The 2018 American Heart Association/American College of Cardiology Guideline on the Management of Blood Cholesterol recommended cholesterol-lowering medications in patients with clinical atherosclerotic cardiovascular disease (ASCVD) to achieve a goal of low-density lipoprotein cholesterol (LDL-C) <70 mg/dL.1 Age ≥65 years is one of the conditions that places patients at very high risk of future ASCVD events, and prior studies have shown that the benefits of LDL-C lowering extend to older adults with ASCVD.2 However, the proportion of older adults with ASCVD with LDL-C <70 mg/dL over time is unknown. Therefore, we used the National Health and Nutrition Examination Survey to examine the trends and the proportion of older adults with a history of myocardial infarction (MI) or stroke who have their LDL-C at goal.
We identified older adults, defined as age ≥65 years, from the 10 most recent cycles of the National Health and Nutrition Examination Survey (1999-2000 to 2017-2018) to provide data relevant to contemporary practice. We included all older adults with a history of MI or stroke who underwent testing for LDL-C. We excluded patients with liver disease. We accounted for the complex survey design and multiplied sampling weights in all our analyses to produce findings representative of the noninstitutionalized population in the United States. We stratified the cohort into patients with LDL-C level at goal (<70 mg/dL) and not at goal (≥70 mg/dL) and calculated the percentage of older adults with LDL-C level at goal for each of the survey cycles. We then evaluated the trend from the 1999-2000 cycle to the 2017-2018 cycle using the Cochrane-Armitage test.
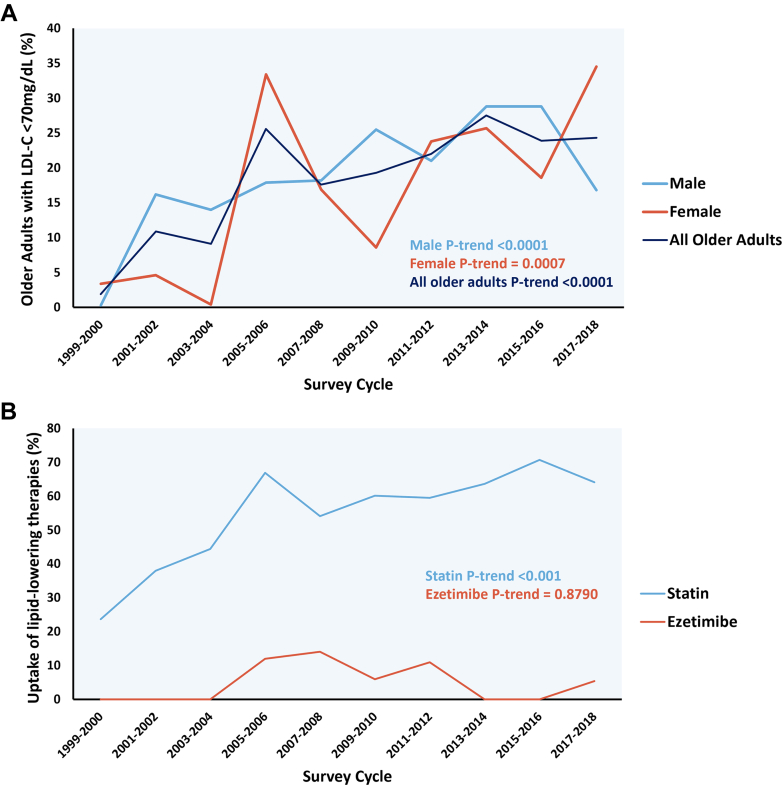
A total of 1,018 older adults with a history of MI (39.9%), stroke (49.3%), or both (10.8%) were included in the survey, nationally representing an extrapolated sample of 6,355,181 older adults. Among them, 1,245,411 (19.6%) older adults had LDL-C <70 mg/dL compared with 5,109,770 (80.4%) older adults who had LDL-C ≥70 mg/dL. The mean age was similar between the 2 groups (75.9 ± 0.6 years vs 75.4 ± 0.4 years, P = 0.152). The proportion of males (57.9% vs 56.7%, P = 0.779) and those with hypertension (75.4% vs 68.6%, P = 0.157) were also not different. Diabetes mellitus was more prevalent (42.9% vs 22.2%, P < 0.001) in older adults with LDL-C <70 mg/dL. Mean LDL-C was 56.6 ± 0.7 mg/dL in older adults with LDL-C level at goal compared with 112.5 ± 1.3 mg/dL in those with uncontrolled LDL-C levels. Statins (77.1% vs 51.9%, P < 0.001), but not ezetimibe (8.7% vs 5.4%, P = 0.206), were more frequently taken in older adults with LDL-C <70 mg/dL. An increasing trend of older adults who achieved LDL-C goal of <70 mg/dL was observed from 1999-2000 to 2017-2018 (1.9%-24.3%, P trend <0.0001) (Figure 1). Similarly, increasing trends were seen when stratified to male (0.3%-16.8%, P trend <0.0001) and female sex (3.4%-34.5%, P trend = 0.0007). An increasing trend of statin use was observed in older adults from 1999-2000 to 2017-2018 (P trend <0.0001).
Figure 1.
Trend of Older Adults Who Achieved a Goal of LDL-C <70 mg/dL and of Lipid-Lowering Therapy Use in Older Adults
(A) Trend of older adults who achieved a goal of LDL-C <70 mg/dL. (B) Trend of older adults taking lipid-lowering therapies. LDL-C = low-density lipoprotein cholesterol.
In this representative sample of older adults with a history of MI or stroke in the United States, we identified a persistent treatment gap in the achievement of LDL-C targets (<70 mg/dL). Despite the increasing trend of controlled LDL-C in older adults over the course of 2 decades, approximately 80% of this demographic still exhibited suboptimal LDL-C levels. This underscores a pronounced disparity between evidence and practice in lipid-lowering interventions for a particularly high-risk population.
Older adults face an elevated risk of major vascular events, which can lead to debilitating outcomes and contribute to disability, functional impairment, and a diminished quality of life. Despite uncertainty around the use of primary prevention lipid-lowering therapies (LLTs) in older adults, the use of LLTs for the secondary prevention of cardiovascular events in older adults is firmly established based on randomized controlled trial evidence.1,2 The improvement in statin use observed over time among older adults in the present study aligns with a large analysis of more than 500,000 MI hospitalizations that saw the high-intensity statin prescription fills nearly triple in older adults from 2011 to 2019.3 A meta-analysis including 244,090 patients from 29 trials demonstrated a substantial reduction in cardiovascular mortality (15%), MI (20%), and stroke (27%) per 1 mmol/L reduction in LDL-C in older patients.2
While lipid control in the United States has improved over time, significant gaps remain. The substandard control of LDL-C levels in older adults persists and may be attributed to multiple factors, encompassing geriatric complexities such as multimorbidity, frailty, cognitive impairment, polypharmacy, falls, and misperceptions about the risks associated with myalgia.4,5 Consequently, a conservative approach often characterizes their treatment. A multicenter retrospective cohort study of older adults with ASCVD revealed that less than half of older adults were on statins and were also less likely to be prescribed nonstatin therapies, including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors. 4 With regard to the misperception of adverse events, a study from the PALM (Patient and Provider Assessment of Lipid Management) registry demonstrated that older adults were less likely to experience adverse symptoms or myalgias specifically compared with younger counterparts. Additionally, older adults were less likely to receive high-intensity statin therapy.5 The present study provides further evidence for the undertreatment of lipids in a nationally representative cohort of older adults and underscores quality improvement projects to address the barriers contributing to the under-prescription of LLTs and/or suboptimal LDL-C levels.
Our study is subject to several limitations. The cross-sectional nature of the study design precludes definitive explanations for the causes behind the observed trends. We also lacked information on the adverse events, dosage, and duration of the prescribed LLT, as well as variables such as baseline cognitive function, polypharmacy, and frailty, which can influence prescription patterns.
Footnotes
Dr Damluji has received research funding from the Pepper Scholars Program of the Johns Hopkins University Claude D. Pepper Older Americans Independence Center funded by the National Institute on Aging P30-AG021334; and has received mentored patient-oriented research career development award from the National Heart, Lung, and Blood Institute K23-HL153771-01. Dr Nanna has received current research support from the American College of Cardiology Foundation supported by the George F. and Ann Harris Bellows Foundation, the Patient-Centered Outcomes Research Institute (PCORI), the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342), and the National Institute on Aging/National Institutes of Health from R03AG074067 (GEMSSTAR award); and also has served as a consultant for Heartflow, Novo Nordisk, and Merck. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 2.Gencer B., Marston N.A., Im K., et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2020;396:1637–1643. doi: 10.1016/S0140-6736(20)32332-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colantonio L.D., Wang Z., Chen L., et al. Trends in high-intensity statin therapy after myocardial infarction among U.S. adults, 2011-2019. J Am Coll Cardiol. 2022;79:1870–1872. doi: 10.1016/j.jacc.2022.02.049. [DOI] [PubMed] [Google Scholar]
- 4.Nanna M.G., Nelson A.J., Haynes K., et al. Lipid-lowering treatment among older patients with atherosclerotic cardiovascular disease. J Am Geriatr Soc. 2023;71:1243–1249. doi: 10.1111/jgs.18172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nanna M.G., Navar A.M., Wang T.Y., et al. Statin use and adverse effects among adults >75 years of age: insights from the patient and provider assessment of lipid Management (PALM) registry. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.008546. [DOI] [PMC free article] [PubMed] [Google Scholar]