 17β-E2 was shown to regulate the differential expression of the PR isoforms in the ventromedial and arcuate nuclei and the medial preoptic area in the hypothalamus where it induced more PR-A than PR-B [16]. Administration of progesterone or progestins leads to decrease of estrogen and PRs. Stromal decidualization and subsequent thinning of the endometrium ensue.
Fig. 3.
Mediation of progesterone and allopregnanolone cellular actions via their membrane, receptors in the cytoplasmic membrane, the nucleus and organelles [mitochondrion, endoplasmic reticulum (ER)] in the central nervous system. SRC proto-oncogene (SRC), non-receptor tyrosine kinase [previously named: v-src avian sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog], progesterone receptor [(PR), the classic nuclear receptor], sigma-1 receptor (Sigma − 1R), membrane-associated protein progesterone receptor-membrane component 1 (PGRMC1), progesterone membrane receptor (mPR), γ-aminobutyric acid receptor A (GABA)A
Five isoforms (α, β, γ, δ, ε) of PRs have also been found on the cell membrane. When bound to progesterone, these trans-membrane proteins activate G-proteins mediating thus, acute non-genomic actions of progesterone. These highly expressed in the brain PRs mediate progesterone actions upon gonadotropin releasing hormone (GnRH) secretion, oocyte meiotic maturation, and granulosa cell apoptosis as well as the neuroprotective (anti-apoptotic) effects of progesterone and allopregnanolone [17]. Progesterone is also a ligand of progesterone receptor membrane component 1, which appears to mediate non-genomic actions of progesterone such as the anti-apoptotic action on granulosa cells [Fig. 3] [18]. Progesterone also acts as an antagonist of the sigma-receptors, both the sigma 1 and sigma 2 subtypes. Sigma1-receptors are chaperone proteins at the endoplasmic reticulum; they modulate intracellular calcium mobilization, extracellular calcium influx, N-methyl-D-aspartate-mediated actions, acetylocholine release, and may interfere with memory, learning, depression, stress reaction, and neuroprotection [Fig. 3] [19]. Furthermore, progesterone and some of its metabolites, such as 5β- dihydroprogesterone, are agonists of the pregnane X nuclear receptor, one of the most important defense mechanisms of the human body against toxic substances and chemical insults [20].
Progesterone is a potent antagonist of the mineralocorticoid receptor; a partial agonist of the glucocorticoid receptor (GR); a negative allosteric modulator of nicotinic acetylcholine receptors; a positive allosteric modulator of the γ-amino-butyric acid (GABA)Areceptor acting indirectly via its neurosteroid metabolites (such as 5α- dihydroprogesterone and allopregnanolone) [21–22]. Through the GABAAreceptor it exerts neuroprotective effects and plays a modulatory role in sleep, memory, sexual behavior, respiratory function, control of appetite, weight gain, and tumorigenesis in CNS [22].
Progesterone actions in the endocrine and the central nervous systems
Progesterone actions in the endocrine system comprise:
In the female reproductive system, progesterone: contributes to the control of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion and their pulsatility, via its receptors on the kisspeptin, neurokinin B, and dynorphin neurons in the hypothalamus under the main control of hypothalamus [23]; controls cyclical proliferation and decidualization of the endometrium; exerts anti-mitogenic actions on endometrial epithelial cells, by counter-acting estrogen effects and by modulating growth factor pathways [24]; increases the amounts of insulin growth factor (IGF)-binding protein 1 which inactivates IGF-1 when increased cyclically in endometrial stromal cells; represses epidermal growth factor, a mitogenic factor; suppresses the expression of matrix metalloproteinases in the same cells; regulates normal menstrual bleeding with progesterone-withdrawal bleeding mechanism (progesterone or progestins lead to cell differentiation, inhibit growth and are considered an inhibitor of endometrial cancerogenesis) [25–26]; enables successful implantation of the ovum; contributes to pregnancy maintenance; decreases maternal immune response and contractility of uterine smooth muscles; participates in the onset of labor. Progesterone or progestins are produce a secretory endometrium and preserve an established pregnancy. Interestingly, medroxyprogesterone, a progestin, sits on the osteoblast PR and on the breast glucocorticoid receptor 1 and it is biochemically the closest progestin to MP [27, 28].
In other endocrine systems, progesterone: contributes to the development of the lobuloalveolar breast; controls lactation [29]; peaks in the serum during luteal phase coinciding with increased proliferation of epithelial mammary cells and increased apoptosis (progesterone metabolites 3α- and 20α- hydroxyprogesterone act as apoptosis-increasing factors) [30]; inhibits competitively mineralocorticoid receptor inducing thus, natriuresis, which together with progesterone-induced vasodilation may lead to compensatory activation of the renin-angiotensin-aldosterone axis [31]; mediates signaling of insulin release in pancreatic cells; promotes gluconeogenesis, ketogenesis, lipoprotein-lipase action, fat deposition and protein catabolism [32]; increases core temperature during ovulation; enhances elasticity of the skin (PRs are found in the skin) [33]. Progesterone is produced and released in high levels by the corpus luteum following ovulation (at least at 5 ng/ml if a successful ovulation happened, while its average concentration is of 2–25 ng/ml). Thus, measuring progesterone concentrations or direct progesterone effects (i.e. quantitatively documented and sustained increase in core/basal temperature) is the only way in most situations to know that ovulation occurred [34].
In the brain, progesterone: increases serotoninergic neurotransmission via regulation of serotonin-related genes; supports normal brain development; exerts anti-inflammatorry action in damaged brain tissue via inhibition of neuron apoptosis, via reduction of brain edema and increase of macrophages and microglia near injured tissue, via triggering increase of the circulation of endothelial progenitor brain cells and possibly via remyelinization in CNS and peripheral nervous system [35–36]. Progesterone and neurosteroids in CNS act on brain function via ligand-gated ion channels and other cell surface receptors. Thus, they impact neuronal excitability by either genomic or rapid, non-genomic ways [6]. Neurosteroids (particularly progesterone and its metabolites) act beneficially on premenstrual syndrome (PMS), epilepsy, anxiety and depression, learning and memory, alcohol withdrawal, on which they can play a new therapeutic role.
Pharmacology and physiology of micronized progesterone
Micronization is a process which decreases particle size to less than 10 μm, increases the surface area of the active chemical particles and enriches the dilution rate of the micronized compound, increasing thus, gastrointestinal absorption, and bioavailability of the drug. Progesterone is lipophilic, stimulates bile salts secretion and emulsification, making this way the water-soluble micelles easily absorbed by the lymphatic system and bypassing thus, the first-pass metabolism via the liver. Sustained release MP tablets were designed by employing hydrophilic polymers which gradually swell, dissolve and erode in a continuous way in order to release the drug in a controlled manner over 16–24 h [37]. With sustained release tablets, there is minimal drug release in gastric fluids while gradual erosion of the polymeric matrix is achieved within the intestine. Thus MP escapes 5α-reductase, a progesterone-metabolizing enzyme, found in the upper intestinal wall and the intestinal bacteria. Sustained release MP is commercially available since 1986 [37]. The MP physiology is almost identical to that of natural progesterone demonstrating thus, many of the positive effects of the latter. Several routes of MP administration and their respective pharmakocinetic profiles have been tested [38]:
Per os administration: Radioimmunoassay measurement of progesterone, following per os administration of MP presents increased cross-reaction with progesterone metabolites resulting falsely to 8-fold greater concentrations than those obtained with liquid chromatography-mass spectrometry [39]. Mean plasma progesterone concentration achieved after per os administration of 100 or more mg MP, is at least as high as the luteal phase concentrations of progesterone [40]. Following 100–300 mg MP per os, maximum concentrations of progesterone are reached within 2–3 h, remain significantly elevated for up to 12 h and greater than baseline concentrations for at least 24 h. With a MP two-dose per os regimen (100 mg in the morning and 200 mg in the evening) for 5 days, progesterone plasma concentrations remain significantly elevated for up to 36 h, without returning to baseline until after 84 h [41]. A moderate increase in plasma concentration of progesterone is related to a greater increase at tissue level (i.e. endometrium, myometrium, breast, glandular and adipose tissue) remaining in therapeutic range of concentrations throughout 24 h [42]. The absorption of MP per os is related to individual differences regarding the site of absorption in the gastrointestinal tract and the level of absorption in adipose tissue [1]. Food ingestion enhances absorption of MP without altering the time of peak concentration [38]. It seems that maximum achieved concentration of MP augments with age, as a result of increased absorption and decreased clearance [38–42]. Although oral MP has been associated with more frequent drowsiness and dizziness in some patients, it can be well tolerated with nocturnal administration [43]. With oral administration, progesterone accounts for less than 20% of the dose in circulation while 5α- and 5β- reduced products, such as allopregnanolone and pregnanolone, account for around 80%. Micronized progesterone is less effective when administrated per os than via vaginal or muscular administration. With vaginal administration, circulating progesterone accounts for around 50% of the dose and its 5α- and 5β- reduced metabolites account for around 40% [44]. When MP is administrated per os, circulating DOC concentrations increase during the first hour after the oral administration and arrive at the maximum concentrations four hours later. Progesterone conversion to DOC occurs in the duodenum. Circulating DOC concentrations increase also following injectable MP forms in a more stable pattern. Increased DOC concentrations could reduce the antialdosteronic and anti-inflammatory effect of oral progesterone more than in the case of vaginal or parenteral administration [44].
Intravaginal administration: Intravaginal MP administration results to normal secretory transformation of the endometrium, possibly due to a first-pass progesterone uterine effect, while when compared to per os MP administration, it demonstrates a slower drug metabolism, longer time to peak concentration, and more constant, plateau-profile, plasma progesterone concentrations over time [45–46].
Intramuscular administration: It induces significantly greater peak plasma concentrations and areas under the concentration curve as compared to per os MP administration. Peak concentrations are achieved 8 h after administration, later than with per os MP, and decline thereafter, but still remain within the luteal phase range after 48 h [44].
Apart the soft MP capsules, hard MP capsules were introduced in drug industry, in 2004. This progesterone capsule is synthesized by diosgenin from the plant Dioscorea zingiberensis resulting into a chemical structure similar to that of natural progesterone. It is produced by solid dispersion at the nanometer level, in order to enhance progesterone dissolution rate. In a prospective randomized open-label trial from China, hard versus soft MP capsules were compared when administrated either per os or vaginally. In per os administration, metabolism and absorption of soft MP capsules were superior to that of hard capsules, while in vaginal administration hard MP capsules produce greater absorption concentrations and better pharmacokinetic profile [47].
Use of oral micronized progesterone in endocrinology
During reproductive life, MP is used for diagnostic purposes in the evaluation of primary or secondary amenorrhea. In addition, the use of MP, alone or combined with estrogens is a useful therapeutic tool in various endocrine disorders during the reproductive and menopausal life of women [Table 1].
Table 1.
Use of oral micronized progesterone in endocrine practice
| Diagnostic use (progesterone or progestin challenge test) |
| Primary and secondary amenorrhea |
| Therapeutic use |
| Primary amenorrhea |
| Abnormal uterine bleeding associated to ovulatory dysfunction |
| Luteal phase deficiency |
| Polycystic ovary syndrome |
| Secondary amenorrhea |
| Functional hypothalamic amenorrhea |
| Premature ovarian insufficiency |
| Perimenopause |
| Menopause |
Diagnostic use of micronized progesterone
The administration of a progesterone or progestins in a challenge test can provide information about a patient’s adequate endometrial estrogenization and outflow tract integrity and the hypothalamic-pituitary-ovarian (HPO) axis functionality. Because the use of MP is safe during pregnancy, it can be prescribed without hesitation as a challenge test [48]. In the litterature, MP has been prescribed per os in variable regimens: 300 mg once per day for 10 days [39]; 100 mg in the morning and 200 mg before bedtime for 7 days [49]; 400 mg once per day for 7 to 10 days [50]; 200 mg per day for 7 days [51]; 300 mg per day for 5–7 days [52]; 200 to 300 mg per day for 10 days [53]. It appears that there is no established consensus protocol for the administration of MP in this test. When 300 or 200 mg MP vs. placebo were administrated daily per os for 10 days in women 18 to 52 years old suffering from secondary amenorrhea or oligomenorrhea, withdrawal bleeding occurred in 90% of women on 300 mg, in 58% of women on 200 mg, and in 29% of women on placebo [48]. Side effects did not differ significantly among the studied groups. However, because some patients do not tolerate well progesterone, a shorter (5-day) course of 200 or 300 mg per day of MP is proposed. A progestin is often administrated for much shorter periods to induce menstruation and may be more appropriate in patients who do not tolerate well MP. In absence of withdrawal bleeding, this test can be repeated a few weeks later for 10 days with greater dose (300–400 mg MP per day). The test is considered positive when bleeding occurs within 7 days after completion of progesterone or progestin administration [54]. Absence of withdrawal bleeding may indicate outflow tract obstruction or low endometrial estrogen exposure [54]. The response to progesterone or progestin challenge can provide additional information about a patient’s estrogen status, especially in those cases in which there is overlay between functional hypothalamic amenorrhea (FHA) and polycystic ovary syndrome (PCOS) [53]. Moreover, progesterone or progestin challenge test can be prescribed to women presenting with amenorrhea or oligomenorrhea (particularly in PCOS) for induction of withdrawal bleeding in order to time blood-sampling for diagnostic purposes (hormonal measurements) in early follicular phase.
Therapeutic use of micronized progesterone
Primary amenorrhea
Primary amenorrhea is the failure of initiation of menses by the age of 13 in absence of secondary sexual characteristics or absence of menarche by the age of 15 regardless of the presence of normal growth and development of secondary sexual characteristics [55]. Its etiology comprises genetic, anatomical and functional defects including gonadal dysgenesis (i.e. Turner syndrome) (43%), müllerian agenesis (15%), physiological delay of puberty (14%), PCOS (7%), isolated GnRH deficiency (5%), transverse vaginal septum (3%), hypothalamic amenorrhea (due to stress and/or energy deficit) (2%) and hypopituitarism (2%). Less common etiologies (≤ 1% each) include imperforate hymen, complete androgen insensitivity syndrome, hyperprolactinemia/prolactinoma, other pituitary tumors, congenital adrenal hyperplasia, CNS defects, craniopharyngioma, Cushing syndrome and hypothyroidism [56–57]. Τreatment depends on the etiology and aims at correcting the underlying pathology, enabling fertility and preventing complications such as osteoporosis. Patients with uterus and primary (i.e. gonadal dysgenesis, etc.), secondary (i.e. hypopituitarism, etc.) or tertiary (i.e. isolated GnRH deficiency, hypothalamic amenorrhea, etc.) will need initiation of hormone therapy, consisting of estrogen only (if they present inadequate breast development) or estrogen combined with cyclic progesterone or progestins for patients with a uterus and fully developed breasts. Progesterone or progestins administration will restore cycles and reduce the risk for endometrial hyperplasia [57]. Estrogen therapy is initiated with low doses between 11 and 12 years of age. After 2 years approximately of estrogen treatment, or earlier, particularly if a patient presents menstrual bleeding or spotting, progesterone or progestins should be added [58]. Micronized progesterone appears as a good therapeutic option because of its favorable safety profile, especially with regard to breast cancer and veno-thromboembolism risk, particularly in case of patients who present an increased risk of cardiovascular and all-cause mortality (i.e. Turner syndrome) [58–59]. A dose of 200–300 mg per day in a cyclic combined regimen has been proposed [60]. In a non-controlled retrospective study of a Turner syndrome cohort, the prolonged cyclic (10 days per month) use of either MP or medroxyprogesterone acetate or levonorgestrel showed no metabolic change, except for weight gain, which was significantly lesser with levonorgestrel [61]. Regimens of estrogen plus progesterone or progestins are cyclic combining an estrogen and progesterone or a progestin (for 10 to 14 days) [62]. Of note, MP plus transdermal estrogen treatment has been successfully used in patients with Turner syndrome undergoing in vitro fertilization (IVF) as well [63]. However, use of progestins is sometimes more appropriate than MP use. This could be the case in primary amenorrhea in Turner syndrome, when the side effect of weight gain is concerned [61]. In a double-blind 1-year randomized controlled trial (RCT) possible prevention of bone density loss was investigated in young women who suffered amenorrhea or ovulatory disturbances. Specifically, 61 physically activated normal-weight premenopausal women, who suffered the full range of hypothalamic adaptive, reversible reproductive suppressive changes, were enrolled in the study [64]. The full range of hypothalamic changes includes: amenorrhea, oligomenorrhea, anovulation, or short luteal phase cycles [65]. The participants were divided into four groups receiving cyclic medroxyprogesterone (10 mg/day for 10 days per month) plus calcium carbonate (1,000 mg/day); cyclic medroxyprogesterone with calcium placebo group; medroxyprogesterone placebo with calcium carbonate; and medroxyprogesterone placebo and calcium placebo, respectively. Bone density improved in women under cyclic medroxyprogesterone acetate, whereas in the placebo group bone density decreased. Calcium supplementation presented positive results but without statistical significance [64].
Abnormal uterine bleeding associated to ovulatory dysfunction
A positive therapeutic effect of progesterone in abnormal uterine bleeding (AUB) was recognized in the first half of 20th century. According to the International Federation of Gynecology and Obstetrics, chronic AUB is a bleeding from the uterine corpus which is abnormal in duration, volume, frequency, and/or regularity (cycle variation: ±4 days; cycles of ≥ 24 days to ≤ 38 days are considered normal in terms of frequency), and it has been present for the majority of the preceding 6 months. Acute AUB is an episode of heavy bleeding, requiring immediate intervention [66]. The term dysfunctional uterine bleeding (DUB), was previously employed in the absence of structural cause of AUB. Furthermore, ovulatory dysfunction (AUB-O), which may be present in a spectrum of menstrual abnormalities, encompasses disorders in which ovulation is either absent or infrequent or irregular [67]. Irregular progesterone production from the corpus luteum is involved in these pathologies [67].
In adolescence: In the first post-menarche year at least 50% of cycles are anovulatory and they can remain anovulatory for some years, propably due to improper function of the positive feedback of E2 to LH and subsequent absence of midcycle LH surge (immaturity or dysregulation of the HPO axis) [68]. Monophasic and anovulatory menstrual cycles ensue, follicles undergo atresia and become cystic, while progesterone is not produced because of non-developed corpus luteum [69]. Unopposed activity of estrogens, derived from ovarian follicles as well as from extragonadal androgen aromatization, induces endometrial proliferation followed by abnormal shedding of the endometrium [69]. Of note, obesity is an important contributor to anovulatory cycles in adolescents, while in some young women, particularly those with high body mass index, AUB may be an early presentation of PCOS [70]. Management of AUB in adolescence aims at preventing anemia and at establishing regular cyclic bleeding [71]. Progesterone or progestins are efficient in treating AUB due to AUB-O by stabilizing endometrial fragility and triggering apoptosis, thus inhibiting growth of the endometrium, while they inhibit angiogenesis and stimulate conversion of E2 to the less active E1 [71]. There is a great variation in the dose and type of progesterone or progestin as well as the schedule of administration proposed. Progestin-only therapy may be used to mature and slough the endometrium [72]. Oral MP can be used alone for maintenance therapy, at a dose of 200 mg each night for the first 12 days of each calendar month [73]. Another regimen of MP (200-400 mg, once daily for 2 weeks every 4 weeks) has been proposed for the treatment of heavy menstrual bleeding attributed to AUB-O [73]. The same daily dose of MP has been proposed for a longer period (for 21 days, starting on day 5) [73]. When initial control of bleeding is achieved, continuation of a per os progesterone- or progestin- only cyclic regimen (10–14 days starting on the 16th or 12th day of the cycle, respectively) is suggested for at least 6 months after bleeding control [74]. Cyclic progesterone therapy could be also recommended for adolescents with irregular cycles, far-apart cycles or heavy flow. It could be prescribed as oral MP therapy of 300 mg per day at bedtime. For adolescent patients with menstrual cycles of usually 26 to 32 days, suggested regimen is cyclic administration of MP from 14th to 27th day. Otherwise, in presence of shorter cycles (i.e. 21 to 26 days or shorter), suggested cyclic MP regimen could be initiated on the 12th up to the 25th day [75]. Sometimes an unpredictable heavy flow may occur after cyclic MP therapy. Clinical experience suggests that if this heavy or early flow persists, then the woman may need either an increase of the dose of cyclic MP therapy to 400 mg or daily MP treatment for three months [75].
In reproductive age: Among other etiologies, AUB ensues from hormonal disorders associated to AUB-O (chronic estrogen stimulation of the endometrium seen in PCOS or in hypothyroidism) [66]. Therapy should be tailored to each patient’s needs, taking into account medical history and comorbidities. In an RCT, vaginal MP or per os dydrogesterone were administrated cyclically to women with DUB for 3 months, resulting to a regular bleeding pattern at the end of the first month in 93% and 81% of the patients, respectively. No statistically significant difference was shown in menstrual recordings and endometrial histology between the two groups at the end of the treatment [76].
Luteal phase deficiency
Luteal phase deficiency is a condition of insufficient progesterone production to maintain a regular secretory endometrium and to allow normal embryo implantation and growth, although certain authors have disputed the contribution of this pathologic entity to subfertility [77]. It may increase the frequency of iron-deficiency anemia due to repeated cycles shorter than 24 days which are often accompanied by premenstrual spotting [78]. Currently, there is no pathognomonic test for the diagnosis of this pathologic entity. It is encountered in women with polycystic ovarian morphology, PCOS, thyroid and prolactin disorders, FHA, obesity, or it could be iatrogenic, due to assisted reproduction-related interventions [77]. To treat luteal phase deficiency, the underlying condition should be identified and corrected. Treatment with MP or a progestin seems reasonable although substantial studies on this therapeutic approach are missing. There is no consensus for the use of MP in luteal phase insufficiency.
Premenstrual syndrome
Premenstrual syndrome is characterized by recurrent moderate affective and physical symptoms that occur during the luteal phase in 3–8% of women and resolve with menstruation [79]. Clinically significant PMS consists of at least one affective (i.e. angry outbursts, exhaustion, anxiety, irritability, depression and mood swings) or somatic (i.e. bloating, breast tenderness, joint pain) symptom occurring during the five days before the onset of menses while present in at least three consecutive menstrual cycles [80]. The term premenstrual dysphoric disorder refers to the most severe form of PMS, in which symptoms of anger, irritability and internal tension are prominent [80]. Etiologically, an estrogen/progesterone imbalance in favor of the former has been proposed as the underlying basis for this syndrome [81], although patients with PMS and premenstrual dysphoric disorder seem to have normal concentrations of serum estrogen and progesterone [82]. It has been hypothesized that, in genetically predisposed women, PMS results from alterations in female gonadal hormones and CNS neurotransmitters such as serotonin (which appears to play the most important role), GABA, endorphins and other neurosteroid modulators [83]. Certain progesterone metabolites are barbiturate-like modulators of GABA receptors [84]. Allopregnanolone and pregnanolone are propably responsible for the anxiolytic and hypnotic effects of per os administrated progesterone [84] [Fig. 2]. In women with premenstrual dysphoric disorder, alterations in these neurosteroid metabolic pathways result in decreased conversion to either pregnanolone and/or DOC-derived neurosteroids [85], while patients with PMS present reduced sensitivity for GABAAreceptor allosteric agonists [86] [Fig. 2]. Luteal phase progesterone supplementation for PMS treatment might increase the concentrations of progesterone metabolites and, subsequently, enhance GABAAreceptor activation in the CNS [87]. Following vaginal administration of progesterone, these metabolites are not found in clinically significant concentrations [88]. Progesterone supplementation decreases luteal water retention due to its diuretic properties (promotion of renal sodium excretion) counteracting thus, fluid retention and bloating symptoms associated with increased activity of the plasma renin activity and aldosterone system in PMS [89].
In a 4-month double-blind crossover RCT with administration of MP per os or placebo to women with PMS, a beneficial effect of progesterone treatment for affective symptoms (anxiety, depression and stress) and somatic symptoms (swelling, hot flushes) was observed [90]. On the other hand, in a 3-month double-blind, placebo-controlled RCT in women with PMS, luteal administration of MP per os in high daily doses (1200 mg initially, 1760 mg mean dosage in the third treatment cycle) was more effective than placebo for the somatic symptoms, although no better regarding the overall symptomatology [91]. Furthermore, in a double-blind crossover trial, comparing premenstrual administration of MP per os with vaginal MP or matched placebo for 10 days in women with PMS, no difference was found among the three groups, in spite of a significant positive effect upon affective and somatic symptoms in all intervention groups [92]. Interestingly, in the per os MP administration group, increased concentrations of 5α- and 5β- pregnanolone in serum were found while a significant negative correlation between 5α-pregnanolone concentrations and anxiety scores was observed [92]. A meta-analysis of these three trials demonstrated a significant positive effect of MP per os over placebo [93]. In contrast, when RCTs on administration of progesterone suppositories or pessaries were analyzed, progesterone had no beneficial effect on PMS symptoms [93]. From the existing data, it seems that treatment with MP per os might be beneficial for managing PMS symptoms. Of note, progesterone hypersensitivity is sometimes linked to PMS. Sensitivity to sex hormones was initially reported in 1921 by H. Geber, who demonstrated a flare in the cyclic urticaria following administration of the patient’s own pre-menstrual serum [94]. Subsequently, cases of severe generalized erythema multiform caused by sensitivity to progesterone have been reported [95]. Perimenstrual fluctuations of sex hormones in women is probably, at least partially, responsible for different perimenstrual symptoms especially in autoimmune and pain-related conditions, such as headache and pelvic pain. Thus, severe PMS is related with high predominance (> 90%) of sensitivity to one’s own female hormones, such as progesterone and estradiol [95].
Polycystic ovary syndrome
Polycystic ovary syndrome represents the most common endocrine-metabolic disorder of reproductive age in women. Its prevalence, depending on different definitions, varies between 5 and 14% [96]. These definitions comprise clinical or biochemical hyperandrogenism, oligoanovulation, and/or polycystic ovarian morphology, while the majority of women with PCOS are insulin resistant and hyperinsulinemic [96–98]. Inadequate production of ovarian progesterone concentrations during both early, mid- and late luteal phase has been found in infertile women with either polycystic ovarian morphology or oligomenorrhea, as well as in women with PCOS-associated anovulation [97–100]. Luteal progesterone concentrations increase in PCOS women following treatment with metformin, suggesting that hyperinsulinemia/insulin resistance may be responsible directly and/or indirectly for the decreased progesterone concentrations. An inverse relationship between fasting insulin and progesterone sensitivity in the hypothalamus has been shown in hyperandrogenemic adolescent girls implying that insulin resistance may modulate hypothalamic sensitivity to progesterone as well [101]. Decreased luteal progesterone production contributes to increased frequency of GnRH pulsatiliy which results in increased LH production [102]. Increased LH concentrations, in their turn, lead to additional excessive ovarian androgen production, initiating thus, a vicious circle [101]. Of note, administration of flutamide, an anti-androgen, restores sensitivity of the GnRH pulse generator to the negative feedback of E2 and progesterone [101, 103]. In female rats, experimental hyperandrogenemia suppresses PR mRNA expression in the preoptic area in the hypothalamus, and abolishes LH surges [104]. To override the hyperandrogenemia-induced impairment of progesterone regulation of GnRH pulsatility and normalize menstrual cycle, treatment with MP in the adequate posology could be proposed [100] [Table 2]. There is a paucity of data on the utility and usage of MP as therapy for hyperandrogenemia and irregular cycles, in women with PCOS. In these women, short-term treatment with MP per os resulted either to isolated reduction of LH concentrations alone or together with total testosterone concentrations [103] [Table 2]. Per os MP had beneficial effects on insulin resistance or lipids in these women [51, 105].
Table 2.
Suggested doses, administration routes, regimens and side effects of micronized progesterone administrated in PCOS patients [day (d), once a day (q.d.)] (*Concentrations of 17-OH P and HOMA-IR values increased and decreased, respectively, following MP administration. Progesterone and 17-OH P concentrations were significantly lower during menstrual bleeding, whereas LH concentrations were significantly decreased and HOMA-IR values increased)
| Reference | Aim | Regimen and administration route | Side effect | Primary outcome |
|---|---|---|---|---|
| Woods et al., 2002 [49] | Induction of withdrawal bleeding |
100 mg MP q.d. per os (morning) and 200 mg MP q.d. per os (before bedtime) x 7 d |
Non reported | Effects on androgens |
| Livadas et al., 2010 [51] | Induction of withdrawal bleeding | 200 mg MP q.d. per os x 7d | Non reported | Effects on hormones and glucose metabolism* |
| Bagis et al., 2002 [105] | Evaluation of insulin sensitivity | 300 mg MP q.d. per os or 600 mg MP vaginally x 10d | Non reported | Effects on glucose metabolism, lipids and hormones |
| Stanosz et al., 2014 [109] | Avoid hyperplastic endometrium in PCOS patients with preinvasive endometrial cancer | 50 mg MP q.d. vaginally x 6d followed by 100 mg MP q.d. vaginally x 6d, plus 17β-E2 transdermally (22 d cycle) | Non reported | Effects on hormones, lipids and endometrium |
In PCOS, endometrial hyperplasia ensues from persistent, due to anovulation, estrogen stimulation, while moderately elevated concentrations of E2 result from the peripheral aromatization of A4 to E1 in the adipose tissue of the frequently overweight PCOS patients. In addition, free E2 is increased in the circulation in the context of hyperinsulinemia, due in part to insulin down-regulation of sex-hormone-binding globulin (SHBG) [106]. In face of this accentuated unopposed estrogen activity in women with PCOS, per os MP is beneficial, regarding endometrial hyperplasia, while it downregulates endometrial androgen receptors, found in increased numbers in these women [107–108] [Table 2]. In young women with PCOS and concomitant, primary, pre-invasive endometrial cancer, a 6-month treatment with vaginally administrated MP, in combination with transdermal patches of E2, led to increased estrogens(E1, E2) and progesterone concentrations and a normal histopathologic picture without neoplasmatic texture of the endometrium [109] [Table 2]. One year after completion of the study, 14 out of 57 women were pregnant and delivered healthy newborns at term. In PCOS, there are therapeutic choices among progestins, such as spironolactone. Under certain circumstances, a progestin might be administrated for much shorter periods to induce menstruation or to prevent mid-cycle bleeding as it is the case of spironolactone therapy in PCOS. Treatment of PCOS with 100 or rarely 200 mg per day of spironolactone, for 6 to 9 months, is very effective in most cases of PCOS, for improvement of hirsutism, acne and seborrhea [110].
Secondary amenorrhea
Functional hypothalamic amenorrhea
Functional hypothalamic amenorrhea is a form of chronic anovulation unrelated to identifiable organic causes (diagnosis of exclusion) [53]. Common causes include nutritional restriction and/or excessive exercise, with negative energy balance, and extreme stress, which are associated with functional reduction in GnRH drive and subsequent decrease in LH pulse frequency [111–112]. While gonadotropin concentrations are insufficient to maintain full folliculogenesis and ovulatory ovarian function, the hypothalamic-pituitary-adrenal axis is activated and patients present with relative hypercortisolemia [111–112]. Functional hypothalamic amenorrhea is commonly encountered in female athletes manifesting as the “female athlete triad” (low energy availability, menstrual dysfunction, and low bone mineral density (BMD) [113]. Genetic predisposition and endocrine-disrupting chemicals, such as bisphenol A and some polychlorinated biphenyls, have been implicated in the pathogenesis of FHA [114–115]. Prolonged follicular or inadequate luteal phases may also be observed. Therapeutically, correction or amelioration of causal behavioral factors can enable ovarian, neuroendocrine, and metabolic recovery. Oral contraceptives do not prevent bone loss in women with FHA [116]. Short-term therapy with transdermal E2 and cyclic MP or progestins per os have been proposed for adolescents and women without restoration of menses after 6 to 12 months of nutritional, psychological and exercise-related interventions, especially in case of low BMD and/or evidence of skeletal fragility [117]. Suggested regimen includes 17β E2 patches (100 µg) applied continuously, in combination with cyclic MP 200 mg for 12 days every month, targeting endometrial protection [117]. Hormone therapy, however, and induced menses may give a false sense of security despite persistence of FHA-related deleterious effects if causal factors are not corrected [53].
Premature ovarian insufficiency
Premature ovarian insufficiency (POI), previously referred to as premature ovarian failure, manifests as hypergonadotropic hypogonadism before the age of 40 years with poorly understood etiology (no identifiable cause in 90% of the cases) [118]. There is a lack of international consensus on diagnostic criteria for POI. Its incidence is approximately 1 in 250 by age 35 years and 1 in 100 by age 40 years [119]. Patients suffer from climacteric symptoms, subfertility, osteoporosis, and cardiovascular disease [120]. Hormone therapy is recommended til the normal average age of menopause [118, 121]. The European Society of Human Reproduction and Embryology recognizes, in their guideline, strong evidence for per os cyclic combined treatment to protect the endomerium [122]. An ACOG Committee on Gynecologic Practice recommended daily estrogen therapy with 100 µg of transdermal E2 or 1–2 mg E2per os, or 0.625–1.25 mg conjugated equine estrogens per os, combined with either cyclic administration of 200 mg of MP or 10 mg medroxyprogesterone acetate per os, daily, for 12 days each month, or continuous daily administration of 100 mg MP or 2.5-5 mg medroxyprogesterone acetate per os [123]. Because MP appears to have a better safety profile when compared to progestins in multiple trials in postmenopausal women, it is considered a first-line therapeutic choice [124]. According to recently published data, both MP and medroxyprogesterone acetate had a neutral effect on the global coagulation assay, when administrated cyclically in women with POI treated with transdermal E2 [125]. Although, a positive effect on traditional cardiovascular disease markers was noted only in the MP treatment arm, there was no significant change in carotid-femoral pulse wave velocity, a biomarker with greater positive predictive value for cardiovascular events [126]. With regard to treatment tolerability, MP appeared to be better tolerated than medroxyprogesterone acetate in estrogen-treated women with POI, with fewer women reporting psychological concerns (mood swings and irritability) [127]. Compared to a standard regimen with ethinylestradiol and norethisterone per os, replacement with E2 and vaginal MP in women with POI resulted in lower blood pressure, better renal function, and less activation of the renin-angiotensin system [128]. Furthermore, in a prospective pilot RCT in patients with POI, administration of vaginal MP resulted in significantly more in-phase endometria (examined by endometrial histology) and significantly greater progesterone and lower LH and FSH serum concentrations on day 21 of the cycle (considered as day 7 of the luteal phase) when compared with dydrogesterone per os [129]. Vaginal, but not per os MP administration led to secretory transformation of the endometrium in POI patients on estrogen therapy [130].
Perimenopause
The term perimenopause is used to describe the time before and after menopause which begins with the initiation of the early menopausal transition (Stage − 2, according to the Stages of Reproductive Aging Workshop criteria) characterized by a persistent difference of 7 days or more in the length of consecutive cycles, elevated but variable early follicular phase FSH concentrations, low antimüllerian hormone concentrations and antral follicle count; it ends 12 months after the final menstrual period [131]. Perimenopause-related disorders (i.e. AUB, hot flushes and night sweats) may constitute a significant health burden. Progressive oocyte depletion and abnormal follicular development lead to anovulatory cycles which result to decreased progesterone production [68]. Thus, perimenopause is characterized by unopposed estrogen production [132]. Vasomotor symptoms (VMS), also called hot flushes/flashes and night swets, are the hallmark of the period of perimenopause and menopause. They affect the majority of menopausal women within a range of mild, moderate and severe intensity [133]. They may start during perimenopause or during the postmenopausal period and might last up to 5 to 8 years. The primary reason for treatment of VMS during perimenopause and menopause is the fact that they cause distress in the affected women and a worsering in their quality of life [134]. Vasomotor symptoms have also been associated with adverse effects on other systems, such as the cardiovascular system [135]. Thus, certain authors suggested that the effective treatment of VMS might be useful for treating the effects of menopause upon other areas of female physiology as well [136–137]. Treatment of perimenopausal symptoms is important for the reasons referred above. The hormonal changes during this women’s midlife transition, which is for the majority of the women a long period of 2 to 10 years, include peripheral blood estradiol concentrations greater than premenopausal ones and decreased progesterone concentrations [131, 138, 139]. In detail, the 2001 Stages of Reproductive Aging Workshop proposed a staging system for ovarian aging including menstrual and qualitative hormonal criteria to define each out of seven stages. In detail, during late reproductive/premenopausal period FSH concentrations vary, while antimüllerian hormone and inhibin B concentrations are low. The last two hormones continue to decrease during all the following perimenopausal and menopausal periods, till very low concentrations found at the early postmenopausal years [131, 138, 139]. In the published literature menopausal hormone therapy seem to be more effective for VMS when compared to placebo. However, a 25% of treated women discontinue menopausal hormone therapy due to adverse effects, such as menstrual disturbances, breast pain or lack of effectiveness. Taking this data into consideration, recommendation of menopausal hormone therapy for perimenopausal VMS treatment could not be a universal policy [140]. Regarding oral combined hormonal contraceptive, there is not documented a statistically significant improvement when compared to placebo in the treatment of perimenopausal VMS [141]. In addition, according to a pilot 50-days-study there is no statistical difference in the prevalence of VMS in perimenopausal women on levonorgestrel intrauterine device (LNG-IUD) with E2 treatment versus women on placebo [142]. There is currently no clear recommendation of how to best and most safely treat perimenopausal VMS [134].
Cyclic progestin therapy is proposed to replace the decreased or absent progesterone concentrations during the second phase of the cycle at this period of life [68]. Although data are scarce at present, progesterone treatment (specifically MP per os) may be recommended for different indications in these women (i.e. anemia-inducing heavy menstrual flow due to estrogen preponderance over progesterone concentrations) [143]. In a RCT in 189 perimenopausal women, comparing treatment with MP (300 mg daily per os) or placebo taken for a 3-month period, self-reported perceived decrease in intensity of VMS and improvement in night sweats were significantly greater in patients treated with MP vs. placebo [144]. Participants on daily 300 mg MP therapy at bedtime perceived, apart from significantly decreased night sweats and improved sleep quality, significantly decreased perimenopausal interference with daily activities, too. The mean Perimenopausal Interference Questionnaire on the third month of this RCT showed a significantly greater improvement in patients treated with oral MP than in those treated with placebo. These results suggest women on MP therapy have less symptomatic daily lives than those on placebo [134]. Duration and intensity of bleeding as well as endometrial thickness decreased significantly, after 6 months of treatment with vaginal application of MP for 16 to 12 days from the 10th or 14th day of the menstrual cycle, respectively [145]. In premenopausal women with endometrial hyperplasia and AUB, MP per os had significantly fewer metabolic side effects compared to the progestin lynestrenol and it was equally effective for endometrial protection, although in women older than 45 years it is less effective than lynestrenol [146]. In another trial, 300 mg/d MP administrated per os on days 15–24 of each cycle for 6 months in women with AUB (related to anovulation or incomplete progesterone effect), although less effective for cycle control compared to 15 mg/d norethisterone, it had an apparent advantage over the latter with regard to lipid profile. Many of these patients were perimenopausal. Hyperplastic changes of the endometrium disappeared during the first three cycles of the 6-month therapy with both molecules, but their carry-over effect was short, suggesting that therapy should be administrated long-term to these women [147]. Because perimenopausal women present erratically greater concentrations of estrogens and lower progesterone concentrations, treatment only with progesterone may be advantageous compared to combined hormone therapy [144]. Of note, treatment with MP or dydrogesterone combined with E2valerate, respectively, improved sleep quality of perimenopausal and postmenopausal women who suffered from insomnia in a prospective RCT [148].
While the association between cyclic progestins and perimenstrual symptoms, headaches and migraine has long been recognized, there are no data regarding the effect of MP on migraine [149]. In a RCT on 172 women (the Perimenopausal Estrogen Replacement Therapy study) MP (200 mg/d per os for 12 days, every 2 to 3 months) was administrated per os for 12 months, for endometrial protection, to euthymic perimenopausal and early postmenopausal women who also received transdermalE2 (patches of 0.1 mg). During the intervention, rates of clinically significant depressive symptoms (CES-D score ≥ 16) were found to be 17% in the active treatment group and 32% in the placebo group, suggesting that this combination prevents the development of clinically significant depressive symptoms in this population. This effect was independent from treatment-induced amelioration in menopausal symptoms [150]. In addition, in healthy perimenopausal and early postmenopausal women, aged 45–60, 12-month treatment with 0.1 mg/day transdermal E2 and cyclical 200 mg/day MP for 12 days tended to improve cardiac autonomic control and prevented age-related changes in stress reactivity and endothelial function [151].
Menopause
Natural menopause is defined as the permanent cessation of menstruation, determined retrospectively, after 12 months of amenorrhea without any other obvious pathologic or physiologic cause [152]. Up to 57% of women report onset or significant increases of VMS at menopause [153], while they admit that hormone therapy is highly effective for the treatment of these symptoms [154]. Because unopposed estrogens have been demonstrated to increase the risk for endometrial cancer, a combined estrogen and progestin continuous hormone therapy is strongly recommended in women with an intact uterus [155]. Progesterone and progestins do not behave all in a similar way with regard to potential adverse metabolic effects or associated breast cancer risk when combined with long-term estrogen therapy [156–158]. Two hundred to 300 mg MP daily combined to estrogen therapy are devoid of side effects on blood pressure, lipid profile or glucose homeostasis and display physiologic effects on the endometrium [159–162]. This combined therapy with MP is a natural and safer option in comparison with combined therapies with progestins, though not yet proven in a RCT [163–165].
In a single 3-month randomized double-blind placebo-controlled trial in healthy, nonsmoking, menopausal women, 300 mg MP alone administrated per os daily, were significantly more effective than placebo in improving frequency and score of VMS [166] [Table 3]. Four weeks after the end of the trial, the beneficial effect of MP (but not with placebo) on VMS persisted, although at a lesser extent [167] [Table 3].
Table 3.
Randomized control trials with administration of MP to post-menopausal women. Suggested doses, administration routes, regimens and side effects of MP and placebo [once a day (q.d.)]. Side effects did not differ between MP and placebo administration, while they were not severe
| Reference (participants in MP) |
Aim | Regimen and administration route | Side effects of MP | Side effects of placebo | Primary outcome |
|---|---|---|---|---|---|
|
Hitchcock et al., 2012 [166] (75) |
Efficacy of MP regimen | 300 mg MP q.d. per os at bedtime |
Abdominal sensation, depression, anxiety, dizziness, breast lump, daytime drowsiness, dry mouth, facial swelling, rash, vasomotor symptoms, nausea, insomnia, mastalgia, multiday menstrual bleeding. |
Insomnia, leg pain, initial daytime drowsiness, weight gain. | Vasomotor symptoms |
|
Prior et al., 2012 [167] (75) |
Efficacy of MP regimen | 300 mg MP q.d. per os at bedtime | No serious side effects | No serious side effects |
Vasomotor symptoms, withdrawal effects |
|
Schüssler et al., 2008 [172] (10) |
Efficacy of MP regimen | 300 mg MP q.d. per os in the evening x 21d | Non reported | Non reported | Sleep quality, cognition |
When four different molecules (MP, medroxyprogesterone acetate, nomegestrol acetate, dydrogesterone) were administrated for 12 cycles to 100 recently menopaused women for at least 12 months combined with transdermal E2 cyclically, transvaginal ultrasonography showed a similar increase in endometrial thickness after treatment in all groups. Administration of 200 mg/day MP was associated with more irregular bleeding pattern and significantly earlier appearing bleeding episodes than in patients receiving the three progestins [168]. In another multicenter, randomized, parallel group study, when chlormadinone acetate was compared to MP combined with transdermal E2 in a combined cyclic therapy in 336 healthy postmenopausal women, chlormadinone acetate was as protective regarding endometrial hyperplasia as MP (96.3% and 92.0% of success, respectively), but a secretory endometrium was found in 81.5% of the chlormadinone acetate patients, compared to only 50.7% in the MP group. Unscheduled bleeding, spotting and/or metrorrhagia, were more frequent under MP than under chlormadinone acetate (17.9% and 13.7%, respectively), while the beneficial effects on hot flushes were more important in the chlormadinone acetate than in the MP group [169].
In the brain, oral MP is rapidly converted into allopregnanolone, which, acting via GABAAreceptors, decreases anxiety and induces sleep [94]. In an unblinded observational study, postmenopausal women who changed their hormone therapy from a medroxyprogesterone acetate- to a MP- containing regimen experienced improvement in VMS and somatic complaints, as well as in symptoms of anxiety and depression, while fewer side effects and greater overall satisfaction with the MP-containing regimen were reported [164]. However, in another 91-day, single-blind pilot randomized study, neither 5 mg/day medroxyprogesterone acetate nor 200 mg/day MP per os, both combined with conjugated equine estrogens, had an effect on mood in normal, non-depressed and non-anxious early postmenopausal women [170]. In any case, menopausal women with intense sleep problems can be effectively treated with oral MP alone [167]. The light sedative effect of oral MP is created by its metabolites, in particular 5α- and 5β- allopregnanolone. Progestins are not converted into these metabolites and thus, they have no soporific effect [156]. Administration of oral non-micronized progesterone improves falling asleep when given at bedtime and may also restore disturbed sleep [171]. A randomized double blind cross-over trial documented significant increases in early rapid-eye movement sleep, decreased sleep interruption and no changes in morning neurocognitive function in menopausal women treated per os with 300 mg MP daily compared to placebo for 21 days [172] [Table 3]. Interestingly, a recent RCT comparing the sleep quality of peri- and post- menopausal women with insomnia, who received daily 1 mg E2valerate combined with either 10mg dydrogesterone or 100 mg oral MP for 3 months, showed an improvement in sleep quality with both regimens, without significant difference between them [150]. Importantly, a recently published systematic review and meta-analysis of RCTs examining the efficacy of MP upon sleep predominantly in postmenopausal women, showed improvement of various sleep parameters on MP, including total sleep time and sleep onset latency, and self-reported sleep outcomes, though studies were inconsistent [173]. All studies employing polysomnography showed improvement in sleep parameters with per os doses of 200-300mg MP. Findings of another recent systematic review and meta-analysis support the use of transdermal 17β-Ε2 combined with MP for at least 6 months in menopausal women with sleep disturbance [174].
Regarding memory, in a small double-blind RCT, the administration of 200 mg MP per os daily to menopausal women from days 1 to 14 combined with 0.625 mg conjugated equine estrogens daily in 28 days cycles resulted to better performance in a working memory test compared to women who received either 10 mg medroxyprogesterone acetate or placebo combined with 0.625 mg conjugated equine estrogens [175]. Thus, it appears that the improvement in working memory was due to MP combined with conjugated equine estrogens and not conjugated equine estrogens alone. Working memory, the ability to hold in mind and manipulate information to produce a response, involves mainly the prefrontal cortex. Thus, the MP-conjugated equine estrogens combination could be beneficial on the prefrontal cortex, when its function declines with age [175–176].
Summary
Micronized progesterone is natural progesterone presented in a pharmacotechnical structure which increases its bioavailability. As it preserves its full potential of activity, while exempt of many of the side-effects of progestins, it may be considered as an attractive diagnostic and therapeutic pharmaceutical substance. For diagnostic purposes, it is used to provide information about a patient’s adequate endometrial estrogenization and outflow tract integrity as well as the HPO axis functionality (progesterone or progestin challenge test). Therapeutically, oral MP is useful in treating several endocrine disorders. In cases of unopposed estrogen exposuse, in women with an intact uterus, cyclic or continuous administration of MP reduces the risk for endometrial hyperplasia which is associated to AUB and endometrial cancer.
In patients with a uterus and fully developed breasts presenting primary amenorrhea, estrogen combined with cyclic MP is proposed as hormone therapy. Because of its better safety profile, especially with regard to breast cancer and veno-thromboembolism risk, MP is the preferred steroid molecule for individuals with Turner syndrome, who exhibit a three- to four- fold increase in cardiovascular and all-cause mortality and an increased risk of metabolic diseases.
In adolescent patients with AUB-O, oral MP can be used alone as a regimen for maintenance therapy and for treating heavy menstrual bleeding, while in patients of reproductive age vaginal MP has been also shown to be effective [76]. Treatment with MP seems a reasonable option for patients with short cycles and anemia in the context of luteal phase insufficiency [78]. Nevertheless, at the moment, there is no consensus regarding progesterone administration protocols for this pathologic entity.
Treatment with oral MP might be beneficial for managing PMS symptoms, as it has been hypothesized that an estrogen/progesterone imbalance in favor of the former is implicated in the pathogenesis of PMS [81]. In patients presenting PMS and premenstrual dysphoric disorder, use of MP per os during the luteal phase might be justified, in order to increase the concentrations of progesterone metabolites and, subsequently, enhance GABAAreceptor activation in CNS [87]. Micronized progesterone decreases luteal water retention due to its diuretic properties counteracting thus, the fluid retention and bloating symptoms of premenstrual dysphoric disorder [89]. Further research is justified regarding the use of MP in premenstrual dysphoric disorder due to paucity of RCTs.
In PCOS, treatment with MP can be justified by the multiple potential mechanisms of progesterone implication in the pathogenesis and manifestations of the syndrome (i.e. inadequate production of ovarian progesterone during the luteal phase; decreased hypothalamic sensitivity to progesterone-mediated negative feedback due to hyperandrogenemia-induced impairment of progesterone regulation of GnRH pulsatility) [101–102]. Interestingly, available data are limited. In women with PCOS of reproductive age, treatment with MP per os reduces LH and total testosterone concentrations and exerts beneficial effects on insulin resistance and lipids [51, 105]. In premenopausal women with PCOS and endometrial hyperplasia, MP administrated per os controls endometrial hyperplasia [107–108]. Of note, in young women with PCOS and concomitant, primary, preinvasive endometrial cancer, a 6-months vaginal administration of MP in combination with transdermal E2 reestablishes normal histopathological endometrial picture [108].
In FHA patients presenting chronic anovulation, cyclic administration of MP, combined with transdermal estrogen can be beneficial [54]. In principle, therapeutic interventions should, at first, focus on correction or amelioration of the causal nutritional, psychological and exercise-related factors [54, 115]. However, because bone health may be compromised even after 6 to 12 months of amenorrhea, short-term therapy with cyclic administration of MP, combined with transdermal estrogen (not oral contraceptives, which appear not to prevent bone loss) have been proposed for adolescents and young women [117].
In women with POI, evidence is limited regarding the therapeutic effect and role of progesterone or progestins used in hormone therapy [118]. In POI, when comparing cyclic to continuous MP administration combined with estrogens, it appears that cyclic treatment protects better the endometrium [122]. In these patients, MP could be considered as first-line therapeutic choice, due to its better safety profile in postmenopausal women, when compared to progestins [124].
In perimenopausal women, cyclic MP per os has been shown an effective treatment for VMS, peri- and post- menopause-associated insomnia and symptoms of anxiety and depression, while being superior to norethisterone with regard to lipid profile [147]. Furthermore, MP may be efficacious for anemia-inducing heavy flow, resulting from endometrial hyperplasia due to the imbalance between E2 and progesterone concentrations (in favor of the former) [131–132, 143]. Replacing the decreased or absent progesterone concentrations during the second phase of the cycle with chronic oral MP administration, in long cycles, stabilizes the endometrium and reduces its thickness. Because these women present erratically greater concentrations of estrogens, progesterone-only treatment may be advantageous compared to combined hormone therapy [143]. It appears that MP seems an efficacious and safe treatment for most perimenopause related disorders.
In menopause, hormone therapy is highly effective for the treatment of VMS [154]. Importantly, MP has been shown to be as effective as progestins for controlling endometrial growth, with significantly fewer metabolic side effects [158]. Estrogen therapy together with 200 to 300 mg MP per os daily appear to be devoid of side effects on blood pressure, lipid profiles or glucose homeostasis [159–162]. Thus, MP use per os should be favored in menopausal women, because it is natural, safer and better tolerated compared to progestins [158, 161–164]. Though not yet proven in a RCT, combined treatment with oral MP and transdermal E2 can be considered as the optimal hormone therapy for menopause [165]. In the brain, oral MP is rapidly converted into allopregnanolone, which acts through GABAAreceptors to decrease anxiety and induce sleep [93]. Furthermore, there are findings supporting the association between mood effects and allopregnanolone serum concentrations during progesterone treatment [175]. The light sedative effect of MP is produced by its metabolites, found in clinically significant concentrations only after oral MP treatment and not vaginal MP administration nor treatment with progestins [156]. Importantly, there are data indicating an improvement in working memory in menopausal women treated with a combination of estrogens and MP [175].
In summary, MP is a natural steroid hormone with increased bioavailability exempt of many of the side-effects of progestins. Because the use of MP is safe during pregnancy, it can be prescribed without hesitation as a challenge test [48]. Its favorable safety profile, especially with regard to breast cancer, veno-thromboembolism risk and metabolic profile (i.e. insulin resistance, lipid profile, blood pressure, renal function), makes MP a good therapeutic option particularly in case of patients who present an increased risk of cardiovascular and all-cause mortality (Turner syndrome, menopause) [56, 58, 100, 128]. In several studies in menopausal women, MP had been shown to be as effective as progestins for controlling endometrial thickness, with significantly fewer metabolic side effects [45, 146]. Furthermore, when administrated per os, it acts as a neurosteroid directly or through its metabolites and exerts numerous beneficial effects on brain function.
However, when compared to progestins, MP was associated to more irregular bleeding in recently menopaused women, but greater doses could probably lead to better cycle control. In estrogen treated patients with POI, vaginal, but not per os MP administration led to secretory transformation of the endometrium, suggesting reduced bioavailability of MP regarding the endometrium upon oral administration. Of note, in a cross-sectional and non-controlled retrospective study of a Turner syndrome cohort, the prolonged cyclic use of MP was less favorable than levonorgestrel with regard to weight gain [61]. Although oral MP has been associated with more frequent drowsiness and dizziness in some patients, it can be well tolerated with nocturnal administration [43].
In conclusion, convincing data suggest that MP is an excellent therapeutic alternative in several endocrinologic pathologic entities. Tailoring the dose and regimen individually to patients may result in an efficacious treatment with a better safety profile than progestins. Further and thorough clinical research, particularly with carefully designed RCTs, should clarify the areas lacking sufficient evidence.
Abbreviations
- A4
androstenedione
- ACOG
American College of Obstetricians and Gynecologists
- AUB
abnormal uterine bleeding
- AUB-O
ovulatory dysfunction
- BMD
bone mineral density
- CNS
central nervous system
- DHEA
dehydroepiandrosterone
- DHEA-S
dehydroepiandrosterone- sulfate
- DOC
deoxycorticosterone
- DUB
dysfunctional uterine bleeding
- E2
estradiol
- E1
estrone
- ERs
estrogen receptors
- FHA
functional hypothalamic amenorrhea
- FSH
follicle-stimulating hormone
- GABA
γ-amino-butyric acid
- GnRH
gonadotropin releasing hormone
- HPO
hypothalamic-pituitary-ovarian
- IGF
insulin growth factor
- IVF
in vitro fertilization
- LH
luteinizing hormone
- MP
micronized progesterone
- mPR
progesterone membrane receptor
- PCOS
polycystic ovary syndrome
- PGRMC1
membrane-associated protein progesterone receptor-membrane component 1
- PMS
premenstrual syndrome
- POI
premature ovarian insufficiency
- PR
progesterone receptor
- PRE
progesterone response element
- RCT
randomized controlled trial
- SHBG
sex-hormone-binding globulin
- VMS
vasomotor symptoms
- 17-OHP
17- OH progesterone
Author contributions
E. M. contributed to the main concept of the review, collection of the data, writing of the manuscript and gave her final approval.P. P. contributed to collection of the data, writing of the manuscript and gave her final approval.M. P. contributed to the appraisal of collected data and gave her final approval.N. V. contributed to the appraisal of collected data and gave his final approval.G. M. contributed to the main concept of the review, writing of the manuscript and gave his final approval.
Funding
No funds, grants, or other support was received. The authors have no relevant financial or non-financial interests to disclose. This study was conducted in the context of the Postgraduate Studies Program “Research in Female Reproduction”, organized by Athens Medical School of the National and Kapodistrian University of Athens, Greece, in collaboration with the Midwifery Department, University of West Attica, Greece.
Open access funding provided by HEAL-Link Greece.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
The original online version of this article was revised to update the authors’ name and affiliations.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/26/2024
A Correction to this paper has been published: 10.1007/s11154-024-09887-9
References
- 1.McAuley JW, Kroboth FJ, Kroboth PD. Oral administration of micronized progesterone:a review and more experience. Pharmacotherapy. 1996;16:453–7. 10.1002/j.1875-9114.1996.tb02977.x [DOI] [PubMed] [Google Scholar]
- 2.Kuhl H. Pharmacology of estrogens and progestogens: influence of different routes of administration. Climacteric. 2005. 10.1080/13697130500148875. 10.1080/13697130500148875 [DOI] [PubMed] [Google Scholar]
- 3.Taraborrelli S. Physiology, production and action of progesterone. Acta Obstet Gynecol Scand. 2015. 10.1111/aogs.12771. 10.1111/aogs.12771 [DOI] [PubMed] [Google Scholar]
- 4.Schiffer L, Barnard L, Baranowski ES, Gilligan LC, Taylor AE, Arlt W, Shackleton Cedric HL, Storbeck KH. Human steroid biosynthesis, metabolism and excretion are differentially reflected by serum and urine steroid metabolomes: a comprehensive review. J Steroid Biochem Mol Biol. 2019. 10.1016/j.jsbmb.2019.105439. 10.1016/j.jsbmb.2019.105439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye L, Guo J, Ge RS. Environmental pollutants and hydroxysteroid dehydrogenases. Vitam Horm. 2014. 10.1016/B978-0-12-800095-3.00013-4. 10.1016/B978-0-12-800095-3.00013-4 [DOI] [PubMed] [Google Scholar]
- 6.Colciago A, Bonalume V, Melfi V, Magnaghi V. Genomic and non-genomic action of neurosteroids in the Peripheral Nervous System. Front Neurosci. 2020. 10.3389/fnins.2020.00796. 10.3389/fnins.2020.00796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schumacher M, Mattern C, Ghoumari A, Oudinet JP, Liere P, Labombarda F, Sitruk-Ware R, De Nicola AF, Guennoun R. Revisiting the roles of progesterone and allopregnanolone in the nervous system: resurgence of the progesterone receptors. Prog Neurobiol. 2014. 10.1016/j.pneurobio.2013.09.004. 10.1016/j.pneurobio.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 8.Pelletier G. Steroidogenic enzymes in the brain: morphological aspects. Prog Brain Res. 2010. 10.1016/S0079-6123(08)81011-4. 10.1016/S0079-6123(08)81011-4 [DOI] [PubMed] [Google Scholar]
- 9.Do Rego JL, Seong JY, Burel D, Leprince J, Luu-The V, Tsutsui K, Tonon MC, Pelletier G, Vaudry H. Neurosteroid biosynthesis: enzymatic pathways and neuroendocrine regulation by neurotransmitters and neuropeptides. Front Neuroendocrinol. 2009. 10.1016/j.yfrne.2009.05.006. 10.1016/j.yfrne.2009.05.006 [DOI] [PubMed] [Google Scholar]
- 10.Stoffel-Wagner B. Neurosteroid biosynthesis in the human brain and its clinical implications. Ann N Y Acad Sci. 2003. 10.1196/annals.1286.007. 10.1196/annals.1286.007 [DOI] [PubMed] [Google Scholar]
- 11.Wyrwoll CS, Holmes MC, Seckl JR. 11β-hydroxysteroid dehydrogenases and the brain: from zero to hero, a decade of progress. Front Neuroendocrinol. 2011. 10.1016/j.yfrne.2010.12.001. 10.1016/j.yfrne.2010.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobsen BM, Horwitz KB. Progesterone receptors, their isoforms and progesterone regulated transcription. Mol Cell Endocrinol. 2012. 10.1016/j.mce.2011.09.016. 10.1016/j.mce.2011.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuhl H. Pharmacology of progestins. Basic aspects-progesterone derivatives. Menopause Rev. 2001;6:9–16. [Google Scholar]
- 14.Kudwa AE, Rissman EF. Double oestrogen receptor alpha and beta knockout mice reveal differences in neural oestrogen-mediated progestin receptor induction and female sexual behaviour. J Neuroendocrinol. 2003;15:978–83. 10.1046/j.1365-2826.2003.01089.x [DOI] [PubMed] [Google Scholar]
- 15.Yu K, Huang ZY, Xu XL, Li J, Fu XW, Deng SL. Estrogen receptor function: impact on the human endometrium. Front Endocrinol (Lausanne). 2022. 10.3389/fendo.2022.827724. 10.3389/fendo.2022.827724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Acharya KD, Finkelstein SD, Bless EP, Nettles SA, Mulac-Jericevic B, Conneely OM, Mani SK, Tetel MJ. Estradiol preferentially induces progestin Receptor-A (PR-A) over PR-B in cells expressing nuclear receptor coactivators in the female mouse hypothalamus. eNeuro. 2015. 10.1523/ENEURO.0012-15.2015. [DOI] [PMC free article] [PubMed]
- 17.Thomas P, Pang Y. Membrane progesterone receptors: evidence for neuroprotective, neurosteroid signaling and neuroendocrine functions in neuronal cells. Neuroendocrinology. 2012. 10.1159/000339822. 10.1159/000339822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo M, Zhang C, Wang Y, Feng L, Wang Z, Niu W, Du X, Tang W, Li Y, Wang C, Chen Z. Progesterone receptor membrane component 1 mediates Progesterone-Induced suppression of Oocyte Meiotic Prophase I and primordial folliculogenesis. Sci Rep. 2016. 10.1038/srep36869. 10.1038/srep36869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maurice T, Urani A, Phan VL, Romieu P. The interaction between neuroactive steroids and the sigma1 receptor function: behavioral consequences and therapeutic opportunities. Brain Res Brain Res Rev. 2001. 10.1016/S0165-0173(01)00112-6. 10.1016/S0165-0173(01)00112-6 [DOI] [PubMed] [Google Scholar]
- 20.Kliewer SA, Goodwin B, Willson TM. The nuclear pregnane X receptor: a key regulator of xenobiotic metabolism. Endocr Rev. 2002. 10.1210/er.2001-0038. 10.1210/er.2001-0038 [DOI] [PubMed] [Google Scholar]
- 21.Baulieu EE, Schumacher M. Progesterone as a neuroactive neurosteroid, with special reference to the effect of progesterone on myelination. Hum Reprod. 2000. 10.1093/humrep/15.suppl_1.1. 10.1093/humrep/15.suppl_1.1 [DOI] [PubMed] [Google Scholar]
- 22.Holmberg E, Sjöstedt J, Malinina E, Johansson M, Turkmen S, Ragagnin G, Lundqvist A, Löfgren M, Jaukkuri L, Bixo M, Bäckström T. Allopregnanolone involvement in feeding regulation, overeating and obesity. Front Neuroendocrinol. 2018. 10.1016/j.yfrne.2017.07.002. 10.1016/j.yfrne.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 23.Antoniou-Tsigkos A, Macut D, Mastorakos G. Physiopathology, diagnosis, and treatment of secondary female hypogonadism. In: Casanueva F, Ghigo E, editors. Hypothalamic-pituitary diseases. Endocrinology. Cham: Springer; 2018. 10.1007/978-3-319-44444-4_9. [Google Scholar]
- 24.Patel B, Elguero S, Thakore S, Dahoud W, Bedaiwy M, Mesiano S. Role of nuclear progesterone receptor isoforms in uterine pathophysiology. Hum Reprod Update. 2015. 10.1093/humupd/dmu056. 10.1093/humupd/dmu056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang S, Thiel KW, Leslie KK. Progesterone: the ultimate endometrial tumor suppressor. Trends Endocrinol Metab. 2011. 10.1016/j.tem.2011.01.005. 10.1016/j.tem.2011.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stanczyk FZ, Hapgood JP, Winer S, Mishell DR Jr. Progestogens used in postmenopausal hormone therapy: differences in their pharmacological properties, intracellular actions, and clinical effects. Endocr Rev. 2013. 10.1210/er.2012-1008. 10.1210/er.2012-1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prior JC, Seifert-Klauss VR, Giustini D, Adachi JD, Kalyan S, Goshtasebi A. Estrogen-progestin therapy causes a greater increase in spinal bone mineral density than estrogen therapy - a systematic review and meta-analysis of controlled trials with direct randomization. J Musculoskelet Neuronal Interact. 2017;17:146–54. [PMC free article] [PubMed] [Google Scholar]
- 28.Poulin R, Baker D, Poirier D, Labrie F. Androgen and glucocorticoid receptor-mediated inhibition of cell proliferation by medroxyprogesterone acetate in ZR-75-1 human breast cancer cells. Breast Cancer Res Treat. 1989;13:161–72. 10.1007/BF01806528 [DOI] [PubMed] [Google Scholar]
- 29.Topper YJ, Freeman CS. Multiple hormone interactions in the developmental biology of the mammary gland. Physiol Rev. 1980. 10.1152/physrev.1980.60.4.1049. 10.1152/physrev.1980.60.4.1049 [DOI] [PubMed] [Google Scholar]
- 30.Navarrete MA, Maier CM, Falzoni R, Quadros LG, Lima GR, Baracat EC, Nazário AC. Assessment of the proliferative, apoptotic and cellular renovation indices of the human mammary epithelium during the follicular and luteal phases of the menstrual cycle. Breast Cancer Res. 2005. 10.1186/bcr994. 10.1186/bcr994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szmuilowicz ED, Adler GK, Williams JS, Green DE, Yao TM, Hopkins PN, Seely EW. Relationship between aldosterone and progesterone in the human menstrual cycle. J Clin Endocrinol Metab. 2006. 10.1210/jc.2006-1154. 10.1210/jc.2006-1154 [DOI] [PubMed] [Google Scholar]
- 32.Kalkhoff RK. Metabolic effects of progesterone. Am J Obstet Gynecol. 1982. 10.1016/S0002-9378(16)32480-2. 10.1016/S0002-9378(16)32480-2 [DOI] [PubMed] [Google Scholar]
- 33.Raine-Fenning NJ, Brincat MP, Muscat-Baron Y. Skin aging and menopause: implications for treatment. Am J Clin Dermatol. 2003. 10.2165/00128071-200304060-00001. 10.2165/00128071-200304060-00001 [DOI] [PubMed] [Google Scholar]
- 34.Händel P, Wahlström J. Digital contraceptives based on basal body temperature measurements. Biomed Signal Process Control. 2019. 10.1016/j.bspc.2019.04.019. 10.1016/j.bspc.2019.04.019 [DOI] [Google Scholar]
- 35.Pan DS, Liu WG, Yang XF, Cao F. Inhibitory effect of progesterone on inflammatory factors after experimental traumatic brain injury. Biomed Environ Sci. 2007;20:432–8. [PubMed] [Google Scholar]
- 36.Jiang C, Zuo F, Wang Y, Wan J, Yang Z, Lu H, Chen W, Zang W, Yang Q, Wang J. Progesterone exerts neuroprotective effects and improves long-term neurologic outcome after intracerebral hemorrhage in middle-aged mice. Neurobiol Aging. 2016. 10.1016/j.neurobiolaging.2016.02.029. 10.1016/j.neurobiolaging.2016.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malik S, Krishnaprasad K. Natural micronized progesterone sustained release (SR) and Luteal Phase: Role Redefined!! J Clin Diagn Res. 2016;10:QE01–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simon JA, Robinson DE, Andrews MC, Hildebrand JR 3rd, Rocci ML Jr, Blake RE, Hodgen GD. The absorption of oral micronized progesterone: the effect of food, dose proportionality, and comparison with intramuscular progesterone. Fertil Steril. 1993;60:26–33. 10.1016/S0015-0282(16)56031-2 [DOI] [PubMed] [Google Scholar]
- 39.Levine H, Watson N. Comparison of the pharmacokinetics of crinone 8% administered vaginally versus Prometrium administered orally in postmenopausal women(3). Fertil Steril. 2000. 10.1016/S0015-0282(99)00553-1. 10.1016/S0015-0282(99)00553-1 [DOI] [PubMed] [Google Scholar]
- 40.Ottosson UB. Oral progesterone and estrogen/progestogen therapy. Effects of natural and synthetic hormones on subfractions of HDL cholesterol and liver proteins. Acta Obstet Gynecol Scand Suppl. 1984;127:1–37. 10.3109/00016348409157016 [DOI] [PubMed] [Google Scholar]
- 41.Padwick ML, Endacott J, Matson C, Whitehead MI. Absorption and metabolism of oral progesterone when administered twice daily. Fertil Steril. 1986;46:402–7. 10.1016/S0015-0282(16)49576-2 [DOI] [PubMed] [Google Scholar]
- 42.Morville R, Dray F, Reynier J, Barrat J. Biodisponibilité De La progestérone naturelle administrée par voie orale. Mesure des concentrations du stéroïde dans le plasma, l’endomètre et le tissu mammaire [The bioavailability of natural progesterone given by mouth. Measurement of steroid concentrations in plasma, endometrium and breast tissue]. J Gynecol Obstet Biol Reprod (Paris). 1982;1:355–63. [PubMed] [Google Scholar]
- 43.de Lignières B. Oral micronized progesterone. Clin Ther. 1999. 10.1016/S0149-2918(00)88267-3. 10.1016/S0149-2918(00)88267-3 [DOI] [PubMed] [Google Scholar]
- 44.Ottoson UB, Carlstrom K, Damber JE, von Schoultz B. Serum levels of progesterone and some of its metabolites including deoxycorticosterone after oral and parenteral administration. Br J Obstet Gynaecol. 1984. 10.1111/j.1471-0528.1984.tb15086.x. 10.1111/j.1471-0528.1984.tb15086.x [DOI] [PubMed] [Google Scholar]
- 45.Nahoul K, Dehennin L, Jondet M, Roger M. Profiles of plasma estrogens, progesterone and their metabolites after oral or vaginal administration of estradiol or progesterone. Maturitas. 1993. 10.1016/0378-5122(93)90064-O. 10.1016/0378-5122(93)90064-O [DOI] [PubMed] [Google Scholar]
- 46.Bulletti C, de Ziegler D, Flamigni C, Giacomucci E, Polli V, Bolelli G, Franceschetti F. Targeted drug delivery in gynaecology: the first uterine pass effect. Hum Reprod. 1997. 10.1093/humrep/12.5.1073. 10.1093/humrep/12.5.1073 [DOI] [PubMed] [Google Scholar]
- 47.Wang H, Liu M, Fu Q, Deng C. Pharmacokinetics of hard micronized progesterone capsules via vaginal or oral route compared with soft micronized capsules in healthy postmenopausal women: a randomized open-label clinical study. Drug Des Devel Ther. 2019. 10.2147/DDDT.S204624. 10.2147/DDDT.S204624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shangold MM, Tomai TP, Cook JD, Jacobs SL, Zinaman MJ, Chin SY, Simon JA. Factors associated with withdrawal bleeding after administration of oral micronized progesterone in women with secondary amenorrhea. Fertil Steril. 1991;56:1040–7. 10.1016/S0015-0282(16)54714-1 [DOI] [PubMed] [Google Scholar]
- 49.Woods KS, Reyna R, Azziz R. Effect of oral micronized progesterone on androgen levels in women with polycystic ovary syndrome. Fertil Steril. 2002. 10.1016/S0015-0282(02)03119-9. 10.1016/S0015-0282(02)03119-9 [DOI] [PubMed] [Google Scholar]
- 50.Master-Hunter T, Heiman DL. Amenorrhea: evaluation and treatment. Am Fam Physician. 2006;73:1374–82. [PubMed] [Google Scholar]
- 51.Livadas S, Boutzios G, Economou F, Alexandraki K, Xyrafis X, Christou M, Zerva A, Karachalios A, Tantalaki E, Diamanti-Kandarakis E. The effect of oral micronized progesterone on hormonal and metabolic parameters in anovulatory patients with polycystic ovary syndrome. Fertil Steril. 2010. 10.1016/j.fertnstert.2009.02.073. 10.1016/j.fertnstert.2009.02.073 [DOI] [PubMed] [Google Scholar]
- 52.Fritz MA, Speroff L. Amenorrhea. Clinical gynecologic endocrinology and infertility. 8th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 53.Gordon CM, Ackerman KE, Berga SL, Kaplan JR, Mastorakos G, Misra M, Murad MH, Santoro NF, Warren MP. Functional hypothalamic amenorrhea: an endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017. 10.1210/jc.2017-00131. 10.1210/jc.2017-00131 [DOI] [PubMed] [Google Scholar]
- 54.Nakamura S, Douchi T, Oki T, Ijuin H, Yamamoto S, Nagata Y. Relationship between sonographic endometrial thickness and progestin-induced withdrawal bleeding. Obstet Gynecol. 1996. 10.1016/0029-7844(96)00016-6. 10.1016/0029-7844(96)00016-6 [DOI] [PubMed] [Google Scholar]
- 55.Practice Committee of American Society for Reproductive Medicine. Current evaluation of amenorrhea. Fertil Steril. 2008;90:219–25. 10.1016/j.fertnstert.2008.08.038 [DOI] [PubMed] [Google Scholar]
- 56.Nezi M, Christopoulos P, Paltoglou G, Gryparis A, Bakoulas V, Deligeoroglou E, Creatsas G, Mastorakos G. Focus on BMI and subclinical hypothyroidism in adolescent girls first examined for amenorrhea or oligomenorrhea. The emerging role of polycystic ovary syndrome. J Pediatr Endocrinol Metab. 2016. 10.1515/jpem-2015-0312. 10.1515/jpem-2015-0312 [DOI] [PubMed] [Google Scholar]
- 57.Marsh CA, Grimstad FW. Primary amenorrhea: diagnosis and management. Obstet Gynecol Surv. 2014;69:603–12. 10.1097/OGX.0000000000000111 [DOI] [PubMed] [Google Scholar]
- 58.Backeljauw P, Klein K. Sex hormone replacement therapy for individuals with Turner syndrome. Am J Med Genet C Semin Med Genet. 2019. 10.1002/ajmg.c.31685. 10.1002/ajmg.c.31685 [DOI] [PubMed] [Google Scholar]
- 59.Giordano R, Forno D, Lanfranco F, Manieri C, Ghizzoni L, Ghigo E. Metabolic and cardiovascular outcomes in a group of adult patients with Turner’s syndrome under hormonal replacement therapy. Eur J Endocrinol. 2011. 10.1530/EJE-11-0002. 10.1530/EJE-11-0002 [DOI] [PubMed] [Google Scholar]
- 60.Federici S, Goggi G, Quinton R, Giovanelli L, Persani L, Cangiano B, Bonomi M. New and Consolidated Therapeutic Options for Pubertal Induction in Hypogonadism: In-depth review of the literature. Endocr Rev. 2022;43:824–51. 10.1210/endrev/bnab043 [DOI] [PubMed] [Google Scholar]
- 61.Mathez ALG, Monteagudo PT, do Nascimento Verreschi IT, Dias-da-Silva MR. Levonorgestrel correlates with less weight gain than other progestins during hormonal replacement therapy in Turner Syndrome patients. Sci Rep. 2020. 10.1038/s41598-020-64992-4. 10.1038/s41598-020-64992-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Klein KO, Rosenfield RL, Santen RJ, Gawlik AM, Backeljauw PF, Gravholt CH, Sas TCJ, Mauras N. Estrogen replacement in Turner Syndrome: Literature Review and practical considerations. J Clin Endocrinol Metab. 2018. 10.1210/jc.2017-02183. 10.1210/jc.2017-02183 [DOI] [PubMed] [Google Scholar]
- 63.Critchley HO, Chard T, Lieberman BA, Buckley CH, Anderson DC. Serum PP14 levels in a patient with Turner’s syndrome pregnant after frozen embryo transfer. Hum Reprod. 1990. 10.1093/oxfordjournals.humrep.a137082. 10.1093/oxfordjournals.humrep.a137082 [DOI] [PubMed] [Google Scholar]
- 64.Prior JC, Vigna YM, Barr SI, Rexworthy C, Lentle BC. Cyclic medroxyprogesterone treatment increases bone density: a controlled trial in active women with menstrual cycle disturbances. Am J Med. 1994;96:521–30. 10.1016/0002-9343(94)90092-2 [DOI] [PubMed] [Google Scholar]
- 65.Prior JC. Adaptive, reversible, hypothalamic reproductive suppression: more than functional hypothalamic amenorrhea. Front Endocrinol (Lausanne). 2022;13:893889. 10.3389/fendo.2022.893889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Munro MG, Critchley HOD, Fraser IS, FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet. 2018. 10.1002/ijgo.12666. 10.1002/ijgo.12666 [DOI] [PubMed] [Google Scholar]
- 67.Munro MG, Critchley HO, Broder MS, Fraser IS, FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011. 10.1016/j.ijgo.2010.11.011. 10.1016/j.ijgo.2010.11.011 [DOI] [PubMed] [Google Scholar]
- 68.ACOG Committee on Adolescent Health Care. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Obstet Gynecol. 2006;108:1323–8. ACOG Committee Opinion 349, November 2006. [DOI] [PubMed]
- 69.Casablanca Y. Management of dysfunctional uterine bleeding. Obstet Gynecol Clin North Am. 2008. 10.1016/j.ogc.2008.03.001. 10.1016/j.ogc.2008.03.001 [DOI] [PubMed] [Google Scholar]
- 70.Management of abnormal uterine bleeding associated with ovulatory dysfunction. Practice Bulletin 136. American College of Obstetricians and gynecologists. Obstet Gynecol. 2013;122:176–85. [DOI] [PubMed] [Google Scholar]
- 71.Deligeoroglou E, Karountzos V, Creatsas G. Abnormal uterine bleeding and dysfunctional uterine bleeding in pediatric and adolescent gynecology. Gynecol Endocrinol. 2013. 10.3109/09513590.2012.705384. 10.3109/09513590.2012.705384 [DOI] [PubMed] [Google Scholar]
- 72.Santos M, Hendry D, Sangi-Haghpeykar H, Dietrich JE. Retrospective review of norethindrone use in adolescents. J Pediatr Adolesc Gynecol. 2014. 10.1016/j.jpag.2013.09.002. 10.1016/j.jpag.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 73.Bradley LD, Gueye NA. The medical management of abnormal uterine bleeding in reproductive-aged women. Am J Obstet Gynecol. 2016. 10.1016/j.ajog.2015.07.044. 10.1016/j.ajog.2015.07.044 [DOI] [PubMed] [Google Scholar]
- 74.Benetti-Pinto CL, Rosa-E-Silva ACJS, Yela DA. Soares Júnior JM. Abnormal uterine bleeding. Rev Bras Ginecol Obstet. 2017;39:358–68. 10.1055/s-0037-1603807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Elmaoğulları S, Aycan Z. Abnormal uterine bleeding in adolescents. J Clin Res Pediatr Endocrinol. 2018;10(3):191–7. 10.4274/jcrpe.0014. 10.4274/jcrpe.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Karakus S, Kiran G, Ciralik H. Efficacy of micronised vaginal progesterone versus oral dydrogestrone in the treatment of irregular dysfunctional uterine bleeding: a pilot randomised controlled trial. Aust N Z J Obstet Gynaecol. 2009. 10.1111/j.1479-828X.2009.01093.x. 10.1111/j.1479-828X.2009.01093.x [DOI] [PubMed] [Google Scholar]
- 77.Palomba S, Santagni S, La Sala GB. Progesterone administration for luteal phase deficiency in human reproduction: an old or new issue? J Ovarian Res. 2015. 10.1186/s13048-015-0205-8. 10.1186/s13048-015-0205-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Orazov MR, Radzinskiy VE, Nosenko EN, Khamoshina MB, Lebedeva MG, Tokaeva ES, Barsegyan LK, Novginov DS, Zakirova YR, Minayeva AV. Combination therapeutic options in the treatment of the luteal phase deficiency. Gynecol Endocrinol. 2017. 10.1080/09513590.2017.1399695. 10.1080/09513590.2017.1399695 [DOI] [PubMed] [Google Scholar]
- 79.Biggs WS, Demuth RH. Premenstrual syndrome and premenstrual dysphoric disorder. Am Fam Physician. 2011;84:918–24. [PubMed] [Google Scholar]
- 80.Yonkers KA, O’Brien PMS, Eriksson E. Premenstrual syndrome. Lancet. 2008. 10.1016/S0140-6736(08)60527-9. 10.1016/S0140-6736(08)60527-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ford O, Lethaby A, Roberts H, Mol BW. Progesterone for premenstrual syndrome. Cochrane Database Syst Rev. 2012. 10.1002/14651858.CD003415.pub4. 10.1002/14651858.CD003415.pub4 [DOI] [PubMed] [Google Scholar]
- 82.Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med. 1998;338:209–16. 10.1056/NEJM199801223380401 [DOI] [PubMed] [Google Scholar]
- 83.Rapkin AJ, Winer SA. Premenstrual syndrome and premenstrual dysphoric disorder: quality of life and burden of illness. Expert Rev Pharmacoecon Outcomes Res. 2009. 10.1586/erp.09.14. 10.1586/erp.09.14 [DOI] [PubMed] [Google Scholar]
- 84.Majewska MD, Harrison NL, Schwartz RD, Barker JL, Paul SM. Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor. Science. 1986;232:1004–7. 10.1126/science.2422758 [DOI] [PubMed] [Google Scholar]
- 85.Klatzkin RR, Morrow AL, Light KC, Pedersen CA, Girdler SS. Associations of histories of depression and PMDD diagnosis with allopregnanolone concentrations following the oral administration of micronized progesterone. Psychoneuroendocrinology. 2006. 10.1016/j.psyneuen.2006.09.002. 10.1016/j.psyneuen.2006.09.002 [DOI] [PubMed] [Google Scholar]
- 86.Sundström I, Ashbrook D, Bäckström T. Reduced benzodiazepine sensitivity in patients with premenstrual syndrome: a pilot study. Psychoneuroendocrinology. 1997. 10.1016/S0306-4530(96)00035-2. 10.1016/S0306-4530(96)00035-2 [DOI] [PubMed] [Google Scholar]
- 87.Monteleone P, Luisi S, Tonetti A, Bernardi F, Genazzani AD, Luisi M, Petraglia F, Genazzani AR. Allopregnanolone concentrations and premenstrual syndrome. Eur J Endocrinol. 2000. 10.1530/eje.0.1420269. 10.1530/eje.0.1420269 [DOI] [PubMed] [Google Scholar]
- 88.de Lignieres B, Dennerstein L, Backstrom T. Influence of route of administration on progesterone metabolism. Maturitas. 1995;21:251–7. 10.1016/0378-5122(94)00882-8 [DOI] [PubMed] [Google Scholar]
- 89.Rosenfeld R, Livne D, Nevo O, Dayan L, Milloul V, Lavi S, Jacob G. Hormonal and volume dysregulation in women with premenstrual syndrome. Hypertension. 2008. 10.1161/HYPERTENSIONAHA.107.107136. 10.1161/HYPERTENSIONAHA.107.107136 [DOI] [PubMed] [Google Scholar]
- 90.Dennerstein L, Spencer-Gardner C, Gotts G, Brown JB, Smith MA, Burrows GD. Progesterone and the premenstrual syndrome: a double blind crossover trial. Br Med J (Clin Res Ed). 1985. 10.1136/bmj.290.6482.1617. 10.1136/bmj.290.6482.1617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Freeman EW, Rickels K, Sondheimer SJ, Polansky M. A double-blind trial of oral progesterone, alprazolam, and placebo in treatment of severe premenstrual syndrome. JAMA. 1995;274:51–7. 10.1001/jama.1995.03530010065036 [DOI] [PubMed] [Google Scholar]
- 92.Vanselow W, Dennerstein L, Greenwood KM, de Lignieres B. Effect of progesterone and its 5 alpha and 5 beta metabolites on symptoms of premenstrual syndrome according to route of administration. J Psychosom Obstet Gynaecol. 1996. 10.3109/01674829609025661. 10.3109/01674829609025661 [DOI] [PubMed] [Google Scholar]
- 93.Wyatt K, Dimmock P, Jones P, Obhrai M, O’Brien S. Efficacy of progesterone and progestogens in management of premenstrual syndrome: systematic review. BMJ. 2001. 10.1136/bmj.323.7316.776. 10.1136/bmj.323.7316.776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Geber H. Einege Daten Zur Pathologie Der Urticaria menstrationalis. Dermat Z. 1921;32:143. 10.1159/000248242 [DOI] [Google Scholar]
- 95.Itsekson AM, Yonit B, Ze’ev IH, Matitiyahu Z, Shmuel K. Safety and value of skin test to sex hormones and sex hormone sensitivity desensitization in women with premenstrual syndrome. World Allergy Organ J. 2019. 10.1016/j.waojou.2019.100041. 10.1016/j.waojou.2019.100041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz BO. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016. 10.1093/humrep/dew218. 10.1093/humrep/dew218 [DOI] [PubMed] [Google Scholar]
- 97.DeUgarte CM, Bartolucci AA, Azziz R. Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil Steril. 2005. 10.1016/j.fertnstert.2004.11.070. 10.1016/j.fertnstert.2004.11.070 [DOI] [PubMed] [Google Scholar]
- 98.Cassar S, Misso ML, Hopkins WG, Shaw CS, Teede HJ, Stepto NK. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic-hyperinsulinaemic clamp studies. Hum Reprod. 2016. 10.1093/humrep/dew243. 10.1093/humrep/dew243 [DOI] [PubMed] [Google Scholar]
- 99.Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016. 10.1210/er.2015-1104. 10.1210/er.2015-1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Unfer V, Casini ML, Marelli G, Costabile L, Gerli S, Di Renzo GC. Different routes of progesterone administration and polycystic ovary syndrome: a review of the literature. Gynecol Endocrinol. 2005. 10.1080/09513590500170049. 10.1080/09513590500170049 [DOI] [PubMed] [Google Scholar]
- 101.Blank SK, McCartney CR, Chhabra S, Helm KD, Eagleson CA, Chang RJ, Marshall JC. Modulation of gonadotropin-releasing hormone pulse generator sensitivity to progesterone inhibition in hyperandrogenic adolescent girls–implications for regulation of pubertal maturation. J Clin Endocrinol Metab. 2009. 10.1210/jc.2008-2606. 10.1210/jc.2008-2606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fiad TM, Cunningham SK, McKenna TJ. Role of progesterone deficiency in the development of luteinizing hormone and androgen abnormalities in polycystic ovary syndrome. Eur J Endocrinol. 1996. 10.1530/eje.0.1350335. 10.1530/eje.0.1350335 [DOI] [PubMed] [Google Scholar]
- 103.Eagleson CA, Gingrich MB, Pastor CL, Arora TK, Burt CM, Evans WS, Marshall JC. Polycystic ovarian syndrome: evidence that flutamide restores sensitivity of the gonadotropin-releasing hormone pulse generator to inhibition by estradiol and progesterone. J Clin Endocrinol Metab. 2000;85:4047–52. [DOI] [PubMed] [Google Scholar]
- 104.Foecking EM, Szabo M, Schwartz NB, Levine JE. Neuroendocrine consequences of prenatal androgen exposure in the female rat: absence of luteinizing hormone surges, suppression of progesterone receptor gene expression, and acceleration of the gonadotropin-releasing hormone pulse generator. Biol Reprod. 2005. 10.1095/biolreprod.105.039800. 10.1095/biolreprod.105.039800 [DOI] [PubMed] [Google Scholar]
- 105.Bagis T, Gokcel A, Zeyneloglu HB, Tarim E, Kilicdag EB, Haydardedeoglu B. The effects of short-term medroxyprogesterone acetate and micronized progesterone on glucose metabolism and lipid profiles in patients with polycystic ovary syndrome: a prospective randomized study. J Clin Endocrinol Metab. 2002. 10.1210/jc.2002-020294. 10.1210/jc.2002-020294 [DOI] [PubMed] [Google Scholar]
- 106.Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, Clore JN, Blackard WG. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991. 10.1210/jcem-72-1-83. 10.1210/jcem-72-1-83 [DOI] [PubMed] [Google Scholar]
- 107.McCartney CR, Marshall JC. CLINICAL PRACTICE. Polycystic ovary syndrome. N Engl J Med. 2016;375:54–64. 10.1056/NEJMcp1514916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Apparao KB, Lovely LP, Gui Y, Lininger RA, Lessey BA. Elevated endometrial androgen receptor expression in women with polycystic ovarian syndrome. Biol Reprod. 2002. 10.1095/biolreprod66.2.297. 10.1095/biolreprod66.2.297 [DOI] [PubMed] [Google Scholar]
- 109.Stanosz S, von Mach- Szczypinski J, Sieja K, Kooeciuszkiewicz J. Micronized estradiol and progesterone therapy in primary, preinvasive endometrial cancer (1A/G1) in young women with polycystic ovarian syndrome. J Clin Endocrinol Metab. 2014. 10.1210/jc.2014-1693. 10.1210/jc.2014-1693 [DOI] [PubMed] [Google Scholar]
- 110.Spritzer PM, Lisboa KO, Mattiello S, Lhullier F. Spironolactone as a single agent for long-term therapy of hirsute patients. Clin Endocrinol (Oxf). 2000;52:587–94. 10.1046/j.1365-2265.2000.00982.x [DOI] [PubMed] [Google Scholar]
- 111.Berga SL, Mortola JF, Girton L, Suh B, Laughlin G, Pham P, Yen SS. Neuroendocrine aberrations in women with functional hypothalamic amenorrhea. J Clin Endocrinol Metab. 1989. 10.1210/jcem-68-2-301. 10.1210/jcem-68-2-301 [DOI] [PubMed] [Google Scholar]
- 112.Marcus MD, Loucks TL, Berga SL. Psychological correlates of functional hypothalamic amenorrhea. Fertil Steril. 2001. 10.1016/S0015-0282(01)01921-5. 10.1016/S0015-0282(01)01921-5 [DOI] [PubMed] [Google Scholar]
- 113.Weiss Kelly AK, Hecht S. Council on sports Medicine and Fitness. The female athlete triad. Pediatrics. 2016. 10.1542/peds.2016-0922. 10.1542/peds.2016-0922 [DOI] [PubMed] [Google Scholar]
- 114.Caronia LM, Martin C, Welt CK, Sykiotis GP, Quinton R, Thambundit A, Avbelj M, Dhruvakumar S, Plummer L, HughesVA, Seminara SB, Boepple PA, Sidis Y, Crowley WF Jr, Martin KA, Hall JE, Pitteloud N. A genetic basis for functional hypothalamic amenorrhea. N Engl J Med. 2011;364:215–25. 10.1056/NEJMoa0911064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, Toppari J, Zoeller RT. EDC-2: the Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr Rev. 2015. 10.1210/er.2015-1010. 10.1210/er.2015-1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cobb KL, Bachrach LK, Sowers M, Nieves J, Greendale GA, Kent KK, Brown BWJr, Pettit K, Harper DM, Kelsey JL. The effect of oral contraceptives on bone mass and stress fractures in female runners. Med Sci Sports Exerc. 2007;39:1464–73. 10.1249/mss.0b013e318074e532 [DOI] [PubMed] [Google Scholar]
- 117.Misra M, Katzman D, Miller KK, Mendes N, Snelgrove D, Russell M, Goldstein MA, Ebrahimi S, Clauss L, Weigel T, Mickley D, Schoenfeld DA, Herzog DB, Klibanski A. Physiologic estrogen replacement increases bone density in adolescent girls with anorexia nervosa. J Bone Min Res. 2011;26:2430–8. 10.1002/jbmr.447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nelson LM. Clinical practice. Primary ovarian insufficiency. N Engl J Med. 2009;360:606–14. 10.1056/NEJMcp0808697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Coulam CB, Adamson SC, Annegers JF. Incidence of premature ovarian failure. Obstet Gynecol. 1986;67:604–6. [PubMed] [Google Scholar]
- 120.Bompoula MS, Valsamakis G, Neofytou S, Messaropoulos P, Salakos N, Mastorakos G, Kalantaridou SN. Demographic, clinical and hormonal characteristics of patients with premature ovarian insufficiency and those of early menopause: data from two tertiary premature ovarian insufficiency centers in Greece. Gynecol Endocrinol. 2020. 10.1080/09513590.2020.1739266. 10.1080/09513590.2020.1739266 [DOI] [PubMed] [Google Scholar]
- 121.Committee opinion no. 605: primary ovarian insufficiency in adolescents and young women. Obstet Gynecol. 2014;124:193–7. [DOI] [PubMed]
- 122.Webber L, Davies M, Anderson R, Bartlett J, Braat D, Cartwright B, Cifkova R, de Muinck Keizer-Schrama S, Hogervorst E, Janse F, Liao L, Vlaisavljevic V, Zillikens C, Vermeulen N. ESHRE Guideline: management of women with premature ovarian insufficiency. European Society for Human Reproduction and Embryology (ESHRE) Guideline Group on POI. Hum Reprod. 2016. 10.1093/humrep/dew027. 10.1093/humrep/dew027 [DOI] [PubMed] [Google Scholar]
- 123.Committee Opinion No. 698: hormone therapy in primary ovarian insufficiency. Obstet Gynecol. 2017;129:134–41. 10.1097/AOG.0000000000002044 [DOI] [PubMed] [Google Scholar]
- 124.Mittal M, Savvas M, Arya R, McEniery C, Narvekar N, Cardozo L, Panay N, Hamoda H. A randomised controlled trial comparing the effects of micronized progesterone to medroxyprogesterone acetate on cardiovascular health, lipid metabolism and the coagulation cascade in women with premature ovarian insufficiency: study protocol and review of the literature. Menopause Int. 2013. 10.1177/1754045313503635. 10.1177/1754045313503635 [DOI] [PubMed] [Google Scholar]
- 125.Mittal M, Chitongo P, Supramaniam PR, Cardozo L, Savvas M, Panay N, Arya R, Hamoda H. The effect of micronized progesterone and medroxyprogesterone acetate in combination with transdermal estradiol on hemostatic biomarkers in postmenopausal women diagnosed with POI and early menopause: a randomized trial. Menopause. 2022;29:580–9. 10.1097/GME.0000000000001944 [DOI] [PubMed] [Google Scholar]
- 126.Mittal M, McEniery C, Supramaniam PR, Cardozo L, Savvas M, Panay N, Hamoda H. Impact of micronised progesterone and medroxyprogesterone acetate in combination with transdermal oestradiol on cardiovascular markers in women diagnosed with premature ovarian insufficiency or an early menopause: a randomised pilot trial. Maturitas. 2022. 10.1016/j.maturitas.2022.01.012. 10.1016/j.maturitas.2022.01.012 [DOI] [PubMed] [Google Scholar]
- 127.Mittal M, Panay N, Supramaniam PR, Savvas M, Cardozo L, Hamoda H. A direct comparison of women’s perceptions and acceptability of micronised progesterone and medroxyprogesterone acetate in combination with transdermal oestradiol in the management of young postmenopausal women, under 45 years of age. Post Reprod Health. 2020. 10.1177/2053369120960960. 10.1177/2053369120960960 [DOI] [PubMed] [Google Scholar]
- 128.Langrish JP, Mills NL, Bath LE, Warner P, Webb DJ, Kelnar CJ, Critchley HOD, Newby DE, Wallace WH. Cardiovascular effects of physiological and standard sex steroid replacement regimens in premature ovarian failure. Hypertension. 2009. 10.1161/HYPERTENSIONAHA.108.126516. 10.1161/HYPERTENSIONAHA.108.126516 [DOI] [PubMed] [Google Scholar]
- 129.Fatemi HM, Bourgain C, Donoso P, Blockeel C, Papanikolaou EG, Popovic-Todorovic B, Devroey P. Effect of oral administration of dydrogestrone versus vaginal administration of natural micronized progesterone on the secretory transformation of endometrium and luteal endocrine profile in patients with premature ovarian failure: a proof of concept. Hum Reprod. 2007. 10.1093/humrep/del520. 10.1093/humrep/del520 [DOI] [PubMed] [Google Scholar]
- 130.Bourgain C, Devroey P, Van Waesberghe L, Smitz J, Van Steirteghem AC. Effects of natural progesterone on the morphology of the endometrium in patients with primary ovarian failure. Hum Reprod. 1990. 10.1093/oxfordjournals.humrep.a137138. 10.1093/oxfordjournals.humrep.a137138 [DOI] [PubMed] [Google Scholar]
- 131.Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, de Villiers TJ. STRAW + 10 Collaborative Group. Executive summary of the stages of Reproductive Aging workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012. 10.1210/jc.2011-3362. 10.1210/jc.2011-3362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.O’Connor KA, Ferrell RJ, Brindle E, Shofer J, Holman DJ, Miller RC, Schechter DE, Singer B, Weinstein M. Total and unopposed estrogen exposure across stages of the transition to menopause. Cancer Epidemiol Biomarkers Prev. 2009. 10.1158/1055-9965.EPI-08-0996. 10.1158/1055-9965.EPI-08-0996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Stefanick ML. Estrogens and progestins: background and history, trends in use, and guidelines and regimens approved by the US Food and Drug Administration. Am J Med. 2005. 10.1016/j.amjmed.2005.09.059. 10.1016/j.amjmed.2005.09.059 [DOI] [PubMed] [Google Scholar]
- 134.Notelovitz M, Lenihan JP, McDermott M, Kerber IJ, Nanavati N, Arce J. Initial 17beta-estradiol dose for treating vasomotor symptoms. Obstet Gynecol. 2000. 10.1016/S0029-7844(99)00643-2. 10.1016/S0029-7844(99)00643-2 [DOI] [PubMed] [Google Scholar]
- 135.Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH. Classification and pharmacology of progestins. Maturitas. 2008;61:171–80. 10.1016/j.maturitas.2008.11.013 [DOI] [PubMed] [Google Scholar]
- 136.Sriprasert I, Hodis HN, Karim R, Stanczyk FZ, Shoupe D, Henderson VW, Mack WJ. Differential Effect of plasma estradiol on subclinical atherosclerosis progression in early vs late postmenopause. J Clin Endocrinol Metab. 2019;104:293–300. 10.1210/jc.2018-01600. 10.1210/jc.2018-01600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Park CW, Lim SJ, Moon YW, Choi SH, Shin MH, Min YK, Yoon BK, Park YS. Fracture recurrence in hip fracture with menopausal hormone therapy versus risedronate: a clinical trial. Climacteric. 2021;24:408–14. 10.1080/13697137.2021. 10.1080/13697137.2021 [DOI] [PubMed] [Google Scholar]
- 138.Prior JC. Perimenopause: the complex endocrinology of the menopausal transition. Endocr Rev. 1998;19:397–428. 10.1210/edrv.19.4.0341 [DOI] [PubMed] [Google Scholar]
- 139.Prior JC. The ageing female reproductive axis II: ovulatory changes with perimenopause. Novartis Found Symp. 2002;242:172–86. [PubMed]
- 140.Newton KM, Reed SD, LaCroix AZ, Grothaus LC, Ehrlich K, Guiltinan J. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo: a randomized trial. Ann Intern Med. 2006. 10.7326/0003-4819-145-12-200612190-00003. 10.7326/0003-4819-145-12-200612190-00003 [DOI] [PubMed] [Google Scholar]
- 141.Casper RF, Dodin S, Reid RL. The Effect of 20 µg Ethinyl Estradiol/1 mg norethindrone acetate (MinestrinTM), a low-dose oral contraceptive, on vaginal bleeding patterns, hot flashes, and quality of life in symptomatic Perimenopausal women. Menopause. 1997;4:139–47. [Google Scholar]
- 142.Santoro N, Teal S, Gavito C, Cano S, Chosich J, Sheeder J. Use of a levonorgestrel-containing intrauterine system with supplemental estrogen improves symptoms in perimenopausal women: a pilot study. Menopause. 2015;22:1301–7. 10.1097/GME.0000000000000557 [DOI] [PubMed] [Google Scholar]
- 143.Prior JC. Progesterone for symptomatic perimenopause treatment - progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obgyn. 2011;3:109–20. [PMC free article] [PubMed] [Google Scholar]
- 144.Prior JC, Cameron A, Fung M, Hitchcock CL, Janssen P, Lee T, Singer J. Oral micronized progesterone for perimenopausal night sweats and hot flushes a phase III Canada-wide randomized placebo-controlled 4 month trial. Sci Rep. 2023. 10.1038/s41598-023-35826-w. 10.1038/s41598-023-35826-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kostova P, Zlatkov V. Clinical study on the effect of vaginal administration of MP at dysfunctional uterine bleeding in premenopause. Akush Ginekol. 2009;48:3–7. [PubMed] [Google Scholar]
- 146.Tasci Y, Polat OG, Ozdogan S, Karcaaltincaba D, Seckin L, Erkaya S. Comparison of the efficacy of micronized progesterone and lynestrenol in treatment of simple endometrial hyperplasia without atypia. Arch Gynecol Obstet. 2014. 10.1007/s00404-014-3161-4. 10.1007/s00404-014-3161-4 [DOI] [PubMed] [Google Scholar]
- 147.Saarikoski S, Yliskoski M, Penttilä I. Sequential use of norethisterone and natural progesterone in pre-menopausal bleeding disorders. Maturitas. 1990. 10.1016/0378-5122(90)90086-L. 10.1016/0378-5122(90)90086-L [DOI] [PubMed] [Google Scholar]
- 148.Leeangkoonsathian E, Pantasri T, Chaovisitseree S, Morakot N. The effect of different progestogens on sleep in postmenopausal women: a randomized trial. Gynecol Endocrinol. 2017. 10.1080/09513590.2017.1333094. 10.1080/09513590.2017.1333094 [DOI] [PubMed] [Google Scholar]
- 149.Magos AL, Brewster E, Singh R, O’Dowd T, Brincat M, Studd JW. The effects of norethisterone in postmenopausal women on oestrogen replacement therapy: a model for the premenstrual syndrome. Br J Obstet Gynaecol. 1986;93:1290–6. 10.1111/j.1471-0528.1986.tb07868.x [DOI] [PubMed] [Google Scholar]
- 150.Gordon JL, Rubinow DR, Eisenlohr-Moul TA, Xia K, Schmidt PJ, Girdler SS. Efficacy of Transdermal Estradiol and Micronized Progesterone in the Prevention of depressive symptoms in the menopause transition: a Randomized Clinical Trial. JAMA Psychiatry. 2018;75:149–57. 10.1001/jamapsychiatry.2017.3998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gordon JL, Rubinow DR, Watkins L, Hinderliter AL, Caughey MC, Girdler SS. The Effect of Perimenopausal Transdermal Estradiol and Micronized progesterone on markers of risk for arterial disease. J Clin Endocrinol Metab. 2020. 10.1210/clinem/dgz262. 10.1210/clinem/dgz262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ambikairajah A, Walsh E, Cherbuin N. A review of menopause nomenclature. Reprod Health. 2022;19:29. 10.1186/s12978-022-01336-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ockene JK, Barad DH, Cochrane BB, Larson JC, Gass M, Wassertheil-Smoller S, Manson JE, Barnabei VM, Lane DS, Brzyski RG, Rosal MC, Wylie-Rosett J, Hays J. Symptom experience after discontinuing use of estrogen plus progestin. JAMA. 2005;294:183–93. 10.1001/jama.294.2.183 [DOI] [PubMed] [Google Scholar]
- 154.Grady D. Postmenopausal hormones-therapy for symptoms only. N Engl J Med. 2003;348:1835–7. 10.1056/NEJMp030038 [DOI] [PubMed] [Google Scholar]
- 155.Goodman NF, Cobin RH, Ginzburg SB, Katz IA, Woode DE. American Association of Clinical Endocrinologists.American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the diagnosis and treatment of menopause. Endocr Pract. 2011. 10.4158/EP.17.S6.1. 10.4158/EP.17.S6.1 [DOI] [PubMed] [Google Scholar]
- 156.Regidor PA. Progesterone in Peri- and postmenopause: a review. Geburtshilfe Frauenheilkd. 2014;74:995–1002. 10.1055/s-0034-1383297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gompel A. Micronized progesterone and its impact on the endometrium and breast vs. progestogens. Climacteric. 2012. 10.3109/13697137.2012.669584. 10.3109/13697137.2012.669584 [DOI] [PubMed] [Google Scholar]
- 158.Anagnostis P, Bitzer J, Cano A, Ceausu I, Chedraui P, Durmusoglu F, Erkkola R, Goulis DG, Hirschberg AL, Kiesel L, Lopes P, Pines A, van Trotsenburg M, Lambrinoudaki I, Rees M. Menopause symptom management in women with dyslipidemias: an EMAS clinical guide. Maturitas. 2020. 10.1016/j.maturitas.2020.03.007. 10.1016/j.maturitas.2020.03.007 [DOI] [PubMed] [Google Scholar]
- 159.Cuadros JL, Fernández-Alonso AM, Chedraui P, Cuadros AM, Sabatel RM, Pérez-López FR. Metabolic and hormonal parameters in post-menopausal women 10 years after transdermal oestradiol treatment, alone or combined to micronized oral progesterone. Gynecol Endocrinol. 2011. 10.3109/09513590.2010.487613. 10.3109/09513590.2010.487613 [DOI] [PubMed] [Google Scholar]
- 160.Prior JC, Elliott TG, Norman E, Stajic V, Hitchcock CL. Progesterone therapy, endothelial function and cardiovascular risk factors: a 3-month randomized, placebo-controlled trial in healthy early postmenopausal women. PLoS ONE. 2014;9:e84698. 10.1371/journal.pone.0084698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Casanova G, Spritzer PM. Effects of micronized progesterone added to non-oral estradiol on lipids and cardiovascular risk factors in early postmenopause: a clinical trial. Lipids Health Dis. 2012. 10.1186/1476-511X-11-133. 10.1186/1476-511X-11-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Harman SM, Black DM, Naftolin F, Brinton EA, Budoff MJ, Cedars MI, Hopkins PN, Lobo RA, Manson JE, Merriam GR, Miller VM, Neal-Perry G, Santoro N, Taylor HS, Vittinghoff E, Yan M, Hodis HN. Arterial imaging outcomes and cardiovascular risk factors in recently menopausal women: a randomized trial. Ann Intern Med. 2014. 10.7326/M14-0353. 10.7326/M14-0353 [DOI] [PubMed] [Google Scholar]
- 163.Gompel A. Progesterone and endometrial cancer. Best Pract Res Clin Obstet Gynaecol. 2020. 10.1016/j.bpobgyn.2020.05.003. 10.1016/j.bpobgyn.2020.05.003 [DOI] [PubMed] [Google Scholar]
- 164.Fitzpatrick LA, Pace C, Wiita B. Comparison of regimens containing oral micronized progesterone or medroxyprogesterone acetate on quality of life in postmenopausal woman: a cross-sectional study. J Womens Health Gend Based Med. 2000. 10.1089/15246090050020691. 10.1089/15246090050020691 [DOI] [PubMed] [Google Scholar]
- 165.L’Hermite M. Bioidentical menopausal hormone therapy: registered hormones (non-oral estradiol ± progesterone) are optimal. Climacteric. 2017. 10.1080/13697137.2017.1291607. 10.1080/13697137.2017.1291607 [DOI] [PubMed] [Google Scholar]
- 166.Hitchcock CL, Prior JC. Oral micronized progesterone for vasomotor symptoms–a placebo-controlled randomized trial in healthy postmenopausal women. Menopause. 2012;19:886–93. 10.1097/gme.0b013e318247f07a [DOI] [PubMed] [Google Scholar]
- 167.Prior JC, Hitchcock CL. Progesterone for hot flush and night sweat treatment–effectiveness for severe vasomotor symptoms and lack of withdrawal rebound. Gynecol Endocrinol. 2012. 10.3109/09513590.2012.705390. 10.3109/09513590.2012.705390 [DOI] [PubMed] [Google Scholar]
- 168.Di Carlo C, Sammartino A, Di Spiezio Sardo A, Tommaselli GA, Guida M, Mandato VD, D’Elia A, Nappi C. Bleeding patterns during continuous estradiol with different sequential progestogens therapy. Menopause. 2005;12:520–5. 10.1097/01.gme.0000178450.29377.c9 [DOI] [PubMed] [Google Scholar]
- 169.Pélissier C, Maroni M, Yaneva H, Brin S, Peltier-Pujol F, Jondet M. Chlormadinone acetate versus micronized progesterone in the sequential combined hormone replacement therapy of the menopause. Maturitas. 2001. 10.1016/S0378-5122(01)00170-0. 10.1016/S0378-5122(01)00170-0 [DOI] [PubMed] [Google Scholar]
- 170.Collins A, Landgren BM. Psychosocial factors associated with the use of hormonal replacement therapy in a longitudinal follow-up of Swedish women. Maturitas. 1997;28:1–9. 10.1016/s0378-5122(97)00063-7. 10.1016/s0378-5122(97)00063-7 [DOI] [PubMed] [Google Scholar]
- 171.Sturdee DW, Pines A, Archer DF, Baber RJ, Barlow D, Birkhäuser MH, Brincat M, Cardozo L, de Villiers TJ, Gambacciani M, Gompel AA, Henderson VW, Kluft C, Lobo RA, MacLennan AH, Marsden J, Nappi RE, Panay N, Pickar JH, Robinson D, Simon J, Sitruk-Ware RL, Stevenson JC. Updated IMS recommendations on postmenopausal hormone therapy and preventive strategies for midlife health. Climacteric. 2011. 10.3109/13697137.2011.570590. 10.3109/13697137.2011.570590 [DOI] [PubMed] [Google Scholar]
- 172.Schüssler P, Kluge M, Yassouridis A, Dresler M, Held K, Zihl J, Steiger A. Progesterone reduces wakefulness in sleep EEG and has no effect on cognition in healthy postmenopausal women. Psychoneuroendocrinology. 2008. 10.1016/j.psyneuen.2008.05.013. 10.1016/j.psyneuen.2008.05.013 [DOI] [PubMed] [Google Scholar]
- 173.Nolan BJ, Liang B, Cheung AS. Efficacy of Micronized Progesterone for Sleep: a systematic review and Meta-analysis of Randomized Controlled Trial Data. J Clin Endocrinol Metab. 2021. 10.1210/clinem/dgaa873. 10.1210/clinem/dgaa873 [DOI] [PubMed] [Google Scholar]
- 174.Pan Z, Wen S, Qiao X, Yang M, Shen X, Xu L. Different regimens of menopausal hormone therapy for improving sleep quality: a systematic review and meta-analysis. Menopause. 2022;29:627–35. 10.1097/GME.0000000000001945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Sherwin BB, Grigorova M. Differential effects of estrogen and micronized progesterone or medroxyprogesterone acetate on cognition in postmenopausal women. Fertil Steril. 2011. 10.1016/j.fertnstert.2011.05.079. 10.1016/j.fertnstert.2011.05.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Andréen L, Sundström-Poromaa I, Bixo M, Nyberg S, Bäckström T. Allopregnanolone concentration and mood-a bimodal association in postmenopausal women treated with oral progesterone. Psychopharmacology. 2006. 10.1007/s00213-006-0417-0. 10.1007/s00213-006-0417-0 [DOI] [PubMed] [Google Scholar]